- Clinical Laboratory, DongYang People's Hospital, Dongyang, China
This study aimed to assess the association of early severe thrombocytopenia and platelet course with in-hospital mortality in critically ill children. Data of critically ill children in this study were obtained from the Pediatric Intensive Care Database. Patients with and without severe thrombocytopenia were adjusted for covariates using propensity score matching (PSM) to ensure the robustness of the results. Univariate and multivariate logistic regression analyses were performed on the original and PSM cohorts, respectively. Results are presented as odds ratios (ORs) with 95% confidence intervals (95% CI). In studies of the platelet course, logistic regression analysis was used to assess the effect of different degrees of recovery on in-hospital mortality in critically ill children with early severe thrombocytopenia. The study included 4,848 critically ill children, of whom 450 with early severe thrombocytopenia were matched to 450 without early severe thrombocytopenia. Univariate and multivariate logistic regression results showed that early severe thrombocytopenia was an independent risk factor for in-hospital mortality in critically ill children in both the original and PSM groups. In addition, the study results of platelet course showed that the recovery of platelet count to ≥150 × 109/L in the short term was a protective factor for the prognosis of patients (OR, 0.301; 95% CI, 0.139–0.648, P = 0.002). Our study revealed that early severe thrombocytopenia is an independent risk factor for in-hospital mortality in critically ill children. In addition, in-hospital mortality was significantly reduced in children with early severe thrombocytopenia, whose platelet count returned to normal levels in the short term.
Introduction
Early prognostic assessment of critically ill children is critical. If children with poor prognoses are identified earlier, the clinical interventions can be immediately implemented, resulting in a higher survival rate. However, children are less able to describe their own conditions than adults and find it more difficult to cooperate with some clinical examinations. Although intensive care for pediatric patients has greatly improved in recent decades, there are few independent, objective, and easily accessible early indicators of mortality in critically ill children.
Platelets serve various functions, including hemostasis, thrombosis, inflammation, and vascular regeneration (1). Platelet count is an objective indicator determined by routine blood tests. As a result, changes in absolute platelet count can be observed in a wide range of diseases involving various organ systems (2–4). A decrease in platelet count is common in critically ill patients (5, 6). The most common explanation is that platelets are activated to help with hemostasis, resulting in “consumption” exceeding “production” (7).
Patients with absolute platelet counts of <50 × 109/L, as opposed to mild thrombocytopenia, frequently require clinical interventions, such as platelet transfusions, to prevent bleeding (8). Therefore, severe thrombocytopenia requires more medical attention. Severe thrombocytopenia is a prognostic risk factor in critically ill neonatal and adult patients, with increased mortality and hospital stay (9, 10). However, owing to a lack of relevant studies, the prognostic value of early severe thrombocytopenia in critically ill children remains unknown.
Therefore, we verified the prognostic value of early severe thrombocytopenia in critically ill children using a retrospective analysis of a large public database called Pediatric Intensive Care (PIC). This study aimed to investigate the association between early severe thrombocytopenia and platelet course and in-hospital mortality in critically ill children.
Materials and Methods
Data source
Pediatric Intensive Care is a pediatric-specific database that contains data on more than 13,000 admissions of critically ill pediatric patients admitted to the Children's Hospital of Zhejiang University School of Medicine between 2010 and 2018 (11). Children's Hospital of Zhejiang University School of Medicine is China's National Clinical Research Center for Children's Health. As a medical center exclusive to children, it contains 119 intensive care beds in cardiac, general, pediatric, surgical, and neonatal intensive care units (ICUs). Patient statistics of the PIC database stratified by care units can be found in the introduction to the original database (http://pic.nbscn.org) (11). Demographics, vital signs, laboratory measures, medications, and other clinical data were collected. This project was approved by the Institutional Review Board of the Children's Hospital affiliated with the Zhejiang University School of Medicine. As data were de-identified and retrospective research had no impact on clinical treatment, the requirement for patient consent was waived.
