- 1Department of Urology, The Affiliated Nanchong Central Hospital of North Sichuan Medical College (University), Nanchong, China
- 2Department of Urology, The Second Hospital of Lanzhou University Medical School, Lanzhou, China
- 3Department of Urology, Institute of Urology, West China Hospital, Sichuan University, Chengdu, China
- 4Department of Medical Genetics and Cell Biology, North Sichuan Medical College (University), Nanchong, China
Objective: To evaluate and compare the efficacy and safety between an external stent and a Double J stent for pediatric Pyeloplasty.
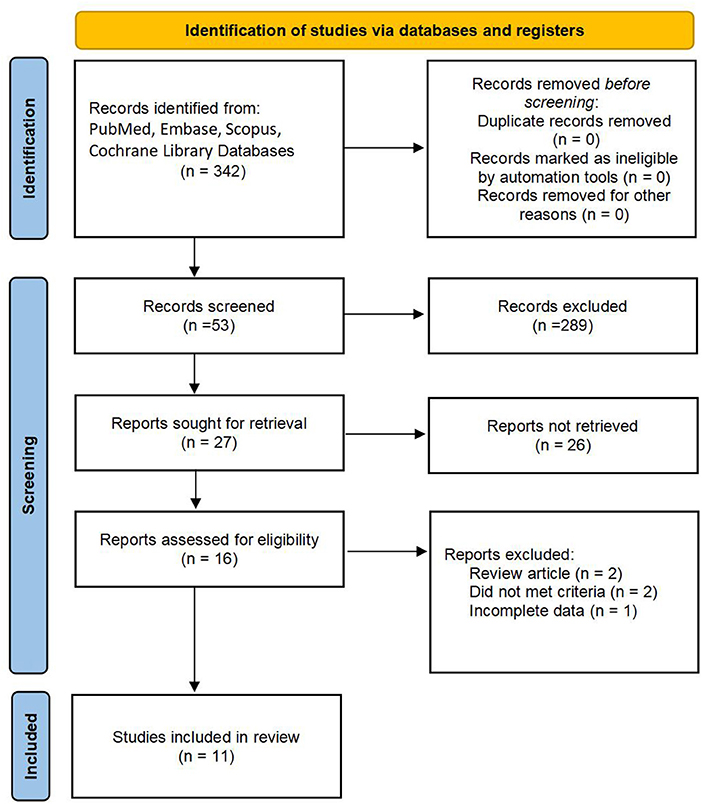
Methods: Through a systematical search of multiple scientific databases in July 2022, we performed a systematic review and meta-analysis of the primary outcomes of interest according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses), whose protocol was registered with PROSPERO(CRD42021274087).
Results: Eleven studies involving 1,758 patients were included. No significant differences were observed in operative time (MD: 2.26; 95% CI −9.62 to 14.14; P = 0.79), operative success rate (OR: 1.10; 95% CI 0.57 to 2.10; P = 0.780), length of hospital stay (MD: 0.65; 95% CI −0.04 to 1.34; P = 0.063), or complications (OR: 0.87; 95%CI 0.48 to 1.56; P = 0.630) between external stents and DJ stents in pediatric pyeloplasty. According to the subgroup analysis, we found the external stent group had a shorter operative time than the DJ stent group in terms of robot-assisted laparoscopic pyeloplasty (MD: −17.13; 95% CI −32.8 to −1.45; P = 0.032).
Conclusions: There were no significant differences in operative time, operative success rate, length of hospital stay, or complications between external stents and DJ stents in pediatric pyeloplasty. The external stented procedure seemed to have less operative time when using robot-assisted laparoscopic pyeloplasty. However, due to the limitations of our analysis, more studies are still required to support our conclusion.
Systematic review registration: This systematic review has been registered on PROSPERO, the registration ID is CRD42021274087.
Introduction
The most common congenital abnormality of the upper urinary tract is Uretero-Pelvic Junction Obstruction (UPJO) and the incidence in newborns is 1 in 1,500. Approximately 20–50% of children with hydronephrosis will eventually undergo surgical intervention (1). Since it was first described, Anderson-Hynes dismembered pyeloplasty has been considered the standard surgical treatment for UPJO (2). Not only for open pyeloplasty but also minimally pyeloplasty, encouraging outcomes have been demonstrated (3–5). The management of anastomosis drainage after pyeloplasty includes no stent, internal Double J(DJ) stent, and external stent. Although researchers have described outstanding outcomes of unstented pyeloplasty (6, 7), a large number of surgeons still prefer to stent the newly formed anastomosis.
Several methods of postoperative renal drainage have been described, and internal DJ stents or external stents are used most often. DJ stents are usually placed in an antegrade manner, and the size is chosen by surgeon preference. The most commonly used size is 4.7 French in pediatric pyeloplasty. Kidney-ureter-bladder X-ray was performed the next day to confirm the position (8). DJ stents are not easy to insert, and their use may be accompanied by the risk of stent migration, urinary tract infection, and second anesthesia for removal (9). The external stent is passed from the ureteropelvic junction to the skin through the kidney parenchyma, and the lower end of the stent reaches the mid or lower ureter. It is fixed with sutures on the renal capsule or skin to reduce the risk of displacement (10). An external stent has the advantage that it can be removed in the outpatient department without anesthesia. However, the risk of bleeding and stent leakage cannot be ignored when using an external stent (4, 11).
