- 1Division of Developmental Behavioral Pediatrics, Department of Pediatrics, Stanford University School of Medicine, Palo Alto, CA, United States
- 2Quantitative Science Unit, Department of Medicine, Stanford School of Medicine, Palo Alto, CA, United States
Objectives: To describe medication management of children diagnosed with anxiety and/or depression by primary care providers within a primary care network.
Study Design/Methods: We performed a retrospective cross-sectional analysis of electronic health record (EHR) structured data from all children seen at least twice in a 4-year observation period within a network of primary care clinics in Northern California. For children who had visit diagnoses of anxiety, depression, anxiety+depression or symptoms characteristic of these conditions, we analyzed the rates and types of medications prescribed. A logistic regression model considered patient variables for the combined sample.
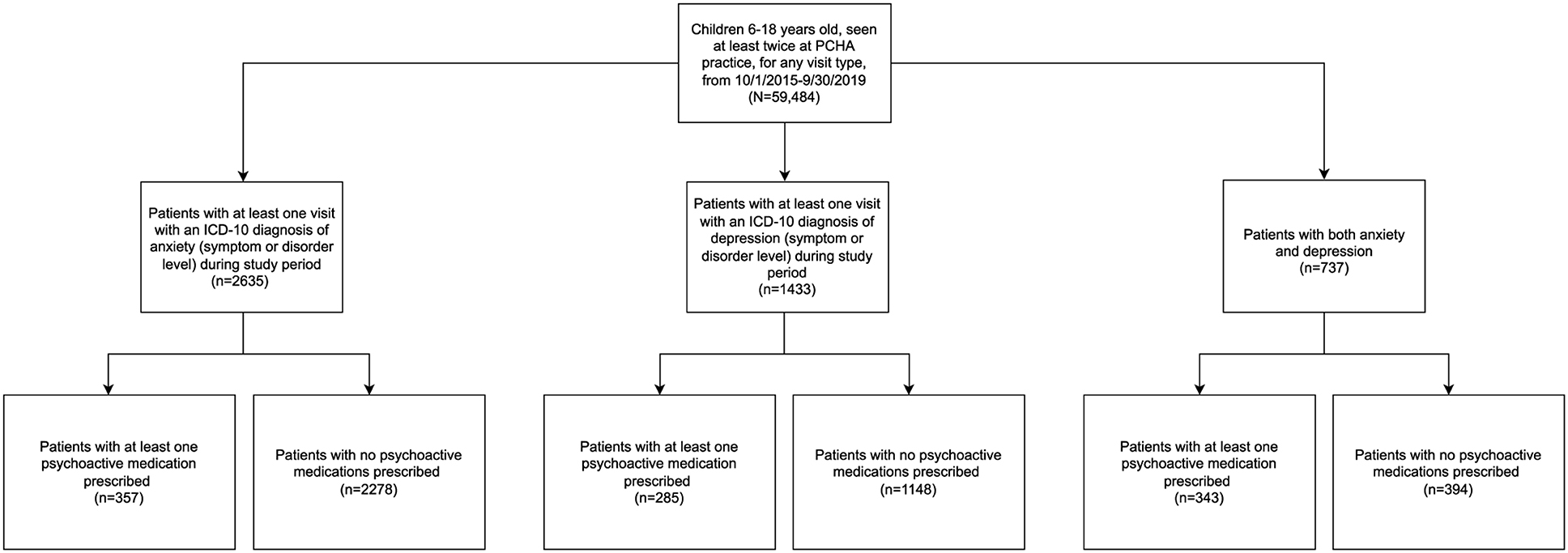
Results: Of all patients 6–18 years old (N = 59,484), 4.4% (n = 2,635) had a diagnosis of anxiety only, 2.4% (n = 1,433) depression only, and 1.2% (n = 737) both anxiety and depression (anxiety + depression); 18% of children with anxiety and/or depression had comorbid ADHD. A total of 15.0% with anxiety only (n = 357), 20.5% with depression only (n = 285), and 47.4% with anxiety+depression (n=343) were prescribed a psychoactive non-stimulant medication. For anxiety and depression only, the top three medications prescribed were sertraline, fluoxetine, and citalopram. For anxiety + depression, the top three medications prescribed were citalopram, sertraline, and escitalopram. Frequently prescribed medications also included benzodiazepines. Logistic regression modeling showed that the depression only and anxety + depression categories had increased likelihood of medication prescription. Older age and mental health comorbidities were independently associated with increased likelihood of medication prescription.
Conclusions: In this network, ~8% of children carried a diagnosis of anxiety and/or depression. Medication choices generally aligned with current recommendations with the exception of use of benzodiazepines.
