- Department of Pediatric Intensive Care Unit, The First Hospital of Jilin University, Changchun, China
Objective: Survivors of critical illness may experience short- and long-term physical function impairments. This review aimed to identify the risk factors for physical function impairments from the current literature.
Data Sources: A systematic search of the PubMed, Embase, Web of Science, and Cochrane Library databases following the Preferred Reporting Items for Systematic Reviews and Meta-analyses extension for Scoping Reviews guideline was performed.
Study Selection: The risk factors reported in all human studies reporting physical function impairments in children admitted to the pediatric intensive care unit (PICU) were reviewed and categorized. Two investigators independently screened, evaluated, and selected studies for inclusion. Data from eligible studies were extracted by one investigator, and another investigator reviewed and verified the data. A systematic narrative approach was employed to review and summarize the data.
Results: A total of 264 studies were found to be eligible, with 19 studies meeting the inclusion criteria. Children admitted to the PICU experienced physical function impairments during their stay, which can last for years. The studies varied primarily in the measurement timing and tools used. The most frequently reported risk factors for physical function impairments were age, race or ethnicity, a pre-admission chronic condition, sex, disease severity, duration or the presence of mechanical ventilation, and admission diagnosis.
Conclusions: Physical function impairments may be persistent in PICU survivors. To prevent these impairments in critically ill patients, pediatricians should pay attention to modifiable risk factors, such as the duration of mechanical ventilation. Future studies need to promote a combination of standardized measures for the detection and prevention of physical function impairments.
Introduction
A widespread range of temporary or long-term impairments can develop during and after stay in an intensive care unit (ICU) (1). Impairments refer to new or worsened physical function, mental health, or cognitive function, and they are known as postintensive care syndrome (PICS) (1, 2). PICS is a new term introduced in 2010, and there is still no clear operational definition, pathophysiology, or specific blood or radiologic tests to diagnose it (3, 4). Nevertheless, more physical and psychological problems following ICU discharge have been reported due to the increased survival rate.
Over the past decades, physical impairments seem to outlast neuropsychologic impairments, and they lead to limitations in activities of daily living, fatigue, weakness, pain, and delayed return to work (5–7). For instance, limitations in global muscle strength, called ICU-acquired weakness (ICUAW), have now been widely studied in adults, and it is likely a primary cause of significant financial, social, and medical burden to ICU survivors and their families (8–10). Although PICS has been well-conceptualized in adults, little is known about PICS in children. To systematically identify PICS in children, the PICS in pediatrics (PICS-p) framework was developed in 2018 (11). Similar to adults, children admitted to the pediatric intensive care unit (PICU) are at risk for long-term morbidities, including physical function impairments and ongoing morbidity following discharge even if the child had been previously healthy (12–14). A prior cohort study found that PICU survivors had a high physical impairment rate of 85.1% at discharge and a high rate of 55.7% at 6 months following hospital discharge (15). A poor level of physical function may have a substantial impact on both future health and developmental trajectories (11, 16, 17). It is important to identify the risk factors for physical function impairments and optimize preventative action to reduce their incidence and promote recovery.
To more efficiently manage physical function impairments in PICU survivors, a clearer understanding of the risk factors is needed. This review aimed to summarize the risk factors for physical function impairments during hospitalization or post-PICU/hospital discharge. In addition, it can provide a basis for the development of relevant interventions.
Materials and Methods
Study Design
This was a systematic review to identify the risk factors for physical function impairments. A comprehensive study protocol was recommended by the Preferred Reporting Items for Systematic Reviews and Meta-analyses extension for Scoping Reviews guidelines (18). This protocol is provided as Supplementary Material 1.
Inclusion and Exclusion Criteria
Inclusion Criteria
- Patients: PICU survivors (<18 years old).
- Exposures: Risk factors for physical function impairments.
- Comparators: No physical function impairments risk factors.
- Outcomes: Any assessment method of physical function impairments.
- Study design: Cohort, case–control, and cross-sectional studies.
- Journal articles published in English from the earliest database records to October 2021.
Exclusion Criteria
- Studies conducted in neonatal ICUs.
- Reviews, qualitative research (e.g., letters to the editor, editorials, and study protocols), and studies that had not been peer-reviewed (e.g., published abstracts, conference proceedings, or dissertations).
- Full texts were retrieved, and articles not meeting this definition of physical function (e.g., endocrine and cardiac function).
- Studies that did not assess the risk factors for physical function impairments as an outcome variable.
- Multidimensional measures of “quality of life (QoL),” which cover a variety of physical and psychosocial outcomes.
