- 1Division of Pediatric Critical Care Medicine, Department of Pediatrics, University of Washington School of Medicine, Seattle, WA, United States
- 2Division of Pediatric Bioethics and Palliative Care, Department of Pediatrics, University of Washington School of Medicine, Seattle, WA, United States
- 3Treuman Katz Center for Pediatric Bioethics, Seattle Children's Research Institute, Seattle, WA, United States
- 4Fred Hutchinson Cancer Research Center, University of Washington School of Medicine, Seattle, WA, United States
- 5Department of Anesthesiology and Pain Medicine, University of Washington School of Medicine, Seattle, WA, United States
- 6Department of Biobehavioral Nursing Science, College of Nursing, University of Illinois, Chicago, IL, United States
- 7Division of Pediatric Cardiothoracic Surgery, University of Washington School of Medicine, Seattle, WA, United States
- 8Division of Pediatric Critical Care Medicine, Department of Pediatrics, Vanderbilt University Medical Center, Nashville, TN, United States
- 9Center for Biomedical Ethics and Society, Vanderbilt University Medical Center, Nashville, TN, United States
Technological advancements and rapid expansion in the clinical use of extracorporeal life support (ECLS) across all age ranges in the last decade, including during the COVID-19 pandemic, has led to important ethical considerations. As a costly and resource intensive therapy, ECLS is used emergently under high stakes circumstances where there is often prognostic uncertainty and risk for serious complications. To develop a research agenda to further characterize and address these ethical dilemmas, a working group of specialists in ECLS, critical care, cardiothoracic surgery, palliative care, and bioethics convened at a single pediatric academic institution over the course of 18 months. Using an iterative consensus process, research questions were selected based on: (1) frequency, (2) uniqueness to ECLS, (3) urgency, (4) feasibility to study, and (5) potential to improve patient care. Questions were categorized into broad domains of societal decision-making, bedside decision-making, patient and family communication, medical team dynamics, and research design and implementation. A deeper exploration of these ethical dilemmas through formalized research and deliberation may improve equitable access and quality of ECLS-related medical care.
Introduction
“Almost every action within the medical setting either explicitly or implicitly contains two judgements, one ethical and one scientific, and there is constant interplay between what is technically possible and what is morally desirable” (1).
Although traditionally used in neonatology and pediatric medicine for acute respiratory failure, extracorporeal life support (ECLS) is now the standard of care for an expanding number of pediatric and adult medical conditions. ECLS is commonly deployed to allow recovery from potentially reversible conditions, such as acute respiratory distress syndrome (ARDS) and shock; as a bridge to decision, when prognosis is uncertain; as a rescue therapy during cardiopulmonary arrest that is unresponsive to initial resuscitation measures; and as a bridge to transplant or destination therapy with mechanical circulatory support (2–5). Over the last decade, exponential growth of ECLS utilization in adults (6, 7) has surpassed its utilization in children. As of March 2022, 92,389 adults and 79,604 children (age <18 years of age) were supported by ECLS with survival rates ranging from 49% (adults) to 65% (neonates) (8). The COVID-19 pandemic likely contributed to this expansion in the adult population, as 13,341 patients with ARDS secondary to SARS-CoV-2 infection have been managed with ECLS (8–10).
Rapid technological advancements and the exponential expansion of ECLS utilization, as exemplified by the SARS-CoV-2 pandemic, are generating an increasing number of ethical and societal considerations (11–16). Clinical and ethical guidance for the utilization of ECLS are often based on expert consensus, case series, and retrospective cohort analyses due to inherent challenges in prospective outcomes studies and randomized control trials in these populations (17, 18). Over the last decade, clinical guidelines (9, 19–21), position and opinion papers (2, 22–26), surveys of clinician perceptions (27–31), and discourse surrounding ethical considerations (32–36) have proliferated. Notably, explicit discussions regarding ethical considerations are often implied or excluded from these clinical guidelines, position statements, and surveys of clinician perceptions. Furthermore, thoughtful and detailed manuscripts that explicitly highlight general ethical principles often do not provide practical guidance for clinicians. Hence, these limitations in the current medical literature compel further exploration of complex ethical questions through additional empirical and normative research (2). Failure to address ethical implications associated with complex decision making in ECLS increases the risk of unnecessary and undesired burdens for patients, families, staff, and health care systems (37). In addition, institutional, regional and global variation in ECLS application may exacerbate already existing health care disparities (27, 38, 39).
Brief History and Description of ECLS
Since its introduction nearly fifty years ago, ECLS has provided life-support to over 170,000 patients globally (8). ECLS is based on John H. Gibbon's work beginning in the 1930s and culminating with the first successful extracorporeal cardiopulmonary bypass case in 1953 enabling surgeons to perform open-heart operations (7, 40). ECLS utilizes an extracorporeal blood pump coupled with a gas exchange unit to provide cardiopulmonary support for patients with severe cardiac and/or respiratory failure. Venovenous (VV) ECLS provides gas exchange and returns blood to a central vein or the right atrium for respiratory support alone. In contrast, venoarterial (VA) ECLS provides gas exchange and cardiovascular support by returning blood to a central artery for combined respiratory and circulatory support. ECLS is often conventionally referred to as ECMO (extracorporeal membrane oxygenation support). However, newer ECLS technologies do not utilize a “membrane oxygenator” leading to the adoption of the newer more inclusive term of ECLS (41).
