- 1Professional Development, Continuing Education and Research Service, Bambino Gesù Children’s Hospital, IRCCS, Rome, Italy
- 2Department of Paediatric Emergency, Bambino Gesù Children’s Hospital, IRCCS, Rome, Italy
- 3Pediatric Semi-Intensive Care Area/Unit, Bambino Gesù Children’s Hospital, IRCCS, Rome, Italy
- 4Rheumatology Unit, Bambino Gesù Children’s Hospital, IRCCS, Rome, Italy
- 5Department of Biomedicine and Prevention, University of Rome “Tor Vergata,” Rome, Italy
Children and young adults (CYAs) with chronic conditions need to engage in self-care to improve their quality of life. This study aimed to retrieve the literature on instruments to assess self-care in CYAs living with chronic conditions and evaluate the psychometric proprieties of the instruments retrieved. A systematic literature review was conducted on six databases to identify peer-reviewed papers that described or used an evaluation instrument of self-care in CYAs with chronic conditions. Twenty-three articles describing 11 instruments of self-care were identified. Five instruments (45.45%) were developed for specific diseases, while six (54.54%) for various chronic illnesses. Most of the instruments were focused on treatment adherence within self-care maintenance (i.e., behaviors to maintain illness stability), excluding the monitoring of clinical parameters or the management of exacerbations. This review provides an overview of available instruments that measure self-care in CYAs with chronic conditions, which health professionals could use for patient education.
Introduction
Chronic diseases are defined broadly as conditions that last for a year or longer and require ongoing medical attention or limit activities of daily living or both (1). The prevalence of pediatric-onset chronic diseases is gradually increasing around the world (2), contributing to both morbidity and mortality (3). The number of children and young adults (CYAs), children aged 0–24 years (4, 5), living with a chronic condition is growing due to higher survival rates (6). In the United States, 25% of the pediatric population is affected by a chronic condition and 5% by multiple chronic conditions (7). In Europe, in 2016, 16% of the population aged between 16 and 29 had a long-standing health problem (8). In Italy, 91.8% of children aged 0–14 are in good health, 9.6% have one or more chronic conditions, 1.6% suffer from two or more chronic illnesses (9). In addition, children with complex conditions have to deal with multiple transitions across providers and care settings (10), and those requiring technology support and home care bear even higher costs (11–13). Furthermore, long-term chronic conditions have a strong impact on wellbeing and require ongoing management over a period of years or decades (14).
In the pediatric population, the most common pediatric chronic conditions, including those with medical complexity (15), are asthma, cystic fibrosis, type 1 diabetes mellitus, and chronic lung disease (16). In particular, children with the highest levels of medical complexity are estimated to be about 0.4–0.7% of all US children (17). Therefore, it is important to promote the quality of life of CYAs with chronic conditions and their family members. This requires a life-long process of self-care or self-management to preserve and improve personal wellbeing, to maintain a good health-related quality of life, and to reduce health costs (18, 19).
The concepts of self-care and self-management have been used with considerable overlap and interchangeably among scholars (20). Self-management refers to the process that individuals with a health problem intentionally use to gain control of their disease, in partnership with health professionals (21). Self-care is a more encompassing concept, referring to patients’ ability and performance of activities to achieve, maintain, and promote optimal health and wellbeing, including monitoring and managing acute and chronic health conditions (22, 23). WHO defines self-care as “the ability of individuals, families and communities to promote health, prevent disease, maintain health, and to cope with illness and disability with or without the support of a healthcare provider” (24). According to Riegel and Dickson (25), self-care is a naturalist decision-making process based on patient experience (25).
In particular, the Middle-Range Theory of Self-Care of Chronic Illness identifies behaviors of self-care maintenance, characterized by those actions performed to maintain chronic condition stable (e.g., taking medications as prescribed); self-care monitoring, concerning all those behaviors performed to keep signs and symptoms under control (e.g., monitoring weight); and self-care management, concerning the reaction to symptoms when they occur (e.g., call the healthcare provider in case of fever) (26, 27). However, this Middle-Range Theory was developed for adults. In the pediatrics, especially for CYAs, few theoretical models have been described, such as the new comprehensive model of self-care in CYAs (28). This model emphasized that self-care is a very broad concept since it not only includes personal skills but also healthcare actions provided by others. Others include informal caregivers (parents, relatives, friends, volunteers) who play a crucial role in chronic patient care, but also formal caregivers (healthcare professionals) who provide specific professional support to families in terms of care management (28). Healthcare professionals cooperate with the patient and/or the family who maintain, if possible, the responsibility for their own care (29).
Self-care and quality of life, distress, and depression are interrelated (18). On the one hand, better self-care is associated with positive outcomes, such as more adequate disease control, greater patient safety, higher quality of life, and better personal development, which may lead to lower depression and distress (28, 30). On the other hand, psychological aspects can also be considered as influencing factors; for example, if CYAs are depressed, then they are more likely to neglect self-care behaviors (31, 32). Moreover, healthcare systems admit that self-care has a positive impact on reducing chronic diseases and on reducing health costs (33). Indeed, in general, chronic diseases requires a great amount of human and economic resources (34). Managing chronic diseases requires specialized professional competences and health facilities suited to the health care pathways. Therefore, the chronic diseases during childhood have a strong social impact (35).
In addition, the health consequences are related to the child’s age at the onset of chronic alteration (36). Children with chronic diseases occurring during childhood showed a different outcome compared to those in which the diseases onset during their adolescence. Indeed, many aspects of adolescent daily life require a life-long process of self-care such as the need for precisely scheduled daily medications, consumption of special dietary products, regular physical exercise, regular visits to healthcare providers and monitoring of blood glucose levels (37).
Furthermore, adolescents with a chronic disease may deal with the burden of independence incapability and the need to ask for support from parents and other caregivers for most of their daily activities (37). Parents should encourage adolescents to develop self-esteem and avoid an excessively protective attitude (38). Adolescence is a key development period for establishing lifelong health-related behaviors (39). Furthermore, patients with complex chronic diseases, along with developmental changes in adolescence, face challenges related to their health-related quality of life (40).
There is evidence that self-care actions have a positive impact on the health of CYAs with complex chronic diseases, such as diabetes and fibrosis cystic (28, 41). Therefore, it is essential that these patients perform self-care (38, 42). The higher educational level of the population has generated a higher demand for specific information and education regarding healthcare topics (43). This demand has caused an increase of CYAs’ care competency for their own health and wellbeing (43). Assessing self-care in the pediatric population with chronic diseases may contribute to improve self-care activities and address any deficiencies.
Therefore, the aims of this study were: (a) to retrieve and describe the literature on instruments (scales or questionnaires) that assess self-care in CYAs living with chronic conditions; and (b) to evaluate the psychometric proprieties of the retrieved instruments that assess self-care in CYAs with chronic conditions.
Methods
Search Strategy
A systematic review was conducted to explore studies that described self-care scales for pediatric patients with chronic diseases. Search procedures followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines for writing systematic reviews (44). The review was conducted through six databases: PubMed, Scopus, CINAHL, Embase, PsycInfo, and the Cochrane Library. In addition, a manual search was carried out to broaden the search. The study selection was conducted in July 2021. The main keywords were “self-care,” “self-management,” “Scale,” “Questionnaire,” “Chronic Disease,” “Pediatric,” “Adolescent,” “Young Adult,” “Parents.” Boolean operators—NOT, AND, OR—were also used to narrow and widen the search. The search was conducted by two reviewers independently. The search strategy is described in Supplementary Material.
Eligibility Criteria
The review included all types of peer-reviewed papers with no limits of time or language. Eligible studies for inclusion had to meet the following criteria: (a) any study published on a peer-reviewed journal; (b) patients with chronic diseases or complex chronic diseases; (c) patients aged between 0 and 24 years; (d) studies that described or used a self-care evaluation scale; (e) studies describing self-care in children or young adults and/or the parental role; (f) studies in any language describing self-care evaluation instruments.
The exclusion criteria were: (a) papers that did not include instruments that evaluated self-care; (b) self-care scales not developed for the population included in this review; (c) unavailable full-texts; (d) scales that did not describe self-care activities; (e) papers published in journal that were not peer-reviewed; (f) scales did not include at least one of the self-care dimensions (self-care maintenance, self-care monitoring, self-care management); (g) studies that evaluated only self-efficacy.
Study Selection
Firstly, duplicate records were identified and removed. Secondly, titles and abstracts were screened by two independent authors. The full texts of potential eligible studies were read to determine if the papers were eligible. In case of disagreement between the two authors, a third author was involved to make the final decision.
