- 1Department of Neonatology, Fujian Maternity and Child Health Hospital College of Clinical Medicine for Obstetrics and Gynecology and Pediatrics, Fujian Medical University, Fuzhou, China
- 2Department of Neonatology, Northwest Women’s Children’s Hospital, Xi’an, China
- 3NHC Key Laboratory of Neonatal Diseases (Fudan University), Children’s Hospital of Fudan University, Shanghai, China
- 4Department of Neonatology, Children’s Hospital of Fudan University, Shanghai, China
- 5Department of Neonatology, Guiyang Maternal Child Health Care Hospital, Guiyang, China
- 6Department of Neonatology, Shanghai Children’s Medical Center, Shanghai Jiao Tong University School of Medicine, Shanghai, China
- 7Maternal-Infant Care Research Centre and Department of Pediatrics, Mount Sinai Hospital, Toronto, ON, Canada
- 8University of Toronto, Toronto, ON, Canada
Background: Previous studies demonstrated high rates of discharge against medical advice (DAMA) among very preterm infants (VPIs) in China.
Objectives: The aim of this study was to investigate the concurrent incidence, variation, and predictors of DAMA, along with the effect of DAMA on mortality of VPIs in China using data from the Chinese Neonatal Network (CHNN).
Methods: All infants born at 24–31 completed weeks’ gestation and admitted to 57 CHNN neonatal intensive care units (NICUs) in 2019 were included for this cohort study, excluding infants with major congenital anomalies. Patient information was prospectively collected using the CHNN database. Multivariable log-linear regression analysis was used to assess the association of perinatal factors and DAMA.
Results: A total of 9,442 infants born at 24–31 completed weeks’ gestation and admitted to 57 CHNN participating sites in 2019 were included in the study. Overall, 1,341 infants (14.2%) were discharged against medical advice. Rates of DAMA decreased with increasing gestational age (GA), and infants with lower GA were discharged earlier. DAMA infants had significantly higher rates of necrotizing enterocolitis, severe brain impairment, and bronchopulmonary dysplasia than non-DAMA infants. A total of 58.2% DAMA infants were predicted to die after discharge. The attributable risk percentage of mortality among DAMA infants was 92.4%. Younger maternal age, lower gestational age, small for gestational age, and Apgar score ≤3 at 5 min were independently associated with an increased risk of DAMA, while infants with antenatal steroids were less likely to be DAMA.
Conclusion: The rate of DAMA in preterm infants between 24 and 31 weeks’ gestation remained high in China with a significant impact on the mortality rates. Continuous efforts to reduce DAMA would result in substantial improvement of outcomes for VPIs in China.
Introduction
Infants born at less than 32 weeks (very preterm infants, VPIs) account for about 15–16% of all preterm births, with the highest mortality and morbidity rates (1, 2). In China and many other middle- or low-income countries, it has been reported that discharge against medical advice (DAMA) contributes significantly to the high mortality and morbidity of VPIs (3–8). DAMA refers to a situation wherein parents terminate treatment before the treating physicians recommend discharge. With limited physiological reserve of VPIs, they are at a very high risk of adverse outcomes in morbidity and mortality after DAMA (3, 4). Previous literature demonstrated that 70% of VPIs died following DAMA in China (9). Therefore, it is essential to collect detailed and high-quality data on DAMA of VPIs in China and to explore possible modified practices, aiming to reduce DAMA and improve overall outcomes of VPIs.
The Chinese Neonatal Network (CHNN) is a national collaborative research network focusing on neonatal and perinatal clinical studies in China (10). Established in 2018, CHNN has been maintaining a standardized database for all VPIs or very low birth weight infants admitted to NICUs across China from 1 January 2019. The objective of this study was to investigate the incidence, site variation, and predictors of DAMA, along with the impact of DAMA on mortality of VPIs in China using data from the CHNN.
Materials and methods
Study setting
This cohort study used the prospectively collected data from CHNN database. A total of 57 tertiary hospitals from 25 provinces and municipalities across China collected the whole year data using CHNN database in 2019, including all three national medical centers of children, all five regional medical centers of children, 30 provincial perinatal or children’s medical centers, and 19 major referral centers in large cities across China. Notably, 43 hospitals were perinatal centers with delivery facilities, and 14 hospitals were free-standing children’s hospitals. The ethics review board approved this study of Children’s Hospital of Fudan University (No. 2018-296), which all participating hospitals recognized. Waiver of consent was granted at all sites because of de-identified patient data.
The incidence of preterm birth in China was about 7.04% in 2015–2016 (11), with approximately 160,000 VPIs born in China each year (2). Therefore, CHNN database covered around 5% of VPIs who were born in China. VPIs not included in the database were either admitted to other NICUs or lower-level units, or not admitted to NICUs for treatment. Therefore, our data only represent outcomes of VPIs who received the highest level of care in major tertiary NICUs in China.
Study design and population
All infants born at 24–31 completed weeks’ gestation and admitted to CHNN-participating neonatal intensive care units (NICUs) between 1 January 2019 and 31 December 2019 were eligible for this study. Infants with major congenital anomalies were excluded. Stillborn, delivery room deaths, moribund neonates on admission, and infants transferred to non-participating hospitals within 24 h after birth were not captured by the CHNN database. Re-admissions and transfers between participating hospitals were tracked as data from the same infants. Infants were followed until death or discharge.
Data collection
Patient information was abstracted from patient charts by trained personnel using predefined standard definitions. Data were directly entered into a customized data entry program with built-in error checking. Data were subsequently sent electronically to the CHNN coordinating center located at the National Children’s Medical Center in Children’s Hospital of Fudan University in Shanghai, with patient identity kept confidential. Site investigator was responsible for data quality control in each site. The coordinating center checked data for quality and completeness and conducted audits to ensure the quality of data (12).
Exposure
Discharge against medical advice, which is the exposure, was defined as when parents terminated treatment before the treating physicians recommended discharge according to discharge criteria in participating NICUs.
Outcomes
Outcomes included mortality (primary outcome) and the five major neonatal morbidities, including necrotizing enterocolitis (NEC), severe brain injury, sepsis, bronchopulmonary dysplasia (BPD), and severe retinopathy of prematurity (ROP).
We did not follow up the DAMA infants after discharge and there were no other reliable sources of the information on the outcome of these infants. Therefore, we used predefined criteria to predict the likelihood of death for DAMA infants (13). If infants required invasive or non-invasive mechanical ventilation, inotropes infusion, or total parenteral nutrition (no enteral feeds initiated) on the day of discharge, we considered that they would not survive after discharge.