Historically, the earliest clinical trial with ECLS failed to demonstrate improved survival in adults (42); however, improved outcomes were observed in neonatal and pediatric patients with respiratory or cardiac failure (43–46). Thus, over the subsequent few decades, ECLS was primarily used to support neonates and pediatric patients with acute respiratory and cardiac failure, including children following cardiac surgery. With improvements in technology and experience, indications for the utilization of ECLS have increased rapidly, and include children and adults with acute respiratory failure and shock, as a bridge to decision when prognosis is uncertain, as a bridge to heart and/or lung transplant, and in rescue of patients with cardiac arrest refractory to cardiopulmonary resuscitation (E-CPR) (3–5, 7, 47, 48). Medical conditions that were once absolute contraindications, such as organ failure following stem cell transplant and chimeric antigen T cell therapy (CAR-T), are now reconsidered for support with ECLS (28, 49). Previously the domain of quaternary care centers, technological advancements have led to an increased number and greater variety of types of centers to offer ECLS. When ECLS is not available at certain locations, mobile ECLS programs have allowed patients to be cannulated locally and transferred to specialized ECLS centers (50).
Outcomes following ECLS vary with patient age and indication for support, ranging from >90% survival in neonates with meconium aspiration syndrome, 65% for all pediatric ECLS indications, 46% in adults with ARDS, to 30% in adults following cardiac arrest (2, 6, 9, 51, 52). While overall survival rates for ECLS patients continue to modestly improve for both adults and children (52), utilization in increasingly complex conditions has led to a plateau in mortality rates for certain conditions, such as cardiac failure in children and neonates (53). When evaluating the potential risks and benefits of ECLS, risk of mortality and ECLS-associated morbidities should be assessed. Serious complications, including bleeding, infection, central nervous system injury, severe deconditioning, and acute kidney injury (54–57) are not uncommon. The impact and potential risk to other patients related to ECLS-associated resource utilization (e.g., intensive care nurses, intensive care beds, blood products) also may need to be considered in the global calculus of risk and benefit of ECLS utilization.
Clinical Cases
As ECLS technology advances at a rapid pace, there are few technical limitations to offering ECLS as a potentially life saving intervention—therefore, “we can.” However, within the context of a wide range of mortality rates, risks for severe morbidities, limited outcome data, and clinician ethical duty to save lives, ECLS clinicians are often faced with the extremely difficult medical and moral decision—“should we?” Unfortunately, there is little ethical guidance to assist bedside clinicians in making these complex decisions.
The following hypothetical cases, based on an amalgam of actual clinical cases, highlight several important ethical dilemmas that arise in the provision of ECLS.
Case 1
Lily (pseudonym) was a 4-year-old girl found 90 minutes after being submerged in a cold-water lake. Rescuers initiated cardiopulmonary resuscitation at the scene. CPR (cardiopulmonary resuscitation) was provided for 30 minutes en route to the nearest community hospital with return of spontaneous circulation upon arrival. An adult cardiothoracic surgeon had recently established an adult ECLS program at this community hospital. Based on the possibility of neurologic recovery following cold water drowning, the medical team cannulated Lily onto ECLS despite minimal evidence of neurological function. Open chest cannulation was performed given that only adult-size ECLS cannulas were available. The child was then transported to a nearby quaternary academic pediatric center using a portable ECLS team. After rewarming to normothermia, Lily's physical examination revealed lack of neurologic function except for abnormal spontaneous respirations. Head CT revealed diffuse cerebral edema with loss of gray-white matter differentiation, concerning for devastating and likely irreversible neurologic injury. Based on the low likelihood of any neurologic recovery, the family and the medical team jointly decided to compassionately withdraw life support. Lily's parents wished to pursue organ donation and found significant meaning out of this tragedy when her liver and kidneys were successfully transplanted following a circulatory determination of death (DCDD) protocol.
In this case, urgent medical decision making is complex and challenging when the potential risks and benefits are unpredictable, and there is substantial prognostic uncertainty. ECLS did not provide direct benefit to the child, however the utilization of this intense resource provided benefit to the family and society. The family had additional time to grieve the loss of their child and were given the opportunity to graciously offer the gift of organ donation.
Case 2
Betty (pseudonym) is a previously healthy obese unvaccinated 22-year-old woman who was critically ill with severe acute respiratory distress syndrome (ARDS) secondary to SARS-CoV-2 pneumonia complicated by secondary bacterial infection. Despite maximal support with mechanical ventilation, her oxygenation remained quite poor, and she was placed on venovenous ECLS on hospital day five. Due to limited clinical staff and ECLS pumps at the adult hospital during the pandemic, she was transferred from an adult facility to a pediatric ECLS center using a mobile ECLS transport team. While she remained on ECLS, the pediatric intensive care unit (PICU) reached capacity, and critically ill children were diverted to other community-based facilities. After four weeks of ongoing support via ECLS, she was ultimately decannulated. Due to severe deconditioning and lung disease, she remained in the PICU for an additional three weeks during which time a tracheotomy was performed, and she was transitioned to a portable ventilator.
This case highlights the challenges and consequences of allocation of resource intense therapies during a pandemic. While rapid advancements in technology allow for portable ECLS, transferring this young adult patient to a pediatric facility consequently impacted the ability of the institution to provide specialized pediatric care to other pediatric patients.
