- 1Department of Clinical Pharmacy, College of Pharmacy, Jouf University, Sakaka, Al-Jouf, Saudi Arabia
- 2Institute of Pharmacy, Lahore College for Women University, Lahore, Pakistan
- 3Institute of Pharmacy, Faculty of Pharmaceutical and Allied Health Sciences, Lahore College for Women University, Lahore, Pakistan
- 4Department of Biochemistry, College of Medicine, Imam Mohammad Ibn Saud Islamic University, Riyadh, Saudi Arabia
- 5Department of Medicinal Chemistry, Faculty of Pharmacy, Uppsala University, Uppsala, Sweden
- 6Department of Pharmacology, College of Pharmacy, Jouf University, Sakaka, Al-Jouf, Saudi Arabia
- 7Security Forces Hospital Program, Riyadh, Saudi Arabia
- 8Department of Clinical Pharmacy, College of Pharmacy, Taif University, Taif, Saudi Arabia
- 9Department of Clinical Pharmacy, College of Pharmacy, Prince Sattam Bin Abdulaziz University, Al-Kharj, Saudi Arabia
Background: The acceptance of vaccination against COVID-19 among parents of young children plays a significant role in controlling the current pandemic. A wide range of factors that influence vaccine hesitancy in adults has been reported worldwide, but less attention has been given to COVID-19 vaccination among children. Vaccine hesitancy is considered a major challenge in achieving herd immunity, and it is more challenging among parents as they remain deeply concerned about their child’s health. In this context, a systematic review of the current literature is inevitable to assess vaccine hesitancy among parents of young children to ensure a successful ongoing vaccination program.
Method: A systematic search of peer-reviewed English literature indexed in Google Scholar, PubMed, Embase, and Web of science was performed using developed keywords between 1 January 2020 and August 2022. This systematic review included only those studies that focused on parental concerns about COVID-19 vaccines in children up to 12 years without a diagnosis of COVID-19. Following PRISMA guidelines, a total of 108 studies were included. The quality appraisal of the study was performed by Newcastle–Ottawa Scale (NOS).
Results: The results of 108 studies depict that vaccine hesitancy rates differed globally with a considerably large number of factors associated with it. The highest vaccine hesitancy rates among parents were reported in a study from the USA (86.1%) and two studies from Saudi Arabia (>85%) and Turkey (89.6%). Conversely, the lowest vaccine hesitancy rates ranging from 0.69 and 2% were found in two studies from South Africa and Switzerland, respectively. The largest study (n = 227,740) was conducted in Switzerland while the smallest sample size (n = 12) was represented by a study conducted in the USA. The most commonly reported barriers to childhood vaccination were mothers’ lower education level (N = 46/108, 43%), followed by financial instability (N = 19/108, 18%), low confidence in new vaccines (N = 13/108, 12%), and unmonitored social media platforms (N = 5/108, 4.6%). These factors were significantly associated with vaccine refusal among parents. However, the potential facilitators for vaccine uptake among respondents who intended to have their children vaccinated include higher education level (N = 12/108, 11%), followed by information obtained through healthcare professionals (N = 9/108, 8.3%) and strong confidence in preventive measures taken by the government (N = 5/81, 4.6%).
Conclusion: This review underscores that parents around the globe are hesitant to vaccinate their kids against COVID-19. The spectrum of factors associated with vaccine hesitancy and uptake varies across the globe. There is a dire need to address vaccine hesitancy concerns regarding the efficacy and safety of approved vaccines. Local context is inevitable to take into account while developing programs to reduce vaccine hesitancy. There is a dire need to devise strategies to address vaccine hesitancy among parents through the identification of attributing factors.
Introduction
The COVID-19 pandemic resulted in serious disruptions in the healthcare system and economics across the globe. The SARS-CoV-2 infections ranged from 3 to 17 million daily worldwide from April 2020 to October 2021 (1, 2). This pandemic has considerable mortality reaching up to millions worldwide (3). As compared to adults, children present with mild flu-like symptoms but there is increasing evidence of complications, such as severe acute respiratory disorder and cardiac inflammation, due to the emergence of new variants (4–8). Tireless efforts have been undertaken to alleviate the disease spread and its impact nationwide. These include maintaining physical distances, wearing masks, limiting social contacts, and developing vaccines (9–13). Vaccines play a significant role in drastically reducing and completely eradicating vaccines preventable diseases (VPDs) (14). Initially, COVID-19 vaccines were prioritized for healthcare workers and high-risk groups, especially older people with multiple comorbidities (15, 16). However, the administration of vaccines in children is now considered inevitable owing to multisystem inflammatory syndrome reported in the children (3, 4).
Owing to the emergence of new variants with rapid transmissibility, a high vaccination uptake is needed among general population including children to ensure the achievement of herd immunity (17). The current situation necessitates the administration of COVID-19 vaccines in children, but still, vaccine hesitancy has become a global challenge (18). Although the vaccine hesitancy varies across the globe and is terrifyingly high in many regions encompassing substantial proportion of world’s population, the vaccination rate is below the average number required for herd immunity and rates of vaccination intentions are declining especially among parents of young children despite recent advances (19). “Parental vaccine hesitancy is defined as the delay in the acceptance or refusal of vaccines from parents of children despite their availability” (20). As parents are decision makers related to their children’s vaccination, reluctance or refusal to vaccinate their kids may result in developing VPDs. In particular, the most important factor influencing the decision-making on COVID-19 childhood vaccination includes parents’ knowledge and attitude. Lower knowledge would ultimately result in decreased acceptance (21, 22). The predominant factors reported to play a key role in parental vaccine hesitancy include social, cognitive, and contextual factors (23).
The primary focus of health authorities is to ensure a prosperous campaign among children regarding COVID-19 vaccination. However, the major hindrance toward the prospective and approved COVID-19 vaccination among children is linked to parental vaccine hesitancy as parents are actual decision makers. Parents’ attitude toward COVID-19 vaccination varies widely across geographical regions. The literature shows wide variations in vaccination hesitancy rates and factors associated with vaccine acceptability and hesitancy among parents. There is a dire need to systematically collect the available evidence to draw a firm conclusion from this scenario. To the best of our knowledge, till date there is no systematic review (SR) synthesizing the diverse information into a composite document on parenteral hesitancy toward COVID-19 vaccination from different regions across the globe. In this context, this SR was aimed to (1) check parents’ hesitancy toward children vaccination against COVID-19 and (2) ascertain the barriers and facilitators of vaccine uptake. The findings of this review will aid to map and understand the parental concern about the childhood COVID-19 vaccine and will underscore the areas of action plans.
Methods
Ethics
Since all the data were obtained from publicly available evidence, this study was exempted from ethics approval.
Review design
The PRISMA guidelines were followed to perform a systematic literature search (24). The framework of the current review is divided into five stages: (1) Identification of the research question. (2) Identification of relevant studies. (3) Study selection. (4) Data extraction. (5) Quality assessment. (6) Reporting of findings.
Stage 1: Identifying research questions
This systematic review is guided by the following questions: (1) What is the prevalence parental vaccine hesitancy toward childhood COVID-19 vaccines? (2) What are the barriers of childhood COVID-19 vaccines uptake? (3) What are the facilitators of childhood COVID-19 vaccines uptake?
Stage 2: Identifying relevant studies (eligibility criteria)
Information sources and search strategy
Two review authors performed an independent systematic search in Google scholar, PubMed, Web of Science, and EMBASE databases between 1 January 2020 and 30 August 2022. The keywords used to identify the relevant studies were “2019-nCoV” or “SARS-CoV-2” or “COVID-19” or “Coronavirus Disease,” and “vaccine hesitancy” or “vaccine uptake” or “vaccine acceptance” or “vaccine reluctance” or “vaccination” or “vaccination rate” or “vaccination readiness” or “vaccine acceptance” and “parents” or “parenteral” or “childhood” or “pediatrics” or “children.”
