- 1National Clinical Research Center for Child Health and Disorders, Ministry of Education Key Laboratory of Child Development and Disorders, Chongqing Key Laboratory of Pediatrics, Clinical Epidemiology and Biostatistics Department, Children's Hospital of Chongqing Medical University, Chongqing, China
- 2Department of Public Health and Preventive Medicine, School of Medicine, Jinan University, Guangzhou, China
- 3Department of Medicine, Medical College of Georgia, Georgia Prevention Institute, Augusta University, Augusta, GA, United States
Background: Epidemiologic evidence linking environmental noise to obesity and hypertension remains scarce, especially in children, and the results remain inconclusive. This study aims to examine the cross-sectional associations of self-reported residential noise exposure with obesity and hypertension in children and adolescents.
Methods: As an ongoing study, a representative sample of the children aged 6–9 years in Chongqing were selected in 2014. In 2019, self-reported residential noise (answer categories: “very quiet,” “moderately quiet,” “slightly quiet,” and “not at all quiet”) data were collected, and 3,412 participants with completed data were included in the analyses.
Results: Participants living in a quieter area had a significantly lower risk of obesity than those living in a noisy area (very quiet: OR = 0.50, 95%CI: 0.29–0.88, P = 0.015; moderately quiet: OR = 0.61, 95%CI: 0.36–1.02, P = 0.059). Similar associations were observed for abdominal obesity, although did not reach statistical significance. Consistently, residential noise exposure was significantly associated with body mass index (BMI) and waist-to-height ratio. Self-reported residential noise exposure was positively associated with systolic blood pressure (β = −1.808; 95%CI = −3.495, −0.110; P = 0.037). When sleep quality, study stress, BMI, and vegetable/fruits consumption were further adjusted, all effect estimates decreased, and no statistical association was observed between noise exposure and blood pressure. Furthermore, we found that the mediating effects of obesity on the associations of self-reported residential noise exposure with hypertension were 6.8% (% of total effect mediated = 0.068, 95%CI: −2.58, 3.99), although did not reach statistical significance.
Conclusions: Self-reported residential noise exposure was associated with a higher risk of obesity or abdominal obesity. Also, self-reported residential noise exposure was positively associated with hypertension, and obesity may partially mediate this association, but did not reach statistical significance.
Introduction
Childhood obesity and hypertension continue to increase worldwide. It is estimated that 8% of children and adolescents had hypertension during 2010-14, and 6% of girls and 8% of boys were obese in 2016 (1, 2). Childhood obesity and hypertension contribute to many chronic diseases in adults, such as heart disease and kidney disease. (3–5) The increase in health risks and socioeconomic losses related to obesity and hypertension have aroused widespread concern (6). Therefore, identifying early modifiable factors for preventing childhood obesity and hypertension is required.
Poor dietary quality and sedentary lifestyles have been known to cause obesity and hypertension (7, 8). In recent decades, environmental noise has been attracting growing attention. Previous studies have investigated the associations of environmental noise with the risk of obesity and hypertension in children or adults, but the results are controversial and the effect size was small even though a positive association was observed (9–13). It is suggested that noise sensitivity, rather than the noise level, predicts the non-auditory health hazards of noise (14). However, almost all these studies adopted model estimated road traffic noise in the analysis, which may be inaccurate as the layout of rooms in the house, window opening habits, and indoor noise levels were not taken into account (15), indeed, noise sensitivity was also not considered. Also, most of these findings come from Europe and North American countries. In this study, we examined the cross-sectional associations of self-reported residential noise exposure with obesity and hypertension among Chinese children and adolescents.
Methods
In 2014, a stratified cluster sampling was used to obtain a representative sample of the children aged 6–9 years in Chongqing (16). The first stage of sampling was to randomly select one rural and one urban county, then two communities per county were randomly selected. Participants were recruited if they: (1) were aged between six and nine years in 2014, (2) resided in the target region for more than 6 months, (3) did not have serious diseases (e.g., nephropathy, cardiovascular disease, or cancer), and obtained consent both from the parents and children for participation. A total of 5,246 children living in the selected communities were informed and included if they satisfied the inclusion criteria. At baseline, demographic information and physical examination data were collected. As an ongoing study, 4,162 participants were followed up in 2019. Besides the physical examination, self-reported residential noise was collected. In this study, 3,412 participants with completed data in 2019 were included in the analyses. All work in this study was conducted following the ethical guidelines of the 1964 Declaration of Helsinki and its later amendments. The Institutional Review Board at the Children's Hospital of Chongqing Medical University approved the study (File No.: 2019–86). Informed consent was obtained from all participants and their parents/guardians.
