- Department of Pediatric Orthopedics, Children's Hospital of Fudan University, National Children's Medical Center, Shanghai, China
Objectives: Congenital malformation, trauma, tumor, or metabolic disease can cause length deformity of the radius or ulna, affecting the appearance and function of the forearm. Osteotomy and lengthening with external fixation can obviously improve the length of the radius and ulna (LRU). However, the extent of lengthening required is still unclear. This study analyzed the LRU in children, to provide suggested standards for various orthopedic treatments.
Methods: Normal LRUs were measured on X-ray images in children who came to hospital for emergency treatment, with measurements including anterior–posterior (AP) radiographs, lateral (LAT) radiographs, full LRU (total length), and LRU without the epiphysis (short length). Any cases of fracture or deformity affecting measurement were excluded. Three hundred twenty-six cases were divided into 16 groups according to age from 1 year old to 16 years old.
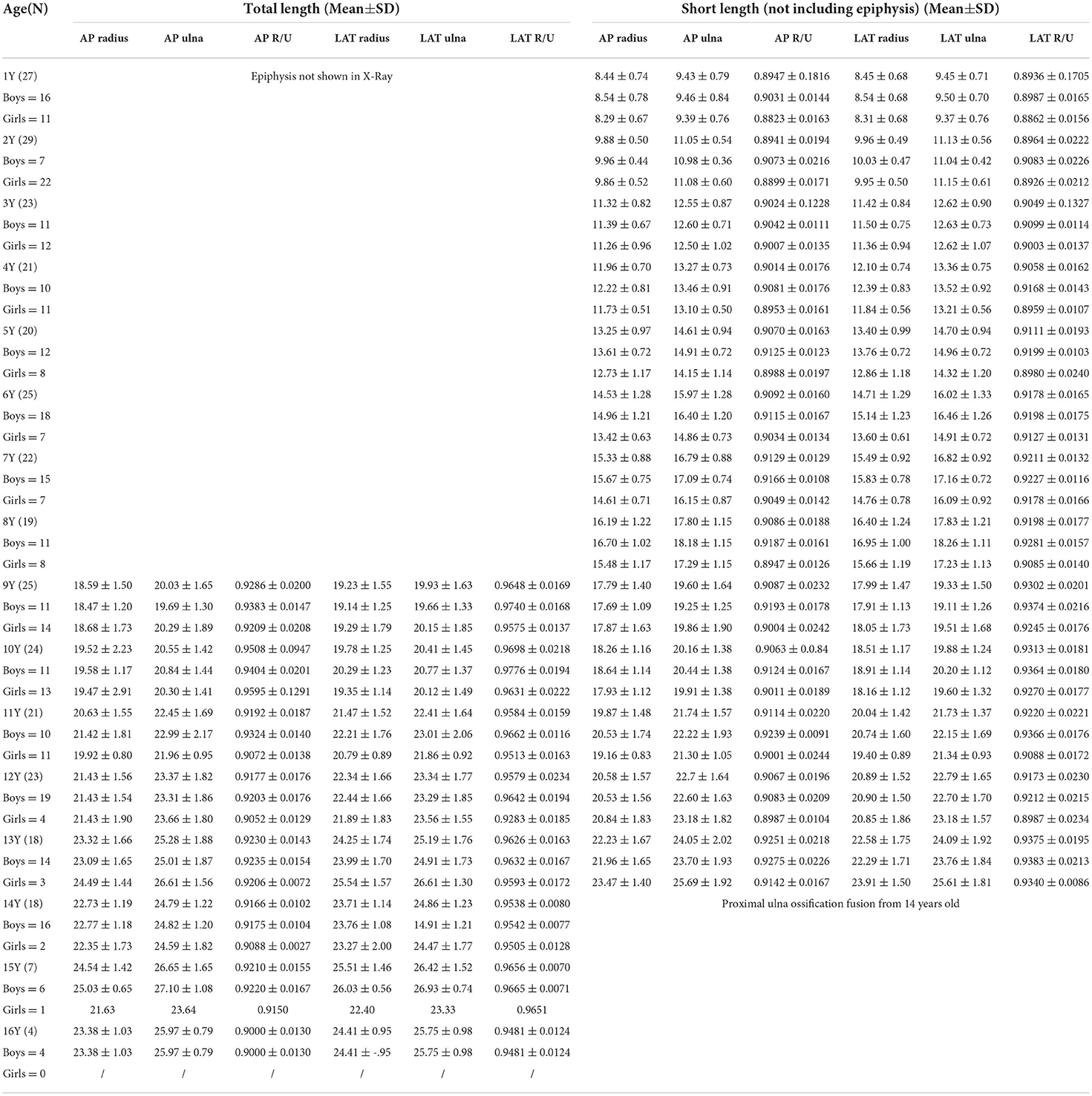
Results: The earliest epiphyseal plate and ossification center were observed in the distal part of the radius at 1 year old, and in the proximal part at 3 years old in both boys and girls. In the ulna, at the distal end it was 6 years old in girls and 7 years old in boys, while in the proximal part ossification was observed at 9 years old in both boys and girls. The proximal epiphyseal plate of the ulna began to close on X-ray images at 12 years old in girls and 13 years in boys. LRU increased with age, and there was a strong positive correlation and consistent ratio between radius, ulna and age. In short length, the ratio of the length of radius to ulna (RLRU) ranged from 0.8941 to 0.9251 AP, from 0.8936 to 0.9375 LAT. In total length, RLRU ranged from 0.9286 to 0.9508 AP, and 0.9579 to 0.9698 LAT.
Conclusions: The length and epiphyseal ossification of the radius and ulna are associated with age. RLRU is also limited to a certain range and tends to remain stable with age. These characteristics have clinical significance for deformity correction of the forearm.