Study selection
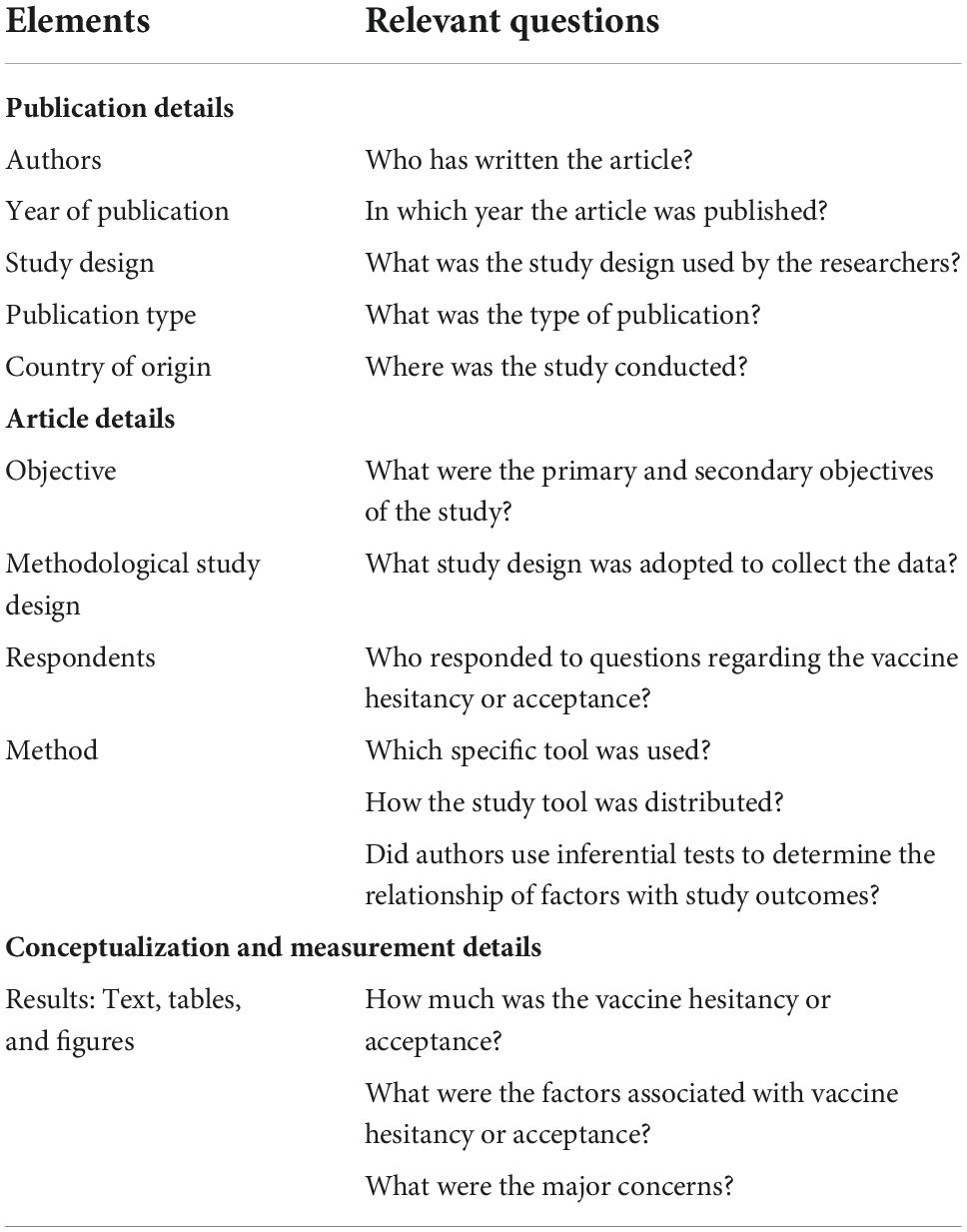
Eligible studies were selected according to research questions and Population–Concept–Context (PCC) framework proposed by Joanna Briggs Institute (JBI) as shown in Table 1. JBI reviews are aimed to provide unbiased and comprehensive synthesis of a large number of relevant studies. This systematic review included only those studies that focused on parental concerns about COVID-19 vaccines in children up to 12 years without a diagnosis of COVID-19. Studies in English language or English language translation were included due to the lack of financial and language resources although authors are in the view that English is not the universal language of science. The current review included a cross-sectional online survey, mixed methods, and observational studies. Gray literature and unpublished studies were not included. This review did not include letters, reports, documentaries, or editorials as these studies do not provide empirical evidence required to ascertain the answers to review questions.
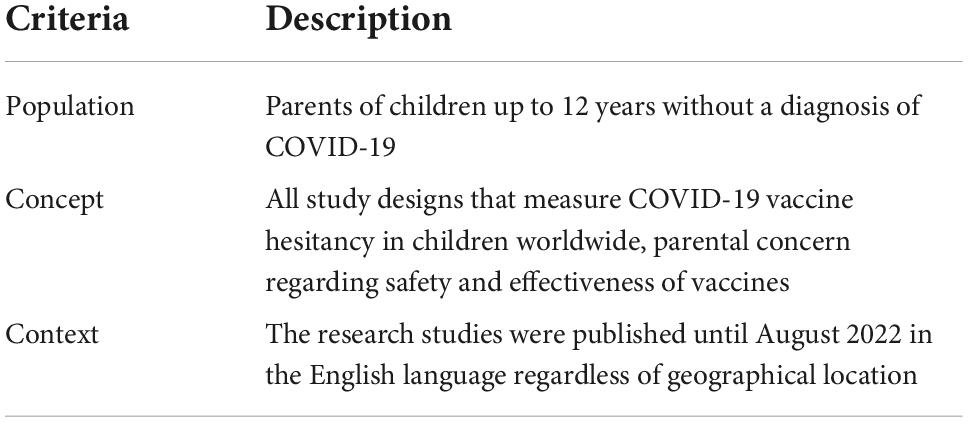
Table 1. PCC (Population, Concept, Context) framework to identify main concepts in review questions.
Inclusion and exclusion criteria
All the studies containing data on parents’ vaccine hesitancy of children up to 12 years without a diagnosis of COVID-19 were included, as vaccine hesitancy has been more pronounced among parents of children with compromised health conditions. Therefore, articles containing data on children with compromised health conditions, for example, cancer and attention-deficit/hyperactivity disorder (ADHD), were also included. We excluded studies with data on teenagers and adolescents. Studies that do not include data on parental concern about the COVID-19 vaccine in children or that have data on childhood vaccine hesitancy in other immunization programs were excluded.
Stage 3: Selection of relevant studies (search strategy)
The key terms for search strategy were collaboratively identified by two investigators (M.R and N.B). The authors also kept in mind sensitivity and specificity. The search strategy was developed by investigators focusing on four major concepts: COVID-19 vaccine hesitancy, childhood COVID-19, vaccine hesitancy, parental concern about COVID-19 vaccine hesitancy, barriers and facilitators of COVID-19 vaccine uptake. To achieve a comprehensive set of citations, the authors truncated necessary keywords and included relevant subject heading for each concept. The strategies were modified to ensure appropriateness for each database. The adopted search strategies along with databases are described earlier.
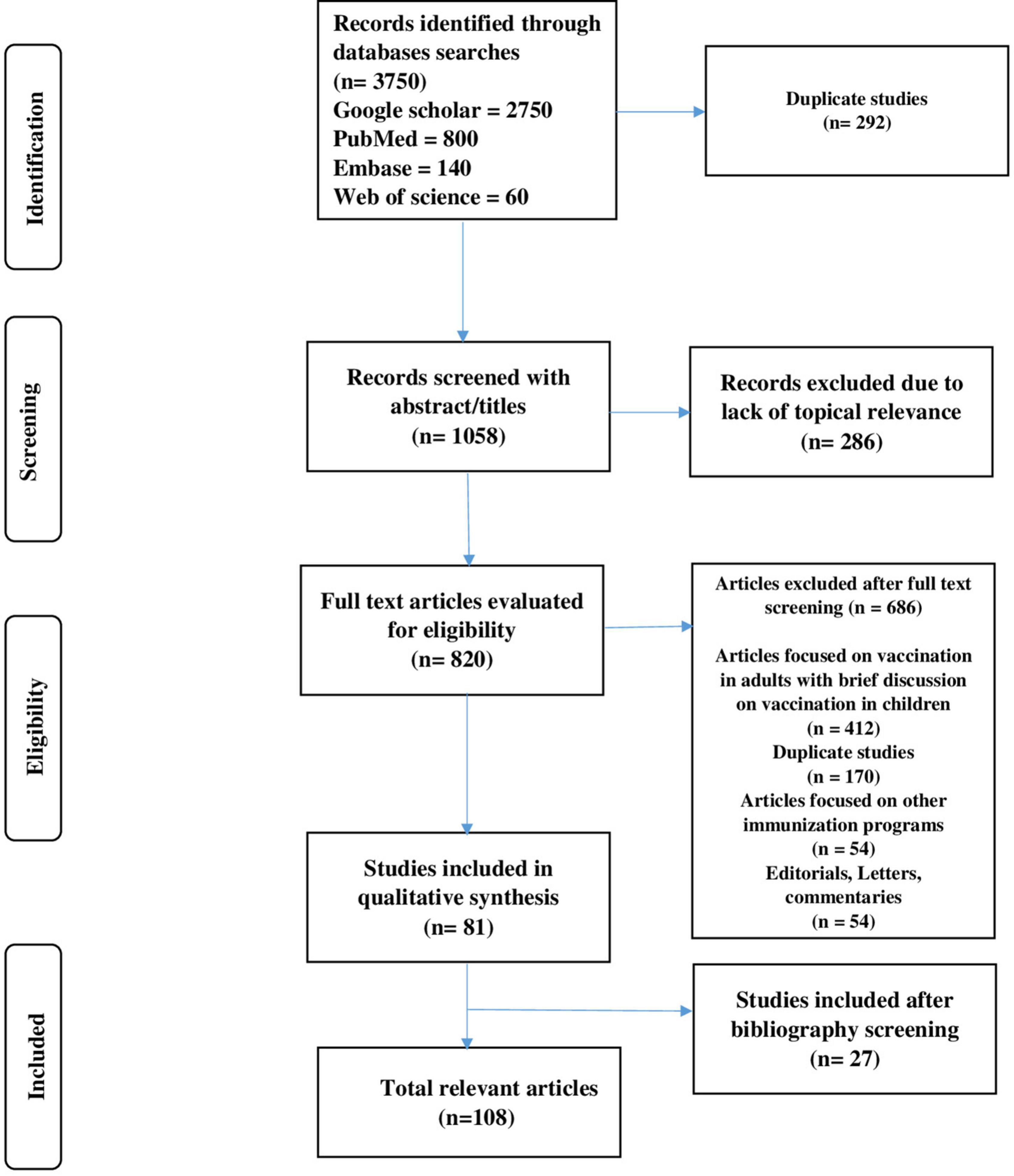
Metadata were collected and uploaded by a research team from all identified records to Endnote, and subsequently, duplicates were removed. The review team used two-stage screening due to a large number of studies. The irrelevant articles were removed from the titles and abstracts, while the second stage comprised of reviewing full-text articles. Furthermore, irrelevant articles were removed from the study sample after reading each article. Data extraction was performed from the remaining articles with relevance to the study question. A total of 27 studies were included after the bibliographic screening. Two reviewers (MR and MHB) collectively searched the data, and disagreement was resolved by the third reviewer (Y.H.K). A summary of the study selection process has been given in the PRISMA flowchart (Figure 1).