Measurements and definitions
Anthropometric measurements were performed by well-trained pediatric nurses as described in a previous publication. (16) A mobile medical ultrasonic machine (models-H300D) was used to measure height and weight, and body mass index (BMI) was calculated as weight/height2 (kg/m2). Obesity was defined according to Chinese guidelines for children and adolescents (Supplementary Table 1) (17). Waist circumstance (WC) (18) was measured twice at the center of the umbilicus over one T-shirt and the values were averaged. The waist-to-height ratio (WHtR) was calculated as WC divided by the height. The cut-off value of 0.48 was used for WHtR to classify abdominal obesity (19).
Blood pressure (BP) was measured using an OMRON arm-type electronic sphygmomanometer (HEM7051) (16). BP measurements were taken at 11, 13, and 15 min after a 10-min seated rest in the morning (09:00–12:00) using a proper sized cuff on the right arm. The average of the three measurements was taken to represent resting systolic blood pressure (SBP) and diastolic blood pressure (DBP) levels. Hypertension was defined as a mean SBP and/or DBP ≥95th percentile (20).
Residential noise was assessed by the question “is your flat or house quiet (answer categories: ‘very quiet', ‘moderately quiet', ‘slightly quiet', and ‘not at all')?”
Demographic information was collected by a standardized questionnaire. Study stress was assessed by the question ‘Do you feel study stress over last year 1) extremely, 2) very, 3) moderately, 4) slightly, or 5) no at all.' The participants answered 1) extremely, 2) very, or 3) moderately were defined as having study stress. A previously reported quantitative food frequency questionnaire (FFQ) was used to collect dietary information (21). The questionnaire was filled by the parents or guardians of the children after standard training by the research team. The Children's Sleep Habits Questionnaire (CSHQ) was used to assess the children's sleep quality (22). A score 1 to 3 was assigned to each response. The overall score ranged from 0 to 99 by summarizing the scores of all 33 items. A higher score indicated a worse sleep quality. The exercise was assessed by the self-reported vigorous/moderate physical activity (including playing basketball, swimming, hiking, running, riding a bike, etc.). The number of minutes per day was calculated (16).
Statistical analyses
Differences of continuous variables in general characteristics of participants were assessed using a t-test, and a χ2 test was used to compare the difference of categorical variables. Logistic regression was used to analyze the associations of residential noise exposure with obesity, abdominal obesity, and hypertension, while a linear regression model was performed to test the associations of self-reported residential noise exposure with BMI, WHtR, SBP, and DBP. For estimating the direct effect and total effect of self-reported noise exposure on outcomes, a Directed Acyclic Graph (DAG) was constructed to represent plausible causal assumptions in the context of possible confounding factors and intermediate pathways (Supplementary Figure 1) (23). For obesity, univariate analyses were performed in Model 1. Model 2 was adjusted for age, sex, exercise, father's education, and region (urban/rural). Model 3 additionally controlled for sleep quality, study stress, and vegetable/fruits consumption. For hypertension, BMI was further adjusted in model 3. Also, the mediation effect of BMI on the association between self-reported residential noise exposure and hypertension (“medeff” package). All statistical analyses were implemented using Stata software version 12 (STATA Corp., TX, US). A two-sided P < 0.05 was considered statistically significant.
Results
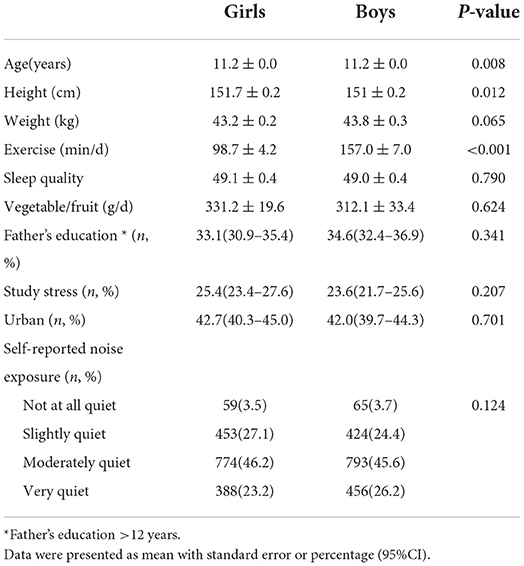
The general characteristics of the participants are presented in Table 1. A total of 3,412 participants were included, who were aged 11.2 years on average, and 49.1% were boys. About 50% of participants were living in very quiet or moderately quiet areas.
