
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Pediatr., 04 October 2022
Sec. Pediatric Cardiology
Volume 10 - 2022 | https://doi.org/10.3389/fped.2022.915045
This article is part of the Research TopicInsights in Pediatric Cardiology: 2021View all 17 articles
Background: Meta-analysis of the impact on clinical outcome from transcatheter closure of Fontan fenestration.
Methods: Cochrane, Embase, MEDLINE, and Open-Gray were searched. Parameters such as changes in oxygen saturation, cavo-pulmonary pressure, maximum heart rate during exercise, exercise duration, and oxygen saturation after fenestration closure were pooled and statistical analysis performed.
Results: Among 922 publications, 12 retrospective observational studies were included. The included studies involved 610 patients, of which 552 patients (90.5%) had a fenestration. Of those patients, 505 patients (91.5%) underwent attempt at trans-catheter closure. When it could be estimated, the pooled overall mean age at trans-catheter fenestration closure was 6.6 ± 7.4 years, and the mean follow-up time was 34.4 ± 10.7 months. There were 32 minor (6.3%) and 20 major (4.0%) complications during or after trans-catheter Fontan fenestration closure. The forest plots demonstrate that following fenestration closure, there was a significant increase in the mean arterial oxygen saturation of 7.9% (95% CI 6.4–9.4%, p < 0.01). There was also a significant increase in the mean cavo-pulmonary pressure of 1.4 mmHg (95% CI 1.0–1.8 mmHg, p < 0.01) following fenestration closure. The exercise parameters reported in 3 studies also favored closing the fenestration as well, yet the exercise duration increase of 1.7 min (95% CI 0.7–2.8 min, p < 0.01) after fenestration closure is probably clinically insignificant.
Conclusion: Late closure of a Fontan fenestration has the impact of improving resting oxygen saturation, exercise oxygen saturation, and a modest improvement of exercise duration. These clinical benefits, however, may be at the expense of tolerating slightly higher cavo-pulmonary mean pressures.
In the 50 years following the introduction of the procedure named after Francis Fontan (1), the indications as well as the surgical techniques have substantially evolved. The Fontan operation, which may be performed with various surgical techniques, is the final stage of surgical palliation for functionally univentricular hearts (1–20). A surgically created fenestration (or connection) between the Fontan circuit and the atrial cavity to reduce excessively elevated systemic venous pressures and to improve cardiac output by increasing the filling of the single ventricle may be beneficial in the immediate post-operative period (21–24). To date, the only available prospective randomized study examining the impact of Fontan fenestration demonstrated a reduction in hospital and intensive care unit length of stays with a fenestration (25), even if other studies reported data on this issue (26–28). These potential benefits, however, may be realized at the expense of lower systemic oxygenation, an increased risk of systemic embolism, and the possible need for catheter-based fenestration closure later in life (29, 30).
The long-term management of Fontan fenestrations remains controversial. First, catheter-based Fontan fenestration closure is not without risk, and the concerns related to a closed or absent fenestration are still present long after the postoperative period. Second, long-term systemic thromboembolic risk with an open fenestration has to be balanced against the Fontan paradox of relative systemic venous hypertension and pulmonary arterial hypotension. Third, after Fontan failure develops, the gold standard of treatment is heart transplant. As donor hearts for transplantation remain a scarce resource, other palliative strategies including trans-catheter Fontan fenestration enlargement or creation have been attempted. These attempts were made to improve quality of life, reduce failure symptoms, and possibly improve waitlist safety.
Unfortunately, the overwhelming majority of published literature examining outcomes after transcatheter closure of Fontan fenestrations are observational in nature and underpowered to detect important differences. Heterogenous indications between centers and unclear indications within centers, prevent concrete conclusions of management of the Fontan fenestration in the catheterization lab. To address these limitations, the present systematic review and meta-analysis was conducted to assess the consequences of trans-catheter Fontan fenestration closure on clinical outcomes.
This analysis was registered on Prospero (CRD42019139395) on August 21st, 2019. The study was conducted in accordance with the Meta-Analysis of Observational Studies in Epidemiology Guidelines (31). The manuscript was structured in accordance with Systematic Reviews and Meta-Analyses (PRISMA) guidelines and recommendations (32). All reviewed literature was assessed using the Cochrane tools, which cover six domains of bias: selection bias, performance bias, detection bias, attrition bias, reporting bias, and other bias (33). The PICO question for this systematic review and meta-analysis is in fenestrated Fontan patients, what is the change in clinical outcomes from baseline or fenestrations that are left open associated with transcatheter fenestration closure?
A systematic search was conducted on Cochrane, Embase and MEDLINE. Search terms are provided in Figure 1. Moreover, to avoid losing any related publications, an Open-Gray search was conducted. Related journals and reference lists of identified articles were cross-checked for other relevant studies of interest. Retrospective and prospective observational or randomized controlled trials from the year 200, written in English, reporting the pre-determined outcomes including children or adults undergoing catheter-based intervention on a Fontan fenestration in human subjects were included. Exclusion criteria were case reports, non-original articles, systematic reviews, meta-analyses, non-published works, studies not describing any of the pre-determined outcome measures, or studies that included > 20% of spontaneous fenestration closures. The search was conducted with the assistance of two experienced librarians.
Two independent reviewers (Z.N.L. and A.F.C.) screened all identified studies. In case of multiple publications with sample overlap, the most recent report was included. In each article, the criteria for inclusion and exclusion were independently evaluated by the two reviewers to verify the correctness of selection. In the case of disagreement between reviewers, a consensus was agreed upon. In multiple studies with overlapping study populations, the study with the greatest overall follow-up was included. The first author and/or the corresponding author of three of the included studies were contacted to clarify reported data, particularly regarding the size of the fenestration at the time of surgery.
