- 1Department of Ultrasound, The Affiliated Hospital of Southwest Medical University, Luzhou, China
- 2Department of Pathology, The Affiliated Hospital of Southwest Medical University, Luzhou, China
Facial artery pseudoaneurysms are rare and mostly a result of blunt injury. Since the facial arteries are well protected by facial soft tissue and the lumen of the facial artery is thin and small in diameter, a sharp injury usually leads to complete transection rather than partial laceration of the blood vessel. As a non-invasive method, ultrasound does not involve radiation and sedation. Diagnosis of facial artery pseudoaneurysms is most commonly made with ultrasound, and Doppler ultrasound is essential. On grayscale imaging, facial artery pseudoaneurysms often appearanced of a fluid collection, Color Doppler imaging often show a well-defined swirl pattern named “yin and yang sign,” the Spectral Doppler showed a diagnostic “to and fro” two-phase bidirectional arterial blood flow spectrum. It’s particularly for the examination of facial artery pseudoaneurysms in children. Here, we report a case of facial foreign body abscess and facial artery pseudoaneurysm in a 19-month-old child 1 week after a sharpness injury that was diagnosed by ultrasound.
Case Report
A 19-month-old girl who suffered from pain and bleeding on the right cheek due to a puncture from a glass bottle was presented to the local hospital. She was treated with local anesthesia and debridement and suturing. One week later, the suture was removed. One week after the suture removal, the child had redness and swelling on the right cheek wound which was aggravated for 3 days. Upon physical examination, the right cheek was red and swollen, the skin temperature was high, and a black necrotic area with a diameter of about 0.5 cm was seen in the center. The surface was palpable and throbbing. When squeezed, the wound was painful and oozed pus. In addition, systolic murmurs could be heard on auscultation. A computerized tomography (CT) scan of the head and face (plain scan) showed a short strips of “U” shaped high density structure (red arrow) due to foreign body in the right cheek space with a diameter of about 1.8 cm (Figure 1). The formation of a foreign body in the right cheek space with local hematoma was considered. Upon ultrasound examination, an irregular dark area was seen on the right cheek, a “C” type strong echo was seen in the dark area, and color Doppler flow imaging (CDFI) showed no blood flow signal in the dark area. Additionally, a “C” type strong echo was seen in the dark area immediately adjacent to the irregular dark area, and a round cystic mass with a diameter of about 1.7 × 1.7 cm was seen on the deep surface with clear boundaries and obvious pulsation. CDFI showed the red and blue blood flow signals are shown as “yin and yang sign” (Figure 2), which was continuous with a branch of the facial artery (Figure 3). PW showed the “bi-phase bidirectional” arterial blood flow spectrum at the breach. Based on these findings, the patient was diagnosed with a foreign body on the right cheek with surrounding abscess and facial artery pseudoaneurysm. Surgery was performed immediately. A ring-shaped glass bottle with a length of about 1.2 cm and a diameter of 0.5 cm and three pieces of rice-sized glass slag were removed during the operation (Figure 4). A pseudoaneurysm with a diameter of about 1.8 cm was seen on the deep side next to the glass foreign body, and the tumor was ligated and excised. Pathological analysis revealed that the tumor wall was composed of mixed thrombus with organization (Figure 5). The patient was followed up after the operation, and the wound healed well.
