- 1Department of Paediatrics, Institute of Clinical Sciences, University of Gothenburg, Sahlgrenska Academy, Gothenburg, Sweden
- 2Region Västra Götaland, Department of Paediatrics, The Queen Silvia Children's Hospital, Sahlgrenska University Hospital, Gothenburg, Sweden
- 3Department of Paediatrics and Child Health, Charlotte Maxeke Johannesburg Academic Hospital, Johannesburg, South Africa
- 4School of Clinical Medicine, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
Background: The neonatal mortality rate in South Africa is lower than the global average, but still approximately five times higher than some European and Scandinavian countries. Prematurity, and its complications, is the main cause (35%) of neonatal deaths.
Objective: To review the maternal, delivery period and infant characteristics in relation to mortality in very low birth weight (VLBW) infants at Charlotte Maxeke Johannesburg Academic Hospital (CMJAH).
Methods: This was a retrospective descriptive study of VLBW infants admitted to CMJAH between 1 January 2017 and 31 December 2018. All infants with a birth weight between 500 to ≤ 1,500 grams were included. The characteristics and survival of these infants were described using univariate analysis.
Results: Overall survival was 66.5%. Provision of antenatal steroids, antenatal care, Cesarean section, female sex, resuscitation at birth, and 5-min Apgar score more than five was related with better survival to discharge. Among respiratory diagnoses, 82.8% were diagnosed with RDS, 70.8% received surfactant therapy and 90.7% received non-invasive respiratory support after resuscitation. At discharge, 59.5% of the mothers were breastfeeding and 30.8% spent time in kangaroo mother care.
Conclusion: The two-thirds survival rate of VLBW infants is similar to those in other developing countries but still remains lower than developed countries. This may be improved with better antenatal care attendance, coverage of antenatal steroids, temperature control after birth, improving infection prevention and control practices, breastfeeding rates and kangaroo mother care. The survival rate was lowest amongst extremely low birth weight (ELBW) infants.
Introduction
In South Africa, the under-5 mortality rate in 2017 was 37.1 per 1,000 live births (1). South Africa and the rest of Sub-Saharan Africa failed to achieve the fourth Millennium Development Goal from the United Nations of a two-thirds reduction in the under-5 mortality rate (2). This is largely due to the relatively slow decline in the neonatal mortality rate over the last two decades (3).
During the neonatal period the mortality was 10.7 per 1,000 live births (4). While this is lower than the global average during the same time period (18.0 per 1,000 live births), it is higher than rates found in developed countries, such as Japan (0.9 per 1,000 live births), and approximately five times higher than some European and Scandinavian countries (4).
Prematurity, and its complications, is the main cause (35%) of neonatal deaths according to estimates developed by the United Nations Inter-agency Group for Child Mortality Estimation in their report from 2019. The second and third largest reasons contributing to neonatal mortality are intrapartum-related complications (24%) and sepsis (15%) (5). According to a review from The Gambia, factors which contribute to neonatal mortality include lack of antenatal care, birth weight <1,500 grams, hypothermia after birth and delivery outside teaching hospital (6).
The complications of preterm birth are many, due to immaturity of multiple organ systems (7). Some of these are intraventricular hemorrhage (IVH), respiratory distress syndrome (RDS), pulmonary hemorrhage, bronchopulmonary dysplasia (BPD), necrotizing enterocolitis (NEC), patent ductus arteriosus (PDA), and retinopathy of prematurity (ROP).
This study aimed to review the maternal, delivery period and infant characteristics in relation to mortality in VLBW infants at the CMJAH. The acquired information will be useful to improve the neonatal care and neonatal survival at CMJAH.
Materials and methods
Study design
This was a retrospective observational study of VLBW infants admitted to CMJAH. All infants with birth weight between 500 to ≤ 1,500 grams, born between 1 January 2017 and 31 December 2018 and admitted to the neonatal unit at CMJAH were included. Infants with incomplete data for birth weight, place of birth and date of outcome were excluded.
Setting
Charlotte Maxeke Johannesburg Academic Hospital (CMJAH) is a large tertiary referral hospital within the public hospital framework in South Africa. South Africa is considered a developing country and has limited health resources and high patient numbers. In this setting it is not possible to provide full support to every very low birth weight (VLBW) infant due to necessity of rationing care. Therefore, intermittent positive pressure ventilation (IPPV) after the resuscitation period is not routinely provided to infants who weigh <800 grams in this institution based on anticipated poor outcome, prolonged ventilation, and high use of resources.
