- 1Department of Children Health and Development, Capital Institute of Pediatrics, Beijing, China
- 2National Institute for Nutrition and Health, Chinese Center for Disease Control and Prevention, Beijing, China
- 3National Center for Women and Children’s Health, Chinese Center for Disease Control and Prevention, Beijing, China
Objective: The purpose of this survey was to explore the association of delivery mode with overweight and neurodevelopment of Chinese infants aged 1–5 months.
Materials and methods: This study was based on a cross-sectional survey. Data for this study were obtained from the Children’s Nutrition and Health System Survey in China which was conducted from 2019 to 2020. Characteristics of parents and children and the delivery mode were obtained using interview-administered questionnaires. Body mass index-for age z-score (BMI z) was calculated using World Health Organization (WHO) child growth standards. Children’s neurodevelopment was assessed by a trained child health care physician using the Child Psychological Development Scale. The association of delivery mode with infant overweight was analyzed using a multivariable logistic regression model. We conducted a multivariable linear regression model to explore the relationship between delivery modes with neurodevelopment.
Results: In total, the present analysis included 1,347 children aged 1–5 months, 35.61% were born via cesarean section, of which 15.21% were overweight. After adjustment for infant characteristics and parental factors, the cesarean section was significantly related with the likehood of being overweight [OR = 1.95; 95% confidence interval (CI): 1.27 to 2.98]. Children born via cesarean section had a 3.41-point decrease in gross motor development (β = −3.41; 95% CI: −5.77 to −1.05), a 3.65-point decrease in fine motor development (β = −3.65; 95% CI: −6.03 to −1.28), and a 2.96-point in language development (β = −2.96; 95% CI: −5.20 to −0.73), a 1.65-point in total development (β = −1.65; 95% CI: −3.17 to −0.14) compared with those who were vaginal birth.
Conclusion: In our study population, cesarean section was associated with overweight and neurodevelopment outcomes. The cesarean section might increase the likehood of infant overweight, and might decrease the developmental scores of gross motor, fine motor and language. Further studies should be conducted to verify the associations and explore the possible mechanisms.
Introduction
The rising rate of cesarean section has become a social public issue worldwide. Originally, the cesarean section was a life-saving surgery for women and newborns when complications occurred. Over time, the cesarean section rate in both developed and developing countries has increased rapidly. During the past three decades, global cesarean section rates have increased from approximately 6% in 1990 to 21% in 2015 (1), well above the 10–15% recommended by the WHO (2). In the United States, the cesarean section rate has increased from 27% in 1997 to 31.8% in 2011, the rate of cesarean section has increased from 18% in 1997 to 25% in 2010 in the United Kingdom, while in Iran, the cesarean section rate is almost 40% (3). Nevertheless, the proportion of cesarean section have risen from 18% in 1990–1992 to 34.9% in 2014 and was over 50% in some major cities of China (4). One study conducted in China from 2013 to 2016 showed 20% of cesarean section might be non-medically necessary (5). Previous research has found that cesarean section increases the risk of a variety of diseases in the offspring, including allergies (6), type 1 diabetes (7), overweight/obesity (8, 9) and may be linked to poor child cognitive outcome (10) and lower academic performance (11). Some studies have discussed the biological mechanism hypothesis of the relationship between cesarean section and the negative health of the offspring. The cesarean section may interfere sensory activation and immune due to be short of stress response, affect immune system development, modifying epigenetic regulation in DNA methylation, or disrupting bacterial colonization (10, 12).
The cesarean section was linked with childhood overweight and excess weight gain in the first 1,000 days (13, 14). The United States infants born by cesarean section gained more weight than those delivered vaginally (15). Compared to vaginal delivery, the risk of being overweight was 2.44 times higher for 1 year old infants born by elective cesarean section in an Indian study (14). Also, one Chinese cohort study showed that the risk of being overweight and obese increased by 24 and 29%, respectively, in preschool children delivered by cesarean section (8). However, few studies had reported that cesarean section was not significantly associated with overweight/obesity in children (16, 17). Whether cesarean section is associated with children’s development, the existing research is inconsistent. Previous studies have found that pre-labor cesarean section may be associated with school performance (11), and poor child cognitive score outcomes (10) and a higher incidence of autism spectrum disorders (18). Zaigham M et al. reported that the infants born by pre-labor cesarean section had obviously lower assessment scores in all developmental domains at the 4-month assessment and lower score in the gross-motor skills domain at the 12-month evaluation compared to vaginally born infants (19). But other studies did not support a strong link between cesarean section and neurodevelopment or poorer health in children (20, 21).
Given the inconsistencies of the findings, the conflicting results can be partly interpreted by different adjustment confounding factors, mainly the children’s age when the assessment was conducted. In China, few studies have explored the relationship between cesarean section and overweight in childhood; however, study sample didn’t focus on infants’ overweight. So, the hypothesis of this study was that there was a link between cesarean section and the infant’s overweight and neurodevelopment.
Materials and methods
Participants
This study was based on a cross-sectional survey. The data were extracted from the Children’s Nutrition and Health System Survey in China. The sampling method in this study has been detailed previously (22). In short, stratified multi-stage cluster sampling was used to select participants in each province. This study included children aged 1 to 5 months and the data were selected from nine provinces: Zhejiang (n = 156), Beijing (n = 143), Jilin (n = 148), Liaoning (n = 146), Shanxi (n = 152), Jiangxi (n = 146), Hunan (n = 164), Qinghai (n = 148), and Yunnan (n = 144). The survey was conducted in 2019–2020. The inclusion criteria were (1) healthy children who had lived locally at the survey site for more than 6 months; (2) birth weight ≥ 2,500 g; (3) gestational age ≥ 37 weeks; (4) not a twin or multiple births; and (5) having no serious illnesses or chronic health problems.