Stage 4: Data extraction
Data extraction table was created in Microsoft word to ensure that the relevant information is systematically extracted in the table. Data from all relevant publications containing the following information were recorded: (1) Authors. (2) Publication year and duration of study. (3) Number of respondents. (4) Parental concern. (5) Vaccine hesitancy/vaccine acceptance percentages. (6) Barriers and facilitators of vaccine uptake (Table 2). Few modifications were also made to the data extraction tool according to the requirement after reviewing the first three articles. To achieve a comprehensive set of relevant data that was not included initially during the extraction process, further refinements were added. Data were charted by the first reviewer (M.R), and extraction was checked by the second reviewer (N.B).
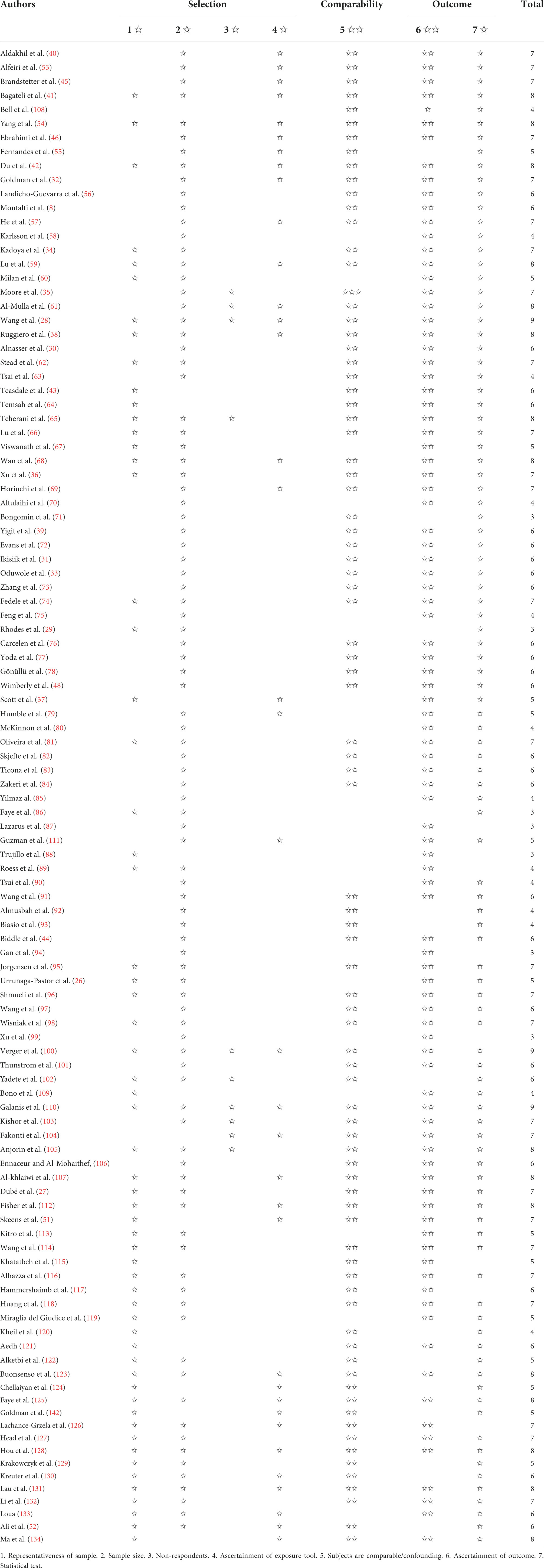
Stage 5: Quality appraisal
The methodological quality of primary studies was appraised by Newcastle–Ottawa scale (NOS). The scale contains seven domains and uses a star system to appraise the studies. These domains include the following: (1) Selection (four subcategories; maximum four stars). (2) Comparability (one subcategory; maximum two stars). (3) Outcome (two subcategories; maximum three stars).
Stage 6: Collating, summarizing, and reporting the findings
This stage consisted of three major steps including numerical, tabular, and narrative summaries of the data. The current review collated and summarized the results systematically by adopting the framework recommended by Arksey and O’Malley (25). Therefore, the first step provided a descriptive numerical summary including the total number of articles searched, the total number of included studies, excluded studies, and reasons for exclusion. The second analytical step was aimed at answering the research questions through a tabular summary. The information included the author’s name, year of publication, study design, vaccine hesitancy/acceptance, and barriers/facilitators for uptake of vaccines. The third analytical step described similarities and differences in such a way in which parental concern and vaccine hesitancy have been defined within each country.
Results
Study selection
The literature review generated 3,750 records, and removing duplicates (n = 292) resulted in 958 studies. Of these, 286 articles were excluded due to the lack of topical relevance following abstract and title screening (Figure 1). A total of 820 articles were subjected to full-text screening. Of these, 686 articles were excluded for the following reasons: 412 articles focused on vaccination in adults and only mentioned childhood vaccination in conclusion, 170 articles were excluded due to repetition, 54 articles focused on other immunization programs with only future aspects of COVID-19 vaccination, and 54 records were published as editorials, letters, and commentaries. We included the oldest publication in the set-in case of duplication. In addition, 27 records were included that were not part of the original search results but were present in the bibliography of the selected studies. Finally, 108 relevant articles reporting the data either on vaccine hesitance or acceptance were identified for inclusion in this review (8, 26–46, 48, 51–135, 143). Some additional articles were also used during data synthesis as supportive evidence (47, 49, 50).
Characteristics of studies
The current review is comprised of studies on COVID-19 acceptance/hesitancy from 27 countries. The dates of survey distribution ranged from January 2020 to August 2022. Stratified per country, the largest sample size (n = 227,740) was reported in a study conducted in Switzerland by Urrunaga-Pastor et al. (26), while the smallest sample size (n = 12) was present in a study conducted in the USA (27). The majority of the studies in this review were conducted in USA (n = 22), China (n = 16), and Saudi Arabia (n = 10) (Supplementary Table 1).
Prevalence of vaccine hesitancy
Vaccine hesitancy was presented in terms of percentage in all studies except two studies where vaccine hesitancy scores were estimated (28, 29). As per classification in the study, the highest vaccine hesitancy rates (>85%) among parents were reported in two studies conducted in Saudi Arabia and Turkey (30, 31). On the contrary, the lowest vaccine hesitancy rates (<4%) were found in two studies conducted in South Africa and Switzerland with 0.69 and 2%, respectively (32, 33) (Table 3).
Table 3. COVID-19 vaccine hesitancy in children, parental concerns, vaccine acceptance, facilitators, and barriers.
Defining the problem of vaccine hesitancy
We distinguished three different approaches to vaccine hesitancy, namely, parental concerns (N = 108/108, 100%), vaccine safety (N = 60/108, 55%), and barriers (N = 70/108, 65%). Most of the studies focused on parental concern, and an increasing number of articles on this topic were published between 2020 and 2022 (Table 3).
Parental concerns
The contribution of parents toward vaccine hesitancy among children has been elucidated in many studies. Cognitive biases of parents have been attributed to decreasing trust in vaccination according to public health experts (31). The reason behind distrust was the risk associated with new vaccines in terms of adverse effects. The current review revealed that parents’ concerns about vaccine safety, side effects, and lack of evidence were significantly associated with vaccine hesitancy according to 62 (76%) studies conducted globally followed by psychological distress and adverse effects (N = 5/108, 4.6%). The reported reasons include cynicism about the efficacy and safety of vaccines and social media influence and a history of unknown allergies, respectively (34–38). Mothers were more hesitant to vaccinate their children in Turkey due to a lack of information about the effectiveness of vaccines and distrust of foreign vaccines (39) (Table 3).
Factors associated with vaccine hesitancy
The current review identified twenty-four barriers to COVID-19 vaccine uptake. It is inevitable to explore the reasons for vaccine hesitancy, reluctance, or outright refusal. The most commonly reported barriers include mothers’ lower education level (N = 46/108, 43%), followed by financial instability (N = 19/108, 16%), low confidence in new vaccines (N = 13/108, 12%) and unmonitored social media platforms (N = 5/108, 4.6%) were associated with vaccine refusal (8, 40–44). Low confidence in the new vaccine was reported in the USA and Saudi Arabia (N = 9/18, 60%) and financial instability was most commonly reported in China (N = 5/20, 25%) (Table 3).
Facilitators of vaccine uptake
Fifty-three studies investigated twenty-two facilitators of vaccine uptake. The significant facilitators for vaccine uptake among respondents who intended to have their children vaccinated include higher education level (N = 12/108, 11%) followed by information obtained through healthcare professionals (N = 9/108, 8.3%) and strong confidence in preventive measures taken by the government (N = 5/108, 4.6%) (40, 41, 45–47). Protecting the people around was another possible reason for the increased intention of vaccine uptake. Information obtained through healthcare workers was commonly reported determinant in the USA, while fear of COVID-19 was highly observed in China (Table 3).
Vaccine hesitancy/acceptance rates in children with comorbidities
Approximately 80% of parents in the USA showed willingness toward vaccination for their children with cancer due to the information obtained through oncologists, and the acceptance rate was quite higher than observed among parents with healthy children (48, 49). However, another study conducted in Taiwan highlighted the vaccine hesitancy among parents of children with ADHD owing to the regular use of medications for ADHD (50). In addition, parents of children with cancer and neurodevelopmental disorders were also unwilling to vaccinate their children against COVID-19 as revealed in studies conducted in USA and Bangladesh, respectively (51, 52) (Table 3).
Quality appraisal of studies
All the studies were subjected to NOS for quality appraisal. Overall, the majority of studies have a medium quality with an average of around six stars (range = 3–9 stars). Seven studies received three stars, thirteen studies received four stars, sixteen received five stars, twenty-eight studies received six stars, twenty-seven received seven stars, sixteen studies received eight stars, and only three studies received nine stars. Table 4 indicates the results of quality assessment of primary studies included in this review.
Discussion
Vaccine hesitancy is a global challenge that causes serious health consequences due to relaying of vaccine-preventable infectious diseases (135). Despite the development of safe and effective vaccines, trends in COVID-19 vaccine acceptance decreased between January 2020 and August 2022 as a result of an array of various factors (136). There is a scarcity of systematic review in the literature on childhood COVID-19 vaccine hesitancy among parents although a plethora of studies exists on COVID-19 vaccine hesitancy. In this context, this study is the first of its kind systematically evaluating both the acceptance and hesitancy of the childhood COVID-19 vaccine among parents.
