
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Pediatr., 15 March 2022
Sec. Pediatric Urology
Volume 10 - 2022 | https://doi.org/10.3389/fped.2022.805579
 Chengjun Yu1,2,3,4
Chengjun Yu1,2,3,4 Yang Hu1,2,3
Yang Hu1,2,3 Ling Wang1,2,3
Ling Wang1,2,3 Lian Kang1,2,3,5
Lian Kang1,2,3,5 Jie Zhao1,2,3
Jie Zhao1,2,3 Jiandong Lu1,2,3
Jiandong Lu1,2,3 Tao Lin1,2,3,4,6
Tao Lin1,2,3,4,6 Dawei He1,2,3,4,5,6
Dawei He1,2,3,4,5,6 Shengde Wu1,2,3,4,5,6*
Shengde Wu1,2,3,4,5,6* Guanghui Wei1,2,3,4,5,6
Guanghui Wei1,2,3,4,5,6Purpose: To compare the safety, efficacy, and cosmetic results of single-incision scrotal orchiopexy (SISO) and traditional two-incision inguinal orchiopexy (TTIO) for primary palpable undescended testes (PUDTs) in children.
Materials and Methods: A systematic literature search of all relevant studies published on PubMed, Embase, Medline, Cochrane Library, Web of Science database, and Wanfang data until July 2021 was conducted. The operative time, hospitalization duration, conversion rate, wound infection or dehiscence, scrotal hematoma or swelling, testicular atrophy, reascent, hernia or hydrocele, analgesics needs, and cosmetic results were compared between SISO and TTIO using the Mantel–Haenszel or inverse-variance method.
Results: A total of 17 studies involving 2,627 children (1,362 SISOs and 1,265 TTIOs) were included in the final analysis. The conversion rate of SISO was 3.6%. The SISO approach had a statistically significant shorter operative time than the TTIO approach for PUDT (weighted mean difference−11.96, 95% confidence interval −14.33 to −9.59, I2 = 79%, P < 0.00001) and a shorter hospital stay (weighted mean difference−1.05, 95% confidence interval −2.07 to −0.03, P = 0.04). SISO needed fewer analgesics and had better cosmetic results than TTIO. SISO had a similar total, short-term, or long-term complication rate with TTIO.
Conclusion: Compared with TTIO, SISO has the advantages of shorter operative time, shorter hospitalization duration, less postoperative pain, and better cosmetic appealing results. SISO is a safe, effective, promising, and potential minimal invasive surgical approach for PUDT. SISO is an alternative to TTIO in selected cryptorchid patients, especially for lower positioned ones.
Systematic Review Registration: https://www.crd.york.ac.uk/PROSPERO/, identifier: CRD42021268562.
Cryptorchidism, or undescended testes (UDTs), is one of the most common congenital abnormalities in male neonates, with a prevalence of 1.0–4.6% in full-term boys and a higher incidence in preterm boys (1). Cryptorchidism is a well-known independent risk fact for infertility, testicular cancer, testicular torsion, and other disease (2). It is vital to correct the UDT at an early age to avoid subsequent testicular degeneration. Fortunately, ~80% of the UDT are palpable and located in the inguinal canal, external inguinal ring, or even upper scrotal (3), making the traditional two-incision inguinal orchiopexy (TTIO) the best surgical approach to correct cryptorchidism (4).
The TTIO has two incisions: one inguinal incision to open the external oblique fascia and inguinal canal to visualize the cord structure and dissect the processus vaginalis; another second scrotal incision to fix the descended testis within the scrotum (5, 6). It was believed that the TTIO was convenient and helpful for sufficient mobilization of the spermatic cord, separation and high ligation of the processus vaginalis or hernia sac to avoid subsequent hernia or hydrocele, and most importantly, to achieve adequate vessel length for cryptorchid testis to be placed in the scrotum without tension (7, 8).
In 1989, Bianchi and Squire proposed the single-incision scrotal orchiopexy (SISO) for palpable undescended testes (PUDTs) to reduce the potential morbidity and reach a goal for better cosmetic appearance (9). From then on, more and more authors pointed out that SISO had the advantages of shorter operative time and less pain; in the meanwhile, it also had considerable complication rates compared with TTIO (10–15). This trans-scrotal surgical technique could also be applied to secondary cryptorchidism, hydrocele, and even indirect hernias (16).
In 2016, Feng et al. conducted the first systematic review and meta-analysis to compare the SISO with TTIO strategy regarding operative time and complications (17). Although the evidence was still largely limited by the small sample size in their study, these several newly published randomized controlled studies would provide more evidence. Therefore, we updated this study and compared the operative time, hospitalization duration, patent processus vaginalis, short-term and long-term complications, analgesic needs, scarring, and conversions between SISO and TTIO for primary PUDT to provide strengthened evidence and to serve clinical decision and guideline making.
This systematic review and meta-analysis were conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analysis statement. The initial systematic literature retrieve was conducted on July 11, 2021, without the restriction of language and region. The searched databases were the following: PubMed, Medline, Embase, Cochrane Library, Web of Science Database, China National Knowledge Infrastructure, and WanFang Data. Using the Boolean approach, these databases were individually searched for the following key terms, mainly in titles, keywords, and abstracts: (cryptorchidism OR undescended test* OR non-descended test* OR non descended test*) AND (orchidopexy OR scrotal OR inguinal OR single incision OR trans-scrotal approach). Both the Mesh Term search and keyword search were combined. In addition, the reference lists were manually retrieved to broaden the search.
The inclusion criteria for our systematic review and meta-analysis were (1) clinical trials comparing the SISO and TTIO surgical strategy regardless of prospective or retrospective designed studies and (2) children who were diagnosed with primary PUDTs and (3) have a follow-up time of more than 3 months and adequate initial data available. Exclusion criteria were (1) no TTIO as a control group, (2) secondary cryptorchidism or has a history of former orchiopexy or inguinal operation, and (3) studies that did not provide sufficient data or repeated or duplicate publications. Only the latest study was included if there were more than one report paper from one clinical center or duplicate publications detected.
