- 1College of Health Sciences, Debre Tabor University, Debre Tabor, Ethiopia
- 2College of Health Sciences, Woldia University, Woldia, Ethiopia
- 3School of Public Health, The University of Queensland, Brisbane, QLD, Australia
- 4School of Health Sciences, College of Medicine and Health Sciences, Bahir Dar University, Bahir Dar, Ethiopia
- 5St. Paul’s Hospital, Addis Ababa, Ethiopia
- 6College of Medicine and Health Sciences, Wollo University, Dessie, Ethiopia
- 7College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Background: High neonatal mortality rates continue to be a major public health issue in Ethiopia. Despite different maternal and neonatal care interventions, neonatal mortality in Ethiopia is at a steady state. This could be due to the low utilization of neonatal checkups. Thus, nationally assessing the level and predictors of postnatal checkups could provide important information for further improving neonatal healthcare services.
Materials and Methods: A secondary data analysis of the 2016 Ethiopia Demographic and Health Survey (EDHS) was performed on 7,586 women who had live births in the 2 years before the survey. All variables with a p-value of ≤0.25 in the bivariable analysis were entered into the final model for multivariable analysis, and the level of statistical significance was declared at a P-value of <0.05.
Results: According to the national survey, only 8.3% [95% CI: 8.19, 8.41] of neonates received postnatal checkups. About two-thirds of women, 62.8% had antenatal care visits, 67.9%, gave birth at home, and 95.7% were unaware of neonatal danger signs. Distance from health care institutions [AOR = 1.42; 95% CI: 1.06, 1.89], giving birth in a healthcare facility [AOR = 1.55; 95% CI: 1.12, 2.15], antenatal care visit [AOR = 3.0; 95% CI: 1.99, 4.53], and neonatal danger signs awareness [AOR = 3.06; 95% CI: 2.09, 4.5] were all associated with postnatal care visits.
Conclusion: The number of neonates who had a postnatal checkup was low. Increasing antenatal care visit utilization, improving institutional delivery, raising awareness about neonatal danger signs, increasing access to health care facilities, and implementing home-based neonatal care visits by healthcare providers could all help to improve postnatal checkups.
Introduction
The postnatal period is defined as the period from 1 h after delivery of the placenta until 6 weeks postpartum. This period marks the establishment of a new phase of family life for women and their partners and the beginning of lifelong health for the newborns (1). Most neonatal deaths occur during this critical period in the lives of mothers and newborns (2).
In 2019, 2.4 million neonates died in their first month of life worldwide, with approximately 7,000 newborns dying every day. Despite a decrease in neonatal deaths from 5 million in 1990 to 2.4 million in 2019, the burden in Sub-Saharan Africa and Southern Asia remains high (3). Ethiopia, with 30 deaths per 1,000 live births, is one of the Sub-Saharan African countries with a high burden of neonatal mortality. Prematurity (21.8%), birth asphyxia (31.6%), and sepsis (18.5%) are the leading causes of neonatal deaths in Ethiopia (4).
The World Health Organization (WHO) proposed that by 2035, all countries will have achieved the goal of 10 or fewer newborn deaths per 1,000 live births and that they will continue to reduce death and disability, ensuring that no newborn is left behind. Improved skilled birth attendants, antenatal care visits, and neonatal care coverage, including home-based newborn care, could help achieve this goal. In addition, another WHO strategic objective to achieve reduced neonatal mortality is to leverage the power of parents, families, and communities (5).
Furthermore, all babies, regardless of birthplace, should receive neonatal care within the first 24 h of life, should be discharged from the birthing facility no sooner than 24 h after birth, and should receive at least four checkups within the first 6 weeks of life. Neonatal checkups are one of the milestones in the continuum of care required to achieve optimal maternal and child health. Neonatal care should be provided from a woman-friendly perspective. WHO emphasizes the importance of early post-hospital discharge follow-up by an experienced clinician for both women and their families (6) with the involvement of health workforce support, a woman-friendly perspective, and adequate infrastructure (7). As a result, psychosocial postpartum support programs have been promoted to improve maternal knowledge, attitudes, and skills related to parenting, maternal mental health, maternal quality of life, maternal physical health, timely recognition of danger signs, financial availability to arrange for transportation, affordability of health care costs, and accessibility to a health facility (8, 9).
Evidence shows that poor healthcare-seeking behaviors for neonatal illness, poorly perceived seriousness of the illness, cultural malpractices, and poor socioeconomic status are some of the barriers to utilization of neonatal care visits (10). Furthermore, delays in seeking healthcare, a lack of women’s autonomy to seek care, a lack of money, a heavy workload at home, deeply rooted cultural beliefs and rituals that guide care-seeking behavior, and restrictions on new mothers’ and newborns’ mobility for care-seeking all contribute to the problem (11, 12). Furthermore, the low coverage and poor quality of neonatal care provided reflect a persistently neglected component of maternity services and a gap in the continuum of neonatal care visit utilization (13). As a result, timely neonatal care visits and community-based intervention strategies, such as home visiting, health education, and counseling, are recommended (14, 15).