Anthropometrics
The infants’ weight and height were measured by well-trained staff from local Centers for Disease Control and Prevention and community health center according to standard procedures (23). The weight was measured on a lever scale to an accuracy of 0.1 kg. Length was measured using a pediatric length board to an accuracy of 0.1 cm with the infants in a recumbent position. The age-and sex-specific BMI z-scores (BMI z) was calculated according to the WHO Child Growth Standards for infants aged 0–60 months. Overweight of infants was categorized by BMI z ≥ 85th percentile.
Variables
Characteristics of parents, children, and the mode of delivery were obtained using interview-administered questionnaires. The mode of delivery was divided into cesarean section and vaginal delivery. Parental characteristics included maternal age (“< 35 years” or “≥ 35 years”), maternal education (“Bachelor and above” or “College” or “High school” or “Middle school and below”), gestational weight gain (continuous variable), paternal age (“< 35 years” or “≥ 35 years”), paternal education (“Bachelor and above” or “College” or “High school” or “Middle school and below”), and monthly household income per capita (“1,501–3,000 RMB” or “3,001–5,000 RMB” or “≥ 5,000 RMB”). The child characteristics comprised sex (“Male” or “Female”), birth weight (“Formal” or “Macrosomia”), feeding methods (“Breast feeding” or “Formula feeding” or “Mixed feeding”), residential area (“Urban” or “Rural”), and parity (“Primipara” or “Multipara”).
Assessment of neurodevelopment
The children’s neurodevelopment was assessed by a standardized trained child health care physician using the Child Psychological Development Scale (WS/T 580-2017). The scale is an effective, reliable, and accredited tool, developed by the Capital Institute of Pediatrics in China. This scale is used to assess the neurodevelopmental level of children aged 0–6 years and has been widely used in pediatric and maternal and child health care institutions in China since 1984. The scale is consisted of five domains (gross motor, fine motor, adaptability, language, and social behavior). And the developmental quotient (DQ, DQ = mental age÷actual age in months × 100) is used to assess children’s total neurodevelopmental level and five domains [gross motor development quotient (GMDQ), fine motor development quotient (FMDQ), adaptability developmental quotient (ADQ), language development quotient (LDQ), and social behavior developmental quotient (SBDQ)].
Statistical analysis