At CMJAH there is a quality improvement project called PRINCE—the Project to Improve Neonatal Care—with the purpose to develop targeted interventions to improve the neonatal care and clinical outcome of infants at CMJAH. PRINCE has been accredited as a research programme within the Faculty of Health Science at the University of Witwatersrand.
Database and data collection
Data was managed using the Research Electronic Data Capture (REDCap) computer database, hosted by the University of Witwatersrand (8, 9). The REDCap computer database at CMJAH started in 2013 and information is collected at discharge. Medical staff collect the data from the patient records, before it is entered on to a computer summary form and then the database itself, with multiple checks and verification. Records contain information such as demographics, clinical characteristics, hospital course, and outcome at discharge.
Variables
Variables were selected from amongst those available from the database and considered as of possible importance for preterm delivery and the short-term outcome. The studied maternal characteristics were: maternal age, multiple gestation, parity, maternal HIV status, maternal syphilis, antenatal care, antenatal steroids. The studied characteristics for the delivery period were: place of birth (inborn or outborn), mode of delivery (vaginal or Cesarean section), 5-min Apgar score. The studied infant characteristics were: gestational age, birth weight, head circumference at birth, sex, birth HIV PCR, initial resuscitation in the delivery room, and hypothermia.
Factors related to hospital stay and neonatal complications that were studied included age on admission, age at outcome, respiratory diagnosis (RDS, congenital pneumonia, pulmonary hemorrhage, pneumothorax), surfactant therapy at any time, respiratory support after initial resuscitation (non-invasive or invasive), any respiratory support after 36 weeks, steroids for BPD, screening for ROP, ROP stage 3 or 4, IVH grade 3 or 4, PDA, NEC grade 2 or 3, early-onset sepsis, late-onset sepsis, surgery for NEC, other surgery, blood transfusion, neonatal jaundice requiring phototherapy, congenital anomalies, Kangaroo Mother Care (KMC), and breastfed at discharge.
Definitions
VLBW infants were defined as birth weight ≤ 1,500 grams. Extremely low birth weight (ELBW) infants were defined as birth weight ≤ 1,000. Short-term outcome was defined as death or survival to discharge. For diseases, standard definitions as per the Vermont Oxford Network were used (10). Sepsis was defined as blood-culture proven isolation of a pathogenic organism. Early-onset sepsis was defined as onset within 72 h of life and late-onset sepsis after 72 h of life. Patent ductus arteriosus was diagnosed with echocardiography (performed by cardiologists) after clinical suspicion.
Attendance at antenatal care constituted at least one antenatal visit during pregnancy. Place of birth was divided into inborn (infants born within CMJAH) and outborn, including infants born before arrival, at midwife obstetric units or born at other hospitals and referred to CMJAH. Mode of delivery was divided into vaginal delivery (including vertex and breech presentation) and Cesarean section (including elective and emergency cases). Gestational age at birth was decided from the best obstetric estimation available (firstly maternal dates, secondly early ultrasound or thirdly late ultrasound). If none of the above was available, gestational age was estimated using the Ballard Score (11).
Hypothermia was defined as body temperature <36.5 degrees Celsius, measured within 1 h of admission to the neonatal unit. Respiratory support after initial resuscitation was divided into non-invasive and invasive ventilation. Non-invasive respiratory support included nasal-prong oxygen, nasal continuous positive airway pressure (NCPAP) and high flow nasal cannula oxygen, whereas invasive respiratory support included conventional mechanical ventilation and high frequency ventilation. Similarly, respiratory support at 36 weeks was used to determine severity of BPD, based on the level of support of the earlier mentioned alternatives. During the study period, there was a weight cut off for invasive ventilation at 800 grams and for NCPAP at 750 grams. ELBW who did not qualify for invasive or non-invasive ventilation due to their birth weight, were offered surfactant then placed on nasal prong oxygen.
Mothers were screened for HIV at antenatal care visits and again at delivery. Babies born to HIV-positive mothers had an HIV PCR test performed at birth and were put on to HIV prophylaxis dependent on their level of exposure risk. The requirements for surfactant therapy were preterm infants who were hemodynamically stable, with changes suggestive of RDS on chest X-ray, who had respiratory distress and who required fraction of inspired oxygen ≥40% oxygen to keep oxygen saturations >89%. Cranial ultrasound was performed within the first seven days of life and repeated at 10–14 days of life and then again prior to discharge.
