- 1Institute for Maternal and Child Health IRCCS Burlo Garofolo, Trieste, Italy
- 2University of Trieste, Trieste, Italy
- 3Unit of Biostatistics, Department of Cardiac, Thoracic, Vascular Sciences and Public Health, University of Padova, Padua, Italy
Aim: Emergency cases are uncommon events in the pediatric emergency setting. This study aimed to evaluate the effect of the Coronavirus disease 2019 (COVID-19) pandemic by describing the number and type of pediatric emergency cases that arrived at the pediatric emergency department (PED) of a tertiary-level children’s hospital in Italy.
Methods: We performed a retrospective study, collecting the main features of pediatric emergency patients who arrived during the first year of the COVID-19 pandemic (March 2020–February 2021) compared to the pre-pandemic period (March 2016–February 2020).
Results: During the study period, 112,168 patients were visited at the PED, and 237 (0.21%) were emergency cases, median age of 4 years (IQR: 1–12). In the first year of the pandemic, 42 children were coded as emergency cases compared to 195 (49/year) during the pre-pandemic period. The proportion of emergency cases was stable (0.27% during the COVID-19 period versus 0.20% during the pre-COVID-19 period, p = 0.19). No differences were found regarding the age, gender, hour of arrival, and outcome of patients. We found a significant decrease in the proportion of emergency cases related to respiratory diseases (9/42, 21.4% during the COVID-19 period versus 83/195 during the pre-COVID-19 period (42.6%), p = 0.01).
Conclusion: In conclusion, our data suggest that the pandemic had a more significant impact on respiratory emergency cases than on pediatric emergencies in general.
Introduction
The triage process in emergency medicine allows a rapid and precise sorting of children who arrive at the hospital, assigning them to priority levels according to their medical needs.
Children and adolescents in critical conditions, and/or with compromised vital signs, needing immediate medical care or resuscitation maneuvers are assigned as pediatric emergency codes at triage.
Despite a natural variability among departments, pediatric cases triaged with the highest clinical priority code are relatively uncommon (1, 2). At our pediatric emergency department (PED), emergency cases represent less than 1% of visits (2).
Several reports highlighted a delay in the care in the early phase of the pandemic (3–5). Nevertheless, these data were not confirmed in all settings (6, 7). Moreover, most of the reports describing the influence of the Coronavirus disease 2019 (COVID-19) pandemic on PED visits referred only to the first few months of the pandemic (2, 6–8).
This study aimed to investigate the impact of the pandemic on pediatric emergency healthcare utilization at our Institution, comparing the rate and type of emergency cases during the first year of the COVID-19 pandemic to the previous years. Secondarily, we wanted to describe the main features of children and adolescents who arrived at the PED and received an emergency code at triage in the last 5 years.
Methods
We conducted a retrospective study on the clinical characteristics of children and adolescents who accessed the PED at the tertiary level, university teaching, children’s hospital, Institute for Maternal and Child Health, IRCCS Burlo Garofolo of Trieste, Italy, from March 1, 2016 to February 28, 2021, and who received an emergency code at triage.
Our Institution’s triage process was based on a four-priority level of increasing severity: white for non-urgent cases, green for minor urgency, yellow for urgent, and red for emergencies and resuscitation cases. We collected data about triage code classification for the five periods. Subsequently, we collected each record of patients assigned with an emergency code: the date and hour of the visit, demographical features of the patients, discharge diagnosis, admission status, and ward of destination of admitted subjects.
Discharge diagnoses were grouped into respiratory disease, neurologic disease, injury, psychiatric disease, cardiovascular disease, non-respiratory infections, intoxication, and others. Respiratory diseases included bronchiolitis, viral wheezing, asthma, pneumonia, and croup. Neurologic diseases included status epilepticus, seizures, encephalitis, and ischemic or hemorrhagic stroke. Injuries included amputations, partial amputations, burns, fractures, drawing, head, chest, or abdominal trauma. Psychiatric diseases included severe agitation/aggressiveness, testament, depression, conversion disorder, and anxiety disorder. Cardiovascular diseases included paroxysmal supraventricular tachycardia, heart failure, and cardiac arrest. Non-respiratory infections included urosepsis, sepsis, and gastroenteritis.