Background
According to recent estimates, one in six children aged 6–17 have a treatable mental health disorder (1, 2). Among mental health disorders, depression and anxiety are common, and occur in 3 and 7% of pediatric patients, respectively, in the United States (3). The burden of anxiety and depression in the pediatric population has implications both during childhood and into adulthood (4). In childhood, anxiety disorders and depression are both associated with lower levels of academic achievement, social problems, and disruption in the home (5–7). Both anxiety and depression diagnoses are associated with increased risk of suicide, which is the second most common cause of death in children 10–19 years old (8). In adulthood, anxiety and depression can lead to decreased work productivity, relationship problems, and overall decreased quality of life. Mental health conditions also represent a significant financial burden on the US economy (9, 10). Evidence suggests that early and appropriate treatment of mental health disorders leads to better outcomes than non-treatment (11, 12). Studies suggest that many children with mental health conditions are not receiving adequate care (13). Increasing the use of evidence-based treatment of pediatric mental health conditions would be highly beneficial for both individuals and society.
Most children with anxiety and depression present first to a primary care provider (PCP) (2). Standard of care for childhood anxiety and depression is a multimodal approach, including pharmacological and non-pharmacological treatments. Current guidelines indicate that medication should be considered in moderate and severe cases (14–17). When medication is indicated for pediatric patients with anxiety or depression, the selective serotonin reuptake inhibitor (SSRI) class of medication has a substantial evidence base (14, 18, 19). Among the SSRIs, fluoxetine has the most evidence for good response for both anxiety and depression (18). For anxiety disorders, sertraline and fluvoxamine also have high-quality multisite studies demonstrating efficacy and safety in children (18, 19). For major depressive disorder, fluoxetine is FDA-approved for children, and fluoxetine and escitalopram both are approved for adolescents.
Pediatric patients may be prescribed psychoactive medications that lack evidence for use in the pediatric population (20). Benzodiazepines, once first-line medications for anxiety, are no longer considered first choice medications for general anxiety or panic disorder as a subtype of anxiety (15, 19). Benzodiazepine prescription for pediatric patients is decreasing over time, but they continue to be prescribed without approved indications (21). For example, Toce et al. found that only 24–33% of benzodiazepines prescriptions had an approved indication in adolescents and young adults (21). Knowledge about rates and types of psychotropic medication prescription would be valuable information to guide medical school education and pediatric training about pediatric mental health. Moreover, information about rates and types of medication prescription could serve as baseline information for quality improvement efforts to increase clinician engagement in evidence-based treatment.
A substantial barrier to the provision of adequate pediatric mental health care is the limited number of appropriately trained subspecialists, such as child psychiatrists and developmental-behavioral pediatricians (7, 13). Anderson et al. found that PCPs are the sole managers of 1/3 of children with mental health conditions (22). Given the high prevalence of mental health conditions, the engagement of primary care clinicians in treatment is of paramount importance. However, primary care clinicians frequently report inadequate training about mental health conditions and many remain reluctant to prescribe evidence-based treatments even when they either make the diagnosis or learn that the child was diagnosed by another subspecialty clinician (23–25). Prior studies investigating the role of primary care providers in managing patients with anxiety and depression have utilized provider report to assess comfort level and prescribing practices. Stein et al. surveyed pediatricians and found that 80% agreed that pediatricians should be able to identify conditions of attention-deficit/hyperactivity disorder, eating disorders, substance use, and behavior problems. Eighty-eight percentage agreed that pediatricians should be identifying depression, but only 25% felt pediatricians should be responsible for treating and managing depression (26). Response percentages were similar for pediatric anxiety. Another recent study found that 27% of PCPs do not prescribe psychiatric medications, and of the ones who do, 37% do not feel comfortable prescribing (27).
Surprisingly, few studies include objective data on the clinical care provided for children with anxiety and depression by PCPs (28). Therefore, information about what primary care clinicians actually do in practice (i.e., provider behavior) when caring for children with anxiety and depression, including rates of prescribing medication and types of medications used, is limited. The majority of existing studies include claims or survey data. Limitations of claims data include: incomplete, inaccurate, or missing data, and difficulty tracking specific providers (29, 30). One study of claims data on privately and commercially insured children showed that clinicians do not follow practice guidelines for recommended duration of treatment with antidepressant medications (31).
In this study, we used objective electronic health record data to describe the rates of medication management for children with anxiety and/or depression by pediatric PCPs and the types of medications prescribed in a large primary care network. We anticipated that even when primary care clinicians include depression or anxiety as a visit diagnosis, the rates of prescribing psychoactive medications would be low. We identified patient characteristics associated with prescription of medication to understand when primary care clinicians were willing to prescribe medication. We hypothesized that older age and higher number of comorbidities would be associated with likelihood to be prescribed medication for anxiety or depression. We conceptualize these data as providing a foundation for improving pediatric training and for conducting quality improvement activities in pediatric mental health.
Methods
Setting and Population
Packard Children's Healthcare Alliance (PCHA) is a community-based network of 25 primary care offices in Northern California, affiliated with Lucille Packard Children's Hospital and Stanford Children's Health. The Stanford University School of Medicine institutional review board (IRB) determined that this study was not human subjects research.
Study Design
We conducted a retrospective review of electronic health records for a cohort including all pediatric patients 6–18 years old seen at PCHA clinics for at least two visits during a 4-year study period (October 1, 2015 to September 30, 2019). Two visits were required within the study period in order to ensure that included patients were active within the network.