Study design, year of Fontan surgery, surgical type of Fontan, fenestration use, and clinical follow-up were documented. The baseline demographics were extracted from the individual studies. The outcomes extracted included early or late mortality, Fontan takedown, heart transplantation, stroke, thromboembolism, or peri-interventional complications. Per-interventional changes in vital signs and changes in hemodynamic parameters including cardiac index, exercise duration, minute ventilation, maximal oxygen consumption, peak exercise oxygen pulse, and ventilatory anaerobic threshold were extracted. Additional clinical outcomes of interest, including protein-losing enteropathy, plastic bronchitis, and arrhythmias were similarly recorded. Complications were deemed major if the grade was > 2 or minor if the grade was ≤ 2 on the Clavien-Dindo classification system (34).
A meta-analysis was performed to compare the outcomes before and after catheter-based Fontan fenestration closure. Outcomes were compared before and after fenestration enlargement or creation for Fontan failure. The mean differences and the corresponding 95% confidence intervals (CI) were estimated using a random effects meta-analysis model, which accounts for variability induced by between-study heterogeneity. Cochran’s Q statistic and I2 index was used to quantify and test heterogeneity between studies (35). All statistical analyses were performed using R software version 3.6.3 (36) and the meta-package (37). Probabilities with P-value < 0.05 were considered statistically significant, and all statistical tests were two-sided.
A complete literature search resulted in 922 candidate publications, of which 263 were removed as duplicates. Of the remaining 659 articles, 389 were excluded due to irrelevance. Of the remaining 151 studies, 12 articles met final inclusion criteria (Figure 2). References are represented together with the baseline characteristics of all individual studies. Of the included studies, only 1 study (8%) included all of their Fontan patients done at their center. The rest of the studies used a selected cohort of their overall Fontan population to describe in their study. The included studies involved 610 patients, of which 552 patients (90.5%) had a fenestration. Of those patients, 505 patients (91.5%) underwent attempt at trans-catheter closure.
When it could be estimated, the pooled overall mean age at trans-catheter fenestration closure was 6.6 ± 7.4 years, and the mean follow-up time was 34.4 ± 10.7 months (Table 1). There were 32 minor (6.3%) and 20 major (4.0%) complications during or after trans-catheter Fontan fenestration closure. The 3 most common minor complications were 10 patients (2.0%) who needed new medications for a diagnosis of heart failure, 8 patients (1.6%) with an arrhythmia, and 4 patients (0.8%) with a vascular access site bleed. The 3 most common major complications were 6 patients (1.2%) who needed device retrieval for failure or malposition, 2 long-term mortalities (0.4%), and 1 early death (0.2%). Forest plots were constructed containing the individual and pooled mean differences for the oxygen saturation, cavo-pulmonary pressure, maximum heart rate during exercise, and exercise duration and oxygen saturation after fenestration closure are presented in Figures 3A–E. The forest plots demonstrate that following fenestration closure, there was a significant increase in the mean arterial oxygen saturation of 7.9% (95% CI 6.4–9.4%, p < 0.01) (Figure 3A). There was also a significant increase in the mean cavo-pulmonary pressure of 1.4 mmHg (95% CI 1.0–1.8 mmHg, p < 0.01) (Figure 3B) following fenestration closure. The exercise parameters reported in 3 studies also favored closing the fenestration as well (Figures 3C–E), yet the exercise duration increase of 1.7 min (95% CI 0.7–2.8 min, p < 0.01) (Figure 3D) after fenestration closure is probably clinically insignificant.
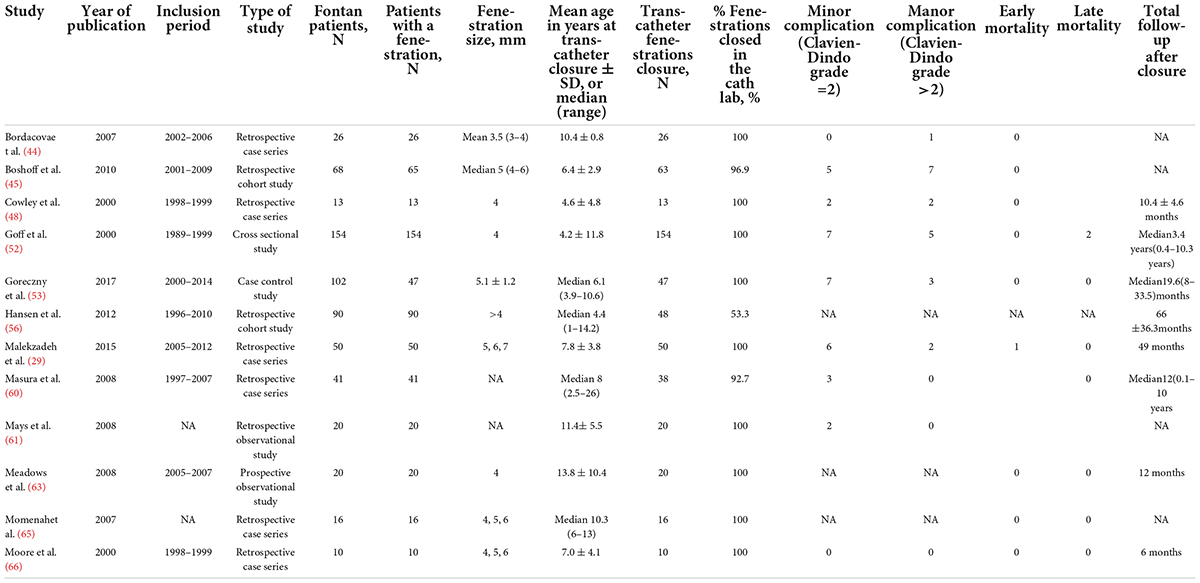
Table 1. Patients who underwent late closure of the fenestration (> 30 days after Fontan procedure).