Maternal and child health care coverage is low in Ethiopia. Among pregnant women, an estimated 62% receive ANC and the rate of delivery in a health facility is 27%. The proportion of women receiving a postnatal check-up within 2 days of delivery is higher in urban areas (48%) than in rural areas (29%), lowest in Somalia (10%), and highest (74%) in Addis Ababa (16). Studies conducted in Ethiopia to identify the magnitude and determinants of postnatal care visits for neonates have inconsistent and inconclusive findings (17–22). ANC visit, place of delivery, residence, distance from the healthcare facility, educational status, age of the respondents, and mode of delivery were some of the factors that affect the postnatal checkup (17, 22–24). Therefore, this study helps estimate the overall rate of neonatal checkups and the factors associated with completing neonatal checkups in Ethiopia.
Materials and Methods
Data Source and Sampling Design
The data was taken from the 2016 EDHS report, which was conducted from January 18 to June 27, 2016. In Ethiopia, there are nine regional states and two city administrations. Each region was stratified into urban and rural areas. Stratified two-stage cluster sampling was performed. Samples of enumeration areas (EAs) were selected independently in each stratum in two stages. A total of 645 EAs (202 in urban areas and 443 in rural areas) were selected with a probability proportional to EA size. The full details are available from reference 16 (16).
Lists of households were used as a sampling frame for the second stage of household selection, and a fixed number of 28 households per cluster were chosen with an equal probability of systematic selection from the newly created household listing. The study population consisted of women with postpartum with a baby in the selected enumeration areas (EAs) and all postpartum mothers who had neonates in Ethiopia (16).
The data was extracted from 7,586 women with postpartum. The approval letter was obtained from the measure demographic and health survey (DHS), and the data set was downloaded from the DHS website1.
Inclusion Criteria
All women with postpartum aged 15–49, who were either permanent residents or visitors who stayed in the selected households the night before the survey, were eligible.
Dependent variable: The primary outcome of interest was postnatal checkups for neonates (PNC). This variable was dummy-coded, so respondents who reported having PNC checkups for neonates were coded as “Yes,” while those who did not have PNC checkups were coded as “No.”
A postnatal care visit for a neonate was defined as at least one PNC visit within the first 42 days of the neonate’s postpartum period (25).
Exposure Variables
Socio-demographic variables: Age of the mother’s residence (urban or rural), religion, marital status, and educational status (no education, primary education, secondary education, and above education).
Antenatal care visit (ANC) is defined based on self-reported frequency of any ANC services provided by skilled healthcare providers in the healthcare institutions, and categorized as “Yes” for any ANC visit and “No” for no ANC visit.
Place of delivery: Refers to whether the delivery was at a healthcare institution or home.
Fertility-related factors include the most recent child’s birth order (1st, 2nd, 3rd, 4th, etc.).
Mode of delivery: How did you give birth (vaginally, C/S, or instrumentally)?
Facility-related variables include the mother’s perceived distance from home to a health facility categorized as a “big problem” or “not a big problem.”
Statistical Analysis
Data cleaning, recording, and analysis were carried out using SPSS statistical software version 24. Sample weight was applied to all analysis procedures to account for complex survey design and unequal probabilities of selection. A Rao-Scott chi-square test that adjusts for complex sample design was used to examine the bivariate associations between each covariate and the outcome variable. The data was a national survey data set with a hierarchical and cluster nature, which emphasizes the need for us to use a multilevel model of analysis. To use this model, the interclass calculation should be calculated, and be greater than 10%. The ICC in the current study was found to be 8.9%, which is lower than expected. As such, we used the binary logistic regression model. All variables with a p-value of ≤0.25 in the bivariable analysis were entered into the final model for multivariable analysis, and variables with p-values of <0.05 in the multivariable binary logistic regression model analysis were considered statistically significant. Finally, the result was presented using frequencies, tables, and texts.