Data Extraction and Synthesis
The following data were extracted: authors and year of publication; country where the study was conducted; aim; study design; population (patient and/or parents age); type of chronic diseases and if mental diseases were included; scales or questionnaires; administration method; timing of administration; whether the instrument was validated; and findings. To describe and synthesize information on every instrument included in this review, the included papers were examined by focusing on the following information: name of the scale; description of the scale or part of it; original author and year; authors who included the scale in their paper; whether the scale was original or adapted; language; whether the entire scale or only one of its dimensions were used; patients’ age; chronic diseases; self-care maintenance, self-care monitoring, self-care management; the population that responded to questionnaire (patients, parents, or both), the way the scale and/or questionnaire was administered, and the conceptual model (25). The psychometric characteristics of each included instrument were analyzed using the COSMIN criteria (45). In addition, two researchers independently investigated the dimension of self-care reported in each scale (self-care maintenance, self-care monitoring, and self-care management) according to the Middle-Range Theory of Self-Care of Chronic Illness (26).
Results
The study selection process is shown in Figure 1. The initial search identified 3,326 records across the six databases and six articles after a manual search. After removing the duplicates, 2,545 articles were reviewed by reading the title and abstract and 2,468 were excluded because they did not meet the inclusion criteria. The full texts of the remaining 77 articles were read and, of these, 23 papers were included in the final review and analysis. The reasons for the exclusion of 54 papers are reported in Figure 1.
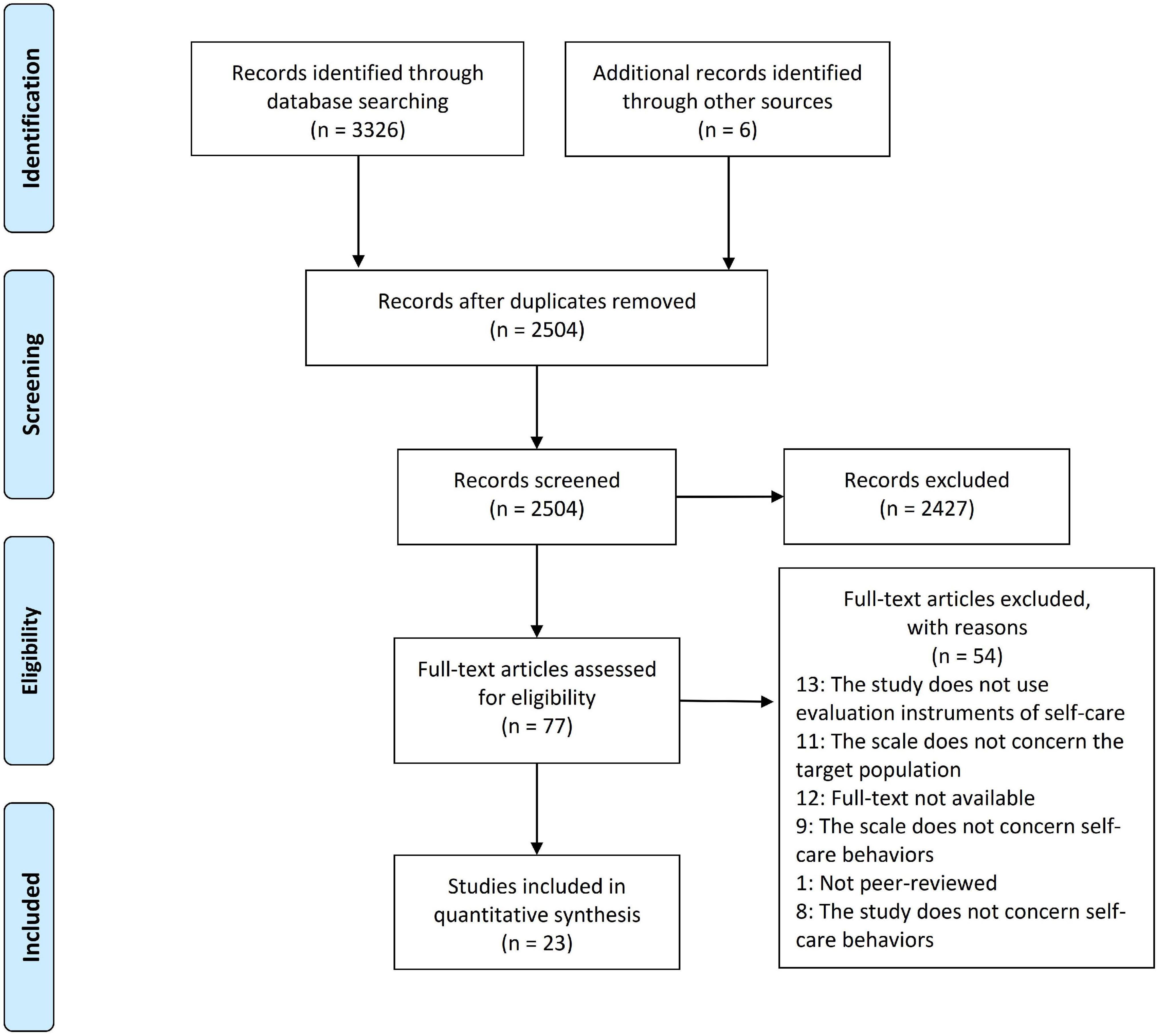
Figure 1. The Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) flow diagram showing the study selection process.
Characteristics of the Included Studies
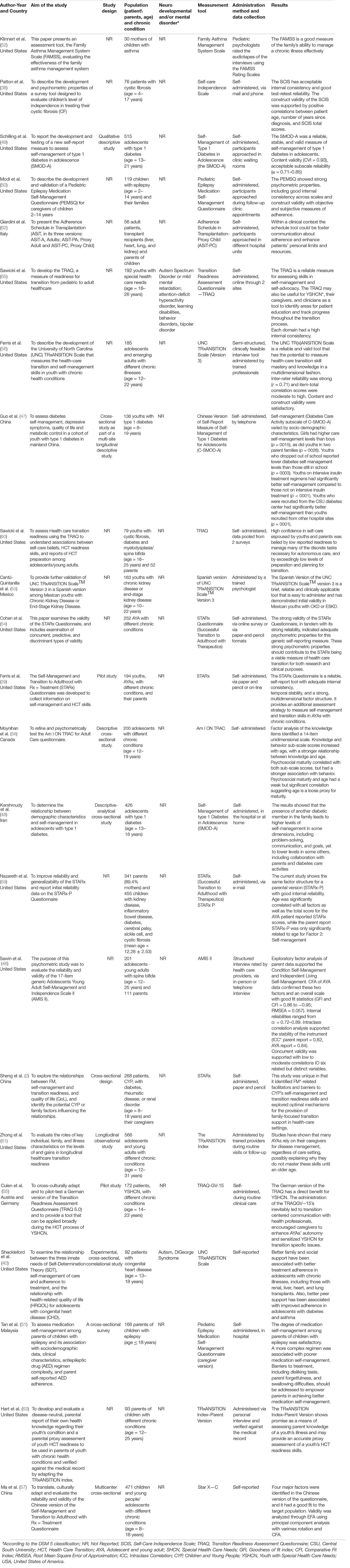
Most of the 23 studies included in this review were published in the last decade (n = 20; 86.95%) and mainly conducted in North America (n = 15; 65.21%), followed by Asia (n = 5; 21.73%), Europe (n = 2; 8.69%), and Mexico (n = 1; 4.34%) (Table 1). Seven studies (30.43%) used a cross-sectional approach, two (8.69%) were pilots, one (4.34%) was a longitudinal observational study, one (4.34%) used a qualitative design, and 12 (52.17%) did not report their study design. The age of the study samples ranged from two to 28 years, including children, adolescents and/or young adults. The samples of six of the 23 included studies (26.08%) included both children and their parents, whereas one study (4.34%) only the parents.
Nine studies (39.13%) developed or used self-care instruments only for one type of chronic condition: spina bifida (n = 1; 4.76%) (46), type 1 diabetes (n = 3; 14.28%) (47–49), epilepsy (n = 2; 9.52%) (50, 51), asthma (n = 1; 4.76%) (52), cystic fibrosis (n = 1; 4.76%) (38), and congenital heart disease (n = 1; 4.76%) (40). Ten studies focused on multiple chronic conditions such as kidney disease, systemic lupus erythematosus, inflammatory bowel disease, hypertension, renal transplant, and systemic lupus erythematosus (2, 29, 53–61). Four studies did not specify the chronic condition of their sample (57, 62–64).