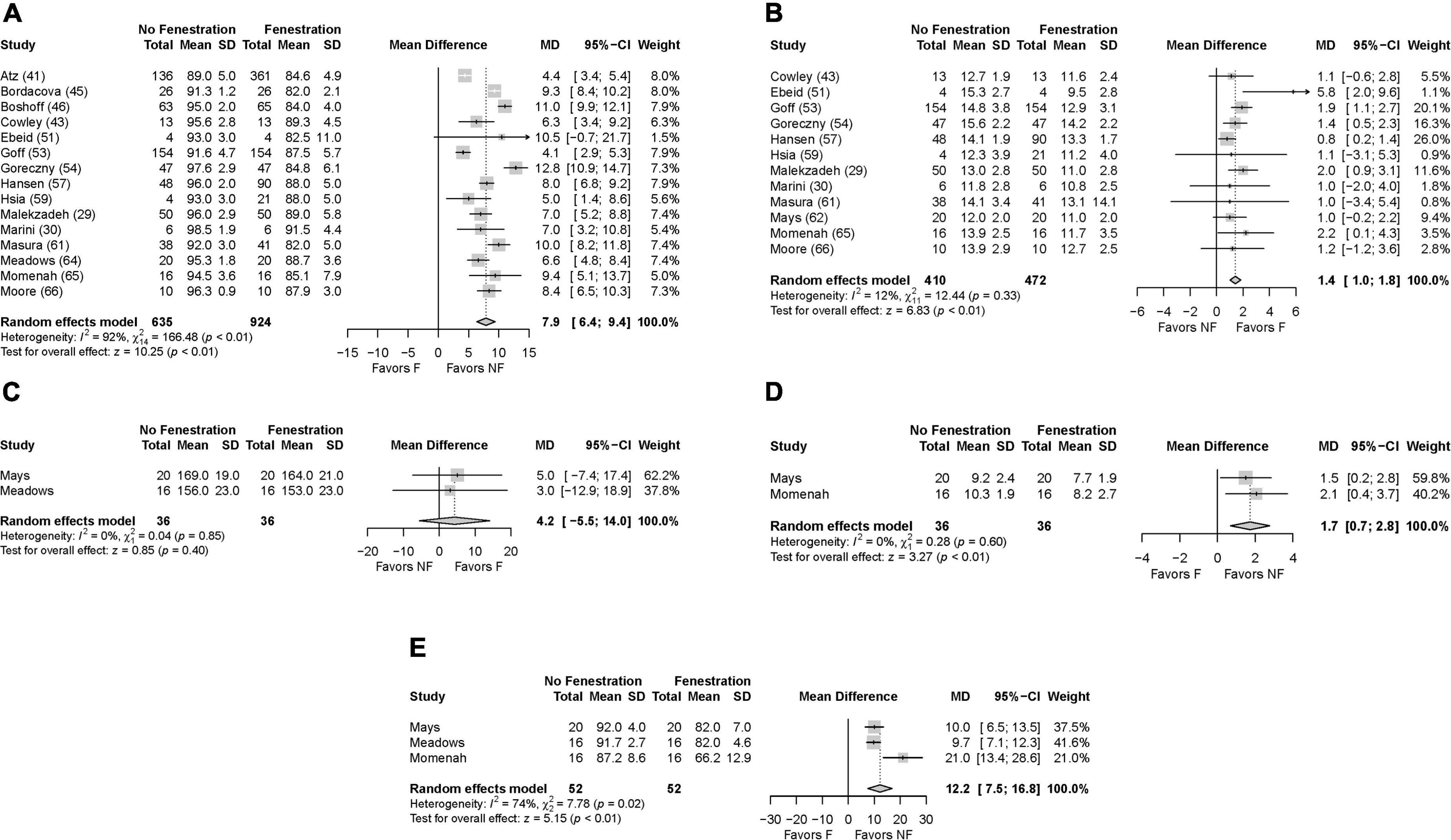
Figure 3. Forest plots after closure of the fenestration. (A) Oxygen saturation, (B) pulmonary artery pressure, (C) exercise heart rate, (D) exercise duration, (E) exercise oxygen saturation.
The present systematic review and meta-analysis suggests that trans-catheter closure of a Fontan fenestration is associated with improved resting and exercise oxygenation, lower maximal heart rate during exercise, and longer exercise duration (Figures 3A,C–E), even if this is at the expense of slightly higher pulmonary artery mean pressures (Figure 3B). This analysis demonstrates that the immediate results of Fontan fenestration closure are fairly consistent. There is a systemic oxygen saturation mean increase of 7.9% (range 4.1–12.8%, Figure 3A). The pulmonary pressure slightly increases by 1.4 mm Hg (range 0.8–5.8 mm Hg, Figure 3B). Exercise tolerance does increase, but this length is short and was only tested in 2 studies (Figure 3C).
A fenestration eases the transition to the Fontan circulation for patients by providing a consistent source of systemic ventricular preload. Secondary benefits include decreased postoperative pleural effusions and hospital length of stay (25, 38). Fenestrating most Fontans has become commonplace in the modern era of Fontan management.