All babies with a birth weight ≤ 1,500 grams or gestational age at birth below 32 weeks, were screened for ROP, at 4 to 6 weeks chronological age. Breastfed on discharge included breastmilk only, fortified breastmilk or breastmilk and formula together. KMC included both intermittent and continuous. KMC was introduced once a baby weighed over 1,200 grams, tolerated full enteral feeds, had an adequate weight gain (>15 g/kg/day), was off supplemental oxygen and could maintain temperature and glucose levels. Survival as outcome included discharged to home or transferred to another hospital. Babies were discharged home once they had achieved a weight of 1,600 grams, established enteral feds, were off supplemental oxygen, maintained temperature and glucose levels.
Statistical analysis
Statistical analysis was performed using IBM SPSS Statistics version 25. Frequencies and percentages were used to describe categorical variables. Continuous variables were described using mean and standard deviation if they were normally distributed, and median and interquartile ranges (IQR) if they were skewed. Univariate analysis was performed to determine significant associations of various factors with survival at discharge. Unpaired t-tests were used comparing normally distributed continuous variables and Mann-Whitney U tests for skewed distribution. Chi-Square tests were used to compare categorical variables. A p-value of <0.05 was considered significant. Only valid cases were analyzed for each variable (i.e., cases with missing data were excluded from the analysis). Thereafter a multiple logistic regression model with mortality as the binary outcome variable was performed. Variables that were (1) significantly associated with mortality in univariate analysis, (2) had a sufficient number of valid cases, (3) passed the assumption of linearity using Box-Tidwell procedure, (4) were not transformed as part of the initial univariate analysis, and (5) were appropriate were included in the model.
Ethics
Ethical approval for the study was obtained from the Human Research Ethics Committee of the University of the Witwatersrand (clearance certificate number M190874). As this was a retrospective audit of an existing database, informed consent was waived. All methods were carried out in accordance with relevant guidelines and regulations.
Results
There were 946 VLBW infants admitted during the study period. Eight infants were excluded (seven infants weighed <500 grams at birth, one infant did not have a date of outcome recorded), 938 VLBW infants were included in the study. The overall survival rate was 66.5% (624/938). The mean birth weight was 1,093.6 grams (SD: ± 249.9), mean gestational age at birth was 28.9 weeks (SD: ± 2.8) and median age at outcome was 27.0 days (IQR: 38).
Maternal details and delivery period
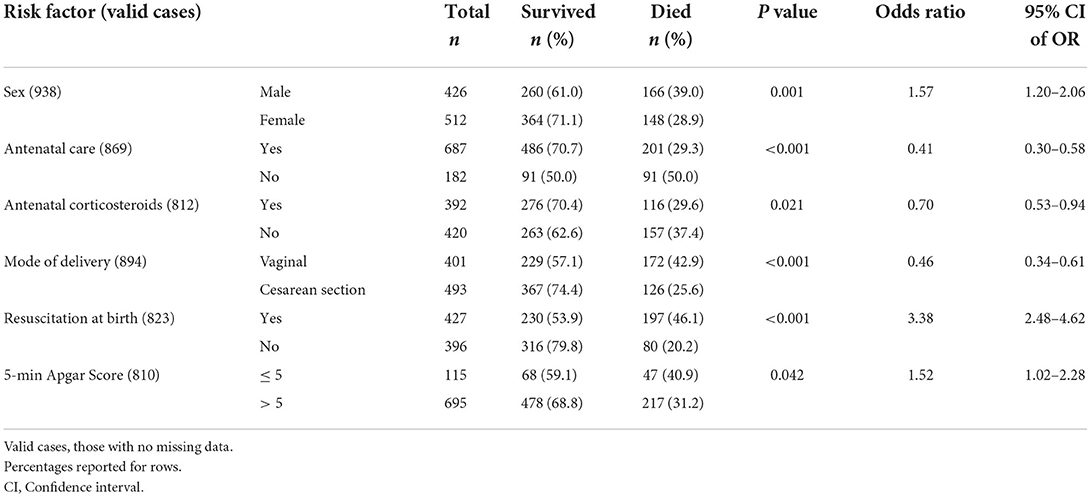
The mean maternal age was 28.8 years (SD: ± 6.4) and 28.5% (222/780) were primiparous. There were 16.6% (152/913) multiple gestation. Risk factors with significant result for mortality related to antenatal care, labor and delivery are presented in Table 1.
Among the mothers 29.6% (275/929) were HIV positive and 1.7% (16/868) positive for syphilis. A total of 78.6% (737/938) infants were inborn. Temperature measured within 1 h of admission showed 60.8% (463/762) of the infants had hypothermia. These results were not significant in relation to mortality.