Search Strategy and Selection
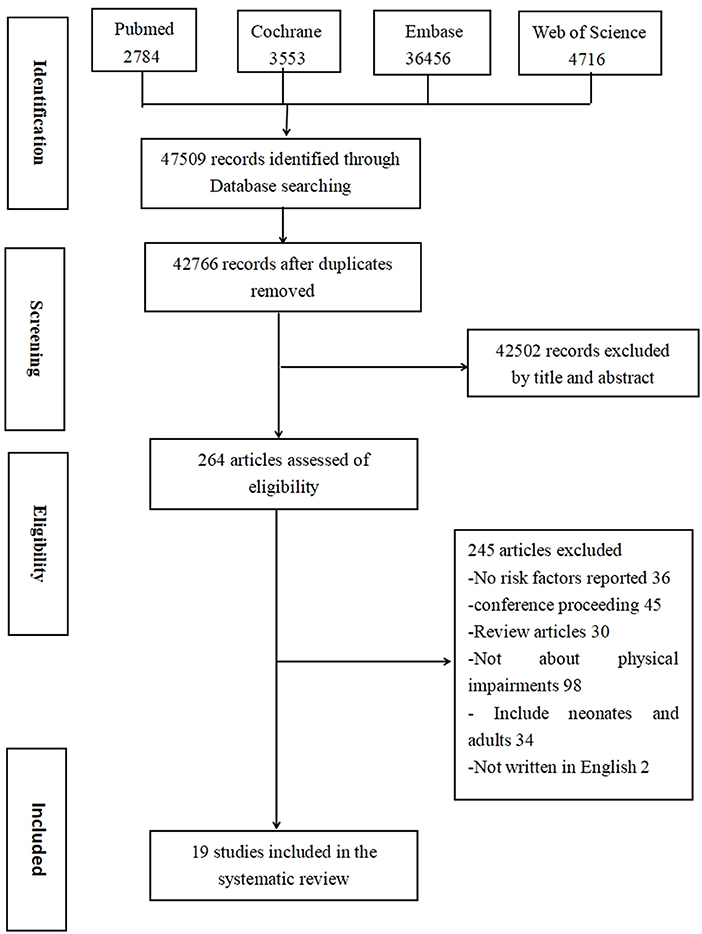
The literature search and selection process was performed based on the Preferred Reporting Items for Systematic Reviews and Meta-analyses flow diagram. The following literature databases were searched: PubMed, Embase, Web of Science, and Cochrane Library. A combination of MeSH terms and keywords was used for the search, and the detailed search strategy is provided in Supplementary Material 2. Two of the authors (MD and CY) reviewed all the identified records and conducted the entire process independently. They discussed all disagreements throughout the process until a consensus was reached.
Data Extraction and Analyses
Data were extracted using a structured form designed by the authors. The following characteristics were extracted and collected from the 19 included studies: author, publication year, country, study design, study subjects, sample size, selection criteria (length of ICU stay), sex and mean age of participants, measurement tools, timing and number of measurements, participants' diseases, and risk factors for physical function impairments. Data were independently extracted by two researchers (MD and CY) and entered into an Excel spreadsheet after a third researcher (YL) confirmed agreement. Due to the heterogeneity of the studies, no statistical synthesis was conducted, and a narrative approach was employed instead to interpret the literature.
Results
Study Selection
The screening and selection process is presented in Figure 1. A total of 47,509 articles were screened, and 42,766 articles were identified after eliminating duplicates. After researchers reviewed the title, abstract, and full text, 19 studies were selected for final inclusion.
