
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pediatr. , 25 February 2022
Sec. Pediatric Gastroenterology, Hepatology and Nutrition
Volume 10 - 2022 | https://doi.org/10.3389/fped.2022.812201
Background and Aim: Per-oral endoscopic myotomy (POEM) is emerging as an effective treatment for pediatric achalasia. There are limited data on the long-term efficacy of POEM in children and adolescents with achalasia. In this study, we aim to evaluate the outcomes of POEM at ≥4 years follow-up.
Method: The data of consecutive children who underwent POEM (September 2013–July 2021) and completed at least 4 years follow-up were analyzed retrospectively. The primary outcome was clinical success (Eckardt ≤ 3) at ≥4 years follow-up. The secondary outcomes included the prevalence of gastroesophageal reflux disease (GERD) and predictors of recurrent symptoms (Eckardt ≥2) after POEM.
Results: A total of 69 children underwent POEM for achalasia during the study period. Of these, 41 (59.4%) children completed ≥4 years [mean 68.5 months (range 48–94)] follow-up, and 38 were included in the final analysis. The subtypes of achalasia included type I (28.9%), type II (60.5%), and type III (2.6%). There was a history of prior treatment in 11 children (28.9%). Clinical success was recorded in 36 (94.7%) patients who successfully underwent POEM. Recurrent symptoms (Eckardt ≥ 2) were noticed in 12 (31.6%) children at ≥4 years. On multivariate analysis, there were no identifiable factors which predicted recurrent symptoms after POEM. Symptomatic GERD and erosive esophagitis were detected in 13.8% (4/29) and 57.1% (8/14) of the children, respectively.
Conclusion: POEM is a durable treatment modality for achalasia in the pediatric population irrespective of the sub-type of achalasia and history of prior treatment.
Achalasia cardia is rare in the pediatric population, and <5% of all cases present below 15 years of age. The major modalities for the management of achalasia include pneumatic dilatation and Heller's myotomy. More recently, per-oral endoscopic myotomy (POEM) has been introduced as an endoscopic treatment option for achalasia. Multiple studies have established the safety and efficacy of POEM in adults with achalasia. Emerging data suggest that POEM may be an effective treatment in children and adolescents as well (1–10). However, there are limited data on the long-term outcomes of POEM in the pediatric population.
In this study, we aimed to analyze the long-term outcomes of POEM in children and adolescents with achalasia.
The data of children and adolescents (age ≤ 19 years) who underwent POEM for achalasia from September 2013 to July 2021 were analyzed retrospectively. Pediatric cases who completed at least 4 years of follow-up were included in the study. The study was approved by the institutional review board committee (AIG/AHF IRB: 34/2015).
The inclusion criteria were as follows:
a) Treatment naïve or previously treated cases with achalasia
b) Age ≤ 19 years
c) Minimum follow-up of 4 years
The exclusion driteria were as follows:
a) Follow-up <4 years
b) Refusal to provide written informed consent
The diagnosis of achalasia was established using high-resolution esophageal manometry (HREM), timed barium esophagogram, and upper gastrointestinal endoscopy. The technique of manometry in children has been described in our previous study (7). The type of esophageal motility disorder and lower esophageal sphincter (LES) pressures were recorded on manometry.
All the POEM procedures were performed by three operators (MR, ZN, and DNR) by anterior or posterior route using standard technique previously described (Figure 1) (11). Posterior myotomy was preferred in cases with a history of Heller's myotomy. Post-procedure, oral contrast study was performed on the second post-operative day before initiating oral diet.