For morbidities, NEC was defined as stage ≥2 according to Bell’s stage (14, 15). Severe brain impairment was defined as degree ≥3 intraventricular hemorrhage (IVH) or cystic periventricular leukomalacia (cPVL). The diagnosis of severity of IVH was according to Papile’s criteria (16). cPVL was defined as the presence of periventricular cysts on cranial ultrasound or magnetic resonance imaging. Sepsis was defined as positive blood or cerebrospinal fluid culture (17). BPD was defined as ventilation or oxygen dependency at 36 weeks’ corrected age or at discharge, transfer, or death before 36 weeks (18). Severe ROP was defined as ROP stage III or above.
Covariable definitions
Gestational age (GA) was determined using the hierarchy of best obstetric estimate based on prenatal ultrasound, menstrual history, obstetric examination, or all three. If the obstetric estimate was not available or was different from the postnatal pediatric estimate of gestation by more than 2 weeks, the GA was estimated using the Ballard score (19). Small for gestational age (SGA) was defined as birth weight <10th percentile for the GA according to the Chinese neonatal birth weight values (20). Prenatal care was defined as at least one pregnancy-related hospital visit during pregnancy. Antenatal steroids were defined as partial or complete courses of antenatal corticosteroids before birth.
Statistical analysis
We described demographic characteristics by DAMA and non-DAMA group and provided crude risk ratios with 95% confidence interval to show the observed association between characteristics and DAMA. Kaplan–Meier curves were used to show the probability of non-DAMA over time after birth, while log-rank tests were applied to examine whether the probabilities were significantly different across GA groups. The Cochran–Armitage trend test was applied to examine the significance of the association between rate of DAMA and GA, and Jonckheere–Terpstra trend test was applied to determine the association between the median age at DAMA and GA. Attributable risk percent (ARP) was calculated to show the percentage of neonatal mortality that is predicted to be related to DAMA.
Multivariable log-linear regression models were used to measure the independent association between DAMA and perinatal factors. The model accounted for the cluster effect of different sites by applying generalized estimating equations.
Missing data
The proportion of missing data were <10% for those variables included in the model and we believed that the data were not missing at random; therefore, we did not do multiple imputation. The data management and all statistical analyses were performed using SAS version 9.4 (SAS Institute, Inc., Cary, NC, United States). All analysis is done by SAS 9.4 software.
Results
Rates of discharge against medical advice
During the study period, a total of 9,520 infants born at 24–31 completed weeks’ gestation were admitted to 57 CHNN sites, and 78 patients were excluded for major congenital anomalies. Thus, 9,442 cases were finally included in our study (Figure 1).
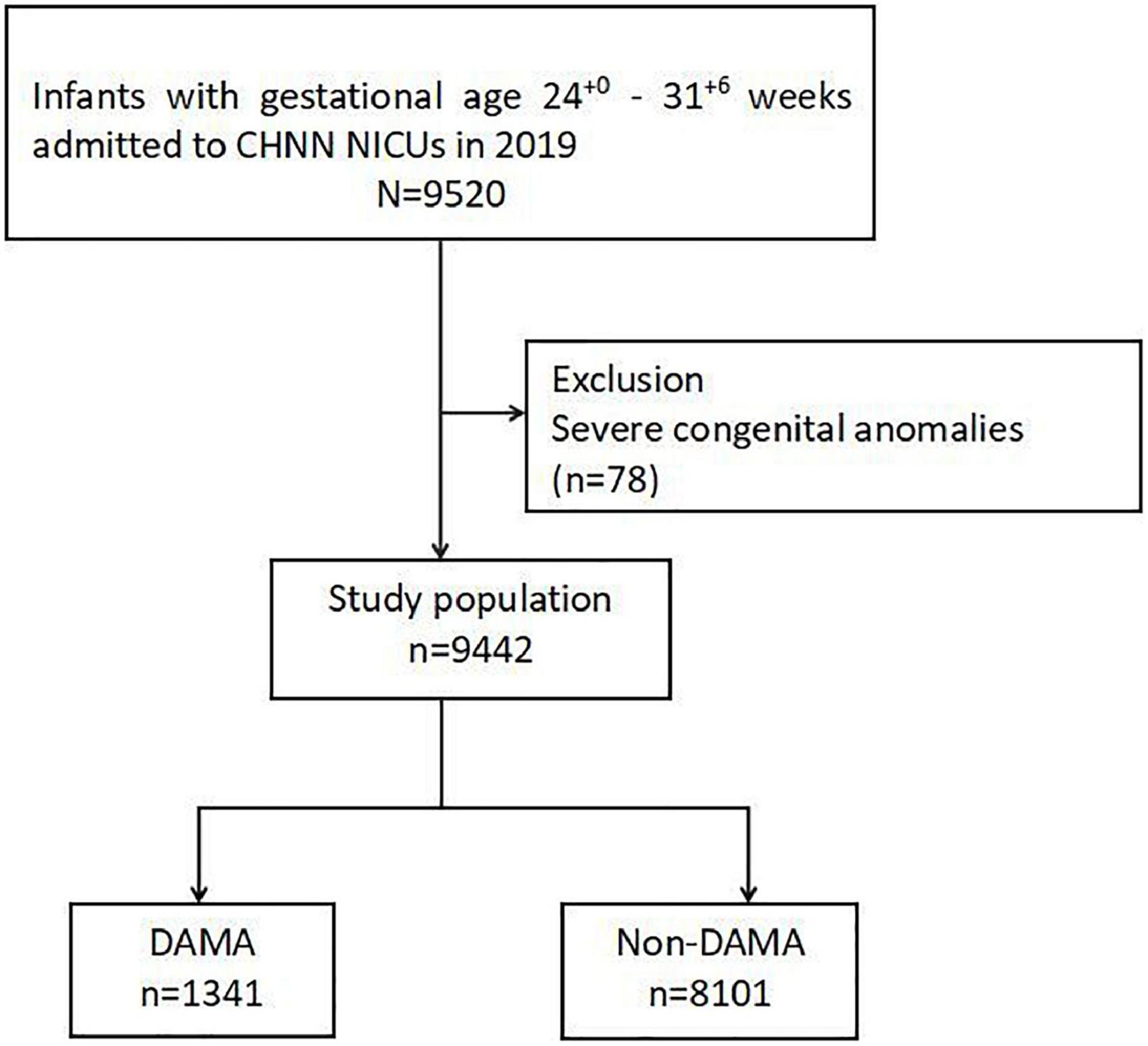
Figure 1. Study population. CHNN, Chinese Neonatal Network; DAMA, discharge against medical advice; NICU, neonatal intensive care unit.