Data Sources
Deidentified structured data from all office encounters were included. Data from all practices were combined. Figure 1 shows the study cohort flow-chart. Patient data included age in years, sex, race, ethnicity, and medical insurance. Children under 6 years old were not included due to low rate of medication prescription (Supplementary Material 1).
Measures
Identifying Patients With Anxiety and Depression
Patients with anxiety and/or depression were identified based on the presence of at least one ICD-10 visit diagnosis code associated with anxiety or depression. Patients with these diagnoses were included, irrespective of pre-existing diagnoses. Both disorder-level codes (“F codes”, for example: “Generalized Anxiety Disorder”) and symptom-level codes (“R codes”, for example: “worries”) were included. See Supplementary Material 2 for a full list of ICD-10 codes used. Once selected for inclusion, patients were defined as an “anxiety patient” if they had only an anxiety diagnosis (with no depression), “depression patient” if they had only a depression diagnosis (with no anxiety) or “anxiety+depression patient” if they had both anxiety and depression diagnoses during the study period, although the two diagnoses were not required to be present at the same visit.
Defining Medication List
A list of all medications prescribed during the study period at visits with anxiety and/or depression diagnoses was reviewed, and a comprehensive list of psychoactive medications (excluding stimulants) was generated. Patients were defined as being prescribed medication if they had a prescription for any medication from this list associated with the encounter, including both initial prescriptions and refill prescriptions.
Defining Comorbidities
Behavioral and mental health comorbidities were identified based upon the presence of ICD-10 diagnosis codes associated with the following: Attention-deficit/hyperactivity disorder (ADHD), Sleep Disorders, Trauma and Stressor Related Disorders, Autism Spectrum Disorders (ASD), Obsessive Compulsive and Related Disorders, Feeding and Eating Disorders, Disruptive, Impulse Control, and Conduct Disorders, Substance-Related and Addictive Disorders, and Bipolar and Related Disorders. These disorders were chosen based on the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) (32). The comorbid diagnosis was not required to be present at the same visit as the anxiety and/or depression diagnosis.
Statistical Analyses
Descriptive Statistics
For patients with anxiety and/or depression, frequency counts, proportions, means and standard deviations were used to summarize data representing patient characteristics (demographics, comorbidities) and most commonly prescribed medications.
Regression Analysis
A logistic regression model including patients with anxiety, depression, and anxiety + depression was performed to determine association of patient characteristics with likelihood to be prescribed medication. Independent variables included: age group (6–12 and 13–18 years old), sex, insurance (private, public, military, or unknown), referral to developmental-behavioral pediatrics or psychiatry services within Stanford Children's Health, number of mental health and/or behavioral comorbidities (0, 1, or 2+), and primary diagnostic category (anxiety, depression, or anxiety + depression). Anxiety was selected as the reference group because it is the largest group and is the most prevalent condition across the included age range. We calculated adjusted odds ratios (aOR) and 95% confidence intervals (CI) from the regression model.
Since there was a high rate of missing race and ethnicity data in our cohort (~30%), race and ethnicity were not included in the regression model. Imputation was not attempted since missingness was highly dependent on practice/clinic.
Data cleaning and reformatting were performed using R version 3.6.2. Analyses were conducted using SPSS 26 and 27 and R Version 3.6.2 (33, 34). All statistical tests were two-sided and conducted at the 0.05 significance level.
Results
Patient Characteristics and Prevalence of Anxiety and/or Depression
Of 59,484 patients 6–18 years old seen at least twice during the study period for any reason, 4,498 (7.5%) had a diagnosis of anxiety and/or depression.
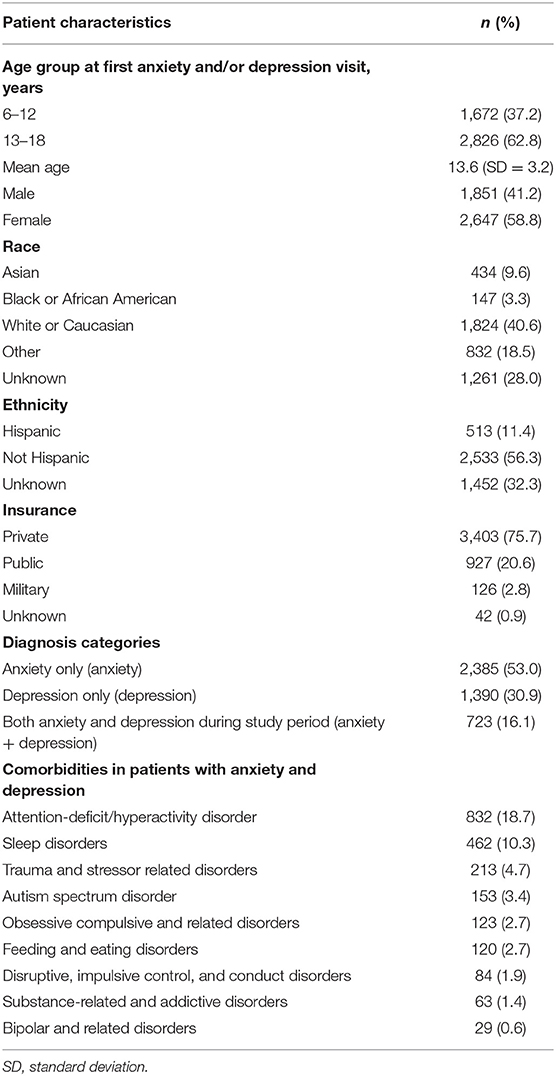
Of the 4,498, 41.2% were male, 40.6% were white, and 75.7% were privately insured. Table 1 describes characteristics of the 4,498 patients: 2,385 (53.0%) had at least one visit with a diagnosis of anxiety only (symptom or disorder level), n = 1,390 (30.9) had at least one visit with a diagnosis of depression only (symptom or disorder), and n = 723 (16.1%) had diagnoses of both anxiety and depression (anxiety + depression) (symptom or disorder).