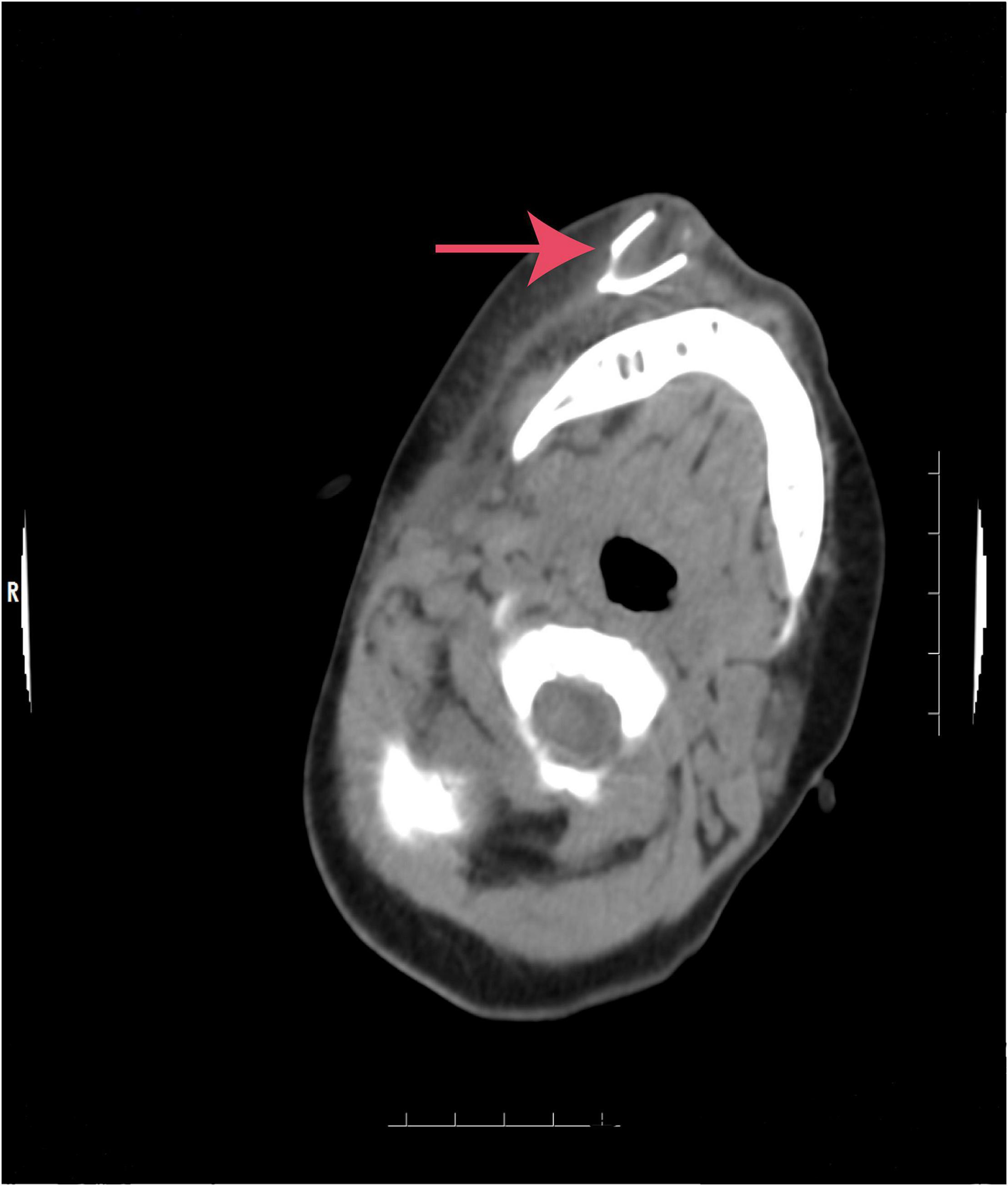
Figure 1. Computerized tomography (CT) scan of the head and face. A short strips of “U” shaped high density structure (red arrow) due to foreign body in the right cheek.
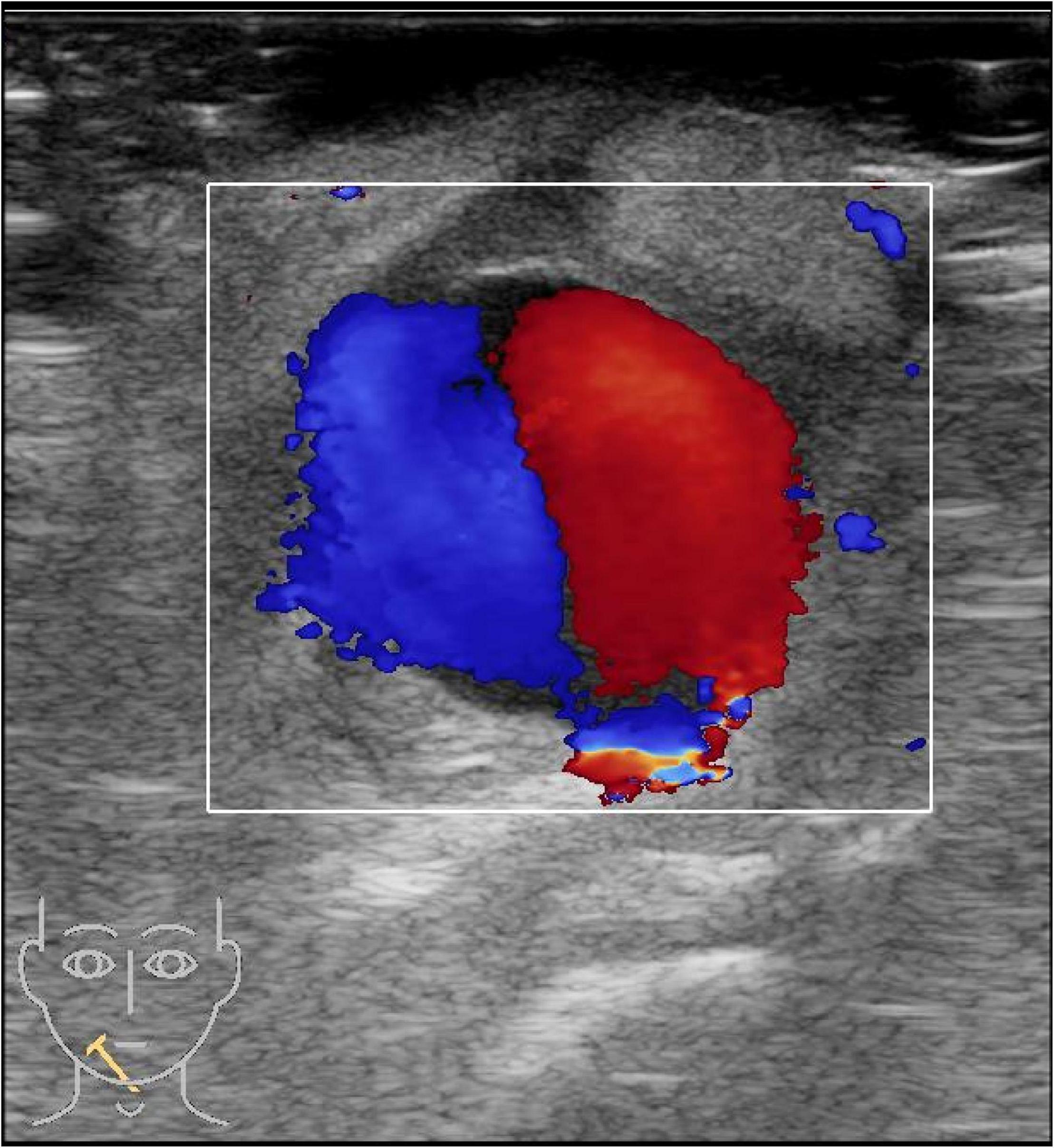
Figure 2. A color Doppler ultrasound of the right cheek. The red and blue blood flow signals are shown as “yin and yang sign”.

Figure 3. A color Doppler ultrasound of the right cheek. The pseudoaneurysm is connected to a branch of the facial artery.
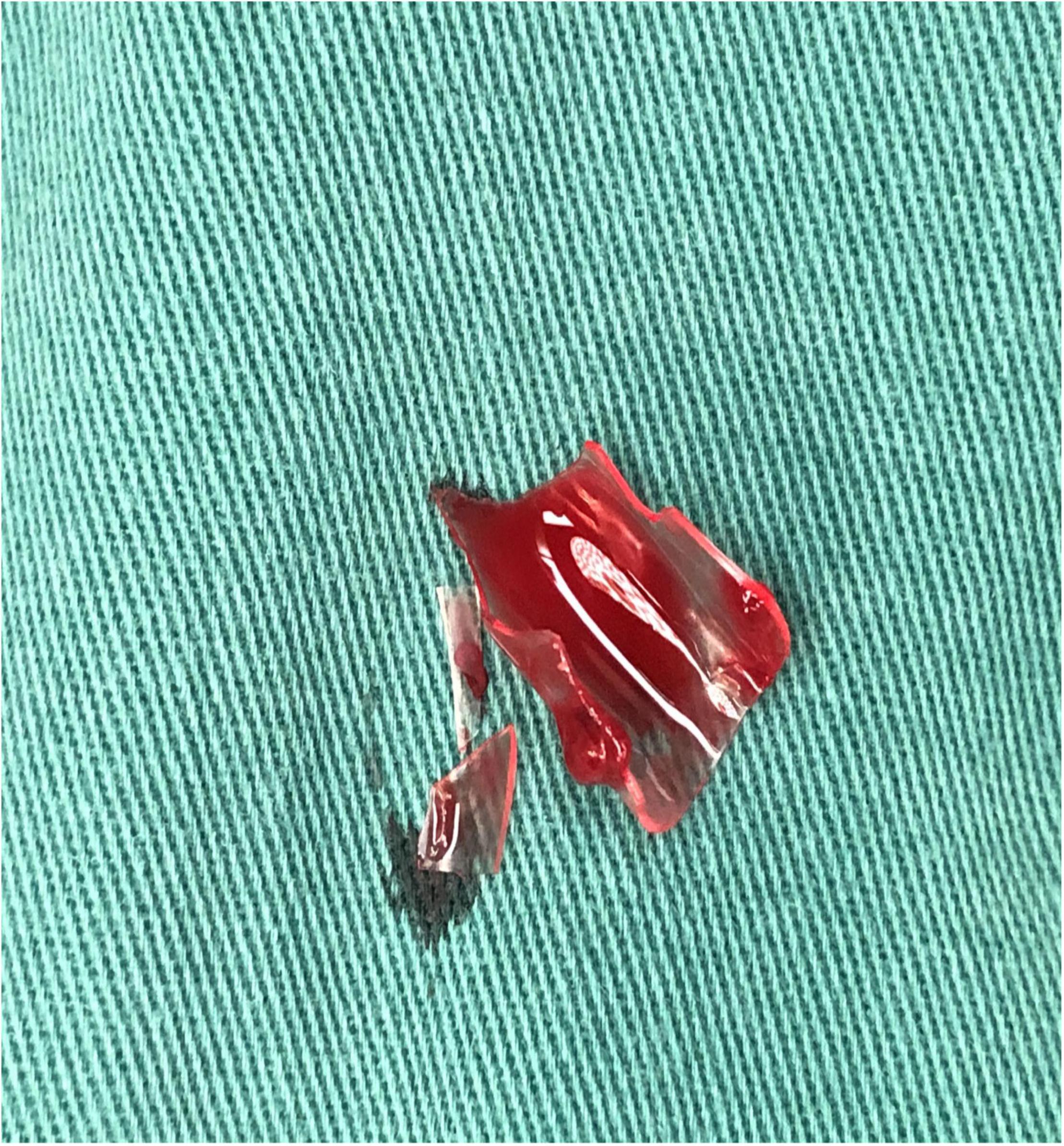
Figure 4. Surgical specimen. A ring-shaped glass bottle with a length of about 1.2 cm and a diameter of 0.5 cm and three pieces of rice-sized glass slag were removed during the operation.
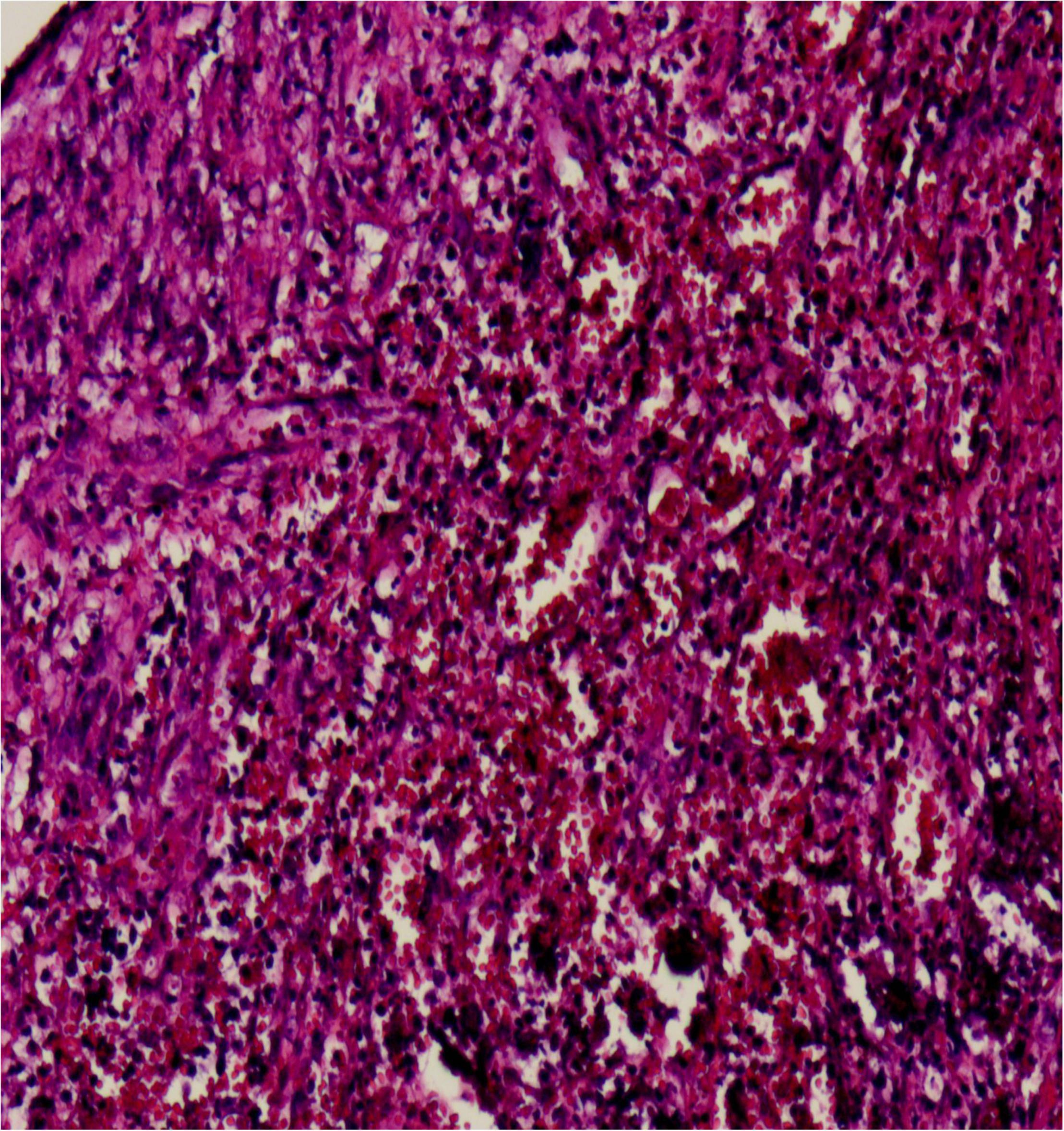
Figure 5. Microscopic image of the lesion (hematoxylin and eosin staining, magnification ×200). Showing the tumor wall was composed of mixed thrombus with organization.
Discussion
