- 1Neonatal Department, Hunan Children's Hospital, Changsha, China
- 2Nursing Department, Hunan Children's Hospital, Changsha, China
- 3Faculty of Health, University of Plymouth, Plymouth, United Kingdom
Background: There are no specific validated questionnaires assessing satisfaction of family-centered care experienced by parents of infants hospitalized in Chinese Neonatal Intensive Care Units (NICU).
Aim: To adapt and test the reliability and validity of the Chinese version of the EMPATHIC-30 questionnaire in NICU settings.
Methods: A prospective, cross-sectional design was adopted. The EMPATHIC-30 questionnaires were completed by parents of infants admitted to one of the four NICUs at Hunan Children's Hospital, China, between November 2018 and 2019. Inclusion criteria were parents whose infants were admitted to the NICU for at least 5 days. Exclusion criteria were parents whose children were discharged within 5 days after admission or whose infants died in the NICU. Reliability was tested with Cronbach's alpha. The congruent validity was tested using Spearman's Rank correlation analysis, and the non-differential validity was tested using Cohen's d.
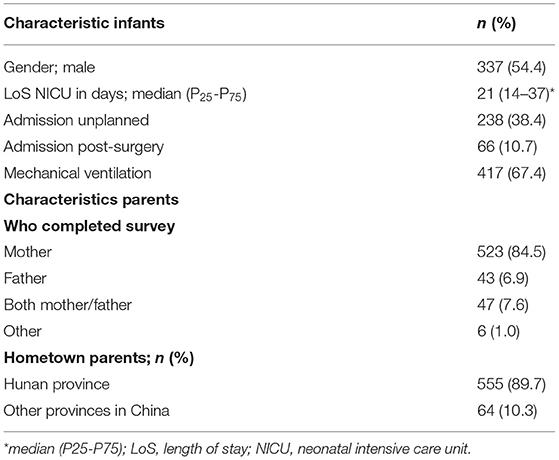
Results: Parents of 619 infants discharged from the NICUs completed and returned the questionnaire. Most infants were male (n = 337, 54.4%) and infants' length of stay was a median of 21 days (IQR = 14–37). Mostly, mothers completed the questionnaire (n = 523, 84.5%). The Cronbach's alpha values of the five individual domains were between 0.67 and 0.95, and the alpha of the total questionnaire was.90, providing an adequate internal consistency. Congruent validity was measured by correlating the five domains with four standard satisfaction scales, documenting a weak correlation (rs −0.025–0.327). Non-differential validity showed some significant effect size between four binary variables (mechanical ventilation, unplanned admission, admission after surgery, length of stay) four of the five domains.
Conclusion: The Chinese version of EMPATHIC-30 questionnaire showed acceptable psychometric properties. This instrument might be considered a suitable instrument to measure parent satisfaction among Chinese parents whose infants are admitted to an NICU. Measuring parent satisfaction with this instrument might contribute to improving family-centered care initiatives in NICUs with Chinese parents.
Introduction
Integrating patients' views into the development of patient-reported experience measures is important to capture the items that matter most to the patients (1, 2). Satisfaction instruments are often designed for hospital-wide patient satisfaction assessment and do not specifically address the various specialties within a hospital setting (3, 4). Within pediatrics, the family-centered care (FCC) approach is well developed, and parents are usually involved in the care of infants and children (5, 6). Consequently, satisfaction instruments for specific pediatric populations have been developed (7–9).
Family-centered care practices encourage parents to participate in the care and decisions of their children (10). Neonatal Intensive Care Unit (NICU) settings are environments with a complexity of treatments and care for critically ill infants. Admission to a NICU is often acute, and parents have little opportunity to shape expectations about the care for their infants. Still, they often face critical decisions and can experience stress during their admission (11–13). Standardized assessment of the experiences of parents in the care of their infants in the NICU is not formally assessed, which could potentially provide data for improving clinical practice.
Studies on patient satisfaction seem to be primarily aimed at assessing the care, with little regard for the overall experiences of perceived care (14). The value of satisfaction outcomes is the ability to benchmark practices that can lead to quality improvements. As such, a multidisciplinary approach is recommended, and the involvement of parents must be incorporated in these initiatives (15). The implementation of parent satisfaction outcomes in NICU settings provides a closer collaboration between parents and healthcare professionals that, ultimately, can improve the care of critically ill neonates and their parents (16).
In NICU, the parent satisfaction questionnaire, EMPATHIC-N, has been developed and used in several countries (17–19). This 57-item questionnaire has similarities with the short version of the EMPATHIC-30, developed in pediatric intensive care units (PICU) (20). This short version has been validated in PICU, NICU, and pediatric wards in Australia and showed good reliability and validity metrics (21). Therefore, the EMPATHIC-30 questionnaire can be considered a valuable instrument to measure parent satisfaction in pediatric and neonatal settings.