There is no concrete guidance on what should be done for the fenestration over the medium or the long-term. Because of this, there is dramatic heterogeneity fenestration management amongst centers. Because of the theoretic risk of thromboembolism and detrimental effects of prolonged cyanosis, some centers routinely close all fenestrations in the catheterization lab at about 12 months postoperatively (39). Patients who had spontaneous closure of their fenestration probably did so because of low trans-pulmonary pressures and resultant minimal relative flow across their fenestrations. This patient population, who can make up to about 40% of fenestrated Fontan patients, represent a low risk for Fontan failure (40). The long-term answer surrounding the question of what to do for the other 60% of patients was not clear. A persistent fenestration may be a surrogate for physiologic intolerance of the Fontan circulation, and this difference may not be readily apparent by pre-Fontan hemodynamic parameters (41–75). This has led some centers to either shift from routine closure to not closing any fenestrations (76) or to be very selective in which patients are referred for transcatheter closure (54, 62). For instance, McCrossan and Walsh (62). Will refer patients for trans-catheter Fontan fenestration closure if there is persistent hypoxia, satisfactory ventricular function, and absence of significant Fontan circuit obstruction.
After the patient is referred to the catheterization lab, the interventional cardiologist may find that the patient is not appropriate for closure. Many centers use the parameters set forth by the group at Boston Children’s Hospital in 1995 (77). At the time of catheterization and after measuring baseline features, the fenestration is then test occluded for 10 min. If the right atrial pressure exceeded 18 mmHg, or the arteriovenous difference in oxygen saturation increased by > 33%, or the right atrial saturation was < 40%, then the patient was considered to have an unfavorable response to test occlusion ad the fenestration was left open. Similarly, Goreczny et al. will do the 10-min test occlusion and will avoid permanent fenestration closure if the systemic venous pressure is above 18 mmHg or if there is an increase of 5 mmHg after balloon occlusion (53). At the Children’s Hospital of Michigan closure is deferred after balloon occlusion if the Fontan pressure is ≥ 20 mmHg, the Fontan pressure increases by 4 mmHg or more, if there is a decrease in cardiac output by ≥ 50%, or a decrease in systemic oxygen transport of ≥ 46% (78).
These strict criteria during test occlusion may identify patients that would not tolerate fenestration closure, but it may be that this provocative measure is sensitive but not specific for those patients that may not have the proper hemodynamics but would tolerate closure anyway. Ozawa et al. studied the long-term outcomes after fenestration closure in patients at risk for Fontan failure. They compared high-risk Fontan patients, as defined by pre-Fontan mean pulmonary arterial pressure ≥ 15 mmHg or systemic atrio-ventricular valve regurgitation ≥ moderate, compared to a standard risk group and a group whose fenestration had closed spontaneously. Protein-losing enteropathy-free survival rates did not differ between groups (p = 0.72). This was at the expense, in the high-risk group, of persistent cyanosis from veno-venous collaterals and lower peak oxygen consumption (p = 0.019) and lower anaerobic threshold (p = 0.023) compared to the standard risk group (79).
Exercise capacity as described by maximal oxygen consumption (VO2 max) has found diametrically opposite conclusions in certain reports. Mays et al. investigated 20 patients before and after Fontan fenestration closure. In their analysis, the VO2 max increased to 1.24 ± 0.35 L/min from 1.18 ± 0.46 L/min, p < 0.005 (61). Conversely, Meadows and colleagues also investigated 20 patients before and after fenestration closure. In this series, the percent predicted VO2 max increased to 74 ± 18.6% from 70.9 ± 18.6%, P = NS. In both studies, there was a wide variation in patient age and size (63). To take into account growth-related changes between pre- and post-fenestration closure exercise tests, different measurement endpoints were considered. Such differences may explain why exercise capacity was statistically significant in one study but not the other. Another potential explanation may be a combination of competing interests. One would surmise that increasing systemic arterial saturation would improve VO2 max and exercise duration, but this increase in systemic arterial saturation was at the expense of cardiac index and mixed venous oxygen saturation. Furthermore, neither study was able to define the amount of right to left shunting under exercise conditions. In his series Meadows stated that, at rest in the catheterization lab, all patients had no more than trivial shunting at the end of the catheterization, but that does not exclude the possibility that more significant shunting could have occurred with effort (63). The cardiopulmonary response to exercise in the Fontan circulation is complicated by an inability to regulate heart rate or stroke volume in response to exercise, systemic venous flow dynamics, and the compound contribution of ventilation on the Fontan circuit.
As stated earlier, the Fontan fenestration is associated with well documented early postoperative benefits. Studies identifying long-term benefits are sparse. Atz et al. showed a significant increase in the rate of fenestration across multiple centers between 1987 and 2002. After adjusting for era, patient age, and year of Fontan, this large, multi-center cross-sectional study found few associations between a persistent fenestration and negative long-term outcomes (40). There was a greater number of non-fenestrations associated catheter re-interventions, most commonly for coiling of systemic venous and aorticopulmonary collaterals. Unsurprisingly, the resting oxygen saturation was lower with a fenestration in the long-term, but they found no difference in the number of long-term re-interventions, incidence of protein-losing enteropathy or arrhythmias. The Australian and New Zealand Fontan registry has been a wealth of knowledge in understanding the Fontan outcomes in the modern era (80). In a propensity score-matched analysis they demonstrated that there was no difference in long-term survival (87% vs. 90% at 20 years; p = 0.16) or freedom from failure (73% vs. 80% at 20 years; p = 0.10) between patients with and without fenestration, respectively. There was more freedom from thromboembolism in the non-fenestrated vs. the fenestrated group (89% vs. 84%; p = 0.03) (80). On the other hand, in the study from Children’s Hospital of Michigan, the incidence of a composite outcome of death, transplant, deteriorated heart failure, plastic bronchitis, or protein-losing enteropathy was significantly higher when there was an open fenestration (60% vs. 6%; p < 0.01) (78). As mentioned earlier the patients with the open fenestration in this study were a select group of patients who failed to meet proper hemodynamics with test occlusion which may be the difference in the findings between these studies (78).