Overall, 1,341 infants (14.2%) were discharged against medical advice (Figure 1). Rates of DAMA decreased with increasing GA (Table 1). DAMA rates reached the peak of 43.5% at the GA of 24 weeks, while there were still 10.0% of infants born at 31 weeks discharged against medical advice.
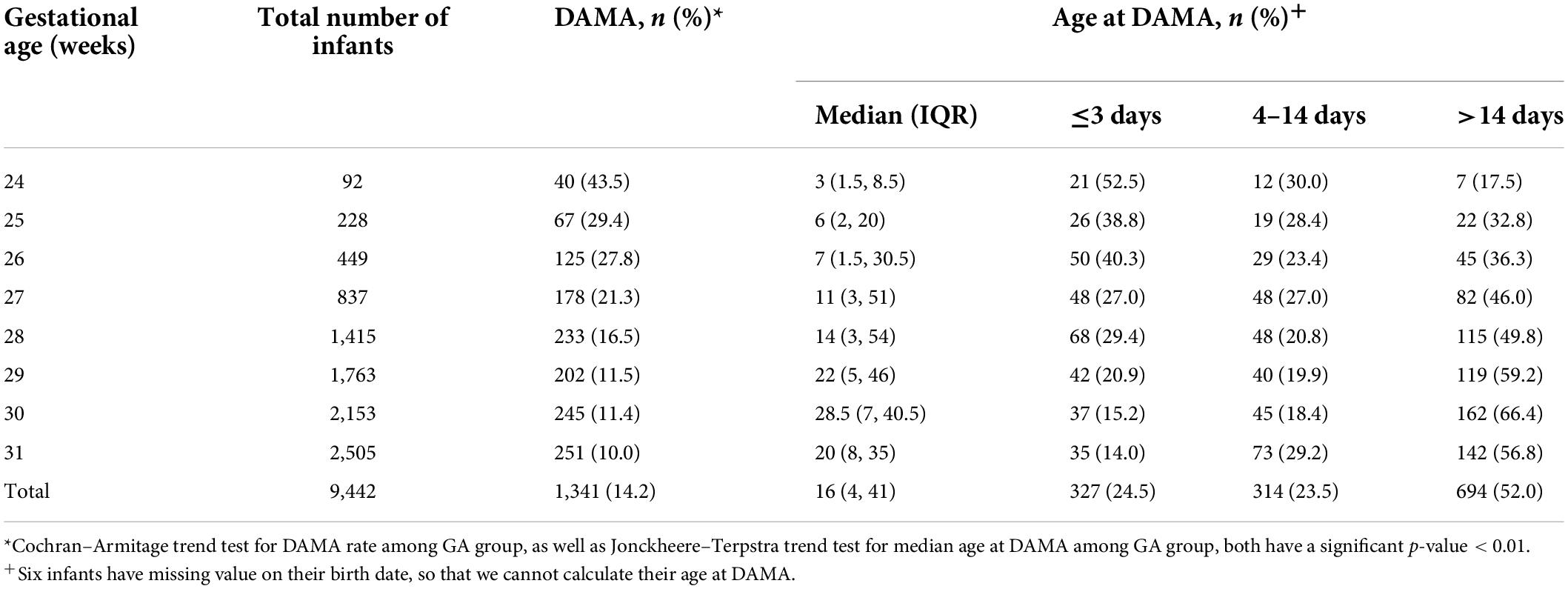
Table 1. Rates of discharge against medical advice among infants born at 24+0–31+6 weeks’ gestation in Chinese NICUs by gestational age.
There was a huge variation of DAMA rates among different hospitals (Supplementary Figure 1). The range of DAMA rates among different hospitals was from 0 to 66.7% in 24–27 weeks infants, and 0.9–34.8% in 28–31 weeks infants.
Age at discharge against medical advice
The median age at discharge for DAMA infants was 16 (IQR: 4–41) days. Age at discharge decreased with decreasing GA (Table 1 and Supplementary Figure 2). DAMA infants at 24 weeks were most likely to be discharged within 3 days after birth. In comparison, the majority of DAMA infants at 29–31 weeks were discharged after 14 days after birth.
Maternal and infant characteristics
Baseline characteristics are summarized in Table 2. Infants in the DAMA group had lower GA and lower birth weight than infants who received complete care. They were also more likely to be female and outborn. Their mothers were younger, less likely to have maternal diabetes, and premature rupture of membranes. They were less likely to receive antenatal steroids and antenatal antibiotics and be delivered by cesarean section, compared with the non-DAMA group. Infants in the DAMA group were more likely to be SGA and had low Apgar scores (≤3) at 5 min.
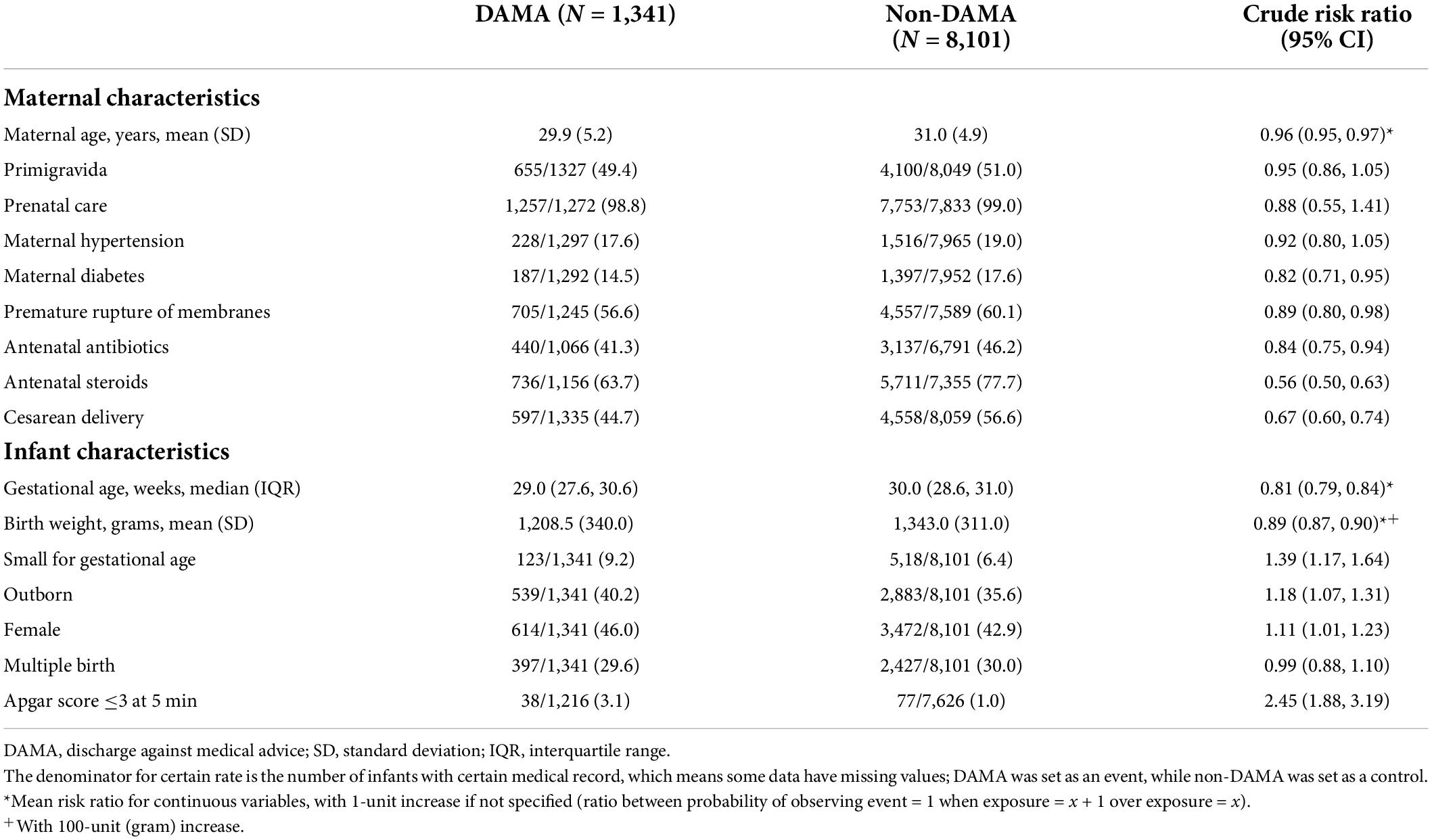
Table 2. Baseline characteristics among infants born at 24+0–31+6 weeks’ gestation in China by DAMA and non-DAMA group.