Vaccine hesitancy (VH) has been reported across countries among parents and healthcare professionals (135). Lower vaccine acceptance among children has been observed as a result of parents’ perceptions that children are at lower risk of COVID-19. Although lower COVID-19 mortality rates have been reported in children, they still account for a significant proportion of COVID-19 cases. Children are 2.5 times more likely to be infected with Delta variant according to recent estimates from the UK (137). It has also been reported in Taiwan that approximately 50% of children retain symptoms even after 6 months of infection. Therefore, COVID-19 vaccine hesitancy plays a significant role in the current pandemic by casting a negative impact on socio-economic status and health.
Vaccine hesitancy may hinder the progress of childhood vaccination programs which in turn results in the increasing prevalence of vaccine-preventable diseases (VPDs). VH influenced the parent’s intention in vaccinating their children. Overcoming this challenge to increase vaccine uptake is inevitable during the COVID-19 pandemic. Thus, an estimate of vaccine hesitancy rates can be helpful for effective intervention and planning inevitably to increase awareness among people regarding the safety and efficacy of vaccines which in turn would help to control the negative influence of the current pandemic by reducing viral spread (138, 139).
The current review represents a large variability in vaccine hesitancy rates globally. The overall vaccine hesitancy rate (>85%) was very high in Saudi Arabia. This finding is close (but not similar) to the findings of studies conducted in Turkey but different from the conclusions of studies performed in China, Brazil, Switzerland, and Zambia where (>85%) vaccine acceptance rates were reported.
The determinants of vaccination hesitancy have been extensively analyzed in this review. Age and gender were effective predictors of sociodemographic factors. All the included studies revealed that younger parents were less likely to vaccinate their children as compared to older parents. The reason may be that younger parents could not judge the pros and cons of vaccines as effectively and accurately as older parents can (45). Several included studies showed that mothers were more hesitant toward vaccination of their children against COVID-19, which was consistent with vaccine intention for other diseases (32, 53, 108, 140). It may be because women are less engaged in riskier behavior as compared to men concerning psychological aspects. In addition, mothers with higher education levels are more concerned about health-related illnesses in daily life (68). However, contradictory results were reported regarding the association between vaccination intention and higher education level. Higher education provides parents with sufficient knowledge about disease and vaccines which play a significant role in effective decision-making regarding vaccination against COVID-19 (8). Economic factors should be taken into account while promoting vaccination. Financial instability was observed to be a negative factor related to vaccination intention most commonly reported in China. Furthermore, parents’ concerns relating to vaccine safety, efficacy, the novelty of vaccines, and adverse effects also contributed to high rates of vaccine hesitancy (141, 142). Another pertinent point is that social media platforms are considered more biased toward conspiratorial and misleading information about COVID-19. Falsehood was more widely shared by interconnected clusters of vaccine opponents globally through social media or web sources. Therefore, those who relied on information obtained through these unmonitored sources were reluctant toward vaccination (8, 46, 71).
Also, the finding related to knowledge and acceptance among different groups of the population should not be underestimated. Parents with fear of contracting COVID-19 were in favor of COVID-19 vaccine uptake as reported in studies conducted in China and Malaysia (28, 94). These findings are in line with available literature demonstrating parents’ willingness toward vaccination due to fear of being infected with COVID-19 (143). A higher level of knowledge associated with a higher education level of the female gender was significantly associated with increased vaccine uptake most commonly observed in Saudi Arabia, Switzerland, and Brazil (40, 41, 142). These findings are consistent with another study conducted in Italy evaluating knowledge related to COVID-19 pandemic (144). Place of residence may also affect the awareness of COVID-19. Residents of urban areas are more inclined to the uptake of COVID-19 vaccine as reported in a study conducted in China (59). These findings are in line with a previously published study highlighting the importance of institutionalization in raising awareness of COVID-19 (144).
The current review provides a high level of evidence regarding vaccine hesitancy among parents by synthesizing a variety of research published till date. In addition, it includes wider scope of studies and also inspects the relationship of sociodemographic factors with vaccine hesitancy. Our study emphasizes that sharing of non-factual data should be avoided through social media and the provision of accurate scientific information should be encouraged. People should be informed correctly regarding the efficacy and safety of vaccines through health authorities to develop trust and confidence in new vaccines. However, data obtained through this review will facilitate the scientists and other healthcare authorities to further promote COVID-19 vaccination in children.
The adoption of a systematic review methodology provides an overview of COVID-19 vaccine hesitancy globally. This review provides deep insight into childhood COVID-19 vaccine hesitancy as the data are not assembled in the form of a systematic review, particularly on parents’ concern about childhood COVID-19 vaccination. Robust estimates of factors are provided in this study through simultaneous investigations of multitudes of relevant variables. Moreover, this review has also identified various predictors of vaccine hesitancy. Quality appraisal of included studies revealed that 88 studies have obtained five and more than five stars and only 20 studies scored less than five stars. However, the findings of this review should be estimated in light of certain limitations. Our review is limited to the studies published only in English language. In addition, our review is comprised of cross-sectional studies, and these studies are usually unable to develop causation as they collect data in a short span. Selection bias could not be ruled out either, because several surveys were conducted in vaccination clinics, emergency departments, or other medical settings. The current review did not comprise of meta-analysis due to the wide variation in methodologies of the primary studies. This review does not provide a comparison between adult and childhood vaccine hesitancy rates across the world. The current review included only those studies that encompass vaccine hesitancy rates among parents of young children and exclude adolescent. Another pertinent point is that we solely focused on scholarly articles and excluded gray literature. There was heterogeneity both in terms of the specific questions asked of participants as well as the provenance of those questions in theory or from standardized questionnaire sets. The use of variable questionnaires may under- or over-estimate the VH. Despite these limitations, this is the first review offering a picture of COVID-19 vaccine hesitancy among parents of young children and provides greater insight into parenteral behaviors toward childhood COVID-19 vaccine. Moreover, the current review was not only confined to parental vaccine hesitancy rates but also evaluated vaccine acceptance patterns. With regard to barriers and facilitators, few data are reported in the previously published scientific literature regarding this age group. The current review will help health authorities that are primarily engaged in childhood immunization to attain herd immunity against COVID-19.
Conclusion
Large variability in COVID-19 vaccine hesitancy was reported across the world. Vaccine safety was considered the most important factor of childhood COVID-19 vaccine hesitancy. In addition, a diverse range of factors influences parents’ beliefs on COVID-19 vaccination. A sizeable number of studies reported COVID-19 vaccine hesitancy rates up to 60%. Uncertainty regarding long-term adverse effects, the novelty of vaccines, non-reliable information obtained through social media, and financial instability were the major challenges faced during the implementation of the COVID-19 vaccination program for children. The worldwide prevalence of COVID-19 necessitates the collaborative efforts of government, media sources, and healthcare authorities. Nevertheless, advocating the safety and efficacy of vaccines through trusted sources might help in developing trust among parents and the general public.