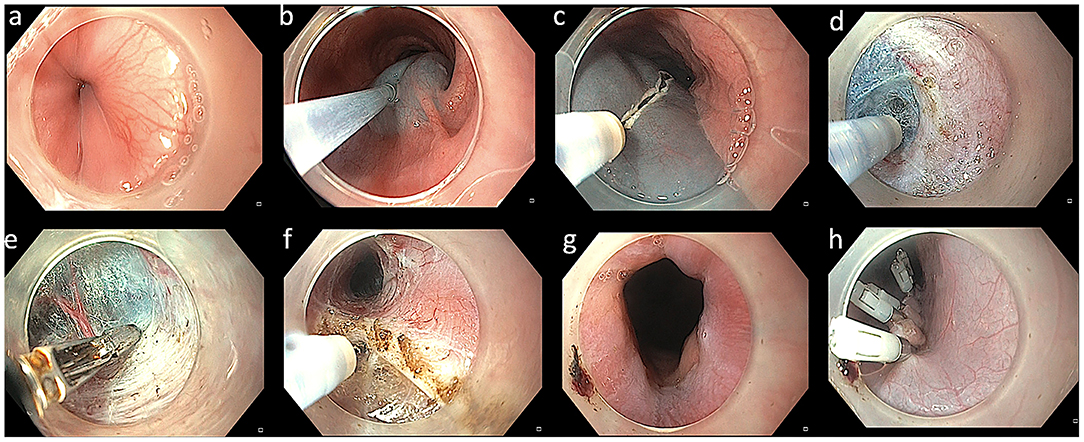
Figure 1. Technique of per-oral endoscopic myotomy in a case with achalasia. (a) Endoscopy revealing a tight gastroesophageal junction. (b) Mucosal lifting injection with diluted indigocarmine dye. (c) Mucosal incision using triangular tip knife. (d) Submucosal dissection using triangular knife. (e) Coagulation of vessels using coagulation forceps. (f) Myotomy using triangular knife. (g) Wide open gastroesophageal junction after completion of myotomy. (h) Closure of mucosal incision using multiple endoclips.
All patients were followed at pre-defined intervals, i.e., 3 months, 1 year, and annually thereafter. Evaluation at each visit included symptom assessment for achalasia (Eckardt score) as well as gastroesophageal reflux (heartburn and regurgitation). Objective evaluation including esophageal manometry and 24-h pH impedance study were performed at 3 months after POEM.
The primary outcome of the study was clinical efficacy at ≥4 years follow-up. Clinical success was defined using Eckardt score which is a composite score consisting of sub-scores for dysphagia (0–3), regurgitation (0–3), chest pain (0–3), and weight loss (0–3). The minimum and maximum possible scores are 0 and 12, respectively. Clinical success was defined as Eckardt score ≤ 3. The outcomes were recorded during annual follow-up visits. All the patients who completed ≥4 years and could not come for physical visits were contacted by telephonic questionnaire for clinical success and symptomatic gastroesophageal reflux disease (GERD). Clinical failure was defined as Eckardt score >3. Recurrence of symptoms was defined as any degree of symptoms but not amounting to clinical failure (Eckardt >1 and ≤ 3).
The secondary outcomes included the predictors of recurrent symptoms (Eckardt ≥ 2) after POEM. Reflux esophagitis was graded according to the Los Angeles classification system (LA grades A to D) (12).
The continuous data were expressed as mean (standard deviation) or median (interquartile range) and compared with independent sample t-test and the categorical data as frequencies and compared with chi-square test unless otherwise specified. The comparison of Eckardt score between pre- and post-POEM (at 1 and 4 years) was done using repeated measure analysis of variance (ANOVA). Multivariate analysis was performed using binominal logistic regression to ascertain the effects of age, gender, type of achalasia, Eckardt score, and LES pressures (pre- and post-POEM) on recurrence of symptoms at long-term follow-up. The linearity of the continuous variables with respect to the logit of the dependent variable was assessed via the Box–Tidwell procedure. All the tests of significance were two-tailed, and a p < 0.05 was considered to indicate statistical significance.
A total of 69 children underwent POEM for achalasia during the study period. Of these, 41 (59.4%) children completed ≥4 years [mean 68.5 months (range 48–94)] follow-up. Data on clinical efficacy were available in 38 children and were included in the final analysis. The spectrum of motility disorders included 11 (28.9%) with type I achalasia, 23 (60.5%) with type II achalasia, and 1 (2.6%) with type III achalasia. Manometry data were not available in three children. A history of prior treatment was present in 11 (28.9%; Table 1).
POEM was technically successful in 37 (97.4%) children. POEM was deferred in one child due to the child's small size and neurological problems. Baseline Eckardt score, manometry parameters, and intra-operative details including length and orientation of myotomy have been outlined in Table 1.