The EMPATHIC-30 questionnaire has been translated, culturally adapted, and validated among 101 parents in a Chinese PICU (22). To our knowledge, there are no validated questionnaires in Chinese to assess the satisfaction of parents of infants hospitalized in a NICU. Therefore, the aim of this study is to adapt and test the reliability and validity of the Chinese version of the EMPATHIC-30 questionnaire in NICU settings.
Materials and Methods
Setting
The setting of the study is the neonatal department at the stand-alone Hunan Children's Hospital, a regional tertiary center in Changsha, China. The department has four NICUs. NICU-1 is a 40-bed ward, admitting critically ill preterm infants, including mechanical ventilation; NICU-2 is a 60-bed ward, admitting stable term infants; NICU-3 is a 60-bed ward, admitting stable preterm infants; NICU-4 is a 40-bed ward, admitting critically term infants, including mechanical ventilation. The annual admission rate in 2018–2019 of all four NICUs was around 6,200 infants.
Population and Recruitment
Inclusion criteria were parents whose infants were admitted to one of the four NICUs for at least 5 days. The exclusion criteria were parents whose children were discharged within 5 days after admission. The rationale for excluding these parents was the fact that many parents are unable to visit the NICU in these first days because the mothers were admitted to the maternity unit in another hospital or if mothers wished to follow the traditional 30-day confinement period. This Chinese tradition, zuò yuè zi (sitting the month), expects new mothers to stay home for a month to recover from childbirth. Also excluded were parents whose infants died in the NICU because these parents might have different views, and their discharge planning is different.
Non-probability sampling was used in our study. The sample size was calculated with the software G * Power 3.1 using the data of the development study of the EMPATHIC questionnaire (23). A sample size of 134 participants was estimated using the two-tailed test priori Wilcoxon–Mann–Whitney test for two independent groups, with an effect size of 0.5, an α of 0.05, and a power of 0.8. The data collection period was scheduled for 4 months, with the aim to recruit at least 134 parents from each individual participating NICU, with a total of 536 parents from all participating NICUs. Considering an estimated response rate between 30 and 40% in this type of research, we expect to recruit between 600–800 parents who will respond to the questionnaire. Data were collected between November 2018 and November 2019. Within this time, the total data collection time was 4 months as the study was paused for 8 months due to the recruitment of parents into an international study using other parent outcome measures.
Recruitment took place by the nurses in the NICUs. Parents were provided an invitation letter, consent form, and the EMPATHIC-30 Chinese questionnaire on the day of discharge. Once completed, the parents could deposit the completed questionnaire in specially dedicated return boxes in the NICUs. Unfortunately, the recruitment details of how many parents received the study invitation letter and the questionnaire were not completely recorded by the staff nurses. This limited us from calculating the response rate.
Instrument
The EMPATHIC-30 has been translated and validated for the PICU at the Children's Hospital of Fudan University in Shanghai (22). A 10-step translation process included forward and backward translation followed by testing the instrument for cognitive equivalence by asking 10 parents. Debriefing among researchers took place during the process. The results of the validation testing were positive. The congruent validity of the instrument showed adequate correlation with four gold standard questions measuring overall satisfaction. Cronbach's alpha of the total score (30 items) was 0.96, and the split-half reliability coefficient of the total score was 0.879.
We accepted this version and reassessed the translation and cultural adaptation by consulting local parents to ensure the Chinese version can be adapted for parents whose infants are admitted to the NICU. The research team organized a parent consultation round with 10 mothers who have been involved in FCC in our NICUs. All mothers reported that they found the questionnaire easy to understand and that the answer option scale was easy to follow. We estimated that the average completion time of the questionnaire was around 15 min. After the consultation with the parents, few changes were made related to the wording of items to reflect the readability and understandability as suggested by the parents. The final version of the EMPATHIC-30 Chinese version for NICUs is provided in Supplementary Material 1.
Data Analysis
Data analysis was performed using the Statistical Package for Social Scientists (SPSS, version 19.0). Descriptive statistics and non-parametric tests of difference were applied, and significance was set at p < 0.05.