The present review and meta-analysis have select limitations. First, a large number of published articles reported incomplete data. For instance, no suitable data were reported to analyze the impact of complications after closure of the fenestration, such as stroke and/or systemic thrombo-embolism, as well as the occurrence of liver failure due to the increased systemic venous pressure. We therefore limited our presentation of the results to the most relevant information in regard to the long-term outcome of fenestration. Second, data extracted from observational study designs should be interpreted with caution due to the inherent limitations of confounding and a high degree of selection bias. Most importantly, select studies on the management of Fontan fenestration in patients with failed Fontan circulation had inadequate statistical analyses, which limited the ability to rigorously assess this fundamental question in the present analysis. Third, the first two limits are the consequence of the considerable controversy and widely varying institutional practices concerning Fontan fenestrations in respect to indication for establishment as well as management during long-term follow-up.
Late closure of a Fontan fenestration has the impact of improving resting oxygen saturation, exercise oxygen saturation, and a modest improvement of exercise duration. These clinical benefits, however, may be at the expense of tolerating slightly higher cavo-pulmonary mean pressures. There is a substantial lack of high-quality evidence supporting any therapeutic decision regarding Fontan fenestration, and this is reflected in the difficulties encountered in our literature review and meta-analysis.
The original contributions presented in this study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
All authors contributed to the idea and design of the study, preparation, review and approval of the manuscript.
We would like to acknowledge Coral Pepper, librarian at the University Hospitals of Leicester, and Keith Nockels, librarian at the University of Leicester, for their highly professional help in the preparation of the protocols, and their help in running the search on Cochrane, Embase and Medline.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2022.915045/full#supplementary-material
1. Fontan F, Baudet E. Surgical repair of tricuspid atresia. Thorax. (1971) 26:240–8. doi: 10.1136/thx.26.3.240
2. Choussat A, Fontan F, Besse P, Vallot F, Chauve A, Bricaud H. Selection criteria for Fontan’s procedure. In: Anderson RH, Shinebourne EA editors. Paediatric Cardiology. Edinburgh: Churchill Livingstone (1977). p. 559–66.
3. Corno AF, Becker AE, Bulterijs AHK, Lam J, Nijveld A, Schuller JL, et al. Univentricular heart: can we alter the natural history? Ann Thorac Surg. (1982) 34:716–26. doi: 10.1016/S0003-4975(10)60917-4
4. Fontan F, Kirklin JW, Fernandez G, Costa F, Naftel DC, Tritto F, et al. Outcome after a “perfect” Fontan operation. Circulation. (1990) 81:1520–36. doi: 10.1161/01.CIR.81.5.1520
5. Gewillig M, Brown SC. The Fontan circulation after 45 years: update in physiology. Heart. (2016) 102:1081–6. doi: 10.1136/heartjnl-2015-307467
6. Kreutzer GO, Galindez E, Bono H, de Palma C, Laura JP. An operation for the correction of tricuspid atresia. J Thorac Cardiovasc Surg. (1973) 66:613–21. doi: 10.1016/S0022-5223(19)40598-9
7. Yacoub MH, Radle-Smith R. Use of a valved conduit from right atrium to pulmonary artery for “correction” of a single ventricle. Circulation. (1976) 54:III63–70.
8. Lee CN, Schaff HV, Danielson GK, Puga FJ, Driscoll DJ. Comparison of atriopulmonary versus atrioventricular connections for modified Fontan/Kreutzer repair of tricuspid valve atresia. J Thorac Cardiovasc Surg. (1986) 92:1038–43. doi: 10.1016/S0022-5223(19)35820-9
9. Bjork VO, Olin CL, Bjarke BB, Thoren CA. Right atrial-right ventricular anastomosis for correction of tricuspid atresia. J Thorac Cardiovasc Surg. (1979) 77:452–8. doi: 10.1016/S0022-5223(19)40916-1
10. Coles JG, Leung M, Kielmanowicz S, Freedom RM, Benson LN, Rabinovitch M, et al. Repair of tricuspid atresia: utility of right ventricular incorporation. Ann Thorac Surg. (1988) 45:384–9. doi: 10.1016/S0003-4975(98)90010-8
11. Ilbawi MN, Idriss FS, DeLeon SY, Kucich VA, Muster AJ, Paul MH, et al. When should the hypoplastic right ventricle be used in a Fontan operation? An experimental and clinical correlation. Ann Thorac Surg. (1989) 47:533–8. doi: 10.1016/0003-4975(89)90428-1
12. de Leval MR, Kilner P, Gewillig M, Bull C. Total cavopulmonary connection: a logical alternative to atriopulmonary connection for complex Fontan operations. J Thorac Cardiovasc Surg. (1988) 96:682–95. doi: 10.1016/S0022-5223(19)35174-8
13. Jonas RA, Castaneda AR. Total cavo-pulmonary connection. J Thorac Cardiovasc Surg. (1988) 96:830. doi: 10.1016/S0022-5223(19)35196-7
14. Marcelletti C, Corno AF, Giannico S, Marino B. Inferior vena cava to pulmonary artery extracardiac conduit: a new form of right heart bypass. J Thorac Cardiovasc Surg. (1990) 100:228–32. doi: 10.1016/S0022-5223(19)35562-X
15. Giannico S, Corno AF, Marino B, Cicini MP, Gagliardi MG, Amodeo A, et al. Total extracardiac right heart bypass. Circulation. (1992) 86(Suppl.):II110–7.