Study and Sample Characteristics
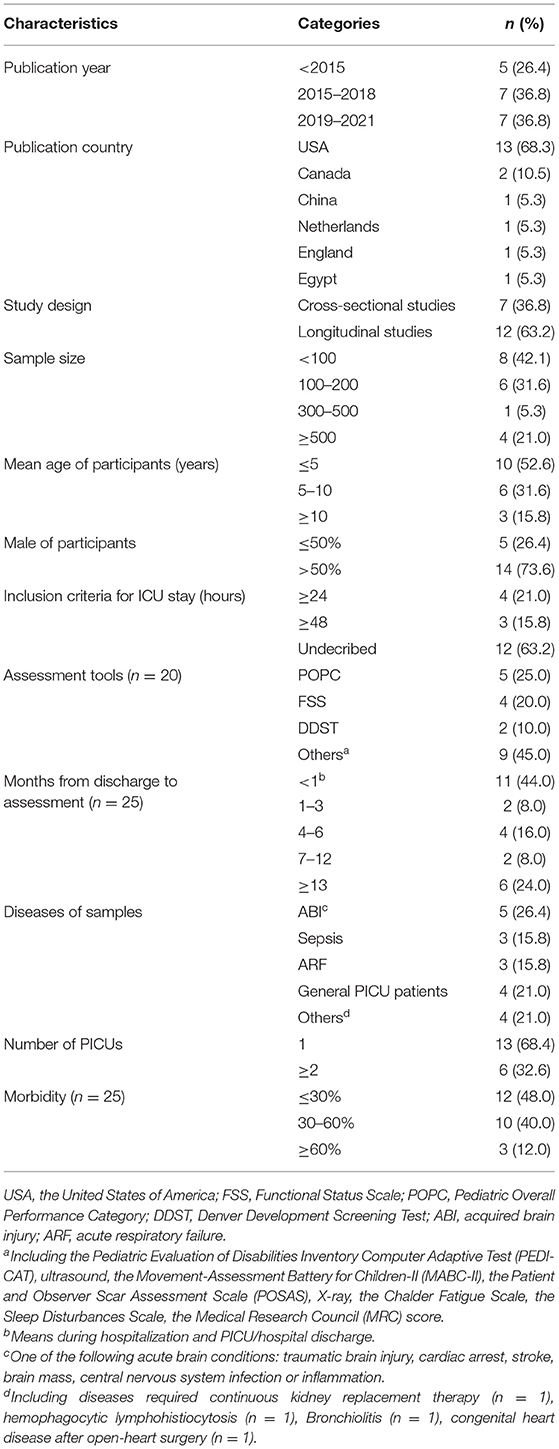
The characteristics of the 19 studies in the final analysis are presented in Table 1. The included studies were conducted in six different countries, and 13 studies (68.3%) were conducted in the United States. The publication years ranged from 1995 to 2021, and more than half of the studies (n = 14; 73.6%) were published between 2015 and 2021. Fourteen (73.6%) studies reported sex statistics and included more men than women. In these studies, the mean age of the participants was below 10 years old. Of the 19 included studies, 16 (84.2%) had unique samples involving 11,842 patients whose physical function impairments were reported. Of these, eight studies (50.0%) included heterogeneous samples and eight (50.0%) included homogeneous samples [acute respiratory failure (n = 1), sepsis (n = 3), hemophagocytic lymphohistiocytosis (n = 1), bronchiolitis (n = 1), congenital heart disease after open-heart surgery (n = 1), and bacterial meningitis (n = 1)]. A total of 8 (42.1%) studies included fewer than 100 patients. Multiple different instruments were used to report physical function impairments. A global physical function instrument, such as the Pediatric Overall Performance Category (POPC) (n = 5), was the most frequently used measurement instrument, followed by the Functional Status Scale (FSS) (n = 4). Other measurement instruments included biophysical instruments, such as X-ray (n = 1), ultrasound (n = 1), and physical function scales and scores (e.g., the Patient and Observer Scar Assessment Scale (POSAS) (n = 1), the Chalder Fatigue Scale (n = 1), the Sleep Disturbances Scale (n = 1), and the Medical Research Council score (n = 1)], and motor development instruments, such as the Denver Development Screening Test (n = 2), the Pediatric Evaluation of Disabilities Inventory Computer Adaptive Test (n = 1), and the Movement Assessment Battery for Children-II (MABC-II) (n = 1). Most studies found a morbidity rate of <60%.
Physical function impairments was reported to have occurred after PICU admission by 10 studies (56.0%) and after PICU/hospital discharge by 11 (44.0%) studies. Six (24%) studies included a follow-up time of >1 year. There were 7 (36.8%) cross-sectional studies and 12 (63.2%) longitudinal studies. The cross-sectional studies reported results over different time periods from admission to long-term post-PICU/hospital discharge. Disabilities in physical function after PICU/hospital discharge (range, 1 month to 10 years) showed that PICU survivors had difficulties in physical function years after PICU discharge. These long-term disabilities widely differed across studies ranging from mild to severe. The course of physical function impairments, from PICU admission to post-PICU/hospital discharge, was reported in 12 studies. The studies investigated the longitudinal trajectory of physical function impairments and demonstrated a considerable and persistent decline in physical function during the PICU stay or post-PICU/hospital discharge.
Risk Factors for Physical Function Impairments
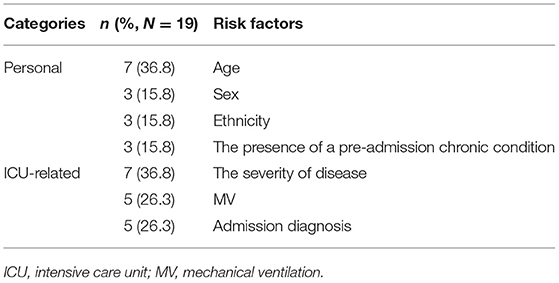
The risk factors for the impairments noted in the selected studies are defined and categorized in Table 2. A total of 41 risk factors were identified, of which 8 were categorized as personal, 11 as laboratory, and 22 as ICU-related factors. Personal factors included personality, social demographics, and medical history. ICU-related factors included ICU admission, ICU treatment, and patient experience. Three studies reported that older age was related to more physical disabilities (15, 19, 20), and another four studies of PICU survivors showed a negative relationship between younger age and impairments (21–24). Being a woman was a risk factor for impairments in two studies (24, 25), but another study determined that being a man with bronchiolitis was a risk factor (22). Two of the included studies reported that white race had worse outcomes than other races or ethnicities (24, 26).
