- 1Research Unit, Lata Medical Research Foundation, Nagpur, India
- 2Department of Medical Research, Datta Meghe Institute of Medical Sciences, Wardha, India
- 3Department of Pediatrics, All India Institute of Medical Sciences, Nagpur, India
- 4Department of Global Health, Boston University School of Public Health, Boston, MA, USA
Introduction: Most neonatal deaths occur in the first week of life, due to birth asphyxia. Helping Babies Breathe (HBB), is a simulation-based neonatal resuscitation training program to improve knowledge and skills. There is little information on which knowledge items or skill steps are challenging for the learners.
Methods: We used training data from NICHD's Global Network study to understand the items most challenging for Birth Attendants (BA) to guide future curriculum modifications. HBB training was provided in 15 primary, secondary and tertiary level care facilities in Nagpur, India. Refresher training was provided 6 months later. Each knowledge item and skill step was ranked from difficulty level 1 to 6 based on whether 91%–100%, 81%–90%, 71%–80%, 61%–70%, 51%–60% or <50% of learners answered/performed the step correctly.
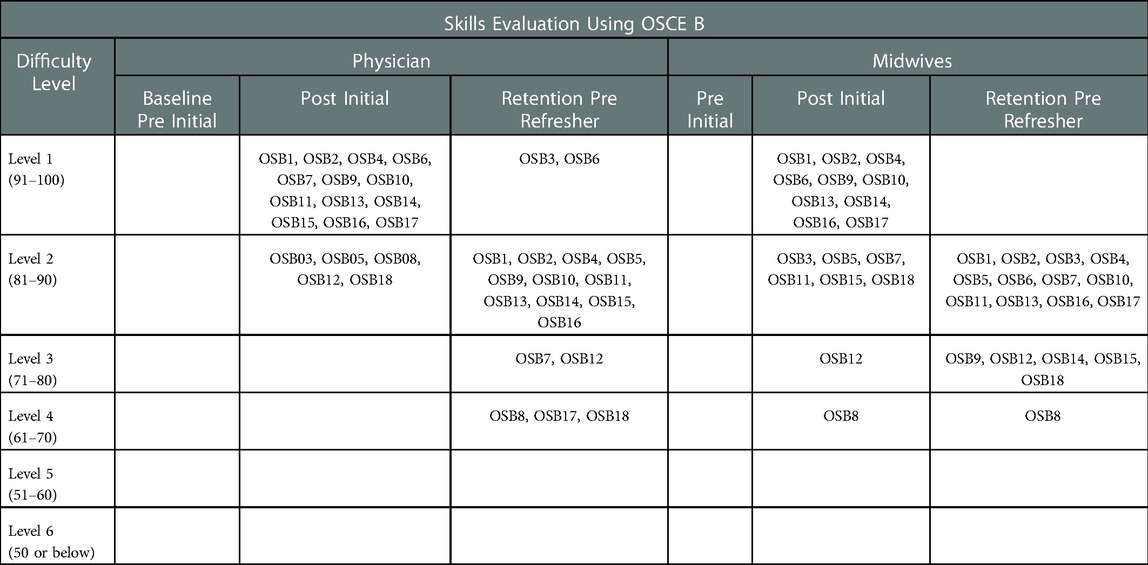
Results: The initial HBB training was conducted in 272 physicians and 516 midwives of which 78 (28%) physicians and 161 (31%) midwives received refresher training. Questions related to timing of cord clamping, management of a meconium-stained baby, and steps to improve ventilation were most difficult for both physicians and midwives. The initial steps of Objective Structured Clinical Examination (OSCE)-A i.e. equipment checking, removing wet linen and immediate skin-to-skin contact were most difficult for both groups. Midwives missed stimulating newborns while physicians missed cord clamping and communicating with mother. In OSCE-B, starting ventilation in the first minute of life was the most missed step after both initial and 6 months refresher training for physicians and midwives. At the retraining, the retention was worst for cutting the cord (physicians level 3), optimal rate of ventilation, improving ventilation & counting heart rate (midwives level 3), calling for help (both groups level 3) and scenario ending step of monitoring the baby and communicating with mother (physicians level 4, midwives 3).
Conclusion: All BAs found skill testing more difficult than knowledge testing. The difficulty level was more for midwives than for physicians. So, the HBB training duration and frequency of retraining can be tailored accordingly. This study will also inform subsequent refinement in the curriculum so that both trainers and trainees will be able to achieve the required proficiency.
Background
Approximately 3.3 million neonatal deaths occurred globally in 2009 (1), accounting for 41% of the deaths among under five years old (1). The vast majority of these deaths occur in low and middle-income countries (LMICs). India has 27.8% of global neonatal deaths and is among the five countries that make up more than half of all deaths (1). Most deaths take place within seven days of delivery (2, 3). A major cause of these deaths is asphyxia at birth (2). In high income countries (HIC) deliveries are usually attended by highly trained physicians/neonatologists or other medical staff who have adequate training to recognize an asphyxiated newborn and provide prompt resuscitation. In LMICs, even births that occur in medical facilities are not always attended by specialists or neonatologists. It is not uncommon that babies who are not breathing at birth are considered to be stillbirths and no efforts are made to provide resuscitation. Neonatal resuscitation trainings have thus helped to reduce perinatal mortality by reducing both the number of fresh stillbirths and early neonatal deaths (4, 5). A number of studies in past and recently published meta-analysis have evaluated the impact of essential newborn care and resuscitation training for physicians, nurses, and other birth attendants (BAs) on delivery outcome and neonatal survival (5). Many studies have also evaluated the impact of resuscitation trainings on the skills and knowledge of the trainees by assessing the changes in knowledge and skill scores before and after training (6, 7). Very few studies have assessed what knowledge items or skills steps are learning challenges for trainees i.e., what items the trainees are least likely to answer correctly during the resuscitation trainings or to retain over time. If the items that are most important for successful resuscitation are most difficult to master, then this failure to learn will impact survival of a newborn experiencing birth asphyxia. This information will also help guide the frequency of re-training to attain adequate proficiency in the items found most challenging for the trainees.
The HBB, is an evidence-based newborn resuscitation training program developed by a Global Development Alliance of five partners namely the American Academy of Pediatrics, the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) Global Network, Save the Children, the Laerdal Global Health and the United States Agency for International Development (8, 9). It was developed to improve neonatal survival in low-resource settings by training first level birth attendants (BAs) to resuscitate neonates wherever they are born (10–12). The training module includes learning activities such as knowledge assessment using multiple choice questions, interactive scenario-based exercises, drills, simulation and role playing.