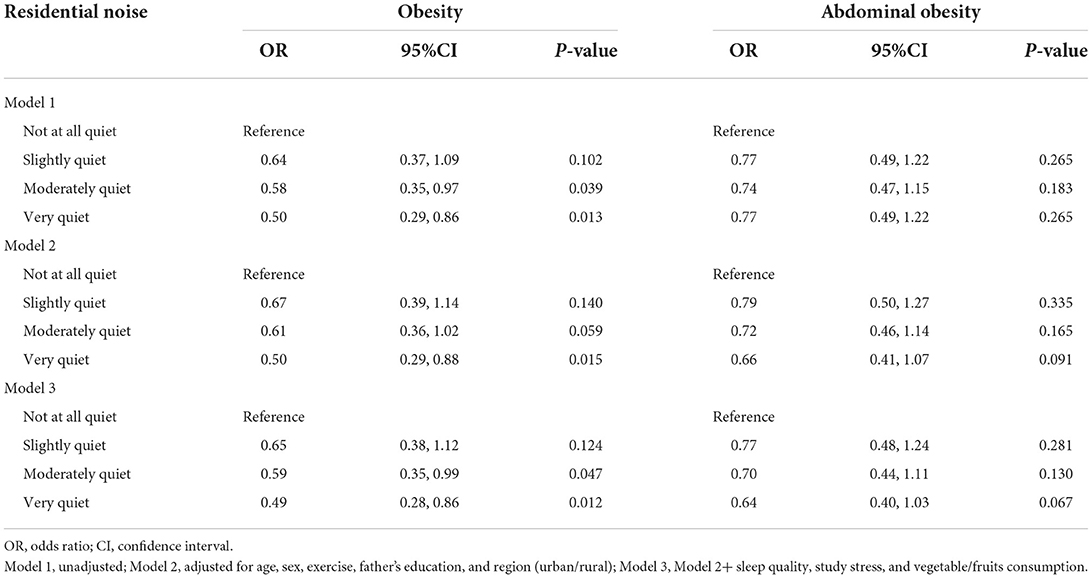
The proportions of obesity were 15.3, 10.4, 9.5, and 8.3% in participants living in not at all, slightly, moderately and very quiet areas, while these proportions for abdominal obesity were 21.8, 17.7, 17.0, and 16.6%, respectively (Figure 1). The participants living in a quieter area had a significantly lower risk of obesity than those living in a noisy area (very quiet: OR = 0.50, 95%CI: 0.29–0.88, P = 0.015; moderately quiet: OR = 0.61, 95%CI: 0.36–1.02, P = 0.059). Model 3 further controlled for the sleep quality, study stress, and vegetable/fruits consumption, the results remain similar (very quiet: OR = 0.49, 95%CI: 0.28–0.86, P = 0.012; moderately quiet: OR = 0.59, 95%CI: 0.35–0.99, P = 0.047). Similar associations were observed for abdominal obesity, although did not reach statistical significance (Table 2). Consistently, residential noise exposure was significantly associated with BMI and WHtR (Table 3).

Figure 1. Proportions of (A) obesity and (B) abdominal obesity by self-reported residential noise exposure.
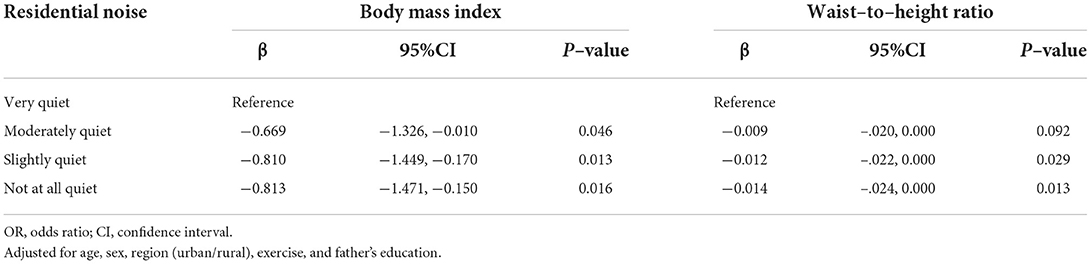
Table 3. Associations of self-reported noise exposure with body mass index and waist-to-height ratio.