All included initial trials were thoroughly understood and analyzed; the baseline characteristics summarized were authors, publication years, countries, study periods and designs, age of participants, single-incision scrotal techniques (high transverse stria scrotal orchiopexy or low trans-scrotal mid raphe orchiopexy), laterality, and location of testes. Operative time, hospitalization duration, patent processus vaginalis, short-term complications (wound infection or dehiscence, scrotal hematoma or severe swelling), and long-term complications (testicular atrophy, testicular reascent, hernia, or hydrocele) were extracted to compare these two surgical approaches for PUDT. We also made possible comparisons between each single-incision technique and conventional two-incision orchiopexy. Moreover, conversion rates, postoperative analgesics needs, and cosmetic results were also concerned. Cometic results were only evaluated upon exerted operation scars. Two reviewers (CJY and YH) independently conducted the literature search, screening, and data extraction. All discrepancies were resolved by discussion or, still unresolved, by a mediating reviewer (SDW).
There was no best suitable tool to assess the quality of included studies in this study. For compromising reasons, the methodological quality of retrospective case–control studies was assessed using the Newcastle–Ottawa Quality Assessment Scale (NOS), and the prospective randomized controlled trials were assessed using the Jadad Scale. This NOS used a star system (measured 0–9) to assess the quality of a study in three domains: the selection of the study groups, the comparability of the groups, and the ascertainment of exposure of interest for case–control studies. Also, the Jadad Scale evaluated the quality of a randomized study by randomization, blinding, and withdrawals, which marked 0–5; 1–2 indicated low quality and 3–5 high quality.
All statistical data analyses were completed by Review Manager version 5.3 (Cochrane Collaboration, Oxford, United Kingdom). The odds ratios (ORs) and 95% confidence intervals (CI) were calculated for dichotomous variables using the Mantel–Haenszel method. In addition, for continuous variables, mean difference (MD) and 95% CI were applied using the inverse-variance method. The pooled heterogeneity of included studies was tested using both the chi-square test (p ≥ 0.1, indicating low heterogeneity) and I2 index statistics (0%, indicating no inter-study heterogeneity) (18). The fixed-effect model was applied if I2 <50%; otherwise, the random effect model was used (19). Sensitivity analysis was conducted by removing a study per circle to detect the heterogeneity contribution of each study. Funnel plots visually detected publication basis. A P < 0.05 was considered statistically significant in this study.
Initial electronic databases search yielded 5,738 possible articles (Figure 1). In addition, three papers were added from a manual search of the retrieved articles and relevant reviews. A total of 4,333 titles and abstracts were screened after eliminating 1,408 duplicates. Eventually, only 17 studies involving 2,627 children (1,362 underwent SISOs and 1,265 TTIOs) met our inclusion criteria after a comprehensive full-text screen. There were seven prospective trials (6, 12, 15, 20–23) and 10 retrospective studies (10, 11, 13, 14, 24–29).
The baseline characteristics of included studies are summarized in Table 1. Tables 2, 3 demonstrate the extracted data information of the operative time, hospitalization duration, patent processus vaginalis, short-term complications (wound infection or dehiscence, scrotal hematoma or severe swelling), long-term complications (testicular atrophy, testicular reascent, hernia, or hydrocele), postoperative analgesics needs, and cosmetic result between SISO and TTIO for PUDT in detail.
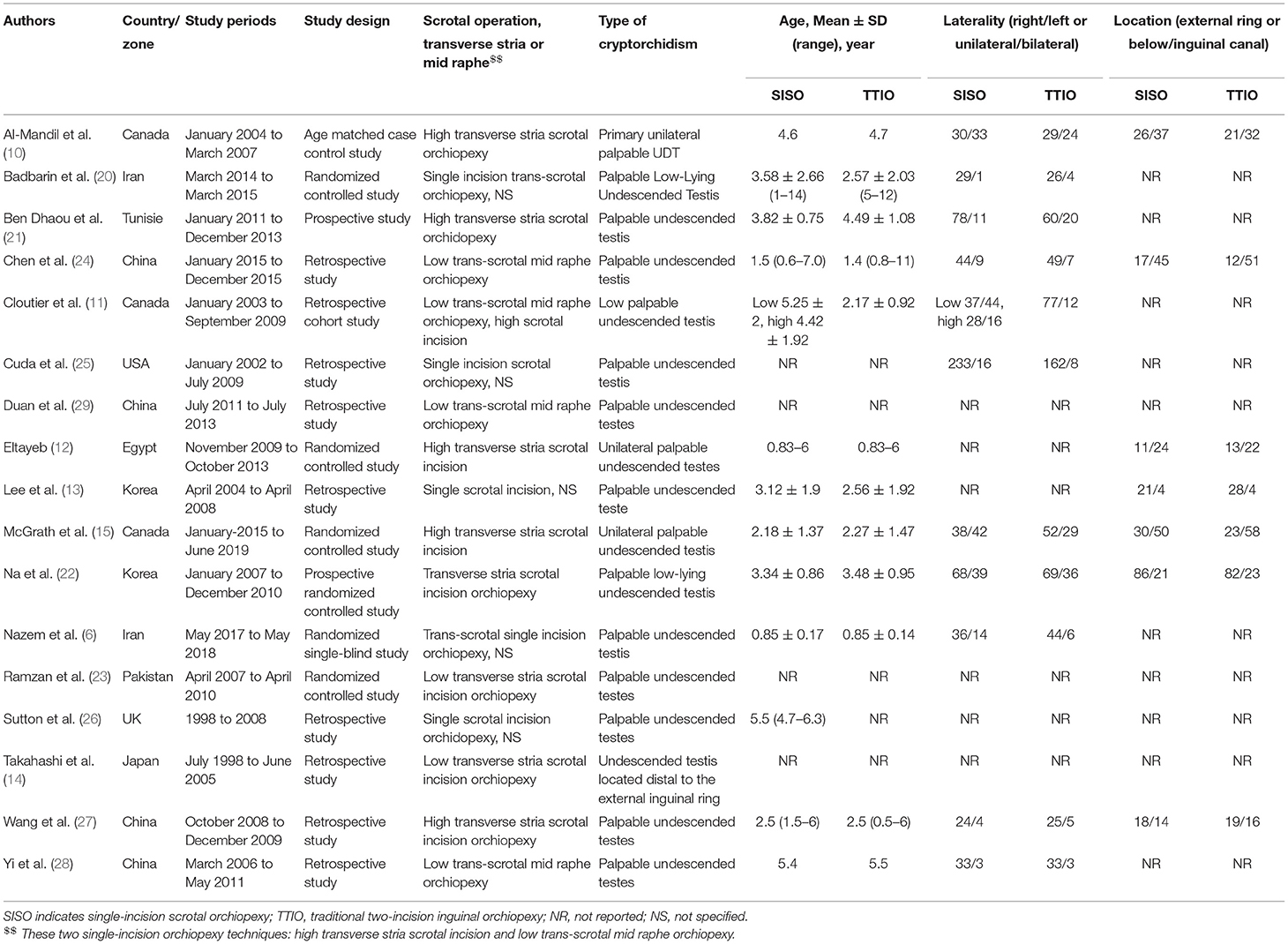
Table 1. Baseline characteristics of these included 17 initial studies comparing single-incision scrotal orchiopexy and traditional two-incision inguinal orchiopexy for primary palpable undescended testes.