Recommendations For a Research Agenda
Proactive and explicit exploration through collaboration and research of ethical considerations that arise in clinical cases like these may mitigate potential risks and promote: (1) respect for the well-being and autonomy of patients, families, and staff; (2) optimization of patient outcomes while minimizing undue burdens for patients and families; and (3) responsible, equitable, and fair allocation of resources. Navigating complex and challenging questions that arise in ECLS will hopefully lead to improved quality of patient care through a better understanding of the ethical and societal considerations.
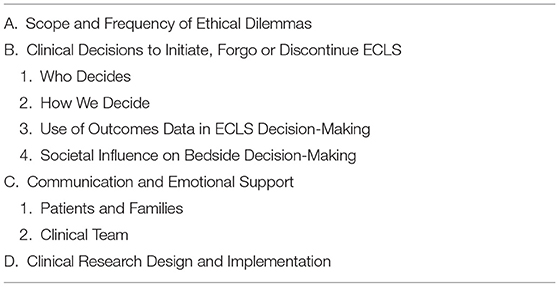
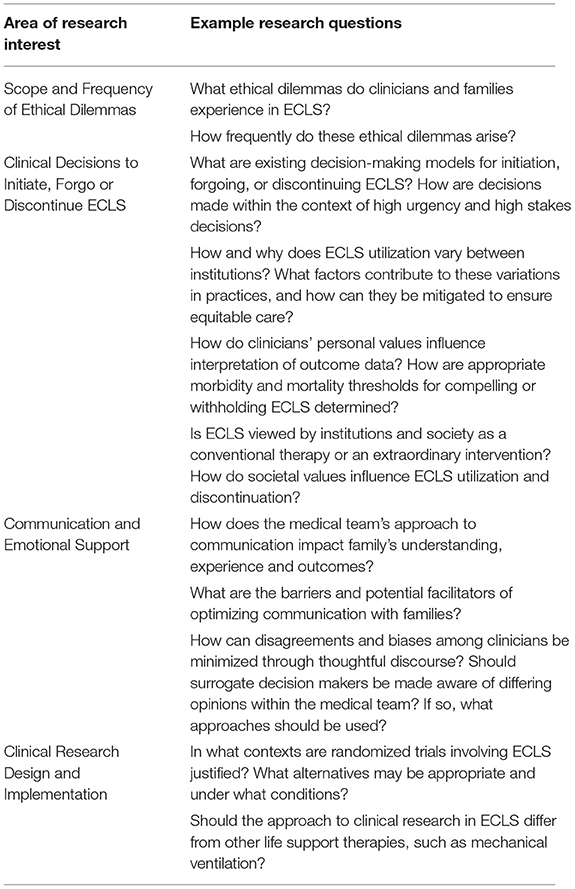
To develop a research agenda to inform ethical guidance for clinicians and institutions in the utilization of ECLS, a multi-disciplinary team of pediatric specialists in ECLS, critical care, cardiothoracic surgery, palliative care, and bioethics convened at a single academic institution. Using an iterative consensus process, a broad range of research questions were collected and refined by the group over a series of monthly meetings for approximately 18 months. The broad list was refined by removing duplicates and then selecting questions according to the following criteria: (1) frequency of occurrence in ECLS; (2) uniqueness to ECLS; (3) urgency; (4) feasibility to study; and (5) potential to advance the practice of ECLS and improve quality of patient care. To create the research agenda, refined questions were categorized into the following themes: (1) scope and frequency of ethical dilemmas involving ECLS; (2) clinical decisions and ethical guidance to initiate, forgo, or discontinue ECLS; (3) approaches to optimize communication with and provide emotional support for families and clinical team members; and (4) research design and implementation in ECLS (Tables 1, 2).
A. Scope and Frequency of Ethical Dilemmas
Ethical dilemmas are common in the provision of ECLS, as highlighted by the COVID-19 pandemic. However, few empirical data describe the nature and frequency of ethical issues that arise in ECLS. In order to identify solutions, the problems need to be clearly defined.
• What ethical dilemmas do clinicians and families experience in ECLS and how frequently do these arise?
B. Clinical Decisions and Ethical Guidance to Initiate, Forgo, or Discontinue ECLS
ECLS decision-making is complex and influenced by a myriad of interacting forces at the bedside, the institution and in society. Decisions may be fraught with challenges and complexity due to the combination of several factors: (1) limited time frame for decision-making; (2) life and death circumstances; (3) large, multidisciplinary clinical teams with potential for differing opinions; (4) prognostic uncertainty; (5) potential for serious complications; (6) increasingly heterogenous patient populations with greater complexity in which ECLS is utilized; and (7) national and international guidelines based on expert opinion rather than clinical data. These challenging circumstances often lead to variability in decisions made by individual or relatively small groups of clinicians potentially resulting in the inconsistent use of ECLS (e.g., variability among diagnoses, patient populations, and geographic regions) (27, 29, 38, 39). As a complex technology requiring a multi-disciplinary team, the quality of ECLS delivered may be variable among centers. To determine if access to high quality ECLS is distributed justly, these forces and the extent of their influence may be explored through the following questions:
1. Who Decides
• What are existing decision-making models for ECLS and how do they lead to variability in use? What does shared medical decision making look like within the context of high urgency and high stakes decisions?
• What impact does including and excluding various clinical team members from the decision-making process have on: complexity of the decision-making process, quality of medical care, utilization of ECLS, job satisfaction of clinicians, and family support?