A total of 13 studies (56.52%) considered neurodevelopmental and/or mental disorders (according to the DSM 5 classification) as an exclusion criterion; two studies (8.69%) included also patients with neurodevelopmental and/or mental disorders, eight studies (34.78%) did not specify whether these disorders were considered exclusion criteria.
Twenty-two of the studies included in this review reported the administration method of the instruments. The authors of four studies (18.2%) specified that the questions were asked by an assistant researcher. With regard to data collection, seven studies (69.56%) used paper-and-pencil instruments administered in hospital settings, nine studies (39.13%) used online or telephone or mail interviews, while seven studies (69.56%) did not specify this. Most of the selected papers included information about the validity and reliability of the instruments (n = 20; 86.9%), while in three papers this information was not provided because they were based on previous validation studies.
Characteristics of the Self-Care Instruments
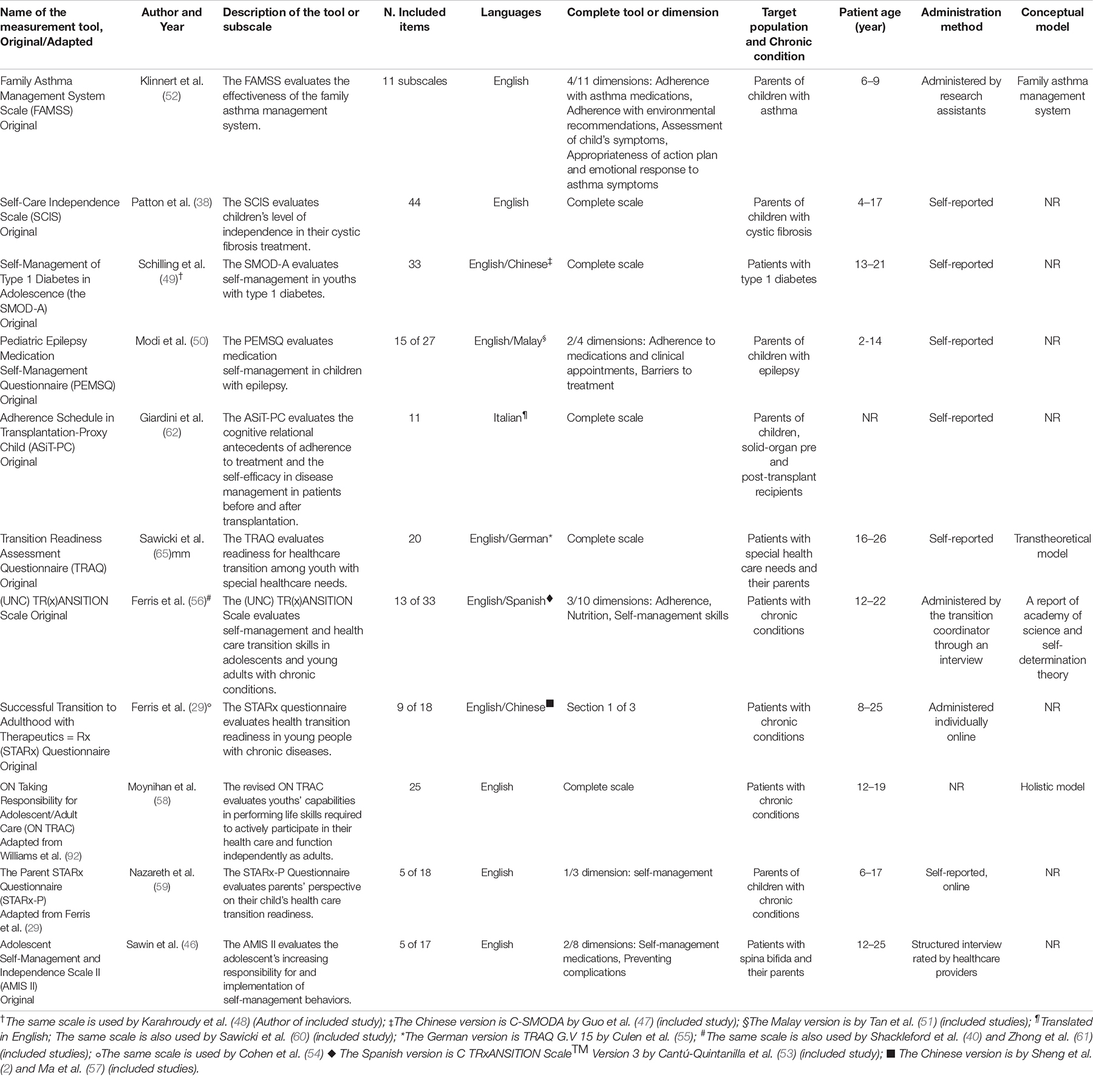
Overall, 11 self-care instruments focusing on pediatric patients with chronic conditions were described in the studies included in this review (Table 2). Seven instruments were adapted, translated or modified from previous instruments developed by other authors (2, 40, 47, 51, 53, 55, 61). Five (45.45%) of the 11 instruments were specifically used to assess self-care of pediatric patients during the transition process from pediatric to adult care (29, 55, 59–61, 65). Five (45.45%) instruments were published in English (38, 46, 52, 58, 59); one instrument was available in English and Spanish (9.09%) (56); one was published both in English and German (9.09%) (65); two were available in English and Chinese (18.18%) (29, 49); one instrument was both in English and Italian (9.09%) (62), and one is available in English and Malaysian (9.09%) (50). Five (45.45%) instruments were entirely in line with the purposes of this review (38, 49, 58, 62, 65). Indeed, every dimension of the instruments included the concept of self-care and thus were analyzed in every part. The remaining instruments (n = 6; 54.54%) were analyzed only for those dimensions that were relevant to the aim of this review.
The self-care instruments were developed for patients (n = 4; 36.36%) (49, 56, 58, 65), for parents (n = 5; 45.45%) (38, 50, 52, 59, 62), or both (n = 2; 18.18%) (46, 65). The target population of the instruments were adolescents/young adults (n = 4; 36.36%) (29, 46, 49, 56, 58, 65), children/adolescents (n = 4; 36.36%) (29, 50, 58, 59), children (n = 1; 9.09%) (52). One instrument (9.09%) (62) did not describe the target population. Five instruments (45.45%) were developed for specific conditions. In particular, these instruments were: the Self-Care Independence Scale (SCIS) for cystic fibrosis (38), FAMSS (38, 46, 49, 50, 52) the Pediatric Epilepsy Medication Self-Management Questionnaire (PEMSQ) (50), Self-Management of Type 1 Diabetes in Adolescence (SMOD-A) (49), the Adolescent Self-Management and Independence Scale II (AMIS II) (46). The remainder (n = 6.54; 54%) were developed for non-specific chronic conditions (29, 56, 58, 59, 62, 65). Five of the 11 instruments were self-administered (45.45%) (38, 49, 50, 62, 65), three instruments were administered by others, such as the research assistant (27.27%) (29, 46, 52, 56, 59) and one (9.09%) did not specify this (58).
Four of the 11 instruments (36.36%) described the conceptual models of reference, the other seven instruments (63.63%) did not refer to any conceptual model. In particular, the UNC TRxANSITION scale used the self-determination theory as reference model (56), the TRAQ scale used the Transtheoretical model (65), the Family Asthma Management System Scale (FAMMS) was developed according to the Family asthma management system model (52), and the ON Taking Responsibility for Adolescent/Adult Care (ON TRAC) used the Holistic model (58). Psychometric characteristics of the tools (Validity and Reliability).