The reliability of the questionnaire was assessed using Cronbach's alpha as a measure of internal consistency of the items within the five domains of the EMPATHIC-30 questionnaire and the total scale of the 30 items. Preferably, a Cronbach's alpha of >0.70 represents satisfactory reliability estimates (24, 25). The Spearman's Rank correlation for estimating the relationship between the statements on the domain level and four overall satisfaction-with-care questions (recommend NICU, return to NICU if needed, overall satisfaction with doctors, and overall satisfaction with nurses) was used for congruent validity. The non-differential validity was assessed by Cohen's d of the overall means of the individual domains and levels of four binary variables (mechanical ventilation, unplanned admission, admission after surgery, and length of stay). Means and standard deviations on the item level were calculated to determine the outcome of the satisfaction items.
Ethics
Ethical approval of the study was granted by the Ethical Committee of Hunan Children's Hospital (Reference No. HCHLL-2018-34). All the participants were invited by means of an information letter, outlining the aim and methods of the study. Participation was voluntary and all questionnaires were anonymous. Written and signed consent forms were collected.
Results
A total of 619 questionnaires were returned between November 2018 and November 2019. Mothers were the most frequent parents who completed the questionnaire (n = 523; 84.5%). The characteristics of infants and parents are presented in Table 1.
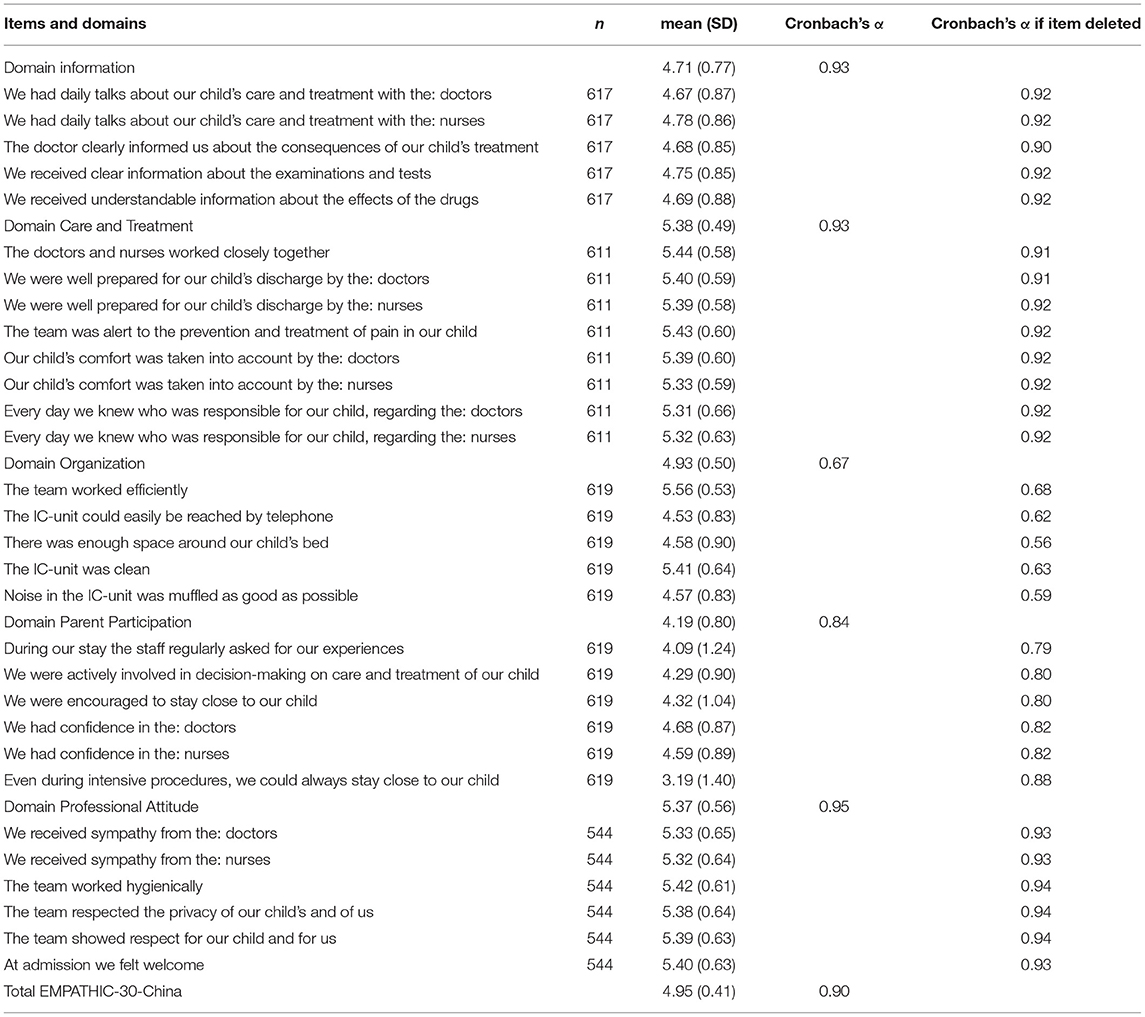
Of the 30 individual items, 14 items (46.7%) scored a mean value <5.; all five items in the domain Information, three of the five items in the domain Organization, and all six items in the domain Parent Participation (Table 2). The item “Even during intensive procedures, we could always stay close to our child” scored the lowest among all the items (mean, 3.19; SD, 1.40). If this item was deleted from the domain Parent Participation, the alpha of the domain would increase from 0.84 to 0.88.