This program has now been implemented in several countries and has had an impact on resuscitation processes as well as neonatal survival (13, 14). However there is scope for improvement in order to accomplish the Every Newborn Action Plan goal of a global neonatal mortality rate of 7 per 1,000 live births by 2,035 (15). The NICHD's Global Network in collaboration with American Academy of Paediatrics and Laerdal Medical, conducted a study to evaluate the impact of implementation of HBB training and equipment package with continuous monitoring and quality improvement activities of the resuscitation practices on the perinatal mortality in Nagpur (India), Belgaum (India) and Eldoret (Kenya) (16, 17). During these trainings, pre-training and post-training tests were conducted to assess knowledge and skills of the trainees. At Nagpur site, training performance data was recorded for all the participants trained in HBB. This study aims to provide information regarding which knowledge items or skills steps were formidable for trainees' learning, thereby giving an insight into how the HBB training module can be further improved in terms of achieving its educational outcomes. It will allow policymakers, partners and trainers to adapt and improve the HBB training module curriculum with enhanced focus on areas which participants find difficult to learn. Thus, the objectives of this study were to determine, for birth attendants (physicians and midwives), the following - 1) the difficulty level of each knowledge and skill item of the HBB training package based on percent of trainees who could answer/perform it correctly, 2) to identify the items that were most responsive to HBB training, and, 3) to identify specific items for which the retention of knowledge and skills were lost over time.
Methods
This study is secondary analysis of training performance data from a pre-post evaluation of a health facility-based training program in HBB at the Nagpur (India) site (16, 17). The HBB training program was implemented at 15 facilities (2 primary, 4 sary and 9 tertiary level care facilities) in and around Nagpur district, that provided round the clock delivery services (16). HBB curriculum and evaluation tools developed by American Academy of Pediatrics (AAP) for adult trainees of different backgrounds, with its high-quality teaching materials, were used according to their stated guidelines to train the BAs of the 15 participating facilities. The master trainers (MTs) were chosen carefully among doctors and nurses with adult education experience or an aptitude for teaching and expertise in neonatal resuscitation. These MTs first underwent a training of trainers (contact period of 24 h) where they had to give short demonstrations of their teaching and evaluation skills to ensure uniformity in teaching and evaluation thus preserving the integrity of the intervention (6).