Introduction
Congenital malformation, trauma, tumor, or metabolic disease can cause the radius or ulna to develop too long or too short in some children. Length deformities such as ulnar deviation or radial deviation, cubitus varus or valgus, limited pronation or supination affect the appearance and function of the forearm (1, 2). For deformity caused by differences in the lengths of the ulna and radius, the technique of osteotomy and limb lengthening can be used to correct the deformity by lengthening the short bone (3).
For example, multiple osteochondromas can cause limb deformities. In children with disability due to multiple osteochondromas, lengthening of the radius or ulna can also be used to restore the relationship of the radius to the ulna in the forearm. However, in clinical practice, there is no general agreement regarding the indications for surgery, and the long-term outcomes after surgery remain uncertain (4–10). Consequently, it is difficult to determine what length is considered excessive for limb lengthening. Excessive lengthening may lead to new problems, such as wrist pain, joint impact, or restricted joint function (3, 10, 11). Even if the outcome of the lengthening is as expected, with further growth of the radius or ulna, the affected bone may become relatively shorter again, causing the previous deformity to recur. Accurate knowledge of the expected length can avoid these problems. How to lengthen the affected bone to the ideal length, how to predict the final length and lengthen the affected bone to the target length in advance, and how to achieve optimal recovery with the fewest operations, are all questions which pediatric orthopedic surgeons must consider (12–15).
These treatments require an accurate understanding of the length and angle of the radius and ulna in their natural state. In addition, these demands are increasing. Many researchers have taken physical measurements on adult cadavers, or locally at the elbow, wrist, hand and other landmarks (16, 17). However, there have been few studies on the normal radius and ulna in children (18, 19).
Some studies have been carried out but are mainly based on body surface measurements. For example, Zhang et al. (20) measured the forearm length (body surface) of children aged from 3 to 5 years old, and Chen et al. (21) measured the arm span length or forearm ulnar length in children aged from 1 to 17 years old. Rasouli et al. (22) measured ulnar length using digital calipers to predict body height in children and adults aged 1 month to 23 years, while Edmond et al. (23) measured upper arm length, upper arm circumference, forearm length, and forearm circumference in children aged 0 to 17 years old.
However, the extent of lengthening required is still unclear. Is there a relationship between age and the length of the ulna or radius? Is there a ratio between the length of the ulna and radius? There has been a lack of comprehensive research into these questions. In this study we measured, analyzed and summarized the basic characteristics of the normal length and ratio of the radius and ulna in Chinese children, to provide background data which will help with various orthopedic surgeries.
Materials and methods
Inclusion criteria: anterior–posterior (AP) and lateral (LAT) radiographs of normal ulna and radius that were measured in the emergency department due to trauma. Patients were divided into 16 groups aged from 1 to 16 years old.
Exclusion criteria: fracture, malformation, neurodevelopmental disorder, and other abnormal images such as tumor, metabolic disease.
Two experienced pediatric orthopedic surgeons received training and measured the dimensions separately on X-rays, and the average of their measurements was taken. Measurements included total length of radius (TLR), total length of ulna (TLU), short length of radius (radius without epiphysis) (SLR), and short length of ulna (ulna without epiphysis) (SLU) on AP and LAT radiographs. The lengths of the midpoint line from the proximal part to the distal part were selected as TLR, SLR, SLU. Because the midpoint of the proximal part of the ulna is difficult to identify both on AP and LAT radiographs, TLU was measured based on the connecting line from the most prominent, nearest point at the proximal part of the ulna to the midpoint of the distal part of the ulna. Data were then analyzed according to age, gender, left/right, AP and LAT, TLR, TLU, SLR, SLU, and ratio of radius to ulna.
SPSS 17 statistical software (SPSS Inc., Chicago, IL, USA) was used for statistical analysis, one-way analysis of variance (ANOVA), reliability analysis, correlation analysis, and regression analysis. P < 0.05 indicated a significant difference.
Figure 1 is a graphical representation of the measurement of TLR, TLU, SLR, and SLU on AP and LAT radiographs.
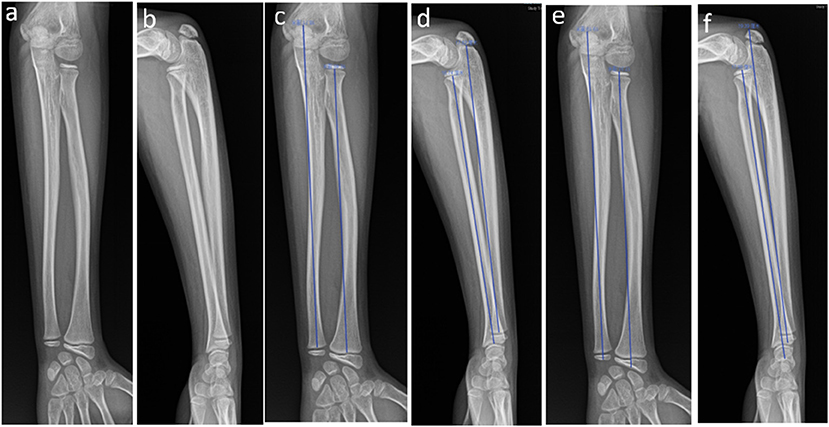
Figure 1. Anterior–posterior (AP) and lateral (LAT) radiographs of the left radius and ulna in a 10-year-old girl. (a) AP of the left forearm; (b) LAT of the left forearm; (c) AP showing measurement of the SLR and SLU; (d) LAT showing measurement of the SLR and SLU; (e) AP showing measurement of the TLR and TLU; (f) LAT showing measurement of the TLR and TLU.