About 85% of craniofacial pseudoaneurysms involve the superficial temporal artery because the artery passes through the frontal bone between the temporal and frontal muscles and lacks muscle tissue protection. Other arteries that can be involved include the maxillary artery and the facial artery. Maxillary artery pseudoaneurysm is usually caused by iatrogenic injury, and facial artery pseudoaneurysm is often secondary to facial blunt injury (1). Facial arteries are protected by facial soft tissues. They have a thin lumen and small diameter (about 1.3–2.2 mm). Sharpness damage usually leads to a complete transection; thus, part of the vessel wall rupture is rare (2). Previously reported injury factors include sudden trauma, gunshot wounds, glass, intraoral stents, infections, etc. (3–5). In this case, the pseudoaneurysm was close to the foreign body, the abscess surrounded the upper part of the pseudoaneurysm, and the pulsatile mass on the face appeared after suture removal; so risk factors included iatrogenic injury, glass foreign body injury, and infection, which have not been reported previously. The diagnosis mainly included clinical manifestations such as pulsating masses and systolic murmurs and imaging examinations. Magnetic Resonance Angiography (MRA) and Computed Tomography Angiography (CTA) can comprehensively display the shape and branch of the facial artery while excluding more extensive lesions (6), but this latter requires radiation and needs to be braked during the inspection, so it has relatively poor practicality in children. Ultrasonography is the best modality to assess these pseudoaneurysms (7), as a non-invasive examination method, requires no radiation and the patient does not need to remain stationary; thus, has diagnostic value for pseudoaneurysms, particularly for the detection of facial artery pseudoaneurysms in children (8, 9). In our case, the grayscale imaging showed an anechoic zone with weak and echogenic light spots rotating and fluttering, thrombus attachment on the wall, and pulsatile tubular anechoic on the periphery connected to the dark zone. Color Doppler is useful for the diagnosis, to evaluate the neck of pseudoaneurysm and to trace the feeding artery (10). The color Doppler showed a systolic breach with bright and colorful; the blood flow in the tumor body was red and blue depicting the “yin and yang sign” due to turbulent internal flow (11). Chen et al. suggested that the “yin and yang sign” is diagnostic of a pseudoaneurysm (12). Lastly, the spectral Doppler showed a diagnostic “to and fro” two-phase bidirectional arterial blood flow spectrum. This occurs due to blood flowing into the tumor body during systole and out of the tumor body during diastole. Ultrasound provides excellent detection and characterization of soft tissue foreign bodies. According to the foreign body biological characteristics of soft tissues, they are hyperechoic to varying degrees on ultrasound and similar in shape to the foreign body morphology. High frequency linear array transducers are the most useful in detection of radiopaque and non-radiopaque Soft tissue foreign bodies (13). The utility of ultrasound can also be applied intraoperatively, allowing the surgeon to locate the foreign body in real-time. In the case of a false facial artery aneurysm, facial artery ligation is the preferred treatment method as it has the advantage of a simple operation and low complication rates (3, 4).