• What role does ECLS-specific training of clinical team members have on the decision-making process?
• Should ECLS ever be initiated or withdrawn against a family's wishes? If so, what are the morbidity and mortality thresholds for such decisions?
2. How We Decide
• Do clinicians ever limit the use of ECLS based on perceived ethical barriers that are not empirically substantiated? If so, what are the perceived ethical barriers, and how should they be addressed?
• What biases and assumptions exist among the clinical team, institutions, and organizations that may impact how decisions are made?
• How are bedside decisions influenced by clinical outcome data, patient comorbidities, and institutional availability of ECLS resources?
• Why and how does ECLS utilization (initiation, forgoing, withdrawing) vary between institutions or between clinical teams within an institution? What factors contribute to these variations in practices, and how can they be mitigated to ensure equitable care?
• What factors influence the decision to end life by withdrawing ECLS? How are these decisions made? How are conflicting opinions resolved?
• How does the urgency of the clinical situation impact clinician decision-making? How does this urgency impact the process of obtaining informed consent from patients and their surrogates?
• What role, if any, should ECLS center volume and experience play in determining which patient diagnoses are supported by ECLS?
• How should relatively scarce ECLS equipment and staff be allocated during conventional, contingency, and crisis standards of care?
• Are there clinical situations when E-CPR should be considered obligatory or prohibited? If so, how are these clinical situations determined and assessed?
• What is the appropriate level of training and experience needed to determine ECLS candidacy and initiate support? How does the advent of mobile ECLS influence these decisions?
3. Use of Outcomes Data in ECLS Decision-Making
• Are current outcome data adequate to drive or support decision-making in ECLS? What additional outcome data would improve decision-making?
• How do clinicians' personal values influence interpretation of outcome data and how does this lead to variability in use of ECLS?
• How do we determine appropriate morbidity and mortality thresholds for compelling or withholding ECLS?
• Are outcome data commonly used in decision making or are decisions based primarily on clinical experiences? How accurately do clinicians prognosticate?
• What are the most important long-term outcomes (e.g., physical and psychologic health, cognitive function, social function, quality of life, development and educational) for survivors of ECLS and their families? How should these outcomes influence bedside decision-making in ECLS?
4. Societal Influence on Bedside Decision-Making
• Is ECLS viewed by institutions and society as a conventional therapy (i.e., obligatory) or as an extraordinary intervention (i.e., not obligatory) or both? How does this view influence ECLS utilization at the bedside?
• How do societal values and beliefs (e.g., values and perceptions of physical and cognitive disabilities, cultural views about life and death, allocation of health care spending) influence the use of ECLS?
• Does society have an obligation to ensure equitable access to ECLS for all patients? For example, can individual institutions refuse to offer ECLS without obligation to transfer or should referral networks be required? Should ECLS centers of excellence be required to have mobile ECLS teams to improve equitable access?
• At the societal level, what factors should be included in the calculation of the costs and benefits [e.g., quality or disability-adjusted life years (QALY, DALY), real costs, use of scarce resources such as highly specialized personnel or intensive care beds] of ECLS? How should these factors be prioritized and who determines the prioritization paradigm? How should these analyses affect bedside decision-making?
• What role should ECLS play in organ donation for patients declared deceased based on neurologic criteria? Should ECLS be utilized to support organ donors who are declared deceased after circulatory death? What are the ethical implications of these practices?
• How does systemic racism potentially exacerbate health care disparities when considering utilization of ECLS?
C. Communication and Emotional Support
A paucity of literature exists describing communication related to ECLS. The following questions seek to measure the quality of communication and to explore the influence that communication content and style has on patients and families and within the medical team.
1. Patients and Families
Communicating with patients and their families can be difficult in the critical care environment, especially under the stressful circumstances that often surround ECLS (58). Effective communication with ECLS patients and their families is essential for: (1) eliciting patient and family values, preferences, and needs; (2) optimizing patient and surrogate provided permission and informed consent processes; and (3) promoting beneficial psycho-social outcomes. The focus of the following questions is to understand how clinicians communicate with patients and families around ECLS, both assessing the quality of communication and identifying ways to improve communication with patients and their families:
• How do clinicians communicate with families regarding risks, benefits, alternative options, and outcomes of ECLS prior to initiating ECLS and during support? What are barriers and potential facilitators of optimal communication?
• How does the urgency of the clinical situation impact communication with families?
• Is the conventional model for “informed consent” applicable to the initiation of ECLS? Should informed consent be obtained for every ECLS encounter? Are there any modifications to the informed consent process that may improve communication and guide decision making for families?
• What is the optimal approach to support the family cognitively and emotionally during the decision-making process to initiate ECLS?
• How can clinicians balance hope and realistic expectations during communication with families when ECLS is initiated and throughout the course of ECLS?
• How does language used by clinicians impact the experiences of families and their decisions related to ECLS? How do clinicians' views of appropriateness of ECLS use influence their language? For families who speak a language other than English (or other than the primary language of the medical team), how does the use of language interpreters impact the quality and accuracy of communication?
• What is the role of cultural navigators when navigating complex decisions regarding ECLS? How are cultural barriers that may arise in complex decision making identified and mitigated?
• What is the balance between resource utilization and family support when a family requests to continue ECLS after the recommendation has been made to discontinue life support?
• How should clinicians optimally provide psycho-social support for patients and their families both acutely and long-term when ECLS is utilized?