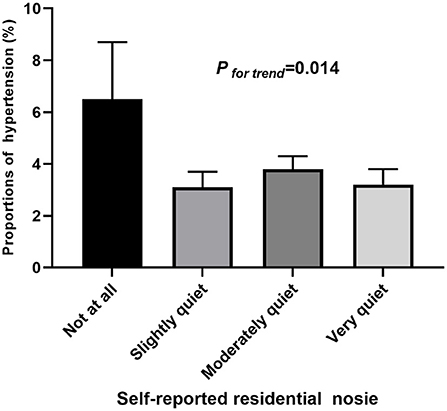
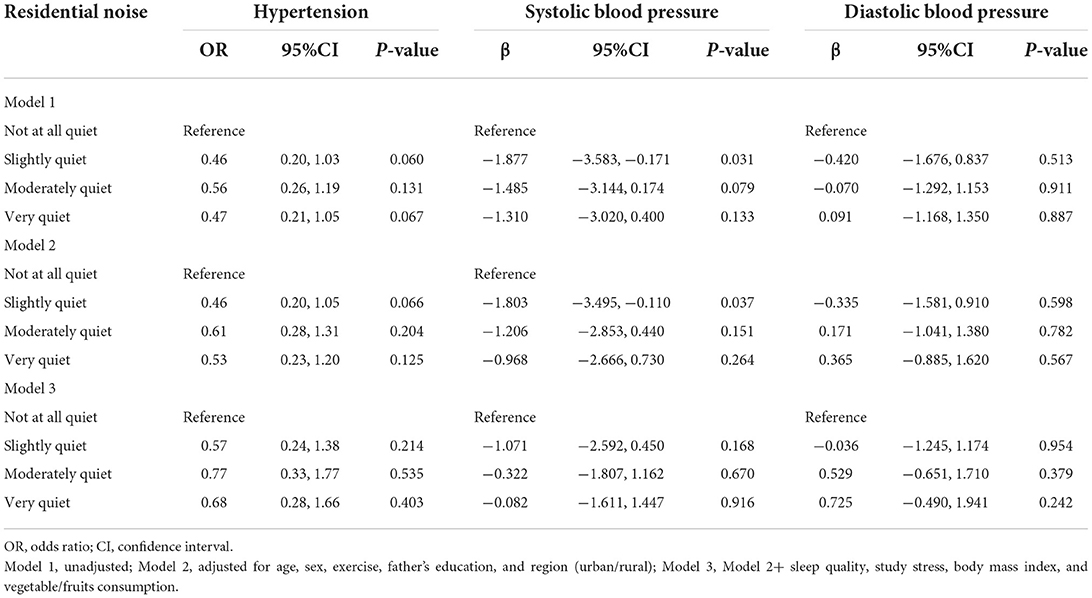
The proportions of hypertension were 6.5, 3.1, 3.8, and 3.2% in participants living in not at all, slightly, moderately, and very quiet areas (Figure 2). Self-reported residential noise exposure was positively associated with hypertension and SBP after adjusting for age, sex, exercise, father's education, and region (urban/rural) (β = −1.808; 95%CI = −3.495, −0.110; P = 0.037) in model 2. After further adjusting for sleep quality, study stress, BMI, and vegetable/fruits consumption, all effect estimates decreased, and no statistical association was observed (Table 4). Furthermore, we found that the mediating effect of obesity on the associations of self-reported residential noise exposure with hypertension was 6.8% (% of total effect mediated = 0.068, 95%CI: −2.58, 3.99), although failed to achieve statistical significance.
Discussions
We found that self-reported residential noise exposure was significantly associated with a higher risk of obesity and abdominal obesity. Also, self-reported residential noise exposure was positively associated with hypertension, and obesity may partially mediate this association, although these findings did not reach statistical significance.
Several studies, most performed in European countries, examined the associations between transportation noise exposure and obesity or its markers in adults using cross-sectional and longitudinal designs. Overall, current results are mixed (24–27), and the magnitude was small even if a significant association was reported (25, 28). Few studies investigated whether transportation noise is related to obesity and its markers in children and adolescents, and the results were also inconsistent (29). The Danish National Birth Cohort reported marginally significant associations between residential road traffic noise exposure during pregnancy and childhood and risk for childhood overweight and statistically non-significant associations for BMI z-scores (30). However, another longitudinal study reported that BMI curves from birth to 8 years were only associated with road traffic noise exposure during pregnancy, but not with the exposure during childhood (31). A Norwegian study observed associations with both adipose markers only in highly noise-sensitive women (14). In line with this study to some extent, we found a significant association between self-reported residential noise exposure and obesity with a large effect size in children and adolescents.