Results
Socio-Demographic and Economic Characteristics of Mothers
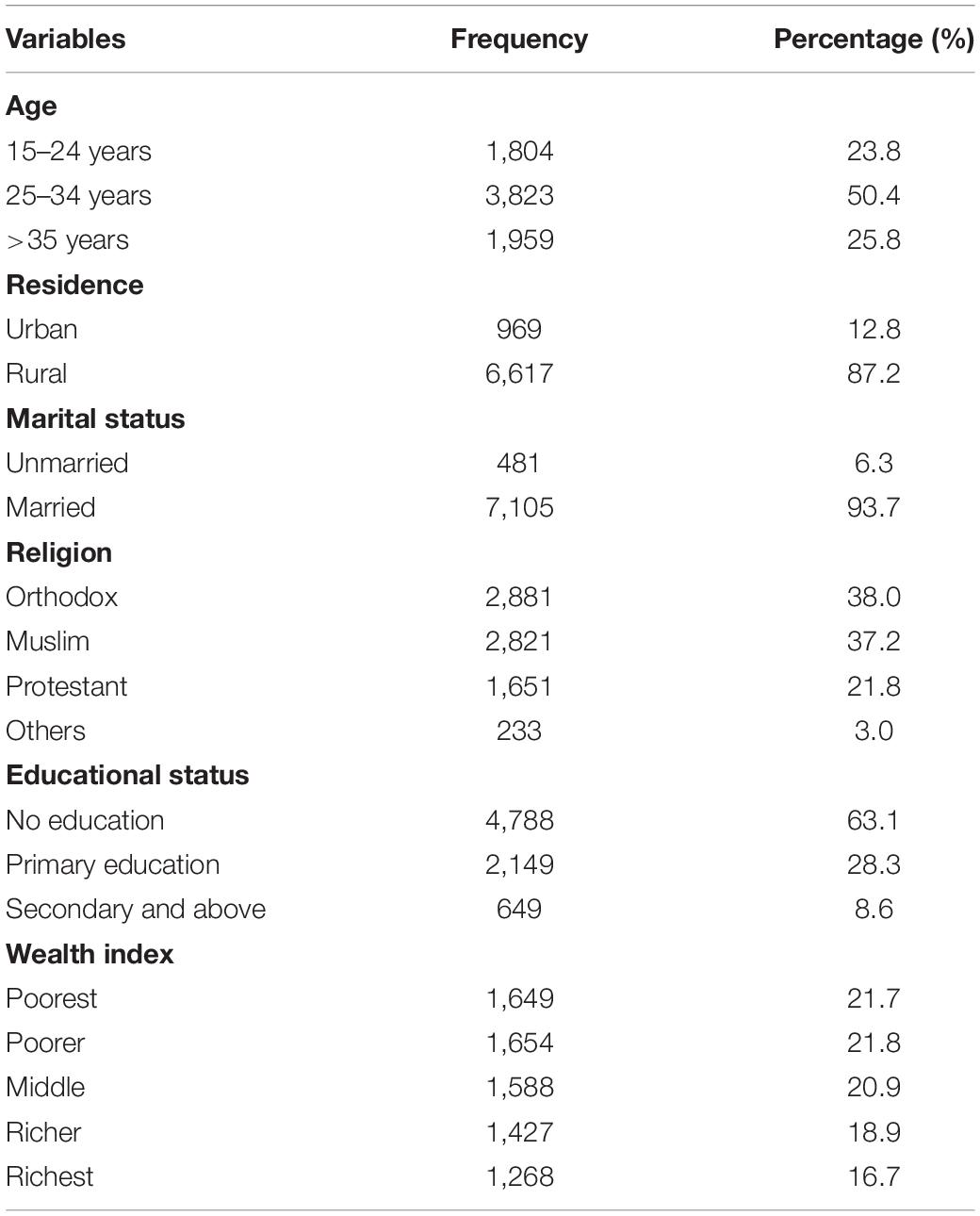
The current EDHS analysis included 7,586 women who had a live birth in the 2 years preceding the survey. Almost half of the women (50.4%) were between the ages of 25 and 34, and 93.7% were married. The vast majority, 87.2%, came from rural areas. Seventy-eight percent of women were orthodox, while 37.2% were Muslim. Almost two-thirds of women, or 63.1%, were illiterate (Table 1).
Characteristics of Mothers and Neonatal Visit
More than half of women (58.1%) perceived the distance from nearby health facilities as a major problem for utilization of PNC checkups. Regarding ANC visits, 62.8% of women had antenatal care visits, and more than two-thirds (67.9%) of women gave birth at home. The majority (97.6%) of women gave birth vaginally and 95.7% had no awareness of danger signs (Table 2).