Comorbid Behavioral and Mental Health Conditions in Patients With Anxiety and/or Depression
Table 1 also includes the most common comorbid behavioral and mental health disorders: Attention-deficit/hyperactivity disorder (18.7%), sleep disorders (10.3%), trauma and stressor-related disorders (4.7%) and autism spectrum disorder (3.4%). Eight hundred and fifteen (34.2%) of patients with anxiety, 466 (33.5%) of patients with depression, and 357 (49.4%) of patients with anxiety + depression, had one or more co-existing behavioral or mental health condition.
Medications for Patients With Anxiety and/or Depression
Of 2,385 patients with anxiety, 15.0% (n = 357) were prescribed a psychoactive (non-stimulant) medication. Of 1,390 children with depression, 20.5% (n = 285) were prescribed a psychoactive medication. Of 723 children with anxiety + depression diagnoses during the study period, 47.4% (n = 343) were prescribed a psychoactive medication.
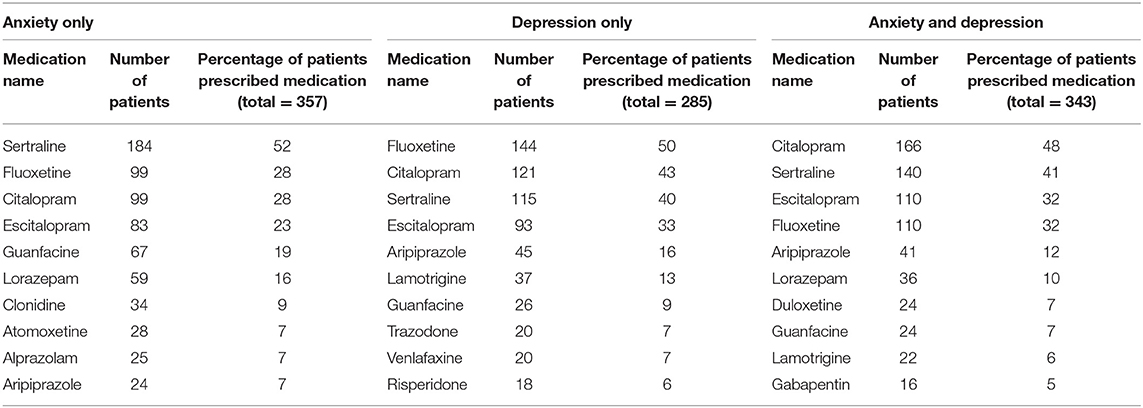
Table 2 shows the ten most commonly prescribed medications for each diagnosis. Most medications were in the class of serotonin reuptake inhibitors (SSRIs). For patients with anxiety, the top three prescribed medications were: (1) sertraline (prescribed to 52% of all anxiety patients who were prescribed medication during the study period) and (2) citalopram (28%) and fluoxetine (28%). For patients with depression, the top three prescribed medications were: (1) fluoxetine (50%), (2) citalopram (43%), and (3) sertraline (40%). For patients with anxiety + depression, the top three prescribed medications were: (1) citalopram (48%), (2) sertraline (41%), and (3) escitalopram (32%).
Two benzodiazepines appear on the list of ten most commonly prescribed medications for anxiety. Lorazepam was prescribed to 16.0% of patients and alprazolam was prescribed to 7.0% of patients. Lorazepam also appears on the list of ten most commonly prescribed medications for anxiety + depression (prescribed to 10% of patients). Benzodiazepines were not on the list of ten most commonly prescribed medications for depression.
Diagnoses Associated With Benzodiazepine Prescription
We collected the diagnostic codes most frequently associated with benzodiazepine prescription for patients with anxiety, depression, and anxiety + depression as a combined category. F41.9 (anxiety disorder), F32.9 (major depressive disorder), and F41.0 (panic disorder) were the top three anxiety and/or depression diagnostic codes associated with prescription. Z00.129 (encounter for routine child health examination), J02.9 (acute pharyngitis), and Z23 (encounter for immunizations) were the top three non-anxiety/depression diagnostic codes associated with benzodiazepine prescription.