Conclusion
We suggest that it is necessary to examine and follow up the wound site after an acute facial injury. Ultrasound should be used as a non-invasive, safe, and effective method for the diagnosis of facial artery pseudoaneurysm.
Ethics Statement
Ethics review and approval/written informed consent was not required as per local legislation and institutional requirements.
Author Contributions
RK wrote all drafts. JZ discussed the meaning of the draft. JD collected all the references. TX carried out the pathology and collected the clinical data. ML offered conception and finalized the draft. All authors read and approved the final manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Ali ZA, Malis DD, Wilson JW. Pseudoaneurysm of the maxillary artery after a stab wound treated by endovascular embolization. J Oral Maxillofac Surg. (2007) 65:790–4. doi: 10.1016/j.joms.2005.11.070
2. Myer CM III, Donegan JO. Traumatic aneurysm of the proximal superficial temporal artery. Head and Neck. (1982) 5:181–5. doi: 10.1002/hed.2890050214
3. Payami A, Montazem AH. Surgical treatment of facial artery pseudoaneurysm following blunt trauma: report of a case. J Oral Maxillofac Surg. (2017) 75: 362–2.e5. doi: 10.1016/j.joms.2016.10.008
4. Ribeiro-Ribeiro AL, de Melo Alves Junior S, de Jesus Viana Pinheiro J. Traumatic pseudoaneurysm of the facial artery: late complication and effects on local blood flow. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. (2011) 112:e4–9. doi: 10.1016/j.tripleo.2011.03.018
5. Abulfaraj MM, Deanehan JK. Facial Artery Pseudoaneurysm in a Child Diagnosed With Point of Care Ultrasound. Pediatr Emerg Care. (2019) 35:733–5. doi: 10.1097/PEC.0000000000001943
6. Namin A, Starnes SE, Plikaitis CM. Pediatric craniofacial pseudoaneurysm with a variable history of antecedent trauma. J Craniofac Surg. (2015) 26:796–9. doi: 10.1097/SCS.0000000000001425
7. Srinivasan S, Lohan R, Tan HK, Chung R, Babu SB. Usefulness of ultrasonography in diagnosis, percutaneous management and follow up of post-traumatic scalp pseudoaneurysms. J Clin Ultrasound. (2018) 46:558–61. doi: 10.1002/jcu.22580
8. Madani M, Veznedaroglu E, Pazoki A, Danesh J, Matson SL. Pseudoaneurysm of the facial artery as a late complication of bilateral sagittal split osteotomy and facial trauma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. (2010) 110:579–84. doi: 10.1016/j.tripleo.2010.03.021
9. Jenq KY, Panebianco NL, Lee PA, Chen EH, Dean AJ. Diagnosis of a facial artery pseudoaneurysm using emergency bedside ultrasound. J Emerg Med. (2010) 38:642–4. doi: 10.1016/j.jemermed.2008.03.046
10. Mennitt K, Deol M, Gao J. Emergency color Doppler sonography of the extremity artery: a pictorial essay. Clin Imaging. (2017) 42:240–8. doi: 10.1016/j.clinimag.2017.01.005
12. Chen SP, Su X. Superficial Temporal artery arteriovenous fistula and pseudoaneurysm: the yin-yang sign. Radiology. (2020) 294:508. doi: 10.1148/radiol.2019191983
Keywords: traumatic, glass, foreign body, abscess, aneurysm, face
Citation: Kuang R, Zhou J, Deng J, Xia T and Li M (2022) Case Report: A Case of a Child With Facial Foreign Body Abscess and Facial Artery Pseudoaneurysm. Front. Pediatr. 10:886031. doi: 10.3389/fped.2022.886031
Received: 11 March 2022; Accepted: 05 April 2022;
Published: 28 April 2022.
Edited by:
Emanuele Monda, University of Campania Luigi Vanvitelli, ItalyReviewed by:
Miguel Montorfano, Hospital de Emergencias Dr. Clemente Álvarez, ArgentinaFabio Sandomenico, Ospedale Buon Consiglio Fatebenefratelli, Italy
Copyright © 2022 Kuang, Zhou, Deng, Xia and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mingxing Li, bG14NTI2QHNpbmEuY29t
†These authors have contributed equally to this work
 Rong Kuang
Rong Kuang Jing Zhou1†
Jing Zhou1†