Morbidities and mortality among discharge against medical advice infants
Discharge against medical advice infants had higher rates of neonatal morbidities, including NEC, severe brain impairment, and BPD, compared with infants who received complete care (Table 3 and Supplementary Table 1). Overall, 58.2% (781/1,341) of DAMA infants required at least one type of intensive treatment at the time of discharge; hence, they were predicted to die after discharge (Supplementary Table 2). The predicted mortality among DAMA infants was 80.5 and 48.4% for infants <28 and 28–31 weeks, which was significantly higher than the observed mortality among infants who received complete care (14.2 and 6.4%, respectively) (Table 4).
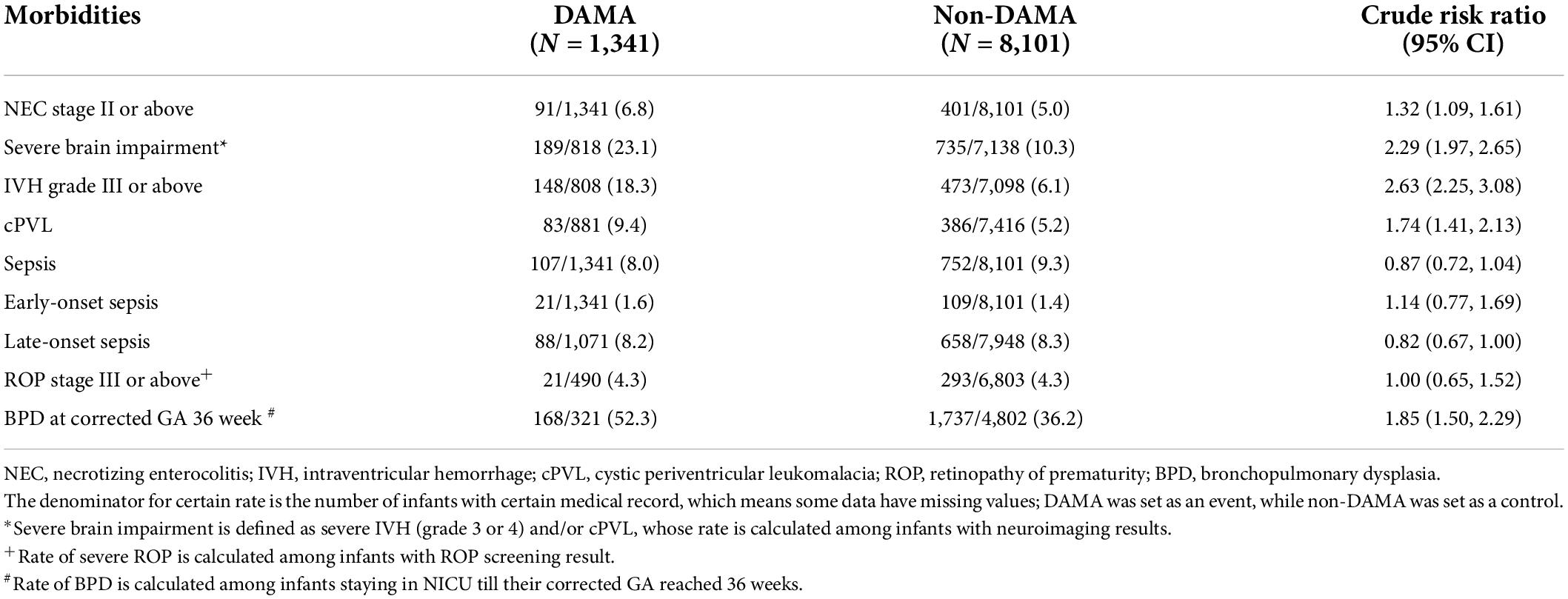
Table 3. Major neonatal morbidities among infants born at 24+0–31+6 weeks’ gestation in China by DAMA and non-DAMA group.