We used SAS for Windows, Version 9.2 (SAS Institute Inc., Cary, NC, United States) to conduct all the analyses in this study. Characteristics of the children and their parents were analyzed using t test for continuous measures or χ2 tests of independence (for categorical variables). Comparisons of DQs scores in different domains in cesarean section and vaginal delivery children were conducted using a t-test. The association of infant overweight with the delivery mode was examined using multivariable logistic regression, and we conducted multivariable linear regression models to assess the associations between DQ scores (total scale and five domains) and delivery models (cesarean section and vaginal delivery) after adjusting for several confounders (birth weight, maternal age, paternal age, gestational weight gain, child sex, delivery mode, residential area, maternal education, paternal education, parity, feeding methods, and monthly household income per capita). In all the statistical tests, P < 0.05 was considered statistical significance.
Results
Characteristics of the participants
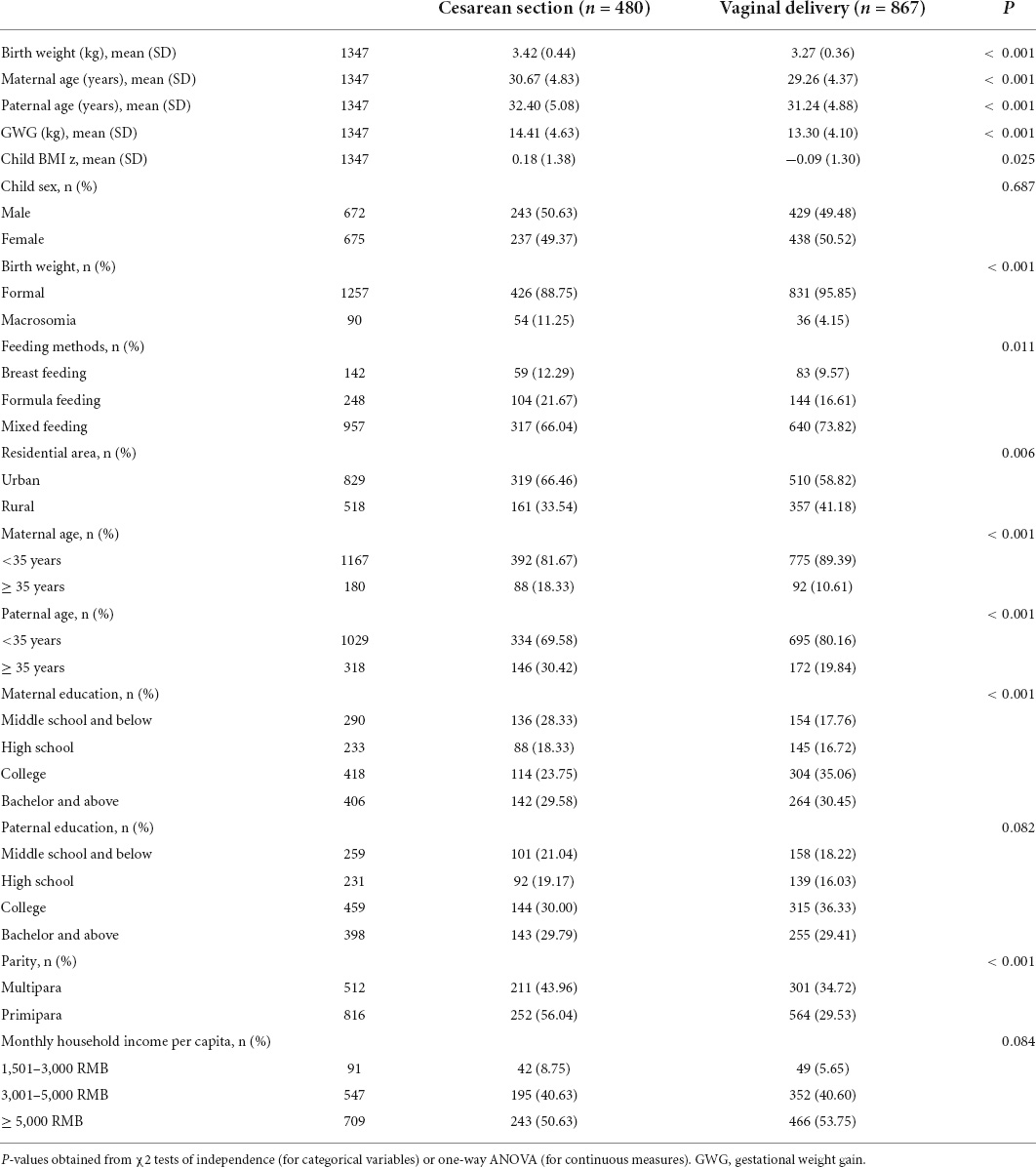
As shown in Table 1, our study included a total of 1,347 children aged 1–5 months. Approximately 35.63% of children (n = 480) were born by cesarean section and 64.37% of children (n = 867) were vaginal delivery. The mean maternal age was 29.97 years. Mothers who were 35 years or older, with a higher education level, who lived in an urban area, were primipara, and gained more weight during pregnancy were tend to deliver their children via cesarean section (p < 0.05). Out of 480 children born via cesarean section, the BMI z was 0.18 (SD: 1.38), of 11.25% were macrosomia and 21.67% were formula fed, and 16.61% of the vaginal delivery children were formula fed. Children’s sex, paternal education level, and monthly household income per capita were not significantly related with delivery mode (p > 0.05).
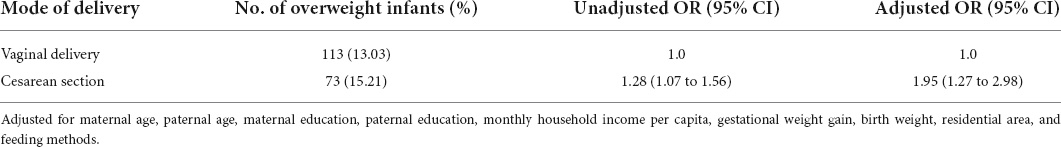
Results of cesarean section and infant overweight
The result of the logistic regression model was shown in Table 2. Among infants delivered by cesarean section, the percentage of overweight was 15.21%, and it was higher than the overweight rate (13.03%) in the vaginal delivery group. Compared to vaginal born, infants born by cesarean section had 1.28 times the likehood of being overweight before adjusting for covariates (95% CI: 1.07–1.56). After adjustment for infant characteristics and parental factors, the cesarean section was significantly related with the likehood of being overweight (OR = 1.95; 95% CI: 1.27 to 2.98) compared to those vaginal born.
Compare of the total and five subscale scores between cesarean section and vaginal delivery groups
Figure 1 presents the comparison of the total and five subscale scores between cesarean and vaginal birth groups. There was a statistical significance in the scores of GDDQ, FMDQ, ADQ, and DQ between vaginal delivery and cesarean section groups (P < 0.05). The children in the cesarean section group had lower scores in GDDQ (98.56 ± 21.54), FMDQ (98.82 ± 20.49), ADQ (99.82 ± 19.58), and DQ (100.90 ± 13.31) than the vaginal delivery group [GDDQ (101.10 ± 19.74), FMDQ (103.30 ± 20.17), ADQ (102.80 ± 18.87), and DQ (102.60 ± 13.17)]. There was no significant difference in language and social behavior development domains (P > 0.05).