Data availability statement
The original contributions presented in this study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
YK, MR, TM, AIA, ASA, and NA provided substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work. YK, MR, TM, MS, AIA, ASA, NA, S-U-DK, ADA, MB, SIA, KA, SSA, MA, AKA, ZA, and MI drafted the work or revised it critically for important intellectual content. All authors consented to publication and agreed to be accountable for the accuracy or integrity of the work.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2022.950406/full#supplementary-material
References
1. Gostic K, Gomez AC, Mummah RO, Kucharski AJ, Lloyd-Smith JO. Estimated effectiveness of symptom and risk screening to prevent the spread of COVID-19. Elife. (2020) 9:e55570. doi: 10.7554/eLife.55570
2. Misbah S, Ahmad A, Butt MH, Khan YH, Alotaibi NH, Mallhi TH. A systematic analysis of studies on corona virus disease 19 (COVID-19) from viral emergence to treatment. J Coll Physicians Surg Pak. (2020) 30:9–18. doi: 10.29271/jcpsp.2020.Supp1.S9
3. Ludvigsson JF. Systematic review of COVID−19 in children shows milder cases and a better prognosis than adults. Acta Paediatr. (2020) 109:1088–95. doi: 10.1111/apa.15270
4. Ebina-Shibuya R, Namkoong H, Shibuya Y, Horita N. Multisystem inflammatory syndrome in children (MIS-C) with COVID-19: insights from simultaneous familial Kawasaki disease cases. Int J Infect Dis. (2020) 97:371–3. doi: 10.1016/j.ijid.2020.06.014
5. Maltezou HC, Magaziotou I, Dedoukou X, Eleftheriou E, Raftopoulos V, Michos A, et al. Children and adolescents with SARS-CoV-2 infection: epidemiology, clinical course and viral loads. J Pediatr Infect Dis. (2020) 39:e388–92. doi: 10.1097/INF.0000000000002899
6. Schauer J, Buddhe S, Colyer J, Sagiv E, Law Y, Chikkabyrappa SM, et al. Myopericarditis after the Pfizer messenger ribonucleic acid coronavirus disease vaccine in adolescents. J Pediatr. (2021) 238:317–20. doi: 10.1016/j.jpeds.2021.06.083
7. Han B, Song Y, Li C, Yang W, Ma Q, Jiang Z, et al. Safety, tolerability, and immunogenicity of an inactivated SARS-CoV-2 vaccine (CoronaVac) in healthy children and adolescents: a double-blind, randomised, controlled, phase 1/2 clinical trial. Lancet Infect Dis. (2021) 21:1645–53. doi: 10.1016/S1473-3099(21)00319-4
8. Montalti M, Rallo F, Guaraldi F, Bartoli L, Po G, Stillo M, et al. Would parents get their children vaccinated against SARS-CoV-2? Rate and predictors of vaccine hesitancy according to a survey over 5000 families from Bologna, Italy. Vaccines. (2021) 9:366. doi: 10.3390/vaccines9040366
9. Anderson M, Mckee M, Mossialos E. Covid-19 exposes weaknesses in European response to outbreaks. BMJ. (2020) 368:m1075. doi: 10.1136/bmj.m1075
10. Anderson RM, Heesterbeek H, Klinkenberg D, Hollingsworth TD. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet. (2020) 395:931–4. doi: 10.1016/S0140-6736(20)30567-5
11. Chu DK, Akl EA, Duda S, Solo K, Yaacoub S, Schünemann HJ. COVID-19 systematic urgent review group effort (SURGE) study authors. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. (2020) 395:1973–87. doi: 10.1016/S0140-6736(20)31142-9
12. Eibensteiner F, Ritschl V, Stamm T, Cetin A, Schmitt CP, Ariceta G, et al. Countermeasures against COVID-19: how to navigate medical practice through a nascent, evolving evidence base—a European multicentre mixed methods study. BMJ Open. (2021) 11:e043015. doi: 10.1136/bmjopen-2020-043015
13. Butt MH, Ahmad A, Misbah S, Mallhi TH, Khan YH, Muhammad K, et al. Ensuring the quality and appropriate use of hand sanitizers during the COVID-19 pandemic: suggestions and recommendations with the role of the pharmacist. Disaster Med Public Health Prep. (2021). Epub ahead of print. doi: 10.1017/dmp.2021.55
14. Alzarea AI, Khan YH, Alatawi AD, Alanazi AS, Alzarea SI, Butt MH, et al. Surveillance of post-vaccination side effects of COVID-19 vaccines among saudi population: a real-world estimation of safety profile. Vaccines. (2022) 10:924. doi: 10.3390/vaccines10060924
15. Gharpure R, Patel A, Link-Gelles R. First-dose COVID-19 vaccination coverage among skilled nursing facility residents and staff. JAMA. (2021) 325:1670–1. doi: 10.1001/jama.2021.2352
16. Windpessl M, Bruchfeld A, Anders H-J, Kramer H, Waldman M, Renia L, et al. COVID-19 vaccines and kidney disease. Nat Rev Nephrol. (2021) 17:291–3. doi: 10.1038/s41581-021-00406-6
17. Haque A, Pant AB. Mitigating Covid-19 in the face of emerging virus variants, breakthrough infections and vaccine hesitancy. J Autoimmun. (2022) 127:102792. doi: 10.1016/j.jaut.2021.102792
18. Cooper DM, Afghani B, Byington CL, Cunningham CK, Golub S, Lu KD, et al. SARS-CoV-2 vaccine testing and trials in the pediatric population: biologic, ethical, research, and implementation challenges. Pediatr Res. (2021) 90:966–70. doi: 10.1038/s41390-021-01402-z
19. Anakpo G, Mishi S. Hesitancy of COVID-19 vaccines: rapid systematic review of the measurement, predictors, and preventive strategies. Hum Vaccines Immunother. (2022) 18:2074716. doi: 10.1080/21645515.2022.2074716
20. Shen SC, Dubey V. Addressing vaccine hesitancy: clinical guidance for primary care physicians working with parents. Can Fam Physician. (2019) 65:175–81.
21. Riccò M, Vezzosi L, Gualerzi G, Signorelli C. Knowledge, attitudes and practices (KAP) towards vaccinations in the school settings: an explorative survey. J Prev Med Hyg. (2017) 58:E266. doi: 10.15167/2421-4248/jpmh2017.58.4.673
22. Filia A, Bella A, D’Ancona F, Fabiani M, Giambi C, Rizzo C, et al. Childhood vaccinations: knowledge, attitudes and practices of paediatricians and factors associated with their confidence in addressing parental concerns, Italy, 2016. Eurosurveillance. (2019) 24:1800275. doi: 10.2807/1560-7917.ES.2019.24.6.1800275
23. Larson HJ, Jarrett C, Eckersberger E, Smith DM, Paterson P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007–2012. Vaccine. (2014) 32:2150–9. doi: 10.1016/j.vaccine.2014.01.081
24. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. (2021) 10:1–11. doi: 10.1186/s13643-021-01626-4
25. Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. (2005) 8:19–32. doi: 10.1080/1364557032000119616
26. Urrunaga-Pastor D, Herrera-Añazco P, Uyen-Cateriano A, Toro-Huamanchumo CJ, Rodriguez-Morales AJ, Hernandez AV, et al. Prevalence and factors associated with parents’ non-intention to vaccinate their children and adolescents against COVID-19 in Latin America and the caribbean. Vaccines. (2021) 9:1303. doi: 10.3390/vaccines9111303
27. Dubé E, Gagnon D, Pelletier C. COVID-19 vaccination in 5-11 years old children: drivers of vaccine hesitancy among parents in Quebec. Hum Vaccines Immunother. (2022) 18:2028516. doi: 10.1080/21645515.2022.2028516
28. Wang Q, Xiu S, Zhao S, Wang J, Han Y, Dong S, et al. Vaccine hesitancy: COVID-19 and influenza vaccine willingness among parents in wuxi, China—A cross-sectional study. Vaccines. (2021) 9:342. doi: 10.3390/vaccines9040342
29. Rhodes ME, Sundstrom B, Ritter E, McKeever BW, McKeever R. Preparing for a COVID-19 vaccine: a mixed methods study of vaccine hesitant parents. J Health Commun. (2020) 25:831–7. doi: 10.1080/10810730.2021.1871986
30. Alnasser Y, Alnamnakani MA, Abuhaimed JM, Alshiha LZ, Alhamid NM, Alalshaikh GA. Preparedness of current and future Saudi Pediatricians to face vaccine hesitancy: cross-sectional study within the capital city of Saudi Arabia, Riyadh. Ann Med Surg. (2021) 69:102718. doi: 10.1016/j.amsu.2021.102718
31. İkiışık H, Akif Sezerol M, Taşçı Y, Maral I. COVID−19 vaccine hesitancy: a community−based research in Turkey. Int J Clin Pract. (2021) 75:e14336. doi: 10.1111/ijcp.14336
32. Goldman RD, Yan TD, Seiler M, Cotanda CP, Brown JC, Klein EJ, et al. Caregiver willingness to vaccinate their children against COVID-19: cross sectional survey. Vaccine. (2020) 38:7668–73. doi: 10.1016/j.vaccine.2020.09.084
33. Oduwole EO, Mahomed H, Ayele BT, Wiysonge CS. Estimating vaccine confidence levels among healthcare students and staff of a tertiary institution in South Africa: protocol of a cross-sectional survey. BMJ Open. (2021) 11:e049877. doi: 10.1136/bmjopen-2021-049877
34. Kadoya Y, Watanapongvanich S, Yuktadatta P, Putthinun P, Lartey ST, Khan MSR. Willing or hesitant? A socioeconomic study on the potential acceptance of COVID-19 vaccine in Japan. Int J Environ Res Public Health. (2021) 18:4864.
35. Moore DCBC, Nehab MF, Camacho KG, Reis AT, de Fátima Junqueira-Marinho M, Abramov DM, et al. Low COVID-19 vaccine hesitancy in Brazil. Vaccine. (2021) 39:6262–8. doi: 10.1016/j.vaccine.2021.09.013
36. Xu Y, Zhang R, Zhou Z, Fan J, Liang J, Cai L, et al. Parental psychological distress and attitudes towards COVID-19 vaccination: a cross-sectional survey in Shenzhen, China. J Affect Disord. (2021) 292:552–8. doi: 10.1016/j.jad.2021.06.003
37. Scott HM, Coombes L, Braybrook D, Roach A, Harðardóttir D, Bristowe K, et al. COVID-19: impact on pediatric palliative care. J Pain Symptom Manage. (2022) 64:e1–5. doi: 10.1016/j.jpainsymman.2022.02.330
38. Ruggiero KM, Wong J, Sweeney CF, Avola A, Auger A, Macaluso M, et al. Parents’ intentions to vaccinate their children against COVID-19. J Pediatr Health Care. (2021) 35:509–17. doi: 10.1016/j.pedhc.2021.04.005
39. Yigit M, Ozkaya-Parlakay A, Senel E. Evaluation of COVID-19 vaccine refusal in parents. J Pediatr Infect Dis. (2021) 40:e134–6. doi: 10.1097/INF.0000000000003042
40. Aldakhil H, Albedah N, Alturaiki N, Alajlan R, Abusalih H. Vaccine hesitancy towards childhood immunizations as a predictor of mothers’ intention to vaccinate their children against COVID-19 in Saudi Arabia. J Infect Public Health. (2021) 14:1497–504. doi: 10.1016/j.jiph.2021.08.028
41. Bagateli LE, Saeki EY, Fadda M, Agostoni C, Marchisio P, Milani GP. COVID-19 vaccine hesitancy among parents of children and adolescents living in Brazil. Vaccines. (2021) 9:1115. doi: 10.3390/vaccines9101115
42. Du M, Tao L, Liu J. The association between risk perception and COVID-19 vaccine hesitancy for children among reproductive women in China: an online survey. Front Med (Lausanne). (2021) 8:741298. doi: 10.3389/fmed.2021.741298
43. Teasdale CA, Borrell LN, Shen Y, Kimball S, Rinke ML, Fleary SA, et al. Parental plans to vaccinate children for COVID-19 in New York city. Vaccine. (2021) 39:5082–6. doi: 10.1016/j.vaccine.2021.07.058
44. Biddle N, Edwards B, Gray M, Sollis K. Determinants of COVID-19 Vaccination and Views of Parents about Vaccination of Children in Australia: August 2021 ANU Centre for Social Research and Methods. Guntur: ANU (2021).
