
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
PERSPECTIVE article
Front. Pediatr. , 30 December 2022
Sec. Pediatric Surgery
Volume 10 - 2022 | https://doi.org/10.3389/fped.2022.1101184
This article is part of the Research Topic Congenital Craniofacial Deformities: Genetic and Clinical Aspects View all 11 articles
Objective: This brief research report aimed to evaluate the short-term efficacy of presurgical nasoalveolar molding (PNAM) therapy on the nasolabial morphology three dimensionally in patients with non-syndromic complete unilateral cleft lip and palate (UCLP).
Methods: Thirty-six patients with non-syndromic complete unilateral complete cleft lip and palate were enrolled retrospectively and categorized into 2 groups: 18 patients who had received PNAM treatment (PNAM group) and 18 age-matched patients who have not receive PNAM treatment (no PNAM group) from 2017 to 2021. The average starting age for PNAM therapy was 18.33 days, and the average PNAM treatment duration was 99.08 days. Twelve nasolabial parameters were measured to compare the postsurgical outcomes of two groups.
Results: In PNAM groups, cleft width, vertical distance between double Crista philtri and columellar deviation were reduced compared to that in no PNAM group. And nostril height was larger than that in no PNAM group. The differences between two groups were statistically significant (p < .05). There were no statistical differences in columellar length, nostril width and bi-alar width between two groups. However, the nostril width on cleft side in PNAM group was decreased by an average of 1.1 mm.
Conclusion: Our result indicated that PNAM therapy decreased cleft width and vertical distance between Crista philtri. It also increased nasal symmetry by decreasing columellar deviation, increasing nostril height.
The difficulties of primary surgical treatment for unilateral complete cleft lip (UCLP) are the discrepancies and displacement of the nasomaxillary morphology, such as wide cleft gap and the displacement of alveolar segments. Presurgical nasoalveolar molding (PNAM), established by Grayson et al. (1), is a non-surgical method of reducing cleft width, aligning the alveolar segments and deforming nasal lower lateral cartilages to minimize the severity of cleft deformity before primary unilateral cleft lip repair and palatoplasty and consequently improving surgical outcomes. In the past few decades, there have been many reports documented favorable efficacy of PNAM in decreasing cleft avelo (2–5).
Precise imaging of craniofacial malformation is a crucial precondition for UCLP patients' treatment. The introduction of three-dimensional (3D) measurements such as stereophotogrammetry (6–9) and 3D laser scanning (10–13), facilitates the recording and assessment of CLP patients’ dento-maxillofacial morphology compared to traditional direct anthropometric and two-dimensional measurement based on photographs. However, the 3D reconstruction of dento-maxillofacial profile might have distortion due to insufficient instrument precision, change in patient's facial expression and head movement etc. The profile deviation, stringent specification of the measuring device and high expense limit the promotion in clinical application. Another frequently used method is facial plaster casts. It is economic, accessible and guarantees the verisimilitude and accuracy of facial details. Therefore, the present study used dental plaster casts to quantify facial landmarks of infants with complete UCLP and retrospectively evaluate the short-term effect of PNAM therapy on nasolabial symmetry.
Patient data were retrieved from the electronic records of the department of cleft lip and palate at West China Hospital of Stomatology, Sichuan University. 18 complete UCLP patients (11 boys, 7 girls) aged 3 to 6 months who received PNAM from November 2017 to November 2021 were extracted for the study. Besides, 18 age-matched complete UCLP patients (10 boys, 8 girls) who didn't undergo any non-surgical treatment were enrolled as control group. The participants were selected for inclusion in the present study based on the following criteria: (1) infants with non-syndromic complete UCLP; (2) no other co-existing craniofacial malformations; (3) first consultation during the neonatal period, (4) written consent of one or both parents for any clinical-surgical practice.
The average age of the patients upon commencing PNAM therapy was 18.33 days (range 2 to 32 days), and the average therapy duration was 99.08 days (range 65 to 126 days). The procedure of PNAM therapy was basically in accordance with the Grayson's technique (1). There were two main differences: first, nasal stent was added to the dental plate when the patients adapted to it (The infant only spent 7–14 days to completely adapt to the nasal stent) and then the nasal stent was adjusted weekly; second, the PNAM appliance was fixed in position with denture adhesive. A horizontal tape (3M Steri strips-1/4 Inch) was placed at the base of nose, stretching the lip segments toward each other. Artificial skin was applied to each cheek to avoid skin irritation created by adhesive tape (Figure 1).
All impressions were taken from participated infants under general anesthesia and the casts were fabricated with dental plaster. The bases of the facial casts were trimmed and adjusted to make the planes of all casts identical. All casts were marked with computerized random numbers for the subsequent blinded measurement. All PNAM therapy and casts were accomplished by the same author (C.Y). The protocol for the current study was reviewed and approved by the Institutional Review Board of West China Hospital of Stomatology, Sichuan University (No. WCHSIRB-D-2016–084R1).