Ethics
The Institutional Review Board (IRB) of the Institute gave ethical approval to the study protocol (RC 10/2020). Due to the retrospective nature of the study, no specific written informed consent was administered.
Statistical Analysis
Data of enrolled children were summarized by descriptive analysis. Categorical variables were reported through absolute frequencies and percentages.
We divided the study cohort into a COVID-19 group and a pre-COVID-19 group. The pandemic group was defined as patients admitted during the first pandemic year (March 1, 2020–February 29, 2021) and the pre-pandemic group as patients admitted during the same time frames of the four previous years (March 1, 2016–February 28, 2020).
We classified patients by age as follows: neonates (0–28 days of life), infants (29 days–11 months), pre-school children (2–5 years), school children (6–12 years), and adolescents (13–17 years).
The chi-square test and Fisher’s Exact test were used to examine the variables of interest in the differences between the COVID-19 period and the pre-COVID-19 period. Data were entered into an Excel spreadsheet, and statistical analyses were performed using R software (version 4.0.3, 2020). Statistical significance was considered for p-values < 0.05 and all tests were 2-tailed.
Results
During the study period, a total of 112,168 patients were visited at the PED; 96,645 arrived, between March 2016 and February 2020, before the outbreak of the COVID-19 pandemic in Italy, and 15,523 during the first year of the pandemic, from March 2020 to February 2021. Two hundred thirty-seven (0.21%) received an emergency code at the nursing triage evaluation, 195 before the COVID-19 outbreak (pre-COVID-19 group), and 42 during the first year of the pandemic (COVID-19 group). In children classified as emergency cases, the median age was 4 years (interquartile range: 1–12), and 92 (40%) were female.
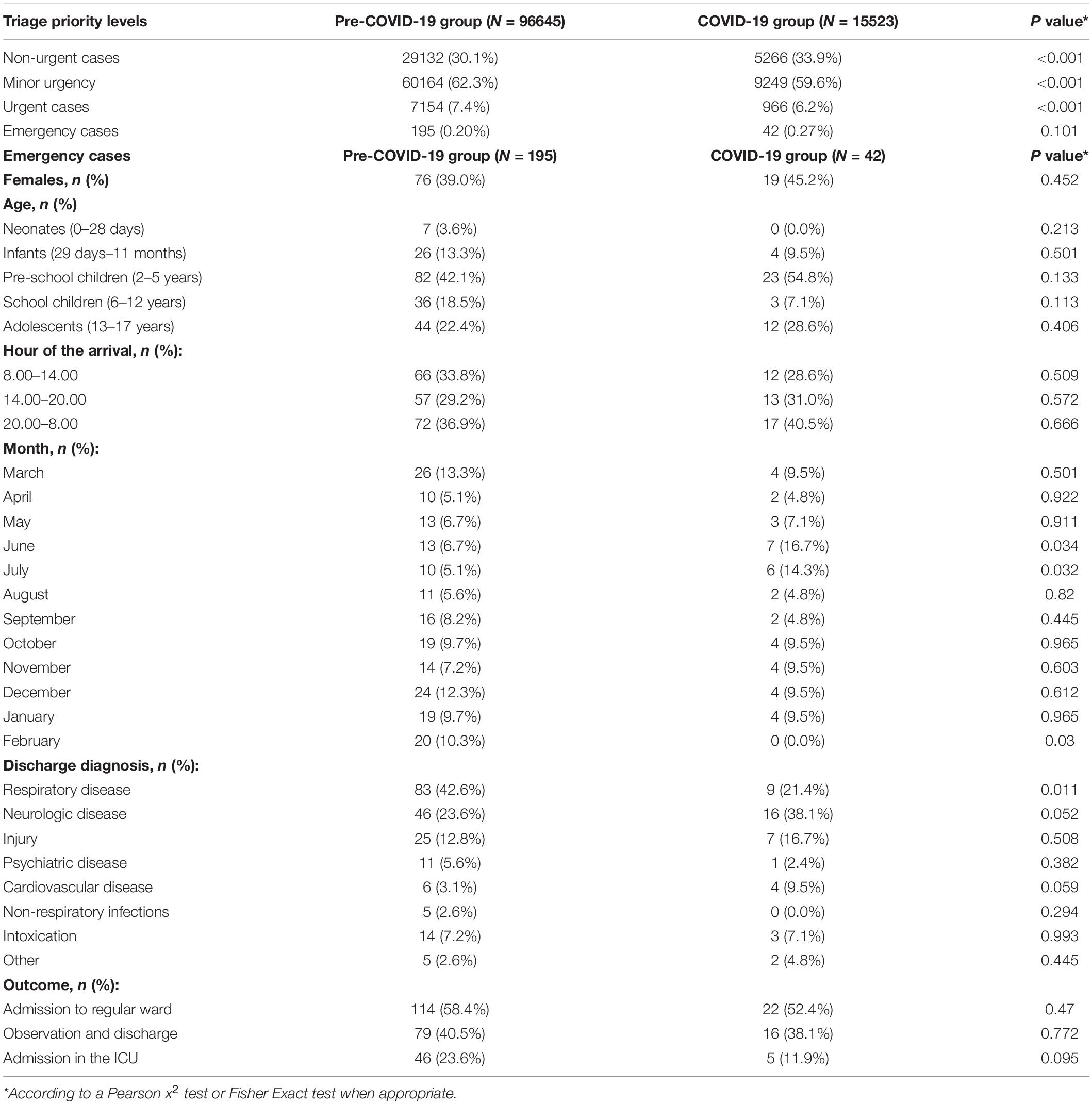
Table 1 describes the distribution of the emergency codes in the pre-COVID-19 group and COVID-19 group.
The rates of non-urgent, minor urgent, and urgent cases dropped (p < 0.001, Table 1). Nevertheless, the proportion of emergency cases remained substantially stable compared to the pre-pandemic period (0.27% vs. 0.20%, p = 0.103).