Currently, the type of stents to place in clinical practice mainly depends on the surgeon's preference and experience. To fill this gap, we performed a meta-analysis to assess and compare the efficacy and safety between external stents and DJ stents.
Methods
Literature search and eligibility criteria
Based on the guidelines of Preferred Reporting Items for Systematic Reviews (12), a systematic search was performed to identify studies in PubMed, Embase, Scopus database, and Cochrane Library. The latest search data was July, 2022.Search terms included “pediatric,” “double J,” “tube,” “DJ,” “stent*,” “external*,” “UPJO,” “Anderson-Hynes,” “pyeloplasty,” etc. We also broadened the search scope by manual retrieval, and the search was not restricted by language.
The studies were included in our meta-analysis if they met the following criteria: (1) patients were diagnosed with UPJO and pyeloplasty was performed, (2) the comparison between external stents and DJ stents, (3) the full paper was full of no < 1 outcome parameter. The exclusion criteria were as follows: (1) patients with another disease except for UPJO, (2) previous history of pyeloplasty, (3) reviews, case reports, letters, and irrelevant studies about our topic, (4) available data could not be extracted.
Data extraction
The extraction process was independently completed by two authors (CY.M and L.P), and the following information was recorded: author, publication year, country, study design, sample size, inventions, mean age, follow-up time, operative time, operative success rate, length of hospital stay, and complications. When continuous variables were described as other forms in the main literature, we calculated the mean and standard deviation (13).
Study quality assessment
Randomized controlled trials were assessed by the Jadad scale (14) and non-randomized controlled trials were evaluated by the NOS scoring rules (15). The Jadad score varied up to seven points, and more than four points were graded as high quality. The NOS scale ranged from zero to nine stars, and scores of more than six stars were considered high quality.
Risk of bias assessments