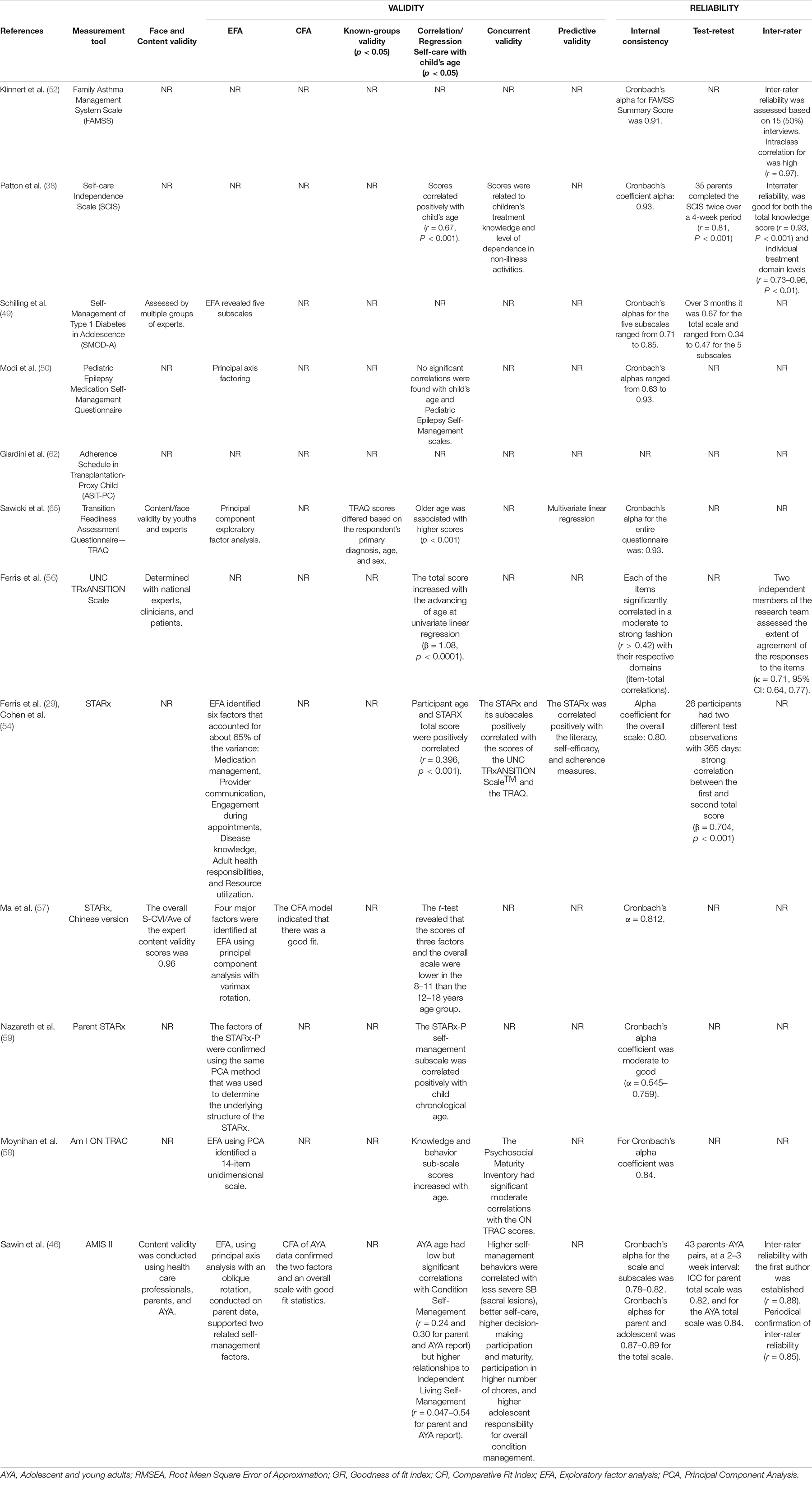
The 13 studies reported in Table 3 explored the psychometric characteristics—validity and reliability—of the 11 measurement tools included in this review. Content validity was tested for five instruments (46, 49, 56, 57, 65), following the COSMIN taxonomy (45). Construct validity was verified through Exploratory Factor Analysis (EFA) for six instruments (29, 49, 50, 57–59, 65), and through Confirmatory Factor Analysis (CFA) for two instruments (46, 57). Only for the Star-x instrument the construct validity was verified both through EFA and CFA (57). With regard to criterion validity, concurrent validity was used to analyze four instruments (38, 46, 54, 58), and among these instruments, predictive validity was verified only for StarX and TRAQ (54, 65). The Known-groups validity was tested for the TRAQ instrument (65). Furthermore, the correlation/regression between self-care and child age was explored in seven instruments (29, 38, 50, 54, 56–59, 65).
Regarding reliability, internal consistency was verified in 11 instruments (29, 38, 46, 49, 50, 52, 56–59, 65). Test-retest reliability was tested in four instruments (29, 38, 46, 49), and inter-rater reliability was also verified for the SCIS e the AMIS II scale (38, 46). With regard to the FAMSS and the UNC TRxANSITION Scale, inter-rater reliability was verified in addition to internal consistency (52, 56). Lastly, responsiveness and non-differential validity were not reported for any instruments.
Self-Care Aspects of Each Instrument
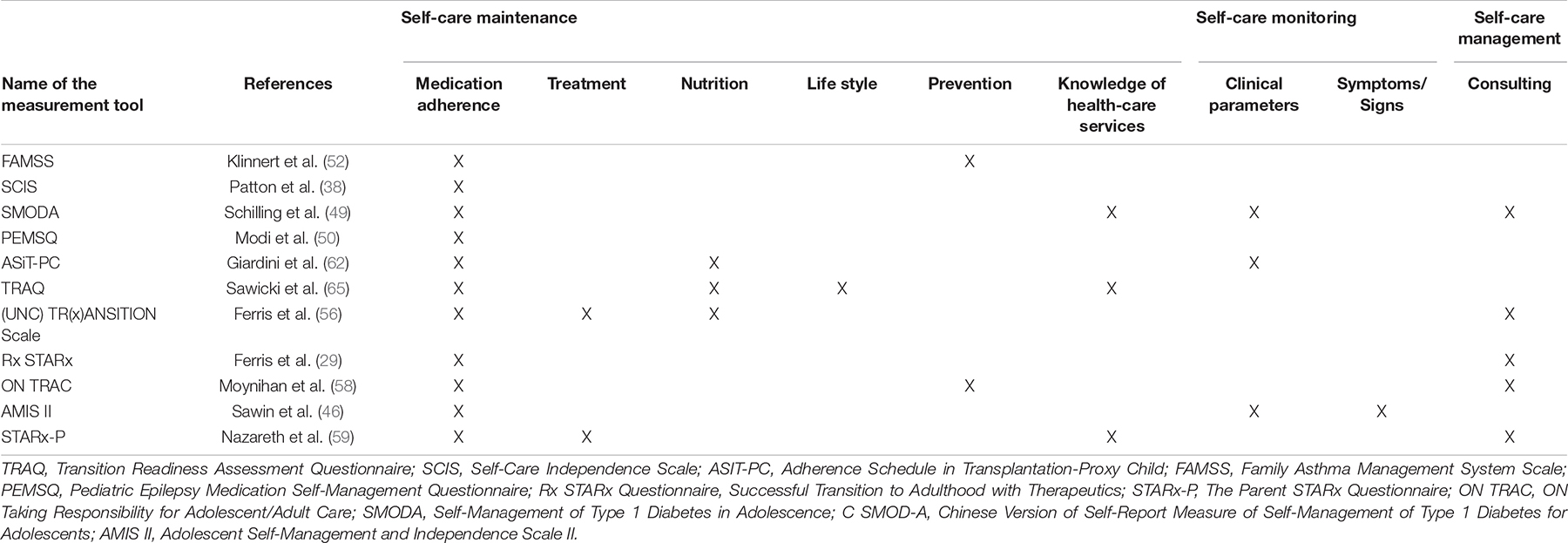
In this review, the self-care aspects/areas reported in the 11 instruments were described according to Riegel’s self-care theory focusing on the aspects of each of the three self-care domains (self-care maintenance, self-care monitoring, self-care management) by Riegel (Table 4). As regards to self-care maintenance, all the 11 instruments included the aspect/area of medication adherence and only the (UNC) TR(x)ANSITION Scale and The Parent STARx Questionnaire (STARx-P) included the aspect of treatment adherence (56, 59). Feeding was explored in three instruments: the UNC Tr(x)ansition scale, Transition Readiness Assessment Questionnaire (TRAQ) and Adherence Schedule in Transplantation-Proxy Child (ASiT-PC) (56, 62, 65). The aspect of lifestyle was examined only in the TRAQ (65), whereas the prevention aspect was included in two instruments: FAMSS and ON TRAC (52, 58). The knowledge of health-care services was explored in two instruments, the Parent STARx Questionnaire (STARx-P) and TRAQ (59, 65).
With regard to self-care monitoring, the area of vital signs monitoring was explored only in the Adherence Schedule in Transplantation-Proxy Child (ASiT-PC) and in the Adolescent Self-Management and Independence Scale II (AMIS II) (46, 62). The signs and symptoms aspect was treated in the Self-Management and Independence Scale II (AMIS II) (46).
For the self-care management domain, only one aspect (i.e., consulting) was described in four instruments: Successful Transition to Adulthood with Therapeutics = Rx (STARx) Questionnaire, (UNC) TR(x)ANSITION Scale, ON TRAC and The Parent STARx Questionnaire (STARx-P) (29, 56, 58, 59).