16. Corno AF, Horisberger J, Jegger D, von Segesser LK. Right atrial surgery with unsnared inferior vena cava. Eur J Cardiothorac Surg. (2004) 26:219–20. doi: 10.1016/j.ejcts.2004.03.023
17. Nakano T, Kado H, Ishikawa S, Shiokawa Y, Ushinohama H, Sagawa K, et al. Midterm surgical results of total cavopulmonary connection: clinical advantages of the extracardiac conduit method. J Thorac Cardiovasc Surg. (2004) 127:730–7. doi: 10.1016/S0022-5223(03)01184-X
18. Yetman AT, Drummond-Webb J, Fiser WP, Schmitz ML, Imamura M, Ullah S, et al. The extracardiac Fontan procedure without cardiopulmonary bypass technique and intermediate-term results. Ann Thorac Surg. (2002) 74:S1416–21. doi: 10.1016/S0003-4975(02)03922-X
19. Klima U, Peters T, Peuster M, Hausdorf G, Haverich A. A novel technique for establishing total cavopulmonary connection: from surgical preconditioning to interventional completion. J Thorac Cardiovasc Surg. (2000) 120:1007–9. doi: 10.1067/mtc.2000.107824
20. Prabhu S, Maiya S, Shetty R, Murthy K, Ramachandra P, Karl TR. Improved technique for interventional extracardiac Fontan. World J Pediatr Congenit Heart Surg. (2020) 11:488–92. doi: 10.1177/2150135120918541
21. Laks H, Pearl JM, Haas GS, Drinkwater DC, Milgalter E, Jarmakani JM, et al. Partial Fontan: advantages of an adjustable interatrial communication. Ann Thorac Surg. (1991) 52:1084–94. doi: 10.1016/0003-4975(91)91286-5
22. Bridges ND, Lock JE, Castaneda AR. Baffle fenestration with subsequent catheter closure: modification of the Fontan operation for patients with increased risk. Circulation. (1990) 82:1681–9. doi: 10.1161/01.CIR.82.5.1681
23. Do-Nguyen CC, Kilcoyne MF, Gray P, Jonas RA. The evolution of surgical technique of the fenestrated Fontan procedure. J Card Surg. (2020) 35:1407–9. doi: 10.1111/jocs.14617
24. Guariento A, Pradegan N, Castaldi B, Cattapan C, Weixler V, Blitzer D, et al. Modified extracardiac Fontan with a fenestrated pericardial patch. J Card Surg. (2020) 35:1618–20. doi: 10.1111/jocs.14595
25. Lemler MS, Scott WA, Leonard SR, Stromberg D, Ramaciotti C. Fenestration improves clinical outcome of the Fontan procedure: a prospective randomized study. Circulation. (2002) 105:207-12. doi: 10.1161/hc0202.102237
26. Salazar JD, Zafar F, Siddiqui K, Coleman RD, Morales DLS, Heinle JS, et al. Fenestration during Fontan palliation: now the exception instead of the rule. J Thorac Cardiovasc Surg. (2010) 140:129–36. doi: 10.1016/j.jtcvs.2010.03.013
27. Li D, Li M, Zhou X, An Q. Comparison of the fenestrated and non-fenestrated Fontan procedures. A meta-analysis. Medicine. (2019) 98:29–39. doi: 10.1097/MD.0000000000016554
28. Bouhout I, Ben-Ali W, Khalaf D, Raboisson MJ, Poirier N. Effect of fenestration on Fontan procedure outcomes: a meta-analysis and review. Ann Thorac Surg. (2020) 109:1467–74. doi: 10.1016/j.athoracsur.2019.12.020
29. Malekzadeh-Milani S, Ladouceur M, Bajolle F, Bonnet D, Boudjemline Y. Closure of Fontan fenestration with the use of covered stents: short- and mid-term results in a cohort of 50 patients. Cardiol Young. (2015) 25:868–73. doi: 10.1017/S1047951114000894
30. Marini D, Boudjemline Y, Agnoletti G. Closure of extracardiac Fontan fenestration by using the covered Cheatham platinum stent. Cath Cardiovasc Int. (2007) 69:1003–6. doi: 10.1002/ccd.20664
31. Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA. (2000) 283:2008–12. doi: 10.1001/jama.283.15.2008
32. Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. Br Med J. (2015) 350:g7647. doi: 10.1136/bmj.g7647
33. Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomized trials. Br Med J. (2011) 343:d5928. doi: 10.1136/bmj.d5928
34. Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. (2009) 250:187–96. doi: 10.1097/SLA.0b013e3181b13ca2
35. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. Br Med J. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
36. R Core Team. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing, Vienna, Austria. Vienna: R Core Team (2021).
37. Balduzzi S, Rücker G, Schwarzer G. How to perform a meta-analysis with R: a practical tutorial. Evid Based Ment Health. (2019) 22:153–60. doi: 10.1136/ebmental-2019-300117
38. Anderson PAW, Sleeper LA, Mahony L, Colan SD, Atz AM, Breitbart RE, et al. Contemporary outcomes after the Fontan procedure: a Pediatric Heart Network multicenter study. J Am Coll Cardiol. (2008) 52:85–98. doi: 10.1016/j.jacc.2008.01.074
39. Webb MK, Hunter LE, Kremer TR, Huddleston CB, Fiore AC, Danon S, et al. Extracardiac Fontan fenestration device closure with Amplatzer vascular plug II and septal occlude: procedure results and medium-term follow-up. Pediatr Cardiol. (2020) 41:703–8. doi: 10.1007/s00246-019-02283-0
40. Atz AM, Travison TG, McCrindle BW, Mahony L, Quartermain M, Williams RV, et al. Late status of Fontan patients with persistent surgical fenestration. J Am Coll Cardiol. (2011) 57:2437–43. doi: 10.1016/j.jacc.2011.01.031
41. Al-Hay AAA, Shaban LA, Al-Qbandi M, Al-Anbaei M. Occlusion of Fontan fenestration using Amplatzer septal occluder. Int J Cardiovasc Imaging. (2011) 27:483–90. doi: 10.1007/s10554-010-9694-0
42. Apostolopoulou SC, Laskari CV, Kiaffas M, Papagiannis J, Rammos S. Diverse experience with CardioSEAL and STARFlex septal occluders. Cardiol Young. (2004) 14:367–72. doi: 10.1017/S1047951104004032
43. Azakie A, McCrindle BW, Benson LN, Van Arsdell GS, Russell J, Coles JG, et al. Total cavopulmonary connection in children with a previous Norwood procedure. Ann Thorac Surg. (2001) 71:1541–6. doi: 10.1016/S0003-4975(01)02465-1
44. Bordacova L, Kaldararova M, Masura TP. Experiences with fenestration closure in patients after the Fontan operation. Bratisl Lek Listy. (2007) 108:344–7.