45. Brandstetter S, Böhmer MM, Pawellek M, Seelbach-Göbel B, Melter M, Kabesch M, et al. Parents’ intention to get vaccinated and to have their child vaccinated against COVID-19: cross-sectional analyses using data from the KUNO-Kids health study. Eur J Pediatr. (2021) 180:3405–10. doi: 10.1007/s00431-021-04094-z
46. Ebrahimi OV, Johnson MS, Ebling S, Amundsen OM, Halsøy Ø, Hoffart A, et al. Risk, trust, and flawed assumptions: vaccine hesitancy during the COVID-19 pandemic. Front Public Health. (2021) 9:700213. doi: 10.3389/fpubh.2021.700213
47. Goldman RD, Bone JN, Gelernter R, Krupik D, Ali S, Mater A, et al. National COVID-19 vaccine program progress and parents’ willingness to vaccinate their children. Hum Vaccin Immunother. (2021) 17:4889–95. doi: 10.1080/21645515.2021.1999144
48. Wimberly CE, Towry L, Davis E, Johnston EE, Walsh KM. SARS−CoV−2 vaccine acceptability among caregivers of childhood cancer survivors. Pediatr Blood Cancer. (2021) 69:e29443. doi: 10.1002/pbc.29443
49. Tsui J, Martinez B, Shin MB, Allee-Munoz A, Rodriguez I, Navarro J, et al. Understanding medical mistrust and HPV vaccine hesitancy among multiethnic parents in Los Angeles. J Behav Med. (2022). Epub ahead of print. doi: 10.1007/s10865-022-00283-9
50. Tsai R, Hervey J, Hoffman K, Wood J, Johnson J, Deighton D, et al. COVID-19 vaccine hesitancy and acceptance among individuals with cancer, autoimmune diseases, or other serious comorbid conditions: cross-sectional, internet-based survey. JMIR Public Health Surveill. (2022) 8:e29872. doi: 10.2196/29872
51. Skeens MA, Hill K, Olsavsky A, Buff K, Stevens J, Akard TF, et al. Factors affecting COVID−19 vaccine hesitancy in parents of children with cancer. Pediatr Blood Cancer. (2022) 69:e29707. doi: 10.1002/pbc.29707
52. Ali M, Proma TS, Tasnim Z, Islam M, Urmi TA, Ahmed S, et al. Parental COVID-19 vaccine hesitancy for children with neurodevelopmental disorders: a cross-sectional survey. Trop Med Health. (2022) 50:24. doi: 10.1186/s41182-022-00415-6
53. Alfieri NL, Kusma JD, Heard-Garris N, Davis MM, Golbeck E, Barrera L, et al. Parental COVID-19 vaccine hesitancy for children: vulnerability in an urban hotspot. BMC Public Health. (2021) 21:1662. doi: 10.1186/s12889-021-11725-5
54. Yang J, Zhang T, Qi W, Zhang X, Jia M, Leng Z, et al. COVID-19 vaccination in Chinese children: a cross-sectional study on the cognition, psychological anxiety state and the willingness toward vaccination. Hum Vaccin Immunother. (2021) 18:1–7. doi: 10.1080/21645515.2021.1949950
55. Fernandes N, Costa D, Costa D, Keating J, Arantes J. Predicting COVID-19 vaccination intention: the determinants of vaccine hesitancy. Vaccines. (2021) 9:1161. doi: 10.3390/vaccines9101161
56. Landicho-Guevarra J, Reñosa MDC, Wachinger J, Endoma V, Aligato MF, Bravo TA, et al. Scared, powerless, insulted and embarrassed: hesitancy towards vaccines among caregivers in Cavite Province, the Philippines. BMJ Glob Health. (2021) 6:e006529. doi: 10.1136/bmjgh-2021-006529
57. He K, Mack WJ, Neely M, Lewis L, Anand V. Parental perspectives on immunizations: impact of the COVID-19 pandemic on childhood vaccine hesitancy. J Community Health. (2021) 47:39–52. doi: 10.1007/s10900-021-01017-9
58. Karlsson LC, Soveri A, Lewandowsky S, Karlsson L, Karlsson H, Nolvi S, et al. Fearing the disease or the vaccine: the case of COVID-19. Pers Individ Differ. (2021) 172:110590. doi: 10.1016/j.paid.2020.110590
59. Lu J, Wen X, Guo Q, Ji M, Zhang F, Wagner AL, et al. Sensitivity to COVID-19 vaccine effectiveness and safety in Shanghai, China. Vaccines. (2021) 9:472. doi: 10.3390/vaccines9050472
60. Milan S, Dáu ALB. The role of trauma in mothers’ COVID-19 vaccine beliefs and intentions. J Pediatr Psychol. (2021) 46:526–35. doi: 10.1093/jpepsy/jsab043
61. Al-Mulla R, Abu-Madi M, Talafha QM, Tayyem RF, Abdallah AM. COVID-19 vaccine hesitancy in a representative education sector population in Qatar. Vaccines. (2021) 9:665. doi: 10.3390/vaccines9060665
62. Stead M, Jessop C, Angus K, Bedford H, Ussher M, Ford A, et al. National survey of attitudes towards and intentions to vaccinate against COVID-19: implications for communications. BMJ Open. (2021) 11:e055085. doi: 10.1136/bmjopen-2021-055085
63. Tsai C-S, Hsiao RC, Chen Y-M, Yen C-F. Factors related to caregiver intentions to vaccinate their children with attention-deficit/hyperactivity disorder against COVID-19 in Taiwan. Vaccines. (2021) 9:983. doi: 10.3390/vaccines9090983
64. Temsah M-H, Alhuzaimi AN, Aljamaan F, Bahkali F, Al-Eyadhy A, Alrabiaah A, et al. Parental attitudes and hesitancy about COVID-19 versus routine childhood vaccinations: a national survey. Front Public Health. (2021) 9:752323. doi: 10.3389/fpubh.2021.752323
65. Teherani M, Banskota S, Camacho-Gonzalez A, Smith AG, Anderson EJ, Kao CM, et al. Intent to vaccinate SARS-CoV-2 infected children in US households: a survey. Vaccines. (2021) 9:1049. doi: 10.3390/vaccines9091049
66. Lu X, Wang J, Hu L, Li B, Lu Y. Association between Adult vaccine hesitancy and parental acceptance of childhood COVID-19 vaccines: a web-based survey in a North western region in China. Vaccines. (2021) 9:1088. doi: 10.3390/vaccines9101088
67. Viswanath K, Bekalu M, Dhawan D, Pinnamaneni R, Lang J, McLoud R. Individual and social determinants of COVID-19 vaccine uptake. BMC Public Health. (2021) 21:818. doi: 10.1186/s12889-021-10862-1
68. Wan X, Huang H, Shang J, Xie Z, Jia R, Lu G, et al. Willingness and influential factors of parents of 3-6-year-old children to vaccinate their children with the COVID-19 vaccine in China. Hum Vaccines Immunother. (2021) 17:3969–74. doi: 10.1080/21645515.2021.1955606
69. Horiuchi S, Sakamoto H, Abe SK, Shinohara R, Kushima M, Otawa S, et al. Factors of parental COVID-19 vaccine hesitancy: a cross sectional study in Japan. PLoS One. (2021) 16:e0261121. doi: 10.1371/journal.pone.0261121
70. Altulaihi BA, Alaboodi T, Alharbi KG, Alajmi MS, Alkanhal H, Alshehri A. Perception of parents towards COVID-19 vaccine for children in Saudi population. Cureus. (2021) 13:e18342. doi: 10.7759/cureus.18342
71. Bongomin F, Olum R, Andia-Biraro I, Nakwagala FN, Hassan KH, Nassozi DR, et al. COVID-19 vaccine acceptance among high-risk populations in Uganda. Ther Adv Infect Dis. (2021) 8:20499361211024376.
72. Evans S, Klas A, Mikocka-Walus A, German B, Rogers G, Ling M, et al. “Poison” or “protection”? A mixed methods exploration of Australian parents’ COVID-19 vaccination intentions. J Psychosom Res. (2021) 150:110626. doi: 10.1016/j.jpsychores.2021.110626
73. Zhang M-X, Lin X-Q, Chen Y, Tung T-H, Zhu J-S. Determinants of parental hesitancy to vaccinate their children against COVID-19 in China. Expert Rev Vaccines. (2021) 20:1339–49. doi: 10.1080/14760584.2021.1967147
74. Fedele F, Aria M, Esposito V, Micillo M, Cecere G, Spano M, et al. COVID-19 vaccine hesitancy: a survey in a population highly compliant to common vaccinations. Hum Vaccines Immunother. (2021) 17:3348–54. doi: 10.1080/21645515.2021.1928460
75. Feng H, Zhu H, Zhang H, Cao L, Li L, Wang J, et al. Caregivers’ intentions to COVID-19 vaccination for their children in China: a cross-sectional survey. Hum Vaccines Immunother. (2021) 17:4799–805. doi: 10.1080/21645515.2021.1985355
76. Carcelen AC, Prosperi C, Mutembo S, Chongwe G, Mwansa FD, Ndubani P, et al. COVID-19 vaccine hesitancy in Zambia: a glimpse at the possible challenges ahead for COVID-19 vaccination rollout in sub-Saharan Africa. Hum Vaccines Immunother. (2021) 18:1–6. doi: 10.1080/21645515.2021.1948784
77. Yoda T, Katsuyama H. Parents’ hesitation about getting their children vaccinated against COVID-19 in Japan. Hum Vaccines Immunother. (2021) 17:4993–8. doi: 10.1080/21645515.2021.1981087
78. Gönüllü E, Soysal A, Atici S, Engin M, Yesilbas O, Kasap T, et al. Pediatricians’ COVID-19 experiences and views on the willingness to receive COVID-19 vaccines: a cross-sectional survey in Turkey. Hum Vaccines Immunother. (2021) 17:2389–96.