Study population and data extraction
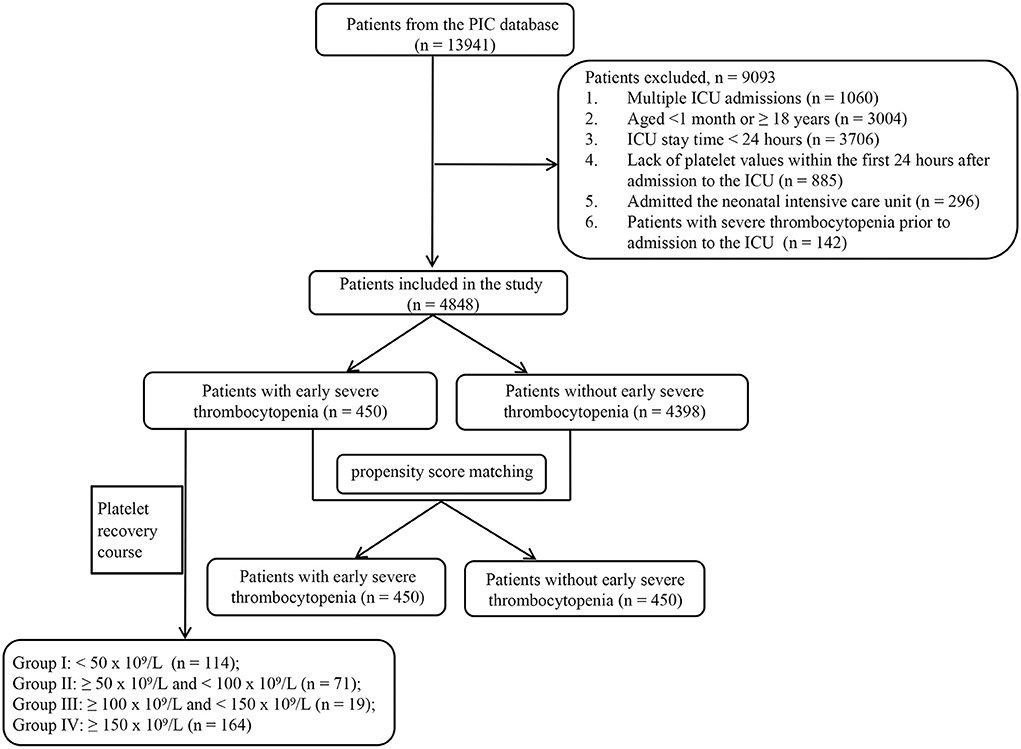
Only patients hospitalized for the first time were included in this study. The exclusion criteria were as follows: (1) age <1 month or ≥18 years; (2) time in the ICU of <24 h; (3) lack of data on platelet counts within the first 24 h after admission to the ICU; (4) admission to the neonatal ICU; and (5) severe thrombocytopenia prior to admission to the ICU. Early severe thrombocytopenia was defined as a platelet count of <50 × 109/L within the first 24 h of ICU admission. Patients with early thrombocytopenia who met one or more of the following criteria were included in the platelet course study: (1) patients whose maximum platelet count obtained within 72 h of ICU admission exceeded 150 × 109/L after the minimum platelet count appeared in the first 24 h; (2) patients who had at least one platelet record every 24 h within 72 h of ICU admission. The patient's maximal platelet count within 72 h of ICU admission after the minimum platelet count within the first 24 h was considered short-term platelet recovery. Figure 1 illustrates the screening procedure.
The primary outcome of this study was all-cause mortality during the hospital stay. The secondary outcome was the length of the ICU stay. Data were collected using the PostgreSQL 10 software, including age, sex, first care unit, primary diagnosis on ICU admission, laboratory results, and length of ICU stay.
Statistical analysis
Categorical variables were reported as numbers and percentages, and chi-square tests were used to assess differences between the groups. Continuous variables were reported as medians and interquartile distances, and Wilcoxon tests were used to assess differences between the groups. Stata software (version 14.0; Stata Corp., College Station, TX, USA) was used for all statistical analyses. P < 0.05 was considered statistically significant.
The primary diagnosis on ICU admission was extracted from the admission diagnosis according to the International Classification of Diseases 10 (ICD-10) code, and the underlying disease was determined if the patient was diagnosed with this disease category. A patient may have multiple diseases. Laboratory results were extracted from the worst results within 24 h after the patient entered the ICU.