Epidemiologic evidence linking environmental noise to hypertension also remains scarce, especially in children, and the results remain inconclusive. In a large case-control study, Zeeb et al. found no association between residential traffic noise exposure and hypertension in the primary analysis, but a significant positive association in persons with an initial hypertension diagnosis (32). A study from Canada reported that long-term exposure to road traffic noise was longitudinally associated with an increased risk of hypertension in adults (33). A research conducted among Indian adult population reported that the exposure to road traffic noise at L den > 65 dB(A) in male and L den > 60 dB(A) in female was correlated to the prevalence of hypertension (34). A cross-sectional study involving 500 Chinese adults found that indoor nocturnal noise was associated with BMI and BP in females but only BP in males (35). One possible explanation is that females might be more annoyed by noise than males (36). To our best knowledge, this study, for the first time, reported the association between self-reported residential noise and hypertension in children and adolescents, and the results suggested that obesity may partially mediate this association.
The mechanisms underlying the associations of environmental noise and obesity and hypertension are not fully understood. Multiple health conditions, physically or mentally, have been linked to the environmental noise exposure, which includes sleep disorders (37, 38). Noise-induced sleep disorders may play a role in these associations. Children's sleep duration is negatively associated with overweight in both cross-sectional and longitudinal studies, possibly through the influence on insulin resistance, sedentarism, and unhealthy dietary patterns (39–41). On the other hand, children with obstructive sleep apnea have increased sympathetic activation during sleep, blunted dipping, or elevated systolic or diastolic pressures (42). Moreover, traffic noise exposure has been suggested to trigger stress in children in previous studies (43). Stress caused by exposure to environmental noise could be increasing the risk of obesity and hypertension (44, 45).
Limitations and strengths
One major strength was that we investigated the associations of residential noise exposure with obesity and hypertension in children and adolescents using self-reported residential noise data, to some extent, which may be a better index taking account of noise sensitivity at the same time to test the effect of residential noise on health. There were also several limitations in our study. First, exposure to noise at school may have a more substantial effect on BP in children (46), but we did not account for exposure outside of the home in this analysis. Second, this study cannot infer causality due to the cross-sectional study design. Moreover, estimating mediation analysis with cross-sectional data will overestimate or underestimate the mediation effect. Third, we could not include all risk factors due to the limitation of the data, such as genotypes, air pollution et al. More cohort studies, including objective and individual level environmental noise measurement, are desirable to confirm the results. Fourthly, the father's education may not the best indicator of the family's socioeconomic status. Finally, the noise level was divided into four categories by participants' subjective feelings, so future studies considering the objective measurement of noise exposure using a noise meter and subjective measurement of noise sensitivity using standardized questionnaire are required.
Conclusion
In conclusion, this study showed that self-reported residential noise exposure was associated with a higher risk of obesity and abdominal obesity. Also, self-reported residential noise exposure was positively associated with the risk of hypertension, and obesity may partially mediate this association, although these findings did not reach statistical significance. Further studies will be necessary to confirm our results.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Institutional Review Board at the Children's Hospital of Chongqing Medical University. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author contributions
GH conceived and designed the study. XT, XHL, and YR collected the data. XHL contributed to the performance of the statistical analysis and interpretation of the results and wrote the first draft of this manuscript. ML, XC, LZ. XT, XYL, LC, and YR critically reviewed and approved the final paper. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the Basic Research Project of Key Laboratory of Ministry of Education of China in 2021(GBRP-202106), Major Health Project of Chongqing Science and Technology Bureau (No. CSTC2021jscx-gksb-N0001), Research and Innovation Team of Chongqing Medical University (No. W0088), Joint Medical Research Project of Chongqing Municipal Health Commission and Chongqing Science and Technology Bureau (No. 2020MSXM062), National Key Research and Development Project (2017YFC0211705), Education Commission of Chongqing Municipality (KJQN201900443) and National Natural Science Foundation of China (82003521, 81502826). The research is also financially supported by Hunan Provincial Key Laboratory of Clinical Epidemiology (2021ZNDXLCL002).