Results
Data
A total of 326 subjects (192 boys and 134 girls, 173 left and 153 right) were enrolled in this study. Between 18 and 29 patients were enrolled in each age group ranging from 1 to 14 years old, 7 patients were in the 15 year-old group, and four in the 16 year-old group.
We assessed interobserver agreement using the intraclass correlation coefficient (ICC). Poor reliability was suggested for values between 0 and 0.20; fair reliability from 0.21 to 0.40; moderate reliability from 0.41 to 0.60; substantial or good reliability from 0.61 to 0.80, and almost perfect or very good reliability from 0.81 to 1.0 (24). The interobserver agreement was considered almost perfect, the ICC varied between 0.90 and 0.99 for all analyses.
Age of appearance and close of radial epiphyseal plate
Due to the characteristics of radius and ulna development in children, the epiphyseal plate and the ossification center appeared and closed at both ends of the radius and ulna at different ages. In this study, the age of appearance of the epiphyseal plate and ossification center at the distal and proximal parts of the radius and ulna were different, but there were also objective rules. In the development of the radius, the earliest epiphyseal plate and ossification center occurred in the distal part of the radius at 1 year old both in boys (3/15 boys, 20%) and girls (9/11 girls, 82%), in the radial head at 3 years old both in boys (3/11, 27%) and girls (2/12, 17%). In the development of the ulna, the earliest epiphyseal plate and ossification center appeared in the distal part of the ulna at 7 years old in boys (1/15, 7%), at 6 years old in girls (2/7, 29%), and in the proximal part at 9 years old both in boys (1/11, 9%) and girls (11/14, 79%). Fusion of the ossification center of the ulnar olecranon began at 13 years old in boys (9/15, 60%) and at 12 years old in girls (4/4, 100%) (Tables 1, 2).
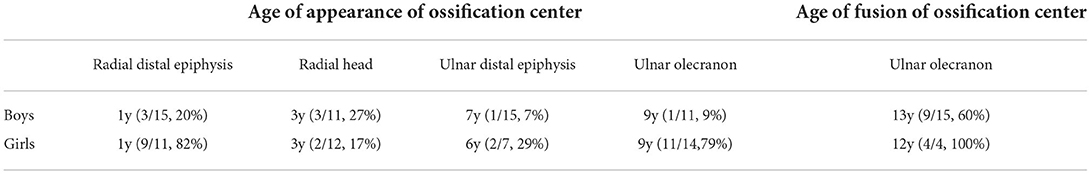
Table 1. Age (in years) of appearance and fusion of the forearm ossification centers for boys and girls.
Characteristics of the length and ratio of radius and ulna
Since epiphyseal plates and ossification centers do not develop at the proximal part of the ulna until 9 years of age, measurement of the TLU and TLR began at 9 years old and continued up to 16 years old. The epiphyseal plate began to close in some children from 14 years old, so because the SLU and SLR needed to exclude the epiphyseal plate and the ossification center, this was measured from 1 year old up to 13 years old.
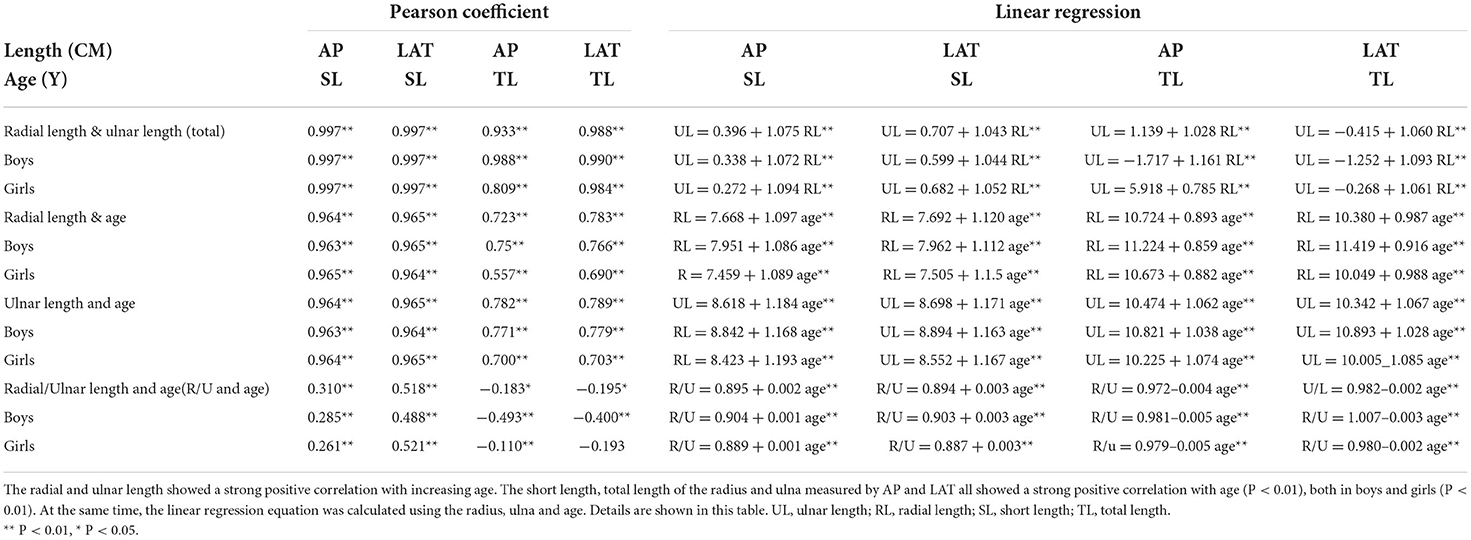
The lengths, and the ratio between the radius and ulna, differed according to age, as shown in Table 3.
The ulna and radius gradually become longer with age, as shown in Figures 2A–D, 3A–D.