2. Clinical Team
ECLS requires a collaborative and multidisciplinary approach to patient care. Guidelines for ECLS based on expert opinion and experience rather than on clinical data may lead to disparate opinions among clinical team members. Unresolved discord among clinical team members may negatively impact quality of care and patient safety. Understanding and improving communication among clinical team members may help to reconcile these differences. Optimal communication may limit intramural discord, reduce individual moral distress, and thereby improve the quality of patient care. Understanding of the impact of communication among the clinical team requires investigation.
• How does verbal and non-verbal language used by ECLS teams bias the institutional culture surrounding the “appropriate” use of ECLS? How do institutional cultures and biases affect decision-making in ECLS?
• How does the interaction and communication among a diverse clinical team impact the experience of patients and their families, team performance, and clinical outcome?
• How should team leaders manage dissent among clinical team members?
• How does a lack of consensus among clinical team members affect the quality of patient care, patient emotional well-being, family members, clinical team, unit morale, and other unit patients?
• Should parents and/or surrogates be made aware of differing opinions within the clinical team? If so, what approach should be used?
D. Clinical Research Design and Implementation
Research in ECLS may be ethically challenging due to the complexity and intensity of the clinical circumstances. Additionally, because ECLS clinicians and researchers are typically one and the same, ambiguity between clinical and research practices of ECLS may exist. These overlapping relationships and the clinical context may unduly influence family expectations, decision-making, and participation in clinical research. Furthermore, designing optimal research studies to advance ECLS may be difficult given the life-threatening context, heterogeneity and complexity of clinical diagnoses, lack of standardized processes, and diversity of clinical opinions about effectiveness. The following questions should be addressed to optimize research practices in ECLS:
• How do the clinical context and provider relationships influence families' expectations, understanding, and willingness to participate in ECLS research?
• How do families experience participation in ECLS research?
• How do researchers ensure that patients and families are optimally protected during ECLS research and improve their experiences?
• How do provider views about benefit or futility of ECLS in a particular population influence provider endorsement of or participation in research studies in ECLS?
• In what contexts are randomized trials involving ECLS justified? What alternatives may be appropriate and under what conditions?
• Should the approach to clinical research in ECLS differ from other “life support therapies”?
Conclusions
The Seattle Ethics in ECLS Consortium identified and prioritized important ethical questions that warrant further empirical and normative research in the domains of societal decision-making, bedside decision-making, patient/family communication, medical team dynamics, and research ethics. Identifying ethical considerations in the delivery of ECLS is an initial step toward: (1) better understanding the ethical dilemmas encountered, (2) developing approaches to address these ethical dilemmas, and ultimately (3) improving the quality of medical care provided and support for families when utilizing ECLS.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary materials, further inquiries can be directed to the corresponding author/s.
Author Contributions
ML-N founded and led the SEE Consortium and conceptualized the initial manuscript. ML-N and JC co-facilitated the SEE Consortium discussions to develop the ECLS research agenda and drafted, revised, and approved the final manuscript as submitted. JC and JD performed background literature searches. HB, EBo, TB, JD, AD, DM, JR, JT, and BW all participated in the SEE Consortium, vetted the research questions, edited and approved the final manuscript. EBe vetted the research questions, edited and approved the final manuscript. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We would like to acknowledge Helene Starks PHD MPH, Ross Hays MD, and Rob Mazor MD, three additional members of the SEE Consortium, who contributed to the development of the questions for this research agenda. We would also like to acknowledge and honor all the patients and their families whose lives have been touched by ECLS while in our care. We are forever grateful for the opportunity to share their journeys, listen to their narratives, and learn from their experiences so we can provide the highest quality of care for our future patients and their families.
References
1. Moros DA, Rhodes R, Baumrin B, Strain JJ. Thinking critically in medicine and its ethics: relating applied science and applied ethics. In: Almond B, Hill D, editors. Applied Philosophy. London: Routledge (1987). p. 229–43. doi: 10.1111/j.1468-5930.1987.tb00220.x
2. DellaVolpe J, Barbaro RJ, Cannon JW, Fan E, Greene WR, Gunnerson KJ, et al. Joint SCCM-ELSO Task Force position paper on the role of the intensivist in the initiation and management of extracorporeal membrane oxygenation. Crit Care Med. (2020) 48:838–46. doi: 10.1097/CCM.0000000000004330
3. Hoetzenecker K, Donahoe L, Yeung JC, Azad S, Fan E, Ferguson ND, et al. Extracorporeal life support as a bridge to lung transplantation-experience of a high volume transplant center. J Throacic Cardiovasc Surg. (2018) 155:1316–28. doi: 10.1016/j.jtcvs.2017.09.161
4. Nasir B, Klapper J, Harwig M. Lung transplant from ECMO: Current results and predictors of post-transplant mortality. Curr Transplanation Rep. (2021) 8:140–50. doi: 10.1007/s40472-021-00323-4
5. Ouweneel DM, Schotborgh JV, Limpens J, Sjauw KD, Engstrom AE, Lagrand WK, et al. Extracorporeal life support during cardiac arrest and during cardiogenic shock: a systematic review and meta-analysis. Intens Care Med. (2016). 42:1922–34. doi: 10.1007/s00134-016-4536-8
6. Friedrichson B, Mutlak H, Zacharowski K, Piekarski F. Insight into ECMO, mortality, and ARDS: a nationwide analysis of 45,647 ECMO runs. Critical Care. (2021) 25:38. doi: 10.1186/s13054-021-03463-2
7. Lescouflair T, Figura R, Tran A, Kilic A. Adult veno-arterial extracorporeal life support. J Thoracic Diseases. (2018) 10:S1811–8. doi: 10.21037/jtd.2018.01.25
8. Extracorporeal Life Support Organization (ELSO). ELSO live registry dashboard of ECMO patient data. (2022). Available online at: https://www.elso.org (accessed March 9, 2022).