The Cronbach's alpha values on the domain level were between 0.67 and 0.95. The domain Organization had the lowest alpha (0.67), while the Cronbach's alpha of the total scale was 0.90 (Table 2).
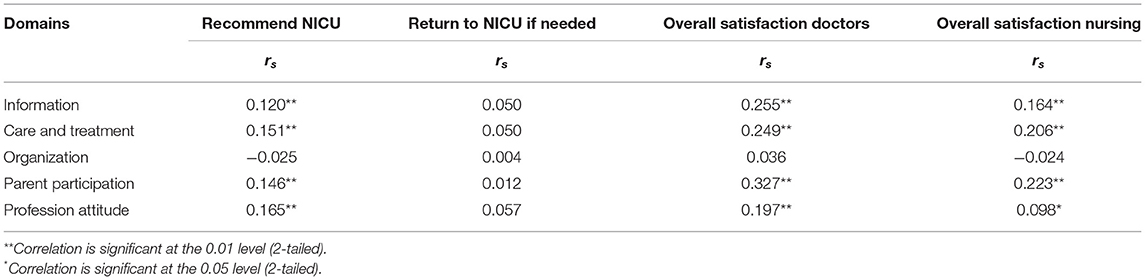
The congruent validity of the questionnaire was assessed by calculating the correlation between the answers of the five domains and the four standard satisfaction questions (recommend NICU, return to NICU if needed, overall satisfaction with doctors, and overall satisfaction with nurses). Overall, there was a weak correlation between the domains and the standard satisfaction scales (Table 3).
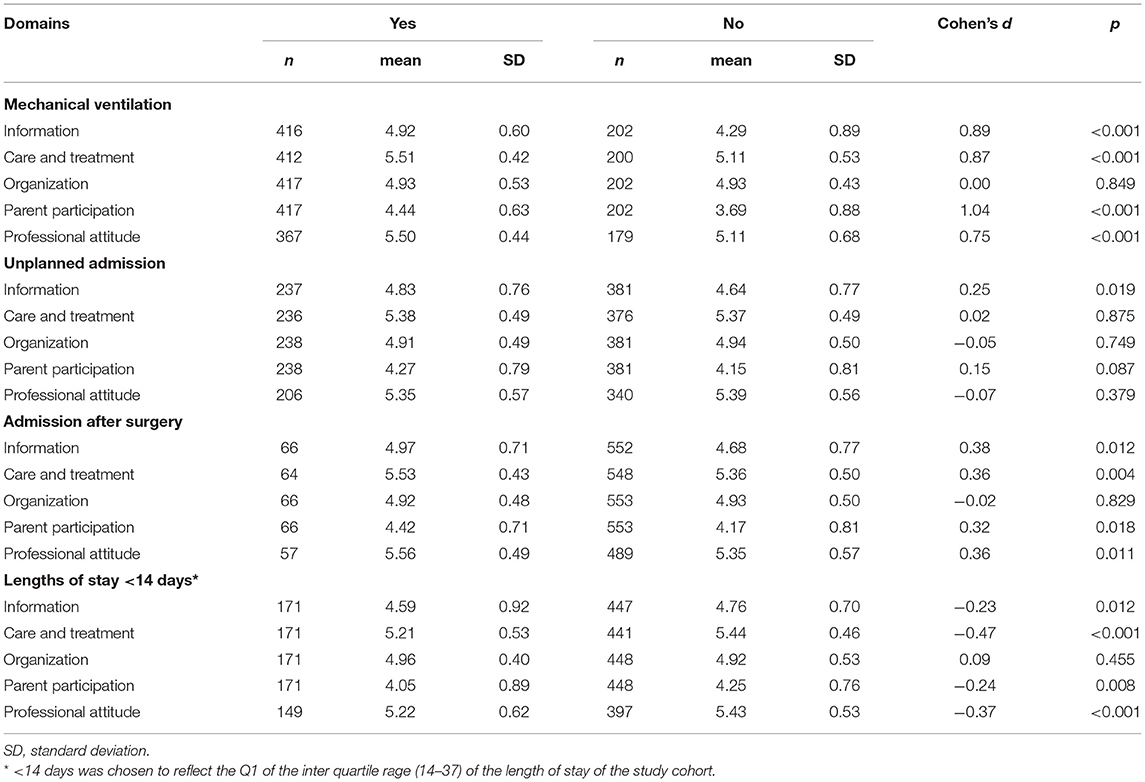
The non-differential validity, comparing the mean score in each domain between the binary characteristics of the infants, showed a large effect size in four of the domains related to mechanical ventilation of the infants and in two domains related to the length of stay. The parents whose infants had mechanical ventilation were more satisfied compared to the parents whose infants had no mechanical ventilation in the domains Information, Care and Treatment, Parent Participation, and Professional Attitude (Table 4). In the “unplanned admission” group, only a modest effect size in the domain Information was significant (Cohen's d, 0.25; p = 0.019). Although the cases in the variable “admission after surgery” were small, the effect size of the Cohen's d was moderate between 0.32 and 0.36, p < 0.02. In terms of the infants' length of stay, the parents in the <14-day group were less satisfied compared to the parents in the ≥14-day group in three domains of the questionnaire: Cohen's d between −0.47 and −0.23, p < 0.013 (Table 4).