Table 3 presents the most common risk factors reported in >3 studies for physical impairments. The most frequently reported personal risk factors associated with decreased physical function were age, race or ethnicity, a pre-admission chronic condition, and sex; age was observed in 7 (36.8%) studies (15, 19–24). ICU-related determinants were also associated with impairments, including disease severity, duration or the presence of mechanical ventilation (MV), and admission diagnosis. Disease severity was the most reported risk factor in the studies (n = 7, 36.8%) (19–21, 23–25, 27), followed by the duration or presence of MV (n = 5, 26.3%) (19, 22, 25, 28, 29) and admission diagnosis (n = 5, 26.3%) (20, 24, 25, 28, 30).
Discussion
In this review, the risk factors for physical function impairments were systematically collected and summarized. Because PICS has been emphasized since its proposal in 2010 (3), more studies were published in the past 6 years. In addition, more studies have been reported in the United States than in other countries. One possibility is that developed countries have more interest in PICS after critical illness because they have higher ICU survival rates and morbidities. The studies included in this review showed a considerable decline in physical function during the PICU/hospital stay or post-PICU/hospital discharge. The most frequently reported personal risk factors associated with physical function impairments were age, race or ethnicity, sex, the presence of a pre-admission chronic condition, and ICU-related risk factors, including disease severity, duration or the presence of MV, and admission diagnosis.
The physical instruments used in the selected studies varied, and the POPC and FSS were the most frequently used global physical function instruments. The FSS was primarily used during the PICU stay (31–33), and the POPC was used during the PICU stay or post-PICU discharge (19, 20, 22, 24, 28), particularly as a longitudinal measurement. In addition, assessment of muscle wasting and atrophy via ultrasound or muscle strength via dynamometry were conducted longitudinally during the PICU/hospital stay (25, 29). This review is similar to a recent review by Ong et al. (34), in which diverse measurement tools were used after PICU discharge, such as the Sleep Disturbance Scale for Children (35), the Chalder Fatigue Scale (26), POSAS (21), and MABC-II (36). Due to the complexity and diversity of the current tools, future research should develop a unique and comprehensive instrument to evaluate physical function impairments in PICU survivors. In accordance with the adult PICS field, more research is needed to detect and diagnose physical function impairments (37).
Physical function impairments rates differed across populations, measurement time, and tools used. The impairments rates in a general PICU population ranged from 0.02 to 10.3% at discharge to 38% at 6 months (19, 20, 26). However, the rates of impairments in acquired brain injury patients ranged from 28.9 to 70% (23, 27, 30, 32, 35), 2 to 69% among those with sepsis (19, 21, 24), and 20 to 34.3% among those needing MV (25, 28, 29). Overall, physical function impairments in the included studies ranged from 0.02 to 85.1% during hospitalization/at discharge (15, 19), 20 to 55.7% at 6 months (15, 28), and 2 to 70% at more than 1 year (19, 27). Within the same patient population impairment was lower using POSAS compared with global measures using POPC (19, 21). Furthermore, the longitudinal trajectory of physical function impairments indicated that PICU survivors may experience disabilities years after PICU discharge. Although some long-term improvements have been reported, most physical function levels were lower compared with reference and baseline function. A longitudinal study demonstrated that some impairments resolve with time as acquired impairments decreased from 18% at 3 months to 2% at 1 year following PICU discharge (19). Some studies measured physical function impairments only once, within 6 months after discharge (19, 25, 26, 29, 35). Because impairments may last more than 10 years after discharge (21, 36), more prospective studies are warranted to determine changes in impairments over time by conducting long-term follow-up studies of survivors. Additional important impairments in adult ICU survivors, including sleep disruption and fatigue, seem to be ignored, but data suggest that these problems also occur in children (26, 38, 39).
Physical function impairments in over a third of PICU survivors can present as loss of muscle mass, neuromuscular weakness, impaired lung function, weight loss, and fatigue (17). These impairments restrict daily functioning and can lead to persistent functional disabilities (e.g., limitations in feeding, dressing, and getting out of bed or in mobility) (3, 11, 34). The PICS-p framework is now recognized for children and has standardized follow-up care following a PICU stay, especially for children with a higher risk for significantly worse physical function (11, 17, 40). Early recognition of children at risk for impairments can help prevent these complications by beginning active or passive exercises immediately after admission (41, 42). A total of 41 risk factors were determined in this review. The most common risk factors were reported in more than three studies, but only seven risk factors were defined. Long-term physical function impairments can be persistent, but few studies explored the related risk factors. Future longitudinal research on individual risk factors is needed to develop consensus on physical function impairments.