Discussion
In this literature review, 11 self-care instruments addressing CYAs with chronic diseases were identified. These instruments differ for pathologic contexts and age range. The instruments providing more valid psychometric measurements were AMIS II and STARx. These are also the instruments published more recently (46, 57).
Although all the identified instruments included at least one of Riegel’s self-care domains, only one instrument, the SMODA, investigated all of the three self-care domains: self-care maintenance, self-care monitoring, self-care management (49). Every instrument included in this review explored self-care maintenance, focusing particularly on medication and treatment adherence. The importance attributed to autonomy in medication administration might be associated to the advantage of reducing use of healthcare services (66). However, few instruments focused on monitoring vital signs and symptom management. Concerning self-care monitoring, only one instrument investigated signs and symptoms monitoring, an important aspect to detect important health status changes. As regards the self-care management area, the instruments explored mostly the consulting aspect, leaving very little space for the management of complications or acute exacerbations through spontaneous self-care strategies. Overall, the medical management of a chronic condition is not new, probably along with paternalistic and directive guidance in the relationship between healthcare providers and families (67), often associated with the passive decision-making of families allowing the provider to choose the course of action (68, 69). This aspect might reflect the persisting belief in the monopoly on health of the healthcare providers (70), and a great trust assigned to healthcare professionals of reference, such as the nurse case managers (71).
Studies showed that also self-care monitoring and self-care management is important. For example, Riegel et al. (27) describe how symptom monitoring affects self-care behaviors, underling the importance of symptom detection, interpretation and response as fundamental elements of the self-care process (27). Sawin et al. (46) found that when CYAs monitored their signs and symptoms they achieved independence much earlier than others (46). Also Nazareth et al. (59) found that when CYAs responded promptly to signs and symptoms of exacerbation they became more knowledgeable about their disease management (59).
Specific instruments were developed for the most common chronic diseases. In particular, the SMOD-A scale was developed for diabetes, SCIS for cystic fibrosis, FAMSS for asthma, PEMSQ for epilepsy, and AMIS II for spina bifida (38, 46, 49, 50, 52). The decision to have an instrument for a specific disease might be due to the large prevalence of these diseases, mostly diabetes and asthma, in the CYA population (72, 73). However, even though having instruments for assessing self-care in CYAs with specific chronic diseases is fundamental, there are also many other chronic and sometimes rare conditions to take into consideration. Therefore, the development of a non-specific instrument for the CYA population with different chronic conditions, considering the main age stages, might represent a useful innovation.
Furthermore, in this review, two instruments were found to be more generic [i.e., (UNC) TR(x)ANSITION Scale and TRAQ)] designed for chronic diseases in general or young adults with special healthcare needs (56, 65). However, these two instruments were focused on the skills required during the healthcare transition from pediatric to adult care services. Transition readiness reflects all the indicators (e.g., disease-specific knowledge, scheduling appointments) that young adults can begin, continue, and finish the transition process, including those skills influencing self-care (74–77). Therefore, self-care might be considered an integral part of transition readiness in the context of a challenging transfer to the adult health care system. To our knowledge, no instrument is currently available to assess self-care behaviors among CYAs of all ages aimed at exploring the shift of agency from family to autonomous self-care, regardless of the patient care context.
Moreover, also complex chronic diseases need to be considered. According to Cohen et al. (15), these conditions in childhood are characterized by four domains: (a) family-identified healthcare service needs, (b) one or more chronic clinical conditions, either diagnosed or unknown, (c) severe functional limitations, and (d) highly projected utilization of health resources. CYAs with complex chronic conditions need standardized approaches, tools and more effective competence to manage the complexity of these diseases (78). Therefore, it would be useful to develop a specific self-care instrument for CYAs with complex chronic conditions.
Furthermore, the present review analyzed also the methods used to administer the instruments. Five instruments were self-reported since the respondents were in school-age or adolescents (38, 49, 50, 62, 65). Four instruments asked also the parents to fill in the questionnaire. This aspect might show how the family maintain a central and vital role in supporting both the children—during the pre and scholar age—and adolescents/young adults (79, 80).
Another aspect analyzed in the current review was the conceptual model underpinning each instrument. The conceptual models were specified in four instruments, such as the self-determination theory, the transtheoretical model, the holistic model, and family management of specific diseases such as asthma. Having instruments based on a theoretical framework, as the models reported above, is fundamental to obtain sounder and valid instruments (81). Recently, a self-care model has been developed for complex chronic conditions (28). This model includes the affecting factors, self-care behaviors and outcomes, highlighting that the more the patients are engaged in self-care behaviors, the more the results are positive.
Implications for Practice
The findings of this review may help researchers identify instruments to assess the level of self-care in CYAs living with chronic conditions for research purposes, as outcome measures for interventional studies, or as a basis for further validation studies. Moreover, we recommend the use of self-care instruments in clinical practice. Although clinicians recognize the importance of promoting self-care in CYAs with chronic conditions, they need standardized approaches and psychometrically sound tools (78). Measuring a patient’s level of self-care using an assessment instrument represents, for the clinician, the first step to identifying educational gaps and factors hindering the engagement process (82). Healthcare providers play an important role in fostering autonomy using educational strategies that take into consideration developmental stages and family support (83–85). Educational interventions have resulted in improvements in health outcomes, knowledge related to the chronic condition, quality of life, attendance at school, participation in social activities, and a decrease in health service interactions (86–88). In a second step, the patient could assume greater responsibility for managing their health alone or with the help of parents and healthcare professionals (89).
Limitations
The findings of this review should be considered in light of some limitations. Firstly, the current review explored the instruments that concerned self-care in CYAs in every context. However, these contexts were found to be very broad and the concept of self-care may overlap with other concepts such as healthcare transition from pediatric to adult clinical setting (56). Therefore, the instruments found could not be considered totally comparable.
Secondly, the search strategy of this review did not include gray literature. Therefore, unquantifiable instruments might have been missed. Thirdly, studies measuring self-care in CYAs with neurocognitive impairment and in those living with cancer were not included in this review. Although the authors of this review believe that these patients deserve specific considerations, important features of the self-care process may have been missed.
Another limitation was the voluntary exclusion of the studies that assessed self-efficacy. Indeed, the aim of this review was to identify the instruments that evaluate self-care behaviors (maintenance, monitoring, management) rather than assessing confidence in self-care (90). However, future quantitative studies could investigate the confidence aspect since the process of self−care implies that self−care confidence (in patients and caregivers) influences the entire process of self−care across the three dimensions of self−care maintenance, monitoring, and management (91).
Conclusion
This review analyzed 23 studies that described 11 self-care instruments for CYAs. Only one instrument assessed each aspect of self-care (maintenance, monitoring, and management) according to our definition. In particular, most of the instruments were focused on treatment adherence within self-care maintenance and ignored the aspects of prevention, feeding, and lifestyle. Less attention was given to vital signs and symptoms monitoring, and to responses to exacerbations of chronic conditions. Therefore, it would be useful to investigate how health professionals are focused on these self-care dimensions while providing education to patients and their families. Furthermore, future research may develop a comprehensive instrument measuring all the dimensions of self-care across all chronic conditions, also including those with medical complexity. Future instruments might be based on “The comprehensive model of self-care in CYA with chronic conditions” (28). This model could guide to a global evaluation of self-care in relation to developmental age, also considering the parent’s contribution and shift of agency.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author Contributions
GS, VB, and VK made substantial contributions to the conception and design of the systematic review, conducted the literature search, data extraction, and drafted the manuscript. RM gave a substantial contribution to the translation of the text, moreover, critically reviewed and revised the manuscript. AL and GM contributed to evaluated the psychometric proprieties of the tools retrieved, updating the reference list, critically reviewed, and revised the manuscript. OG, MS, EV, and ET helped in results analysis, drafting and critically revising the manuscript. ID’O conceived and supervised all the phases of the systematic review, drafted and critically revised the manuscript for important intellectual content. All authors approved the final version of the manuscript as submitted and agreed to be accountable for all the aspects of this study.
Funding
This study was co-funded by the Italian Ministry of Health and the Centre of Excellence for Nursing Scholarship-Nursing Professional Order of Rome.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We thank Alessandra Loreti, Manuela Moncada, and Claudia Sarti for support in consulting some databases and collecting some full texts of the articles. Anna Bellingrath for supporting in the literature search, Giulia Gasperini for initially contributing to the design of the research project. They all work at the Bambino Gesù Children’s Hospital, IRCCS. Moreover, we thank Gennaro Rocco, Scientific Director of the Centre of Excellence for Nursing Scholarship of Nursing Professional Order of Rome for co-funding this study.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2022.832453/full#supplementary-material
References
1. Centers for Disease, Control and Prevention. About Chronic Diseases | CDC. (2021). Available online at: https://www.cdc.gov/chronicdisease/about/index.htm (accessed February 19, 2021).