Infant details
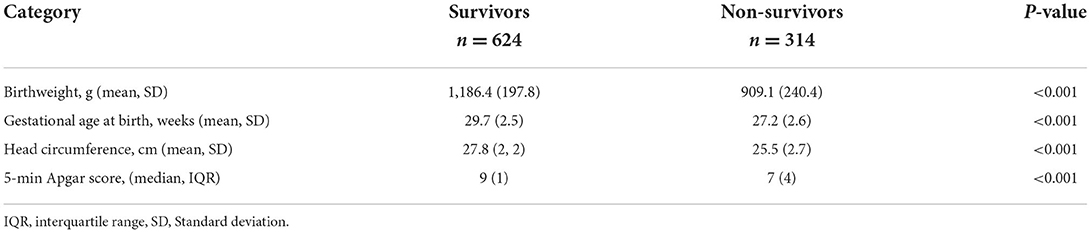
The birthweight, gestational age and head circumference of survivors were significantly greater compared with the infants who died (see Table 2). The 5-min Apgar score of survivors was significantly higher than for the non-survivors (see Table 2). Birth HIV PCR was done in 93.6% (249/266) of cases where the mother was HIV positive and of these 2.8% (7/249) infants were positive for HIV.
Survival by birth weight category is shown in Figure 1. The survival of infants with a birthweight from 1,000 to <1,500 grams was 82.2% (514/625) and was significantly greater (p < 0.001) compared to the group of extremely low birth weight infants (ELBW) at 35.1% (110/313).

Figure 1. Survival by weight category. Survival of very low birth weight infants by birth weight category.
Hospital stay and neonatal period
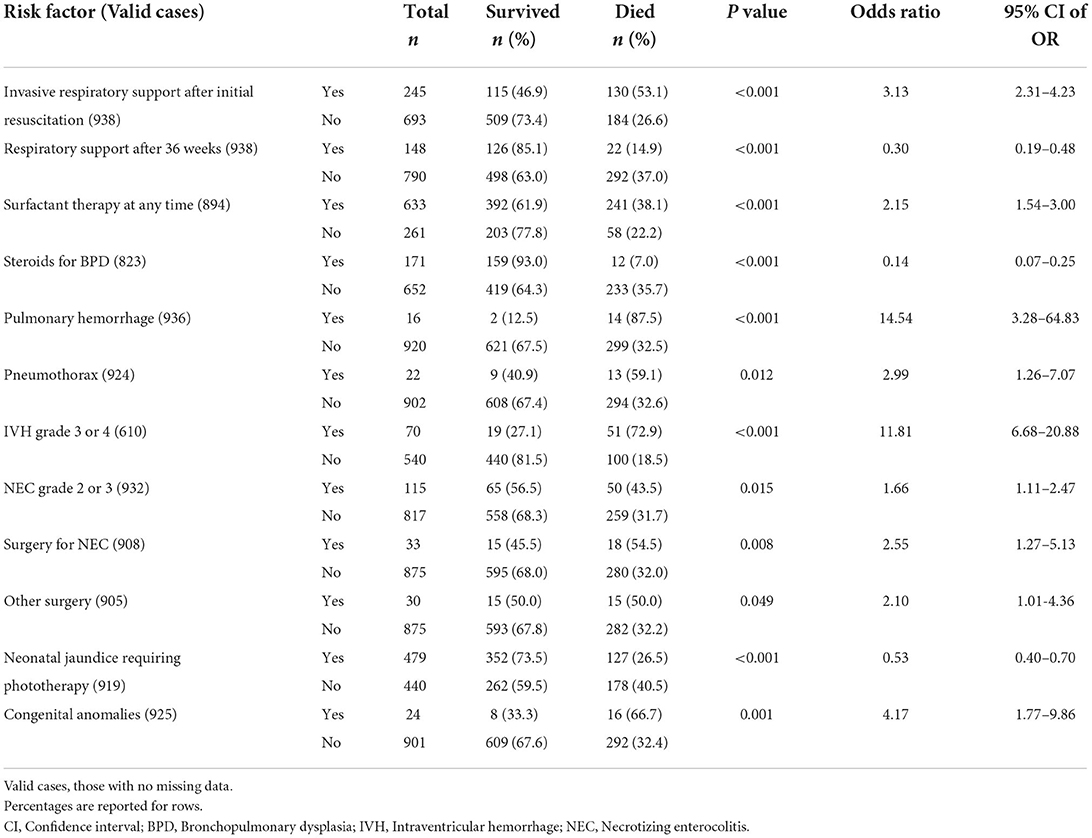
Treatments and complications during the neonatal period and hospital stay with statistically significant result for mortality are shown in Table 3.