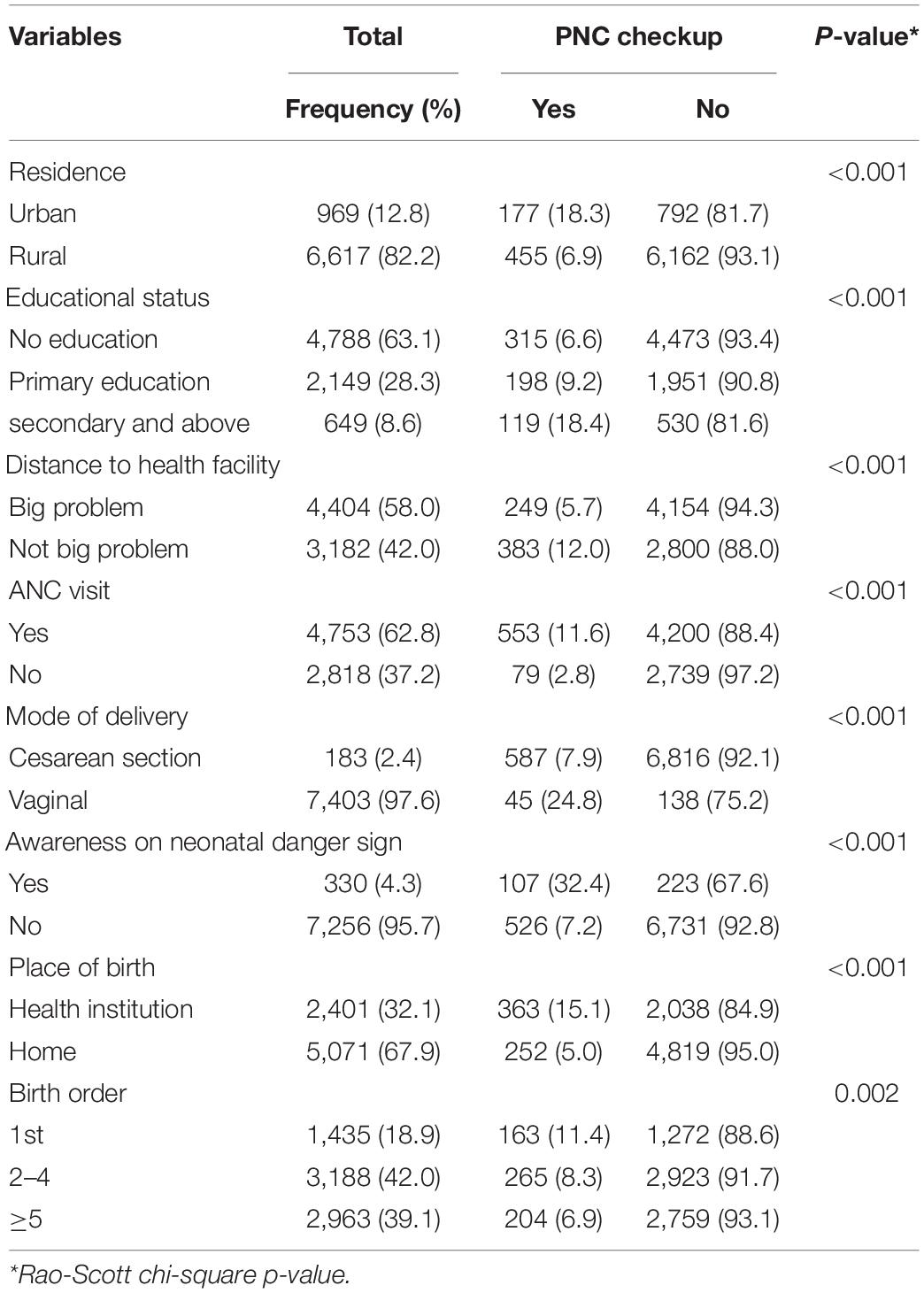
Table 2. Characteristics of the study sample and postnatal checkup for neonates (PNC) in Ethiopia (N = 7,586).
The Magnitude of Postnatal Checkup
Six hundred thirty-two women, or 8.3%, had PNC for neonates within 42 days of giving birth.
Determinants of Postnatal Checkup for Neonate
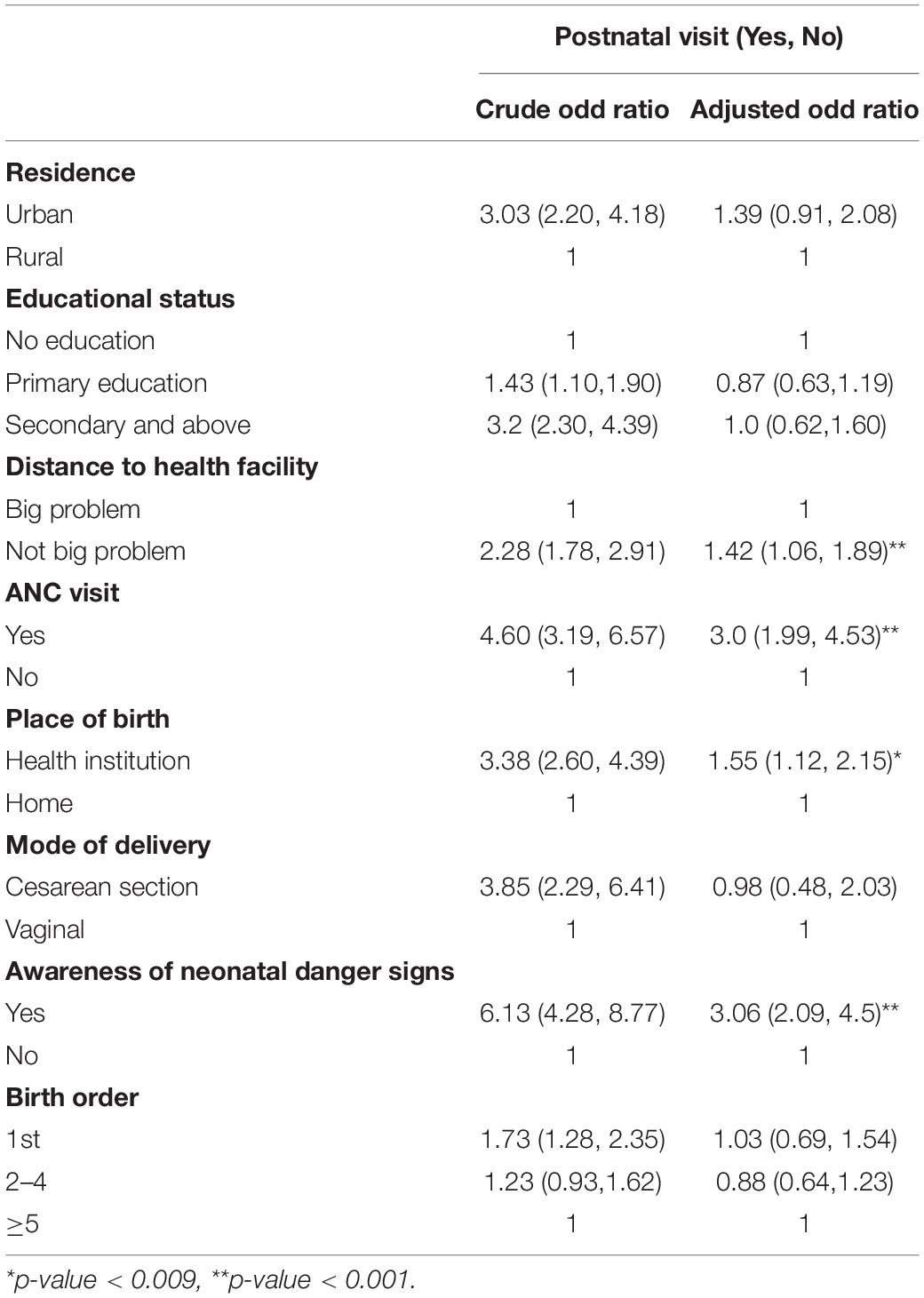
Binary logistic regression, in both bivariable and multivariable forms, was attempted. In a bivariable binary logistic regression analysis, residence, educational status, antenatal care visit, place of delivery, mode of delivery, awareness of neonatal danger signs, perceived distance from the health facility, and birth order were all the significant factors associated with postnatal checkups. The place of birth, ANC visit, and awareness of neonatal danger signs were all statistically significant predictors of postnatal checkups in the multivariable binary logistic regression analysis (Table 3).
Women who perceived distance from healthcare institutions as not being a major issue were 1.42 times more likely than women who perceived distance as a major issue [AOR = 1.42; 95% CI: 1.06, 1.89]. Women who gave birth in a healthcare facility were 1.55 times more likely than women who gave birth at home to have postnatal care visits [AOR = 1.55; 95% CI: 1.12, 2.15]. Furthermore, women who had ANC visits were three times more likely to use neonatal care visits than women who did not have ANC visits [AOR = 3; 95% CI: 1.99, 4.53]. Women who were aware of neonatal danger signs were three times more likely to seek neonatal care than women who were unaware [AOR = 3.06; 95% CI: 2.09, 4.5] (Table 3).
Discussion