2. Sheng N, Ma J, Ding W, Zhang Y. Family management affecting transition readiness and quality of life of Chinese children and young people with chronic diseases. J Child Health Care. (2018) 22:470–85. doi: 10.1177/1367493517753712
3. Al-Hassany L, Kloosterboer SM, Dierckx B, Koch BCP. Assessing methods of measuring medication adherence in chronically ill children–a narrative review. Patient Prefer Adherence. (2019) 13:1175–89. doi: 10.2147/PPA.S200058
4. World Health Organization [WHO]. Adolescence: A Period Needing Special Attention: Recognizing-Adolescence. (2021). Available online at: https://apps.who.int/adolescent/second-decade/section2/page1/recognizingadolescence.html (accessed April 23, 2020).
5. Adolescent and young adult health. (2021). Available online at: https://www.who.int/news-room/fact-sheets/detail/adolescents-health-risks-and-solutions (accessed March 15, 2022).
6. Starmer AJ, Duby JC, Slaw KM, Edwards A, Leslie LK, Members of Vision of Pediatrics 2020 Task Force. Pediatrics in the year 2020 and beyond: preparing for plausible futures. Pediatrics. (2010) 126:971–81. doi: 10.1542/peds.2010-1903
7. Miller GF, Coffield E, Leroy Z, Wallin R. Prevalence and costs of five chronic conditions in children. J Sch Nurs. (2016) 32:357–64. doi: 10.1177/1059840516641190
8. Eurostat. Being Young in Europe Today - Health - Statistics Explained. (2021). Available online at: https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Being_young_in_Europe_today_-_health (accessed February 19, 2021).
9. Italian Ministry of Health. 4.2. Salute Infantile e Dell’adolescente - Relazione Sullo Stato Sanitario del Paese. (2011). Available online at: http://www.salute.gov.it/rssp/paginaParagrafoRssp.jsp?sezione=situazione&capitolo=salute&id=2684 (accessed March 31, 2021).
10. Aldiss S, Cass H, Ellis J, Gibson F. “We sometimes hold on to ours” - professionals’ views on factors that both delay and facilitate transition to adult care. Front Pediatr. (2016) 4:125. doi: 10.3389/fped.2016.00125
11. Cohen E, Berry JG, Camacho X, Anderson G, Wodchis W, Guttmann A. Patterns and costs of health care use of children with medical complexity. Pediatrics. (2012) 130:e1463–70. doi: 10.1542/peds.2012-0175
12. Dinleyici M, Dağlı FŞ. Evaluation of quality of life of healthy siblings of children with chronic disease. Turk Pediatri Ars. (2018) 53:205–13. doi: 10.5152/TurkPediatriArs.2018.6778
13. Khanna AK, Prabhakaran A, Patel P, Ganjiwale JD, Nimbalkar SM. Social, psychological and financial burden on caregivers of children with chronic illness: a cross-sectional study. Indian J Pediatr. (2015) 82:1006–11. doi: 10.1007/s12098-015-1762-y
14. World Health Organization [WHO]. Innovative Care for Chronic Conditions: Building Blocks for Action. (2021). Available online at: https://www.who.int/chp/knowledge/publications/icccreport/en/ (accessed March 31, 2021).
15. Cohen E, Kuo DZ, Agrawal R, Berry JG, Bhagat SKM, Simon TD, et al. Children with medical complexity: an emerging population for clinical and research initiatives. Pediatrics. (2011) 127:529–38. doi: 10.1542/peds.2010-0910
16. Torpy JM, Campbell A, Glass RM. JAMA patient page. Chronic diseases of children. JAMA. (2010) 303:682. doi: 10.1001/jama.303.7.682
17. Berry JG, Hall M, Neff J, Goodman D, Cohen E, Agrawal R, et al. Children with medical complexity and medicaid: spending and cost savings. Health Aff. (2014) 33:2199–206. doi: 10.1377/hlthaff.2014.0828
18. Bravo L, Killela MK, Reyes BL, Santos KMB, Torres V, Huang C-C, et al. Self-management, self-efficacy, and health-related quality of life in children with chronic illness and medical complexity. J Pediatr Health Care. (2020) 34:304–14. doi: 10.1016/j.pedhc.2019.11.009
19. Jiang X, Walker K, Topps AK. A systematic review of self-care measures for adolescents with health needs. Qual Life Res. (2020) 30:967–81. doi: 10.1007/s11136-020-02685-1
20. Matarese M, Lommi M, De Marinis MG, Riegel B. A systematic review and integration of concept analyses of self-care and related concepts. J Nurs Scholarsh. (2018) 50:296–305. doi: 10.1111/jnu.12385
21. Richard AA, Shea K. Delineation of self-care and associated concepts. J Nurs Scholarsh. (2011) 43:255–64. doi: 10.1111/j.1547-5069.2011.01404.x
22. Martínez N, Connelly CD, Pérez A, Calero P. Self-care: a concept analysis. Int J Nurs Sci. (2021) 8:418–25. doi: 10.1016/j.ijnss.2021.08.007
23. Sanson G, Vellone E, Takao-Lopes C, Barrientos-Trigo S, Porcel-Gálvez AM, Riegel B, et al. Filling a gap in standardized nursing terminology. Development of a new nursing diagnosis proposal on heart failure self-care. Int J Nurs Knowl. (2022) 33:18–28. doi: 10.1111/2047-3095.12324
24. World Health Organization [WHO]. Self Care for Health. WHO Regional Office for South-East Asia. (2014). Available online at: https://apps.who.int/iris/handle/10665/205887 (accessed August 25, 2021).
25. Riegel B, Dickson VV. A situation-specific theory of heart failure self-care. J Cardiovasc Nurs. (2008) 23:190–6. doi: 10.1097/01.JCN.0000305091.35259.85
26. Riegel B, Jaarsma T, Strömberg A. A middle-range theory of self-care of chronic illness. ANS Adv Nurs Sci. (2012) 35:194–204. doi: 10.1097/ANS.0b013e318261b1ba
27. Riegel B, Jaarsma T, Lee CS, Strömberg A. Integrating symptoms into the middle-range theory of self-care of chronic illness. ANS Adv Nurs Sci. (2019) 42:206–15. doi: 10.1097/ANS.0000000000000237
28. Dall’Oglio I, Gasperini G, Carlin C, Biagioli V, Gawronski O, Spitaletta G, et al. Self-care in pediatric patients with chronic conditions: a systematic review of theoretical models. Int J Environ Res Public Health. (2021) 18:3513. doi: 10.3390/ijerph18073513
29. Ferris M, Cohen S, Haberman C, Javalkar K, Massengill S, Mahan JD, et al. Self-management and transition readiness assessment: development, reliability, and factor structure of the STARx questionnaire. J Pediatr Nurs. (2015) 30:691–9. doi: 10.1016/j.pedn.2015.05.009
30. Bee P, Pedley R, Rithalia A, Richardson G, Pryjmachuk S, Kirk S, et al. Self-Care Support for Children and Adolescents With Long-Term Conditions: the REfOCUS Evidence Synthesis. Southampton: NIHR Journals Library (2018).
31. Loseby P, Schache K, Cavadino A, Young S, Hofman PL, Serlachius A. The role of protective psychological factors, self-care behaviors, and HbA1c in young adults with type 1 diabetes. Pediatr Diabetes. (2021) 1–10. doi: 10.1111/pedi.13306 [Epub ahead of print].
32. Chen C-Y, Lo F-S, Chen B-H, Lu M-H, Hsin Y-M, Wang R-H. Pathways of emotional autonomy, self-care behaviors, and depressive symptoms on health adaptation in adolescents with type 1 diabetes. Nurs Outlook. (2017) 65:68–76. doi: 10.1016/j.outlook.2016.07.015
33. Steinweg KK, Killingsworth RE, Nannini RJ, Spayde J. The impact on a health care system of a program to facilitate self-care. Mil Med. (1998) 163:139–44. doi: 10.1093/milmed/163.3.139
34. Centers for Disease, Control and Prevention. Health and Economic Costs of Chronic Diseases | CDC. (2021). Available online at: https://www.cdc.gov/chronicdisease/about/costs/index.htm (accessed February 11, 2021).