To ensure the robustness of the study, propensity score matching (PSM) was used to adjust for age, sex, first care unit, and primary diagnosis on ICU admission. A 1:1 nearest-neighbor matching with a caliper width of 0 was applied for patients with early severe thrombocytopenia and without early severe thrombocytopenia. Univariate and multivariate logistic regression analyses were performed on the original and PSM cohorts, respectively. Results are presented as odds ratios (ORs) with 95% confidence intervals (95% CI).
In the study of the platelet course, patients were divided into four groups according to the short-term recovery of platelet counts (Group I: <50 × 109/L; Group II: ≥50 × 109/L and <100 × 109/L; Group III: ≥100 × 109/L and ≥150 × 109/L; Group IV: ≥150 × 109/L). A logistic regression analysis was performed to investigate the influence of varying degrees of recovery on in-hospital mortality in patients with early severe thrombocytopenia.
Results
Patient characteristics in the original cohort
The study included data from 4,848 critically ill children. Early severe thrombocytopenia occurred in 450 patients, with an incidence rate of 9.3%. Table 1 shows the baseline characteristics of patients with and without early severe thrombocytopenia in the original cohort. The number of patients with and without early severe thrombocytopenia was significantly different in the first care unit. Regarding the primary diagnosis upon ICU admission, we found that patients with early severe thrombocytopenia were more likely to develop neoplasms, diseases of the circulatory system, and sepsis compared to patients without early severe thrombocytopenia. In addition, patients with early severe thrombocytopenia showed a higher maximum value of pH, creatinine, serum potassium, prothrombin time, and partial prothrombin time, and exhibited lower minimum partial pressure of oxygen and white blood cells.
The in-hospital mortality rate of patients with early severe thrombocytopenia was 15.8%, which was significantly higher than that of patients without early severe thrombocytopenia (P <0.001). In addition, patients with early severe thrombocytopenia had significantly longer ICU stays than non-patients [5.73 (2.79–12.13) vs. 3.88 (1.96–7.92) days; P < 0.001].
Patient characteristics in the PSM cohort
Age, sex, primary care unit, and underlying conditions were considered in the PSM analysis. A total of 450 patients with early severe thrombocytopenia were matched with 450 patients without early severe thrombocytopenia. In the PSM cohort, patients with early severe thrombocytopenia had a higher in-hospital mortality rate than those without early severe thrombocytopenia (15.8% vs. 8.7%; P = 0.001). However, the length of ICU stay did not differ between the two groups (Table 1).
Early severe thrombocytopenia and in-hospital mortality
In the original cohort, using univariate logistic regression, early severe thrombocytopenia, sex, first care unit, neoplasms, diseases of the respiratory system, sepsis, maximum partial pressure of carbon dioxide, minimum partial pressure of oxygen, maximum value of potassium, maximum value of prothrombin time, and maximum value of partial prothrombin time were considered statistically significant. Multivariate logistic regression analysis demonstrated that early severe thrombocytopenia was an independent risk factor for in-hospital mortality (Table 2).