There were 90.7% (851/938) of infants who received non-invasive respiratory support after initial resuscitation. Under respiratory diagnosis, 82.8% (777/895) of the infants were diagnosed with RDS and 0.5% (5/935) babies with congenital pneumonia. These results were not significant in relation to mortality. Other respiratory diagnoses which were significant in relation to mortality are included in Table 3.
PDA was reported in 9.2% (85/927) of cases. Among the infants with sepsis there were 4.5% (42/902) with early-onset sepsis and 32% (298/930) with late-onset sepsis. 43.2% (399/924) of the infants received blood transfusion. These results were not significant in relation to mortality.
Screening for ROP occurred in 30.1% (273/906) of the infants and among these 2.9% (8/273) of infants had ROP stage 3 or 4. Breastfeeding at discharge occurred in 59.5% (322/541) of the infants and 30.8% (283/920) spent time in KMC.
There were 22 significant variables on univariate analysis. Six variables (steroids for BPD, pulmonary hemorrhage, pneumothorax, congenital anomalies, IVH grade 3 or 4, and other surgery) were excluded as there were not enough valid cases for both outcomes to include in the logistic regression model. The three continuous variables (birthweight, head circumference, and gestational age) all failed the Box-Tidwell procedure for linearity and were thus excluded from the model. 5-min Apgar score was presented as both an ordinal variable and a transformed categorical variable and was excluded as neither were appropriate for this model. NEC surgery was excluded as it is dependent on NEC 2 or 3, to avoid circular reasoning.
Of the 10 predictor variables included (sex, antenatal care, antenatal steroids, mode of delivery, resuscitation at birth, invasive respiratory support after initial resuscitation, respiratory support after 36 weeks, surfactant at any time, NEC 2 or 3, and neonatal jaundice), seven were statistically significant as shown in Table 4. The logistic regression model explained 44.0% of the variance in outcome and correctly classified 79.5% of cases.
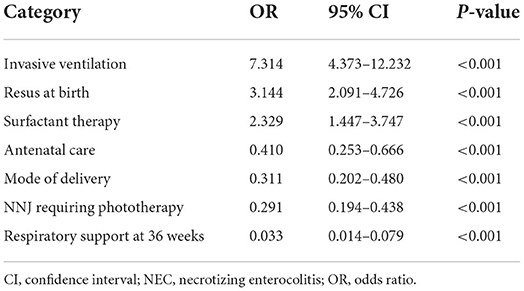
Table 4. Multivariate logistic regression for factors associated with mortality in very low birth weight infants at Charlotte Maxeke Johannesburg Academic Hospital.
Discussion
This retrospective review showed an overall two-thirds survival of VLBW infants. This is decreased when compared with the results from previous studies at the same unit where the overall survival of VLBW infants in 2006/2007 was 70.5% and in 2013 was 73.4% (12, 13). These survival rates are similar to those found in other parts of South Africa namely the Eastern Cape province (68.0%), but lower than reported in the Western Cape (81.7%) and in Limpopo (77.4%) (14–16). Further afield, the survival rate in this study compares to other developing countries (like India and Iran) (17, 18) but still remains lower than developed countries (19).
The survival of ELBW in this study is comparable to that found in the 2006/2007 study (13), but lower than the more recent study from the same unit in 2013 (12). Sadly, our results amount to only about half the survival rate that was achieved in a study from the Western Cape (20).
A possible reason for the lower survival rate could be the increase in late-onset sepsis in this study. In 2013, 19% of the VLBW infants at CMJAH had late-onset sepsis, whereas in this study there was an incidence of 32% (12). This may be a consequence of over-crowding or poor adherence to infection prevention and control practices.
In this study 78.6% of the infants were inborn which could be compared with 81.5% in 2006/2007 and 84.3% in 2013 (12, 13). The result was not significant in relation to mortality, which it was in 2006/2007 and 2013. A study in Cape Town, South Africa, found that being inborn was significantly associated with improved survival and decreased morbidity: mothers of inborn infants were more likely to receive antenatal care and antenatal steroids, inborn infants required less ventilatory support, surfactant administration and developed less late-onset sepsis, IVH and BPD (21).