The ROBINS-I tool was used to evaluate the risk of bias for non-randomized studies. The ROBINS-I tool included seven domains: confounding bias, selection bias, bias in the measurement classification of interventions, bias due to deviations from intended interventions, bias due to missing data, bias in the measurement of outcomes, and bias in the selection of the reported result (16). Moreover, we used the ROB2 tool to evaluate the risk of bias for randomized controlled trials. ROB2 covered the randomization process, deviations from intended interventions, missing outcome data, measurement of the outcome, and selection of the reported result (17).
Data analysis
We accomplished data analysis by using STATA version 16.0. the mean difference (MD) and odds ratio (OR) were considered continuous and dichotomous outcomes, respectively. In addition, we calculated a 95% confidence interval (CI) and used I-square tests to verify the heterogeneity among the included studies. Statistical significance was defined as P < 0.05. Subgroup analysis was performed according to different surgical methods, such as open pyeloplasty, laparoscopic pyeloplasty, and robot-assisted laparoscopic pyeloplasty.
Results
Description of studies
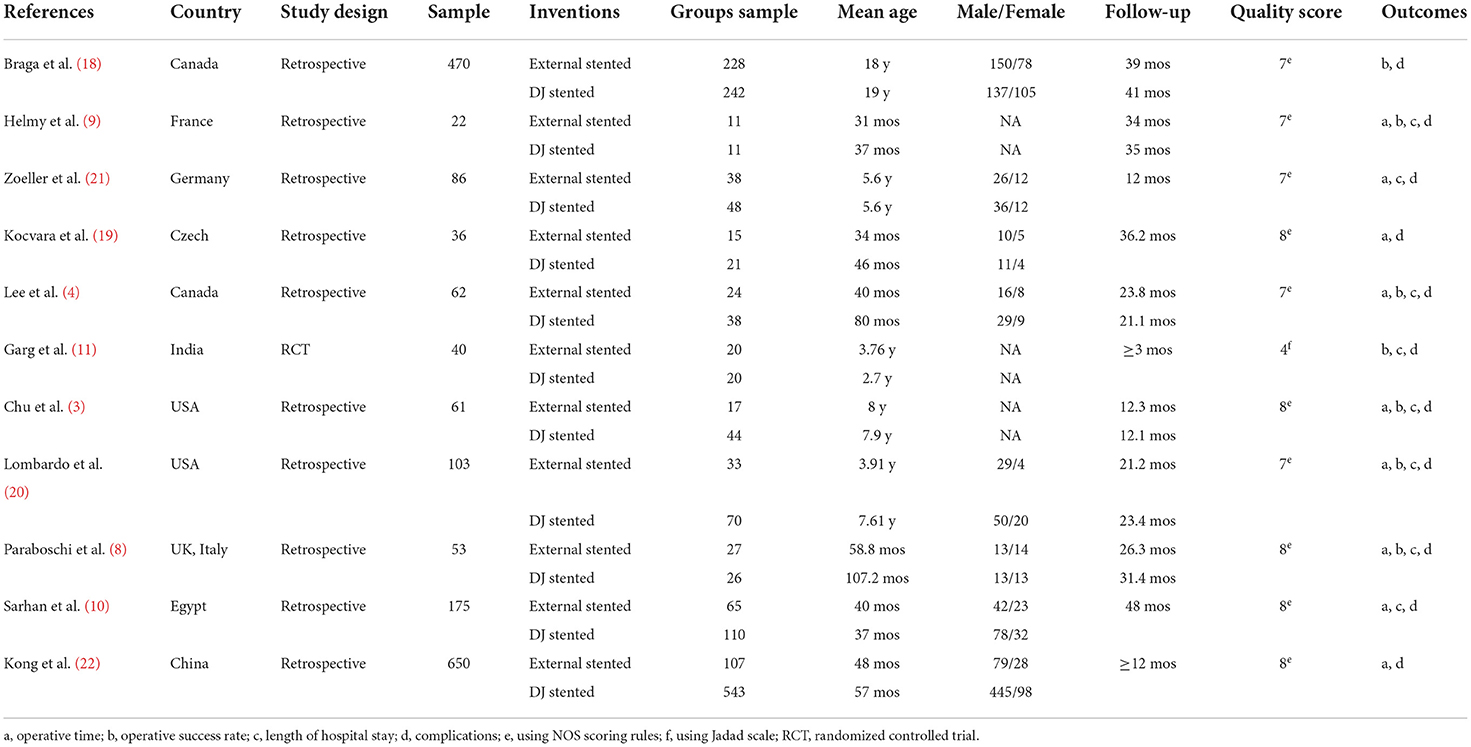
A total of 342 studies were identified, and eleven studies were eventually included in our meta-analysis (3, 4, 8–11, 18–22). The filtering process is shown in Figure 1. The baseline characteristics of the included studies are given in Table 1 eleven studies, including 1,758 patients, were published between 2008 and 2021. Moreover, the sample size ranged from 22 to 650. Among them, ten types of research were retrospective designs, and one was a randomized controlled trial.
Quality assessment
The quality of the randomized controlled trials was relatively high (Jadad scale: 4 points). For non-randomized controlled trials, five studies scored seven stars and four scored eight stars. The ultimate quality assessment list is shown in Table 1.
Risk of bias
The major weakness of randomized controlled trials was in the domains of randomization process and deviations from intended interventions, as shown in Supplementary Figure 1. For non-randomized controlled trials, the final results showed that eight studies were at moderate risk of bias and one was low. The outcome was provided in the Supplementary Table 1.
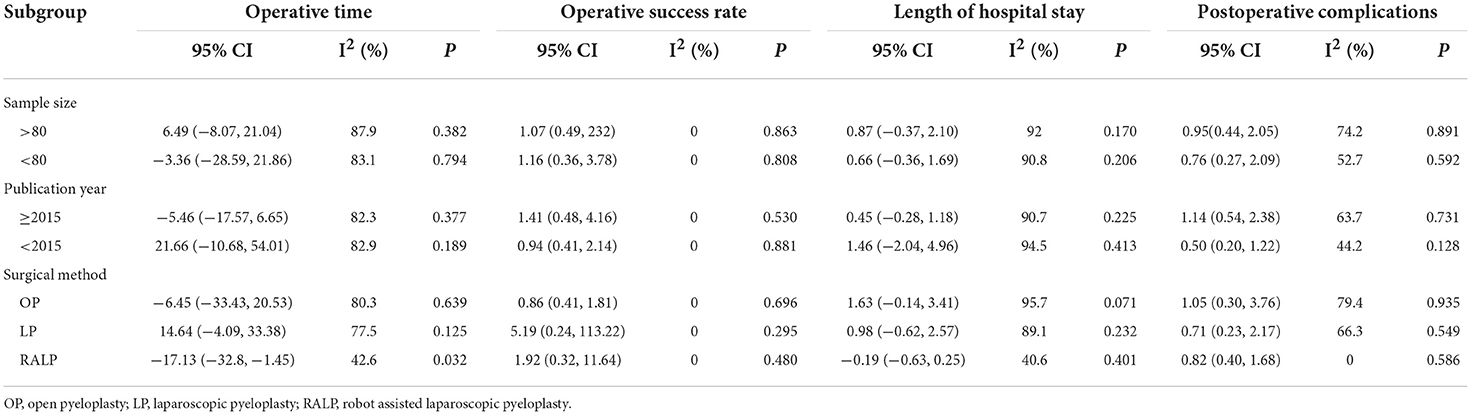
Operative time
Nine studies with 1,287 patients were related to operative time (3, 4, 8–10, 19–22). Due to the high heterogeneity (I2>50%), we used the random-effects model. The pooled meta-analysis results showed that no significant difference was found between the external stent group and the DJ group (MD: 2.26; 95% CI −9.62 to 14.14; P = 0.79; Figure 2A).