35. Sayers SL, Riegel B, Pawlowski S, Coyne JC, Samaha FF. Social support and self-care of patients with heart failure. Ann Behav Med. (2008) 35:70–9. doi: 10.1007/s12160-007-9003-x
36. Baumgarten F, Cohrdes C, Schienkiewitz A, Thamm R, Meyrose A-K, Ravens-Sieberer U. [Health-related quality of life and its relation to chronic diseases and mental health problems among children and adolescents: results from KiGGS Wave 2]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. (2019) 62:1205–14. doi: 10.1007/s00103-019-03006-9
37. Kyngäs H. Compliance of adolescents with chronic disease. J Clin Nurs. (2000) 9:549–56. doi: 10.1046/j.1365-2702.2000.00368.x
38. Patton SR, Graham JL, Varlotta L, Holsclaw D Jr. Measuring self-care independence in children with cystic fibrosis: the self-care independence scale (SCIS). Pediatr Pulmonol. (2003) 36:123–30. doi: 10.1002/ppul.10271
39. Schulenberg JE, Sameroff AJ, Cicchetti D. The transition to adulthood as a critical juncture in the course of psychopathology and mental health. Dev Psychopathol. (2004) 16:799–806. doi: 10.1017/S0954579404040015
40. Shackleford JL, Kelley SJ, Spratling R. Applying the self-determination theory to health-related quality of life for adolescents with congenital heart disease. J Pediatr Nurs. (2019) 46:62–71. doi: 10.1016/j.pedn.2019.02.037
41. Tuohy E, Rawdon C, Gallagher P, Glacken M, Murphy N, Swallow V, et al. Children and young people’s experiences and perceptions of self-management of type 1 diabetes: a qualitative meta-synthesis. Health Psychol Open. (2019) 6:2055102919877105. doi: 10.1177/2055102919877105
42. Lewin AB, LaGreca AM, Geffken GR, Williams LB, Duke DC, Storch EA, et al. Validity and reliability of an adolescent and parent rating scale of type 1 diabetes adherence behaviors: the self-care inventory (SCI). J Pediatr Psychol. (2009) 34:999–1007. doi: 10.1093/jpepsy/jsp032
43. Dabney K, McClarin L, Romano E, Fitzgerald D, Bayne L, Oceanic P, et al. Cultural competence in pediatrics: health care provider knowledge, awareness, and skills. Int J Environ Res Public Health. (2015) 13:ijerh13010014. doi: 10.3390/ijerph13010014
44. Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. (2015) 4:1. doi: 10.1186/2046-4053-4-1
45. Mokkink LB, Terwee CB, Patrick DL, Alonso J, Stratford PW, Knol DL, et al. The COSMIN study reached international consensus on taxonomy, terminology, and definitions of measurement properties for health-related patient-reported outcomes. J Clin Epidemiol. (2010) 63:737–45. doi: 10.1016/j.jclinepi.2010.02.006
46. Sawin KJ, Heffelfinger A, Cashin SE, Brei TJ. The development of the adolescent/young adult self-management and independence scale II: psychometric data. J Pediatr Rehabil Med. (2018) 11:311–22. doi: 10.3233/PRM-170479
47. Guo J, Whittemore R, Grey M, Wang J, Zhou Z, He G. Diabetes self-management, depressive symptoms, quality of life and metabolic control in youth with type 1 diabetes in China. J Clin Nurs. (2013) 22:69–79. doi: 10.1111/j.1365-2702.2012.04299.x
48. Karahroudy FA, Shahboulaghi FM, Hosseini MA, Rasouli M, Biglarian A. Factors associated with self-management in adolescents with type 1 diabetes. Adv Nurs Midwifery. (2018) 27:1–5. doi: 10.21859/ANM-027032
49. Schilling LS, Dixon JK, Knafl KA, Lynn MR, Murphy K, Dumser S, et al. A new self-report measure of self-management of type 1 diabetes for adolescents. Nurs Res. (2009) 58:228–36. doi: 10.1097/NNR.0b013e3181ac142a
50. Modi AC, Monahan S, Daniels D, Glauser TA. Development and validation of the pediatric epilepsy medication self-management questionnaire. Epilepsy Behav. (2010) 18:94–9. doi: 10.1016/j.yebeh.2010.03.009
51. Tan JW, Khoo TB, Burharudin NF, Mohamed Shah N. Medication self-management among parents of children with epilepsy at a tertiary care center in Malaysia. Epilepsy Behav. (2020) 111:107317. doi: 10.1016/j.yebeh.2020.107317
52. Klinnert MD, McQuaid EL, Gavin LA. Assessing the family asthma management system. J Asthma. (1997) 34:77–88. doi: 10.3109/02770909709071206
53. Cantú-Quintanilla G, Ferris M, Otero A, Gutiérrez-Almaraz A, Valverde-Rosas S, Velázquez-Jones L, et al. Validation of the UNC TRxANSITION Scale™version 3 among Mexican adolescents with chronic kidney disease. J Pediatr Nurs. (2015) 30:e71–81. doi: 10.1016/j.pedn.2015.06.011
54. Cohen SE, Hooper SR, Javalkar K, Haberman C, Fenton N, Lai H, et al. Self-management and transition readiness assessment: concurrent, predictive and discriminant validation of the STARx questionnaire. J Pediatr Nurs. (2015) 30:668–76. doi: 10.1016/j.pedn.2015.05.006
55. Culen C, Herle M, König M, Hemberger S-H, Seferagic S, Talaska C, et al. Be on TRAQ-Cross-cultural adaptation of the transition readiness assessment questionnaire (TRAQ 5.0) and pilot testing of the German version (TRAQ-GV-15). J Transit Med. (2019) 1:1–8. doi: 10.1515/jtm-2018-0005
56. Ferris ME, Harward DH, Bickford K, Layton JB, Ferris MT, Hogan SL, et al. A clinical tool to measure the components of health-care transition from pediatric care to adult care: the UNC TRxANSITION scale. Renal Fail. (2012) 34:744–53. doi: 10.3109/0886022X.2012.678171
57. Ma J, Yu Q, Ding W, Zhang T, Zhang Y. Psychometric properties of the “self-management and transition to adulthood with Rx = treatment questionnaire” in Chinese children and young people with chronic diseases. Int J Nurs Pract. (2021) 27:e12880. doi: 10.1111/ijn.12880
58. Moynihan M, Saewyc E, Whitehouse S, Paone M, Mcpherson G. Assessing readiness for transition from paediatric to adult health care: revision and psychometric evaluation of the Am I ON TRAC for adult care questionnaire. J Adv Nurs. (2015) 71:1324–35. doi: 10.1111/jan.12617
59. Nazareth M, Hart L, Ferris M, Rak E, Hooper S, van Tilburg MAL. A parental report of youth transition readiness: the parent STARx questionnaire (STARx-P) and re-evaluation of the STARx child report. J Pediatr Nurs. (2018) 38:122–6. doi: 10.1016/j.pedn.2017.08.033
60. Sawicki GS, Kelemen S, Weitzman ER. Ready, set, stop: mismatch between self-care beliefs, transition readiness skills, and transition planning among adolescents, young adults, and parents. Clin Pediatr. (2014) 53:1062–8. doi: 10.1177/0009922814541169
61. Zhong Y, Gilleskie DB, van Tilburg MAL, Hooper SR, Rak E, Javalkar K, et al. Longitudinal self-management and/or transition readiness per the TR x ANSITION Index among patients with chronic conditions in pediatric or adult care settings. J Pediatr. (2018) 203:361–70.e1. doi: 10.1016/j.jpeds.2018.06.052
62. Giardini A, Pierobon A, Majani G, Biffa G, Volpe B, Sala A, et al. Adherence self report assessment in solid-organ pre and post transplant recipients. G Ital Med Lav Ergon. (2011) 33:A69–76.
63. Hart LC, Díaz-González de Ferris M, Nazareth M, Faldowski RA, Rak E, Hooper SR, et al. Evaluation of the TRxANSITION index–parent version for assessment of readiness to transition to adult care among youth with chronic conditions. J Pediatr Nurs. (2021) 58:1–8. doi: 10.1016/j.pedn.2020.08.010
64. Sawicki GS, Garvey KC, Toomey SL, Williams KA, Chen Y, Hargraves JL, et al. Development and validation of the adolescent assessment of preparation for transition: a novel patient experience measure. J Adolesc Health. (2015) 57:282–7. doi: 10.1016/j.jadohealth.2015.06.004
65. Sawicki GS, Lukens-Bull K, Yin X, Demars N, Huang I-C, Livingood W, et al. Measuring the transition readiness of youth with special healthcare needs: validation of the TRAQ–transition readiness assessment questionnaire. J Pediatr Psychol. (2011) 36:160–71. doi: 10.1093/jpepsy/jsp128
66. McGrady ME, Hommel KA. Medication adherence and health care utilization in pediatric chronic illness: a systematic review. Pediatrics. (2013) 132:730–40. doi: 10.1542/peds.2013-1451
67. Miles LM, Ducharme FM, Collin J, Blais L, Bacon SL, Lavoie KL, et al. Physician’s perspective regarding asthma guided self-management: directives or guidance? J Asthma. (2021):1–6. doi: 10.1080/02770903.2021.1914652 [Epub ahead of print].