The data regarding efficacy was available in 38/41 (92.7%) patients. Clinical success was recorded in 36 (94.7%) patients who successfully underwent POEM and were available for final follow-up. In intention to treat analysis [including technical failures (1, 2.6%) and lost to follow-up (2, 7.9%)], the clinical success in the overall group was observed in 36/42 (85.7%). There was significant reduction in the median Eckardt scores at 1 year [1(0–1)] and ≥4 years [1(0–2)] as compared to baseline [7(6–8)] (p < 0.001; Figure 2 and Table 2).
The secondary outcomes included predictors of recurrent symptoms and incidence of GERD after POEM.
Recurrent symptoms equivalent to Eckardt ≥2 were noticed in 12 (31.6%) children at ≥4 years. On univariate and multivariate analysis, factors including baseline Eckardt score, type of achalasia, length and orientation of myotomy, baseline LES pressure, and history of prior treatment had no significant impact on the recurrence of symptoms after POEM (Table 3).
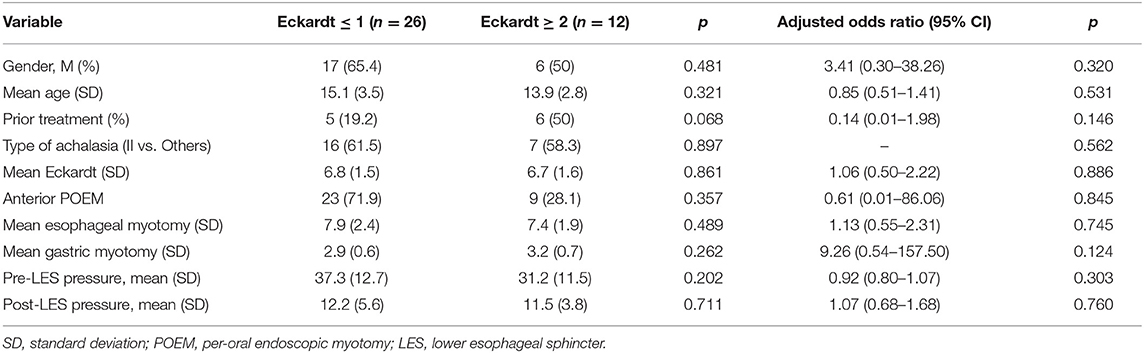
Table 3. Multivariate analysis for prediction of recurrent symptoms after per-oral endoscopic myotomy.
The data on symptomatic GERD and reflux esophagitis was available in 29 (76.3%) and 14 (36.8%) children, respectively. Symptoms of GERD were evident in 4 (13.8%) children. Erosive esophagitis was detected in 8 (57.1%). All cases had mild (LA grade A: 6 and B: 2) esophagitis (Table 2).
In this study, we found POEM to be an effective and durable treatment modality in children and adolescents with achalasia cardia. Although erosive esophagitis was detected in over half of the children, severe esophagitis and symptomatic GERD were uncommon on long-term follow-up.
The safety and short-term efficacy of POEM has been established in adult patients with achalasia as well as non-achalasia spastic motility disorders of the esophagus. In pediatric cases with achalasia, Heller's myotomy and pneumatic dilatation are the preferred treatment modalities (13). Emerging data suggest that POEM is an effective alternative to pneumatic dilatation and Heller's myotomy in pediatric achalasia as well (6–8). However, there is limited data to suggest the long-term efficacy of POEM in children and adolescents. Since achalasia is a progressive disease, long-term outcomes are crucial to establish the durability of POEM in esophageal achalasia.
In this study, we evaluated the outcomes of POEM including clinical success and GERD in pediatric cases who completed at least 4 years follow-up. The mean follow-up of the entire cohort was 69 months, i.e., >5 years. Overall, clinical success was recorded in 95% (per protocol) and 86% (intention to treat) of children at ≥4 years follow-up. In previously published studies with relatively long follow-up periods, the clinical success rate of POEM in pediatric achalasia ranged from 95 to 100% at follow-up ranging from 26 to 40 months (3, 8, 14, 15) (Table 4). Our results suggest that in pediatric achalasia, the response to POEM is sustained for at least 4 years. The results are similar to those in adult patients in whom clinical success has been recorded in 80–95% of cases at a median follow-up ranging from 3 to 7 years (16–25).
Although there is no randomized trial in children, the clinical success rates with POEM appear to be higher as compared to Heller's myotomy and pneumatic dilatation (26, 27). In a recent systematic review, the clinical success with Heller's myotomy was 78% at a mean follow-up of 3 years and 45% with pneumatic dilatation at an average follow-up of 3.5 years (27).