Acknowledgments
The authors would like to acknowledge the laboratory support of the Ministry of Education Key Laboratory of Child Development and Disorders and all the staff members of the 6 elementary schools in the three regions.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2022.902868/full#supplementary-material
References
1. Wang Z, Chen Z, Zhang L, Wang X, Hao G, Zhang Z, et al. Status of hypertension in china: results from the China Hypertension Survey, 2012-2015. Circulation. (2018) 137:2344–56. doi: 10.1161/CIRCULATIONAHA.117.032380
2. Song P, Zhang Y, Yu J, Zha M, Zhu Y, Rahimi K Rudan I, et al. Global prevalence of hypertension in children: a systematic review and meta-analysis. JAMA Pediatr. (2019) 173:1154–63. doi: 10.1001/jamapediatrics.2019.3310
3. Ataey A, Jafarvand E, Adham D, Moradi-Asl E. The relationship between obesity, overweight, and the human development index in World Health Organization Eastern Mediterranean Region Countries. J Prev Med Public Health. (2020) 53:98–105. doi: 10.3961/jpmph.19.100
4. Grace SG. Obesity: a sociological guide for health practitioners. Aust J Prim Health. (2020) 26:362–6. doi: 10.1071/PY20100
5. Kokubo Y, Iwashima Y. Higher blood pressure as a risk factor for diseases other than stroke and ischemic heart disease. Hypertension. (2015) 66:254–9. doi: 10.1161/HYPERTENSIONAHA.115.03480
6. Li Y, Teng D, Shi X, Teng X, Teng W, Shan Z, et al. The thyroid disorders is, diabetes epidemiological survey G changes in the prevalence of obesity and hypertension and demographic risk factor profiles in China over 10 years: two national cross-sectional surveys. Lancet Reg Health West Pac. (2021) 15:100227. doi: 10.1016/j.lanwpc.2021.100227
7. Green M, Arora K, Prakash S. Microbial medicine: prebiotic and probiotic functional foods to target obesity and metabolic syndrome. Int J Mol Sci. (2020) 21:2890. doi: 10.3390/ijms21082890
8. van Oort S, Beulens JWJ, van Ballegooijen AJ, Grobbee DE, Larsson SC. Association of cardiovascular risk factors and lifestyle behaviors with hypertension: a mendelian randomization study. Hypertension. (2020) 76:1971–9. doi: 10.1161/HYPERTENSIONAHA.120.15761
9. Wang Z, Zhao L, Huang Q, Hong A, Yu C, Xiao Q, et al. Traffic-related environmental factors and childhood obesity: A systematic review and meta-analysis. Obes Rev. (2021) 22 (Suppl. 1):e12995. doi: 10.1111/obr.12995
10. Bloemsma LD, Wijga AH, Klompmaker JO, Janssen NAH, Smit HA, Koppelman GH, et al. The associations of air pollution, traffic noise and green space with overweight throughout childhood: The PIAMA birth cohort study. Environ Res. (2019) 169:348–56. doi: 10.1016/j.envres.2018.11.026
11. Wallas A, Ekström S, Bergström A, Eriksson C, Gruzieva O, Sjöström M, et al. Traffic noise exposure in relation to adverse birth outcomes and body mass between birth and adolescence. Environ Res. (2019) 169:362–7. doi: 10.1016/j.envres.2018.11.039
12. de Bont J, Marquez S, Fernandez-Barres S, Warembourg C, Koch S, Persavento C, et al. Urban environment and obesity and weight-related behaviours in primary school children. Environ Int. (2021) 155:106700. doi: 10.1016/j.envint.2021.106700
13. van Kempen E, Babisch W. The quantitative relationship between road traffic noise and hypertension: a meta-analysis. J Hypertens. (2012) 30:1075–86. doi: 10.1097/HJH.0b013e328352ac54
14. Oftedal B, Krog NH, Pyko A, Eriksson C, Graff-Iversen S, Haugen M, et al. Road traffic noise and markers of obesity - a population-based study. Environ Res. (2015) 138:144–53. doi: 10.1016/j.envres.2015.01.011
15. Kupcikova Z, Fecht D, Ramakrishnan R, Clark C, Cai YS. Road traffic noise and cardiovascular disease risk factors in UK Biobank. Eur Heart J. (2021) 42:2072–84. doi: 10.1093/eurheartj/ehab121
16. Liang XH, Xiao L, Luo T, Xu P. Prevalence and risk factors of childhood hypertension from birth through childhood: a retrospective cohort study. J Hum Hypertens. (2020) 34:151–64. doi: 10.1038/s41371-019-0282-z
17. Group of China Obesity Task Force. [Body mass index reference norm for screening overweight and obesity in Chinese children and adolescents]. Zhonghua Liu Xing Bing Xue Za Zhi. (2004) 25:97–102. doi: 10.3760/j.issn:0254-6450.2004.02.003
18. Kapelko-Slowik K, Owczarek TB, Grzymajlo K, Urbaniak-Kujda D, Jazwiec B, Slowik M, et al. Elevated PIM2 gene expression is associated with poor survival of patients with acute myeloid leukemia. Leuk Lymphoma. (2016) 57:2140–9. doi: 10.3109/10428194.2015.1124991
19. Meng LH, Mi J, Cheng H, Hou DQ, Ding XY. Using waist circumference and waist-to-height ratio to access central obesity in children and adolescents [J]. Chi J Evidence-Based Pediatr. (2007) 2:245–52. doi: 10.3969/j.issn.1673-5501.2007.04.002
20. Fan H, Yan YK, Jie MI, Epidemiology DO. Updating blood pressure references for Chinese children aged 3-17 years. Chi J Hyperten. (2017) 25:428–35.