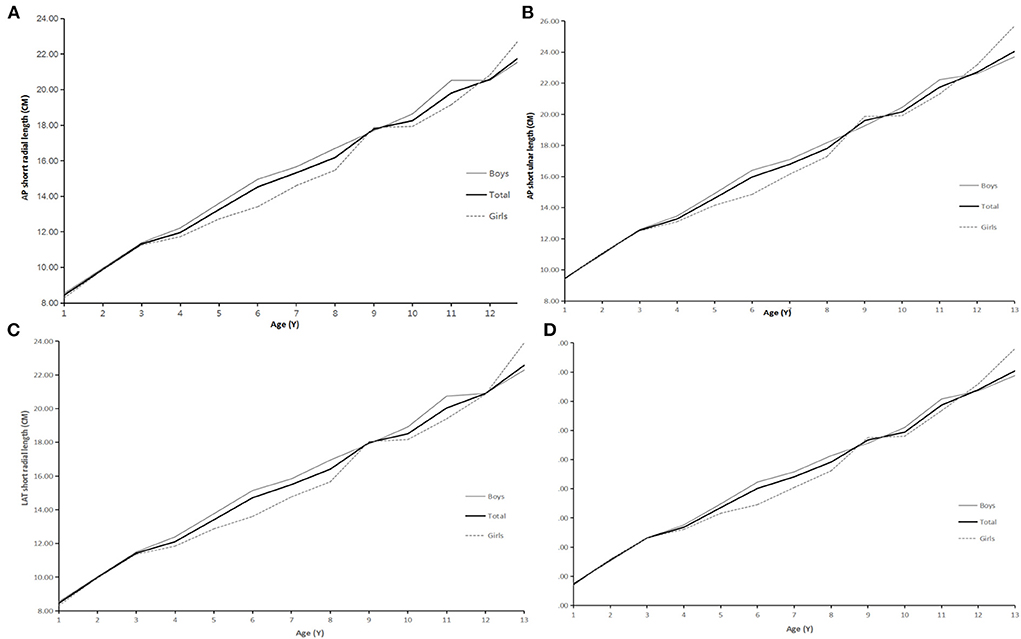
Figure 2. (A) AP short radial length and age. (B) AP short ulnar length and age. (C) LAT short radial length and age. (D) LAT short ulnar length and age.
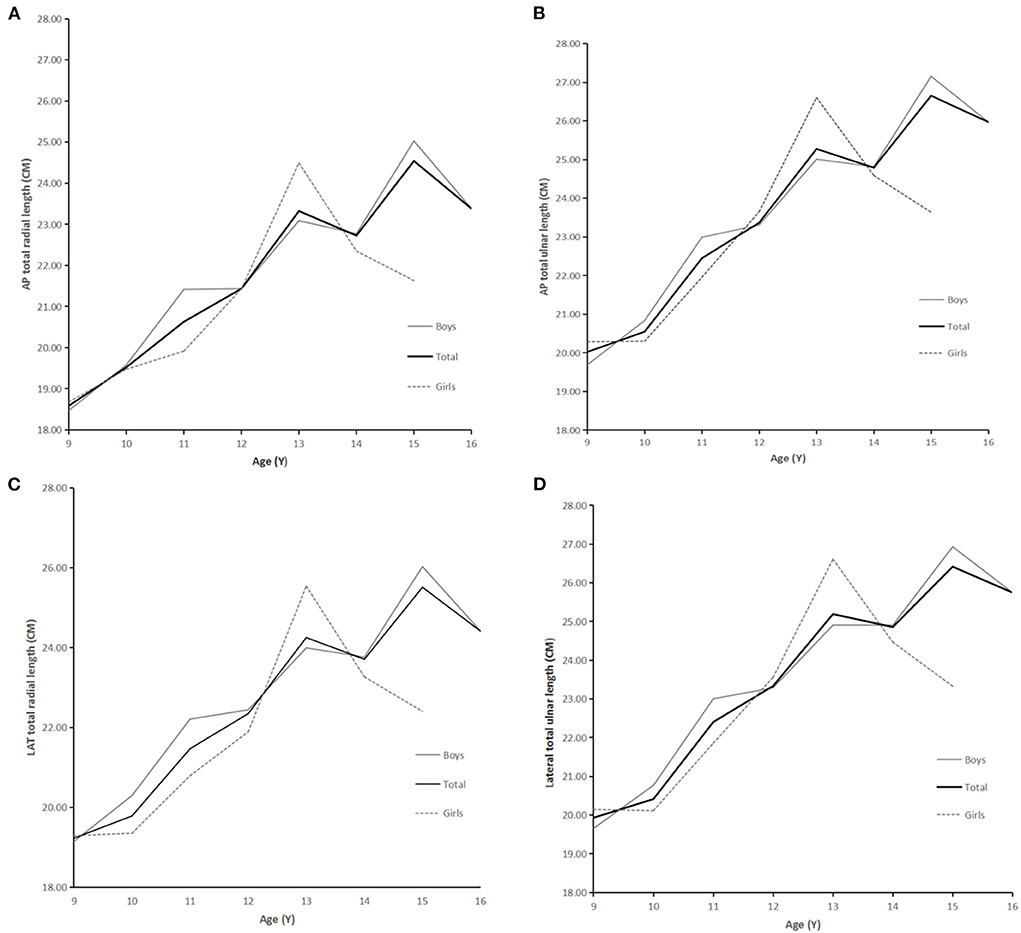
Figure 3. (A) AP total radial length and age. (B) AP total ulnar length and age. (C) LAT total radial length and age. (D) LAT total ulnar length and age.