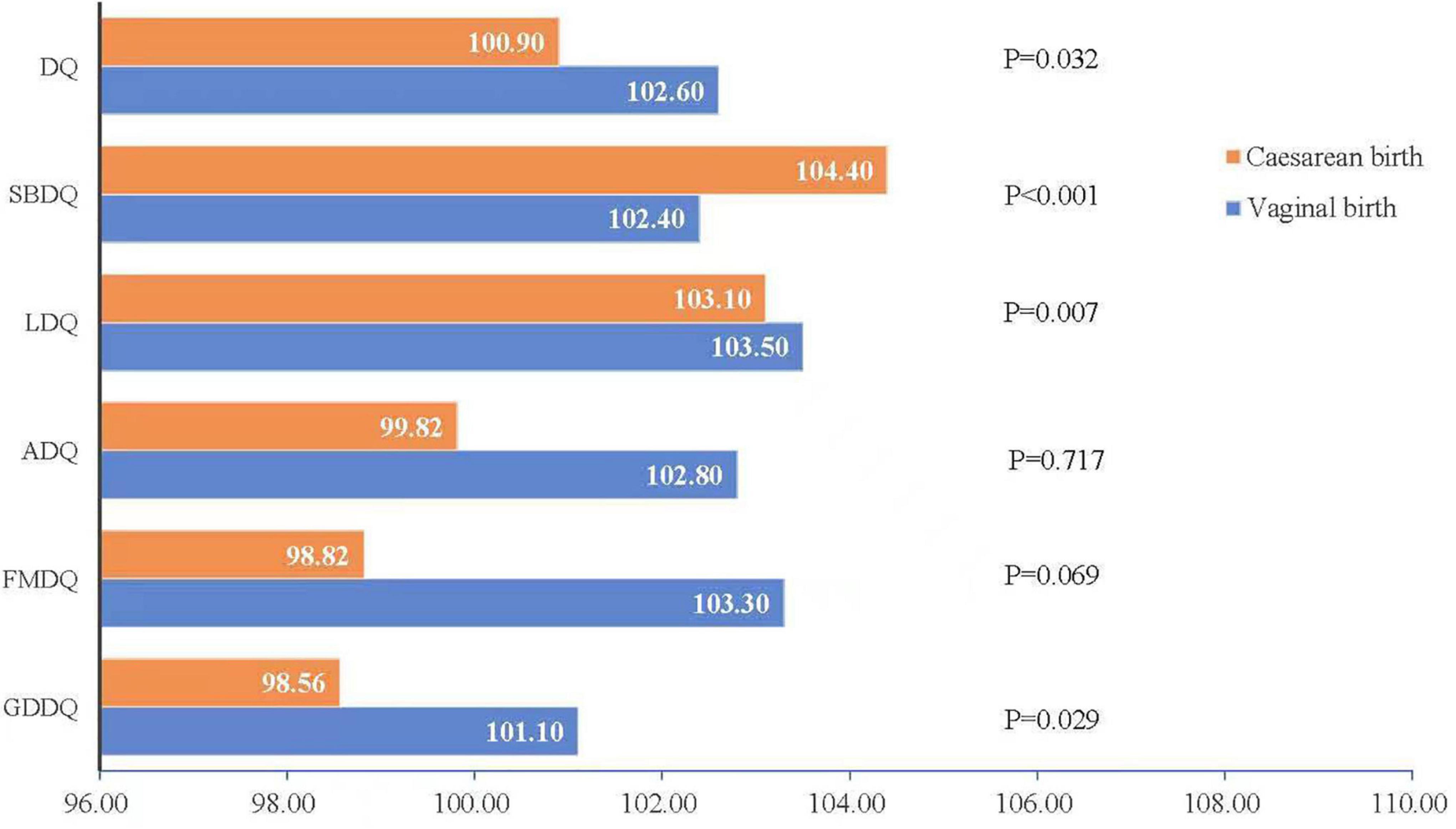
Figure 1. Compare of the total and five subscale scores between cesarean section and vaginal delivery.
Results of cesarean section and infant neurodevelopment
The results of the multivariable linear regression association of delivery mode with infant neurodevelopmental outcomes were shown in Table 3. After adjusting for potential confounders (maternal education, maternal age, paternal education, paternal age, monthly household income per capita, parity, gestational weight gain, birth weight, residential area, and feeding methods), children who were born by cesarean section had a 3.41-point decrease in gross motor development (β = −3.41; 95% CI: −5.77 to −1.05), a 3.65-point decrease in fine motor development (β = −3.65; 95% CI: −6.03 to −1.28), and a 2.96-point in language development (β = −2.96; 95% CI: −5.20 to −0.73), a 1.65-point in total development (β = −1.65; 95% CI: −3.17 to −0.14) compared with those who were vaginal delivery.
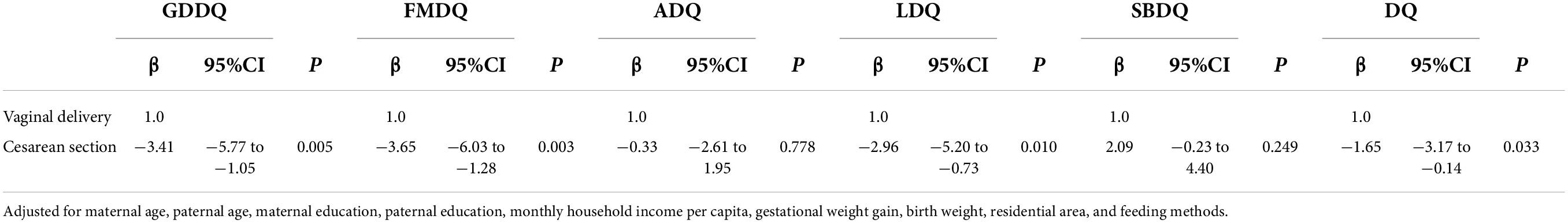
Table 3. Multivariable linear regression association of delivery mode with infant neurodevelopmental outcomes (n = 1,347).