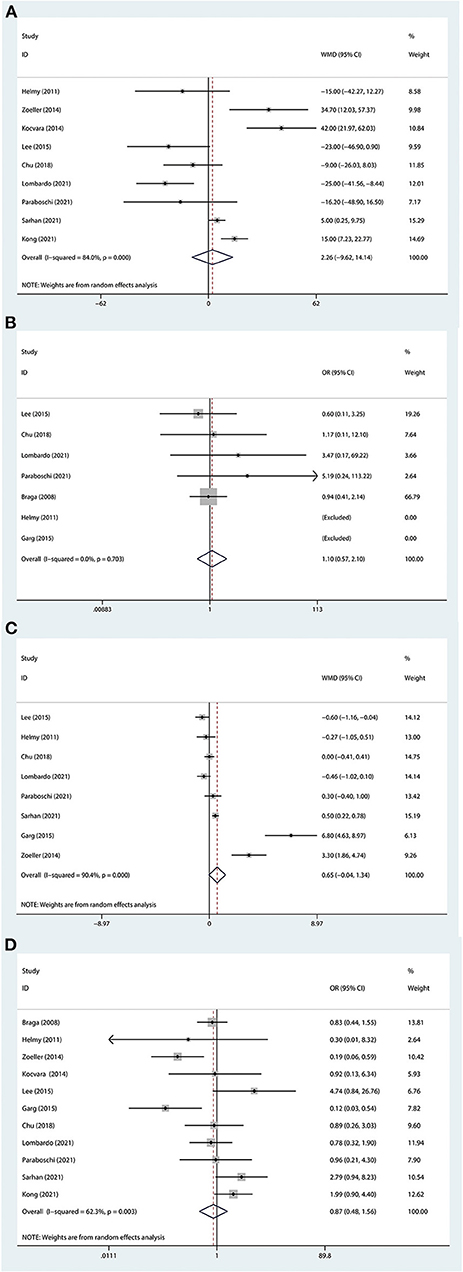
Figure 2. Forest plot of perioperative outcomes. (A) Operative time. (B) Operative success rate. (C) Length of hospital stay. (D) Complication. The horizontal lines represent 95% CI. The intersection of diamond and vertical line means that the difference is not statistically significant.
Operative success rate
The results of the surgery were stated in 7 studies (3, 4, 8, 9, 11, 18, 20), and all included groups reached a high success rate. Based on heterogeneous results (I2 = 0%), the fixed effects model was used. The final results indicated that no significant difference was found between the two groups (OR: 1.10; 95% CI 0.57 to 2.10; P = 0.780; Figure 2B).
Length of hospital stay
The length of hospital stay was observed in 8 studies (3, 4, 8–11, 20, 21), including 602 patients. Given the heterogeneity test outcome (I2>50%), we used the random-effects model. The ultimate result showed that there was no difference between the external stent group and the DJ group (MD: 0.65; 95% CI −0.04 to 1.34; P = 0.063; Figure 2C).
Complications
Eleven studies had been linked to complications (3, 4, 8–11, 18–22), concerning 1,758 patients. Because of the heterogeneous results (I2 = 62.3%), a random effect model was applied. The overall meta-analysis showed that there was no difference between the two groups in terms of complications (OR: 0.87; 95%CI 0.48 to 1.56; P = 0.630; Figure 2D). Moreover, some major complications, which included stent dislodgement, stent leakage, and urinary tract infection, were analyzed and there was no significant difference (Figure 3).