Medications for Patients With Symptom-Level Diagnoses
For patients with anxiety, none of the 51 patients with symptom-level diagnoses only, such as “worries”, received medication. For patients with depression, only 1 of the 216 patients (<1.0%) with symptom-level diagnoses only, such as “sadness”, received medication. For patients with anxiety + depression, 0 of the 2 patients with symptom-level anxiety and depression received medication.
Predictors of Medication Prescription: Regression Model
A logistic regression model was performed to determine patient factors associated with likelihood to be prescribed medication for patients with anxiety and/or depression (Table 3). See Supplementary Material 3 for proportions of patients in each diagnostic category (i.e., anxiety, depression, anxiety + depression) who were prescribed medication. The model explained 15% of the variance (Nagelkerke R2) in medication prescription. Compared to 6–12 year old children, 13–18 year old children had 2.12 higher odds of being prescribed medication (95% CI: 1.78–2.53, p < 0.001). Compared to children with anxiety, children with depression had 1.26 higher odds of being prescribed medication (95% CI: 1.05–2.50, p = 0.01) and children with both anxiety and depression had 4.02 higher odds of being prescribed medication (95% CI: 3.31–4.88, p < 0.001). Compared to children without comorbidities, children with behavioral and mental health comorbidities were more likely to be prescribed medication (one comorbidity: aOR 1.78, 95% CI: 1.50–2.10, p < 0.001), (two or more comorbidities: aOR 2.94 95% CI: 2.30–3.75, p < 0.001).
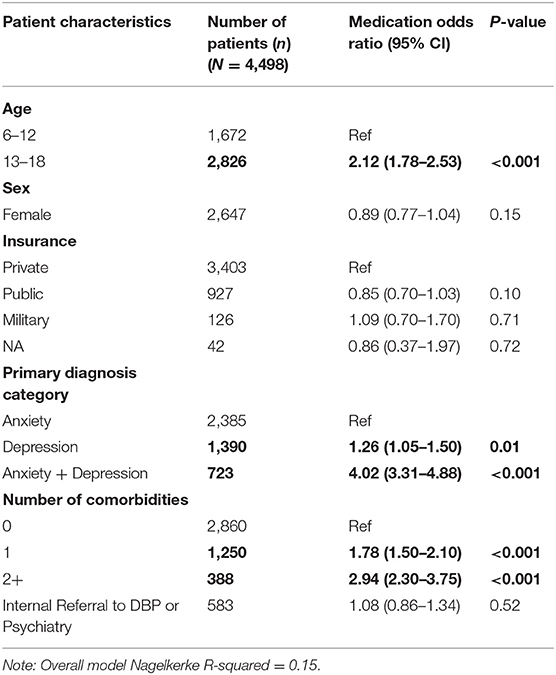
Table 3. Patient characteristics associated with medication prescription for patients with anxiety only, depression only, and both (anxiety/depression).
Patient sex, insurance type (private, public, military, or none/unknown), and referral to developmental-behavioral pediatrics and/or psychiatry within Stanford Children's Health were not associated with the likelihood of being prescribed medication.
Discussion
We found that, within this population of children in Northern CA, 7.5% of patients had a diagnosis of anxiety and/or depression recorded in their primary care electronic health record. Comorbid developmental, behavioral, and mental health conditions were common in all three subcohorts based on diagnostic group. 34.2% of patients with anxiety, 33.5% of patients with depression, and 49.4% of patients with anxiety + depression had one or more co-existing behavioral or mental health conditions. Psychoactive medications were prescribed to 15.0% of patients with anxiety, 20.5% with depression, and 47.4% of patients with anxiety + depression. This aligns with both prior claims data studies as well as provider survey studies which indicate that primary care providers play a major role in medication management for children with anxiety and depression (26, 35). We also found that patients very rarely received medication without a disorder-level ICD-10 code. This suggest that clinician behavior aligns with guideline recommendations that medication is not indicated in most mild cases of anxiety and depression (14, 15).
Current literature indicates that SSRIs have the most evidence of beneficial effect in pharmacological treatment of anxiety and depression in pediatric patients. Clinical practice guidelines and practice parameters also support the use SSRI medications; fluoxetine and escitalopram recommended as first line for depression (19). High quality, NIH-sponsored multisite trials have supported safety and efficacy of fluoxetine (19). In our study, patients with anxiety or with depression most commonly were prescribed sertraline, citalopram, and fluoxetine. For patients with anxiety+depression, citalopram, sertraline, and escitalopram most commonly were prescribed. These findings indicate that the medications most commonly used by PCPs for anxiety and depression generally align with current evidence.