Postnatal care visits are essential for increasing neonatal survival. This study aimed to determine the proportion of PNC and factors associated with PNC among women with postpartum in Ethiopia. We found that the postnatal checkup rate was 8.3%. The magnitude of PNC visits in the current study is lower than findings from Morocco (30.1%) (26), Nigeria (28.9%) (27), Ghana (62%) (28), India (29%) (29), and Nepal (43.2%) (30). One possible reason could be that the current study only included PNC, whereas other studies included postnatal checkups for mothers and neonates, which affects the overall magnitude of the postnatal care visit. Furthermore, it could be due to differences in the study setting, data collection method, and target population.
Women who perceived their distance from healthcare institutions as not being a major issue were 1.42 times more likely to use the neonatal care checkup than women who perceived distance from healthcare institutions as being a major issue. The finding is similar to studies conducted in Indonesia (31) and developing countries (32). This could be because women who live a long distance away from a healthcare facility may have difficulty obtaining transportation (33, 34). Furthermore, it causes a maternal delay in seeking healthcare services (35).
Women who had ANC visits were three times more likely than women who did not have ANC visits to use a PNC checkup. The finding is supported by studies conducted in Ethiopia (22, 27, 28, 30, 36, 37). Previous studies suggest that antenatal care visits increase mothers’ birth preparedness and complication readiness (38). Moreover, women who had antenatal care visits were more knowledgeable about maternal and neonatal complications (39). This increased knowledge could explain increased postnatal care checkups.