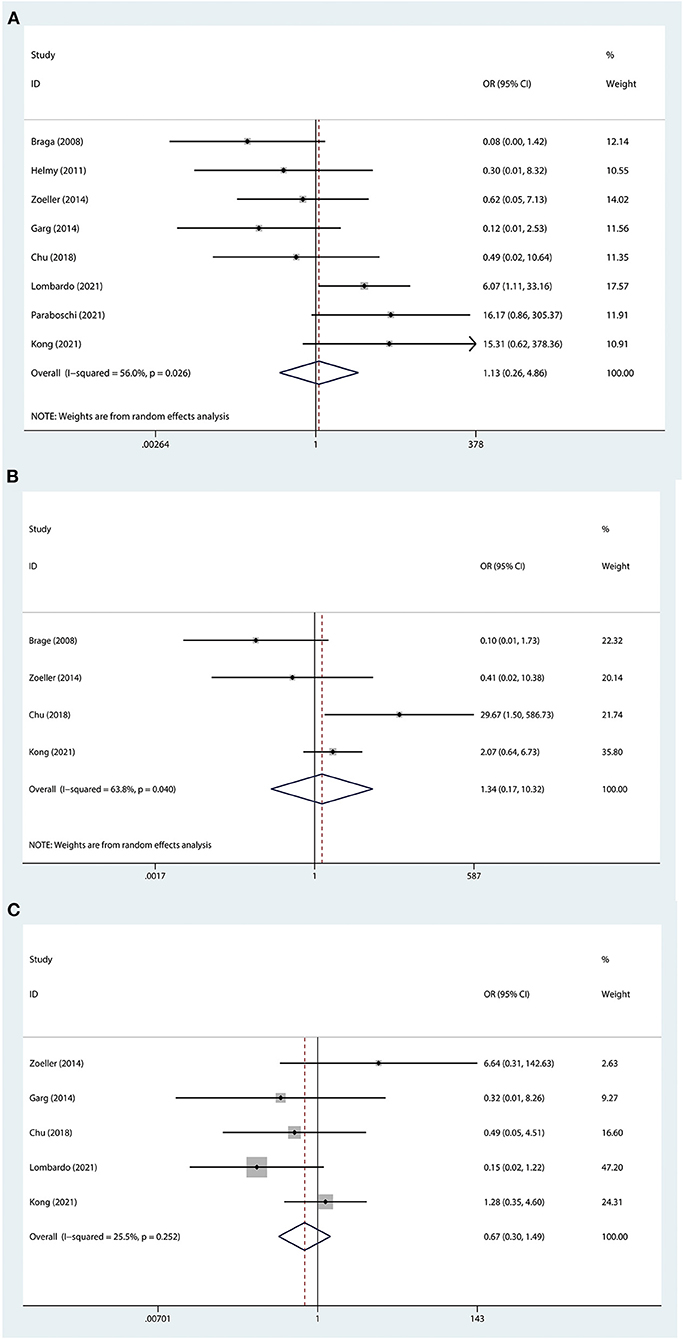
Figure 3. Forest plot of major complication. (A) stent dislodgement. (B) stent leakage. (C) urinary tract infection. The horizontal lines represent 95% CI. The intersection of diamond and vertical line means that the difference is not statistically significant.
Subgroup analysis
Subgroup analysis was performed according to sample size, publication year, and surgical methods, Owing to the lack of sufficient data, the subgroup analysis could not be performed on major complications. The last outcome of the subgroup analysis recommended that the external stent group had a shorter operative time than the DJ stent group in terms of robot-assisted laparoscopic pyeloplasty (MD: −17.13; 95% CI −32.8 to −1.45; P = 0.032; Table 2).
Sensitivity analysis
Seeing the outcomes of heterogeneity, we performed a sensitivity analysis to improve the reliability of the results. Studies were removed one by one to recalculate the combined mean difference, and the outcomes of our meta-analysis were stable except for the length of hospital stay (Figure 4).
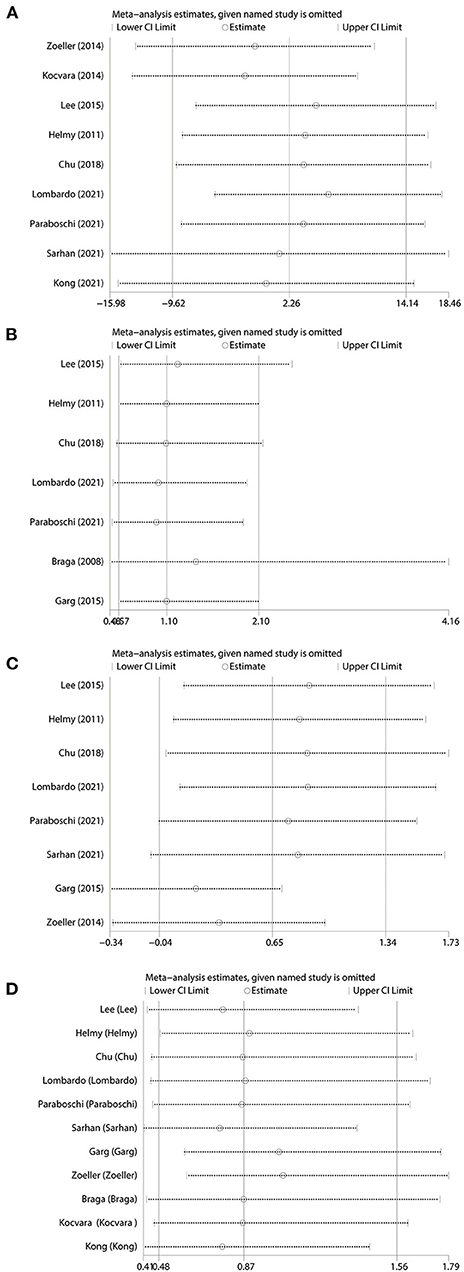
Figure 4. Sensitivity analysis. (A) Operative time. (B) Operative success rate. (C) Length of hospital stay. (D) Complication. Studies are removed one by one to recalculate the combined effect size, and compare the difference with the initial effect size.
Discussion
Even if the safety and efficacy of unstented pyeloplasty were reported, the majority of surgeons prefer to place a trans anastomotic stent to drain urine. This could help to release the stress on the newly formed anastomosis (23). The DJ stent and external stent were the main management of anastomosis drainage after pyeloplasty, and each measure had its advantages and disadvantages (24, 25). The major shortcoming of the DJ stent was that patients, especially infants, needed to undergo second general anesthesia when withdrawing it. Nevertheless, doctors can remove external stents through the renal parenchyma or the renal pelvis even without general anesthesia.