68. Lerch MF, Thrane SE. Adolescents with chronic illness and the transition to self-management: a systematic review. J Adolesc. (2019) 72:152–61. doi: 10.1016/j.adolescence.2019.02.010
69. Miller VA. Involving youth with a chronic illness in decision-making: highlighting the role of providers. Pediatrics. (2018) 142:S142–8. doi: 10.1542/peds.2018-0516D
70. Wilson PM, Brooks F, Procter S, Kendall S. The nursing contribution to chronic disease management: a case of public expectation? Qualitative findings from a multiple case study design in England and Wales. Int J Nurs Stud. (2012) 49:2–14. doi: 10.1016/j.ijnurstu.2011.10.023
71. Figueiredo SV, de Sousa ACC, Gomes ILV. Children with special health needs and family: implications for Nursing. Rev Bras Enferm. (2016) 69:79–85. doi: 10.1590/0034-7167.2016690112i
72. Akinbami LJ, Moorman JE, Bailey C, Zahran HS, King M, Johnson CA, et al. Trends in asthma prevalence, health care use, and mortality in the United States, 2001-2010. NCHS Data Brief. (2012):1–8.
73. To T, Stanojevic S, Moores G, Gershon AS, Bateman ED, Cruz AA, et al. Global asthma prevalence in adults: findings from the cross-sectional world health survey. BMC Public Health. (2012) 12:204. doi: 10.1186/1471-2458-12-204
74. Montali L, Zulato E, Cornara M, Ausili D, Luciani M. Barriers and facilitators of type 1 diabetes self-care in adolescents and young adults. J Pediatr Nurs. (2022) 62:136–43. doi: 10.1016/j.pedn.2021.09.014
75. Schwartz LA, Tuchman LK, Hobbie WL, Ginsberg JP. A social-ecological model of readiness for transition to adult-oriented care for adolescents and young adults with chronic health conditions. Child Care Health Dev. (2011) 37:883–95. doi: 10.1111/j.1365-2214.2011.01282.x
76. Schwartz LA, Daniel LC, Brumley LD, Barakat LP, Wesley KM, Tuchman LK. Measures of readiness to transition to adult health care for youth with chronic physical health conditions: a systematic review and recommendations for measurement testing and development. J Pediatr Psychol. (2014) 39:588–601. doi: 10.1093/jpepsy/jsu028
77. Zhang LF, Ho JSW, Kennedy SE. A systematic review of the psychometric properties of transition readiness assessment tools in adolescents with chronic disease. BMC Pediatr. (2014) 14:4. doi: 10.1186/1471-2431-14-4
78. Lozano P, Houtrow A. Supporting self-management in children and adolescents with complex chronic conditions. Pediatrics. (2018) 141:S233–41. doi: 10.1542/peds.2017-1284H
79. González F, Rodríguez Celin MLM, Roizen M, Mato R, García Arrigoni P, Ugo F, et al. Status of the transition/transfer process for adolescents with chronic diseases at a national pediatric referral hospital in Argentina. Arch Argent Pediatr. (2017) 115:562–9. doi: 10.5546/aap.2017.eng.562
80. Schulman-Green D, Feder SL, Dionne-Odom JN, Batten J, En Long VJ, Harris Y, et al. Family caregiver support of patient self-management during chronic, life-limiting illness: a qualitative metasynthesis. J Fam Nurs. (2021) 27:55–72. doi: 10.1177/1074840720977180
81. Brown MI. Research in the development of nursing theory. The importance of a theoretical framework in nursing research. Nurs Res. (1964) 13:109–12. doi: 10.1097/00006199-196401320-00005
82. Sawin KJ, Margolis RHF, Ridosh MM, Bellin MH, Woodward J, Brei TJ, et al. Self-management and spina bifida: a systematic review of the literature. Disabil Health J. (2021) 14:100940. doi: 10.1016/j.dhjo.2020.100940
83. Saxby N, Beggs S, Battersby M, Lawn S. What are the components of effective chronic condition self-management education interventions for children with asthma, cystic fibrosis, and diabetes? A systematic review. Patient Educ Couns. (2019) 102:607–22. doi: 10.1016/j.pec.2018.11.001
84. Smith BM, Sharma R, Das A, Aboumatar H, Pitts SI, Day J, et al. Patient and family engagement strategies for children and adolescents with chronic diseases: a review of systematic reviews. Patient Educ Couns. (2021) 104:2213–23. doi: 10.1016/j.pec.2021.02.026
85. Catarino M, Charepe Z, Festas C. Promotion of self-management of chronic disease in children and teenagers: scoping review. Healthcare (Basel). (2021) 9:1642. doi: 10.3390/healthcare9121642
86. Wolf FM, Guevara JP, Grum CM, Clark NM, Cates CJ. Educational interventions for asthma in children. Cochrane Database Syst Rev. (2003) 1:CD000326. doi: 10.1002/14651858.CD000326
87. Savage E, Beirne P, Ni Chroinin M, Duff A, Fitzgerald T, Farrell D. Self−management education for cystic fibrosis. Cochrane Database Syst Rev. (2014) 9:CD007641. doi: 10.1002/14651858.CD007641.pub3
88. Rohilla L, Kaur S, Duggal M, Malhi P, Bharti B, Dayal D. Diabetes self-management education and support to improve outcomes for children and young adults with type 1 diabetes: an umbrella review of systematic reviews. Sci Diabetes Self Manag Care. (2021) 47:332–45. doi: 10.1177/26350106211031809
89. Lee CC, Enzler CJ, Garland BH, Zimmerman CJ, Raphael JL, Hergenroeder AC, et al. The development of health self-management among adolescents with chronic conditions: an application of self-determination theory. J Adolesc Health. (2021) 68:394–402. doi: 10.1016/j.jadohealth.2020.05.053
90. Herrmann-Garitz C, Muehlan H, Bomba F, Thyen U, Schmidt S. Conception and measurement of health-related transition competence for adolescents with chronic conditions - Development and testing of a self-report instrument. Gesundheitswesen. (2017) 79:491–6. doi: 10.1055/s-0035-1549986
91. De Maria M, Vellone E, Ausili D, Alvaro R, Di Mauro S, Piredda M, et al. Self-care of patient and caregiver DyAds in multiple chronic conditions: a LongITudinal studY (SODALITY) protocol. J Adv Nurs. (2019) 75:461–71. doi: 10.1111/jan.13834
Keywords: self-care, self-management, instruments, chronic disease, pediatric, adolescent, young adult, parent
Citation: Biagioli V, Spitaletta G, Kania V, Mascolo R, Gawronski O, Liburdi A, Manzi G, Salata M, Vellone E, Tiozzo E and Dall’Oglio I (2022) Instruments Measuring Self-Care in Children and Young Adults With Chronic Conditions: A Systematic Review. Front. Pediatr. 10:832453. doi: 10.3389/fped.2022.832453
Received: 09 December 2021; Accepted: 28 February 2022;
Published: 28 March 2022.
Edited by:
Mitsue Maru, University of Hyogo, JapanReviewed by:
Aviva Michelle Goldberg, University of Manitoba, CanadaJane Sattoe, Rotterdam University of Applied Sciences, Netherlands
Copyright © 2022 Biagioli, Spitaletta, Kania, Mascolo, Gawronski, Liburdi, Manzi, Salata, Vellone, Tiozzo and Dall’Oglio. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Immacolata Dall’Oglio, aW1tYWNvbGF0YS5kYWxsb2dsaW9Ab3BiZy5uZXQ=
†These authors share first authorship
 Valentina Biagioli
Valentina Biagioli Giuseppina Spitaletta1†
Giuseppina Spitaletta1† Rachele Mascolo
Rachele Mascolo Orsola Gawronski
Orsola Gawronski Giulia Manzi
Giulia Manzi Michele Salata
Michele Salata Ercole Vellone
Ercole Vellone Immacolata Dall’Oglio
Immacolata Dall’Oglio