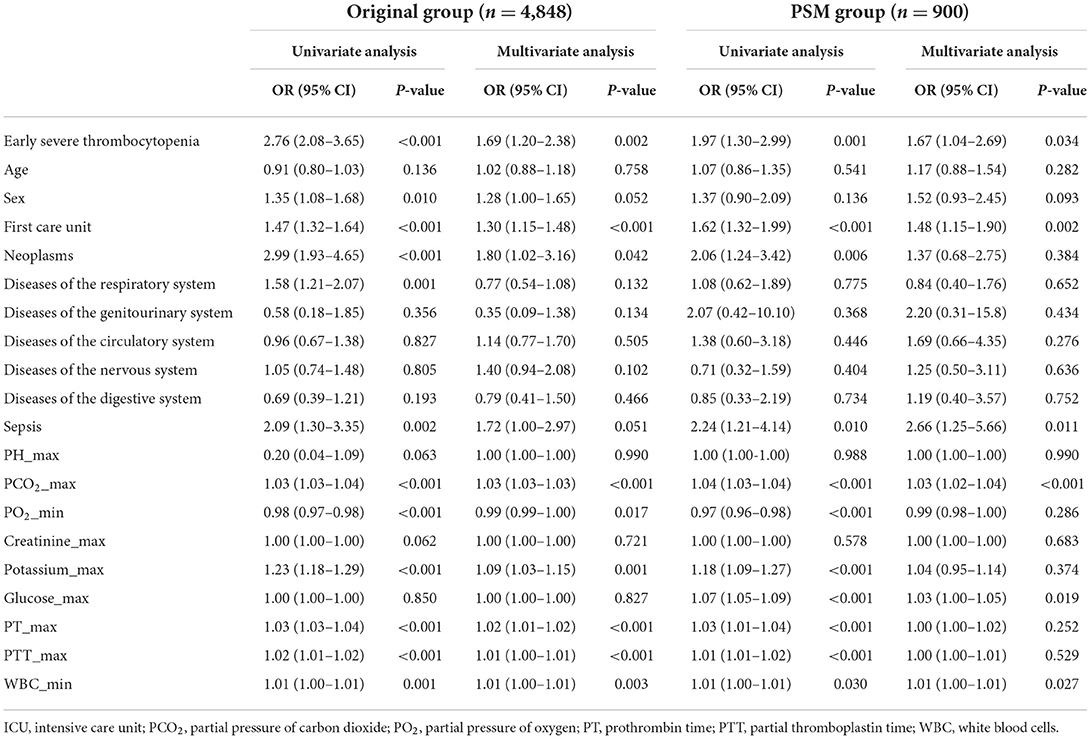
Table 2. Univariate and multivariate logistic regression analysis to assess the association between early severe thrombocytopenia and in-hospital mortality in original group and PSM group.
In the PSM cohort, univariate and multivariate logistic regression analyses demonstrated that early severe thrombocytopenia was an independent risk factor for in-hospital mortality (Table 2).
Platelet course and in-hospital mortality
Of the 450 patients with early severe thrombocytopenia in the original cohort, 368 were included in the platelet course study. A total of 114 patients (Group I) had a maximum platelet count of <50 × 109/L within 72 h of ICU admission after the appearance of the minimum platelet count in the first 24 h. In addition, the maximum platelet count increased to 50–99 × 109/L in 71 patients (Group II), 100–149 × 109/L in 19 patients (Group III), and ≥150 × 109/L in 164 patients (Group IV). Compared with Group I, the risk of in-hospital mortality was significantly lower in Group IV patients (OR, 0.301; 95% CI, 0.139–0.648; P = 0.002). Recovery of platelet count to normal levels in the short term is a protective factor for patient prognosis (Table 3).
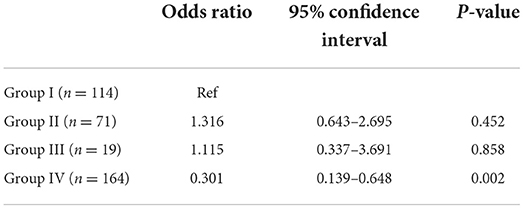
Table 3. Regression analysis based on platelet recovery to assess the association between platelet course and in-hospital mortality in critically ill children with early severe thrombocytopenia.
Discussion
Our study showed that severe thrombocytopenia is common in pediatric ICUs, with an early incidence of ~10%. Logistic regression analysis demonstrated that early severe thrombocytopenia was an independent risk factor for in-hospital mortality in critically ill children. In addition, we studied the platelet course and found that platelet count recovery to normal levels in the short term may indicate a favorable prognosis.
The occurrence of severe thrombocytopenia varies by ICU due to the varying vulnerability of various patients to thrombocytopenia. It occurs in ~20% of medical ICU patients (12) and almost 45% of trauma ICU patients (13). The prognostic relevance of severe thrombocytopenia, a typical indication for coagulopathy in critical care units, is inconclusive. Although many researchers feel that severe thrombocytopenia increases the probability of mortality (14, 15), others argue that early severe thrombocytopenia is a symptom of a more serious underlying cause and is not an independent prognostic factor (16). In this study, we not only showed that early severe thrombocytopenia increases the risk of in-hospital mortality but also discovered that the platelet course is important.