Discussion
The aim of the study was to validate the Chinese version of the EMPATHIC-30 among parents in NICU settings. The main findings of our validation demonstrated that the psychometric properties of this version are acceptable. The reliability estimates were very good for most domains, and the validity outcomes showed a weak correlation with other satisfaction scales. We chose this questionnaire because the EMPATHIC-30 questionnaire has been validated and used in several other countries and in NICU settings (26–29). Having a Chinese version of the EMPATHIC-30 for NICU settings allows us to benchmark parents' satisfaction data with national and international colleagues.
In our study, the items in the domain Parental Participation had the lowest mean scores. Although the Cronbach's alpha was good in this domain (.84), the possible reason is that the concept of FCC in our neonatal department is still in a developmental phase. Several FCC interventions have been implemented in our NICUs, demonstrating positive outcomes of infants and parents (30–32). However, we recognize that limitations in our FCC approach still exist, such as the exclusion of parents during medical rounds and not all staff are trained or prepared in daily communications with parents.
The findings of our study indicated that the parents rated 14 items below 5 on the 6-point Likert scale. Other similar studies using the EMAPTHIC-30 reported either similar low ratings or extremely high ratings. The study in South Africa reported high scores on most of the EMPATHIC-30 items in the PICU (33). Their lowest response scores were found in one item in the domain Information (information about effect of the drugs) and two items in the domain Parental Participation (regularly asked of our experiences and actively involved in decision). In contrast, the Turkish EMPATHIC-30 study in NICU settings reported no mean score >5 while using the same 6-point Likert scale. There were, however, no items with a mean score below 3 (26). The differences might indicate that a larger multinational cultural study is needed to identify factors in measuring parent satisfaction in different settings and different cultures. Recent reports have demonstrated the impact of the COVID-19 pandemic on family satisfaction in adult intensive care (34) or described the impact of the pandemic on zero separation of parents in the NICU (35). Our study period was before the COVID-19 pandemic. While the pandemic changed the FCC practices in our NICUs by limiting the visitation, further research is needed to explore the impact of COVID-19 on FCC practices. Reports have documented that the pandemic challenged the well-being of parents in the NICU, and stronger breastfeeding support was needed (36, 37).
There are several study limitations to address: First, our study was conducted in only one hospital setting, limiting the generalizability of the Chinese version of the EMPATHIC-30 in other Chinese NICUs or Chinese parents across the world. Secondly, we did not assess the test-retest validity of the instrument. Also, the time frame of the data collection might have influenced the results. During the study data collection period, we paused recruitment due to a family-integrated care study using other parent outcome measures. This study might have influenced NICU staff behaviors and attitudes on FCC that could have influenced the results of the parents after we resumed data collection. For example, this study included specific FCC education and training for doctors and nurses, which influenced the support to the parents. Thirdly, the questionnaires were mainly completed by the mothers. Fathers might have different opinions of the perceived care in the NICU, and it is suggested to maximize the efforts to include fathers in the care and support father so their voices are heard (13). Finally, we acknowledge the limitation of the EMPATHIC-30 questionnaire, not including allied health professionals. Most NICUs are expanding their teams with other health professionals, such as physiotherapists, psychologists, and social care workers. Evaluating their services should be recognized and could be the next step in further refining the questionnaire.