The study revealed that women who gave birth at healthcare institutions were 1.55 times more likely to have a PNC visit than women who gave birth at home. This is in line with other studies conducted in Ethiopia (19, 37, 40, 41), and Nepal (30). Giving birth in a health facility increases both women’s awareness and knowledge of the benefits of neonatal checkups, provides better information on postpartum complications, increases access to healthcare services, and increases the mother’s health-seeking behavior. Evidence suggests that education about postnatal care schedules leads to an increase in PNC visits (42).
Women who were aware of neonatal danger signs were 3.06 times more likely than women who were not aware of neonatal danger signs to have a PNC checkup for neonates. The findings are consistent with other studies conducted in various parts of the world (43, 44). This could be related to enhanced awareness of mothers on neonatal danger signs, which may increase those who seek healthcare (45). Understanding neonatal danger signs also assists women in identifying early warning signs of a neonatal problem, which increases neonatal care-seeking behaviors.
A strength of this study was the data taken from a large and representative sample size. A limitation of this study is that, because of its cross-sectional nature, it does not demonstrate a cause-and-effect relationship between the variables examined and the completion of neonatal checkups. Survey responses may also have been affected by social desirability bias.
Conclusion
In this study, the national PNC completion rate was very low at just 8.3%. PNC visit was associated with perceived distance from healthcare institutions, institutional delivery, having ANC visits, and being aware of neonatal danger signs. Our findings suggest that improving ANC visits, delivery in healthcare facilities, maternal awareness of neonatal danger signs, and access to health care, including through home visits, may improve rates of PNC in Ethiopia. Moreover, emphasis should be given to community-based newborn care packages, which have been implemented in Ethiopia.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
Permission was obtained to use the EDHS data from the measure DHS International Program, and approval data was also obtained. All methods were performed in accordance with the relevant guidelines and regulations. Informed consent was given.
Author Contributions
BB, DB, DM, EC, and WA designed the study, interpreted the results, and prepared the manuscript. BB, DB, AE, DA, SD, GN, EA, SN, YT, and DJ analyzed, interpreted, and wrote the manuscript. TM reviewed and edited the manuscript. All authors were involved in design, data interpretation, and reviewed the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We acknowledged the DHS International Program for providing the data set.
Abbreviations
AOR, adjusted odd ratio; ANC, antenatal care visit; CI, confidence interval; DHS, Demographic and Health Survey; EDHS, Ethiopian Demographic and Health Survey; PNC, postnatal care visit; SDG, sustainable development goal; WHO, World Health Organization.
Footnotes
References
1. WHO. WHO Technical Consultation on Postpartum and Postnatal Care. Geneva: World Health Organization (2010).
3. WHO. Newborns: Improving Survival and Well-Being. (2020). Available online at: https://www.who.int/news-room/fact-sheets/detail/newborns-reducing-mortality (accessed October 25, 2020).
6. WHO. WHO Recommendations on Postnatal Care of the Mother and Newborn. Geneva: World Health Organization (2014).
7. Kearns A, Caglia J, ten Hoope-Bender P, Langer A. Antenatal and postnatal care: a review of innovative models for improving availability, accessibility, acceptability and quality of services in low-resource settings. BJOG. (2016) 123:540–8. doi: 10.1111/1471-0528.13818
8. Shaw E, Levitt C, Wong S, Kaczorowski J, Group MUPR. Systematic review of the literature on postpartum care: effectiveness of postpartum support to improve maternal parenting, mental health, quality of life, and physical health. Birth. (2006) 33:210–20. doi: 10.1111/j.1523-536X.2006.00106.x
9. Lassi ZS, Middleton P, Bhutta ZA, Crowther C. Health care seeking formaternal and newborn illnesses in low-and middle-income countries: asystematic review of observational and qualitative studies. F1000Research.(2019) 8:200. doi: 10.12688/f1000research.17828.1
10. Anyanwu FC, Okeke SR. Health care, care provider and client satisfaction: transforming health care delivery system for improved health care seeking behaviour. J Modern Educ Rev. (2014) 4:846–53.
12. Aruldas K, Kant A, Mohanan P. Care-seeking behaviors for maternal and newborn illnesses among self-help group households in Uttar Pradesh, India. J Health Popul Nutr. (2017) 36:49. doi: 10.1186/s41043-017-0121-1
13. Chen L, Qiong W, Van Velthoven MH, Yanfeng Z, Shuyi Z, Ye L, et al. Coverage, quality of and barriers to postnatal care in rural Hebei, China: a mixed method study. BMC Pregnancy Childbirth. (2014) 14:31. doi: 10.1186/1471-2393-14-31
14. Lassi ZS, Middleton PF, Bhutta ZA, Crowther C. Strategies for improving health care seeking for maternal and newborn illnesses in low- and middle-income countries: a systematic review and meta-analysis. Glob Health Action. (2016) 9:31408. doi: 10.3402/gha.v9.31408
15. Gai Tobe R, Islam MT, Yoshimura Y, Hossain J. Strengthening the community support group to improve maternal and neonatal health seeking behaviors: a cluster-randomized controlled trial in Satkhira District, Bangladesh. PLoS One. (2019) 14:e0212847. doi: 10.1371/journal.pone.0212847
17. Tesfahun F, Worku W, Mazengiya F, Kifle M. Knowledge, perception and utilization of postnatal care of mothers in Gondar Zuria district, Ethiopia: a cross-sectional study. Matern Child Health J. (2014) 18:2341–51. doi: 10.1007/s10995-014-1474-3
18. Belachew T, Taye A, Belachew T. Postnatal care service utilization and associated factors among mothers in Lemo Woreda, Ethiopia. J Womens Health Care. (2016) 5:318.