79. Humble RM, Sell H, Dubé E, MacDonald NE, Robinson J, Driedger SM, et al. Canadian parents’ perceptions of COVID-19 vaccination and intention to vaccinate their children: results from a cross-sectional national survey. Vaccine. (2021) 39:7669–76. doi: 10.1016/j.vaccine.2021.10.002
80. McKinnon B, Quach C, Dubé È, Nguyen CT, Zinszer K. Social inequalities in COVID-19 vaccine acceptance and uptake for children and adolescents in Montreal, Canada. Vaccine. (2021) 39:7140–5. doi: 10.1016/j.vaccine.2021.10.077
81. Oliveira BLCA, Campos MAG, Queiroz RCS, Alves MTSSBE, Souza BF, Santos AMD, et al. Prevalence and factors associated with covid-19 vaccine hesitancy in Maranhão, Brazil. Rev Saude Publica. (2021) 55:12.
82. Skjefte M, Ngirbabul M, Akeju O, Escudero D, Hernandez-Diaz S, Wyszynski DF, et al. COVID-19 vaccine acceptance among pregnant women and mothers of young children: results of a survey in 16 countries. Eur J Epidemiol. (2021) 36:197–211. doi: 10.1007/s10654-021-00728-6
83. Aguilar Ticona JP, Nery N, Victoriano R, Fofana MO, Ribeiro GS, Giorgi E, et al. Willingness to get the COVID-19 vaccine among residents of slum settlements. Vaccines. (2021) 9:951. doi: 10.3390/vaccines9090951
84. Zakeri M, Li J, Sadeghi SD, Essien EJ, Sansgiry SS. Strategies to decrease COVID-19 vaccine hesitancy for children. J Pharm Health Serv Res. (2021) 12:539–44.
85. Yılmaz M, Sahin MK. Parents’ willingness and attitudes concerning the COVID−19 vaccine: a cross−sectional study. Int J Clin Pract. (2021) 75:e14364.
86. Faye S, Krumkamp R, Doumbia S, Tounkara M, Strauss R, Ouedraogo HG, et al. Factors Influencing COVID-19 Vaccines Hesitancy in Rural and Urban West Africa: Implications for Vaccination Strategies. Geneva: World Health Organization (2021).
87. Lazarus J, Wyka K, White T, Picchio C, Rabin K, Ratzan S, et al. COVID-VAC: the second global study of COVID-19 vaccine acceptance. Nat. Commun. (2021) [Preprint] doi: 10.21203/rs.3.rs-780128/v1
88. Trujillo KL, Lazer D, Simonson MD, Pippert CH, Perlis RH, Baum M, et al. The COVID States Project #71: Childhood COVID-19 Vaccine Uptake and Intentions. Charlottesville, VA: OSF (2021). doi: 10.31219/osf.io/cu4jz
89. Roess AA, Adams L, Huddleston K, Lawrence GN, Wilson AN, Oetjen C, et al. Political Affiliation and Race Associated With Parents’ Intentions to Have a COVID-19 Vaccination but Not With History of Refusing to Vaccinate a Child: A Cross-Sectional Study. Durham, NC: Research Square (2021). doi: 10.21203/rs.3.rs-469429/v1
90. Tsui J, Martinez B, Bonnell L, Mayet S, Yan X, Kast WM, et al. The relationship between adolescent HPV vaccination and parental hesitancy for COVID-19 vaccination. In: Proceedings of the APHA 2021 Annual Meeting and Expo. Washington, D.C: APHA (2021).
91. Wang B, Nolan R, Marshall H. COVID-19 immunisation, willingness to be vaccinated and vaccination strategies to improve vaccine uptake in Australia. Vaccines. (2021) 9:1467.
92. Almusbah Z, Alhajji Z, Alshayeb Z, Alhabdan R, Alghafli S, Almusabah M, et al. Caregivers’ willingness to vaccinate their children against COVID-19 in Saudi Arabia: a cross-sectional survey. Cureus. (2021) 13:e17243.
93. Biasio LR, Bonaccorsi G, Lorini C, Mazzini D, Pecorelli S. Italian adults’ likelihood of getting covid-19 vaccine: a second online survey. Vaccines. (2021) 9:268. doi: 10.3390/vaccines9030268
94. Gan G-G, Chai C-S, Anuar NAB, Sindeh W, Chua W-J, Said AB, et al. The Willingness of Malaysian Parents To Vaccinate Their Children Below 12 Years Old Against COVID-19–A Large Cross-Sectional Study. Durham, NC: Research Square (2021).
95. Jørgensen FJ, Petersen MB. Considerations underlying parents’ acceptance of COVID-19 vaccines for their child: evidence from Denmark. PsyaRxiv. (2021) [Preprint] doi: 10.31234/osf.io/8e49j
96. Shmueli L. Parents’ intention to vaccinate their 5-11 years old children with the COVID-19 vaccine: rates, predictors and the role of incentives. medRxiv. (2021) [Preprint] doi: 10.1101/2021.11.05.21265900
97. Wang J, Ji Q, Dong S, Zhao S, Li X, Zhu Q, et al. Factors influencing vaccine hesitancy in China: a qualitative study. Vaccines. (2021) 9:1291. doi: 10.3390/vaccines9111291
98. Wisniak A, Baysson H, Pullen N, Nehme M, Pennacchio F, Zaballa M-E, et al. COVID-19 vaccination acceptance in the canton of Geneva: a cross-sectional population-based study. medRxiv. (2021) [Preprint] doi: 10.1101/2021.07.05.21260024
99. Xu Y, Xu D, Luo L, Ma F, Wang P, Li H, et al. A cross-sectional survey on COVID-19 vaccine hesitancy among parents from Shandong vs. Zhejiang. Front Public Health. (2021) 9:779720. doi: 10.3389/fpubh.2021.779720
100. Verger P, Peretti-Watel P, Gagneux-Brunon A, Botelho-Nevers E, Sanchez A, Gauna F, et al. Acceptance of childhood and adolescent vaccination against COVID-19 in France: a national cross-sectional study in May 2021. Hum Vaccin Immunother. (2021) 17:5082–8. doi: 10.1080/21645515.2021.2004838
101. Thunström L, Ashworth M, Finnoff D, Newbold SC. Hesitancy toward a COVID-19 vaccine. Ecohealth. (2021) 18:44–60. doi: 10.1007/s10393-021-01524-0
102. Yadete T, Batra K, Netski DM, Antonio S, Patros MJ, Bester JC. Assessing acceptability of COVID-19 vaccine booster dose among adult Americans: a cross-sectional study. Vaccines. (2021) 9:1424. doi: 10.3390/vaccines9121424
103. Kishore J, Venkatesh U, Ghai G. Perception and attitude towards COVID-19 vaccination: a preliminary online survey from India. J Fam Med Prim Care. (2021) 10:3116. doi: 10.4103/jfmpc.jfmpc_2530_20
104. Fakonti G, Kyprianidou M, Toumbis G, Giannakou K. Attitudes and acceptance of COVID-19 vaccination among nurses and midwives in cyprus: a cross-sectional survey. Front Public Health. (2021) 9:656138. doi: 10.3389/fpubh.2021.656138
105. Anjorin AA, Odetokun IA, Abioye AI, Elnadi H, Umoren MV, Damaris BF, et al. Will Africans take COVID-19 vaccination? PLoS One. (2021) 16:e0260575. doi: 10.1371/journal.pone.0260575
106. Ennaceur S, Al-Mohaithef M. Parents’ willingness to vaccinate children against COVID-19 in Saudi Arabia: a cross-sectional study. Vaccines. (2022) 10:156. doi: 10.3390/vaccines10020156
107. Al-khlaiwi T, Meo SA, Almousa HA, Almebki AA, Albawardy MK, Alshurafa HH, et al. National COVID-19 vaccine program and parent’s perception to vaccinate their children: a cross-sectional study. Vaccines. (2022) 10:168. doi: 10.3390/vaccines10020168
108. Bell S, Clarke R, Mounier-Jack S, Walker JL, Paterson P. Parents’ and guardians’ views on the acceptability of a future COVID-19 vaccine: a multi-methods study in England. Vaccine. (2020) 38:7789–98. doi: 10.1016/j.vaccine.2020.10.027
109. Bono SA, Siau CS, Chen WS, Low WY, Faria de Moura Villela E, Pengpid S, et al. Adults’ acceptance of COVID-19 vaccine for children in selected lower-and middle-income countries. Vaccines. (2021) 10:11. doi: 10.3390/vaccines10010011
110. Galanis PA, Vraka I, Siskou O, Konstantakopoulou O, Katsiroumpa A, Moisoglou I. Predictors of real-world parents acceptance to vaccinate their children against the COVID-19. medRxiv. (2021) [Preprint] doi: 10.1101/2021.09.12.21263456
111. Guzman C, Firew T, Wagh A, Stefan B, Ruscica A, Mitchell C, et al. 24 COVID-19 vaccine hesitancy among emergency department patients and caregivers in New York City. Ann Emerg Med. (2021) 78:S12. doi: 10.1016/j.annemergmed.2021.07.025
112. Fisher CB, Bragard E, Jaber R, Gray A. COVID-19 vaccine hesitancy among parents of children under five years in the United States. Vaccines. (2022) 10:1313. doi: 10.3390/vaccines10081313
113. Kitro A, Sirikul W, Dilokkhamaruk E, Sumitmoh G, Pasirayut S, Wongcharoen A, et al. COVID-19 vaccine hesitancy and influential factors among Thai parents and guardians to vaccinate their children. Vaccine. (2022) 11:100182. doi: 10.1016/j.jvacx.2022.100182
114. Wang CS, Doma R, Westbrook AL, Johnson J, Anderson EJ, Greenbaum LA, et al. Vaccine attitudes and COVID-19 vaccine intention among parents of children with kidney disease or primary hypertension. Am J Kidney Dis. (2022). Epub ahead of print. doi: 10.1053/j.ajkd.2022.04.011