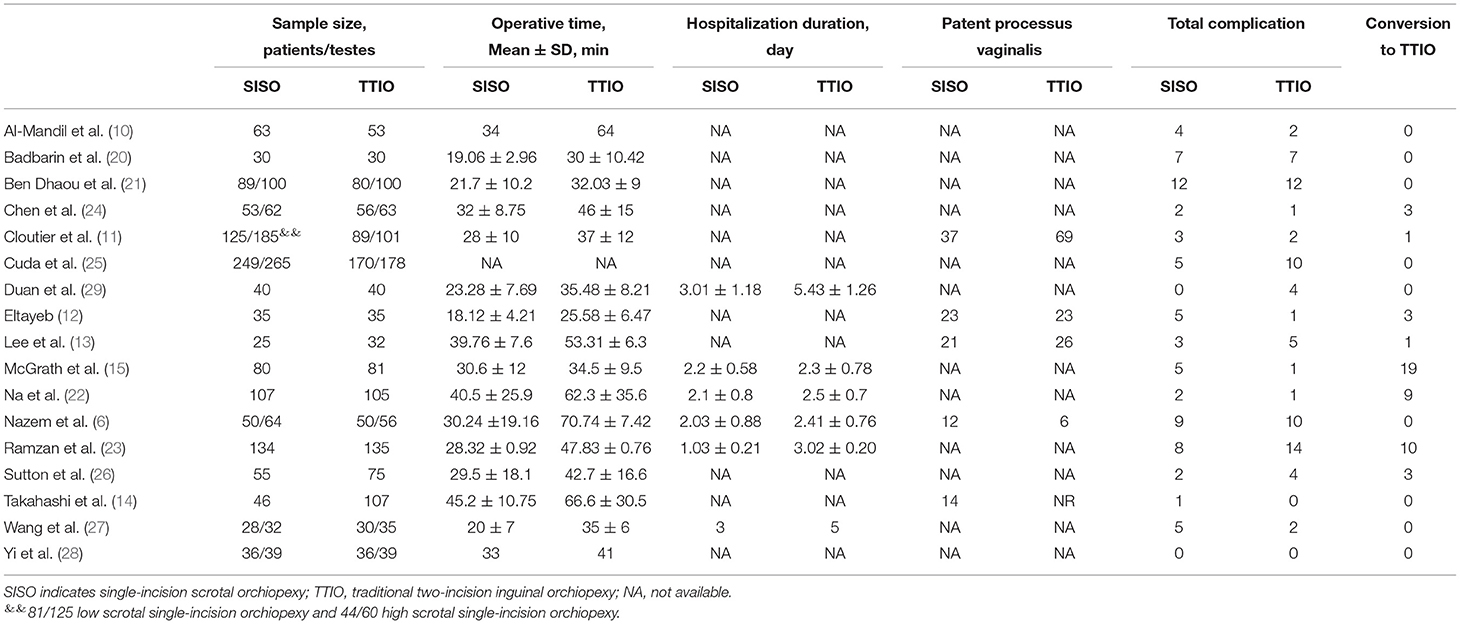
Table 2. Sample size, operative time, hospitalization duration, patent processus vaginalis, total complications and conversions between single-incision scrotal orchiopexy and traditional two-incision inguinal orchiopexy.