Discussion
Our study shows that cesarean section was associated with overweight and neurodevelopment outcome of children aged 1 to 5 months. The cesarean section might increase the likehood of infant overweight, and might decrease the developmental scores of gross motor, fine motor, and language. In our study, the multivariable logistic regression model showed cesarean section was obviously related with the likehood of being overweight. It was in line with a cohort study in Copenhagen which reported that infants delivered by cesarean section had a higher mean BMI z when the infants aged 6 months compared to that vaginal delivery (24). A systematic review reported that cesarean section had a RR of 1.34 for childhood obesity when compared to vaginal delivery across ages 2–18 years (25). A cohort study of 9,103 children in China reported a 29% increased risk of being obesity in children aged 3–6 years who were delivered by cesarean section (8). In the same way, Pei et al. disclosed a distinctly relationship between cesarean section and obesity in 1,734 German children aged 2 years (26) and a Peruvian prospective cohort study also found obviously associations between cesarean section and the risk of obesity (RR: 2.25; 95% CI: 1.36–3.74) and overweight (RR: 1.51; 95% CI: 0.98–2.35) in children aged 5 years (27). Other studies have different conclusion, they classified cesarean section as emergency cesarean section or elective cesarean section, and found elective cesarean section was associated with a higher risk of infant overweight, but emergency cesarean section was not (14, 28). In this study, the cesarean section didn’t differentiate elective cesarean section and emergency cesarean section, which may have some confounding effect on the results. Two other studies found no significant relationship that the cesarean section type varied the risk of being obesity and overweight in children aged 2–5 years (16, 17).
Previous studies showed that cesarean section was linked to poor child cognitive outcomes (10) and school performance (11). Our study reported that it was statistical significance in the scores of DQ, GDDQ, FMDQ, and ADQ between cesarean section and vaginal delivery groups (P < 0.05). The result was consistent with the result of Zaigham M et al., who disclosed that infants born by cesarean section (n = 66) had distinctly lower assessment scores (the validated Ages and Stages Questionnaire-II) in all developmental domains (communication, gross motor, fine motor, problem solving, and personal-social) at the 4 month assessment, and lower score in the gross-motor skills domain at the 12-month evaluation than infants delivered via vaginal delivery (n = 352) (19). Polidano et al. showed that children born by cesarean section performed a tenth of a standard deviation below in the national test scores for numeracy as compared to vaginally born children in 3,666 Australian children aged 4 to 9 years (10). According to a previous systematic review, the children born by cesarean section had an increased risk of attention-deficit/hyperactivity disorder and autism spectrum disorder when compared to vaginal delivery (29). An epidemiological study conducted in Norway, Sweden, Denmark, Finland, and Australia included 671,464 children delivered by cesarean section, reported the overall adjusted OR was 1.26 in cesarean section children compared with vaginal delivery (30). Other research, however, did not support the link between cesarean section and poor neurodevelopment in children (20, 21). Previous studies reported that maternal obesity is related to an excess risk of cesarean delivery and children overweight (31, 32). Also children born to mothers with gestational diabetes, which is linked with maternal obesity, are at higher risk for lower neurodevelopment and behavioral problems (33, 34). However, we did not consider maternal BMI and gestational diabetes in this study, which may have some confounding effect on the results.
There are several possible mechanisms to explain the relationship of delivery mode and child overweight and neurodevelopment. First, the gut microbiota composition was different by mode of delivery (35–37). The gut microbiota of children born by cesarean section was seeded from the mother’s skin and the hospital environment because they were not exposed to the mother’s birth canal. Hence, the infant’s gut microbiota differs from that of vaginal births (38) and this difference persists into adolescence or early adulthood (39). Second, microbiota play a crucial role in children’s overweight and brain development. Alternations in the microbiome of infants lead to changes in metabolic pathways of the infants (40), and the different postnatal development of the immune system was contributed by the differences in microbiota (41). Collins et al. found that gut microbiota can influence the brain development and behavior through communicating with the brain via the gut–brain axis (42). Third, the alternation of mother-child interactions was associated with the cesarean section (43) and the cesarean section was linked with lower rates of infants’ breastfeeding (44). Studies have reported that delivery by cesarean section may increase the risk of posttraumatic stress compare to vaginal delivery (45, 46). Mothers with cesarean section were more susceptible to have postpartum complications, which might affect mother-infant attachment and the infants’ neurodevelopment. After a cesarean section, the mothers might be more likely to have pain or sickness, which can affect the mothers to initiate and maintain the breastfeeding, or even lead to a reduction in breast milk production (47, 48). Lastly, cesarean section as an “artificial labor” might lead to epigenetic modifications of gene expression, and DNA methylation may be altered in certain cases (12).
On account of the cesarean section has some consequences for a child’s health and development, as well as subsequent pregnancies, the WHO recommends that cesarean section should be conducted based on the medical indications. In China, one cross-section survey reported that the national average cesarean section rate is 34.9% (49). In our study, the cesarean section rate was 35.6%, what is not clear of this study is whether all the cesarean sections were performed on medical necessary. The appropriate cesarean section rate in China needs to be discovered in the future studies.