The “initial” HBB training involved 14 contact hours of training of birth attendants by master trainers who were trained by AAP trainers (6, 16). The initial training had to include all facility staff, including the senior and administrative staff to increase the programmatic buy-in. Six months later, only those trainees from initial training that were actively engaged in attending births and resuscitating newborns (the “active” birth attendants- the health care workers that will be conducting deliveries in real world) received a “refresher” training of around five contact hours. There was no selection or sampling involved in this and ALL the “active” birth attendants received refresher training. BAs with previous training in neonatal resuscitation were not excluded. The details of the training including facility selection criteria, level of care these facilities provided and also the detailed characteristics of these active birth attendants have been previously published (6, 16). Between the initial and refresher trainings, the birth attendants underwent several monitoring activities best described as supportive supervision. These included daily practice of BMV skills at a well-equipped practice corner just before each duty shift with logbook entries; regular observation of deliveries by master trainers; debriefing after every resuscitation; and audits of every perinatal death. The current study assessed the knowledge and skill items included in the HBB curriculum that were challenging for the trainees.
Evaluation of knowledge and skill levels
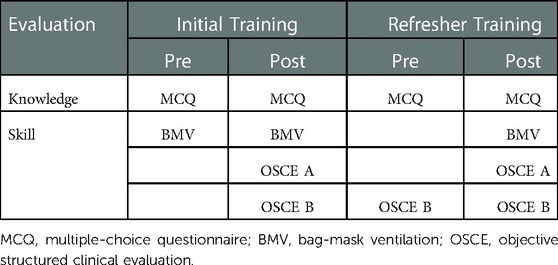
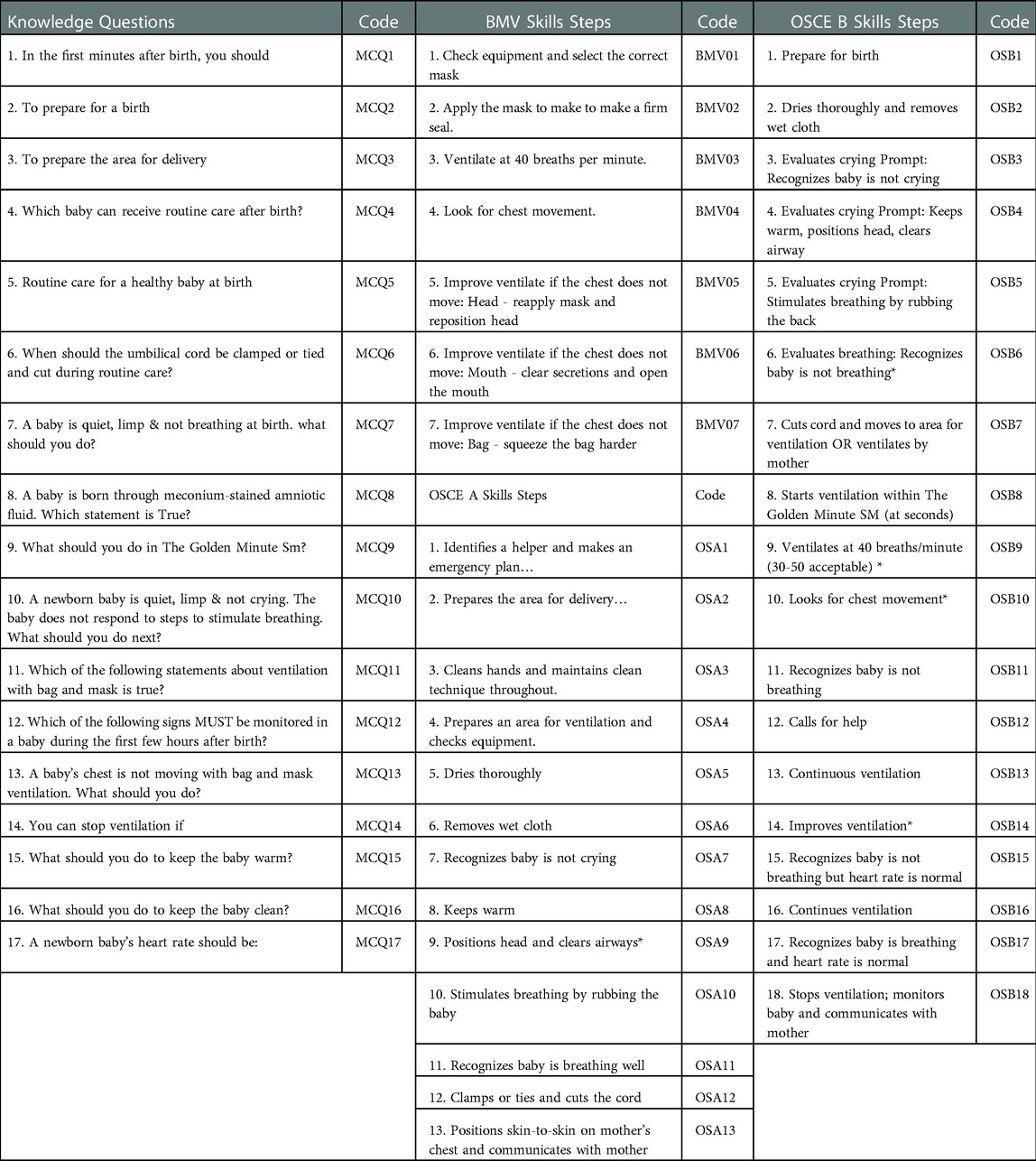
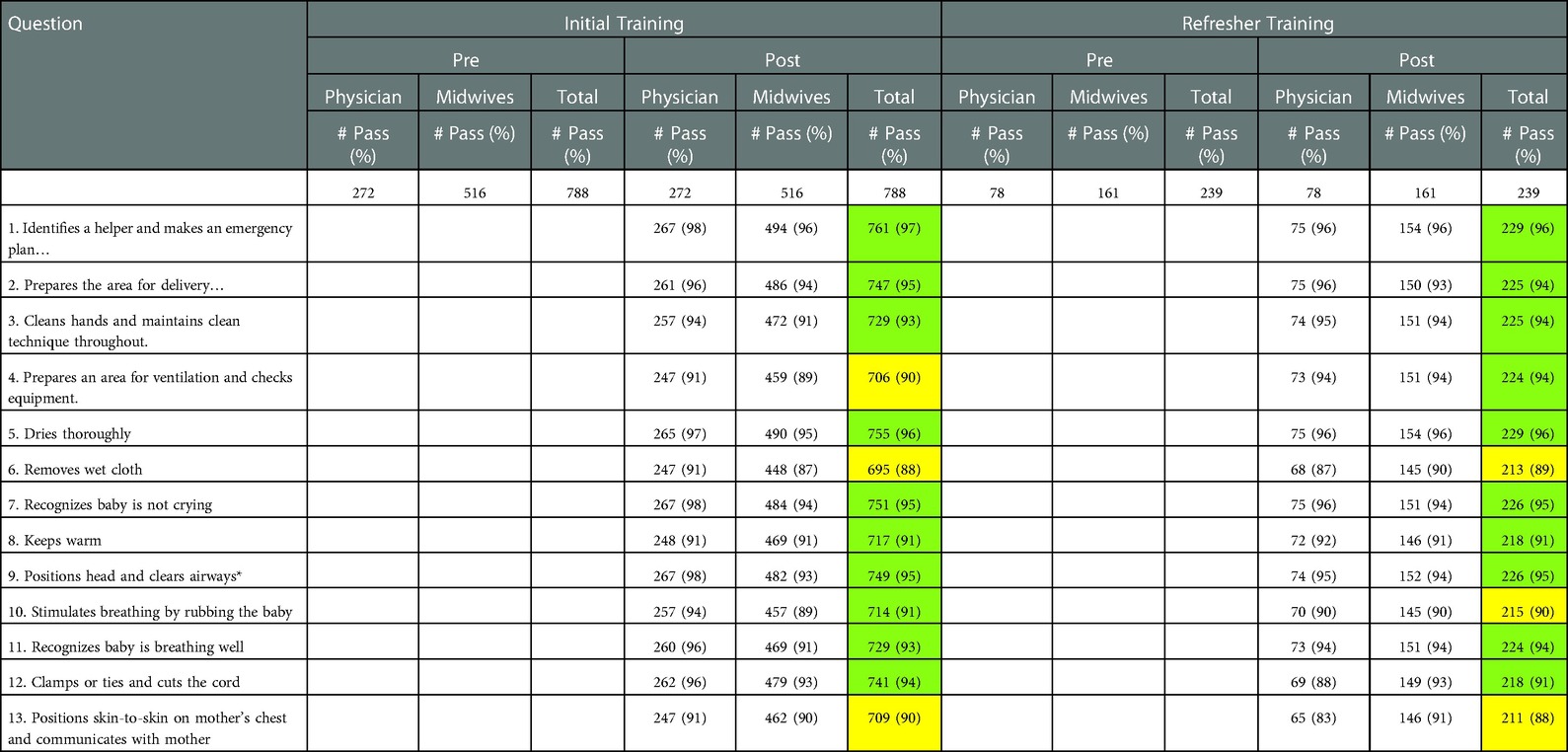
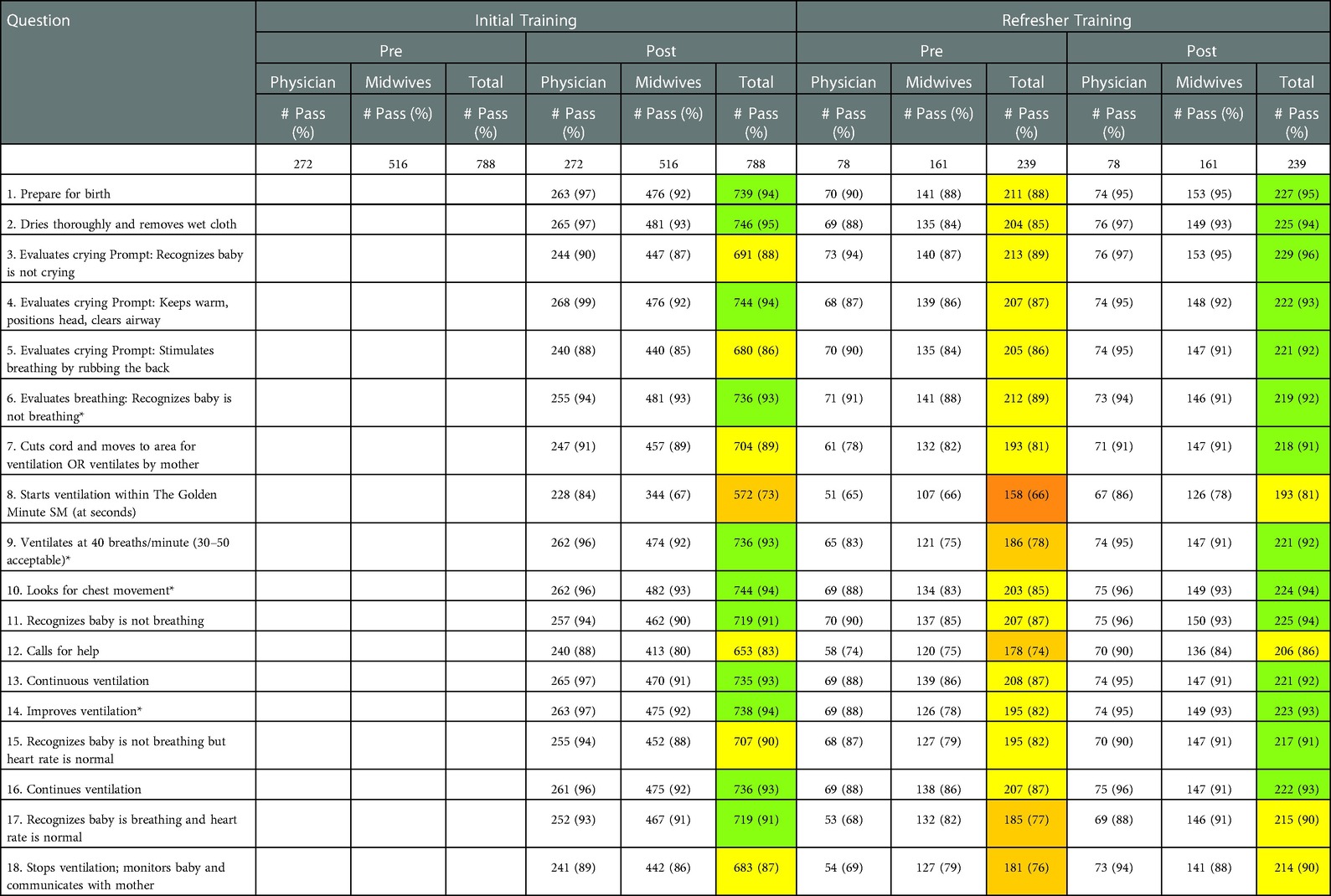
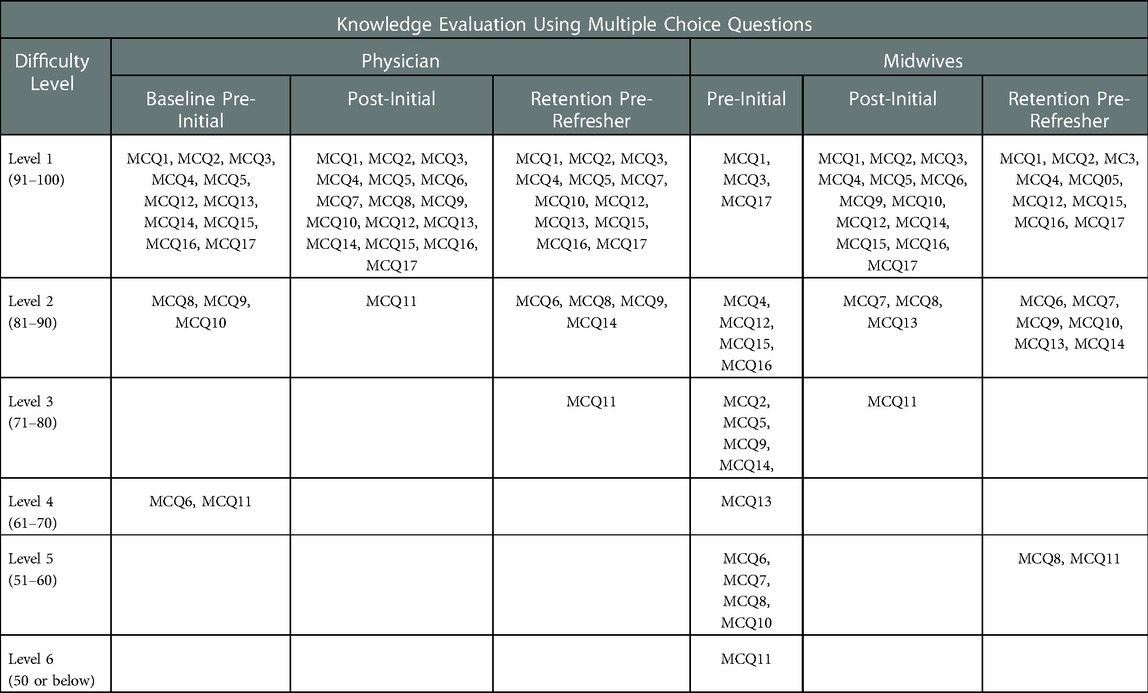
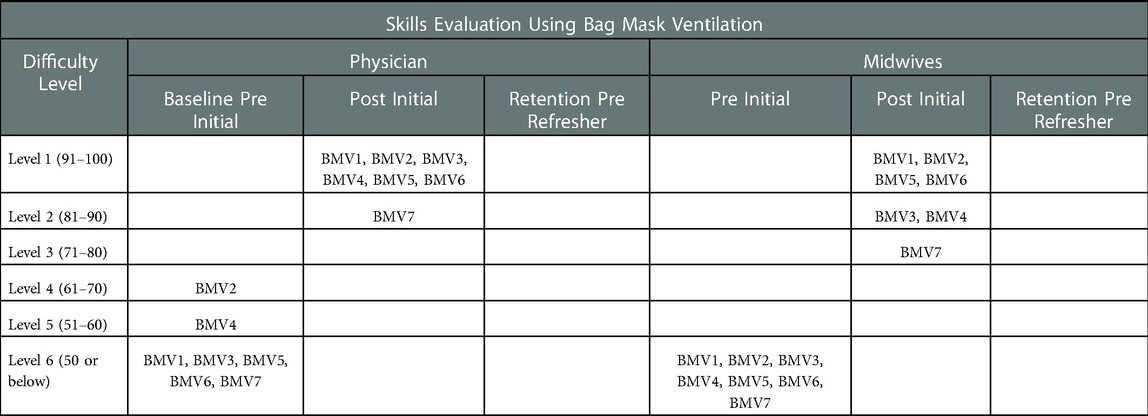
The detailed scheme of the trainings and evaluations is shown in Table 1. A multiple-choice questionnaire (MCQ) of 17 items (Questions) was used to assess “knowledge” of the participants. The knowledge assessment was done at the following time points - prior to the initial training to assess base-line knowledge prior to training. It was then conducted after initial training, prior to refresher training and after refresher training. Bag-Mask Ventilation (BMV) skills were assessed