The most frequently reported personal risk factors associated with decreased physical function were older age, white race, the presence of a pre-admission chronic condition, and being woman. This result is consistent with those of previous studies in adults (43, 44). However, contradictory results were also obtained from some studies. Older age is usually mentioned as a risk factor for physical function impairments in a general PICU population, whereas four of the included studies demonstrated a positive relationship between younger age and impairments among those with specific diagnoses (such as sepsis and acquired brain injury) (21–24). Personal risk factors are not modifiable but can be used to screen for the risk of impairments. The PICS-p framework highlights the baseline status that might possibly impact the health and life of the child for decades (11). A decline in baseline functional status and the presence of pre-admission chronic conditions places the patient at a higher risk for physical function impairments (15, 28, 33, 35). Chronic conditions prior to admission may decrease the patient's baseline function, and it also places the patient at a higher risk of long-term impairments after discharge. In addition, the PICS-p framework emphasizes that family and parents are important for children, but these factors do not seem to have attracted much attention in the currently limited literature (45, 46). In this review, lower maternal education and incomplete family composition were risk factors for physical function impairments (26, 36).
ICU-related determinants, including disease severity, duration or the presence of MV, and admission diagnosis were also associated with decreased levels of physical function. MV during the PICU stay is considered to be one of the main causes leading to ICUAW (47–49). High disease severity, such as an elevated Pediatric Index of Mortality 2 score or Pediatric Risk of Mortality score, and longer duration of MV as risk factors for physical impairments were consistent with the results of the selected studies. Admission diagnosis was also a risk factor for physical function impairments, with trauma and cancer placing the patient at a higher risk compared with other admission diagnoses (20, 24, 28, 30). Although diagnosis at admission and disease severity were unmodifiable factors, they were the key factors in determining the patients' level of physical function and wellbeing (50, 51). Follow-up and rehabilitation programs after PICU discharge focusing on these risk factors might enhance the success of reducing impairments and promote the effective use of health services.
There were several limitations to this review. First, the quality and validity of the included studies were not formally evaluated. Second, some univariate statistical results, but not adjusted statistical results, were accepted. Third, the search term QoL was excluded; thus, some risk factors for impairments may have been missed. Finally, given the limited number of studies and the heterogeneity of the studies (e.g., instruments, population, length of follow-up, design, and outcome measures), it was difficult to calculate and synthesize the data and conclusions. Given such heterogeneity, two of the authors used standardized extraction forms and consensus to determine a more comprehensive evidence summary. This review greatly helps in clearly understanding physical function impairments by integrating studies of risk factors and identifying interventions to prevent or reduce its severity; however, future research is needed.
Conclusion
In summary, children admitted to the PICU will experience physical function impairments during their PICU stay or post-PICU/hospital discharge, which may last for many years. The most frequently reported risk factors for impairments were age, ethnicity, a pre-admission chronic condition, sex, disease severity, duration or the presence of MV, and admission diagnosis. Of these, the duration of MV is important because it is modifiable. Management of critical care can play a significant role in preventing physical impairments in PICS. It is necessary to develop an objective measurement tool that integrates and assesses multidimensional factors based on an operational definition of physical function impairments. Future studies need to be conducted to reach a consensus on identifying risk factors and mechanisms of physical function impairments in critically ill children.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author Contributions
MD: conceptualization, methodology, investigation, and writing—original draft. CY: writing—review and editing, investigation, and software. YL: project administration. All authors contributed to the intellectual content of this manuscript and approved the final manuscript as submitted.