21. Liang X, Chen M, Qu P, Hao G, Huang Y, Chen J, et al. of Vitamin A and Vitamin D with hypertension in children: a case-control study. Int J Hypertens. (2018) 2018:9295147. doi: 10.1155/2018/9295147
22. Owens JA, Spirito A, McGuinn M. The Children's Sleep Habits Questionnaire (CSHQ): psychometric properties of a survey instrument for school-aged children. Sleep. (2000) 23:1043–51. doi: 10.1093/sleep/23.8.1d
23. Textor J, van der Zander B, Gilthorpe MS, Liskiewicz M, Ellison GT. Robust causal inference using directed acyclic graphs: the R package 'dagitty'. Int J Epidemiol. (2016) 45:1887–94. doi: 10.1093/ije/dyw341
24. Pyko A, Eriksson C, Oftedal B, Hilding A, Ostenson CG, Krog NH, et al. Exposure to traffic noise and markers of obesity. Occup Environ Med. (2015) 72:594–601. doi: 10.1136/oemed-2014-102516
25. Christensen JS, Raaschou-Nielsen O, Tjonneland A, Overvad K, Nordsborg RB, Ketzel M, et al. Road traffic and railway noise exposures and adiposity in adults: a cross-sectional analysis of the Danish diet, cancer, and health cohort. Environ Health Perspect. (2016) 124:329–35. doi: 10.1289/ehp.1409052
26. Eriksson C, Hilding A, Pyko A, Bluhm G, Pershagen G, Ostenson CG, et al. Long-term aircraft noise exposure and body mass index, waist circumference, and type 2 diabetes: a prospective study. Environ Health Perspect. (2014) 122:687–94. doi: 10.1289/ehp.1307115
27. Foraster M, Eze IC, Vienneau D, Schaffner E, Jeong A, Heritier H, et al. Long-term exposure to transportation noise and its association with adiposity markers and development of obesity. Environ Int. (2018) 121(Pt 1):879–89. doi: 10.1016/j.envint.2018.09.057
28. Christensen JS, Raaschou-Nielsen O, Tjønneland A, Nordsborg RB, Jensen SS, Sørensen TI, et al. Long-term exposure to residential traffic noise and changes in body weight and waist circumference: a cohort study. Environ Res. (2015) 143(Pt A):154–61. doi: 10.1016/j.envres.2015.10.007
29. Vrijheid M, Fossati S, Maitre L, Marquez S, Roumeliotaki T, Agier L, et al. Early-Life environmental exposures and childhood obesity: an exposome-wide approach. Environ Health Perspect. (2020) 128:67009. doi: 10.1289/EHP5975
30. Christensen JS, Hjortebjerg D, Raaschou-Nielsen O, Ketzel M, Sørensen TIA, Sørensen M, et al.. Pregnancy and childhood exposure to residential traffic noise and overweight at 7years of age. Environ Int. (2016) 94:170–76. doi: 10.1016/j.envint.2016.05.016
31. Weyde KV, Krog NH, Oftedal B, Magnus P, White R, Stansfeld S, et al. Longitudinal study of road traffic noise and body mass index trajectories from birth to 8 years. Epidemiology. (2018) 29:729–38. doi: 10.1097/EDE.0000000000000868
32. Zeeb H, Hegewald J, Schubert M, Wagner M, Dröge P, Swart E, et al. Traffic noise and hypertension - results from a large case-control study. Environ Res. (2017) 157:110–7. doi: 10.1016/j.envres.2017.05.019
33. Shin S, Bai L, Oiamo TH, Burnett RT, Weichenthal S, Jerrett M, et al. Association between road traffic noise and incidence of diabetes mellitus and hypertension in Toronto, Canada: a population-based cohort study. J Am Heart Assoc. (2020) 9:e013021. doi: 10.1161/JAHA.119.013021
34. Banerjee D, Das PP, Fouzdar A. Urban residential road traffic noise and hypertension: a cross-sectional study of adult population. J Urban Health. (2014) 91:1144–57. doi: 10.1007/s11524-014-9916-1