19. Wudineh KG, Nigusie AA, Gesese SS, Tesu AA, Beyene FY. Postnatal care service utilization and associated factors among women who gave birth in Debretabour town, North West Ethiopia: a community-based cross-sectional study. BMC Pregnancy Childbirth. (2018) 18:508. doi: 10.1186/s12884-018-2138-x
20. Sahle G. Ethiopic maternal care data mining: discovering the factors that affect postnatal care visit in Ethiopia. Health Inf Sci Syst. (2016) 4:4. doi: 10.1186/s13755-016-0017-2
21. Akibu M, Tsegaye W, Megersa T, Nurgi S. Prevalence and determinants of complete postnatal care service utilization in northern Shoa, Ethiopia. J Pregnancy. (2018) 2018:8625437. doi: 10.1155/2018/8625437
22. Berhe A, Bayray A, Berhe Y, Teklu A, Desta A, Araya T, et al. Determinants of postnatal care utilization in Tigray, Northern Ethiopia: a community based cross-sectional study. PLoS One. (2019) 14:e0221161. doi: 10.1371/journal.pone.0221161
23. Gebrehiwot G, Medhanyie AA, Gidey G, Abrha K. Postnatal care utilization among urban women in northern Ethiopia: cross-sectional survey. BMC Womens Health. (2018) 18:78. doi: 10.1186/s12905-018-0557-5
24. Ayele BG, Woldu MA, Gebrehiwot HW, Gebre-Egziabher EG, Gebretnsae H, Hadgu T, et al. Magnitude and determinants for place of postnatal care utilization among mothers who delivered at home in Ethiopia: a multinomial analysis from the 2016 Ethiopian demographic health survey. Reprod Health. (2019) 16:1–10. doi: 10.1186/s12978-019-0818-2
25. Sines E, Syed U, Wall S, Worley H. Postnatal care: a critical opportunity to save mothers and newborns. Policy Perspect Newborn Health. (2007) 1–7. doi: 10.1136/bmjgh-2020-002660
26. Elkhoudri N, Baali A. Postnatal care: levels and determinants in Morocco. Iran J Public Health. (2017) 46:242.
27. Dahiru T, Oche OM. Determinants of antenatal care, institutional delivery and postnatal care services utilization in Nigeria. Pan Afr Med J. (2015) 22:321. doi: 10.11604/pamj.2015.21.321.6527
28. Sakeah E, Aborigo R, Sakeah JK, Dalaba M, Kanyomse E, Azongo D, et al. The role of community-based health services in influencing postnatal care visits in the Builsa and the West Mamprusi districts in rural Ghana. BMC Pregnancy Childbirth. (2018) 18:295. doi: 10.1186/s12884-018-1926-7
29. Kaur M, Kaur R. Factors affecting utilization of postnatal services among rural postnatal mothers. J Nurs Sci Pract. (2018) 7:20–3.