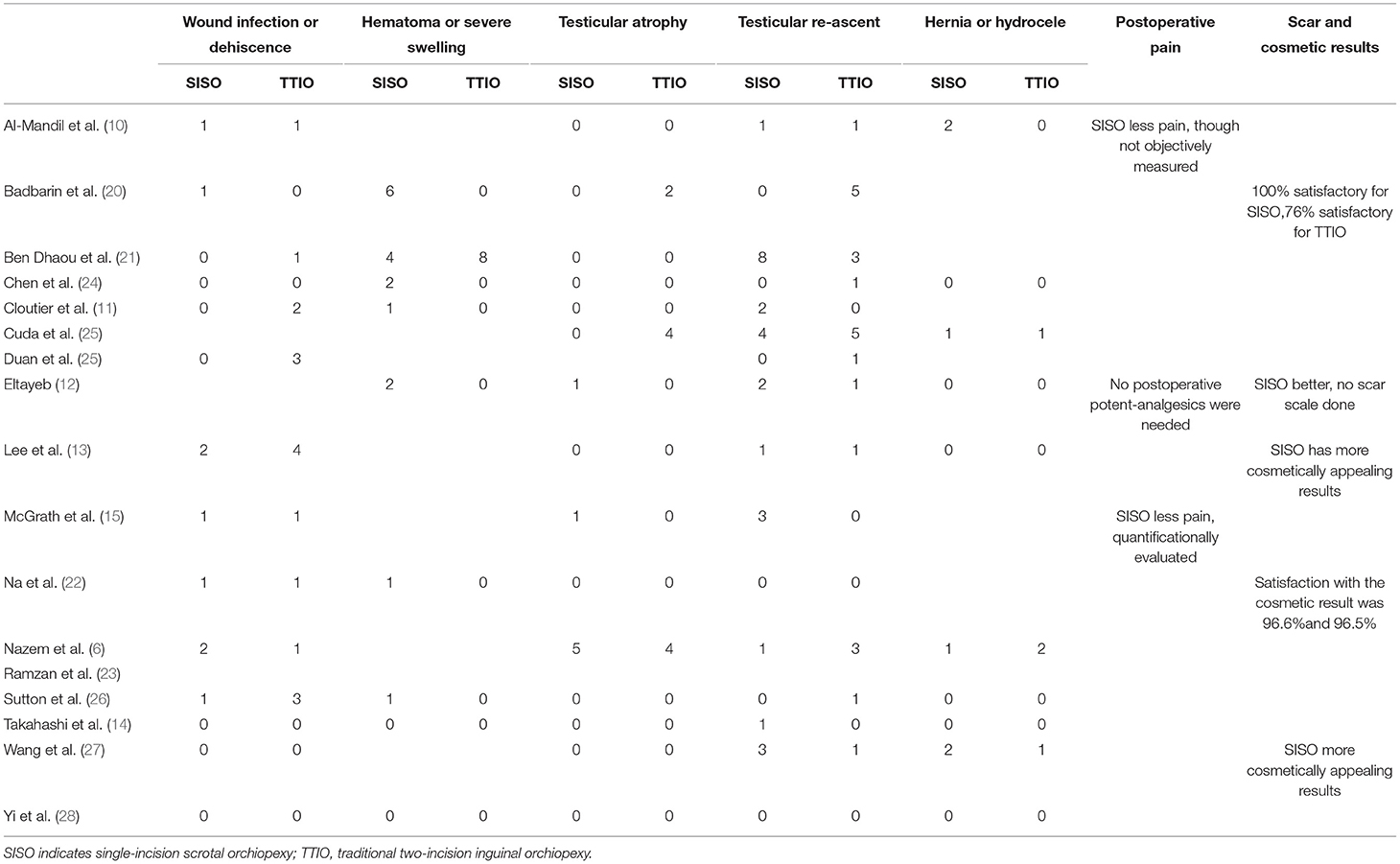
Table 3. The short-term and long-term exact complications, postoperative pain and cosmetic results in these two approaches for primary palpable undescended testes.
The quantitative star NOS scores for retrospective case–control studies ranged from 4 to 6, indicating low to moderate quality (Supplementary Table 1). The Jadad score scale for seven randomized controlled studies ranged from 2 to 5, whereas only two of seven was assessed as high quality (with a score of 3 or 5). Among these seven studies, withdrawals were well-adopted, and the randomization and double-blind method were still a big challenge. For some way, the double-blind method would be greatly restricted by the informed consent of participants and surgical strategy-designed trials.
Fourteen initial studies compared the operative time between SISO and TTIO for PUDT (6, 11–15, 20–24, 26, 27, 29). High heterogeneity (I2 = 97%) was observed, so the random effect model was used (19). Sensitivity analysis revealed that two studies contributed too much heterogeneity; these two studies were removed in the meta-analysis, although this removal would not affect the main results (6, 23). Our meta-analysis yielded that the SISO approach had a statistically significant shorter operative time than the TTIO approach for PUDT (WMD−11.96, 95% CI−14.33 to−9.59, I2 = 79%, P < 0.00001) (Figure 2A).
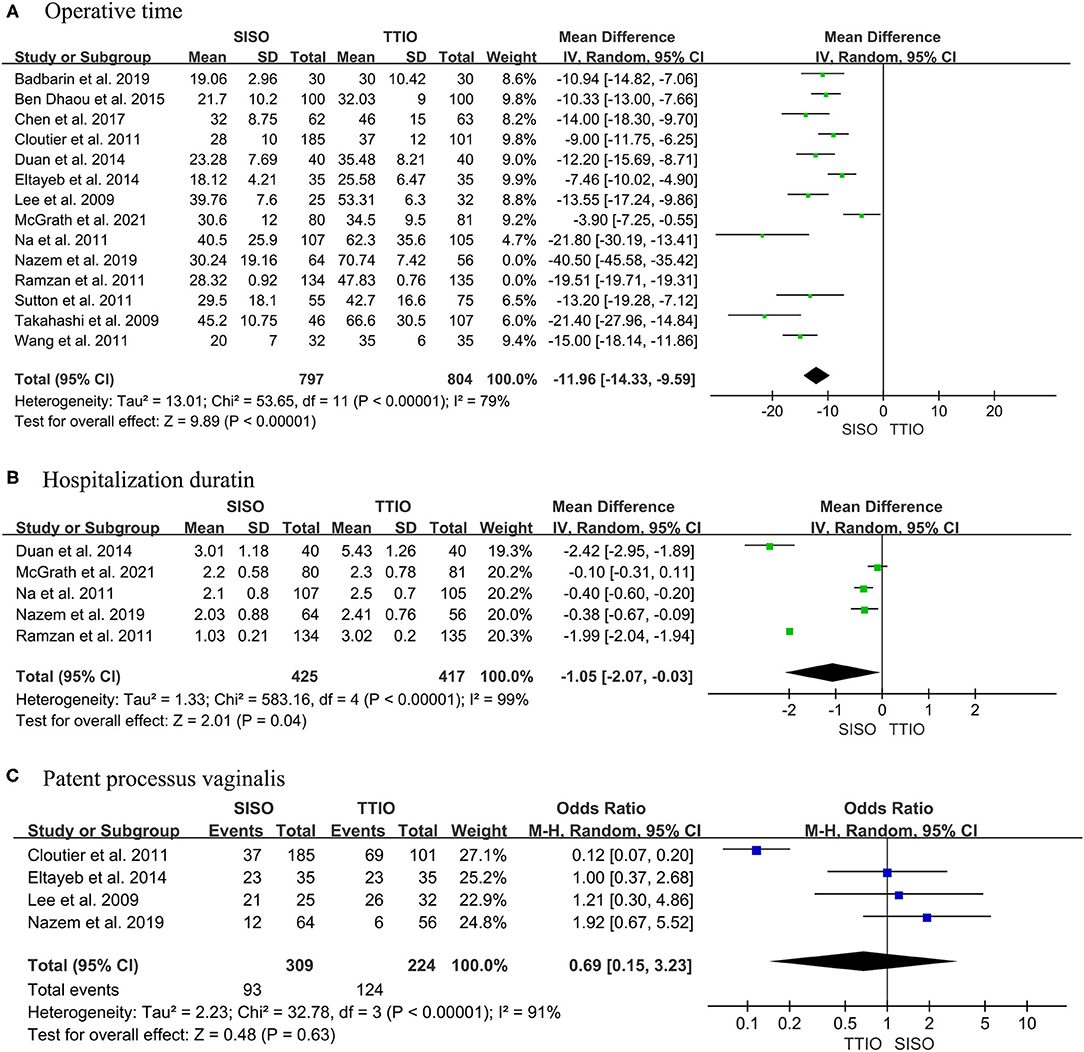
Figure 2. Forest plot of (A) operative time, (B) hospitalization duration, and (C) patent processus vaginalis between single-incision scrotal orchiopexy and traditional two-incision inguinal orchiopexy for primary palpable undescended testes.