Krishnan et al. found higher mortality in critically ill children admitted to the hospital with thrombocytopenia in the pediatric ICUs (17). However, the number of cases included was small, and the number of deaths in the subgroup analysis was <10. This conclusion is supported by extensive research. Using a large sample of data from the PICU database, our study demonstrated this conclusion. At the subsequent follow-up of the platelet course, we discovered that 44.6% of patients with early severe thrombocytopenia reverted to normal platelet counts within 3 days and had lower in-hospital mortality than patients who retained severe thrombocytopenia. A delayed increase in platelet counts could indicate that underlying organ damage has not been addressed, which is typically caused by prolonged sepsis (18, 19). The management of critically ill patients is a race against time, and every delay in the disease necessitates clinical attention and, if necessary, reevaluation of the condition.
The strengths of our study include a large amount of study data on critically ill children and the platelet course follow-up. Our study has some limitations. First, this was a retrospective single-center study, with most patients from China, resulting in an unavoidable potential bias. Therefore, the findings of this study must be confirmed through a multi-center prospective study. Second, in the platelet course study, we only examined the prognosis of patients with early severe thrombocytopenia, which does not represent the entire PICU patient population. Third, data on patients' in-hospital procedures and some laboratory results (e.g., blood urea nitrogen) were missing from the database; therefore, severity scores could not be assessed. Similarly, treatment measures, such as patient blood transfusion and plasma exchange, cannot be obtained from the database. Therefore, studies of the platelet course are considered to report all-cause platelet recovery and need to be interpreted with caution.
Conclusions
Early severe thrombocytopenia is an independent risk factor for in-hospital mortality in critically ill children. Furthermore, in-hospital mortality was significantly reduced in children with early severe thrombocytopenia whose platelet count returned to normal levels in the short term.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics Statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent from the participants' legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author contributions
YL extracted and analyzed the research data. YL and CR wrote the first draft of the manuscript. HG participated in data analysis and review of the final manuscript. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Smyth SS, McEver RP, Weyrich AS, Morrell CN, Hoffman MR, Arepally GM, et al. Platelet functions beyond hemostasis. J Thromb Haemost. (2009) 7:1759–66. doi: 10.1111/j.1538-7836.2009.03586.x
2. Eicher JD, Lettre G, Johnson AD. The genetics of platelet count and volume in humans. Platelets. (2018) 29:125–30. doi: 10.1080/09537104.2017.1317732
3. Lee HS, Koh IH, Kim HS, Kwon YJ. Platelet and white blood cell count are independently associated with sarcopenia: a nationwide population-based study. Thromb Res. (2019) 183:36–44. doi: 10.1016/j.thromres.2019.09.007
4. Parrozzani R, Nacci EB, Bini S, Marchione G, Salvadori S, Nardo D, et al. Severe retinopathy of prematurity is associated with early post-natal low platelet count. Sci Rep. (2021) 11:891. doi: 10.1038/s41598-020-79535-0
5. Kasugai D, Ozaki M, Nishida K, Goto Y, Takahashi K, Matsui S, et al. Relative platelet reductions provide better pathophysiologic signatures of coagulopathies in sepsis. Sci Rep. (2021) 11:14033. doi: 10.1038/s41598-021-93635-5
6. Zhu Y, Zhang J, Li Y, Liu F, Zhou Q. Peng Z. Association between thrombocytopenia and 180-day prognosis of Covid-19 patients in intensive care units: a two-center observational study. PloS ONE. (2021) 16:e0248671. doi: 10.1371/journal.pone.0248671
7. Thachil J, Warkentin TE. How do we approach thrombocytopenia in critically ill patients? Br J Haematol. (2017) 177:27–38. doi: 10.1111/bjh.14482
8. Yuan S, Otrock ZK. Platelet transfusion: an update on indications and guidelines. Clin Lab Med. (2021) 41:621–34. doi: 10.1016/j.cll.2021.07.005
9. Zhou Z, Feng T, Xie Y, Zhang X, Du J, Tian R, et al. Prognosis and rescue therapy for sepsis-related severe thrombocytopenia in critically ill patients. Cytokine. (2020) 136:155227. doi: 10.1016/j.cyto.2020.155227
10. Ribeiro RP, Flor-De-Lima F, Soares H, Rocha G, Guimarães H. Prevalence, risk factors and predictors of severity of neonatal thrombocytopenia in neonatal intensive care units: a single center study. Minerva Pediatr. (2019). doi: 10.23736/S0026-4946.19.05542-7. [Epub ahead of print].