Strengths and limitations
There are several strengths in the present study. First, we used a multistage, stratified, randomized sampling method in this study, so study participants were a good representation of the general population of Chinese children. Second, participants were healthy, full-term infants without pregnancy complications or serious illness; therefore, this study excluded the potential confounding effect of various diseases. Third, the Child Psychological Development Scale (WS/T 580-2017) was used to examine developmental outcomes in our study. The developmental milestones of the children were fully or partially covered in this scale. This is a local scale in China, and the items are very suitable for Chinese children. There are also some limitations in this study. First, this study was cross-sectional designed; thus, the obvious associations found in this study were correlational relationships. The effects of cesarean section on child health outcomes should be conducted in a future study using a longitudinal study design. Second, in our study, the cesarean section didn’t differentiate elective cesarean section and emergency cesarean section, and maternal BMI and gestational diabetes were not accounted for in the present study owing to the limitations of data collection, which may have had some confounding effect on the results. Third, we didn’t include all the risk factors, such as genetic and familial risk factors which may also explain the relationship and these factors will be taken into account in the future studies.
Conclusion
In our study population, cesarean section was associated with overweight and neurodevelopment outcomes. The cesarean section might increase the likehood of infants’ overweight and might decrease the developmental scores of gross motor, fine motor, and language. Further studies should be conducted to verify the associations and explore the possible mechanisms.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committee on Human Research at the National Institute for Nutrition and Health, Chinese Center for Disease Control and Prevention (No. 2019-009). Written informed consent to participate in this study was provided by the participants or their legal guardian/next of kin.
Author contributions
XZ contributed to the performance of the study, analyzed the data, and drafted the manuscript. RL, LW, HY, LL, and JC were responsible for the data collection and reviewed drafts of the manuscript. WZ contributed to the project administration. ZY, QZ, TX, and YW contributed to the methodology, investigation, and supervision. BC contributed to the writing – review and editing. All authors participated in the conceptualization process of review and revision, read, and agreed to the final manuscript.
Funding
This study was funded by the National Special Program for Science and Technology Basic Resources Investigation of China (Grant numbers: 2017FY101106 and 2017FY101100) and Capital Institute of Pediatrics Nurturing Program fund (Grant number: PY-2020-03).
Acknowledgments
We are grateful to the researchers and all the field staff for their hard work in this study. We also appreciated to the guardians of the children who supported this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Boerma T, Ronsmans C, Melesse DY, Barros AJD, Barros FC, Juan L, et al. Global epidemiology of use of and disparities in caesarean sections. Lancet. (2018) 392:1341–8. doi: 10.1016/S0140-6736(18)31928-7
2. Curran EA, Khashan AS, Dalman C, Kenny LC, Cryan JF, Dinan TG, et al. Obstetric mode of delivery and attention-deficit/hyperactivity disorder: A sibling-matched study. Int J Epidemiol. (2016) 45:532–42. doi: 10.1093/ije/dyw001
3. Curran EA, Cryan JF, Kenny LC, Dinan TG, Kearney PM, Khashan AS. Obstetrical mode of delivery and childhood behavior and psychological development in a british cohort. J Autism Dev Disord. (2016) 46:603–14. doi: 10.1007/s10803-015-2616-1
4. Tang S, Li X, Wu Z. Rising cesarean delivery rate in primiparous women in Urban China: Evidence from three nationwide household health surveys. Am J Obstet Gynecol. (2006) 195:1527–32. doi: 10.1016/j.ajog.2006.03.044
5. Liao Z, Zhou Y, Li H, Wang C, Chen D, Liu J. The rates and medical necessity of cesarean delivery in the era of the two-child policy in hubei and gansu provinces, China. Am J Public Health. (2019) 109:476–82. doi: 10.2105/AJPH.2018.304868
6. Bager P, Wohlfahrt J, Westergaard T. Caesarean delivery and risk of atopy and allergic disease: Meta-analyses. Clin Exp Allergy. (2008) 38:634–42. doi: 10.1111/j.1365-2222.2008.02939.x
7. Cardwell CR, Stene LC, Joner G, Cinek O, Svensson J, Goldacre MJ, et al. Caesarean section is associated with an increased risk of childhood-onset type 1 diabetes mellitus: A meta-analysis of observational studies. Diabetologia. (2008) 51:726–35. doi: 10.1007/s00125-008-0941-z