before and after the initial training using a checklist of 7 steps. Two Objective Structured Clinical Examinations (OSCE-A and OSCE-B) were used to evaluate the trainee's skills on the mannequin. OSCE-A had 13 steps and assessed ability of the trainee to resuscitate a newborn that required initial steps of resuscitation. OSCE-B assessed the resuscitation abilities during a more complex scenario of positive pressure ventilation through 18 steps. Individual questions and OSCE steps have been enumerated in Table 2. The OSCE-A and OSCE-B were not conducted prior to the initial training. They were conducted after the initial training. OSCE-B, which includes most skills of OSCE-A was also conducted before and after the refresher training that was conducted six months after the initial training. Based on the performance of participants during these trainings, we assessed the difficulty level of MCQs and skill steps included in BMV, OSCE-A and OSCE-B during the initial and refresher trainings. We also assessed which questions in the MCQs or skill steps of BMV, OSCE-A or OSCE-B were difficult to retain over a period of time. The pre–post training evaluation of trainees was conducted by master trainers and the responses of the all the MCQs and skill steps performed by the trainees were recorded on evaluation forms that provided the data for this study.
Data analysis
The trainees or BAs were categorized into two groups – “Physicians” which included graduate and postgraduate doctors attending deliveries and the “Midwives” which included nurses, auxiliary nurse midwives (ANMs) and all other staff attending a delivery. Each MCQ and skill step was ranked from Level 1 to 6 difficulty level. These difficulty levels were based on the proportion of trainees who performed the knowledge or skill item correctly. The question or skill step that most trainees were able to do correctly was considered as the easiest or having the least level of difficulty. The difficulty levels were graded from 1 to 6 for passing percentage of 91%–100%, 81%–90%, 71%–80%, 61%–70%, 51%–60% and <50% respectively. For example, if an MCQ question was answered correctly by 91% of the learners, it was rated as difficulty Level 1. Although 100% proficiency is most desirable, for this study difficulty Level 1 was considered as an acceptable level of proficiency to assess improvement. If an MCQ question was answered correctly by only 49% of the learners, then it was rated as difficulty Level 6. We elected to use this method as it is intuitive and previously used for assessing difficulty levels of items (18).