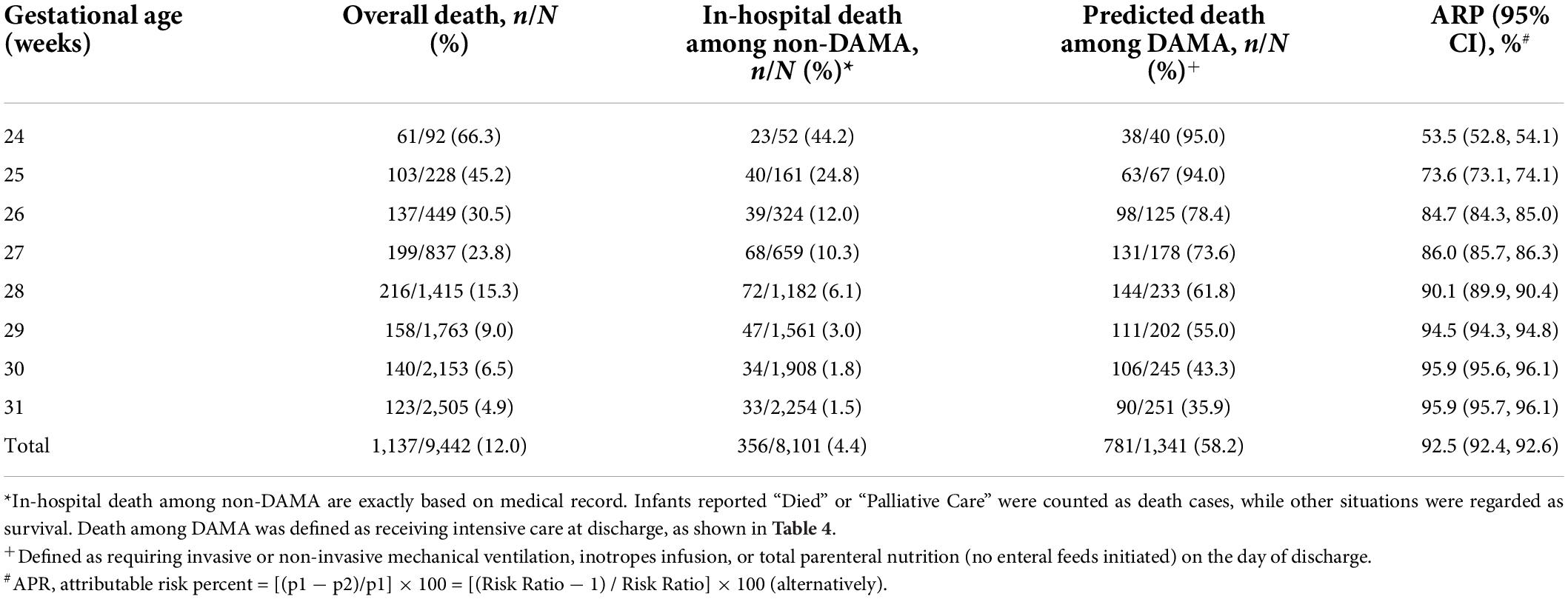
Table 4. Neonatal mortality of DAMA and non-DAMA infants born at 24+0–31+6 weeks’ gestation in China.
Overall, the attributable risk percentage of mortality was 92.4% among DAMA VPIs. The attributable risk percentage of DAMA on mortality increased with advancing GA (Table 4).
Risk factors for discharge against medical advice
Younger mother, lower GA (24–28 weeks), SGA, and Apgar score ≤3 at 5 min were independently associated with an increased risk of DAMA. Infants who received antenatal steroids were less likely to be DAMA (Table 5).
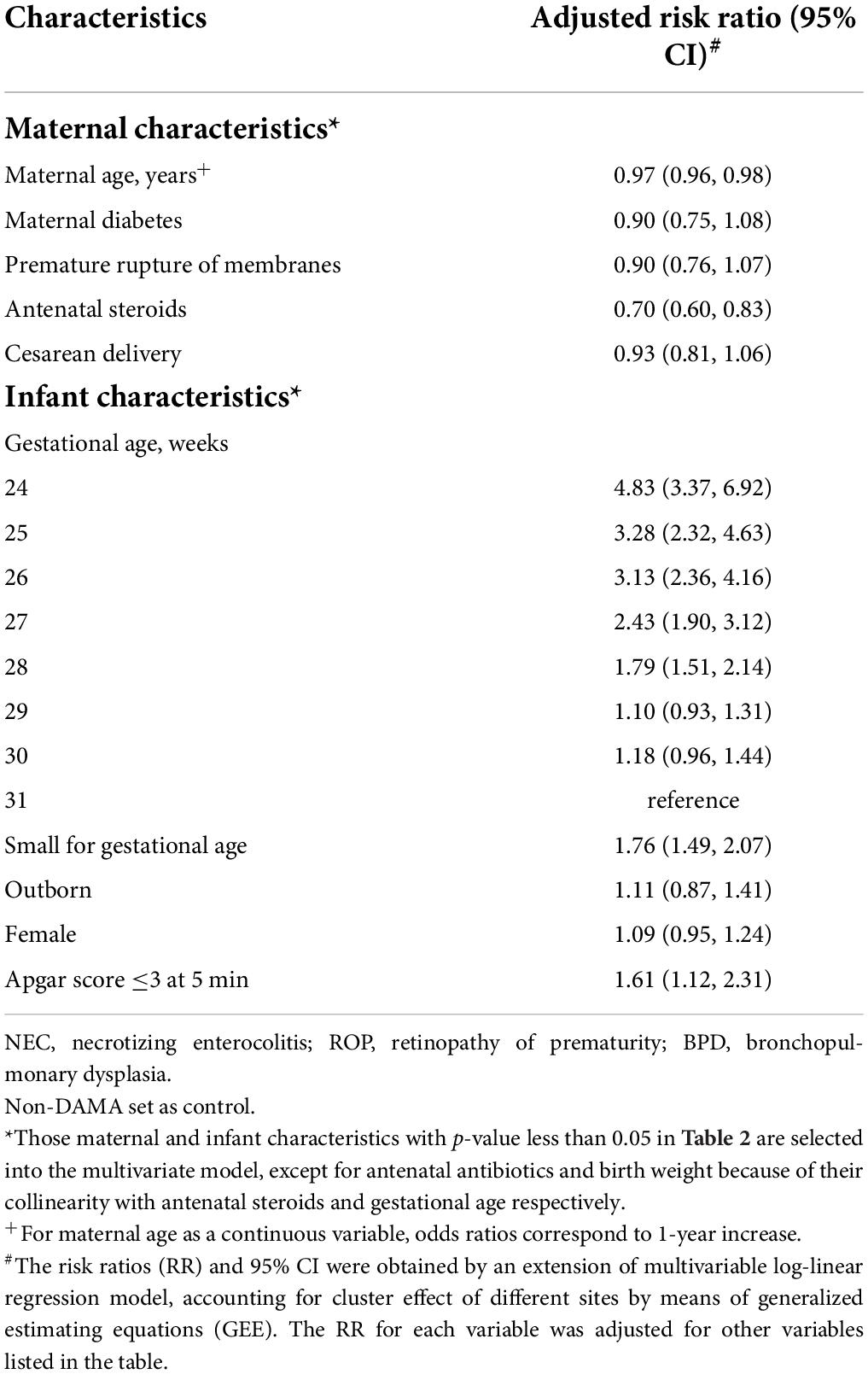
Table 5. Perinatal factors associated with DAMA among infants born at 24+0–31+6 weeks’ gestation in China.