Among children classified as emergency cases, no statistically significant differences were found regarding the age, gender, and hour of the arrival of patients between the first year of the pandemic and the years before.
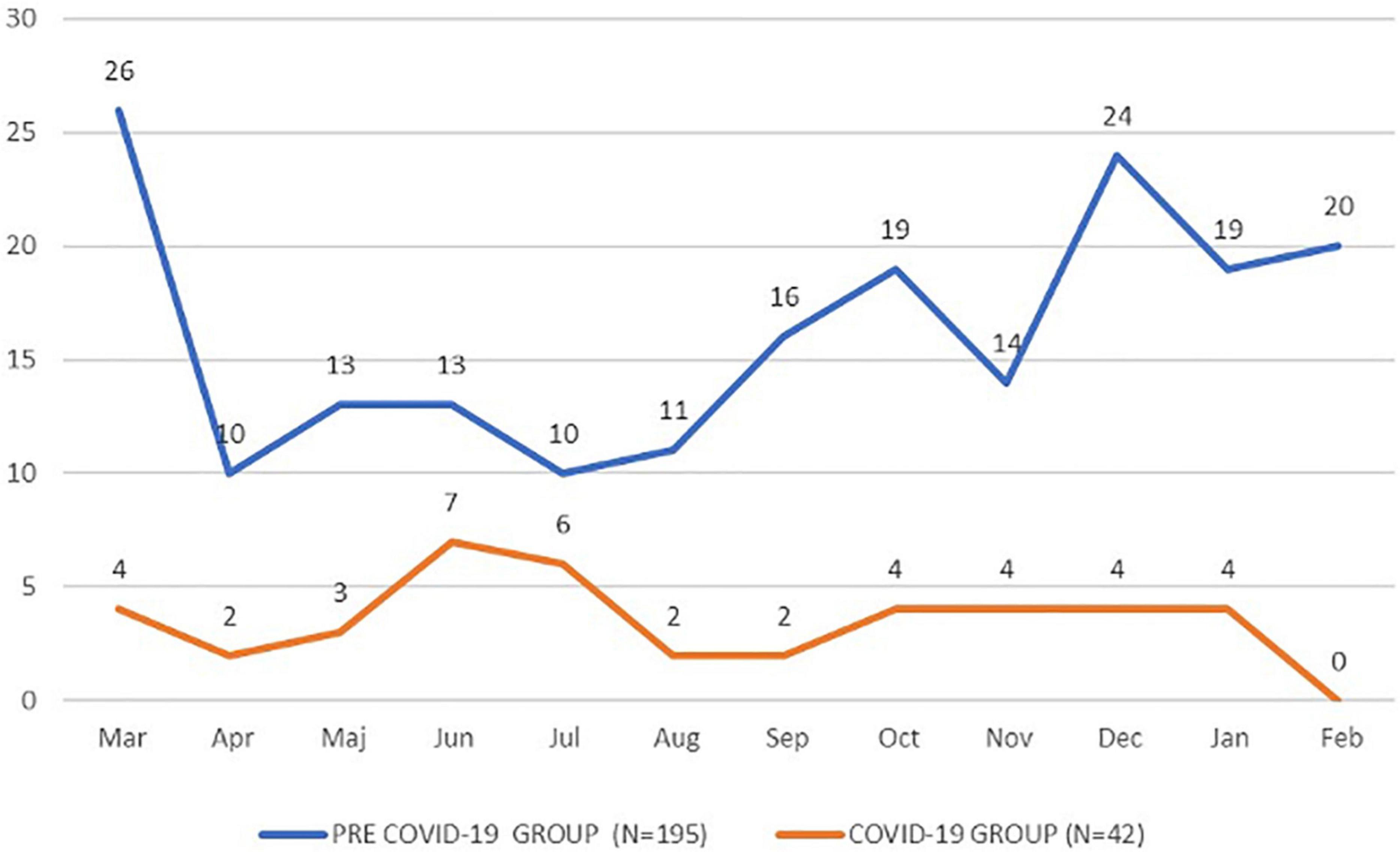
We noted a significantly different distribution in the month of the arrival of the emergency cases (Figure 1), with a significant drop in February (10.3% vs. 0.0%, p = 0.03) and a significant increase in June (6.7% vs. 16.7%, p = 0.03) and in July (5.1% vs. 14.3%, p = 0.03).
We experienced a statistically significant decrease in respiratory diseases during the first year of the pandemic compared to the pre-pandemic years (42.6% vs. 21.4%, p = 0.011).
Among the 237 emergency cases, 137 (57.80%) were admitted to regular wards and 51 (21.51%) to the intensive care unit (ICU). The proportion of patients admitted to the ICU halved during the pandemic year compared to the pre-pandemic period, but this difference was not statistically significant (11.9% vs. 23.6%, p = 0.095).
Discussion
The COVID-19 pandemic and the social measures to counteract its spread have considerably modified the epidemiology of PED cases worldwide (2, 5–11). Considering the first year of the pandemic, this study, performed from a tertiary-level children’s hospital perspective, revealed a drastic decrease in PED visits, 15,523 compared to almost 25/per year before the pandemic, and these data were in line with another report performed in the same period in New York City, United States (12). We described a substantially stable rate of emergency cases, associated with a great decrease in non-emergency cases. These data were similar to the experience in New York City (12). In Italy, COVID-19 began to spread in February 2020. We had a strict national lockdown from March to May 2020. Social distancing measures were suspended during the summer and reimposed from September 2020 until February 2021, without periods of strict lockdown. Previous studies already showed a decrease in the number of PED visits during the pandemic, more pronounced in the periods of strict lockdown (2, 5–8). Nevertheless, they did not focus specifically on pediatric emergency cases, so it was unclear if patients were not seen at the PED for the fear of contagion or because there had less severe diseases. Moreover, some reports highlighted