When it comes to antenatal steroids, the coverage in this study had improved slightly (from 39.1 to 48%) compared to 2013 (12). However, this remains poor compared to other South African studies (15, 16, 22). Despite this improvement the goal should be even higher since antenatal steroids have an effect on RDS (hence the amount of respiratory support required for patients), as well as the rates of NEC and IVH (23). Lategan et al. found that exposure to any antenatal steroids was associated with a nearly three-quarter reduction in mortality in their cohort of preterm infants ≤ 1,800 (15). Concerted efforts need to be made to further improve the coverage of antenatal steroids.
Despite the modest improvement in antenatal steroid coverage, the rates of NEC (12.3% vs. 7.3%) and IVH (11.5% vs. 7.9%) in this study has increased compared to 2013 (12). The increased rate of NEC may be due to the increased rate of late-onset sepsis as mentioned above, and vice versa. The increased rate of IVH may be due to increased screening.
When measuring body temperature within 1 h of admission, 60.8% of the infants had hypothermia (skin temperature <36.5 degrees Celsius). Earlier studies done at the same department had not stated their definition of hypothermia, so no comparison could be made. However, this is interpreted as a large number and needs to be improved. Hypothermia increases morbidity (of which RDS is one) and mortality (22). This may have contributed to the large number of infants diagnosed with RDS in this study. Simple, cost-effective measures can be employed to prevent hypothermia, such as increasing awareness of its dangers, regular body temperature monitoring, warmed delivery rooms, providing infants with caps and plastic bags to limit heat loss, and making use or servo-controlled incubators and radiant warmers (which are already in use).
Several diseases showed significant association with mortality, such as pulmonary hemorrhage, congenital anomalies, IVH and NEC. This indicates the severity of these conditions. In addition, surgery for NEC and other surgery were also significantly associated with mortality, although that may be related to the severity of the condition rather than the surgery itself. Predictably, infants with congenital anomalies had higher mortality. It is unit policy not to offer invasive ventilation to infants with congenital anomalies with poor prognosis (e.g., Trisomy 13 and 18).
Taking logistic regression into consideration, receiving any respiratory support during initial resuscitation, surfactant at any time, as well as invasive ventilation after initial resuscitation was associated with higher odds of mortality. The high use of surfactant replacement therapy found in this study is concerning. During the study period, delays were frequently encountered when instituting NCPAP due to equipment shortages. This may have caused infants to deteriorate sufficiently to necessitate surfactant replacement therapy. Efforts have been made to address the delays and improve the use of NCPAP, thereby decreasing the use of surfactant therapy.
Several improvements can be made in the neonatal care prior to discharge. For instance, screening for ROP is supposed to be done on all VLBW infants and was only performed in one third of them prior to discharge in this study. This is still an improvement compared to 2006/2007 when 18.3% of the infants were screened for ROP prior discharge (13). Since the infants are discharged at 1,600 grams, the appropriate time for screening may be after discharge—infants were referred for ophthalmological screening as an outpatient.
In recent years, efforts have been made to increase the number of breastfed infants at discharge, considering the well-documented benefits of breastfeeding and its affordability. To this end, several lactation consultants have been employed. As a result, the number of breastfed infants at discharge has nearly doubled from 2013 (30.5%) to the current rate in this study, which is commendable (12).
On the other hand, KMC has decreased in this study compared with 2006/2007 (30.8% vs. 44.5%) (13). The limitations of KMC in this unit is the availability of mothers—many are single parent households and have to be at home looking after other children. It is important to improve these numbers again since KMC has shown positive results when it comes to better weight gain, earlier hospital discharge and higher exclusive breastfeeding rates in VLBW infants (24, 25).
Limitations
We acknowledge several limitations to this study. This was a retrospective analysis of an existing database, so some information was missing. Additionally, certain data such as usage of parental nutrition and antibiotics usage, is not routinely collected in the database and were therefore not analyzed. Our study favored maternal dates and Ballard score to determine gestational age as access to early ultrasound is poor. The short-term outcome of survival to discharge included infants discharged home and to other hospitals. We did not look at categorizing the timing of when deaths took place which would be useful in identifying trends. Importantly, this is not a population-based study. This study was conducted in a referral hospital with access to the appropriate level of care, as per national guidelines.