8. Rutayisire E, Wu X, Huang K, Tao S, Chen Y, Tao F. Cesarean section may increase the risk of both overweight and obesity in preschool children. BMC Pregnancy Childbirth. (2016) 16:338. doi: 10.1186/s12884-016-1131-5
9. Ardic CA, Usta OA, Omar EA, Yıldız CA, Memis EA. Caesarean delivery increases the risk of overweight or obesity in 2-year-old children. J Obstet Gynaecol. (2021) 41:374–9. doi: 10.1080/01443615.2020.1803236
10. Polidano C, Zhu A, Bornstein JC. The relation between cesarean birth and child cognitive development. Sci Rep. (2017) 7:11483. doi: 10.1038/s41598-017-10831-y
11. Curran EA, Kenny LC, Dalman C, Kearney PM, Cryan JF, Dinan TG, et al. Birth by caesarean section and school performance in swedish adolescents– a population-based study. BMC Pregnancy Childbirth. (2017) 17:121. doi: 10.1186/s12884-017-1304-x
12. Cho CE, Norman M. Cesarean section and development of the immune system in the offspring. Am J Obstet Gynecol. (2013) 208:249–54. doi: 10.1016/j.ajog.2012.08.009
13. Woo Baidal JA, Locks LM, Cheng ER, Blake-Lamb TL, Perkins ME, Taveras EM. Risk factors for childhood obesity in the first 1,000 days: A systematic review. Am J Prev Med. (2016) 50:761–79. doi: 10.1016/j.amepre.2015.11.012
14. Babu GR, Mueller NT, Lewis MG, Krishnan A, Lobo E, Deepa R, et al. Delivery mode and altered infant growth at 1 year of life in India. Pediatr Res. (2021) 90:1251–7. doi: 10.1038/s41390-021-01417-6
15. Mueller NT, Zhang M, Hoyo C, Ostbye T, Benjamin-Neelon SE. Does cesarean delivery impact infant weight gain and adiposity over the first year of life? Int J Obes. (2019) 43:1549–55. doi: 10.1038/s41366-018-0239-2
16. Masukume GA-O, O’Neill SM, Baker PN, Kenny LC, Morton SMB, Khashan AS. The impact of caesarean section on the risk of childhood overweight and obesity: New evidence from a contemporary cohort study. Sci Rep. (2018) 8:15113. doi: 10.1038/s41598-018-33482-z
17. Masukume G, McCarthy FP, Baker PN, Kenny LC, Morton SM, Murray DM, et al. Association between caesarean section delivery and obesity in childhood: A longitudinal cohort study in Ireland. BMJ Open. (2019) 9:e025051. doi: 10.1136/bmjopen-2018-025051
18. Curran EA, O’Neill SM, Cryan JF, Kenny LC, Dinan TG, Khashan AS, et al. Research review: Birth by caesarean section and development of autism spectrum disorder and attention-deficit/hyperactivity disorder: A systematic review and meta-analysis. J Child Psychol Psychiatry. (2015) 56:500–8. doi: 10.1111/jcpp.12351
19. Zaigham M, Hellstrom-Westas L, Domellof M, Andersson O. Prelabour caesarean section and neurodevelopmental outcome at 4 and 12 months of age: An observational study. BMC Pregnancy Childbirth. (2020) 20:564. doi: 10.1186/s12884-020-03253-8
20. Robson SJ, Vally H, Abdel-Latif ME, Yu M, Westrupp E. Childhood health and developmental outcomes after cesarean birth in an australian cohort. Pediatrics. (2015) 136:e1285–93. doi: 10.1542/peds.2015-1400
21. Zavez A, Thurston SW, Rand MD, Mruzek DW, Love T, Smith T, et al. Delivery mode and child development at 20 months of age and 7 years of age in the republic of seychelles. Matern Child Health J. (2021) 25:1930–8. doi: 10.1007/s10995-021-03239-8
22. Yang ZY, Zhang Q, Zhai Y, Xu T, Wang YY, Chen BW, et al. National nutrition and health systematic survey for children 0-17 years of age in China. Biomed Environ Sci. (2021) 34:891–9.
23. Wang S, Mei Y, Ma ZH, Zhao WH, Tang XJ, Pang XH, et al. The patterns of complementary feeding and growth among 12 to 23 month-old children in China. Biomed Environ Sci. (2021) 34:847–58.
24. Vinding RK, Sejersen TS, Chawes BL, Bønnelykke K, Buhl T, Bisgaard H, et al. Cesarean delivery and body mass index at 6 months and into childhood. Pediatrics. (2017) 139:e20164066. doi: 10.1542/peds.2016-4066
25. Kuhle S, Tong OS, Woolcott CG. Association between caesarean section and childhood obesity: A systematic review and meta-analysis. Obes Rev. (2015) 16:295–303. doi: 10.1111/obr.12267
26. Pei Z, Heinrich J, Fuertes E, Flexeder C, Hoffmann B, Lehmann I, et al. Cesarean delivery and risk of childhood obesity. J Pediatr. (2014) 164:1068.e–73.e. doi: 10.1016/j.jpeds.2013.12.044
27. Carrillo-Larco RM, Miranda JJ, Bernabé-Ortiz A. Delivery by caesarean section and risk of childhood obesity: Analysis of a peruvian prospective cohort. PeerJ. (2015) 3:e1046. doi: 10.7717/peerj.1046
28. Cai M, Loy SL, Tan KH, Godfrey KM, Gluckman PD, Chong YS, et al. Association of elective and emergency cesarean delivery with early childhood overweight at 12 months of age. JAMA Netw Open. (2018) 1:e185025. doi: 10.1001/jamanetworkopen.2018.5025
29. Zhang T, Sidorchuk A, Sevilla-Cermeno L, Vilaplana-Perez A, Chang Z, Larsson H, et al. Association of cesarean delivery with risk of neurodevelopmental and psychiatric disorders in the offspring: A systematic review and meta-analysis. JAMA Netw Open. (2019) 2:e1910236. doi: 10.1001/jamanetworkopen.2019.10236
30. Yip BHK, Leonard H, Stock S, Stoltenberg C, Francis RW, Gissler M, et al. Caesarean section and risk of autism across gestational age: A multi-national cohort study of 5 million births. Int J Epidemiol. (2017) 46:429–39. doi: 10.1093/ije/dyw336