The RLRU increased slightly with age, but remained stable and fluctuated only within a narrow range, whether measured by AP, LAT, short length, or total length. However, one-way analysis of variance (ANOVA) was conducted to evaluate the RLRU data in each age group, and the P values of homogeneity of variance test were all >0.05, indicating homogeneity of variance. On this basis, the LSD method was used to compare the RLRU of different age-groups under the four different measurements.
For short length measurement results (1–13 years old), there were significant differences between different ages (P < 0.01). Specifically, with the increase in age (1–13 years old), the radius/ulna ratio (short length) showed a gradually increasing but significant trend. From 1 to 4 years old, the radius/ulna ratio increased with age and became relatively stable after 5 years old. However, in both AP and LAT, short length ratios were from 0.89 to 0.94 (Figures 4A,B). There was no significant difference in the ratio of radius/ulna (total length) in AP and LAT in groups from 9 to13 years old (AP, P = 0.111; LAT, P = 0.21). Even with the slightly higher at 10 years old, the ratio remained stable. In the case of total length measured on AP radiographs, it was restricted to between 0.91 to 0.95, and in the cases of total length measured on LAT radiographs, it was restricted from 0.95 to 0.97 (Figures 5A,B).
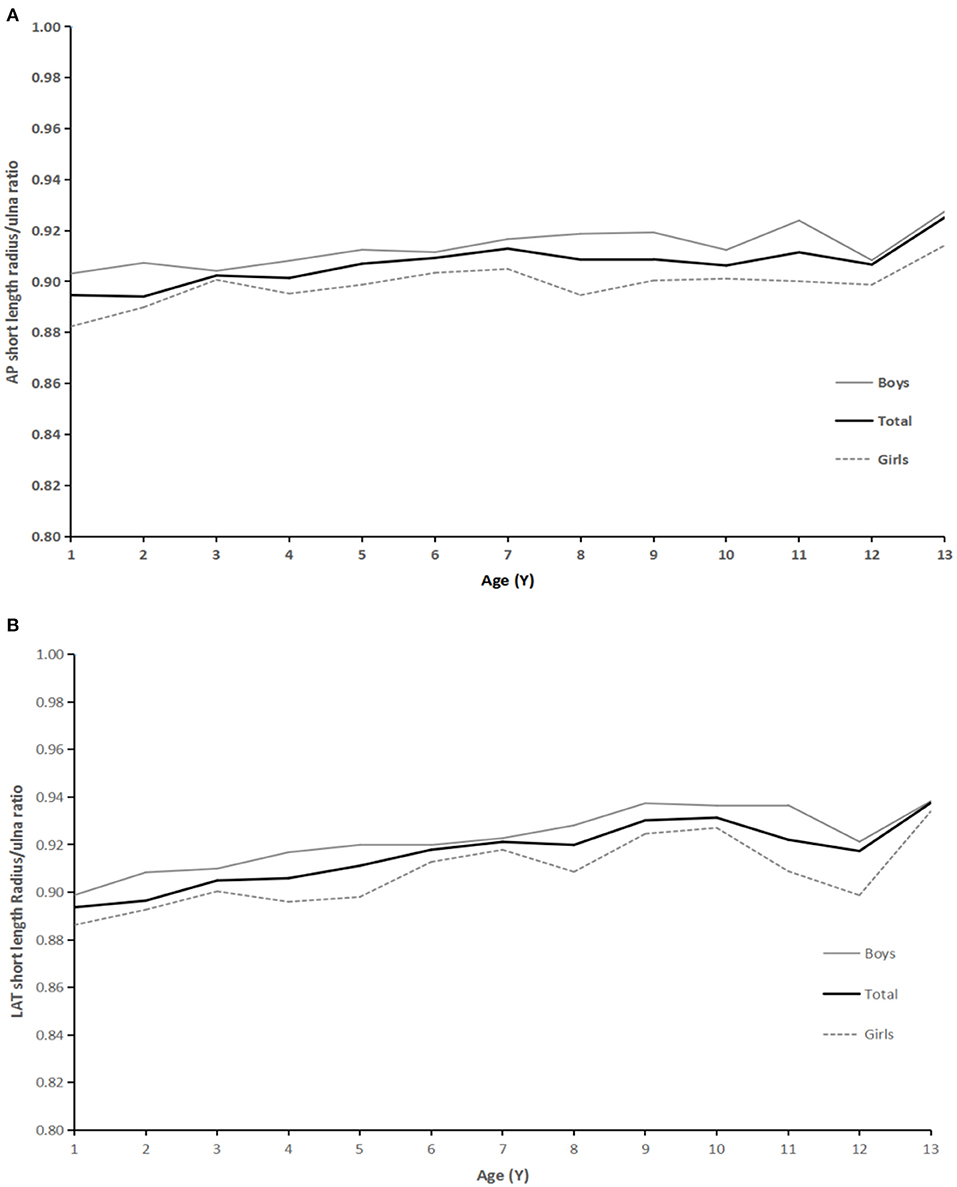
Figure 4. (A) AP radiographs: relationship between age and ratio of radius:ulna short length. (B) LAT: relationship between age and ratio of radius: ulna short length.