a delay in the care during the very early phase of the pandemic in Italy (4). The value of this study was of focusing specifically on pediatric emergency cases during the entire first year of the pandemic. We did not observe a significant increase in the proportion of emergency cases at our PED, suggesting that there was no significant delay in the care of severe acute diseases, not confirming what was already reported in other settings (5, 13). Notably, we observed a significantly lower proportion of emergency cases related to respiratory diseases and a decreased percentage of children and adolescents needing admission to the ICU. This data was in line with previous studies showing the tremendous impact of the social distancing measures on the spread of respiratory infections (14–16) and suggested a role of these measures in the prevention of severe acute respiratory diseases. During the first year of the pandemic, we did not observe a significant change in the number of other causes of severe acute presentation, such as injuries, intoxication, and psychiatric disorders. Therefore, for these kinds of cases, we did not experience a measurable indirect influence of the social measures imposed to limit the spread of COVID-19. In this study, we described a considerable number of pediatric emergency cases with their main features, and this may be useful for readers interested in the characterization of these uncommon events. Some limitations need to be acknowledged: first, we had to rely on the triage codes assigned by different nurses, therefore, we cannot exclude operator variability. Besides, we focused only on emergencies. Therefore, we were not able to describe the variability of the type of accesses in general. A significant increase in severe PED accesses related to mental health problems was reported (17). Nevertheless commonly used triage tools tend to underestimate the urgency of psychiatric presentations (18). So, we cannot exclude that we have missed some severe psychiatric presentations. Secondly, due to the limited size of the samples, random fluctuations in data cannot be excluded. Third, our data referred to a PED of a single Institution, so the generalizability is limited; however, our hospital is the only pediatric hospital serving the whole area of the Trieste Province (about 230.000 inhabitants) for the pediatric population and this remained unchanged over the 5 years of the study. The triage classification did not change during the study period.