Ethical considerations
The study was reviewed and approved by the Institutional Review Board of Lata Medical Research Foundation, Nagpur. The ethics approval for the GN HBB study that trained the Nagpur site facilities in HBB have been published previously (6, 16, 17). Written informed consent was obtained from all trained birth attendants who participated in GN HBB study.
Results
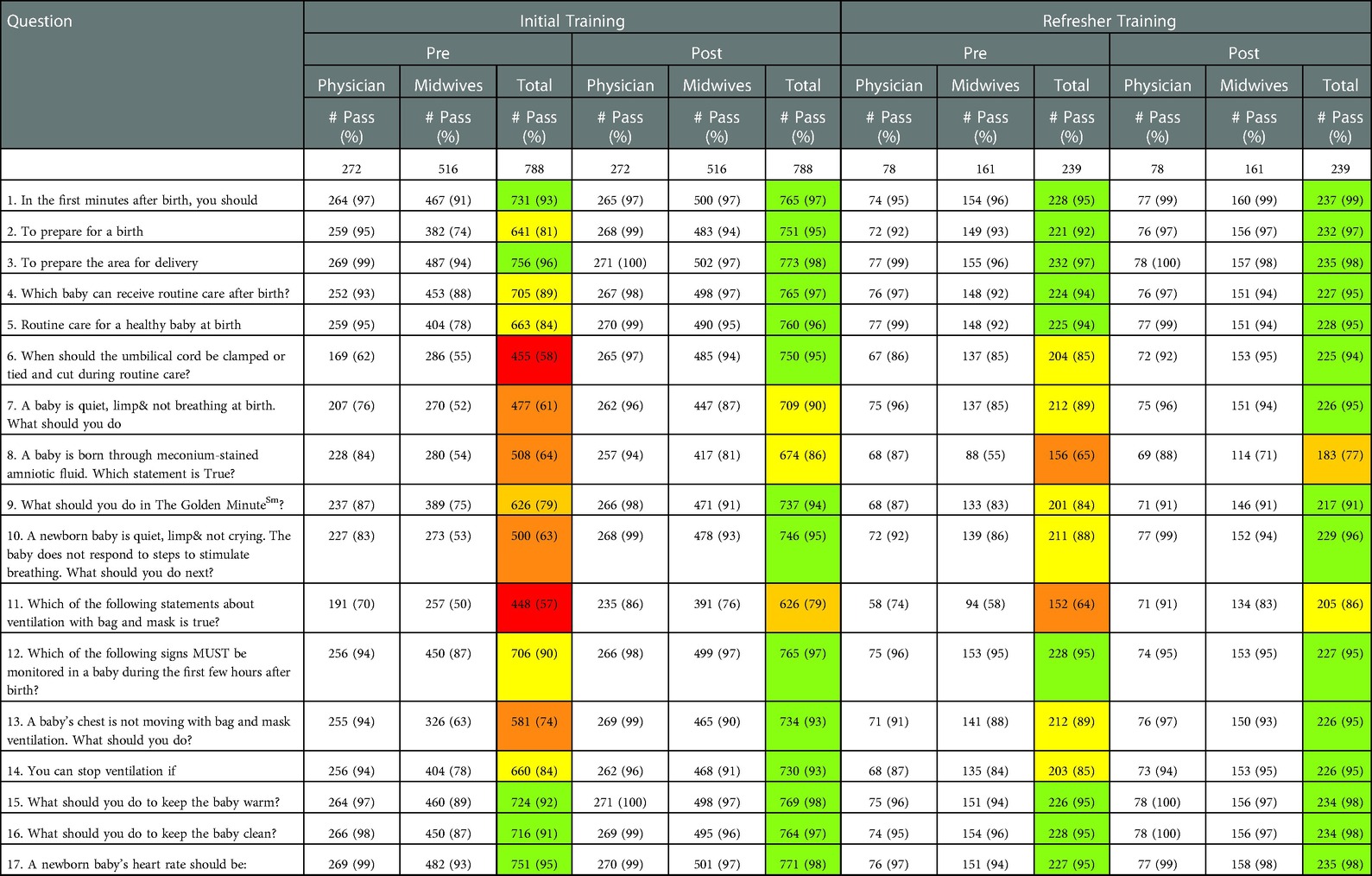
Total 788 trainees (272 physicians and 516 midwives) undertook the initial HBB training. Of these, all the 239 trainees (78 physicians and 161 midwives) who were actively involved as birth attendants received refresher training. Numbers and percentages of trainees passing in individual questions or steps with level wise color coding are provided in Tables 3A–D.
Knowledge assessment – 17 MCQs
In knowledge assessment, at baseline (prior to initial training), for physicians, out of total 17 questions, two questions were graded as Level 4 difficulty (Questions 6, 11) and three were graded as Level 2 (Questions 8, 9, 10) difficulty (Table 3A). The difficulty levels of all questions improved to Level 1 after training with the exception of Question 11 that improved from Level 4 to Level 2. After 6 months, the difficulty level of Question 11 was at Level 3 and for four questions (Questions 6, 8, 9, 14) it was at Level 2 difficulty as compared to difficulty Level 1 observed after the initial training.
At base-line (prior to initial training) midwives found all questions to be above difficulty Level 1 with the exception of three questions i.e., Question 1, Question 3 and Question 17. Of the fourteen questions above difficulty Level 1, one question was of difficulty Level 6 (Question 11), four at Level 5, one at Level 4, four at Level 3 and four at Level 2. After training, four questions remained to be difficult, of these, three questions (Questions 7, 8 and 13) at difficulty Level 2 and Question 11 improved from Level 6 to Level 3. After 6 months, before the refresher training, the midwives found Question 8 and 11 to be of difficulty Level 5 and six other questions (Question 6, 7, 9, 10, 13, 14) at difficulty Level 2. After the refresher training, only two questions remained above difficulty Level 1 i.e., Question 8 at difficulty Level 3 and Question 11 at difficulty Level 2.