11. Zeng X, Yu G, Lu Y, Tan L, Wu X, Shi S., et al. Pic, a paediatric-specific intensive care database. Sci Data. (2020) 7:14. doi: 10.1038/s41597-020-0355-4
12. Crowther MA, Cook DJ, Meade MO, Griffith LE, Guyatt GH, Arnold DM, et al. Thrombocytopenia in medical-surgical critically ill patients: prevalence, incidence, and risk factors. J Crit Care. (2005) 20:348–53. doi: 10.1016/j.jcrc.2005.09.008
13. Hanes SD, Quarles DA, Boucher BA. Incidence and risk factors of thrombocytopenia in critically ill trauma patients. Ann Pharmacother. (1997) 31:285–9. doi: 10.1177/106002809703100302
14. Ito S, Taniguchi T, Shirai S, Ando K, Watanabe Y, Yamamoto M, et al. The impact of baseline thrombocytopenia on late bleeding and mortality after transcatheter aortic valve implantation (from the Japanese multicenter ocean-Tavi registry). Am J Cardiol. (2021) 141:86–92. doi: 10.1016/j.amjcard.2020.11.017
15. Sico JJ, Phipps MS, Concato J, Wells CK, Lo AC, Nadeau SE, et al. Thrombocytopenia and in-hospital mortality risk among ischemic stroke patients. J Stroke Cerebrovasc Dis. (2013) 22:e99–102. doi: 10.1016/j.jstrokecerebrovasdis.2012.08.005
16. Zhou D, Li Z, Wu L, Shi G, Zhou J. Thrombocytopenia and platelet course on hospital mortality in neurological intensive care unit: a retrospective observational study from large database. BMC Neurol. (2020) 20:220. doi: 10.1186/s12883-020-01794-1
17. Krishnan J, Morrison W, Simone S, Ackerman A. Implications of thrombocytopenia and platelet course on pediatric intensive care unit outcomes. Pediatr Crit Care Med. (2008) 9:502–5. doi: 10.1097/PCC.0b013e3181849af1
18. Xu Y, Jin D, Tong W, Duan Y. [Etiology and prognosis of thrombocytopenia in children: a case analysis in 683 children within 10 years of pediatric intensive care unit]. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. (2018) 30:968–72. doi: 10.3760/cma.j.issn.2095-4352.2018.010.013
19. Surti J, Jain I, Shah K, Mishra A, Kandre Y, Garg P, et al. Predictive efficacy of procalcitonin, platelets, and white blood cells for sepsis in pediatric patients undergoing cardiac surgeries who are admitted to intensive care units: single-center experience. Ann Pediatr Cardiol. (2018) 11:137–42. doi: 10.4103/apc.APC_36_17
Keywords: severe thrombocytopenia, platelet course, in-hospital mortality, critically ill children, Pediatric Intensive Care (PIC) database
Citation: Lu Y, Ren C and Guo H (2022) Association of early severe thrombocytopenia and platelet course with in-hospital mortality in critically ill children. Front. Pediatr. 10:922674. doi: 10.3389/fped.2022.922674
Received: 18 April 2022; Accepted: 11 July 2022;
Published: 02 August 2022.
Edited by:
Roberto Manuel Jabornisky, Universidad Nacional del Nordeste, ArgentinaReviewed by:
Phuc Huu Phan, Vietnam National Children's Hospital, VietnamTakanari Ikeyama, Aichi Child Health and Medical General Center, Japan
Copyright © 2022 Lu, Ren and Guo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yan Lu, bHV5YW4xMTIxOUBob3RtYWlsLmNvbQ==
 Yan Lu
Yan Lu Chaoxiang Ren
Chaoxiang Ren