35. Xiong P, Liang X, Chen H, Chen L, Zuo L, Jing C, et al. Association between childhood neighborhood quality and the risk of cognitive dysfunction in Chinese middle-aged and elderly population: the moderation effect of body mass index. Front Aging Neurosci. (2021) 13:645189. doi: 10.3389/fnagi.2021.645189
36. Beheshti MH, Taban E, Samaei SE, Faridan M, Khajehnasiri F, Khaveh LT, et al. The influence of personality traits and gender on noise annoyance in laboratory studies. Personal Individual Diff . (2019):148:95–100. doi: 10.1016/j.paid.2019.05.027
37. van Kamp I, Simon S, Notley H, Baliatsas C, van Kempen E. Evidence relating to environmental noise exposure and annoyance, sleep disturbance, cardio-vascular and metabolic health outcomes in the context of IGCB (N): A scoping review of new evidence. Int J Environ Res Public Health. (2020) 17:3016. doi: 10.3390/ijerph17093016
38. Johannessen A, Bertelsen R, Real FG, Sigsgaard T, Franklin KA, Lindberg E, et al. Exposure to traffic pollution is related to daytime sleepiness and habitual snoring: Results from the RHINE study. Eur Resp J. (2016) 48:A4922. doi: 10.1183/13993003.congress-2016.PA4922
39. O'Dea JA, Dibley MJ, Rankin NM. Low sleep and low socioeconomic status predict high body mass index: a 4-year longitudinal study of Australian schoolchildren. Pediatr Obes. (2012) 7:295–303. doi: 10.1111/j.2047-6310.2012.00054.x
40. Sluggett L, Wagner SL, Harris RL. (2018). Sleep duration and obesity in children and adolescents. Can J Diabetes. (2019) 43:146–52. doi: 10.1016/j.jcjd.2018.06.006
41. Felso R, Lohner S, Hollody K, Erhardt E, Molnar D. Relationship between sleep duration and childhood obesity: Systematic review including the potential underlying mechanisms. NMCD. (2017) 27:751–61. doi: 10.1016/j.numecd.2017.07.008
42. DelRosso LM, Mogavero MP, Ferri R. Effect of sleep disorders on blood pressure and hypertension in children. Curr Hypertens Rep. (2020) 22:88. doi: 10.1007/s11906-020-01100-x
43. Evans GW, Lercher P, Meis M, Ising H, Kofler WW. Community noise exposure and stress in children. J Acoust Soc Am. (2001) 109:1023–7. doi: 10.1121/1.1340642
44. Miller AL, Lumeng JC. Pathways of association from stress to obesity in early childhood. Obesity. (2018) 26:1117–24. doi: 10.1002/oby.22155
45. Falkner B. The childhood role in development of primary hypertension. Am J Hypertens. (2018) 31:762–9. doi: 10.1093/ajh/hpy058
Keywords: transportation noise, obesity, hypertension, children, mediating effect
Citation: Liang X, Tang X, Liu M, Liang X, Chen L, Chen X, Zuo L, Ren Y and Hao G (2022) Associations of self-reported residential noise exposure with obesity and hypertension in children and adolescents. Front. Pediatr. 10:902868. doi: 10.3389/fped.2022.902868
Received: 23 March 2022; Accepted: 18 July 2022;
Published: 12 August 2022.
Edited by:
Fatima Cody Stanford, Massachusetts General Hospital and Harvard Medical School, United StatesReviewed by:
Benedicta Ngwenchi Nkeh-Chungag, Walter Sisulu University, South AfricaDolina Gencheva, Plovdiv Medical University, Bulgaria
Copyright © 2022 Liang, Tang, Liu, Liang, Chen, Chen, Zuo, Ren and Hao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Guang Hao, aGFvZ3VhbmcyMDE1QGhvdG1haWwuY29t
 Xiaohua Liang
Xiaohua Liang Xian Tang1
Xian Tang1 Li Chen
Li Chen Guang Hao
Guang Hao