Conclusion
This study showed a two thirds survival rate in VLBW infants, which is similar to those in other developing countries (like India and Iran) but still remain lower than developed countries. A large number of patients are placing a burden on a hospital with limited resources. The survival rate can be improved by increasing antenatal care attendance, coverage of antenatal steroids, improving temperature control to decrease the high rates of hypothermia, improving infection prevention and control practices, breastfeeding rates and the use of KMC. Improved screening for morbidities such as ROP and IVH should also be emphasized.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by University of the Witwatersrand Human Research Ethics Committee. Written informed consent from the participants' legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author contributions
KI conceptualized and designed the study, collected data, carried out data analysis, drafted the initial manuscript, revised the manuscript, and approved the final manuscript. AE, EH, and RS participated in protocol development, supervised the study, reviewed and revised the manuscript, and approved the final manuscript. DB supervised the study, revised the manuscript, and approved the final manuscript. All authors contributed to the article and approved the submitted version.
Funding
This study was financially supported by Stena A. Olssons Stiftelse för Forskning och Kultur and Adlerbertska Scholarship Foundation with their scholarships. Further, this work was supported by grants from the Swedish state under the agreement between the Swedish government and the county councils, the ALF agreement (ALFGBG- 117661).
Acknowledgments
A special thanks to Rose Bandini for her great knowledge and assistance during the statistical analysis.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
BPD, Bronchopulmonary dysplasia; CMJAH, Charlotte Maxeke Johannesburg Academic Hospital; ELBW, Extremely low birth weight; IPPV, Intermittent positive pressure ventilation; IVH, Intraventricular hemorrhage; KMC, Kangaroo Mother Care; NCPAP, Nasal continuous positive airway pressure; NEC, Necrotizing enterocolitis; NNJ, Neonatal jaundice; PDA, Patent ductus arteriosus; PRINCE, Project to Improve Neonatal Care; RDS, Respiratory distress syndrome; REDCap, Research Electronic Data Capture; ROP, Retinopathy of prematurity; VLBW, Very low birth weight.
References
1. World health organization: World Health Statistics data visualization dashboard. Under-five mortality rate 2017. Available online at: http://apps.who.int/gho/data/node.sdg.3-2-viz?lang=en (2017). (accessed Sep 16, 2019).
2. United Nations. The Millennium Development Goals Report 2015. Available online at: https://www.un.org/millenniumgoals/2015_MDG_Report/pdf/MDG%202015%20rev%20(July%201).pdf (2015). (accessed Sep 17, 2019).
3. Rhoda NR, Velaphi S, Gebhardt GS, Kauchali S, Barron P. Reducing neonatal deaths in South Africa: progress and challenges. S Afr Med J. (2018) 108 (3 Suppl 1):S9–16. doi: 10.7196/SAMJ.2017.v108i3b.12804
4. World Health Organization: World Health Statistics Data Visualization Dashboard. Neonatal Mortality 2017. Available online at: http://apps.who.int/gho/data/node.sdg.3-2-viz-3?lang=en. (accessed 16 Sep 2019).
5. United Nations Inter-agency Group for Child Mortality Estimation. Levels & Trends in Child Mortality Report 2019. Available online at: https://childmortality.org/reports (2019). (accessed October 17, 2019).
6. Okomo UA, Dibbasey T, Kassama K, Lawn JE, Zaman SMA, Kampmann B, et al. Neonatal admissions, quality of care and outcome: 4 years of inpatient audit data from The Gambia's teaching hospital. Paediatr Int Child Health. (2015) 35:252–64. doi: 10.1179/2046905515Y.0000000036
7. Ward RM, Beachy JC. Neonatal complications following preterm birth. BJOG. (2003) 110:8–16. doi: 10.1046/j.1471-0528.2003.00012.x
8. Harris PA, Taylor R, Minor BL, Elliot V, Fernandez M, O'Neal L, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. (2019) 95:103208. doi: 10.1016/j.jbi.2019.103208
9. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. (2009) 42:377–81. doi: 10.1016/j.jbi.2008.08.010
10. Vermont Oxford Network. Available online at: https://public.vtoxford.org. (accessed Oct 30, 2019).
11. Ballard Score: Score Sheet. Availabe online at: https://www.ballardscore.com/ScoreSheet/ScoreSheet (2019). (accessed Jan 07, 2020).