Funding
This study was funded by the subject named Development and Construction of Polydopamine-doped Calcium Alginate Antimicrobial Hydrogel Dressing and Its Application in Wound Repair (No. CGZHYD202012-006).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
All authors thank Enago (http://www.enago.com) for providing English help.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2022.905167/full#supplementary-material
References
1. Inoue S, Hatakeyama J, Kondo Y, Hifumi T, Sakuramoto H, Kawasaki T, et al. Post-intensive care syndrome: its pathophysiology, prevention, and future directions. Acute Med Surg. (2019) 6:233–46. doi: 10.1002/ams2.415
2. Detsky ME, Kohn R, Delman AM, Buehler AE, Kent SA, Ciuffetelli IV, et al. Patients' perceptions and ICU clinicians predictions of quality of life following critical illness. J Crit Care. (2018) 48:352–6. doi: 10.1016/j.jcrc.2018.09.034
3. Needham DM, Davidson J, Cohen H, Hopkins RO, Weinert C, Wunsch H, et al. Improving long-term outcomes after discharge from intensive care unit: report from a stakeholders' conference. Crit Care Med. (2012) 40:502–9. doi: 10.1097/CCM.0b013e318232da75
4. Kosinski S, Mohammad RA, Pitcher M, Haezebrouck E, Coe AB, Costa DK, et al. What is post-intensive care syndrome (PICS)? Am J Respir Crit Care Med. (2020) 201:P15–6. doi: 10.1164/rccm.2018P15
5. Beumeler LFE, van Wieren A, Buter H, van Zutphen T, Bruins NA, de Jager CM, et al. Patient-reported physical functioning is limited in almost half of critical illness survivors 1-year after ICU-admission: a retrospective single-centre study. PLoS ONE. (2020) 15:e0243981. doi: 10.1371/journal.pone.0243981
6. Kerckhoffs MC, Kosasi FFL, Soliman IW, van Delden JJM, Cremer OL, de Lange DW, et al. Determinants of self-reported unacceptable outcome of intensive care treatment 1 year after discharge. Intens Care Med. (2019) 45:806–14. doi: 10.1007/s00134-019-05583-4
7. Ohtake PJ, Lee AC, Scott JC, Hinman RS, Ali NA, Hinkson CR, et al. Physical impairments associated with post-intensive care syndrome: systematic review based on the World Health Organization's International Classification of Functioning, Disability and Health Framework. Phys Ther. (2018) 98:631–45. doi: 10.1093/ptj/pzy059
8. Van Aerde N, Meersseman P, Debaveye Y, Wilmer A, Gunst J, Casaer MP, et al. Five-year impact of ICU-acquired neuromuscular complications: a prospective, observational study. Intens Care Med. (2020) 46:1184–93. doi: 10.1007/s00134-020-05927-5
9. Vanhorebeek I, Latronico N, Van den Berghe G. ICU-acquired weakness. Intens Care Med. (2020) 46:637–53. doi: 10.1007/s00134-020-05944-4
10. Lad H, Saumur TM, Herridge MS, Dos Santos CC, Mathur S, Batt J, et al. Intensive care unit-acquired weakness: not just another muscle atrophying condition. Int J Mol Sci. (2020) 21:7840. doi: 10.3390/ijms21217840
11. Manning JC, Pinto NP, Rennick JE, Colville G, Curley MAQ. Conceptualizing post intensive care syndrome in children-the PICS-p framework. Pediatr Crit Care Med. (2018) 19:298–300. doi: 10.1097/PCC.0000000000001476
12. Hartman ME, Saeed MJ, Bennett T, Typpo K, Matos R, Olsen MA. Readmission and late mortality after critical illness in childhood. Pediatr Crit Care Med. (2017) 18:e112–21. doi: 10.1097/PCC.0000000000001062
13. Kyösti E, Liisanantti JH, Peltoniemi O, Ohtonen P, Rautiainen P, Kataja J, et al. Five-year survival and causes of death in children after intensive care-A National Registry Study. Pediatr Crit Care Med. (2018) 19:e145–51. doi: 10.1097/PCC.0000000000001424
14. Maddux AB, Bennett TD. Mortality after pediatric critical illness: made it home, still vulnerable. Pediatr Crit Care Med. (2018) 19:272–3. doi: 10.1097/PCC.0000000000001432
15. Choong K, Fraser D, Al-Harbi S, Borham A, Cameron J, Cameron S, et al. Functional recovery in critically ill children, the “WeeCover” multicenter study. Pediatr Crit Care Med. (2018) 19:145–54. doi: 10.1097/PCC.0000000000001421
16. Rodriguez-Rubio M, Pinto NP, Manning JC, Kudchadkar SR. Post-intensive care syndrome in paediatrics: setting our sights on survivorship. Lancet Child Adolesc Health. (2020) 4:486–8. doi: 10.1016/S2352-4642(20)30170-X
17. Watson RS, Choong K, Colville G, Crow S, Dervan LA, Hopkins RO, et al. Life after critical illness in children-toward an understanding of pediatric post-intensive care syndrome. J Pediatr. (2018) 198:16–24. doi: 10.1016/j.jpeds.2017.12.084
18. Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. (2018) 169:467–73. doi: 10.7326/M18-0850
19. Field-Ridley A, Dharmar M, Steinhorn D, McDonald C, Marcin JP. ICU-acquired weakness is associated with differences in clinical outcomes in critically ill children. Pediatr Crit Care Med. (2016) 17:53–7. doi: 10.1097/PCC.0000000000000538
20. Bone MF, Feinglass JM, Goodman DM. Risk factors for acquiring functional and cognitive disabilities during admission to a PICU*. Pediatr Crit Care Med. (2014) 15:640–8. doi: 10.1097/PCC.0000000000000199
21. Buysse CM, Oranje AP, Zuidema E, Hazelzet JA, Hop WC, Diepstraten AF, et al. Long-term skin scarring and orthopaedic sequelae in survivors of meningococcal septic shock. Arch Dis Child. (2009) 94:381–6. doi: 10.1136/adc.2007.131862
22. Shein SL, Slain KN, Clayton JA, McKee B, Rotta AT, Wilson-Costello D. Neurologic and functional morbidity in critically ill children with bronchiolitis. Pediatr Crit Care Med. (2017) 18:1106–13. doi: 10.1097/PCC.0000000000001337
23. Thakker JC, Splaingard M, Zhu J, Babel K, Bresnahan J, Havens PL. Survival and functional outcome of children requiring endotracheal intubation during therapy for severe traumatic brain injury. Crit Care Med. (1997) 25:1396–401. doi: 10.1097/00003246-199708000-00030
24. Farris RW, Weiss NS, Zimmerman JJ. Functional outcomes in pediatric severe sepsis: further analysis of the researching severe sepsis and organ dysfunction in children: a global perspective trial. Pediatr Crit Care Med. (2013) 14:835–42. doi: 10.1097/PCC.0b013e3182a551c8
25. Thabet Mahmoud A, Tawfik MAM, Abd El Naby SA, Abo El Fotoh WMM, Saleh NY, Abd El Hady NMS. Neurophysiological study of critical illness polyneuropathy and myopathy in mechanically ventilated children; additional aspects in paediatric critical illness comorbidities. Eur J Neurol. (2018) 25:991–e76. doi: 10.1111/ene.13649
26. Als LC, Picouto MD, Hau SM, Nadel S, Cooper M, Pierce CM, et al. Mental and physical well-being following admission to pediatric intensive care. Pediatr Crit Care Med. (2015) 16:e141–9. doi: 10.1097/PCC.0000000000000424
27. Madagame ET, Havens PL, Bresnahan JM, Babel KL, Splaingard ML. Survival and functional outcome of children requiring mechanical ventilation during therapy for acute bacterial meningitis. Crit Care Med. (1995) 23:1279–83. doi: 10.1097/00003246-199507000-00019
28. Watson RS, Asaro LA, Hutchins L, Bysani GK, Killien EY, Angus DC, et al. Risk factors for functional decline and impaired quality of life after pediatric respiratory failure. Am J Respir Crit Care Med. (2019) 200:900–9. doi: 10.1164/rccm.201810-1881OC
29. Xue Y, Yang CF, Ao Y, Qi J, Jia FY. A prospective observational study on critically ill children with diaphragmatic dysfunction: clinical outcomes and risk factors. BMC Pediatr. (2020) 20:422. doi: 10.1186/s12887-020-02310-7
30. Holding EZ, Turner EM, Hall TA, Leonard S, Bradbury KR, Williams CN. The association between functional status and health-related quality of life following discharge from the pediatric intensive care unit. Neurocrit Care. (2021) 35:347–57. doi: 10.1007/s12028-021-01271-8
31. Gregory J, Greenberg J, Basu S. Outcomes analysis of children diagnosed with hemophagocytic lymphohistiocytosis in the PICU. Pediatr Crit Care Med. (2019) 20:e185–90. doi: 10.1097/PCC.0000000000001827
32. Madurski C, Jarvis JM, Beers SR, Houtrow AJ, Wagner AK, Fabio A, et al. Serum biomarkers of regeneration and plasticity are associated with functional outcome in pediatric neurocritical illness: an exploratory study. Neurocrit Care. (2021) 35:457–67. doi: 10.1007/s12028-021-01199-z
33. Smith M, Bell C, Vega MW, Tufan Pekkucuksen N, Loftis L, McPherson M, et al. Patient-centered outcomes in pediatric continuous kidney replacement therapy: new morbidity and worsened functional status in survivors. Pediatr Nephrol. (2022) 37:189–97. doi: 10.1007/s00467-021-05177-7
34. Ong C, Lee JH, Leow MK, Puthucheary ZA. Functional outcomes and physical impairments in pediatric critical care survivors: a scoping review. Pediatr Crit Care Med. (2016) 17:e247–59. doi: 10.1097/PCC.0000000000000706