We were surprised to find that a substantial proportion of patients who were prescribed medication during the study period were prescribed benzodiazepine medications at some point. Lorazepam appears on the list of most commonly prescribed medications for patients with anxiety only (16% of patients prescribed medication) and anxiety and depression (10% of patients prescribed medication). This finding aligns with other recent literature suggesting that benzodiazepines are commonly prescribed to pediatric patients despite limited evidence for beneficial effect in pediatric patients (18, 20, 36). There are also concerns about safety and the potential of diversion (37, 38). We wondered if benzodiazepines may be prescribed to children with anxiety and depression for other reasons, such as seizure disorders or procedural anxiolysis. We investigated the most common non-anxiety/depression related diagnostic codes associated with benzodiazepine prescription in patients with anxiety, depression, and anxiety + depression, and we found that they did not correlate with a clear non-psychiatric indication that would explain the use of benzodiazepines. Of note, panic disorder (which can be an indication for benzodiazepine use in some clinical scenarios) appears in the most common anxiety- and depression-related diagnostic codes. Further study is needed to understand the rationale for use of these medications by PCPs in this network. In particular, it would be important to determine if subspecialist involvement was associated with prescription of benzodiazepines in these pediatric patients.
We investigated patient factors associated with likelihood to be prescribed medication for patients with anxiety, depression, and anxiety + depression. The model accounted for 15% of the variance in medication use. Thus, it appears that other factors not assessed here are important to the decision to treat with medication. We also found that patients with depression alone and patients with anxiety + depression were more likely to be prescribed medication than patients with anxiety alone. Older age and higher number of comorbidities were associated with increased likelihood to be prescribed medication. Our findings align with a prior interview-based study, which have found that pediatricians are less likely to prescribe medication for anxiety than for depression, due to clinician perception that anxiety disorders are less impairing than depression (39). We speculate that primary care clinicians may be more comfortable identifying anxiety and depression as clear targets for treatment in older patients. We also wonder if the population of patients with both anxiety and depression represents a more clinically severe and/or complex population, where clinicians may perceive that medication is more justifiable. Further research in this area is warranted.
This study has several limitations. First, we were not able to consider the effects of referral to external psychiatry resources or referral to psychotherapy as this information was not captured in the electronic health record structured data. Second, a more thorough understanding of PCP recommendation of non-pharmacologic treatments to these children will require chart review. Although the primary care network from which our data was obtained is community-based, the patient demographics are not representative of demographics in California (our data set includes higher percentage white and private insurance), limiting the generalizability of the findings (40). Data from all practices was combined in the analysis. For that reason, we would not be able to discern prescribing differences at the practice level.
Conclusions
This study of a large community-based network of pediatrics practices showed that medications prescribed by primary care providers for anxiety and depression generally align with current recommendations. The most commonly used medications were SSRIs. Further study is needed to understand why providers use benzodiazepines, which have less evidence for beneficial effect, and more concern for side effects, diversion, and unintended recreational use. PCPs prescribe medications more frequently for patients with anxiety + depression than for patients with either diagnosis alone. Older age and higher number of comorbidities were associated with increased likelihood to be prescribed medication. Having depression only or anxiety + depression were both associated with increased likelihood to be prescribed medication relative to anxiety alone. Further study also is needed to investigate how PCPs collaborate with subspecialists in the care of patients with anxiety and depression.
Data Availability Statement
The data analyzed in this study is subject to the following licenses/restrictions: available with Stanford IRB and privacy office approval. Requests to access these datasets should be directed to aHVmZm1hbmxAc3RhbmZvcmQuZWR1 and eWJhbm5ldHRAc3RhbmZvcmQuZWR1.
Author Contributions
TL, YB, RG, HF, and LH contributed to conception and design of the study. RG completed initial data cleaning and organization. TL, RG, YB, and LH performed statistical analysis. TL wrote the first draft the manuscript. YB, RG, HF, and LH contributed to manuscript revision and read, and approved the submitted version.
Funding
Partial funding was provided by Developmental-Behavioral Pediatrics Fellowship Training from the Maternal Child Health Bureau of Health Resources and Services Administration T77MC09796.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
This manuscript appears as preprint on the MedRxiv Preprint Server indexed under the following doi: https://doi.org/10.1101/2021.04.11.21255276 (41).