Conclusion
The Chinese version of the EMPATHIC-30 performed acceptably on the reliability and validity testing among a large group of parents in the NICUs. The parents in our study had unique experiences and needs during their NICU stay, which have been translated in their responses to the items in the EMPATHIC-30-China questionnaire.
Our validated Chinese parent satisfaction questionnaire is timely and contributes to the international development of validated pediatric patient-reported outcome measures (PREMs) (38). This global expansion has been highlighted in a recent review, identifying 83 studies from 14 countries, describing pediatric PREMs (39). Most of the identified PREMs in this review include features that are related to patient- and family-centered care pratices, including shared decision-making and respecting the children and family values. Our EMPATHIC-30 questionnaire covers the FCC values, and the outcomes of our PREM can play a critical role in informing and transforming FCC practices in Chinese NICUs and beyond.
Further research is suggested to develop and test an online EMPATHIC-30 Chinese questionnaire that allows for ease of use for parents and ease of collecting parent satisfaction data on a national level (40). Such a system can support the implications for clinical practice to benchmark parent satisfaction data and learn from the data to improve clinical practice based on the experiences of parents.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethical Committee of Hunan Children's Hospital. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
YZ, RZ, X-rG, L-hZ, and JL contributed to design of the study. YZ and RZ contributed to the data collection. JL, YZ, and RZ contributed to the data analysis. YZ and JL drafted the first manuscript, and RZ, X-rG, and L-hZ provided revisions. All the authors contributed to the manuscript, read, and approved the submitted version.
Funding
The study was partially supported by the Health and Family Planning Commission of Hunan Province (B2016031).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We thank all the parents who contributed to this study and support of the NICU staff.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2022.851291/full#supplementary-material
References
1. Nickel WK, Weinberger SE, Guze PA, Patient partnership in healthcare committee of the American College of Physicians, Carney J, Ende J. Principles for patient and family partnership in care: an American college of physicians position paper. Ann Intern Med. (2018) 169:796–9. doi: 10.7326/M18-0018
2. Weldring T, Smith SMS. Patient-reported outcomes (PROs) and patient-reported outcome measures (PROMs). Health Serv Insights. (2013) 6:61–8. doi: 10.4137/HSI.S11093
3. Hendriks AA, Oort FJ, Vrielink MR, Smets EM. Reliability and validity of the satisfaction with hospital care questionnaire. Int J Qual Health Care. (2002) 14:471–82. doi: 10.1093/intqhc/14.6.471
4. Bowling A, Rowe G, Lambert N, Waddington M, Mahtani KR, Kenten C, et al. The measurement of patients' expectations for health care: a review and psychometric testing of a measure of patients' expectations. Health Technol Assess. (2012) 16:1–509. doi: 10.3310/hta16300
5. Dudley SK, Carr JM. Vigilance: the experience of parents staying at the bedside of hospitalized children. J Pediatr Nurs. (2004) 19:267–75. doi: 10.1016/j.pedn.2004.05.008
6. Latour JM, Haines C. Families in the ICU: do we truly consider their needs, experiences and satisfaction? Nurs Crit Care. (2007) 12:173–4. doi: 10.1111/j.1478-5153.2007.00234.x
7. Piredda M, Vellone E, Piras G, Fida R, Latour JM, Matarese M, et al. Psychometric evaluation of the newcastle satisfaction with nursing scales. J Nurs Care Qual. (2015) 30:84–92. doi: 10.1097/NCQ.0000000000000078
8. Bragadóttir H, Reed D. Psychometric instrument evaluation: the pediatric family satisfaction questionnaire. Pediatr Nurs. (2002) 28:475–82.
9. Ygge BM, Arnetz JE. Quality of paediatric care: application and validation of an instrument for measuring parent satisfaction with hospital care. Int J Qual Health Care. (2001) 13:33–43. doi: 10.1093/intqhc/13.1.33
10. Committee on Hospital Care, American Academy of Pediatrics. Family-centered care and the pediatrician's role. Pediatrics. (2003) 112:691–7. doi: 10.1542/peds.112.3.691
11. Axelin A, Feeley N, Cambell-Yeo M, Silnes Tandberg B, Szczapa T, Wielenga J, et al. Symptoms of depression in parents after discharge from NICU associated with family-centred care. J Adv Nurs. (2021). doi: 10.1111/jan.15128. [Epub ahead of print].