There were only two clinical failures on long-term follow-up. Consequently, we analyzed the risk factors for recurrent symptoms equivalent to Eckardt >1 on long-term follow-up. A majority of the cases with recurrent symptoms had occasional dysphagia and or regurgitation (equivalent to Eckardt score of ≤2). On multivariate analysis, there were no predictors for recurrent symptoms at long-term follow-up. However, it is important to note that the analysis was intended for the prediction of recurrent symptoms and not clinical failure. Large, multicenter studies are required to establish the predictors of outcomes and optimize the use of POEM in pediatric achalasia.
Symptoms of GERD and erosive esophagitis were detected in 14% and 57% of children, respectively. GERD is a significant issue after POEM and more frequent as compared to pneumatic dilatation and Heller's myotomy with fundoplication (28). In adults, GERD is evident in almost half of the patients on 24-h pH study, and reflux esophagitis is noted in 20–40% of patients after POEM (29–31). In this study, all the children had mild reflux esophagitis (≤LA grade B) suggesting that GERD may not be a major hindrance while adopting POEM in the management algorithm for pediatric cases. Our results are in concordance with a recent study in adult patients in which a majority of the patients were asymptomatic for GERD, developed mild esophagitis (Los Angeles grade A or B), and responded well to proton pump inhibitor therapy (31).
We acknowledge that objective evaluation of GERD could not be performed in a substantial proportion of cases on long-term follow-up. Therefore, the possibility of selection bias cannot be completely ruled out. In addition, the symptoms of GERD like regurgitation, heartburn, and chest pain can closely mimic those of achalasia which may confound the interpretation of results. Nevertheless, our study provides some reassurance regarding this potential long-term complication of POEM.
There are several strengths of our study. To the best of our knowledge, this is one of the largest studies evaluating the long-term outcomes of POEM (≥4 years). The number of cases who were lost to follow-up were within an acceptable range (<10%). We acknowledge a few noteworthy limitations of this study. These include the retrospective design and lack of objective evaluation of success and GERD using timed barium swallow, esophageal manometry, and endoscopy. The evaluation of symptoms was based on Eckardt score, which has not been validated in pediatric patients. Similarly, there is limited information regarding the interpretation of esophageal manometry in children. The impact of POEM on the nutritional status of the children could not be assessed due to incomplete information.
POEM is a durable treatment option for achalasia cardia. There is no substantial impact of the sub-type of achalasia and prior treatment on the long-term outcomes of POEM.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by AIG/AHF IRB. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
ZN and MR were involved in the conception of the study. JB and RG were involved in acquisition and analysis of the data. SD and DR were involved in revising the manuscript for important intellectual content. All authors agreed to the final version of the manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Li C, Tan Y, Wang X, Liu D. Peroral endoscopic myotomy for treatment of achalasia in children and adolescents. J Pediatr Surg. (2015) 50:201–5. doi: 10.1016/j.jpedsurg.2014.10.017
2. Tang X, Gong W, Deng Z, Zhou J, Ren Y, Zhang Q, et al. Usefulness of peroral endoscopic myotomy for treating achalasia in children: experience from a single center. Pediatr Surg Int. (2015) 31:633–8. doi: 10.1007/s00383-015-3717-9