115. Khatatbeh M, Albalas S, Khatatbeh H, Momani W, Melhem O, Al Omari O, et al. Children’s rates of COVID-19 vaccination as reported by parents, vaccine hesitancy, and determinants of COVID-19 vaccine uptake among children: a multi-country study from the Eastern Mediterranean region. BMC Public Health. (2022) 22:1375. doi: 10.1186/s12889-022-13798-2
116. Alhazza SF, Altalhi AM, Alamri KM, Alenazi SS, Alqarni BA, Almohaya AM. Parents’ hesitancy to vaccinate their children against COVID-19, a country-wide survey. Front Public Health. (2022) 10:755073. doi: 10.3389/fpubh.2022.755073
117. Hammershaimb EA, Cole LD, Liang Y, Hendrich MA, Das D, Petrin R, et al. COVID-19 vaccine acceptance among US parents: a nationally representative survey. J Pediatric Infect Dis Soc. (2022) 11:361–70. doi: 10.1093/jpids/piac049
118. Huang L-L, Yang Y-P, Mao H-P, Hu W-W, Jiang Y-H, Jiesisibieke ZL, et al. Parental hesitancy towards vaccinating their children with a booster dose against COVID-19: real-world evidence from Taizhou, China. J Infect Public Health. (2022) 15:1006–12. doi: 10.1016/j.jiph.2022.08.002
119. Miraglia del Giudice G, Napoli A, Corea F, Folcarelli L, Angelillo IF. Evaluating COVID-19 vaccine willingness and hesitancy among parents of children aged 5–11 years with chronic conditions in Italy. Vaccines. (2022) 10:396. doi: 10.3390/vaccines10030396
120. Kheil MH, Jain D, Jomaa J, Askar B, Alcodray Y, Wahbi S, et al. COVID-19 vaccine hesitancy among Arab Americans. Vaccines. (2022) 10:610. doi: 10.3390/vaccines10040610
121. Aedh AI. Parents’ attitudes, their acceptance of the COVID-19 vaccines for children and the contributing factors in Najran, Saudi Arabia: a cross-sectional survey. Vaccines. (2022) 10:1264. doi: 10.3390/vaccines10081264
122. AlKetbi LMB, Al Hosani F, Al Memari S, Al Mazrouei S, Al Shehhi B, AlShamsi N, et al. Parents’ views on the acceptability of a COVID-19 vaccine for their children: a cross-sectional study in Abu Dhabi-United Arab Emirates. Vaccine. (2022) 40:5562–8. doi: 10.1016/j.vaccine.2022.07.056
123. Buonsenso D, Valentini P, Macchi M, Folino F, Pensabene C, Patria MF, et al. Caregivers’ attitudes toward COVID-19 vaccination in children and adolescents with a history of SARS-CoV-2 infection. Front Pediatr. (2022) 10:867968. doi: 10.3389/fped.2022.867968
124. Chellaiyan, VG, Alfred J, Jasmine M. COVID-19 vaccination for children: acceptance by the mothers of children aged 2-12 years in Tamil Nadu. J Commun Dis. (2022):62–7. doi: 10.24321/0019.5138.202210
125. Faye SLB, Krumkamp R, Doumbia S, Tounkara M, Strauss R, Ouedraogo HG, et al. Factors influencing hesitancy towards adult and child COVID-19 vaccines in rural and urban West Africa: a cross-sectional study. BMJ Open. (2022) 12:e059138. doi: 10.1136/bmjopen-2021-059138
126. Lachance-Grzela, M, Charbonneau A, Dubé A, Jbilou J, Richard J. Parents and caregivers’ willingness to vaccinate their children against COVID-19. Can J Behav Sci. (2022):1–6. doi: 10.1037/cbs0000333
127. Head KJ, Zimet GD, Yiannoutsos CT, Silverman RD, Sanner L, Menachemi N. Factors that differentiate COVID-19 vaccine intentions among Indiana parents: implications for targeted vaccine promotion. Prev Med. (2022) 158:107023. doi: 10.1016/j.ypmed.2022.107023
128. Hou Z, Song K, Wang Q, Zang S, Tu S, Chantler T, et al. Childhood COVID-19 vaccine acceptance and preference from caregivers and healthcare workers in China: a survey experiment. Prev Med. (2022) 161:107138. doi: 10.1016/j.ypmed.2022.107138
129. Krakowczyk JB, Bäuerle A, Pape L, Kaup T, Nulle L, Teufel M, et al. COVID-19 vaccine for children: vaccination willingness of parents and its associated factors—a network analysis. Vaccines. (2022) 10:1155. doi: 10.3390/vaccines10071155
130. Kreuter MW, Garg R, Marsh A, Thompson T, Caburnay C, Teshome E, et al. Intention to vaccinate children for COVID-19: a segmentation analysis among medicaid parents in Florida. Prev Med. (2022) 156:106959. doi: 10.1016/j.ypmed.2022.106959
131. Lau EYH, Li J-B, King Chung Chan D. Intention to vaccinate young children against COVID-19: a large-scale survey of Hong Kong parents. Hum Vaccines Immunother. (2022) 18:2065838.
132. Li, T., Qiu, X., Gong, X., Zhan, R., and Zheng, X. (2022). The cross-sectional survey on COVID-19 vaccine hesitancy and it predictors among Chinese parents of 3–17 years aged children in Shenzhen City. Annals of Agricultural and Environmental Medicine, 29(1), 120-125.
133. Loua TO. Reverse Vaccine Hesitancy: A Qualitative Study Assessing Factors that Drive COVID-19 Vaccine Acceptance on Vashon Island, WA. Seattle, WA: Research Works (2022).
134. Ma L, Yang J, Zhang T, Han X, Huang Q, Yang Y, et al. Willingness toward COVID-19 vaccination, coadministration with other vaccines and receive a COVID-19 vaccine booster: a cross-sectional study on the guardians of children in China. Hum Vaccines Immunother. (2022) 18:2049169. doi: 10.1080/21645515.2022.2049169
135. Lin C, Tu P, Beitsch LM. Confidence and receptivity for COVID-19 vaccines: a rapid systematic review. Vaccines. (2021) 9:16. doi: 10.3390/vaccines9010016
136. de Albuquerque Veloso Machado M, Roberts B, Wong BLH, van Kessel R, Mossialos E. The relationship between the COVID-19 pandemic and vaccine hesitancy: a scoping review of literature until august 2021. Front Public Health. (2021) 9:747787. doi: 10.3389/fpubh.2021.747787
137. Lassi ZS, Naseem R, Salam RA, Siddiqui F, Das JK. The impact of the COVID-19 pandemic on immunization campaigns and programs: a systematic review. Int J Environ Res Public Health. (2021) 18:988. doi: 10.3390/ijerph18030988
138. Weintraub RL, Subramanian L, Karlage A, Ahmad I, Rosenberg J. COVID-19 vaccine to vaccination: why leaders must invest in delivery strategies now: analysis describe lessons learned from past pandemics and vaccine campaigns about the path to successful vaccine delivery for COVID-19. Health Aff. (2021) 40:33–41.
139. Habersaat KB, Betsch C, Danchin M, Sunstein CR, Böhm R, Falk A, et al. Ten considerations for effectively managing the COVID-19 transition. Nat Hum Behav. (2020) 4:677–87. doi: 10.1038/s41562-020-0906-x
140. Barry M, Temsah M-H, Alhuzaimi A, Alamro N, Al-Eyadhy A, Aljamaan F, et al. COVID-19 vaccine confidence and hesitancy among health care workers: a cross-sectional survey from a MERS-CoV experienced nation. PLoS One. (2021) 16:e0244415. doi: 10.1371/journal.pone.0244415
141. Hetherington E, Edwards SA, MacDonald SE, Racine N, Madigan S, McDonald S, et al. SARS-CoV-2 vaccination intentions among mothers of children aged 9 to 12 years: a survey of the all our families cohort. Can Med Assoc Open Access J. (2021) 9:E548–55. doi: 10.9778/cmajo.20200302
142. Goldman RD, Krupik D, Ali S, Mater A, Hall JE, Bone JN, et al. Caregiver willingness to vaccinate their children against COVID-19 after adult vaccine approval. Int J Environ Res Public Health. (2021) 18:10224. doi: 10.3390/ijerph181910224
143. Chen F, He Y, Shi Y. Parents’ and guardians’ willingness to vaccinate their children against COVID-19: a systematic review and meta-analysis. Vaccines. (2022) 10:179. doi: 10.3390/vaccines10020179
Keywords: vaccine hesitancy, COVID-19, parental concern, vaccine acceptance, side effects
Citation: Khan YH, Rasheed M, Mallhi TH, Salman M, Alzarea AI, Alanazi AS, Alotaibi NH, Khan S-U-D, Alatawi AD, Butt MH, Alzarea SI, Alharbi KS, Alharthi SS, Algarni MA, Alahmari AK, Almalki ZS and Iqbal MS (2022) Barriers and facilitators of childhood COVID-19 vaccination among parents: A systematic review. Front. Pediatr. 10:950406. doi: 10.3389/fped.2022.950406
Received: 22 May 2022; Accepted: 14 September 2022;
Published: 24 November 2022.
Edited by:
Malik Sallam, The University of Jordan, JordanReviewed by:
Christian Napoli, Sapienza University of Rome, ItalyAaliyah M. Momani, Applied Science Private University, Jordan
Srikanth Umakanthan, The University of the West Indies St. Augustine, Trinidad and Tobago
Copyright © 2022 Khan, Rasheed, Mallhi, Salman, Alzarea, Alanazi, Alotaibi, Khan, Alatawi, Butt, Alzarea, Alharbi, Alharthi, Algarni, Alahmari, Almalki and Iqbal. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yusra Habib Khan, yusrahabib@ymail.com; yhkhan@ju.edu.sa; Tauqeer Hussain Mallhi, thhussain@ju.edu.sa; Tauqeer.hussain.mallhi@hotmail.com
 Yusra Habib Khan
Yusra Habib Khan