12. Ding X, Zhu LH, Zhang R, Wang L, Wang TT, Latour JM. Effects of family-centered care interventions on preterm infants and parents in neonatal intensive care units: a systematic review and meta-analysis of randomized controlled trials. Australian Critical Care. (2019) 32:63–75. doi: 10.1016/j.aucc.2018.10.007
13. Baldoni F, Ancora G, Latour JM. Being the father of a preterm-born child: Contemporary research and recommendations for NICU staff. Front Pediatr. (2021) 9:724992. doi: 10.3389/fped.2021.724992
14. Hagen IH, Svindseth MF, Nesset E, Orner R, Iversen VC. Validation of the neonatal satisfaction survey (NSS-8) in six Norwegian neonatal intensive care units: a quantitative cross-sectional study. BMC Health Serv Res. (2018) 18:222. doi: 10.1186/s12913-018-3031-z
15. van den Hoogen A, Eijsermans R, Ockhuijsen HDL, Jenken F, Oude Maatman SM, Jongmans MJ, et al. Parents' experiences of VOICE: a novel support programme in the NICU. Nurs Crit Care. (2021) 26:201–8. doi: 10.1111/nicc.12569
16. Latour JM, van Goudoever JB, Hazelzet JA. Parent satisfaction in the pediatric ICU. Pediatr Clin North Am. (2008) 55:779–90, xii–xiii. doi: 10.1016/j.pcl.2008.02.013
17. Latour JM, Duivenvoorden HJ, Hazelzet JA, van Goudoever JB. Development and validation of a neonatal intensive care parent satisfaction instrument. Pediatr Crit Care Med. (2012) 13:554–9. doi: 10.1097/PCC.0b013e318238b80a
18. Dall'Oglio I, Fiori M, Tiozzo E, Mascolo R, Portanova A, Gawronski O, et al. Neonatal intensive care parent satisfaction: a multicenter study translating and validating the Italian EMPATHIC-N questionnaire. Ital J Pediatr. (2018) 44:5. doi: 10.1186/s13052-017-0439-8
19. Papamichael E, Loannou M, Talias MA. EMPATHIC-N in a Greek-Cypriot sample: confirming its factorial structure. BMC Health Serv Res. (2018) 18:968. doi: 10.1186/s12913-018-3793-3
20. Latour JM, Duivenvoorden HJ, Tibboel D, Hazelzet JA, EMPATHIC Study Group. The shortened EMpowerment of PArents in THe Intensive Care 30 questionnaire adequately measured parent satisfaction in pediatric intensive care units. J Clin Epidemiol. (2013) 66:1045–50. doi: 10.1016/j.jclinepi.2013.02.010
21. Gill FJ, Wilson S, Aydon L, Leslie GD, Latour JM. Empowering Parents of Australian Infants and Children in Hospital: Translation, Cultural Adaptation, and Validation of the EMpowerment of PArents in The Intensive Care-30-AUS Questionnaire. Pediatr Crit Care Med. (2017) 18:e506–13. doi: 10.1097/PCC.0000000000001309
22. Yu ZW, Zhang Y, Latour JM, Sun B, Lu GP, Gu Y, et al. The reliability and validity of the Chinese version satisfaction in the pediatric intensive care unit. Chin J Nur. (2015) 50:1261–5. doi: 10.3761/j.issn.0254-1769.2015.10.023
23. Latour JM, van Goudoever JB, Duivenvoorden HJ, Albers MJ, van Dam NA, Dullaart E, et al. Construction and psychometric testing of the EMPATHIC questionnaire measuring parent satisfaction in the pediatric intensive care unit. Intensive Care Med. (2011) 37:310–8. doi: 10.1007/s00134-010-2042-y
24. Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. (1951) 16:297–334. doi: 10.1007/BF02310555
25. Taber KS. The use of Cronbach's alpha when developing and reporting research instruments in science education. Res Sci Educ. (2018) 48:1273–96. doi: 10.1007/s11165-016-9602-2
26. Tiryaki Ö, Zengin H, Çinar N, Umaroglu M, Latour JM. Turkish adaptation and validation of the EMpowerment of PArents in THe Intensive Care (EMPATHIC-30) questionnaire to measure parent satisfaction in Neonatal Intensive Care Units. FrontPediatr. (2020) 8:421. doi: 10.3389/fped.2020.00421
27. Pilar Orive FJ, Basabe Lozano J, López Zuñiga A, López Fernández YM, Escudero Argaluza J, Latour JM. Traducción y validación al español del cuestionario EMPATHIC-30 para medir la satisfacción de los padres en cuidados intensivos [Spanish translation and validation of the EMPATHIC-30 questionnaire to measure parental satisfaction in intensive care units]. An Pediatr. (2018) 89:50–7. doi: 10.1016/j.anpedi.2017.08.004