45. Boshoff DE, Brown SC, DeGiovanni J, Stumper O, Wright J, Mertens L, et al. Percutaneous management of a Fontan fenestration: in search of the ideal restriction/occlusion device. Cath Cardiovasc Interv. (2010) 75:60–5. doi: 10.1002/ccd.22275
46. Bradley TJ, Human DG, Culham JAG, Duncan WJ, Patterson MWH, LeBlanc JG, et al. Clipped tube fenestration after extracardiac Fontan allow for simple transcatheter coil occlusion. Ann Thorac Surg. (2003) 76:1923–8. doi: 10.1016/S0003-4975(03)01192-5
47. Brown JW, Ruzmetov M, Dsechner BW, Rodefeld MD, Turrentine MW. Lateral tunnel Fontan in the current era: is it still a good option? Ann Thorac Surg. (2010) 89:556–63. doi: 10.1016/j.athoracsur.2009.10.050
48. Cowley CG, Badran S, Gaffney D, Rocchini AP, Lloyd TR. Transcatheter closure of Fontan fenestrations using the Amplatzer septal occlude: initial experience and follow-up. Cath Cardiovasc Int. (2000) 51:301–4. doi: 10.1002/1522-726X(200011)51:3<301::AID-CCD12>3.0.CO;2-G
49. Day RW, Denton DM, Jackson WD. Growth of children with a functionally sungke ventricle following palliation at moderately increased altitude. Cardiol Young. (2000) 10:193–200. doi: 10.1017/S1047951100009100
50. Ebeid MR, Mehta I, Gaymes CH. Closure of external tunnel Fontan fenestration: a novel use of the Amplatzer vascular plug. Pediatr Cardiol. (2009) 30:15–9. doi: 10.1007/s00246-008-9268-2
51. Franco E, Balbacid Domingo EJ, Arreo del Val V, Guereta da Silva LG, del Cerro Marin MJ, Fernandez Ruiz A, et al. Percutaneous interventions in Fontan circulation. IJC Heart Vasculature. (2015) 8:138–46. doi: 10.1016/j.ijcha.2015.06.008
52. Goff DA, Blume ED, Gauvreau K, Mayer JE, Lock JE, Jenkins KJ. Clinical outcome of fenestrated Fontan patients after closure. The first 10 years. Circulation. (2000) 102:2094–9. doi: 10.1161/01.CIR.102.17.2094
53. Goreczny S, Dryzek P, Morgan GJ, Mazurek-Kula A, Moll JJ, Moll JA, et al. Fenestration closure with Amplatzer duct occlude II in patients after total cavo-pulmonary connection. Arch Med Sci. (2017) 13:337–45. doi: 10.5114/aoms.2016.61836
54. Gorla SR, Jhingoeri NK, Chakraborty A, Raja KR, Garg A, Sandhu S, et al. Incidence and factors influencing the spontaneous closure of Fontan fenestration. Congenit Heart Dis. (2018) 13:776–81. doi: 10.1111/chd.12652
55. Hannah RL, Zabinsky JA, Salvaggio JL, Rossi AF, Khan DM, Alonso FA, et al. The Fontan operation: the pursuit of associated lesions and cumulative trauma. Pediatr Cardiol. (2011) 32:778–84. doi: 10.1007/s00246-011-9973-0
56. Hansen JH, Runge U, Uebing A, Scheewe J, Kramer HH, Fischer G. Cardiac catheterization and interventional procedures as part of staged surgical palliation for hypoplastic left heart syndrome. Congenit Heart Dis. (2012) 7:565–74. doi: 10.1111/j.1747-0803.2012.00709.x
57. Hosein RBM, Clarke AJB, McGuirk SP, Griselli M, Stumper O, DeGiovanni J, et al. Factors influencing early and late outcome following the Fontan procedure in the current era. The “Two commandments”? Eur J Cardiothorac Surg. (2007) 31:344–52. doi: 10.1016/j.ejcts.2006.11.043
58. Hsia TY, Khambadkone S, Redington AN, de Leval MR. Effect of fenestration on the sub-diaphragmatic venous hemodynamics in the total cavo-pulmonary connection. Eur J Cardiothorac Surg. (2001) 19:785–92. doi: 10.1016/S1010-7940(01)00705-9
59. Kim SH, Kang IS, Huh J, Lee HJ, Yang JH, Jun TG. Transcatheter closure of fenestration with detachable coils after the Fontan operation. J Korean Med Sci. (2006) 21:859–64. doi: 10.3346/jkms.2006.21.5.859
60. Masura J, Borodacova L, Tittel P, Berden P, Podnar T. percutaneous management of cyanosis in Fontan patients using Amplatzer occluders. Cath Cardiovasc Interv. (2008) 71:843–9. doi: 10.1002/ccd.21540
61. Mays WA, Border WL, Knecht SK, Gerdes YM, Pfriem H, Claytor RP, et al. Exercise capacity improves after transcatheter closure of the Fontan fenestration in children. Congenit Heart Dis. (2008) 3:254–61. doi: 10.1111/j.1747-0803.2008.00199.x
62. McCrossan BA, Walsh KP. Fontan fenestration closure with Amplatzer duct occlude II device. Cath Cardiovasc Interv. (2015) 85:837–41. doi: 10.1002/ccd.25770
63. Meadows J, Lang P, Marx G, Rhodes J. Fontan fenestration closure has no acute effect on exercise capacity but improves ventilatory response to exercise. J Am Coll Cardiol. (2008) 52:108–13. doi: 10.1016/j.jacc.2007.12.063
64. Momenah TS, Eltayb H, El Oakley R, Al Qethamy H, Al Faraidi Y. Effects of transcatheter closure of Fontan fenestration on exercise tolerance. Pediatr Cardiol. (2008) 29:585–8. doi: 10.1007/s00246-007-9154-3
65. Moore JW, Murdison KA, Baffa GM, Kashow K, Murphy JD. Transcatheter closure of fenestration and excluded hepatic veins after Fontan: versatility of the Amplatzer device. Am Heart J. (2000) 140:534–40. doi: 10.1067/mhj.2000.108517
66. Reinhardt Z, de Giovanni J, Stickley J, Bhole V, Anderson B, Murtuza B, et al. Catheter interventions in the staged management of hypoplastic left heart syndrome. Cardiol Young. (2014) 24:212–9. doi: 10.1017/S1047951113000024
67. Sfyridis PG, Lytrivi ID, Avramidis DP, Zavaropoulos PN, Kirvassilis GV, Papagiannis JK, et al. The Fontan procedure in Greece: early surgical results and excellent mid-term outcome. Hellenic J Cardiol. (2010) 51:323–9.