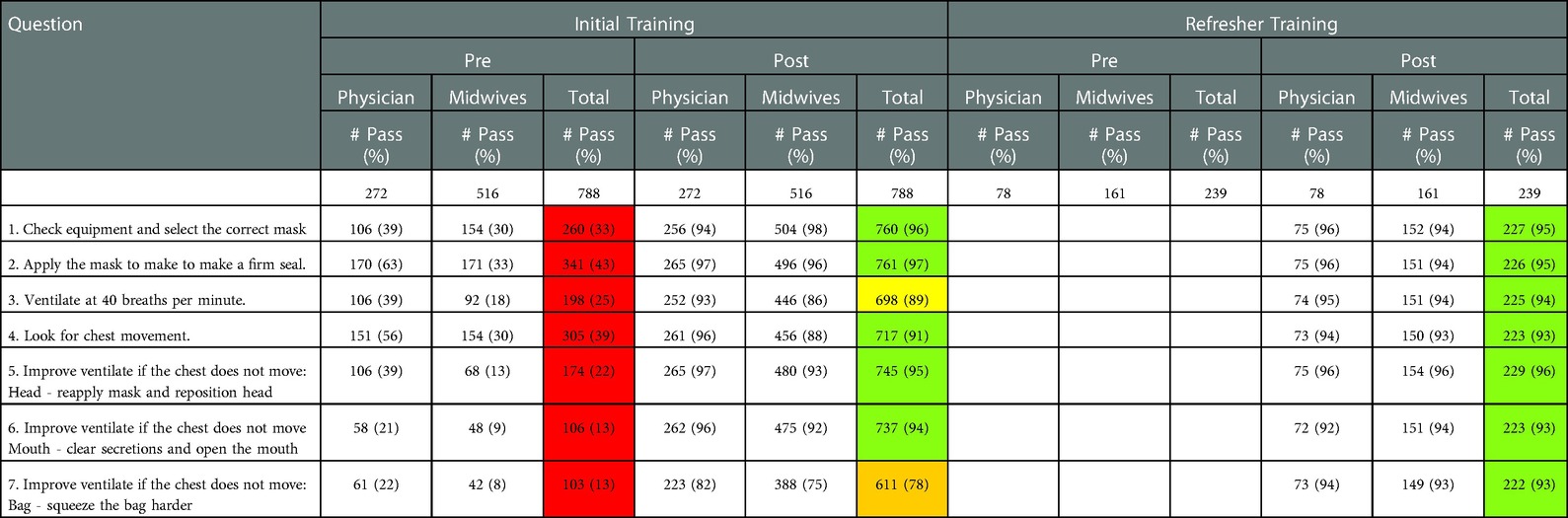
Bag & mask ventilation - 7 skill steps
BMV skill assessment showed that both physicians and midwives found all steps to be of difficulty Level 6 before the initial training (Table 3B). After training, the physicians found only Step 7 to be of difficulty Level 2. The midwives found Step 3 and 4 to be of difficulty Level 2 and Step 7 was at difficulty Level 3. After refresher training, all trainees found the steps to be in the range of difficulty Level 1.
OSCE-A - 13 skill steps
OSCE-A test was conducted after the initial training (Table 1). The physicians performed well in all the steps during this training (Table 3C). After refresher training the physicians faltered on Step 6 on removal of the wet cloth, Step 10 of stimulation of breathing by rubbing the baby, Step 12 regarding cord clamping and Step13 regarding skin-to-skin positioning and communicate with mother (difficulty Level 2). After the initial training, the midwives faltered on Step 4 in preparation of area for ventilation and equipment check, Step 6 on removal of the wet cloth, Step 10 of stimulation of breathing by rubbing the baby and Step 13 on skin-to-skin positioning and communicate with mother. These steps were in the range of difficulty Level 2. After refresher training, midwives again faltered (difficulty Level 2) on Question 6 of removal of wet cloth and Step 10 regarding stimulation of breathing by rubbing the baby.
OSCE-B - 18 skill steps
OSCE-B skill evaluation was conducted after initial training, before refresher, and, after refresher training (Table 1). After initial training, the physicians found five steps (Step 3 recognizing baby not crying, Step 5 stimulation of breathing by rubbing the back, Step 8 on starting the ventilation within Golden Minute, Step 12 call for help and Step 18 monitoring the baby and communicate with mother) to be in the range of difficulty Level 2 (Table 3D). The remaining thirteen steps were within the range of difficulty Level 1. Prior to the refresher training, the evaluation showed that the physicians faltered on all steps (difficult levels ranging from Level 2 to 4) except Step 3 and Step 6 on recognition of failure to cry and failure to breath respectively which were at difficulty Level 1. Step 8 of starting ventilation in Golden Minute, Step 17 of recognition that baby continues to breath and have normal heart rate, and, Step 18 of stopping ventilation, monitoring and communicating with mother were at difficulty Level 4. After the refresher training the performance for Step 8 on starting ventilation in Golden Minute, Step 12 on Call for help, Step 15 on recognition that baby is not breathing but heart rate is normal and Step 17 recognition that baby continues to breath and normal heart rate, failed to reach difficult Level 1 and were at Level 2.
After initial training, the midwives found eight steps difficult - Step 3 on recognition of failure to cry, Step 5 stimulation of breathing by rubbing the back, Step 7 cut the cord and ventilate, Step 8 starting the ventilation within Golden Minute, Step 11 recognition that baby is not breathing, Step 12 call for help, Step 15 recognition that baby in not breathing but heart rate is normal and Step 18 monitoring the baby and communicate with mother. The difficulty level was in the range of Level 2 to 4. Prior to the refresher training, the evaluation showed that the midwives faltered on all the steps (difficult levels ranging from Level 2 to 4).
After the refresher training the performance for Step 8 - starting ventilation in Golden Minute was at difficulty Level 3 whereas Step 12 call for help and Step 18 monitoring the baby and communicate with mother were at level 2.
The summary of the difficulty level grading of individual steps at various time points is presented in the Tables 4A–C.
Discussion
This study was conducted at one of the sites of a large multi-national pre-post study to evaluate the impact of HBB training at facilities on neonatal survival in the communities. In the educational outcomes evaluation, we assessed which knowledge items and skill steps need greater attention and emphasis during training so that optimal performance can be achieved by the trainees. To the best of our knowledge there are few studies world- wide that have conducted an itemized analysis of MCQs or OSCEs used in the HBB training for both physician and nurse learners. This analysis was conducted for the first time in Indian trainees to identify specific deficits in knowledge and performance that can be targeted for improvement and to help strengthen the HBB curriculum. It was observed that both types of BAs found skill testing such as the BMV, OSCE-A and OSCE-B to be more challenging than responding to MCQs. These findings concur with previous studies of resuscitation training that report low concordance between knowledge and skills (10, 19). It has been noted that acquisition of knowledge occurred more easily than skills (20). The physician trainees found both knowledge items and the skill step less difficult to learn as compared to midwives. The same knowledge questions and skill steps that physicians found difficult were also found difficult by the midwives but the degree of difficulty was more for the latter. This was also observed after six months of initial training when knowledge or skill retention was poorer for midwives as compared to physicians and similar questions and steps were found to be difficult (6). Similar findings were observed in the study conducted in Honduras where seventy physicians and nurses participated in the HBB training. It is known that learners arrive with varied prior knowledge and skills. These consistent findings could inform future HBB trainings. It was evident that physicians differed both in awareness of learning strategies and pace of learning compared to the nurses. The program could consider tailoring the training based on learner characteristics and background (21). The physicians and nurses may need to be trained separately as the time to learn can be different. The frequency of subsequent retraining for nurses and physicians could also differ. There could also be a role for incorporating learner-adaptive educational technologies for HBB training that use software and hardware systems that deliver interactive, individualized content by accruing data from a learner to infer what is not understood by the learner so that the simulation models can address those learning needs. Adaptive learning technologies can provide interactive, individualized content that can be delivered at scale. This is particularly relevant for the health personnel who can then train at their convenient times when not on duty.
Among the MCQs, the question that was found to be most difficult and would need attention during future trainings was Question 11 (true of false statements regarding BMV). The midwives also found Question 6 to 14 pertaining to when to clamp cord, recognition of limp baby, response to limp and not breathing baby, steps to be taken for meconium-stained amniotic fluid, what should be done in the Golden Minute, steps to be taken when chest does not move with BMV and when to stop ventilation to be difficult. It was evident that BAs did not perform well in knowledge questions that pertain to resuscitation skills. The trainees need to be well versed with the learner's manual prior to the workshop and the trainers need to explain the resuscitation steps well and carefully using the flip charts.