Discussion
To the best of our knowledge, our report is the largest and latest nationwide study focusing on DAMA of VPIs in China. We identified a high rate of DAMA and substantial variation among different hospitals among VPIs in China. DAMA infants had high rates of severe brain impairment, BPD, and NEC, and showed a significant impact on mortality of VPIs. Younger maternal age, lower GA, SGA, and Apgar score ≤3 at 5 min were independently associated with an increased risk of DAMA, while antenatal steroids were associated with a decreased risk of DAMA.
Previous studies indicated near 21% of neonates with respiratory failure were DAMA in China in 2007–2008 (6–8). Jiang reported that the incidence of DAMA among VPIs in China was 19.7% in 2015–2016 and 13.3% in 2015–2018 (3, 13). Given the observed 14.2% DAMA rates among VPIs in our study, it has to be acknowledged that the rate of DAMA in preterm infants between 24 and 31 weeks’ gestation remained high in China. Therefore, targeted efforts are definitely needed to reduce further or eliminate DAMA.
One improvement target may focus on infants with relatively larger GA. There were still 10–11% of infants born at 31 and 30 weeks discharged prematurely, resulting in high mortality for these infants. Given the large proportion of these infants among all VPIs admitted to Chinese NICUs, reducing DAMA rates among infants at 30–31 weeks will result in a significant reduction of the absolute number of DAMA.
The in-hospital mortality rate of VPIs with complete care in our research was close to that in developed countries, such as the Canada Neonatal Network (CNN) in the same period (4.4% in CHNN vs. 4.8% in CNN) (21). However, our data confirmed that the in-hospital mortality rates for VPIs in China should be interpreted with caution due to the high rate of DAMA and high mortality among DAMA infants. After taking DAMA infants into consideration, the overall mortality rates almost tripled. Also, DAMA infants showed higher rates of major neonatal morbidities. Therefore, when monitoring outcomes longitudinally or comparing outcomes regionally, nationally, or internationally, the DAMA infants should be taken into consideration to avoid overly optimistic estimates.
The attributable risk percentage of mortality was 92.4% among DAMA VPIs in our study, which means that 92.4% of deaths among DAMA infants might be related to the DAMA decision. However, these data should be interpreted with caution. In many instances, DAMA is likely to be motivated by a poor prognosis with regard to impending death or serious disability. Therefore, the overall attributable risk percentage of 92.4% might overestimate the proportion of deaths due to the DAMA decision. Anyhow, efforts to reduce DAMA rates will substantially decrease the mortality of VPIs in Chinese NICUs. Also, one cohort study estimated potential outcomes of DAMA among VPIs in China if they receive complete care based on outcomes of a group of propensity score matched non-DAMA infants. The studies found that 59% DAMA infants aged <32 weeks might have intact survival if intensive care services are provided (13).
Our data showed that infants with the youngest GA were mostly discharged within 3 days after birth, which indicated that parents tended to make an early decision of DAMA for infants with lower GA. Their discharge might be due to parents’ concerns about the continuing suffering and grave outcomes, in terms of death or adverse neurodevelopmental outcomes. It probably reflected their lack of confidence in the chance of survival and outcome of infants born at lower GA both from parents and health providers. However, in recent decades, there have been major advances in the survival rate and outcome of infants with the smallest GAs in China (3, 10, 13). Obstetricians and neonatologists need to be aware of the latest data and inform families to make appropriate choices. For those infants with higher GA (29–31 weeks), their discharge might be associated with neonatal morbidities, which might be a serious blow for parents, giving most of them discharged after 14 days of life. Our data demonstrated that more infants in the DAMA group had severe brain impairment than the non-DAMA group, suggesting that fears for poor long-term outcomes might be one of the major reasons parents terminate the treatment of their babies. There were also more NEC and BPD in the DAMA group than in the non-DAMA group in VPIs. Therefore, more effort should be made to reduce those morbidities in VPIs. Our study also identified that perinatal factors, including low GA, SGA, younger mother, and low Apgar score at 5 min, were associated with an increased risk of DAMA, while antenatal steroids served as a protective factor for DAMA. Appropriate perinatal care may also contribute to the reduction of DAMA.
According to the published literature, besides concern about poor prognosis, the inability to afford the cost might also be a major reason for DAMA (22–24). However, increasing coverage of health insurance for neonates across China, change of one-child policy, and improving neonatal intensive care may result in changes in decision making of DAMA. Unfortunately, we did not collect information on the reasons for DAMA in our study. However, by recognizing this remaining problem, CHNN has launched targeted quality improvement initiatives aiming to reduce DAMA, with the first step as a prospective survey on specific DAMA reasons.
The development of neonatology and neonatal intensive care has been uneven among different districts in China. As found in our study, previous reports also showed significant variation of mortality and DAMA among VPIs in different hospitals in China (3, 4). Besides the variations in medical practice, there are various reasons for this wide variation of DAMA rates among different NICUs in China, which might include the sociocultural, socioeconomic, religious, and ethnic differences. Unfortunately, we did not collect this relevant information, so we were unable to perform a rigorous analysis of the causes of this variation. Recognizing these remaining problems, relevant studies organized by CHNN are underway. And a national network-level collaborative, a multifaceted quality improvement approach may be helpful to decrease the rate of DAMA via benchmarking, best-practice consensus, and sharing expertise.
Our study has several strengths. Our data were from the multicenter standardized database with clear definitions of variables and strict quality control, which reduced information bias. All participating NICUs were large tertiary centers representing the highest level of neonatal care in representing areas of China, which made the comparison of data reasonable. The large sample size enabled detailed stratification of GA, which can provide health providers and policymakers a more precise reference at each week of GA.
There were several limitations in our study. First, this is a hospital-based study instead of a population-based study. Delivery room deaths and live births without active resuscitation who were never admitted to NICUs were not included. This would result in an underestimation of the DAMA rate. Second, we did not actually follow up the DAMA infants after discharge, so we could not obtain an accurate mortality rate for these infants. Third, we could not identify specific reasons for DAMA and the causes of variability of DAMA rates among different NICUs because the database did not include such information.
Conclusion
Discharge against medical advice among VPIs has been decreasing over the past few years but remained high. DAMA had a significant impact on the mortality of VPIs in China. Continuous efforts to reduce DAMA would result in substantial improvement of outcomes for VPIs in China.