3. Tan Y, Zhu H, Li C, Chu Y, Huo J, Liu D. Comparison of peroral endoscopic myotomy and endoscopic balloon dilation for primary treatment of pediatric achalasia. J Pediatr Surg. (2016) 51:1613–8. doi: 10.1016/j.jpedsurg.2016.06.008
4. Kethman WC, Thorson CM, Sinclair TJ, Berquist WE, Chao SD, Wall JK. Initial experience with peroral endoscopic myotomy for treatment of achalasia in children. J Pediatr Surg. (2018) 53:1532–6. doi: 10.1016/j.jpedsurg.2017.07.023
5. Miao S, Wu J, Lu J, Wang Y, Tang Z, Zhou Y, et al. Peroral endoscopic myotomy in children with achalasia: a relatively long-term single-center study. J Pediatr Gastroenterol Nutr. (2018) 66:257–62. doi: 10.1097/MPG.0000000000001675
6. Chone A, Familiari P, von Rahden B, Desai P, Inoue H, Shimamura Y, et al. Multicenter evaluation of clinical efficacy and safety of per-oral endoscopic myotomy in children. J Pediatr Gastroenterol Nutr. (2019) 69:523–7. doi: 10.1097/MPG.0000000000002432
7. Nabi Z, Ramchandani M, Chavan R, Darisetty S, Kalapala R, Shava U, et al. Outcome of peroral endoscopic myotomy in children with achalasia. Surg Endosc. (2019) 33:3656–64. doi: 10.1007/s00464-018-06654-1
8. Liu Z, Wang Y, Fang Y, Huang Y, Yang H, Ren X, et al. Short-term safety and efficacy of peroral endoscopic myotomy for the treatment of achalasia in children. J Gastroenterol. (2020) 55:159–68. doi: 10.1007/s00535-019-01607-4
9. Wood LS, Chandler JM, Portelli KE, Taylor JS, Kethman WC, Wall JK. Treating children with achalasia using per-oral endoscopic myotomy (POEM): Twenty-one cases in review. J Pediatr Surg. (2020) 55:1006–12. doi: 10.1016/j.jpedsurg.2020.02.028
10. Saez J, Mejia R, Pattillo JC, Vuletin F, Monrroy H, Jaime F, et al. Per oral endoscopic myotomy (POEM) in pediatric patients with esophageal achalasia: first Latin-American experience. J Pediatr Surg. (2021) 56:706–10. doi: 10.1016/j.jpedsurg.2020.06.007
11. Nabi Z, Ramchandani M, Reddy DN. Peroral endoscopic myotomy in a child with achalasia cardia. J Pediatr Gastroenterol Nutr. (2017) 65:e44. doi: 10.1097/MPG.0000000000001534
12. Lundell LR, Dent J, Bennett JR, Blum AL, Armstrong D, Galmiche JP, et al. Endoscopic assessment of oesophagitis: clinical and functional correlates and further validation of the Los Angeles classification. Gut. (1999) 45:172–80. doi: 10.1136/gut.45.2.172
13. van Lennep M, van Wijk MP, Omari TIM, Salvatore S, Benninga MA, Singendonk MMJ, et al. Clinical management of pediatric achalasia: a survey of current practice. J Pediatr Gastroenterol Nutr. (2019) 68:521–6. doi: 10.1097/MPG.0000000000002221
14. Mangiola F, Familiari P, Landi R, Calì A, D'Aversa F, Bove V, et al. Peroral endoscopic myotomy for the treatment of achalasia in children: experience of a single center with long term follow-up. Gastrointest Endosc. (2018) 87:AB542. doi: 10.1016/j.gie.2018.04.2179
15. Yamashita K, Shiwaku H, Ohmiya T, Okada H, Inoue H, Hasegawa S. UEG week 2018 poster presentations. United Eur Gastroenterol J. (2018) 6:A336–7. doi: 10.1177/2050640618792819
16. Brewer Gutierrez OI, Moran RA, Familiari P, Dbouk MH, Costamagna G, Ichkhanian Y, et al. Long-term outcomes of per-oral endoscopic myotomy in achalasia patients with a minimum follow-up of 4 years: a multicenter study. Endosc Int Open. (2020) 8:E650–5. doi: 10.1055/a-1120-8125
17. Teitelbaum EN, Dunst CM, Reavis KM, Sharata AM, Ward MA, DeMeester SR, et al. Clinical outcomes five years after POEM for treatment of primary esophageal motility disorders. Surg Endosc. (2018) 32:421–7. doi: 10.1007/s00464-017-5699-2
18. Li QL, Wu QN, Zhang XC, Xu MD, Zhang W, Chen SY, et al. Outcomes of per-oral endoscopic myotomy for treatment of esophageal achalasia with a median follow-up of 49 months. Gastrointest Endosc. (2018) 87:1405–12.e3. doi: 10.1016/j.gie.2017.10.031