68. Stamm C, Friehs I, Duebener LF, Zurakowski D, Mayer JE, Jonas RA, et al. Improving results of the modified Fontan operation in patients with heterotaxy syndrome. Ann Thorac Surg. (2002) 74:1967–78. doi: 10.1016/S0003-4975(02)04124-3
69. Aldoss O, Divekar A. Modified technique to create Diabolo stent configuration. Pediatr Cardiol. (2016) 37:728–33. doi: 10.1007/s00246-015-1339-6
70. Bar-Cohen Y, Perry SB, Keane JF, Lock JE. Use of stent to maintain atrial defects and Fontan fenestrations in congenital heartv disease. J Interven Cardiol. (2005) 18:11–8. doi: 10.1111/j.1540-8183.2005.04049.x
71. Hirsch JC, Goldberg C, Bove EL, Salehian S, Lee T, Ohye RG, et al. Fontan operation in the current era. A 15-year single institution experience. Ann Surg. (2008) 248:52–60. doi: 10.1097/SLA.0b013e3181858286
72. Petko M, Myung RJ, Wernovsky G, Cohen MI, Rychik J, Nicolson SC, et al. Surgical reinterventions following the Fontan procedure. Eur J Cardiothorac Surg. (2003) 24:255–9. doi: 10.1016/S1010-7940(03)00257-4
73. Quandt D, Ramchandani B, Bhole V, Penford G, Mehta C, Dhillon R, et al. Initial experience with the Cook Formula balloon expandable stent in congenital heart disease. Cath Cardiovasc Interv. (2015) 85:259–66. doi: 10.1002/ccd.25543
74. Rupp S, Schieke C, Kerst G, Mazhari N, Moysich H, Latus H, et al. Creation of a transcatheter fenestration in children with failure of Fontan circulation: focus on extra cardiac conduit connection. Cath Cardiovasc Interv. (2015) 86:1189–94. doi: 10.1002/ccd.26042
75. Vyas H, Driscoll DJ, Cabalka AK, Cetta F, Hagler DJ. Results of transcatheter Fontan fenestration to treat protein-losing enteropathy. Cath Cardiovasc Interv. (2007) 69:584–9. doi: 10.1002/ccd.21045
76. Imielski BR, Woods RK, Mussatto KA, Cao Y, Simpson PM, Tweddell JS, et al. Fontan fenestration closure and event-free survival. J Thorac Cardiovasc Surg. (2013) 145:183–7. doi: 10.1016/j.jtcvs.2012.09.006
77. Bridges ND, Lock JE, Mayer JE, Burnett J, Castaneda AR. Cardiac catheterization and test occlusion of the interatrial communication after the fenestrated Fontan operation. J Am Coll Cardiol. (1995) 25:1712–7. doi: 10.1016/0735-1097(95)00055-9
78. Kawasaki Y, Sasaki T, Forbes TJ, Ross RD, Kobayashi D. Optimal criteria for transcatheter closure of Fontan fenestration: a single-center experience with a review of literature. Heart Vessels. (2021) 36:1246–55. doi: 10.1007/s00380-021-01798-y
79. Ozawa H, Hoashi T, Ohuchi H, Kurosaki K, Ichikawa H. Long-term outcomes after fenestration closure in high-risk Fontan candidates. Pediatr Cardiol. (2021) 42:1356–64. doi: 10.1007/s00246-021-02619-9
Keywords: congenital heart defects, congenital heart surgery, fenestration, Fontan circulation, meta-analysis, systematic literature review, univentricular hearts
Citation: Greenleaf CE, Lim ZN, Li W, LaPar DJ, Salazar JD and Corno AF (2022) Impact on clinical outcomes from transcatheter closure of the Fontan fenestration: A systematic review and meta-analysis. Front. Pediatr. 10:915045. doi: 10.3389/fped.2022.915045
Received: 07 April 2022; Accepted: 26 August 2022;
Published: 04 October 2022.
Edited by:
Christian Apitz, Ulm University Medical Center, GermanyReviewed by:
Rachael Cordina, Sydney Local Health District, AustraliaCopyright © 2022 Greenleaf, Lim, Li, LaPar, Salazar and Corno. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Antonio F. Corno, YW50b25pby5mLmNvcm5vQHV0aC50bWMuZWR1; orcid.org/0000-0003-4374-0992
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.