Five studies reported hospitalization duration (6, 15, 22, 23, 29). The same high heterogeneity was observed, so the random effect was applied (I2 = 99%). Meta-analysis revealed that the SISO had a significantly shorter postoperative hospital duration compared with TTIO (WMD−1.05, 95% CI−2.07 to −0.03, P = 0.04) (Figure 2B).
The incidence of patent processus vaginalis was reported in four studies (6, 11–13). Our finding demonstrated no significant differences between these two surgical approaches, even with high heterogeneity between studies (OR 0.69, 95% CI 0.15 to 3.23, I2 = 91%, P = 0.63) (Figure 2C).
All of these include studies reported about complications. Generally, there were 73 (5.4%) total complications in SISO and 76 (6.0%) in the TTIO group. Although the results were comparable, our analysis demonstrated no significant differences between SISO and TTIO (OR 0.92, 95% CI 0.66 to 1.28, I2 = 13%, P = 0.60) (Table 3, Figure 3).
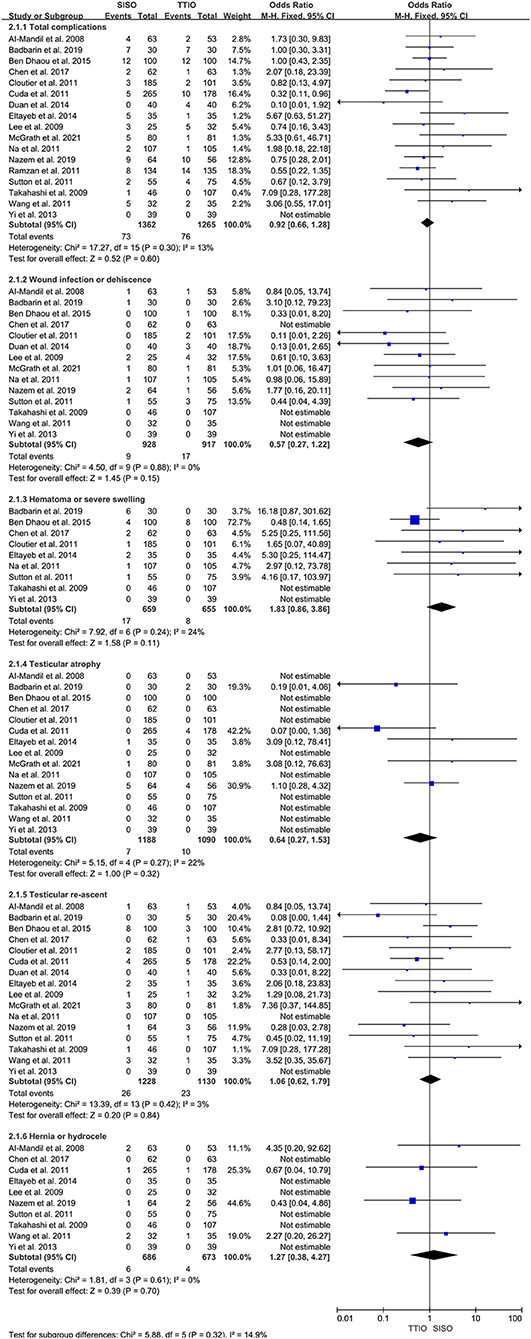
Figure 3. Forest plot of total, short-term, and long-term complications between single-incision scrotal orchiopexy and traditional two-incision inguinal orchiopexy for primary palpable undescended testes.
Wound infection/dehiscence and scrotal hematoma/severe swelling were regarded as short-term complications. There were nine cases (1.0%) who suffered from wound infection or dehiscence in SISO and 17 cases (1.9%) in the TTIO group, whereas meta-analysis demonstrated no statistically significant difference (OR 0.57, 95% CI 0.27 to 1.22, I2 = 0%, P = 0.15). There were 17 cases (2.6%) who suffered from scrotal hematoma or severe swelling in SISO and 8 cases (1.2%) in the TTIO group; meta-analysis demonstrated no significant difference (OR 1.83, 95% CI 0.86 to 3.86, I2 = 24%, P = 0.11) (Figure 3).
Testicular atrophy, reascent, hydrocele, or hernia were regarded as long-term complications. There were 15, 16, and 10 studies that reported testicular atrophy, reascent, and hydrocele or hernia, respectively. In total, there were 7 cases (0.6%) who developed into testicular atrophy in SISO and 10 (0.9%) in the TTIO group; meta-analysis revealed no significant difference (OR 0.64, 95% CI 0.27 to 1.53, I2 = 22%, P = 0.32). Twenty-six cases (2.1%) and 23 cases (2.0%) were detected of testicular reascent in SISO and TTIO, respectively, the same, without statistically significant difference (OR 1.06, 95% CI 0.62 to 1.79, I2 = 3%, P = 0.84). Also, a total of 6 cases (0.9%) and 4 cases (0.6%) were detected of hernia or hydrocele during follow-up in SISO and TTIO, respectively, without significant difference (OR 1.27, 95% CI 0.38 to 4.27, I2 = 0%, P = 0.70) (Figure 3).