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2022.794722/full#supplementary-material
References
1. Whitney DG, Peterson MD. US National and state-level prevalence of mental health disorders and disparities of mental health care use in children. JAMA Pediatr. (2019) 173:389–91. doi: 10.1001/jamapediatrics.2018.5399
2. Wissow LS, van Ginneken N, Chandna J, Rahman A. Integrating children's mental health into primary care. Pediatr Clin N Am. (2016) 63:97–113. doi: 10.1016/j.pcl.2015.08.005
3. Ghandour RM, Sherman LJ, Vladutiu CJ, Ali MM, Lynch SE, Bitsko RH, et al. Prevalence and treatment of depression, anxiety, and conduct problems in US children. J Pediatr. (2019) 206:256–67.e3. doi: 10.1016/j.jpeds.2018.09.021
4. Wolk CB, Beidas RS, Kendall PC. Cognitive-behavioral therapy for child anxiety confers long-term protection from suicidality. J Am Acad Child Adolesc Psychiatry. (2015) 54:175–9. doi: 10.1016/j.jaac.2014.12.004
5. Bittner A, Egger HL, Erkanli A, Jane Costello E, Foley DL, Angold A. What do childhood anxiety disorders predict? J Child Psychol Psychiatry. (2007) 48:1174–83. doi: 10.1111/j.1469-7610.2007.01812.x
6. Beesdo K, Knappe S, Pine DS. Anxiety and anxiety disorders in children and adolescents: developmental issues and implications for DSM-V. Psychiatr Clin N Am. (2009) 32:483–524. doi: 10.1016/j.psc.2009.06.002
7. Bitsko RH, Holbrook JR, Ghandour RM, Blumberg SJ, Visser SN, Perou R, et al. Epidemiology and impact of health care provider-diagnosed anxiety and depression among US children. J Dev Behav Pediatr JDBP. (2018) 39:395–403. doi: 10.1097/DBP.0000000000000571
8. Breslin K, Balaban J, Shubkin CD. Adolescent suicide: what can pediatricians do? Curr Opin Pediatr. (2020) 32:595–600. doi: 10.1097/MOP.0000000000000916
9. Davlasheridze M, Goetz SJ. Han Y. The effect of mental health on US County economic growth. Rev Reg Stud. (2018) 48:155–71. doi: 10.52324/001c.7997
10. Birnbaum HG, Kessler RC, Kelley D, Ben-Hamadi R, Joish VN, Greenberg PE. Employer burden of mild, moderate, and severe major depressive disorder: mental health services utilization and costs, and work performance. Depress Anxiety. (2010) 27:78–89. doi: 10.1002/da.20580
11. McGorry PD, Mei C. Early intervention in youth mental health: progress and future directions. Evid Based Ment Health. (2018) 21:182–4. doi: 10.1136/ebmental-2018-300060
12. Morgan AJ, Rapee RM, Bayer JK. Prevention and early intervention of anxiety problems in young children: a pilot evaluation of Cool Little Kids Online. Internet Interv. (2016) 4:105–12. doi: 10.1016/j.invent.2016.05.001
13. Kataoka SH, Zhang L, Wells KB. Unmet need for mental health care among US children: variation by ethnicity and insurance status. Am J Psychiatry. (2002) 159:1548–55. doi: 10.1176/appi.ajp.159.9.1548
14. Guidelines for Adolescent Depression in Primary Care (GLAD-PC): Part II. Treatment and Ongoing Management. American Academy of Pediatrics. Available online at: https://pediatrics.aappublications.org/content/141/3/e20174082 (accessed January 8, 2020).
15. Walter HJ, Bukstein OG, Abright AR, Keable H, Ramtekkar U, Ripperger-Suhler J, et al. Clinical practice guideline for the assessment and treatment of children and adolescents with anxiety disorders. J Am Acad Child Adolesc Psychiatry. (2020) 59:1107–24. doi: 10.1016/j.jaac.2020.05.005
16. Connolly SD, Bernstein GA. Practice parameter for the assessment and treatment of children and adolescents with anxiety disorders. J Am Acad Child Adolesc Psychiatry. (2007) 46:267–83. doi: 10.1097/01.chi.0000246070.23695.06
17. Birmaher B, Brent D. Practice parameter for the assessment and treatment of children and adolescents with depressive disorders. J Am Acad Child Adolesc Psychiatry. (2007) 46:1503–26. doi: 10.1097/chi.0b013e318145ae1c
18. Ipser JC, Stein DJ, Hawkridge S, Hoppe L. Pharmacotherapy for anxiety disorders in children and adolescents. Cochr Common Mental Disord. (2009) 2:1–88. doi: 10.1002/14651858.CD005170.pub2
19. Riddle MA. Pediatric Psychopharmacology for Primary Care. 2nd ed. Itasca, IL: American Academy of Pediatrics (2019).
20. Bushnell GA, Crystal S, Olfson M. Prescription benzodiazepine use in privately insured US children and adolescents. Am J Prev Med. (2019) 57:775–85. doi: 10.1016/j.amepre.2019.07.006
21. Toce MS, Michelson KA, Hudgins JD, Olson KL, Bourgeois FT. Trends in benzodiazepine prescribing for US adolescents and young adults from 2008 to 2019. JAMA Pediatr. (2021). doi: 10.1001/jamapediatrics.2021.5122. [Epub ahead of print].
22. Anderson LE, Chen ML, Perrin JM, Van Cleave J. Outpatient visits and medication prescribing for US children with mental health conditions. Pediatrics. (2015) 136:e1178–85. doi: 10.1542/peds.2015-0807
23. Walders N, Childs GE, Comer D, Kelleher KJ, Drotar D. Barriers to mental health referral from pediatric primary care settings. Am J Manag Care. (2003) 9:677–83.