30. Khanal V, Adhikari M, Karkee R, Gavidia T. Factors associated with the utilisation of postnatal care services among the mothers of Nepal: analysis of Nepal demographic and health survey 2011. BMC Womens Health. (2014) 14:19. doi: 10.1186/1472-6874-14-19
31. Titaley CR, Dibley MJ, Roberts CL. Factors associated with non-utilisation of postnatal care services in Indonesia. J Epidemiol Commun Health. (2009) 63:827–31. doi: 10.1136/jech.2008.081604
32. Adams YJ, Smith BA. Integrative review of factors that affect the use of postpartum care services in developing countries. J Obstetr Gynecol Neonat Nurs. (2018) 47:371–84. doi: 10.1016/j.jogn.2018.02.006
33. Ononokpono DN, Odimegwu CO, Imasiku EN, Adedini SA. Does it really matter where women live? A multilevel analysis of the determinants of postnatal care in Nigeria. Matern Child Health J. (2014) 18:950–9. doi: 10.1007/s10995-013-1323-9
34. Watson G, Patel K, Leng D, Vanna D, Khut S, Prak M, et al. Barriers and facilitators to neonatal health and care-seeking behaviours in rural Cambodia: a qualitative study. BMJ Open. (2020) 10:e035449. doi: 10.1136/bmjopen-2019-035449
35. Wanaka S, Hussen S, Alagaw A, Tolosie K, Boti N. Maternal delays for institutional delivery and associated factors among postnatal mothers at public health facilities of gamo zone, Southern Ethiopia. Int J Womens Health. (2020) 12:127. doi: 10.2147/IJWH.S240608
36. Yunus A, Iqbal S, Munawar R, Zakar R, Mushtaq SK, Sadaf F, et al. Determinants of postnatal care services utilization in Pakistan-insights from Pakistan demographic and health survey (PDHS) 2006-07. Middle East J Sci Res. (2013) 18:1440–7. doi: 10.12688/f1000research.25700.2
37. Tiruneh GT, Worku A, Berhane Y, Betemariam W, Demissie M. Determinants of postnatal care utilization in Ethiopia: a multilevel analysis. BMC Pregnancy Childbirth. (2020) 20:549. doi: 10.1186/s12884-020-03254-7
38. Bintabara D, Mohamed MA, Mghamba J, Wasswa P, Mpembeni RN. Birth preparedness and complication readiness among recently delivered women in Chamwino district, Central Tanzania: a cross sectional study. Reprod Health. (2015) 12:44. doi: 10.1186/s12978-015-0041-8
39. Yadeta TA. Antenatal care utilization increase the odds of women knowledge on neonatal danger sign: a community-based study, Eastern Ethiopia. BMC Res Notes. (2018) 11:845. doi: 10.1186/s13104-018-3957-6
40. Limenih MA, Endale ZM, Dachew BA. Postnatal care service utilization and associated factors among women who gave birth in the last 12 months prior to the study in Debre Markos town, Northwestern Ethiopia: a community-based cross-sectional study. Int J Reprod Med. (2016) 2016:7095352. doi: 10.1155/2016/7095352
41. Fekadu GA, Kassa GM, Berhe AK, Muche AA, Katiso NA. The effect of antenatal care on use of institutional delivery service and postnatal care in Ethiopia: a systematic review and meta-analysis. BMC Health Serv Res. (2018) 18:577. doi: 10.1186/s12913-018-3370-9
42. Izudi J, Amongin D. Use of early postnatal care among women with postpartum in Eastern Uganda. Int J Gynecol Obstetr. (2015) 129:161–4. doi: 10.1016/j.ijgo.2014.11.017
43. Demis A, Gedefaw G, Wondmieneh A, Getie A, Alemnew B. Women’s knowledge towards neonatal danger signs and its associated factors in Ethiopia: a systematic review and meta-analysis. BMC Pediatr. (2020) 20:217. doi: 10.1186/s12887-020-02098-6
44. Chowdhury SK, Billah SM, Arifeen SE, Hoque DME. Care-seeking practices for sick neonates: findings from cross-sectional survey in 14 rural sub-districts of Bangladesh. PLoS One. (2018) 13:e0204902. doi: 10.1371/journal.pone.0204902
Keywords: EDHS, Ethiopia, neonatal checkup, postnatal visit, neonate
Citation: Birhane BM, Bayih WA, Mekonen DK, Chanie ES, Demis S, Shimelis H, Asferie WN, Abebe E, Addisu D, Nibret G, Endalamaw A, Munye T, Jember DA, Nebiyu S, Tiruneh YM and Belay DM (2022) Level of Postnatal Checkup in Ethiopia – Implications for Child Health Services. Front. Pediatr. 10:895339. doi: 10.3389/fped.2022.895339
Received: 13 March 2022; Accepted: 05 May 2022;
Published: 14 June 2022.
Edited by:
Andrew Steenhoff, Children’s Hospital of Philadelphia, United StatesReviewed by:
Tinsae Alemayehu, American Medical Center, EthiopiaS. Maria Awaluddin, Ministry of Health, Malaysia
Henna Shaikh, Children’s Hospital of Philadelphia, United States
Copyright © 2022 Birhane, Bayih, Mekonen, Chanie, Demis, Shimelis, Asferie, Abebe, Addisu, Nibret, Endalamaw, Munye, Jember, Nebiyu, Tiruneh and Belay. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Binyam Minuye Birhane, YmluaWFtbWludXllQHlhaG9vLmNvbQ==
 Binyam Minuye Birhane
Binyam Minuye Birhane Wubet Alebachew Bayih
Wubet Alebachew Bayih Demewoz Kefale Mekonen
Demewoz Kefale Mekonen Ermias Sisay Chanie
Ermias Sisay Chanie Solomon Demis1
Solomon Demis1 Habtamu Shimelis
Habtamu Shimelis Worku Necho Asferie
Worku Necho Asferie Eskeziaw Abebe
Eskeziaw Abebe Dagne Addisu
Dagne Addisu Gedefaye Nibret
Gedefaye Nibret Aklilu Endalamaw
Aklilu Endalamaw Desalegn Abebaw Jember
Desalegn Abebaw Jember Samuel Nebiyu
Samuel Nebiyu Demeke Mesfin Belay
Demeke Mesfin Belay