12. Ballot DE, Chirwa T, Ramdin T, Chirwa L, Mare I, Davies VA, et al. Comparison of morbidity and mortality of very low birth weight infants in a central hospital in Johannesburg between 2006/2007 and 2013. BMC Pediatr. (2015) 15:20. doi: 10.1186/s12887-015-0337-4
13. Ballot DE, Chirwa TF, Cooper PA. Determinants of survival in very low birth weight neonates in a public sector hospital in Johannesburg. BMC Pediatr. (2010) 10:30. doi: 10.1186/1471-2431-10-30
14. Michaelis IA, Krägeloh-Mann I, Manyisane N, Mazinu MC, Jordaan ER. Prospective cohort study of mortality in very low birthweight infants in a single centre in the eastern cape province, South Africa. BMJ Paediatr Open. (2021) 5:e000918. doi: 10.1136/bmjpo-2020-000918
15. Lategan I, Price C, Rhoda NR, Zar HJ, Tooke L. Respiratory interventions for preterm infants in LMICs: a prospective study from cape town, South Africa. Front Glob Womens Health. (2022) 3:817817. doi: 10.3389/fgwh.2022.817817
16. Ntuli TS, Mashego MPA, Shipalana N, Sutton C, Hamese MHK. Factors associated with preterm very low birthweight infant mortality at a tertiary hospital in Limpopo Province, South Africa. S Afr J Child Health. (2020) 14:10–4. doi: 10.7196/SAJCH.2020.v14.i1.1591
17. Afjeh SA, Sabzehei MK, Fallahi M, Esmaili F. Outcome of very low birth weight infants over 3 years report from an Iranian center. Iran J Pediatr. (2013) 23:579–87.
18. NNPD Network, India. National Neonatal-Perinatal Database Report 2002-2003. Available online at: https://www.newbornwhocc.org/pdf/nnpd_report_2002-03.PDF (2005). (accessed Decembeer 06, 2019).
19. Numerato D, Fattore G, Tediosi F, Zanini R, Peltola M, Banks H, et al. Mortality and length of stay of very low birth weight and very preterm infants: a EuroHOPE study. PLoS ONE. (2015) 10:e0131685. doi: 10.1371/journal.pone.0131685
20. Musiime GM, Lloyd LG, McCaul M, van Zyl N. Holgate SL. Outcomes of extremely low-birthweight neonates at a tertiary hospital in the Western Cape, South Africa: a retrospective cohort study. S Afr J CHild Health. (2021) 15:170–5. doi: 10.7196/SAJCH.2021.v15.i3.1799
21. Gibbs L, Tooke L, Harrison MC. Short-term outcomes of inborn v. outborn very-low-birth-weight neonates (<1 500g) in a neonatal nursey at Groote Schuur Hospital, Cape Town, South Africa. S Afr Med J. (2017) 107:900–3. doi: 10.7196/SAMJ.2017.v107i10.12463
22. Ng'eny JC, Velaphi S. Hypothermia among neonates admitted to the neonatal unit at a tertiary hospital in South Africa. J Perinatol. (2020) 40:433–8. doi: 10.1038/s41372-019-0539-y
23. Bonanno C, Wapner RJ. Antenatal corticosteroids in the management of preterm birth: are we back where we started? Obstet Gynecol Clin North Am. (2012) 39:47–63. doi: 10.1016/j.ogc.2011.12.006
24. Ramanathan K, Paul VK, Deorari AK, Taneja U, George G. Kangaroo mother care in very low birth weight infants. Indian J Pediatr. (2001) 68:1019–23. doi: 10.1007/BF02722345
Keywords: survival, short-term outcomes, infant, prematurity, neonatal mortality, very low birth weight (VLBW), premature neonate, low- and lower-middle-income countries
Citation: Ingemyr K, Elfvin A, Hentz E, Saggers RT and Ballot DE (2022) Factors influencing survival and short-term outcomes of very low birth weight infants in a tertiary hospital in Johannesburg. Front. Pediatr. 10:930338. doi: 10.3389/fped.2022.930338
Received: 27 April 2022; Accepted: 25 August 2022;
Published: 16 September 2022.
Edited by:
Susan Coffin, University of Pennsylvania, United StatesReviewed by:
Lizelle Van Wyk, Tygerberg Hospital, South AfricaLloyd Tooke, University of Cape Town, South Africa
Copyright © 2022 Ingemyr, Elfvin, Hentz, Saggers and Ballot. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kristin Ingemyr, a3Jpc3Rpbi5pbmdlbXlyQGdtYWlsLmNvbQ==
 Kristin Ingemyr
Kristin Ingemyr Anders Elfvin
Anders Elfvin Elisabet Hentz1,2
Elisabet Hentz1,2 Robin T. Saggers
Robin T. Saggers Daynia E. Ballot
Daynia E. Ballot