35. Williams CN, Hartman ME, McEvoy CT, Hall TA, Lim MM, Shea SA, et al. Sleep-wake disturbances after acquired brain injury in children surviving critical care. Pediatr Neurol. (2020) 103:43–51. doi: 10.1016/j.pediatrneurol.2019.08.010
36. Shevell AH, Sahakian SK, Nguyen Q, Fontela P, Rohlicek C, Majnemer A. Associations between postoperative management in the critical care unit and adolescent developmental outcomes following cardiac surgery in infancy: an exploratory study. Pediatr Crit Care Med. (2020) 21:e1010–9. doi: 10.1097/PCC.0000000000002398
37. Major ME, Kwakman R, Kho ME, Connolly B, McWilliams D, Denehy L, et al. Surviving critical illness: what is next? An expert consensus statement on physical rehabilitation after hospital discharge. Crit Care. (2016) 20:354. doi: 10.1186/s13054-016-1508-x
38. Crichton AJ, Babl F, Oakley E, Greenham M, Hearps S, Delzoppo C, et al. Prediction of multidimensional fatigue after childhood brain injury. J Head Trauma Rehabil. (2017) 32:107–16. doi: 10.1097/HTR.0000000000000248
39. Gagner C, Landry-Roy C, Lainé F, Beauchamp MH. Sleep-wake disturbances and fatigue after pediatric traumatic brain injury: a systematic review of the literature. J Neurotrauma. (2015) 32:1539–52. doi: 10.1089/neu.2014.3753
40. Herrup EA, Wieczorek B, Kudchadkar SR. Characteristics of postintensive care syndrome in survivors of pediatric critical illness: a systematic review. World J Crit Care Med. (2017) 6:124–34. doi: 10.5492/wjccm.v6.i2.124
41. Kudchadkar SR, Nelliot A, Awojoodu R, Vaidya D, Traube C, Walker T, et al. Physical rehabilitation in critically ill children: a multicenter point prevalence study in the United States. Crit Care Med. (2020) 48:634–44. doi: 10.1097/CCM.0000000000004291
42. Kondo Y, Fuke R, Hifumi T, Hatakeyama J, Takei T, Yamakawa K, et al. Early rehabilitation for the prevention of postintensive care syndrome in critically ill patients: a study protocol for a systematic review and meta-analysis. BMJ Open. (2017) 7:e013828. doi: 10.1136/bmjopen-2016-013828
43. Lee M, Kang J, Jeong YJ. Risk factors for post-intensive care syndrome: a systematic review and meta-analysis. Aust Crit Care. (2020) 33:287–94. doi: 10.1016/j.aucc.2019.10.004
44. Dowdy DW, Eid MP, Sedrakyan A, Mendez-Tellez PA, Pronovost PJ, Herridge MS, et al. Quality of life in adult survivors of critical illness: a systematic review of the literature. Intens Care Med. (2005) 31:611–20. doi: 10.1007/s00134-005-2704-3
45. Colville G, Pierce C. Patterns of post-traumatic stress symptoms in families after paediatric intensive care. Intens Care Med. (2012) 38:1523–31. doi: 10.1007/s00134-012-2612-2
46. Nelson LP, Gold JI. Posttraumatic stress disorder in children and their parents following admission to the pediatric intensive care unit: a review. Pediatr Crit Care Med. (2012) 13:338–47. doi: 10.1097/PCC.0b013e3182196a8f
47. NHLBI Workshop summary. Respiratory muscle fatigue. Report of the Respiratory Muscle Fatigue Workshop Group. Am Rev Respir Dis. (1990) 142:474–80. doi: 10.1164/ajrccm/142.2.474
48. Crulli B, Kawaguchi A, Praud JP, Petrof BJ, Harrington K, Emeriaud G. Evolution of inspiratory muscle function in children during mechanical ventilation. Crit Care. (2021) 25:229. doi: 10.1186/s13054-021-03647-w
49. MM IJ, Lemson J, van der Hoeven JG, Heunks LMA. The impact of critical illness on the expiratory muscles and the diaphragm assessed by ultrasound in mechanical ventilated children. Ann Intens Care. (2020) 10:115. doi: 10.1186/s13613-020-00731-2
50. Treble-Barna A, Beers SR, Houtrow AJ, Ortiz-Aguayo R, Valenta C, Stanger M, et al. PICU-based rehabilitation and outcomes assessment: a survey of pediatric critical care physicians. Pediatr Crit Care Med. (2019) 20:e274–82. doi: 10.1097/PCC.0000000000001940
Keywords: children, postintensive care syndrome, physical function impairments, pediatric intensive care unit, risk factors
Citation: Ding M, Yang CF and Li YM (2022) Risk Factors for Physical Function Impairments in Postintensive Care Syndrome: A Scoping Review. Front. Pediatr. 10:905167. doi: 10.3389/fped.2022.905167
Received: 26 March 2022; Accepted: 27 May 2022;
Published: 17 June 2022.
Edited by:
Brenda M. Morrow, University of Cape Town, South AfricaCopyright © 2022 Ding, Yang and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yumei Li, eW1fbGlAamx1LmVkdS5jbg==
 Min Ding
Min Ding Chunfeng Yang
Chunfeng Yang Yumei Li
Yumei Li