28. Terp K. Weis J, Lundqvist P. Parents' views of family-centered care at a pediatric intensive care unit-a qualitative study. Front Pediatr. (2021) 9:725040. doi: 10.3389/fped.2021.725040
29. Lake ET, Smith JG, Staiger DO, Schoenauer KM, Rogowski JA. Measuring parent satisfaction with care in neonatal intensive care units: the EMPATHIC-NICU-USA questionnaire. Front Pediatr. (2020) 8:541573. doi: 10.3389/fped.2020.541573
30. He S, Xiong Y, Zhu L, Lv B, Gao X, Xiong H, et al. Impact of family integrated care on infant's clinical outcomes in two children's hospitals in China: A pre-post intervention study. Ital J Pediatr. (2018) 44:65. doi: 10.1186/s13052-018-0506-9
31. Zhang R, Huang RW, Gao XR, Peng XM, Zhu LH, Rangasamy R, et al. Involvement of parents in the care of preterm infants: a pilot study evaluating a family-centered care intervention in a Chinese neonatal ICU. Pediatr Crit Care Med. (2018) 19:741–7. doi: 10.1097/PCC.0000000000001586
32. Zhu LH, Lv B, Gao XR, Sun J, Li TT, Liu ZY, et al. Family-centered care improves clinical outcomes of very-low-birth-weight infants: a quasi-experimental study. Front Pediatr. (2019) 7:138. doi: 10.3389/fped.2019.00138
33. Mol C, Argent AC, Morrow BM. Parental satisfaction with the quality of care in a South African paediatric intensive care unit. S Afr J Crit Care. (2018) 34:50–6. doi: 10.7196/SAJCC.2018.v34i2.366
34. Rodriguez-Ruiz E, Campelo-Izquierdo M, Estany-Gestal A, Rodríguez-Núñez A, Latour JM. Impact of different visiting policies on family satisfaction in two Spanish ICUs before and during COVID-19. Intensive Care Med. (2021) 47:1165–6. doi: 10.1007/s00134-021-06485-0
35. Ryan L, Plötz FB, van den Hoogen A, Latour JM, Degtyareva M, Keuning M, et al. Neonates and COVID-19: state of the art. Pediatr Res. (2022) 91:432–9. doi: 10.1038/s41390-021-01875-y
36. Meesters N, van Dijk M, Sampaio de Carvalho F, Haverman L, Reiss IKM, Simons SHP, van den Bosch GE. COVID-19 lockdown impacts the wellbeing of parents with infants on a Dutch neonatal intensive care unit. J Pediatr Nurs. (2022) 62:106–12. doi: 10.1016/j.pedn.2021.09.024
37. Yi YZ, Su T, Jia YZ, Xue Y, Chen YZ, Zhang QS, et al. Family-centered care management strategies for term and near-term neonates with brief hospitalization in a level III NICU in Shenzhen, China during the time of COVID-19 pandemic. J Matern Fetal Neonatal Med. (2021) 1–4. doi: 10.1080/14767058.2021.1902499
38. Kingsley C, Patel S. Patient-reported outcome measures and patient-reported experience measures. BJA Educ. (2017) 17:137–44. doi: 10.1093/bjaed/mkw060
39. Bele S, Teela L, Zhang M, Rabi S, Ahmed S, van Oers HA, et al. Use of patient-reported experience measures in pediatric care: a systematic review. Front Pediatr. (2021) 9:753536. doi: 10.3389/fped.2021.753536
Keywords: neonatology, parents, infants, patient satisfaction, Neonatal Intensive Care Unit, EMPATHIC-30, reliability, validity
Citation: Zhuang Y, Zhang R, Gao X-r, Zhu L-h and Latour JM (2022) Validation of the Chinese Empowerment of Parents in the Intensive Care (EMPATHIC-30) Questionnaire Among Parents in Neonatal Intensive Care Units: A Prospective Cross-Sectional Study. Front. Pediatr. 10:851291. doi: 10.3389/fped.2022.851291
Received: 09 January 2022; Accepted: 02 March 2022;
Published: 30 March 2022.
Edited by:
Luregn J. Schlapbach, University Children's Hospital Zurich, SwitzerlandReviewed by:
Daniela De Souza, University of São Paulo, BrazilDebbie Long, Queensland University of Technology, Australia
Copyright © 2022 Zhuang, Zhang, Gao, Zhu and Latour. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Li-hui Zhu, ODc3ODQ1Mzc1QHFxLmNvbQ==; Xi-rong Gao, Z2FveGlyb25nQDEyNi5jb20=
 Yan Zhuang
Yan Zhuang Rong Zhang1
Rong Zhang1 Li-hui Zhu
Li-hui Zhu Jos M. Latour
Jos M. Latour