24. Horwitz SM, Kelleher KJ, Stein RE, Storfer-Isser A, Youngstrom EA, Park ER, et al. Barriers to the identification and management of psychosocial problems: changes from 2004 to 2013. Acad Pediatr. (2015) 15:613–20. doi: 10.1016/j.acap.2015.08.006
25. Radovic A, Farris C, Reynolds K, Reis EC, Miller E, Stein BD. Primary care providers' initial treatment decisions and antidepressant prescribing for adolescent depression. J Dev Behav Pediatr. (2014) 35:28–37. doi: 10.1097/DBP.0000000000000008
26. Stein REK, Horwitz SM, Storfer-Isser A, Heneghan A, Olson L, Hoagwood KE. Do pediatricians think they are responsible for identification and management of child mental health problems? Results of the AAP periodic survey. Ambul Pediatr. (2008) 8:11–7. doi: 10.1016/j.ambp.2007.10.006
27. Rozenman M, Patarino KM. Pediatric anxiety in practice: a knowledge and needs assessment of pediatricians and nurses. J Dev Behav Pediatr. (2020) 41:605–11. doi: 10.1097/DBP.0000000000000821
28. Mayne SL, Ross ME, Song L, McCarn B, Steffes J, Liu W, et al. Variations in mental health diagnosis and prescribing across pediatric primary care practices. Pediatrics. (2016) 137:e20152974. doi: 10.1542/peds.2015-2974
29. Stein JD, Lum F, Lee PP, Rich WL, Coleman AL. Use of health care claims data to study patients with ophthalmologic conditions. Ophthalmology. (2014) 121:1134–41. doi: 10.1016/j.ophtha.2013.11.038
30. Tyree PT, Lind BK, Lafferty WE. Challenges of using medical insurance claims data for utilization analysis. Am J Med Qual. (2006) 21:269–75. doi: 10.1177/1062860606288774
31. Bushnell GA, Stürmer T, White A, Pate V, Swanson SA, Azrael D, et al. Predicting persistence to antidepressant treatment in administrative claims data: considering the influence of refill delays and prior persistence on other medications. J Affect Disord. (2016) 196:138–47. doi: 10.1016/j.jad.2016.02.012
32. American Psychiatric Association, American Psychiatric Association (eds). Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 5th ed. Washington, DC: American Psychiatric Association (2013).
34. R Core Team. R: A Language Environment for Statistical Computing. R Foundation for Statistical Computing. Vienna (2020). Available online at: https://www.R-project.org/. (accessed January 19, 2022).
35. Yang BK, Burcu M, Safer DJ, Trinkoff AM, Zito JM. Comparing nurse practitioner and physician prescribing of psychotropic medications for medicaid-insured youths. J Child Adolesc Psychopharmacol. (2018) 28:166–72. doi: 10.1089/cap.2017.0112
36. Hirschtritt ME, Olfson M, Kroenke K. Balancing the risks and benefits of benzodiazepines. JAMA. (2021) 325:347–8. doi: 10.1001/jama.2020.22106
37. Bushnell GA, Gerhard T, Crystal S, Olfson M. Benzodiazepine treatment and fracture risk in young persons with anxiety disorders. Pediatrics. (2020) 146. doi: 10.1542/peds.2019-3478
38. Friedrich JM, Sun C, Geng X, Calello DP, Gillam M, Medeiros KL, et al. Child and adolescent benzodiazepine exposure and overdose in the United States: 16 years of poison center data. Clin Toxicol Phila PA. (2020) 58:725–31. doi: 10.1080/15563650.2019.1674321
39. Tulisiak AK, Klein JA, Harris E, Luft MJ, Schroeder HK, Mossman SA, et al. Antidepressant prescribing by pediatricians: a mixed-methods analysis. Curr Probl Pediatr Adolesc Health Care. (2017) 47:15–24. doi: 10.1016/j.cppeds.2016.11.009
40. [Original Data Source]. www.Kidsdata.org, a Program of Population Reference Bureau. Available online at: https://www.kidsdata.org/ (accessed March 3, 2021).
Keywords: pediatric mental health, pediatric anxiety, pediatric depression, primary care pediatrics, electronic health records, health services research, developmental and behavioral pediatrics
Citation: Lester TR, Bannett Y, Gardner RM, Feldman HM and Huffman LC (2022) Medication Management of Anxiety and Depression by Primary Care Pediatrics Providers: A Retrospective Electronic Health Record Study. Front. Pediatr. 10:794722. doi: 10.3389/fped.2022.794722
Received: 14 October 2021; Accepted: 07 February 2022;
Published: 17 March 2022.
Edited by:
Kelly Kelleher, The Research Institute at Nationwide Children's Hospital, United StatesReviewed by:
Tea Rosic, McMaster University, CanadaLaura Chavez, Nationwide Children's Hospital, United States
Funlola Are, University of Texas Health Science Center at Houston, United States
Copyright © 2022 Lester, Bannett, Gardner, Feldman and Huffman. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lynne C. Huffman, aHVmZm1hbmxAc3RhbmZvcmQuZWR1
 Talia R. Lester
Talia R. Lester Yair Bannett
Yair Bannett Rebecca M. Gardner2
Rebecca M. Gardner2 Heidi M. Feldman
Heidi M. Feldman Lynne C. Huffman
Lynne C. Huffman