31. Minsart AF, N’Guyen TS, Dimtsu H, Ratsimanresy R, Dada F, Ali Hadji R. Maternal obesity and rate of cesarean delivery in Djibouti. Int J Gynaecol Obstet. (2014) 127:167–70. doi: 10.1016/j.ijgo.2014.05.011
32. Marchi J, Berg M, Dencker A, Olander EK, Begley C. Risks associated with obesity in pregnancy, for the mother and baby: A systematic review of reviews. Obes Rev. (2015) 16:621–38. doi: 10.1111/obr.12288
33. Sanchez CE, Barry C, Sabhlok A, Russell K, Majors A, Kollins SH, et al. Maternal pre-pregnancy obesity and child neurodevelopmental outcomes: A meta-analysis. Obes Rev. (2018) 19:464–84. doi: 10.1111/obr.12643
34. Pugh SJ, Richardson GA, Hutcheon JA, Himes KP, Brooks MM, Day NL, et al. Maternal obesity and excessive gestational weight gain are associated with components of child cognition. J Nutr. (2015) 145:2562–9. doi: 10.3945/jn.115.215525
35. Salminen S, Gibson GR, McCartney AL, Isolauri E. Influence of mode of delivery on gut microbiota composition in seven year old children. Gut. (2004) 53:1388–9. doi: 10.1136/gut.2004.041640
36. Bäckhed F, Roswall J, Peng Y, Feng Q, Jia H, Kovatcheva-Datchary P, et al. Dynamics and stabilization of the human gut microbiome during the first year of life. Cell Host Microbe. (2015) 17:690–703. doi: 10.1016/j.chom.2015.04.004
37. Dominguez-Bello MG, Costello EK, Contreras M, Magris M, Hidalgo G, Fierer N, et al. Delivery mode shapes the acquisition and structure of the initial microbiota across multiple body habitats in Newborns. Proc. Natl. Acad. Sci. (2010) 107:11971–5. doi: 10.1073/pnas.1002601107
38. Makino H, Kushiro A, Ishikawa E, Kubota H, Gawad A, Sakai T, et al. Mother-to-infant transmission of intestinal bifidobacterial strains has an impact on the early development of vaginally delivered infant’s microbiota. PLoS One. (2013) 8:e78331. doi: 10.1371/journal.pone.0078331
39. Mueller NT, Bakacs E, Combellick J, Grigoryan Z, Dominguez-Bello MG. The infant microbiome development: Mom matters. Trends Mol Med. (2015) 21:109–17. doi: 10.1016/j.molmed.2014.12.002
40. Ajslev TA, Andersen CS, Gamborg M, Sørensen TI, Jess T. Childhood overweight after establishment of the gut microbiota: The role of delivery mode, pre-pregnancy weight and early administration of antibiotics. Int J Obes. (2011) 35:522–9. doi: 10.1038/ijo.2011.27
41. Prince AL, Chu DM, Seferovic MD, Antony KM, Ma J, Aagaard KM. The perinatal microbiome and pregnancy: Moving beyond the vaginal microbiome. Cold Spring Harb Perspect Med. (2015) 5:a023051. doi: 10.1101/cshperspect.a023051
42. Collins S, Surette M, Bercik P. The interplay between the intestinal microbiota and the brain. Nat Rev Microbiol. (2012) 10:735–42. doi: 10.1038/nrmicro2876
43. Kelly Y, Sacker A, Del Bono E, Francesconi M, Marmot M. What role for the home learning environment and parenting in reducing the socioeconomic gradient in child development? Findings from the millennium cohort study. Arch Dis Child. (2011) 96:832–7. doi: 10.1136/adc.2010.195917
44. Kramer MS, Aboud F, Mironova E, Vanilovich I, Platt RW, Matush L, et al. Breastfeeding and child cognitive development: New evidence from a large randomized trial. Arch Gen Psychiatry. (2008) 65:578–84. doi: 10.1001/archpsyc.65.5.578
45. Ryding EL, Wijma K, Wijma B. Psychological Impact of emergency cesarean section in comparison with elective cesarean section, instrumental and normal vaginal delivery. J Psychosom Obstet Gynaecol. (1998) 19:135–44. doi: 10.3109/01674829809025691
46. Jolly J, Walker J, Bhabra K. Subsequent obstetric performance related to primary mode of delivery. Br J Obstet Gynaecol. (1999) 106:227–32. doi: 10.1111/j.1471-0528.1999.tb08235.x
47. Ramoo S, Trinh TA, Hirst JE, Jeffery HE. Breastfeeding practices in a hospital-based study of vietnamese women. Breastfeed Med. (2014) 9:479–85. doi: 10.1089/bfm.2014.0021
48. Cakmak H, Kuguoglu S. Comparison of the Breastfeeding patterns of mothers who delivered their babies per vagina and via cesarean section: An observational study using the latch breastfeeding charting system. Int J Nurs Stud. (2007) 44:1128–37. doi: 10.1016/j.ijnurstu.2006.04.018
Keywords: cesarean section, mode of delivery, neurodevelopment, development, China
Citation: Zheng X, Li R, Wang L, Yang H, Li L, Cui J, Zhao W, Yang Z, Zhang Q, Xu T, Wang Y and Chen B (2022) The association of cesarean section with overweight and neurodevelopment of Chinese children aged 1–5 months. Front. Pediatr. 10:940422. doi: 10.3389/fped.2022.940422
Received: 10 May 2022; Accepted: 09 August 2022;
Published: 23 August 2022.
Edited by:
Mu Li, The University of Sydney, AustraliaCopyright © 2022 Zheng, Li, Wang, Yang, Li, Cui, Zhao, Yang, Zhang, Xu, Wang and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bowen Chen, Ym93ZW5jQDEyNi5jb20=
 Xiaoguo Zheng
Xiaoguo Zheng Ruili Li
Ruili Li Lihong Wang1
Lihong Wang1 Tao Xu
Tao Xu