In conclusion, our data showed that during the first year of the COVID-19 pandemic, the proportion of emergency cases at a tertiary-level children’s hospital was stable despite a general reduction of visits to the PED.
Furthermore, we noted a significant decrease in the proportion of severe acute respiratory cases during the first year of the pandemic with a decreased percentage of ICU admissions.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Institutional Review Board of the Institute for Maternal and Child Health IRCCS Burlo Garofolo, Trieste, Italy. Written informed consent from the participants’ legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author Contributions
GC and EB designed the study. IM, SR, and VG collected the data. FG performed the statistical analysis and prepared the table. SR and VG drafted the initial version of the study. GC, EB, and AA critically reviewed the manuscript and developed the final version of the manuscript. All authors approved the final version of the manuscript and approved this submission.
Funding
This work was supported by the Ministry of Health, Rome, Italy, in collaboration with the Institute for Maternal and Child Health IRCCS Burlo Garofolo, Trieste, Italy.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We thank Martina Bradaschia for the English revision of the manuscript.
Abbreviations
PED, pediatric emergency department.
References
1. Zook HG, Kharbanda AB, Flood A, Harmon B, Puumala SE, Payne NR. Racial differences in pediatric emergency department triage scores. J Emerg Med. (2016) 50:720–7.
2. Cozzi G, Zanchi C, Giangreco M, Rabach I, Calligaris L, Giorgi R, et al. The impact of the COVID-19 lockdown in Italy on a pediatric emergency setting. Acta Paediatr. (2020) 109:2157–9.
3. Ma X, Liu Y, Du M, Ojo O, Huang L, Feng X, et al. The accuracy of the pediatric assessment triangle in assessing triage of critically ill patients in the emergency pediatric department. Int Emerg Nurs. (2021) 58:101041.
4. Lazzerini M, Barbi E, Apicella A, Marchetti F, Cardinale F, Trobia G. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc Health. (2020) 4:e10–11.