There was no evidence for high heterogeneity for complications was observed, be it short-term, long-term, or total, so the fixed effect model was applied.
All papers reported the conversion status of SISO to TTIO. Added in total, 49 cases (3.6%) needed an extra inguinal incision to assist dissection of the spermatic cord or high ligation of processus vaginalis, and the majority of these testes were intracanalicular. What is more, nine studies (52.9%) did not report the need for any conversion in their surgical practice (Table 2).
Three studies evaluated postoperative pain, whereas only one study quantitatively calculated analgesics intake and pain scale assessment (15). It could be concluded that both SISO and TTIO did not need many analgesics after an operation, and relatively speaking, SISO consumed less. There were five studies that evaluated scar and cosmetic appealing satisfactory of patients. All these studies had the same conclusion that SISO provided more cosmetically appealing results than TTIO (Table 3).
Our updated systematic review and meta-analysis combined the most evidence comparing SISO and TTIO for primary PUDT. We analyzed the differences in aspects of operative time, hospitalization duration, conversion rates, wound infection or dehiscence, scrotal hematoma or severe scrotal, testicular atrophy, reascent, hernia or hydrocele, postoperative analgesics needs, and cosmetic results between these two surgical approaches for PUDT. According to our meta-analysis, SISO had the advantages of shorter operative time and hospital stay, fewer analgesics needs, and better cosmetic appealing results, most importantly, in the meanwhile, did not increase the short-term and long-term complications rates. The total conversion rate of SISO was 3.6%, and the majority of which were intracanalicular. Taking all these evidence and practice into consideration, we recommend that SISO should be the first choice for primary PUDT, especially low palpable cryptorchidism.
Currently, SISO mainly contains a single high transverse stria scrotal incision and low trans-scrotal mid raphe orchiopexy (11, 30). There was also low transverse stria scrotal incision orchiopexy introduced (14). Both high transverse stria scrotal incision and low trans-scrotal mid raphe had shorter operation time than TTIO, and mid raphe incision showed shorter time than stria scrotal incision (P < 0.00001, Supplementary Figure 1). Transverse stria scrotal incision showed more total complications than TTIO (P = 0.03, Supplementary Figure 2); however, differences between mid raphe orchiopexy and TTIO did not reach significance. Intuitively, both surgical technologies have less incision to close, and the incisions are invisible, and this makes SISO have shorter operative time and better cosmetic results than TTIO, although this only concerns the exerted operation scars. In addition, SISO does not open the external oblique fascia and has less dissection and anatomical disruption of the inguinal region, which would undoubtedly account for less postoperative pain and shorter hospitalization duration (10).
The main worrisome trouble of SISO for undescended testes is the difficulty for dissection of the spermatic cord and high ligation of processus vaginalis or hernia sac. This is also why TTIO lasts so long while still classic in the history of orchiopexy for cryptorchidism and could be served as the rescue method for SISO. In contrast, in a recent study, Hyuga et al. concluded that ligation of the processus vaginalis is unnecessary when it is not widely patent (31). In our opinion, this conclusion still needs to be interpreted with great caution, and studies on this topic still have a long way to go.
SISO for treatment of primary, secondary, or even trapped testes can be well-tolerated (4). Furthermore, it was reported that a single-incision scrotal surgical procedure had been successfully applied to treat communicating hydroceles and indirect hernia, or even impalpable cryptorchidism (10, 32). This procedure has its own advantages superiority, and we do believe it would serve the urologists better in more aspects in the future. However, urologists and every surgeon must take their own learning experiences and familiarity with surgical strategy into the deep heart.
There are several surgical techniques to correct cryptorchidism. Cuda et al. reported their clinical experience that the rate of laparoscopic and scrotal orchiopexy increased, whereas the inguinal orchiopexy decreased (25). The laparoscopic technique gradually tends to have fewer incisions and even a single port, and the single practice trend is becoming more and more warrant in minimal invasive surgery (33). SISO meets the concept of being minimally invasive and the demands of patients; it is a safe, effective, promising, and potential surgical approach alternative to TTIO.
Our study still has some limitations that must be taken into consideration. Most importantly, high heterogeneity between studies should not be ignored. Secondly, the small sample size, low quality of the initial study, and different study designs would make the analysis somehow weaker. Third, it was impossible to match all participated children groups with age, body mass index, the accurate location of the testis, and anatomic variations. Fourth, publication bias was still a big limitation, although the funnel plot was evaluated to be acceptable. In addition, selection bias for choosing the techniques cannot really be addressed in these studies, i.e., inguinal orchiopexy for higher located testicles and single incision for the lower ones. For example, 52.9% (9/17) studies reported there was no need for conversion, whereas a randomized controlled study reported that the conversion rate of SISO was as high as 23.8% (15). Alyami et al. also pointed out that only 52.8% of surgeons used SISO for undescended testes, and there was a discrepancy in the reported advantages and success rate according to their investigation (34). Last but not least, testicle positions were not well-evaluated, and only in the low-inguinal undescended testis can the cremaster dissection be adequate for excellent results. On the contrary, the correction of the high-inguinal undescended testis may need high ligation of the processus vaginalis or hernia sac and more extended dissection of the spermatic cord until the level of the internal inguinal ring, and it can provoke more tissue damage compared with the opening of the external oblique fascia. Furthermore, we cannot randomly ignore the high incidence of ipsilateral and contralateral patent processus vaginalis or hernia, especially in lower positioned cryptorchid patients (35). Added in total, SISO should only be applied in highly selected cases. More well-designed, high-quality, large-scale, multicenter prospective trials are still needed to explain this.