The MCQs assess clinical knowledge but the OSCEs help evaluate procedural skills, clinical decision making, communication etc during the resuscitation process. OSCEs are considered as standard assessment tools for clinical competence (22). OSCE-A (13 steps) was tested after initial and after refresher training. The midwives who are usually responsible for preparing the area of ventilation and checking equipment were the ones who faltered on it indicating that during routine clinical practice these steps were perhaps not being followed meticulously. Therefore, trainers should not presume that active midwives are routinely practicing these preparatory steps and provide adequate time and attention to teach these steps. The trainees were also not proficient in removal of wet cloth, stimulation of breathing by rubbing the baby, positioning the baby on mother's chest and communicating with her. Again, the trainers should not rely on the clinical experience of midwives and give sufficient attention to these steps for achieving optimum performance among the trainees as removing the wet cloth is important to prevent hypothermia in the newborn whereas stimulation of breathing by rubbing the baby is often enough to establish respiration and avoid BMV (23). We have previously reported the knowledge and skill gaps amongst the BAs and improvement subsequent to trainings (6). We concluded that skills declined more than knowledge over time and that in addition to frequent refresher training the BAs need to practice daily at practice corners established at their clinical sites.
OSCE-B evaluated the comprehensive skill that included the skills and decision-making in routine care, the initial steps of “The Golden Minute”, bag-mask ventilation and additional decision making based on assessment of heart rate after BMV. Most of the BMV steps and OSCE-A steps are incorporated in 18 steps of OSCE-B. The trainees faltered on most of the steps to establish ventilation and even after establishing it they would falter on how to continue to monitor breathing, monitor heart rate and finally how to communicate with the mother. It is possible that the trainees tend to relax after breathing is established and are less attentive towards subsequent monitoring, when to stop and communicate with the mother. This indicates that trainers need to emphasize on all the steps from preparation to establishment of breathing, subsequent stabilization and final communication with the mother for optimum newborn survival. Seto et al. also conducted an itemized analysis of OSCEs. Despite a different site and study population the study did not yield different results from our study. They found similar steps in both the OSCEs to be challenging or have good item discrimination (ability to differentiate between low and high performers) (21). The authors recommended simplification of multi-steps into single tasks, use of global rating scale, discussions on scenarios, more self-reflection to enhance de-briefings and feedbacks. Poor performance in the OSCEs could possibly be attributed to lack of familiarity with the OSCE format or checklists prior to training. Learners may not have sufficient time to practice and there could be difficulty in remembering and integrating the large number of steps into a continuous series resulting in poor performance. Facilitators also need to be experienced and familiarize themselves well with the structured curriculum to teach it effectively (10).
A study done by the architect of HBB at Kenya and Pakistan conducted a formative evaluation of HBB program which included the course evaluation by facilitators and learners using quantitative ratings and qualitative feedback through comments and focus group discussion on structure, course content, materials and assessment tools. They assessed the participants knowledge, skills and performance but did not analyze the individual question or skill steps that were difficult for trainees to perform (10). The participants expressed satisfaction with the program and the knowledge and skills pre/post-program demonstrated significant gains; however, in that study too, majority of participants could not demonstrate mastery of BMV perhaps due to insufficient practice. The participants cited limited time to practice the integration of separate skills. The formative evaluation helped further revise the course materials by including larger illustrations, integrating the skill practice into the presentation of knowledge content, provide additional exercises with guided instructions and provided for increased time to practice and consolidate the skills. Despite the revision in the curriculum, the trainees of our study faltered in both the knowledge and the skill domain.
The strength of this study is that it provides an itemized assessment of the difficulty level of the curriculum to help future trainings. The limitation is that it could be both site and learner specific. The apparently smaller number at the refresher training was due to exclusion of administrative and senior staff who never attended deliveries. All the active birth attendants received refresher training without any sampling to avoid selection bias. Since these are the health care workers who would be attending the deliveries in the real world, our results can be generalized to all birth attendants in similar settings. Standard, uniform training curriculum; carefully maintained integrity of training and evaluation by ensuring uniformity across trainers; and detailed enlisting of monitoring activities between the initial and refresher trainings are the other strengths of our study.
In conclusion, this study has shown that health care workers find certain skills more difficult to learn and retain. HBB training duration and frequency of retraining can be tailored accordingly with greater emphasis on acquisition of these skills during trainings and during the ongoing practice and monitoring. This study will also inform subsequent refinement in the curriculum so that both trainers and trainees will be able to achieve the required proficiency. Further evaluation and additional learner/facilitator assessment data from diverse settings and study populations will help to inform subsequent refinements to the HBB curriculum.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The study was reviewed and approved by the Institutional Review Board of Lata Medical Research Foundation, Nagpur. The ethics approval for the GN HBB study that trained the Nagpur site facilities in HBB have been published previously (6,16,17). Written informed consent was obtained from all trained birth attendants who participated in GN HBB study.
Author contributions
This concept was proposed, designed and overseen at Nagpur, India site by AP, KK, SB and AB in collaboration with PLH. ABP and KK wrote the first draft. PLH and AB edited, revised and reviewed the final version; SB and KK involved in data monitoring and preparation of data tables, input for the first draft; all co-authors provided input, reviewed and approved the final manuscript. All authors contributed to the article and approved the submitted version.
Funding
The GN HBB Study was funded with the grants from Laerdal Foundation, Norwegian Agency for Development Cooperation (NORAD) and by the Eunice Kennedy Shriver National Institute of Child Health and Human Development's Global Network for Women's and Children's Health Research (grant numbers U01 HD058322, U10 HD078439).
Acknowledgments
We thank the Eunice Kennedy Shriver National Institute of Child Health and Human Development's Global Network for Women's and Children's Health Research, NORAD and Laerdal Foundation for funding the GN HBB. We thank all HBB Master Trainers, Facilitators and BAs from the participating facilities who made the HBB implementation possible. We like to acknowledge Alka Dafare (statistician) and Bharati Dhabale (statistician), for the data entry for the site-specific forms and primary tables.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
AAP, American Academy of Pediatrics; ANMs, auxiliary nurse midwives; BAs, birth attendants; BMV, bag mask ventilation; GN, Global Network; HBB, Helping Babies Breathe; HIC, high income countries; LMICs, low and middle-income countries (LMICs); MCQ, multiple choice questions; NICHD, The Eunice Kennedy Shriver National Institute of Child Health and Human Development; OSCE-A, objective structured clinical examinations-A; OSCE-B, objective structured clinical examinations-B.