5. Lynn RM, Avis JL, Lenton S, Amin-Chowdhury Z, Ladhani SN. Delayed access to care and late presentations in children during the COVID-19 pandemic: a snapshot survey of 4075 p in the UK and Ireland. Arch Dis Child. (2021) 106:e8. doi: 10.1136/archdischild-2020-319848
6. Raucci U, Musolino AM, Di Lallo D, Piga S, Barbieri MA, Pisani M, et al. Impact of the COVID-19 pandemic on the emergency department of a tertiary children’s hospital. Ital J Pediatr. (2021) 47:21. doi: 10.1186/s13052-021-00976-y
7. Liguoro I, Pilotto C, Vergine M, Pusiol A, Vidal E, Cogo P. The impact of COVID-19 on a tertiary care pediatric emergency department. Eur J Pediatr. (2021) 180:1497–504. doi: 10.1007/s00431-020-03909-9
8. Sokoloff WC, Krief WI, Giusto KA, Mohaimin T, Murphy-Hockett C, Rocker J, et al. Pediatric emergency department utilization during the COVID-19 pandemic in New York city. Am J Emerg Med. (2021) 45:100–4. doi: 10.1016/j.ajem.2021.02.029
9. Head WT, Parrado RH, Cina RA. Impact of the coronavirus (COVID-19) pandemic on the care of pediatric acute appendicitis. Am Surg. (2021) 26:31348211067995. doi: 10.1177/00031348211067995
10. Barten DG, Latten GHP, van Osch FHM. Reduced emergency department utilization during the early phase of the COVID-19 pandemic: viral fear or lockdown effect. Dis Med Public Health Prep. (2020) 16:36–39. doi: 10.1017/dmp.2020.303
11. DeLaroche AM, Rodean J, Aronson PL, Fleegler EW, Florin TA, Goyal M, et al. Pediatric emergency department visits at us children’s hospitals during the COVID-19 pandemic. Pediatrics. (2021) 147:e2020039628.
12. Liang T, Chamdawala HS, Tay ET, Chao J, Waseem M, Lee H, et al. Pediatric emergency care in New York city during the COVID-19 pandemic shutdown and reopening periods. Am J Emerg Med. (2022) 56:137–44. doi: 10.1016/j.ajem.2022.03.049
13. Jafari K, Koves I, Rutman L, Brown JC. Impact of the COVID-19 pandemic on the severity of diabetic ketoacidosis presentations in a tertiary pediatric emergency department. Pediatr Qual Saf. (2022) 7:e502. doi: 10.1097/pq9.0000000000000502
14. Risso FM, Cozzi G, Volonnino M, Cossovel F, Ullmann N, Ciofi Degli Atti ML, et al. Social distancing during the COVID-19 pandemic resulted in a marked decrease in hospitalisations for bronchiolitis. Acta Paediatr. (2021) 11:163–4. doi: 10.1111/apa.16075
15. Cozzi G, Blasutig F, De Nardi L, Giangreco M, Barbi E, Amaddeo A, et al. The first winter of social distancing improved most of the health indexes in a paediatric emergency department. Acta Paediatr. (2022) 111:163–4. doi: 10.1111/apa.16271
16. Amaddeo A, Cason C, Cozzi G, Ronfani L, Comar M. Social distancing measures for COVID-19 are changing winter season. Arch Dis Child. (2021) 106:e47. doi: 10.1136/archdischild-2021-322004
17. Bruns N, Willemsen L, Stang A, Kowall B, Holtkamp K, Kamp O, et al. Pediatric intensive care unit admissions after adolescent suicide attemps during the pandemic. Pediatrics. (2022). doi: 10.1542/peds.2021-055973 [Epub ahead of print].
Keywords: children, adolescents, emergencies, emergency department, COVID-19, pandemic
Citation: Cozzi G, Molina Ruiz I, Giudici F, Romano S, Grigoletto V, Barbi E and Amaddeo A (2022) Pediatric Emergency Cases in the First Year of the COVID-19 Pandemic in a Tertiary-Level Emergency Setting. Front. Pediatr. 10:918286. doi: 10.3389/fped.2022.918286
Received: 12 April 2022; Accepted: 31 May 2022;
Published: 30 June 2022.
Edited by:
Enrico Vidal, University of Udine, ItalyReviewed by:
Ilaria Liguoro, University of Udine, ItalyAlexis Rybak, Assistance Publique – Hôpitaux de Paris, France
Copyright © 2022 Cozzi, Molina Ruiz, Giudici, Romano, Grigoletto, Barbi and Amaddeo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Giorgio Cozzi, giorgio.cozzi@burlo.trieste.it
 Giorgio Cozzi
Giorgio Cozzi