Eleven comparative studies, including 1,758 patients, were eventually included in our meta-analysis. Based on the outcomes, we observed that in the terms of operative time, operative success rate, length of hospital stay, and postoperative complications, no significant differences were found. According to the outcome of the subgroup analysis, the external stent group had a shorter operative time than the DJ stent group in terms of robot-assisted pyeloplasty.
In terms of operative time, our conclusion was consistent with most of the previous outcomes, which meant there was no significant difference between the two groups. As a result of the three operative approaches, subgroup analysis was performed by dividing the patients into three groups. The results of the subgroup analysis suggested that only in robot-assisted laparoscopic pyeloplasty did patients in the external stent group have a shorter operative time than those in the DJ stent group. This might mean that, to some extent, the external stent was not second to the DJ stent, especially in robot-assisted laparoscopic pyeloplasty.
Operative success was defined as the improvement of clinical symptoms and radiological evidence of improvement of hydronephrosis. The operative success rate in both two groups was very high, with a range of 87.5–100% in the external stent group and the range of 92.1–100% in the DJ group. No differences were considered significant in our meta-analysis. A recent study of 85 children aged 0–16 years, compared the changes in differential renal function after pyeloplasty in children and showed that most children had preserved or improved renal function after surgery (26). Combining the above evidence, showed similar effectiveness between the two drainage techniques despite the use of different surgical techniques.
For the length of hospital stay, the final result demonstrated that there was no difference between the external stent group and the DJ group. Nevertheless, in some studies, patients in the external stent group stayed longer in the hospital (10, 11, 21). As far as we know, the use of a DJ stent was associated with a lower risk of urinary leakage, thereby enabling patients to recover rapidly. In addition, if successful clamping or poor drainage is lacking, hospitalization for patients with external stents might be longer (11). In Professor Zoeller's study, he pointed out that doctors' decisions on discharge time were affected by parents' fear or inability to manage external drainage (21). This also might prolong hospitalization.
Concerning the result of overall complications, we did not find significant differences between the external stent group and the DJ stent group, which was consistent with most previous studies (3, 4, 18). Some studies have suggested that several postoperative problems can be avoided by choosing a suitable stent length and some tools were offered for choice (27, 28). To avoid the excess length of the stent in the bladder, Professor Garg proposed the formula: Length of DJ stent (cm) = length of the retained ureter (cm)−2. Even so, 9 of 20 patients in the DJ group experienced an increase in the frequency of urination. In contrast, only one person had frequent urination in the control group (11). In Professor Zoeller's study, the main technical problem was the inability to place a DJ stent in infants (21).
Stent dislodgement, stent leakage, and urinary tract infection were the major complications. In a study involving 55 patients, there were 5(9.1%) cases of DJ stent dislodgement, including 3 DJ stents migrating into the bladder and 2 into the upper urinary tract (29). In the study reported by Chu et al., the incidence of DJ stent displacement (4.5%) was higher than that of the external stent (0%) (3). Furthermore, DJ stents in the ureter could cause artificial vesicoureteral reflux and have been associated with a higher incidence of urinary tract infection (3, 19). In addition, DJ stents were forgotten also to be a matter worth the attention of clinicians. The use of external stents avoids bladder-related symptoms, but it may be associated with a higher incidence of stent leakage, bleeding, and skin infection (8). Individualized customized stents may help to abate these issues.
One of the advantages that could not be ignored of the external stent was that it avoided the risk of secondary anesthesia. As far as we know, for most infants or children, additional general anesthesia is inevitable when removing DJ tubes (10). Considering the costs related to stent removal, the average cost of the external stent group was £686.7, which was lower than that of the DJ tube group of £1425.6 (8). In another author's findings, regarding open pyeloplasty, the application of an external stent was associated with a Canadian $565 cost decrease per patient (18).
However, there is not yet a standard type for external stents in pediatric pyeloplasty. Most of the available studies use commercial stents, ie Urosoft® multipurpose stent and Salle intraoperative pyeloplasty stent (Cook® Medical), which were accompanied by some degree of modification (8, 10, 20). The external stents are usually modified by removing the distal bladder curl and stents are terminated in the mid or lower ureter, thus effectively avoiding bladder irritation symptoms (3, 20). Professor Zoller et al. have designed a newly constructed spear for transrenal externalized catheter insertion with a blunt tip and a tapered end, which has the advantages of easy positioning and more minor bleeding (21). The fixation of the external stent is important. Almost all studies secure the catheter to the renal capsule so that the risk of stent displacement and exteriorization of the holes is minimized (9).
Although we performed a comprehensive analysis of the efficacy and safety of external stents and DJ stents, several limitations remained. First, the included studies were almost all retrospective studies, and only one RCT was involved. Due to a lack of evidence, more high-level studies are required to support this hypothesis. Second, the external stents of the included studies had numerous different types, which could be associated with heterogeneity. Third, because of the different definitions of renal function improvement and the small numbers reported on different types of complications, we failed to analyze it.