9. Badulak J, Velia Antonini M, Stead CM, Shekerdemian L, Raman L, Paden ML, et al. Extracorporeal membrane oxygenation for COVID-19: updated 2021 guidelines from the extracoporporeal life support organization. ASAIO J. (2021) 67:485–95. doi: 10.1097/MAT.0000000000001422
10. MacGregor RM, Antiel RM, Najaf T, Said AS, Warner BW, Raval MV, et al. Extracorporeal membrane oxygenation for pediatric patients with coronavirus disease 2019-related illness. Pediatr Crit Care Med. (2020) 21:893–7. doi: 10.1097/PCC.0000000000002432
11. Brodie D, Abrams D, MacLaren G, Brown CE, Evans L, Barbaro RP, et al. ECMO during respiratory pandemics: past, present, and future. AJRCCM. (2022). doi: 10.1164/rccm.202111-2661CP [Epub ahead of print].
12. Dao B, Savulescu J, Suen JY, Fraser JF, Wilkinson DJC. Ethical factors determining ECMO allocation during the COVID-19 pandemic. BMC Med Ethics. (2021) 22:70. doi: 10.1186/s12910-021-00638-y
13. Piscitello GM, Siegler M, Parker WF. Ethics of extracorporeal membrane oxygenation under conventional and crisis standards of care. J Clin Ethics. (2022) 33:13–22.
14. Srinivas G, Maanasa R, Meenakshi M, Adailkalam JM, Seshayyan S, Muthuvel T. Ethical rationing of healthcare resources during COVID-19 outbreak: review. Ethics Med Public Health. (2021) 16:100633. doi: 10.1016/j.jemep.2021.100633
15. Supady A, Badulak J, Evans L, Curtis JR, Brodie D. Should we ration extracorporeal membrane oxygenation during the COVID-19 pandemic? Lancet Respir Med. (2021) 9:326–8. doi: 10.1016/S2213-2600(21)00131-4
16. Van Beusekom M,. Study: 90% of young ECMO-eligbile COVID patients at a US hospital died amid rationing. Center for Infectious Disease Research Policy (CIDRAP). (2022). Available online at: https://www.cidrap.umn.edu/news-perspective/2022/02/study-90-young-ecmo-eligible-covid-patients-us-hospital-died-amid-rationing (accessed March 9, 2022).
17. Bartlett RH. Clinical research in acute fatal illness: lessons from extracorporeal membrane oxygenation. J Intens Care Med. (2014) 1:10. doi: 10.1177/0885066614550278
18. Tramm R, Ilic D, Davies AR, Pellegrino VA, Rmoero L, Hodgson C. Extracorporeal membrane oxygenation for critically ill adults. Cochrane Database Syst Rev. (2015) 1:CD010381. doi: 10.1002/14651858.CD010381.pub2
19. Brodie D, Slutsky AS, Combes A. Extracorporeal life support for adults with respiratory failure and related indications: A review. JAMA. (2019) 322:557–68. doi: 10.1001/jama.2019.9302
20. Gerall C, Cheung EW, Klein-Cloud R, Kreines E, Brewer M, Middlesworth W. Allocation of resources and development of guidelines for extracorporeal membrane oxygenation (ECMO): experience from a pediatric center in the epicenter of the COVID-19 pandemic. J Pediatr Surg. (2020) 55:2548–54. doi: 10.1016/j.jpedsurg.2020.08.015
21. Shekar K, Badulak J, Peek G, Boeken U, Dalton HJ, Arora L, et al. Extracorporeal life support organization coronavirus disease 2019 interim guidelines: a consensus document from an international group of interdisciplinary extracorporeal membrane oxygenation providers. ASAIO J. (2020) 66:707–21. doi: 10.1097/MAT.0000000000001193
22. Abrams D, Garan R, Abdelbary A, Bacchetta M, Bartlett RH, Beck J, et al. Position paper for the organization of ECMO programs for cardiac failure in adults. Intens Care Med. (2018) 44:717–29. doi: 10.1007/s00134-018-5064-5
23. Combes A, Brodie D, Bartlett R, Brochard L, Brower R, Conrad S, et al. Position paper for the organziation fo extracorporeal membrane oxygenation programs for acute respiratory failure in adult patients. Am J Respir Crit Care Med. (2014) 190:488–96. doi: 10.1164/rccm.201404-0630CP
24. Brodie D, Curtis JR, Vincent JL, Bakker J, Brown CR, Creteur J, et al. Treatment limitations in the era of ECMO. Lancet Respir Med. (2017) 5:769–70. doi: 10.1016/S2213-2600(17)30263-1
25. Erickson S. Extra-corporeal membrane oxygenation in paediatric acute respiratory distress syndrome: overrated or underutilized? Ann Trans Med. (2019). 7:512. doi: 10.21037/atm.2019.09.27
26. Lasa JJ, Jain P, Raymond TT, Minard CG, Topjian A, Nadkarni V, et al. Extracorporeal cardiopulmonary resuscitation in the pediatric cardiac population: in search of a standard of care. Pediatr Crit Care Med. (2018) 19:125–30. doi: 10.1097/PCC.0000000000001388