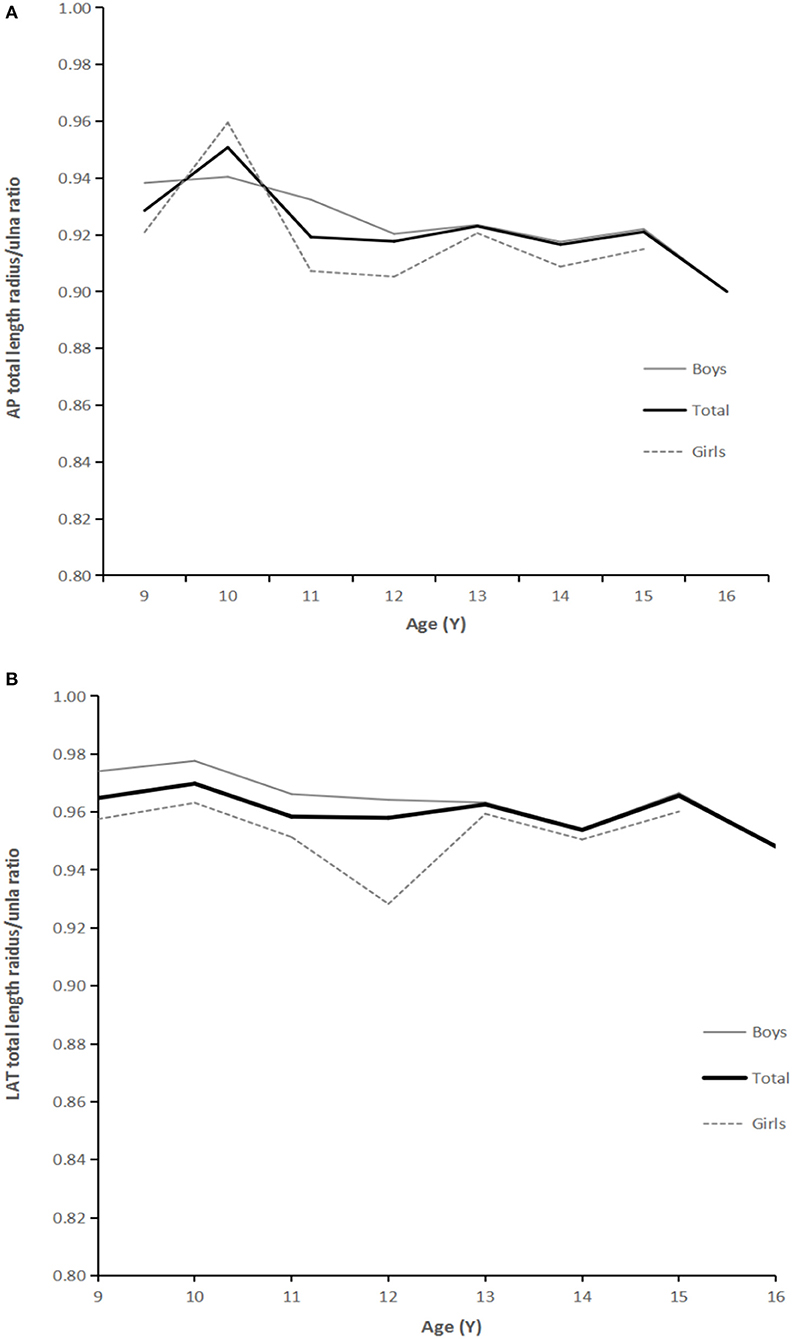
Figure 5. (A) AP radiographs: relationship between age and ratio of radius:ulna total length. (B) LAT: relationship between age and ratio of radius: ulna total length.
Discussion
There has been a lot of research on the lower limbs (25, 26), however there is a lack of research into the natural length and angle of the upper limbs. Upper limb diseases and disorders such as congenital anomalies, tumors and endocrine metabolic abnormalities can cause deformities of the radius and ulna. Currently, these deformities may be treated by lengthening the radius and/or ulna using the extension technique of osteotomy with external fixator, realizing the aim of correcting the deformity and thus restoring limb appearance and function (4–10).
For clinical surgical treatment, there is a lack of objective and accurate measurement data and analysis such as X-rays. The appearance and function of the forearm are compensated by the wrist joint, elbow joint, and shoulder joint. Thus, the need for the length and ratio of the ulna and radius to be corrected is not so urgent (16), and research into the length and ratio of the ulna and radius is lacking. In addition, ethical issues make it impossible to measure the lengths of the normal radius and ulna using X-rays. This study used normal radial and ulnar X-rays taken from children treated for trauma in the emergency department of our hospital, excluding fractures and other deformities of the forearm, thus the study was IRB approved, avoiding ethical problems.
In this study, the proximal and distal parts of the radius and ulna with or without epiphyseal plates and ossification centers were used for measurement; however a mixture of data with or without inclusion of the epiphyseal plate caused confusion, preventing us from making the right analysis and judgment. Therefore, we suggest the concepts of “short length” which excludes the proximal and distal epiphyseal plates of the radius and ulna, and “total length” which includes both the proximal and distal epiphyseal plates of the radius and ulna. Any length measurements which consisted of one end with the epiphyseal plate and the other end without the epiphyseal plate were not included in the statistical analysis.
The second aspect that needs to be addressed is measurement criteria. Since there are concepts such as anatomical axis and mechanical axis which are used in lower limb measurement, most measurements adopt the connection between the midpoint of the joints on both sides or the midpoint of the shaft (27), so ulna and radius measurement also refers to the method of connecting the midpoint at both ends of the ulna and radius. However, it is difficult to determine the midpoint at the proximal end of the ulna when the “total length” is actually measured on AP and LAT radiographs, so the most prominent point at the proximal end of the ulna is used instead of the midpoint to improve the accuracy and repeatability of the measurements.
The epiphyses of the radius and ulna, as well as secondary ossification centers, appeared on X-rays at different times in different age groups. For example, the earliest appearance of epiphyseal plates and ossification centers at the distal end of the radius was at 1 year old, and at the proximal end was 3 years old. The earliest appearance of epiphyseal plates and ossification centers at the distal end of the ulna was 6 years old in girls and 7 years in boys, while at the proximal end it was 9 years old in both boys and girls. These observations were similar to others reported in the literature (24, 28–32).