19. Guo H, Yang H, Zhang X, Wang L, Lv Y, Zou X, et al. Long-term outcomes of peroral endoscopic myotomy for patients with achalasia: a retrospective single-center study. Dis Esophagus. (2017) 30:1–6. doi: 10.1093/dote/dow011
20. McKay SC, Dunst CM, Sharata AM, Fletcher R, Reavis KM, Bradley DD, et al. POEM: clinical outcomes beyond 5 years. Surg Endosc. (2021) 35:5709–16. doi: 10.1007/s00464-020-08031-3
21. Zhang WG, Chai NL, Zhai YQ, Linghu EQ, Li HK. Long-term outcomes of peroral endoscopic myotomy in achalasia patients with a minimum follow-up of 7 years. Chin Med J. (2020) 133:996–8. doi: 10.1097/CM9.0000000000000735
22. Tefas C, Boros C, Ciobanu L, Surdea-Blaga T, Tantau A, Tantau M. POEM: five years of experience in a single east European center. J Gastrointestin Liver Dis. (2020) 29:323–8. doi: 10.15403/jgld-2676
23. Onimaru M, Inoue H, Fujiyoshi Y, Abad MRA, Nishikawa Y, Toshimori A, et al. Long-term clinical results of per-oral endoscopic myotomy (POEM) for achalasia: first report of more than 10-year patient experience as assessed with a questionnaire-based survey. Endosc Int Open. (2021) 9:E409–16. doi: 10.1055/a-1333-1883
24. Campagna RAJ, Cirera A, Holmstrom AL, Triggs JR, Teitelbaum EN, Carlson DA, et al. Outcomes of 100 patients more than 4 years after POEM for achalasia. Ann Surg. (2021) 273:1135–40. doi: 10.1097/SLA.0000000000004830
25. Modayil RJ, Zhang X, Rothberg B, Kollarus M, Galibov I, Peller H, et al. Peroral endoscopic myotomy: 10-year outcomes from a large, single-center U.S. series with high follow-up completion and comprehensive analysis of long-term efficacy, safety, objective GERD, and endoscopic functional luminal assessment. Gastrointest Endosc. (2021) 94:930–42. doi: 10.1016/j.gie.2021.05.014
26. Saliakellis E, Thapar N, Roebuck D, Cristofori F, Cross K, Kiely E, et al. Long-term outcomes of Heller's myotomy and balloon dilatation in childhood achalasia. Eur J Pediatr. (2017) 176:899–907. doi: 10.1007/s00431-017-2924-x
27. Goneidy A, Cory-Wright J, Zhu L, Malakounides G. Surgical management of esophageal achalasia in pediatrics: a systematic review. Eur J Pediatr Surg. (2020) 30:13–20. doi: 10.1055/s-0039-1697958
28. Facciorusso A, Singh S, Abbas Fehmi SM, Annese V, Lipham J, Yadlapati R. Comparative efficacy of first-line therapeutic interventions for achalasia: a systematic review and network meta-analysis. Surg Endosc. (2021) 35:4305–14. doi: 10.1007/s00464-020-07920-x
29. Kumbhari V, Familiari P, Bjerregaard NC, Pioche M, Jones E, Ko WJ, et al. Gastroesophageal reflux after peroral endoscopic myotomy: a multicenter case-control study. Endoscopy. (2017) 49:634–42. doi: 10.1055/s-0043-105485
30. Nabi Z, Ramchandani M, Reddy DN. Per-oral endoscopic myotomy and gastroesophageal reflux: Where do we stand after a decade of “POETRY”? Indian J Gastroenterol. (2019) 38:287–94. doi: 10.1007/s12664-019-00980-5
Keywords: achalasia, child, adolescents, per-oral endoscopic myotomy, outcome (recurrence, chronicity)
Citation: Nabi Z, Ramchandani M, Basha J, Goud R, Darisetty S and Reddy DN (2022) POEM Is a Durable Treatment in Children and Adolescents With Achalasia Cardia. Front. Pediatr. 10:812201. doi: 10.3389/fped.2022.812201
Received: 09 November 2021; Accepted: 14 January 2022;
Published: 25 February 2022.
Edited by:
Jayanta Samanta, Post Graduate Institute of Medical Education and Research (PGIMER), IndiaReviewed by:
Rishi Bolia, All India Institute of Medical Sciences, Rishikesh, IndiaCopyright © 2022 Nabi, Ramchandani, Basha, Goud, Darisetty and Reddy. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zaheer Nabi, emFoZWVybmFiaTE5NzhAZ21haWwuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.