Conclusion
In conclusion, there were no significant differences in operative time, operative success rate, length of hospital stay, or complications between external stents and DJ stents in pediatric pyeloplasty. The external stented procedure seemed to have less operative time when using robot-assisted laparoscopic pyeloplasty. However, due to the limitations of our analysis, more studies are still required to support our conclusion.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author/s.
Author contributions
Conceived and designed the experiments: YL and JY. Analyzed the data: CM, LP, and KL. Contributed reagents, materials, and analysis: LG, KL, and JL. Wrote the manuscript: CM, LP, and LG. All authors have read and approved the final manuscript.
Funding
This study was supported by Sichuan Science and Technology Program under Grant number 2020YFS0320.
Acknowledgments
The authors feel grateful for the financial support by Sichuan Science and Technology Program under Grant number 2020YFS0320.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2022.933845/full#supplementary-material
References
1. Chertin B, Pollack A, Koulikov D, Rabinowitz R, Hain D, Hadas-Halpren I, et al. Conservative treatment of ureteropelvic junction obstruction in children with antenatal diagnosis of hydronephrosis: lessons learned after 16 years of follow-up. Eur Urol. (2006) 49:734–8. doi: 10.1016/j.eururo.2006.01.046
2. Peters CA, Schlussel RN, Retik AB. Pediatric laparoscopic dismembered pyeloplasty. J Urol. (1995) 153:1962–65. doi: 10.1016/S0022-5347(01)67378-6
3. Chu DI, Shrivastava D, Van Batavia JP, Bowen DK, Tong CC, Long CJ, et al. Outcomes of externalized pyeloureteral versus internal ureteral stent in pediatric robotic-assisted laparoscopic pyeloplasty. J Pediatr Urol. (2018) 14:450 e451–6. doi: 10.1016/j.jpurol.2018.04.012
4. Lee LC, Kanaroglou N, Gleason JM, Pippi Salle JL, Bagli DJ, Koyle MA, et al. Impact of drainage technique on pediatric pyeloplasty: comparative analysis of externalized uretero-pyelostomy versus double-J internal stents. Can Urol Assoc J. (2015) 9:E453–457. doi: 10.5489/cuaj.2697
5. Esposito C, Masieri L, Castagnetti M, Sforza S, Farina A, Cerulo M, et al. Robot-assisted vs laparoscopic pyeloplasty in children with uretero-pelvic junction obstruction (UPJO): technical considerations and results. J Pediatr Urol. (2019) 15:667 e661–e668. doi: 10.1016/j.jpurol.2019.09.018
6. Lee YS, Lee CN, Kim MU, Jang WS, Lee H, Im YJ, et al. The risk factors and clinical significance of acute postoperative complications after unstented pediatric pyeloplasty: a single surgeon's experience. J Pediatr Surg. (2014) 49:1166–70. doi: 10.1016/j.jpedsurg.2013.11.003
7. Bayne AP, Lee KA, Nelson ED, Cisek LJ, Gonzales ET Jr, Roth DR. The impact of surgical approach and urinary diversion on patient outcomes in pediatric pyeloplasty. J Urol. (2011) 186(Supp. 4):1693–98. doi: 10.1016/j.juro.2011.03.103
8. Paraboschi I, Jannello L, Mantica G, Roberts L, Olubajo S, Paul A, et al. Outcomes and costs analysis of externalized pyeloureteral versus internal double-j ureteral stents after paediatric laparoscopic anderson-hynes pyeloplasty. J Pediatr Urol. (2021) 17:232 e231–237. doi: 10.1016/j.jpurol.2020.12.006
9. Helmy T, Blanc T, Paye-Jaouen A, El-Ghoneimi A. Preliminary experience with external ureteropelvic stent: alternative to double-j stent in laparoscopic pyeloplasty in children. J Urol. (2011) 185:1065–9. doi: 10.1016/j.juro.2010.10.056
10. Sarhan O, Al Awwad A, Al Otay A, Al Faddagh A, El Helaly A, Al Ghanbar M, et al. Comparison between internal double J and external pyeloureteral stents in open pediatric pyeloplasty: a multicenter study. J Pediatr Urol. (2021) 17:511.e1–7. doi: 10.1016/S2666-1683(20)34006-4
11. Garg RK, Menon P, Narasimha Rao KL, Arora S, Batra YK. Pyeloplasty for hydronephrosis: issues of double J stent versus nephrostomy tube as drainage technique. J Indian Assoc Pediatr Surg. (2015) 20:32–6. doi: 10.4103/0971-9261.145444
12. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
13. Luo D, Wan X, Liu J, Tong T. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res. (2018) 27:1785–805. doi: 10.1177/0962280216669183