References
1. Oestergaard MZ, Inoue M, Yoshida S, Mahanani WR, Gore FM, Cousens S, et al. Neonatal mortality levels for 193 countries in 2009 with trends since 1990: a systematic analysis of progress, projections, and priorities. Byass P, editor. PLoS Med. (2011) 8(8):e1001080. doi: 10.1371/journal.pmed.1001080
2. Carlo WA, Goudar SS, Jehan I, Chomba E, Tshefu A, Garces A, et al. Newborn-Care training and perinatal mortality in developing countries. N Engl J Med. (2010) 362(7):614–23. doi: 10.1056/NEJMsa0806033
3. Lawn JE, Lee AC, Kinney M, Sibley L, Carlo WA, Paul VK, et al. Two million intrapartum-related stillbirths and neonatal deaths: where, why, and what can be done? Int J Gynecol Obstet. (2009) 107(Supplement):S5–19. doi: 10.1016/j.ijgo.2009.07.016
4. Patel A, Bang A, Kurhe K, Bhargav S, Prakash A, Arramraj S, et al. Comparison of perinatal outcomes in facilities before and after global Network's Helping babies breathe implementation study in Nagpur, India. BMC Pregnancy Childbirth. (2019) 19(1):324. doi: 10.1186/s12884-019-2480-7
5. Patel A, Khatib MN, Kurhe K, Bhargava S, Bang A. Impact of neonatal resuscitation trainings on neonatal and perinatal mortality: a systematic review and meta-analysis. BMJ Paediatr Open. (2017) 1(1):e000183. doi: 10.1136/bmjpo-2017-000183
6. Bang A, Patel A, Bellad R, Gisore P, Goudar SS, Esamai F, et al. Helping babies breathe (HBB) training: what happens to knowledge and skills over time? BMC Pregnancy Childbirth. (2016) 16(1):364. doi: 10.1186/s12884-016-1141-3
7. Morris SM, Fratt EM, Rodriguez J, Ruman A, Wibecan L, Nelson BD. Implementation of the helping babies breathe training program: a systematic review. Pediatrics. (2020) 146(3):e20193938. doi: 10.1542/peds.2019-3938
8. Helping Babies Breathe Global Development Alliance. Helping Babies Breathe: Lessons learned guiding the way forward. [cited 2022 Feb 18]. Available at: https://www.healthynewbornnetwork.org/hnn-content/uploads/hbb_report_2010-2015.pdf.
9. Niermeyer S. From the neonatal resuscitation program to helping babies breathe: global impact of educational programs in neonatal resuscitation. Semin Fetal Neonatal Med. (2015) 20(5):300–8. doi: 10.1016/j.siny.2015.06.005
10. Singhal N, Lockyer J, Fidler H, Keenan W, Little G, Bucher S, et al. Helping babies breathe: global neonatal resuscitation program development and formative educational evaluation. Resuscitation. (2012) 83(1):90–6. doi: 10.1016/j.resuscitation.2011.07.010
11. Hoban R, Bucher S, Neuman I, Chen M, Tesfaye N, Spector JM. “Helping babies breathe” training in sub-saharan Africa: educational impact and learner impressions. J Trop Pediatr. (2013) 59(3):180–6. doi: 10.1093/tropej/fms077
12. Kc A, Målqvist M, Wrammert J, Verma S, Aryal DR, Clark R, et al. Implementing a simplified neonatal resuscitation protocol-helping babies breathe at birth (HBB) - at a tertiary level hospital in Nepal for an increased perinatal survival. BMC Pediatr. (2012) 12(1):159. doi: 10.1186/1471-2431-12-159
13. Agudelo-Pérez S, Cifuentes-Serrano A, Ávila-Celis P, Oliveros H. Effect of the helping babies breathe program on newborn outcomes: systematic review and meta-analysis. Medicina (Kaunas). (2022) 58(11):1567. doi: 10.3390/medicina58111567
14. Budhathoki SS, Gurung R, Ewald U, Thapa J, Kc A. Does the helping babies breathe programme impact on neonatal resuscitation care practices? Results from systematic review and meta-analysis. Acta Paediatr. (2019) 108(5):806–13. doi: 10.1111/apa.14706
15. World Health Organization, UNICEF. Every Newborn: an action plan to end preventable deaths. [cited 2022 Feb 18]. Available at: https://www.healthynewbornnetwork.org/hnn-content/uploads/Every_Newborn_Action_Plan-EXECUTIVE_SUMMARY-ENGLISH_updated_July2014.pdf.
16. Bang A, Bellad R, Gisore P, Hibberd P, Patel A, Goudar S, et al. Implementation and evaluation of the helping babies breathe curriculum in three resource limited settings: does helping babies breathe save lives? A study protocol. BMC Pregnancy Childbirth. (2014) 14(1):116. doi: 10.1186/1471-2393-14-116
17. Bellad RM, Bang A, Carlo WA, McClure EM, Meleth S, Goco N, et al. A pre-post study of a multi-country scale up of resuscitation training of facility birth attendants: does helping babies breathe training save lives? BMC Pregnancy Childbirth. (2016) 16(1):222. doi: 10.1186/s12884-016-0997-6
18. Seto TL, Tabangin ME, Taylor KK, Josyula S, Vasquez JC, Kamath-Rayne BD. Breaking down the objective structured clinical examination: an evaluation of the helping babies breathe OSCEs. Simul Healthc. (2017) 12(4):226–32. doi: 10.1097/SIH.0000000000000224
19. Carlo WA, Wright LL, Chomba E, McClure EM, Carlo ME, Bann CM, et al. Educational impact of the neonatal resuscitation program in low-risk delivery centers in a developing country. J Pediatr. (2009) 154(4):504–508.e5. doi: 10.1016/j.jpeds.2008.10.005
20. Miller GE. The assessment of clinical skills/competence/performance. Acad Med. (1990) 65(9):S63–7. doi: 10.1097/00001888-199009000-00045
21. Seto TL, Tabangin ME, Josyula S, Taylor KK, Vasquez JC, Kamath-Rayne BD. Educational outcomes of helping babies breathe training at a community hospital in Honduras. Perspect Med Educ. (2015) 4(5):225–32. doi: 10.1007/s40037-015-0214-8
22. Zabar S, Kachur EK, Kalet A, Hanley K. Objective structured clinical examinations: 10 steps to planning and implementing OSCEs and other standardized patient exercises. New York: Springer (2013). 92.
Keywords: HBB, Helping Babies Breathe, training, neonatal resuscitation, knowledge, skills
Citation: Patel AB, Bang A, Kurhe K, Bhargav S and Hibberd PL (2023) What Helping Babies Breathe knowledge and skills are formidable for healthcare workers?. Front. Pediatr. 10:891266. doi: 10.3389/fped.2022.891266
Received: 7 March 2022; Accepted: 30 December 2022;
Published: 30 January 2023.
Edited by:
Venkataseshan Sundaram, Post Graduate Institute of Medical Education and Research (PGIMER), IndiaReviewed by:
William J. Keenan, Saint Louis University, United StatesDouglas McMillan, Dalhousie University, Canada
© 2023 Patel, Bang, Kurhe, Bhargav and Hibberd. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Akash Bang ZHJha2FzaGJhbmdAZ21haWwuY29t
Specialty Section: This article was submitted to Neonatology, a section of the journal Frontiers in Pediatrics
 Archana B. Patel
Archana B. Patel Akash Bang
Akash Bang Kunal Kurhe
Kunal Kurhe Savita Bhargav1
Savita Bhargav1