27. Abrams D, Pham T, Burns KEA, Combes A, Curtis JR, Mueller T, et al. Practice patterns and ethical considerations in the management of venovenous extracorporeal membrane oxygenation patients: an international survey. Crit Care Med. (2019). 47:1346–55. doi: 10.1097/CCM.0000000000003910
28. Ghafoor S, Fan K, Di Nardo M, Talleur AC, Saini A, Poetera RM, et al. Extracorporeal membrane oxygenation candidacy in pediatric patients treated with hematopoietic stem cell transplant and chimeric antigen receptor T-cell therapy: an international survey. Front Oncol. (2021) 11:798236. doi: 10.3389/fonc.2021.798236
29. Kuo KW, Barabar RP, Gadepalli SK, Davis MM, Bartlett RH, Odetola FO. Should extracorporeal membrane oxygenation be offered? An International Survey J Pediatr. (2017) 182:107–13. doi: 10.1016/j.jpeds.2016.12.025
30. Nguyen D-A, De Mul A, Hoskote AU, Cogo P, da Cruz EM, Erickson S, et al. Factors associated with inititation of extracorporeal cardiopulmonary resuscitation in the pediatric population: an international survey. ASAIO J. (2021) 68:413–18. doi: 10.1097/MAT.0000000000001495
31. Piscitello GM, Bermea RS, Stokes JW, Gannon WD, Kanelidis AJ, Konopka M, et al. Clinician ethical perspectives on extracorporeal membrane oxygenation in practice. Amer J Hospice Palliat Med. (2021) 39:659–66. doi: 10.1177/10499091211041079
32. Abrams DC, Prager K, Blinderman CD, Burkart KM, Brodie D. Ethical dilemmas encountered with the use of extracorporeal membrane oxygenation in adults. Chest. (2014) 145:876–82. doi: 10.1378/chest.13-1138
33. Bein T, Brodie D. Understanding ethical decisions for patients on extracorporeal life support. Intens Care Med. (2017) 43:1510–11. doi: 10.1007/s00134-017-4781-5
34. Enumah ZO, Carrese J, Choi CW. The ethics of extracorporeal membrane oxygenation: revisiting the principles of clinical bioethics. Ann Thorac Surg. (2021) 112:61–7. doi: 10.1016/j.athoracsur.2020.08.045
35. Kirsch R, Munson D. Ethical and end of life considerations for neonates requiring ECMO support. Semin Perinatol. (2018) 42:129–37. doi: 10.1053/j.semperi.2017.12.009
36. Schou A, Molgaard J, Anderson LW, Holm S, Sorenson M. Ethics in extracorporeal life support: a narrative review. Critical Care. (2021) 25:256. doi: 10.1186/s13054-021-03689-0
37. Emanuel E, Persad G, Upshur R, Thome B. Fair allocation of scarce medical resources in the time of COVID-19. NEJM. (2020) 382:2049–55. doi: 10.1056/NEJMsb2005114
38. Chan T, Di Gennaro J, Farris RW, Radman M, McMullan DM. Racial and ethical variation in pediatric cardiac extracorporeal life support survival. Crit Care Med. (2017) 45:670–80. doi: 10.1097/CCM.0000000000002246
39. Olsen J, Tjoeng Y-L, Friedland-Little J, Chan T. Racial disparities in hospital mortality among pediatric cardiomyopathy and myocarditis patients. Pediatr Cardiol. (2021) 42:59–71. doi: 10.1007/s00246-020-02454-4
40. Hill JD. Part I. The development of the first successful heart-lung machine. Ann Thorac Surg. (1982) 34:337–41. doi: 10.1016/S0003-4975(10)62507-6
41. Conrad SA, Broman LM, Taccone FS, Lorusso R, Malfertheiner MV, Pappalardo F, et al. The extracorporeal life support organization Maastricht Treaty for nomenclature in extracorporeal life support. A position paper of the Extracorporeal Life Support Organization. Amer J Respir Crit Care Med. (2018) 198:447–51. doi: 10.1164/rccm.201710-2130CP
42. Zapol WM, Snider MT, Hill JD, Fallat RJ, Bartlett RH, Edmunds LH, et al. Extracorporeal membrane oxygenation in severe acute respiratory failure. A randomized prospective study. JAMA. (1979) 242:2193–6. doi: 10.1001/jama.242.20.2193
43. Bartlett RH, Gazzaniga AB, Huxtable RF, Schippers HC, O'Connor MJ, Jeffries MR. Extracorporeal circulation (ECMO) in neonatal respiratory failure. J Thorac Cardiovasc Surg. (1977) 74: 826–33. doi: 10.1016/S0022-5223(19)41180-X
44. Bartlett RH, Gazzaniga AB, Jefferies MR, Huxtable RF, Haiduc NJ, Fong SW. Extracorporeal membrane oxygenation (ECMO) cardiopulmonary support in infancy. Trans Am Soc Artif Intern Organs. (1976) 22:80–93.