Members of the Chinese Neonatal Network
Chairmen: Chao Chen, Children’s Hospital of Fudan University; Shoo K. Lee, Mount Sinai Hospital, University of Toronto. Vice-Chairmen: Lizhong Du, Children’s Hospital of Zhejiang University School of Medicine; Wenhao Zhou, Children’s Hospital of Fudan University. Site principle investigators of the Chinese Neonatal Network: Children’s Hospital of Fudan University: Yun Cao; The Third Affiliated Hospital of Zhengzhou University: Falin Xu; Tianjin Obstetrics & Gynecology Hospital: Xiuying Tian; Guangzhou Women and Children’s Medical Center: Huayan Zhang; Children’s Hospital of Shanxi: Yong Ji; Northwest Women’s and Children’s Hospital: Zhankui Li; Gansu Provincial Maternity and Child Care Hospital: Jingyun Shi; Shengjing Hospital of China Medical University: Xindong Xue; Shenzhen Maternity and Child Health Care Hospital: Chuanzhong Yang; Quanzhou Women and Children’s Hospital: Dongmei Chen; The Affiliated Suzhou Hospital of Nanjing Medical University: Sannan Wang; Guizhou Women and Children’s Hospital/Guiyang Children’s Hospital: Ling Liu; Hunan Children’s Hospital: Xirong Gao; The First Bethune Hospital of Jilin University: Hui Wu; Fujian Maternity and Child Health Hospital, Affiliated Hospital of Fujian Medical University: Changyi Yang; Nanjing Maternity and Child Health Care Hospital: Shuping Han; Qingdao Women and Children’s Hospital: Ruobing Shan; The Affiliated Hospital of Qingdao University: Hong Jiang; Children’s Hospital of Shanghai: Gang Qiu; Women and Children’s Hospital of Guangxi Zhuang Autonomous Region: Qiufen Wei; Children’s Hospital of Nanjing Medical University: Rui Cheng; Henan Children’s Hospital: Wenqing Kang; The First Affiliated Hospital of Xinjiang Medical University: Mingxia Li; Foshan Women and Children’s Hospital: Yiheng Dai; The First Affiliated Hospital of Anhui Medical University: Lili Wang; Shanghai First Maternity and Infant Hospital: Jiangqin Liu; Yuying Children’s Hospital Affiliated to Wenzhou Medical University: Zhenlang Lin; Children’s Hospital of Chongqing Medical University: Yuan Shi; The First Affiliated Hospital of Zhengzhou University: Xiuyong Cheng; The First Affiliated Hospital of USTC, Division of Life Sciences and Medicine, University of Science and Technology of China: Jiahua Pan; Shaanxi Provincial People’s Hospital: Qin Zhang; Children’s Hospital of Soochow University: Xing Feng; Wuxi Maternity and Child Healthcare Hospital: Qin Zhou; People’s Hospital of Xinjiang Uygur Autonomous Region: Long Li; The Second Xiangya Hospital of Central South University: Pingyang Chen; Qilu Children’s Hospital of Shandong University: Xiaoying Li; Hainan Women and Children’s Hospital: Ling Yang; Xiamen Children’s Hospital: Deyi Zhuang; Xinhua Hospital Affiliated to Shanghai Jiao Tong University School of Medicine: Yongjun Zhang; Shanghai Children’s Medical Center, Shanghai Jiao Tong University School of Medicine: Jianhua Sun; Shenzhen Children’s Hospital: Jinxing Feng; Children’s Hospital Affiliated to Capital Institute of Pediatrics: Li Li; Women and Children’s Hospital, School of Medicine, Xiamen university: Xinzhu Lin; General Hospital of Ningxia Medical University: Yinping Qiu; First Affiliated Hospital of Kunming Medical University: Kun Liang; Hebei Provincial Children’s Hospital: Li Ma; Jiangxi Provincial Children’s Hospital: Liping Chen; Fuzhou Children’s Hospital of Fujian Province: Liyan Zhang; First Affiliated Hospital of Xian Jiao Tong University: Hongxia Song; Dehong People’s Hospital of Yunnan Province: Zhaoqing Yin; Beijing Children’s Hospital, Capital Medical University: Mingyan Hei; Zhuhai Center for Maternal and Child Health Care: Huiwen Huang; Guangdong Women and Children’s Hospital: Jie Yang; Dalian Municipal Women and Children’s Medical Center: Dong Li; Peking Union Medical College Hospital: Guofang Ding; Obstetrics & Gynecology Hospital of Fudan University: Jimei Wang; Shenzhen Hospital of Hongkong University: Qianshen Zhang; Children’s Hospital of Zhejiang University School of Medicine: Xiaolu Ma; Advisor: Joseph Ting; University of Alberta.
Data availability statement
The datasets for this article are not publicly available because part of the data is included in another article under preparation. Requests to access the datasets should be directed to YC, eXVuY2FvQGZ1ZGFuLmVkdS5jbg==.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committee of the Children’s Hospital of Fudan University. Written informed consent from the participants’ legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author contributions
WX, RB, ZL, and CY: study concept and design. WX, RB, XG, SJ, YW, LL, JS, YC, WZ, SL, ZL, and CY: acquisition, analysis, and interpretation of data. WX, RB, XG, and SJ: drafting of manuscripts. All authors: critical revision of the manuscripts for important intellectual content. XG and SJ: statistical analysis. SL: obtained the funding. BZ, YD, LL, JS, YC, WZ, ZL, and CY: administrative and technical or maternal support. JS, YC, WZ, and SL: supervision.
Funding
SL was supported by the Canadian Institutes of Health Research (CTP87518). The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Acknowledgments
We thank the data abstractors from the Chinese Neonatal Network. We also thank all the staff at the Chinese Neonatal Network coordinating center for providing organizational support (Lin Yuan, Ph.D.; Tongling Yang, RN; Hao Yuan, RN; Li Wang, RN; and Yulan Lu, Ph.D.).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2022.943244/full#supplementary-material
References
1. Blencowe H, Cousens S, Chou D, Oestergaard M, Say L, Moller AB, et al. Born too soon: the global epidemiology of 15 million preterm births. Reprod Health. (2013) 10(Suppl. 1):S2. doi: 10.1186/1742-4755-10-S1-S2
2. Chawanpaiboon S, Vogel JP, Moller AB, Lumbiganon P, Petzold M, Hogan D, et al. Global, regional, and national estimates of levels of preterm birth in 2014: a systematic review and modelling analysis. Lancet Glob Health. (2019) 7:e37–46.