14. Clark HD, Wells GA, Huet C, McAlister FA, Salmi LR, Fergusson D, et al. Assessing the quality of randomized trials: reliability of the Jadad scale. Control Clin Trials. (1999) 20:448–52. doi: 10.1016/S0197-2456(99)00026-4
15. Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. (2010) 25:603–5. doi: 10.1007/s10654-010-9491-z
16. Sterne JA, Hernan MA, Reeves BC, Savovic J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. (2016) 355:i4919. doi: 10.1136/bmj.i4919
17. Sterne JAC, Savovic J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. (2019) 366:l4898. doi: 10.1136/bmj.l4898
18. Braga LH, Lorenzo AJ, Farhat WA, Bagli DJ, Khoury AE, Pippi Salle JL. Outcome analysis and cost comparison between externalized pyeloureteral and standard stents in 470 consecutive open pyeloplasties. J Urol. (2008) 180 (Suppl. 4):1693–98. doi: 10.1016/j.juro.2008.05.084
19. Kocvara R, Sedlacek J, Drlik M, Dite Z, Belacek J, Fiala V. Unstented laparoscopic pyeloplasty in young children (1-5 years old): a comparison with a repair using double-J stent or transanastomotic externalized stent. J Pediatr Urol. (2014) 10:1153–9. doi: 10.1016/j.jpurol.2014.04.017
20. Lombardo A, Toni T, Andolfi C, Gundeti MS. Comparative outcomes of double-J and cutaneous pyeloureteral stents in pediatric robot-assisted laparoscopic pyeloplasty. J Endourol. (2021) 35:1616–22. doi: 10.1089/end.2020.1115
21. Zoeller C, Lacher M, Ure B, Petersen C, Kuebler JF. Double J or transrenal transanastomotic stent in laparoscopic pyeloplasty in infants and children: a comparative study and our technique. J Laparoendosc Adv Surg Tech A. (2014) 24:205–9. doi: 10.1089/lap.2013.0338
22. Kong X, Li Z, Li M, Liu X, He D. Comparison of drainage methods after pyeloplasty in children: a 14-year study. Front Pediatr. (2021) 9:779614. doi: 10.3389/fped.2021.779614
23. Weitz M, Portz S, Laube GF, Meerpohl JJ, Bassler D. Surgery versus non-surgical management for unilateral ureteric-pelvic junction obstruction in newborns and infants less than two years of age. Cochrane Database Syst Rev. (2016) 7:CD010716. doi: 10.1002/14651858.CD010716.pub2
24. Zhu H, Wang J, Deng Y, Huang L, Zhu X, Dong J, et al. Use of double-J ureteric stents post-laparoscopic pyeloplasty to treat ureteropelvic junction obstruction in hydronephrosis for pediatric patients: a single-center experience. J Int Med Res. (2020) 48:300060520918781. doi: 10.1177/0300060520918781
25. Nagdeve NG, Bhingare PD, Sarawade P. A randomized control trial comparing outcome after stented and nonstented anderson-hynes dismembered pyeloplasty. J Indian Assoc Pediatr Surg. (2018) 23:186–91. doi: 10.4103/jiaps.JIAPS_58_17
26. Nordenstrom J, Koutozi G, Holmdahl G, Abrahamsson K, Sixt R, Sjostrom S. Changes in differential renal function after pyeloplasty in infants and children. J Pediatr Urol. (2020) 16:329>e321–28. doi: 10.1016/j.jpurol.2020.02.002
27. Kawahara T, Sakamaki K, Ito H, Kuroda S, Terao H, Makiyama K, et al. Developing a preoperative predictive model for ureteral length for ureteral stent insertion. BMC Urol. (2016) 16:70. doi: 10.1186/s12894-016-0189-8
28. Shrewsberry AB, Al-Qassab U, Goodman M, Petros JA, Sullivan JW, et al. A +20% adjustment in the computed tomography measured ureteral length is an accurate predictor of true ureteral length before ureteral stent placement. J Endourol. (2013) 27:1041–5. doi: 10.1089/end.2013.0041
Keywords: UPJO, external stent, Double J, pediatric pyeloplasty, meta-analysis
Citation: Meng C, Gan L, Li K, Peng L, Li J, Yang J and Li Y (2022) Comparison of external stents and DJ stents techniques for pediatric pyeloplasty: A systematic review and meta-analysis. Front. Pediatr. 10:933845. doi: 10.3389/fped.2022.933845
Received: 01 May 2022; Accepted: 01 August 2022;
Published: 25 August 2022.
Edited by:
Lisandro Ariel Piaggio, Universidad Nacional del Sur, ArgentinaReviewed by:
Osama Mahmoud Sarhan, Mansoura University, EgyptRiccardo Tellini, Careggi University Hospital, Italy
Santiago Vallasciani, Sidra Medicine, Qatar
Copyright © 2022 Meng, Gan, Li, Peng, Li, Yang and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yunxiang Li, bGl5dW54aWFuZzM2OUAxMjYuY29t
†These authors have contributed equally to this work
 Chunyang Meng
Chunyang Meng Lijian Gan1†
Lijian Gan1† Yunxiang Li
Yunxiang Li