The lengths of both the radius and ulna increase with age, but there is a strong correlation between length and age, and the corresponding linear regression equation can be calculated. These are important references for predicting the development of radial and ulnar length. Moreover, although the ratio of the length of the radius to that of the ulna increases slightly with age, it is basically maintained within a relatively stable and narrow range, especially in older adolescents. Thus, the ratio of the length of the radius to the ulna is basically kept constant and is not affected by age. These rules suggest that there is a corresponding ratio between the upper limbs, especially the ulna and radius of the forearm, and that this is closely related to age. Only by maintaining the corresponding relationship of these basic features can the structure remain a stable and functional moving complex.
Our study has revealed that there are rules regarding the length of the forearm, there may also be some rules regarding the angles of the forearm. It is possible to introduce the concepts of anatomical and mechanical axes as in lower extremity measurement, joint walking direction, different plane angle formation and bone osteotomy at the center of rotation of angulation (CORA). Rules regarding the angles of the forearm may help us to further implement accurate prediction and treatment for the correction of forearm and upper limb deformity numerically, and thus achieve the best treatment effect. If these characteristics are similar to those of the lower extremities, then for humans who walk on two lower limbs and have their upper limbs liberated to engage in complex activities, the correction of forearm deformity will be supported by more data. It is possible to achieve the ideal recovery state, the best correction of appearance deformity and functional recovery.
Because of the limited number of cases, these data are still speculative. With further research into the relationship between the length and ratio of the deformed radius and ulna, and the development and verification of upper limb deformity correction surgery, these questions may be answered. These will further promote progress in the treatment of upper limb deformity.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was retrospective, it was approved by Ethics Committee of Children's Hospital of Fudan University and individual consent for this retrospective analysis was waived.
Author contributions
CW: study design, performed measurements, cases collection, statistical analysis, and manuscript preparation. DW: study design, performed measurements, and manuscript preparation. YM: performed measurements, statistical analysis, and cases collection. ZZ: cases collection and performed measurements. BN: study design, performed measurements, manuscript preparation, supervision, validation, responsible for literature search, study design, and finalized the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by Science and Technology Commission of Shanghai Municipality (CN) (No. 20Y11912900), Medical Innovation Research Project of Science and Technology Innovation Action Plan of Shanghai Science and Technology Committee 2020, and Key Development Program of Children's Hospital of Fudan University (No. EK2022ZX03).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Abe M, Shirai H, Okamoto M, Onomura T. Lengthening of the forearm by callus distraction. J Hand Surg Br. (1996) 21:151–63. doi: 10.1016/S0266-7681(96)80090-8
2. Demir B, Gursu S, Ozturk K, Yildirim T, Konya MN, Er T. Single-stage treatment of complete dislocation of radial head and forearm deformity using distraction osteogenesis in pediatric patients having multiple cartilaginous exostosis. Arch Orthop Trauma Surg. (2011) 131:1195–201. doi: 10.1007/s00402-011-1261-1
3. Vogt B, Tretow HL, Daniilidis K, Wacker S, Buller TC, Henrichs MP, et al. Reconstruction of forearm deformity by distraction osteogenesis in children with relative shortening of the ulna due to multiple cartilaginous exostosis. J Pediatr Orthop. (2011) 31:393–401. doi: 10.1097/BPO.0b013e31821a5e27
4. Litzelmann E, Mazda K, Jehanno P, Brasher C, Pennegot GF, Ilharreborde B. Forearm deformities in hereditary multiple exostosis: clinical and functional results at maturity. J Pediatr Orthop. (2012)32:835–41. doi: 10.1097/BPO.0b013e3182694e40
5. D'Ambrosi R, Barbato A, Caldarini C, Biancardi E, Facchini RM. Gradual ulnar lengthening in children with multiple exostoses and radial head dislocation: results at skeletal maturity. J Child Orthop. (2016) 10:127–33. doi: 10.1007/s11832-016-0718-8
6. Ahmed AARY. Gradual ulnar lengthening by an Ilizarov ring fifixator for correction of Masada IIb forearm deformity without tumor excision in hereditary multiple exostosis: preliminary results. J Pediatr Orthop B. (2019) 28:67–72. doi: 10.1097/BPB.0000000000000514
7. Iba K, Hanaka M, Ozasa Y, Takahashi N, Kanaya K, Yamashita T. Treatment of forearm deformity with radial head dislocation because of multiple osteochondromas: a series of three cases treated by simple axis correction and distraction osteogenesis of the ulna. J Pediatr Orthop B. (2018) 27:315–21. doi: 10.1097/BPB.0000000000000453
8. El-Sobky TA, Samir S, Atiyya AN, Mahmoud S, Aly AS, Soliman R. Current paediatric orthopaedic practice in hereditary multiple osteochondromas of the forearm: a systematic review. SICOT J. (2018) 4:10. doi: 10.1051/sicotj/2018002