SISO is a safe, effective, promising, and potential minimal invasive surgical approach for PUDT. Compared with TTIO, SISO has the advantages of shorter operative time, shorter hospitalization duration, less postoperative pain, better cosmetic appealing results, and not increasing short-term and long-term complications. SISO is an alternative to TTIO in selected cryptorchid patients, especially lower positioned ones.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
CY and SW conceived and designed the meta-analysis. CY and LK independently searched the electronic databases and independently extracted the data. CY led analysis and interpretation of data, drafted the manuscript, and revised content based on feedback. LK acted as the second reviewer. YH and LW assisted with the retrieval of database and acquisition of data. JZ and JL assisted with the interpretation of data and provided critical revision of drafts. TL, DH, and GW assisted with conception and design and provided critical revision of drafts. SW acted the role of the corresponding author, provided funding support, provided critical revision of drafts, and acted as the third (mediating) reviewer. All authors contributed to the article and approved the submitted version.
This study was supported by the National Natural Science Foundation of China (No. 81873828), the Scientific and Technological Research Program of Chongqing Municipal Education Commission (KJ1600229), the Postgraduate Scientific Research Innovation Project of Chongqing Medical University (CYB16105), and the Senior Medical Talents of Chongqing for Young and Middle-Aged.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2022.805579/full#supplementary-material
Supplementary Figure 1. The forest plot of comparison of operation time between high transverse stria single-incision scrotal orchiopexy and low trans-scrotal mid raphe single-incision orchiopexy and traditional two-incision inguinal orchiopexy.
Supplementary Figure 2. The forest plot of comparison of total complications between high transverse stria single-incision scrotal orchiopexy and low trans-scrotal mid raphe single-incision orchiopexy and traditional two-incision inguinal orchiopexy.
Supplementary Table 1. Quality assessment of included retrospective designed case control studies according to Newcastle–Ottawa Quality Assessment Scale (NOS), and randomized controlled trials according to Jadad Scale.
CI, confidence interval; OR, odds ratio; PUDTs, palpable undescended testes; SISO, single-incision scrotal orchiopexy; TTIO, traditional two-incision inguinal orchiopexy.
1. Braga LH, Lorenzo AJ, Romao RLP. Canadian urological association-pediatric urologists of Canada (CUA-PUC) guideline for the diagnosis, management, and followup of cryptorchidism. Can Urol Assoc J. (2017) 11:E251. doi: 10.5489/cuaj.4585
2. Levine H, Keinan-Boker L, Leiba A, Derazne E, Rais A, Kark JD. Paternal age and risk of testicular germ cell tumors: a cohort study of 1,000,000 men. Andrology. (2017) 5:1124. doi: 10.1111/andr.12422
3. Wang C, Wang Y, Chen X, Wei X, Chen F, Zhong M. Efficacy of single-stage and two-stage Fowler-Stephens laparoscopic orchidopexy in the treatment of intraabdominal high testis. Asian J Surg. (2017) 40:490. doi: 10.1016/j.asjsur.2016.11.008
4. Caruso A, Walsh R, Wolach J, Koyle MA. Single scrotal incision orchiopexy for the palpable undescended testicle. J Urol. (2000) 164:156. doi: 10.1016/S0022-5347(05)67485-X
5. Ritchey M, Bloom D. Modified dartos pouch orchiopexy. Urology. (1995) 45:136. doi: 10.1016/S0090-4295(95)97502-0
6. Nazem M, Hosseinpour M, Alghazali A. Trans-scrotal incision approach versus traditional trans-scrotal incision orchiopexy in children with cryptorchidism: a randomized trial study. Adv Biomed Res. (2019) 8:34. doi: 10.4103/abr.abr_26_19
7. Karaman I, Karaman A, Erdogan D, Çavuşoglu Y, Cavuşglu Y. The transscrotal approach for recurrent and iatrogenic undescended testes. Eur J Pediatr Surg. (2010) 20:267. doi: 10.1055/s-0030-1249048
8. Dayanç M, Kibar Y, Tahmaz L, Yildirim I, Peker A. Scrotal incision orchiopexy for undescended testis. Urology. (2004) 64:1216. doi: 10.1016/j.urology.2004.06.069
9. Lin J, Li D, Chen J, Lin L, Xu Y. Inguinal hernia repair by Bianchi incision in boys: a retrospective study. Pediatr Surg Int. (2018) 34:289. doi: 10.1007/s00383-017-4217-x
10. Al-Mandil M, Khoury AE, Ei-Hout Y, Kogon M, Dave S, Farhat W. Potential complications with the prescrotal approach for the palpable undescended testis? a comparison of single prescrotal incision to the traditional inguinal approach. Urol J. (2008) 180:686. doi: 10.1016/j.juro.2008.04.040
11. Cloutier J, Moore K, Nadeau G, Bolduc S. Modified scrotal (Bianchi) mid raphe single incision orchiopexy for low palpable undescended testis: early outcomes. J Urol. (2011) 185:1088. doi: 10.1016/j.juro.2010.10.039
12. Eltayeb AA. Single high scrotal incision orchidopexy for unilateral palpable testis: a randomised controlled study. Afr J Paediatr Surg. (2014) 11:143. doi: 10.4103/0189-6725.132808
13. Lee Hr, Lee YS, Kim HS, Lee JY, Kim JC, Koh JS. A Comparison between single scrotal incision orchiopexy and the inguinal approach in patients with palpable undescended testes distal to the external inguinal ring. Korean J Urol. (2009) 50:1133. doi: 10.4111/kju.2009.50.11.1133