45. Lequier L. Extracorporeal life support in pediatric and neonatal critical care: a review. J Intensive Care Med. (2004) 19:243–58. doi: 10.1177/0885066604267650
46. Moler FW, Custer JR, Bartlett RH, Palmisano JM, Akingbola O, Taylor RP, et al. Extracorporeal life support for severe pediatric respiratory failure: an updated experience 1991-1993. J Pediatr. (1994) 124:875–80. doi: 10.1016/S0022-3476(05)83174-9
47. Workman JK, Bailly DK, Reeder RW, Dalton HJ, Berg RA, Shanley TP, et al. Risk factors for mortality in refractory pediatric septic shock support with extracorporeal life support. ASAIO J. (2020) 66:1152–60. doi: 10.1097/MAT.0000000000001147
48. De Mul A, Nguyen D-A, Doell C, Perez M-H, Cannizzaro V, Karam O. Prognostic evaluation of mortality after pediatric resuscitation assisted by extracorporeal life support. J Pedatri Intensive Care. (2019) 8:57–63. doi: 10.1055/s-0038-1667012
49. Steppan DA, Coleman RD, Viamonte HK, Hanson SJ, Carroll MK, Klein OR, et al. Outcomes of pediatric patients with oncologic disease or following hematopoietic stem cell transplant supported on extracorporeal membrane oxygenation: the PEDECOR experience. Pediatri Blood Cancer. (2020) 67:e28403. doi: 10.1002/pbc.28403
50. Felix Ehrentraut S, Schroll B, Lenkeit S, Ehrentraut H, Bode C, Kreyer S, et al. Interprofessional two-man team approach for interhospital transport of ARDS-patients under extracorporeal membrane oxygenation: a 10 years retrospective cohort study. BMC Anesthesiol. (2019) 19:19. doi: 10.1186/s12871-019-0687-9
51. Peterec SM, Bizzarro MJ, Mercurio M. Is extracorporeal membrane oxygenation for a neonate ever ethically obligatory? J Pediatr. (2018) 195:297–301. doi: 10.1016/j.jpeds.2017.11.018
52. Sanaiha Y, Khoubian JJ, Williamson CG, Aguayo E, Dobaria V, Srivastava N, et al. Trends in mortality and cost of pediatric extracorporeal life support. Pediatrics. (2020) 146:e20193564. doi: 10.1542/peds.2019-3564
53. Mahmood B, Newton D, Pallotto EK. Current trends in neonatal ECMO. Semin Perinatol. (2018) 42:80–8. doi: 10.1053/j.semperi.2017.12.003
54. Barrett CS, Bratton SL, Salvin JW, Laussen PC, Rycus PT, Thiagarajan RR. Neurological injury after extracorporeal membrane oxygenation to aid pediatric cardiopulmonary resuscitation. Pediatri Crit Care Med. (2009) 10:445–51. doi: 10.1097/PCC.0b013e318198bd85
55. Brunetti MA, Gaynor JW, Retzloff LB, Lehrich JL, Banerjee M, Amula V, et al. Characteristics, risk factors, and outcomes of extracorporeal membrane oxygenation use in pediatric cardiac intensive care units: a report from the PC4 registry. Pediatri Crit Care Med. (2018) 19:544–52. doi: 10.1097/PCC.0000000000001571
56. Madderom MH, Schiller RM, Gischler SJ, van Heijst AFJ, Tibboel D, Aarsen FK, et al. Growing up after critical illness: verbal, visual-spatial, and working memory problems in neonatal extracorporeal membrane oxygenation. Crit Care Med. (2016) 44:1182–90. doi: 10.1097/CCM.0000000000001626
57. Sadhwani A. Neurocognitive deficits in adolescent survivors of neonatal extracorporeal membrane oxygenation: the evidence unfolds. Crit Care Med. (2016) 44:1243–44. doi: 10.1097/CCM.0000000000001725
Keywords: critical care, ethics, extracorporeal life support (ECLS), extracorporeal membrane oxygenation (ECMO), research, communication
Citation: Clark JD, Baden HP, Berkman ER, Bourget E, Brogan TV, Di Gennaro JL, Doorenbos AZ, McMullan DM, Roberts JS, Turnbull JM, Wilfond BS, Lewis-Newby M and Seattle Ethics in ECLS (SEE) Consortium (2022) Ethical Considerations in Ever-Expanding Utilization of ECLS: A Research Agenda. Front. Pediatr. 10:896232. doi: 10.3389/fped.2022.896232
Received: 14 March 2022; Accepted: 26 April 2022;
Published: 19 May 2022.
Edited by:
Melania M. Bembea, Johns Hopkins University, United StatesReviewed by:
Ahmed S. Said, Washington University in St. Louis, United StatesHitesh Singh Sandhu, University of Tennessee Health Science Center (UTHSC), United States
Copyright © 2022 Clark, Baden, Berkman, Bourget, Brogan, Di Gennaro, Doorenbos, McMullan, Roberts, Turnbull, Wilfond, Lewis-Newby and Seattle Ethics in ECLS (SEE) Consortium. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jonna D. Clark, am9ubmEuY2xhcmtAc2VhdHRsZWNoaWxkcmVucy5vcmc=
 Jonna D. Clark
Jonna D. Clark Harris P. Baden1
Harris P. Baden1 Emily R. Berkman
Emily R. Berkman Thomas V. Brogan
Thomas V. Brogan Mithya Lewis-Newby
Mithya Lewis-Newby and Seattle Ethics in ECLS (SEE) Consortium
and Seattle Ethics in ECLS (SEE) Consortium