9. Song SH, Lee H, Youssef H, Oh SM, Park JH, Song HR. Modified Ilizarov technique for the treatment of forearm deformities in multiple cartilaginous exostoses: case series and literature review. J Hand Surg Eur. (2012) 38:288–96. doi: 10.1177/1753193412450651
10. Mader K, Gausepohl T, Pennig D. Shortening and deformity of radius and ulna in children: correction of axis and length by callus distraction. J Pediatr Orthop B. (2003) 12:183–91. doi: 10.1097/01202412-200305000-00003
11. Jo AR, Jung ST, Kim MS, Oh CS, Min BJ. An evaluation of forearm deformities in hereditary multiple exostoses: factors associated with radial head dislocation and comprehensive classifification. J Hand Surg Am. (2017) 42:292.e1–e8. doi: 10.1016/j.jhsa.2017.01.010
12. Pacififici M. Hereditary multiple exostoses: new insights into pathogenesis, clinical complications, and potential treatments. Curr Osteoporos Rep. (2017) 15:142–52. doi: 10.1007/s11914-017-0355-2
13. Hill RA, Ibrahim T, Mann HA, Siapkara A. Forearm lengthening by distraction osteogenesis in children: a report of 22 cases. J Bone Joint Surg Br. (2011) 93:1550–5. doi: 10.1302/0301-620X.93B11.27538
14. Stanton RP, Hansen MO. Function of the upper extremities in hereditary multiple exostoses. J Bone Joint Surg Am. (1996) 78:568–73. doi: 10.2106/00004623-199604000-00010
15. Arms DM, Strecker WB, Manske PR, Schoenecker PL. Management of forearm deformity in multiple hereditary osteochondromatosis. J Pediatr Orthop. (1997) 17:450–4. doi: 10.1097/01241398-199707000-00007
16. Noonan KJ, Levenda A, Snead J, Feinberg JR, Mih A. Evaluation of the forearm in untreated adult subjects with multiple hereditary osteochondromatosis. J Bone Joint Surg Am. (2002) 84:397–403. doi: 10.2106/00004623-200203000-00010
17. Ekblom AG, Dahlin LB, Rosberg HE, Wiig M, Werner M, Arner M. Hand function in adults with radial longitudinal deficiency. J Bone Joint Surg Am. (2014) 96:1178–1184. doi: 10.2106/JBJS.M.00815
18. Paley D, Gelman A, Shualy MB, Herzenberg JE. Multiplier method for limb-length prediction in the upper extremity. J Hand Surg Am. (2008) 33:385–91. doi: 10.1016/j.jhsa.2007.11.007
19. Maresh MM. Linear growth of long bones of extremities from infancy through adolescence; continuing studies. AMA Am J Dis Child. (1955) 89:725–42. doi: 10.1001/archpedi.1955.02050110865010
20. Zhang J, Yu CW, Zeng G, Jing XF, Meng DJ, Ceng QY. The bone growth and devlopment of preschool Children Aged 3~5 in Cheng Du. Chin J Med Guide. (2012) 14:2200–4.
21. Chen WY, Lin YT, Chen Y, Chen KC, Kuo BI, Tsao PC, et al. Reference equations for predicting standing height of children by using arm span or forearm length as an index. J Chin Med Assoc. (2018) 81:649–56. doi: 10.1016/j.jcma.2017.08.023
22. Rasouli MA, Newth CJL, Khemani RG, Ross PA. Predicting body height in a pediatric intensive care unit using ulnar length. Front Pediatr. (2018) 6:187. doi: 10.3389/fped.2018.00187
23. Edmond T, Laps A, Case AL, O'Hara N, Abzug JM. Normal ranges of upper extremity length, circumference, and rate of growth in the pediatric population. Hand (N Y). (2020) 15:713–21. doi: 10.1177/1558944718824706
24. Miyazaki CS, Maranho DA, Agnollitto PM. Nogueira-Barbosa MH. Study of secondary ossification centers of the elbow in the brazilian population. Acta Ortop Bras. (2017) 25:279–82. doi: 10.1590/1413-785220172506170954
25. Leiva-Gea A, Delgado-Rufino FB, Queipo-de-Llano A, Mariscal-Lara J, Lombardo-Torre M, Luna-González F. Staged upper and lower limb lengthening performing bilateral simultaneous surgery of the femur and tibia in achondroplastic patients. Arch Orthop Trauma Surg. (2020) 140:1665–76. doi: 10.1007/s00402-020-03360-3
26. Paley D. Extensive Limb Lengthening for Achondroplasia and Hypochondroplasia. Children (Basel). (2021) 8:540. doi: 10.3390/children8070540
27. Paley D. Principles of Deformity Correction. Verlag Berlin Heidelberg: Springer Press. (2002). p. 1–18.
28. Girdany BR, Golden R. Centers of ossification of the skeleton. Am J Roentgenol Radium Ther Nucl Med. (1952) 68:922–4.
29. Garn SM, Rohmann CG, Blumenthal T, Silverman FN. Ossification communalities of the hand and other body parts: Their implication to skeletal assessment. Am J Phys Anthropol. (1967) 27:75–82. doi: 10.1002/ajpa.1330270109
30. Cheng JC, Wing-Man K, Shen WY, Yurianto H, Xia G, Lau JT, et al. A new look at the sequential development of elbow-ossification centers in children. J Pediatr Orthop. (1998) 18:161–7. doi: 10.1097/01241398-199803000-00006
31. Patel B, Reed M, Patel S. Gender-specific pattern differences of the ossification centers in the pediatric elbow. Pediatr Radiol. (2009) 39:226–31. doi: 10.1007/s00247-008-1078-4
Keywords: children, radius, ulna, length, ratio, age, X-ray
Citation: Wu C, Wang D, Mo Y, Zhang Z and Ning B (2022) Characteristics of the length of the radius and ulna in children. Front. Pediatr. 10:737823. doi: 10.3389/fped.2022.737823
Received: 07 July 2021; Accepted: 15 July 2022;
Published: 09 August 2022.
Edited by:
Jason Pui Yin Cheung, The University of Hong Kong, Hong Kong SAR, ChinaReviewed by:
Annalisa Valore, Casa di cura Pederzoli, ItalyYoonhae Kwak, University of Ulsan, South Korea
Copyright © 2022 Wu, Wang, Mo, Zhang and Ning. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bo Ning, bmluZ2JvQGZ1ZGFuLmVkdS5jbg==
 Chunxing Wu
Chunxing Wu Dahui Wang
Dahui Wang Yueqiang Mo
Yueqiang Mo Zhiqiang Zhang
Zhiqiang Zhang Bo Ning
Bo Ning