14. Takahashi M, Kurokawa Y, Nakanishi R, Koizumi T, Yamaguchi K, Taue R, et al. Low transscrotal orchidopexy is a safe and effective approach for undescended testes distal to the external inguinal ring. Urol Int. (2009) 82:92. doi: 10.1159/000176033
15. McGrath M, Kim J, Farrokhyar F, Braga L. Randomized controlled trial of scrotal versus inguinal orchidopexy on postoperative pain. Urol J. (2021) 205:895. doi: 10.1097/JU.0000000000001379
16. Bassel Y, Scherz H, Kirsch A. Scrotal incision orchiopexy for undescended testes with or without a patent processus vaginalis. Urol J. (2007) 177:1516. doi: 10.1016/j.juro.2006.11.075
17. Feng S, Yang H, Li X, Yang J, Zhang J, Wang A, et al. Single scrotal incision orchiopexy versus the inguinal approach in children with palpable undescended testis: a systematic review and meta-analysis. Pediatr Surg Int. (2016) 32:989. doi: 10.1007/s00383-016-3956-4
18. Gurney J, Richiardi L, McGlynn K, Signal V, Sarfati D. Analgesia use during pregnancy and risk of cryptorchidism: a systematic review and meta-analysis. Hum Reprod. (2017) 32:1118. doi: 10.1093/humrep/dex047
19. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. (2003) 327:557. doi: 10.1136/bmj.327.7414.557
20. Badbarin D, Mousavi Toomatari SE, Aslanabadi S, Farhadi E, Akhavan Salamat S. A comparative study of single scrotal incision orchiopexy of children with palpable low-lying undescended testis with traditional inguinal method. Adv Pediatr Surg. (2019) 25:14. doi: 10.13029/aps.2019.25.1.14
21. Ben Dhaou M, Zouari M, Zitouni H, Jallouli M, Mhiri R. [Comparison of the inguinal and scrotal approaches for the treatment of cryptorchidism in children]. Prog Urol. (2015) 25:598. doi: 10.1016/j.purol.2015.05.005
22. Na SW, Kim SO, Hwang EC, Oh KJ, Jeong SI, Kang W, et al. Single scrotal incision orchiopexy for children with palpable low-lying undescended testis: early outcome of a prospective randomized controlled study. Korean J Urol. (2011) 52:637. doi: 10.4111/kju.2011.52.9.637
23. Ramzan M, Sheikh AH, Qureshi MA, Zubair M, Majid F. Single incision trans scrotal versus standard inguino-scrotal orchidopexy in children with palpable undescended testis: our experience from April 2007 to April 2010. Pak J Med Sci. (2012) 28:827.
24. Chen Y, Zhao JF, Wang FR, Li Y, Shi Z, Zhong HJ, et al. Single scrotal-incision orchidopexy without ligation of processus vaginalis for palpable undescended testis. Zhonghua Nan Ke Xue. (2017) 23:708–12.
25. Cuda SP, Srinivasan AK, Kalisvaart J, Kirsch AJ. Evolution of single practice trends in the surgical approach to the undescended testicle. J Urol. (2011) 185:2451. doi: 10.1016/j.juro.2011.01.010
26. Sutton PA, Greene OJ, Adamson L, Singh SJ. Scrotal fixation in the management of low undescended testes. J Indian Assoc Pediatr Surg. (2011) 16:142. doi: 10.4103/0971-9261.86871
27. Wang JJ, Tang DX, Wu DX, Tao C, Yang HJ. Single scrotal incision orchiopexy (Bianchi technique) for medium and low undescended testicle [In Chinese]. Chin J Pediatr Surg. (2011) 32:354.
28. Yi QJ, He DW, Bian ZD, Li XL, Liu JH, Liu F, et al. Comparison of single prescrotal incision and traditional inguinal orchiopexy [In Chinese]. Chin J Urol. (2013) 34:120.
29. Duan ZN, Lu ZH, Mo SB. Clinical effect observation of tran-scrotal dermatoglyph signle incision in the treatment of palpable cryptorchidism in children. China Mod Med. (2014) 21:180.
30. Ali MS, Khan N, Uddin MB, Hossain MS, Mushtabshirah L. High transverse scrotal incision orchiopexy for undescended testes. Mymensingh Med J. (2019) 28:542–46.
31. Hyuga T, Kawai S, Nakamura S, Kubo T, Nakai H. Long-term outcome of low scrotal approach orchiopexy without ligation of the processus vaginalis. J Urol. (2016) 196:542. doi: 10.1016/j.juro.2016.02.2962
32. Callewaert PR, Rahnama'i MS, Biallosterski BT, van Kerrebroeck PE. Scrotal approach to both palpable and impalpable undescended testes: should it become our first choice? Urology. (2010) 76:73. doi: 10.1016/j.urology.2009.09.096
33. Ma Y, Cai J, Li S, Wang W, Liu L. Single-port laparoscopic assisted transcrotal orchidopexy for palpable inguinal canalicular cryptorchidism accompany with indirect inguinal hernia. Front Pediatr. (2018) 6:293. doi: 10.3389/fped.2018.00293
34. Alyami FA, Bin Yahya AF, Albraidi HF, Almarek NA, Alkhalifa MA, Alhazmi H, et al. Utilization of scrotal orchidopexy for palpable undescended testes among surgeons. Urol Ann. (2018) 10:380. doi: 10.4103/UA.UA_54_18
Keywords: undescended testes, orchiopexy, single-incision, minimal invasive surgery, palpable undescended testes (PUDTs), single-incision scrotal orchiopexy (SISO), traditional two-incision inguinal orchiopexy (TTIO), children
Citation: Yu C, Hu Y, Wang L, Kang L, Zhao J, Lu J, Lin T, He D, Wu S and Wei G (2022) Comparison of Single-Incision Scrotal Orchiopexy and Traditional Two-Incision Inguinal Orchiopexy for Primary Palpable Undescended Testis in Children: A Systematic Review and Meta-Analysis. Front. Pediatr. 10:805579. doi: 10.3389/fped.2022.805579
Received: 30 October 2021; Accepted: 19 January 2022;
Published: 15 March 2022.
Edited by:
Marco Castagnetti, University Hospital of Padua, ItalyReviewed by:
Ana Ludy Lopes Mendes, Bambino Gesù Children's Hospital (IRCCS), ItalyCopyright © 2022 Yu, Hu, Wang, Kang, Zhao, Lu, Lin, He, Wu and Wei. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shengde Wu, c2hlbmdkZXd1QGhvc3BpdGFsLmNxbXUuZWR1LmNu
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.