3. Jiang S, Yan W, Li S, Zhang L, Zhang Y, Shah PS, et al. Mortality and morbidity in infants <34 weeks’ gestation in 25 NICUs in China: a prospective cohort study. Front Pediatr. (2020) 8:33. doi: 10.3389/fped.2020.00033
4. Lin HJ, Du LZ, Ma XL, Shi LP, Pan JH, Tong XM, et al. Mortality and morbidity of extremely low birth weight infants in the mainland of China: a multi-center study. Chin Med J. (2015) 128:2743–50. doi: 10.4103/0366-6999.167312
5. Yang S, Cai S, Liao J, Peng X, Huang J. Risk factors and reasons for discharge against medical advice for Newborns with neonatal surgical diseases: a preliminary study from a tertiary care hospital in Beijing, China. Front Pediatr. (2020) 8:576270. doi: 10.3389/fped.2020.576270
6. Ma L, Liu CQ, Wang YQ, Li SF, Zhai SF, Gu XF, et al. Mortality of neonatal respiratory failure related to socioeconomic factors in Hebei Province of China. Neonatology. (2011) 100:14–22. doi: 10.1159/000320155
7. Wang HH, Gao XR, Liu CQ, Yan CY, Lin XZ, Yang CY, et al. Morbidity and mortality of neonatal respiratory failure in China: surfactant treatment in very immature infants. Pediatrics. (2012) 129:E731–40. doi: 10.1542/peds.2011-0725
8. Zhang L, Qiu Y, Yi B, Ni L, Zhang L, Taxi P, et al. Mortality of neonatal respiratory failure from Chinese northwest NICU network. J Mater Fetal Neonatal Med. (2017) 30:2105–11. doi: 10.1080/14767058.2016.1238894
9. Collaborative Study Group for Extremely Preterm and Extremely Low Birth Weight Infants. Survival and mortality rate of extremely preterm and extremely low birth weight infants admitted to neonatology departments (in Chinese). Chin J Pediatr. (2014) 52:72935.
10. Cao Y, Jiang S, Sun J, Hei M, Wang L, Zhang H, et al. Chinese neonatal network. Assessment of neonatal intensive care unit practices, morbidity, and mortality among very preterm infants in China. JAMA Netw Open. (2021) 4:e2118904. doi: 10.1001/jamanetworkopen.2021.18904
11. Jing S, Chen C, Gan Y, Vogel J, Zhang J. Incidence and trend of preterm birth in China, 1990-2016: a systematic review and meta-analysis. BMJ Open. (2020) 10:e039303. doi: 10.1136/bmjopen-2020-039303
12. Sun J, Cao Y, Hei M, Sun H, Wang L, Zhou W, et al. Data quality improvement and internal data audit of the Chinese neonatal network data collection system. Front Pediatr. (2021) 9:711200. doi: 10.3389/fped.2021.711200
13. Jiang S, Huang X, Zhang L, Han J, Yang Y, Wang W, et al. Reduction of infection in neonatal intensive care units using the evidence-based practice for improving quality (REIN-EPIQ) study group. Estimated survival and major comorbidities of very preterm infants discharged against medical advice vs treated with intensive care in China. JAMA Netw Open. (2021) 4:e2113197. doi: 10.1001/jamanetworkopen.2021.13197
14. Bell MJ, Ternberg JL, Feigin RD, Keating JP, Marshall R, Barton L, et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann Surg. (1978) 187:1–7. doi: 10.1097/00000658-197801000-00001
15. Walsh MC, Kliegman RM. Necrotizing enterocolitis – treatment based on staging criteria. Pediatr Clin N Am. (1986) 33:179–201. doi: 10.1016/s0031-3955(16)34975-6
16. Papile L-A, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr. (1978) 92:529–34. doi: 10.1016/s0022-3476(78)80282-0
17. Jiang S, Yang C, Yang C, Yan W, Shah V, Shah PS, et al. Epidemiology and microbiology of late-onset sepsis among preterm infants in China, 2015–2018: a cohort study. Int J Infect Dis. (2020) 96:1–9. doi: 10.1016/j.ijid.2020.03.034
18. Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. (2001) 163:1723–9. doi: 10.1164/ajrccm.163.7.2011060
19. Ballard JL, Novak KK, Driver M. A simplified score for assessment of fetal maturation of newly born infants. J Pediatr. (1979) 95(5 Pt 1):769–74. doi: 10.1016/s0022-3476(79)80734-9
20. Zhu L, Zhang R, Zhang S, Shi W, Yan W, Wang X, et al. Chinese neonatal birth weight curve for different gestational age. Chin J Pediatr. (2015) 53:97–103.
21. The Canadian Neonatal Network. Canadian Neonatal Network 2019 Annual Report. (2016). Available online at: http://www.canadianneonatalnetwork.org/portal/ (accessed March 6, 2021).
22. Al-Turkistani HK. Discharge against medical advice from neonatal intensive care unit: 10 years experience at a university hospital. J Family Commun Med. (2013) 20:113–5. doi: 10.4103/2230-8229.114774
23. Devpura B, Bhadesia P, Nimbalkar S, Desai S, Phatak A. Discharge against medical advice at neonatal intensive care unit in Gujarat, India. Int J Pediatr. (2016) 2016:1897039. doi: 10.1155/2016/1897039
Keywords: discharge against medical advice, preterm infants, mortality, morbidity, risk factor
Citation: Xiu W, Bai R, Gu X, Jiang S, Zhang B, Ding Y, Wang Y, Liu L, Sun J, Cao Y, Zhou W, Lee SK, Li Z and Yang C (2022) Discharge against medical advice among infants with 24–31 weeks’ gestation admitted to Chinese neonatal intensive care units: A multicenter cohort study. Front. Pediatr. 10:943244. doi: 10.3389/fped.2022.943244
Received: 13 May 2022; Accepted: 18 July 2022;
Published: 16 August 2022.
Edited by:
Ju Lee Oei, University of New South Wales, AustraliaReviewed by:
Fielding Bruder Stapleton, University of Washington, United StatesRuth Gottstein, Manchester University NHS Foundation Trust (MFT), United Kingdom
Copyright © 2022 Xiu, Bai, Gu, Jiang, Zhang, Ding, Wang, Liu, Sun, Cao, Zhou, Lee, Li and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Changyi Yang, bmVvNTk1QDE2My5jb20=; Zhankui Li, MTM3NzIxNTEyMjlAMTYzLmNvbQ==
†These authors have contributed equally to this work and share first authorship
‡These authors have contributed equally to this work
 Wenlong Xiu
Wenlong Xiu Ruimiao Bai
Ruimiao Bai Xinyue Gu
Xinyue Gu Siyuan Jiang
Siyuan Jiang Baoquan Zhang1
Baoquan Zhang1 Yanchen Wang
Yanchen Wang Yun Cao
Yun Cao Wenhao Zhou
Wenhao Zhou Shoo K. Lee
Shoo K. Lee Changyi Yang
Changyi Yang