The facial anatomical landmarks were identified on each cast (Table 1). The horizontal reference line was constructed by connecting the endocanthion points (Enr-Enl). Clefts were standardized to the right side by “mirroring” the facial measurements of patients with left-sided clefts.
Twelve parameters were assessed to evaluate nasolabial symmetry: non-cleft/cleft lip height (Sal-Cphl; Sar-Cphr), non-cleft/cleft lip length (Cphl-Chl; Cphr-Chr), cleft width (Cphr-Cphr'), vertical distance between Crista philtri left and right (h), columellar deviation (CD), columellar length (Sn-C), non-cleft/cleft nostril width (Sn-sar;Sn-sal), cleft nostril height(H); bi-alar width(all-alr) (Figure 2).
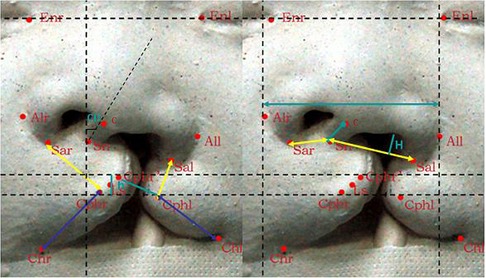
Figure 2. The horizontal reference line and facial anthropometric parameters. The horizontal reference line(Enr-Enl), non-cleft/cleft lip height (Sal-Cphl;Sar-Cphr),non-cleft/cleft lip length (Cphl-Chl;Cphr-Chr), cleft width (Cphr-Cphr’), vertical distance between double Crista philtri (h), columellar deviation (CD), columellar length (Sn-C), non-cleft/cleft nostril width (Sn-sar;Sn-sal), cleft nostril height(H); bi-alar width(All-Alr).
The casts were measured directly using the electronic vernier caliper and protractor. The measurements were completed and repeated the three times by a single operator (S.L) on three different occasions.
Numerical data are presented as means ± SDs. Paired t-test was performed to compare the outcomes of PNAM group and no PNAM group. The statistical analyse was performed using IBM SPSS Statistics 20.0 (IBM Corp., Armonk, NY, USA). The p value <0.05 was considered as statistical significance.
All results are shown in Table 2. The cleft width reduced significantly (p < 0.001), resulting in better approximated lips. The vertical distance between Crista philtri demonstrated significant decrease in PNAM group (p < 0.001). However, lip height and lip length on both sides were not significantly different. In the assessment of nasal morphology, the PNAM group showed significant improvement in columellar deviation (p < 0.001). Columellar length and nostril width on cleft and non-cleft side did not show significant difference between two groups (p = 0.167, p = 0.847 and p = 0.628 respectively). The mean value of columellar length of PNAM group was higher compared to no PNAM group. The mean value of nostril width on non-cleft side was almost identical between the two groups while the mean value of nostril width on cleft side in the PNAM group was decreased by an average of 1.1 mm compared to no PNAM group. The cleft nostril height was larger in PNAM group, and the difference between two groups was statistically significant (p < 0.001). The mean value of bi-alar width exhibited non-statistically significance between two groups.
The prime aim of presurgical treatment in patients with UCLP is rehabilitating the deformed dento-maxillofacial components to allow for better surgical outcomes and reduced need for secondary revisions (14, 15). The present study was conducted to assess the efficacy of PNAM on short-term nasolabial symmetry before primary UCLP repair and the results demonstrated improvement in cleft width, vertical distance between double Crista philtri, columellar deviation and nostril height on cleft side in PNAM-treated patients. The lip taping during PNAM therapy approximated the lip reduction cleft width segments, improved lip symmetry and centralized the columella. The nasal stent contributed to the significant increase of nostril height on cleft side by reshaping the collapse alar cartilage. The columellar length, nostril width on both sides and bi-alar width showed no statistical difference in the present study. Though the current study demonstrated that PNAM group had improved nasolabial outcomes after the procedure in comparison with no PNAM group and the short-term effectiveness has been corroborated by numerous studies (16, 17), the post-surgical outcomes and long-term sustenance of facial symmetry have yet to be determined (8, 18, 19).
In previous studies, the most commonly used method for facial morphological analyses is two-dimensional (2D) photography (2, 18, 20, 21). The 2D photography offers the benefits of non-invasive, simple and quick facial morphology capturing. However, the photographs provide limited information about the 3D anatomical structure (22). The technique of plaster cast measurements in the current study is an easily reproducible and safe method for recording and evaluation of CLP patients' 3D facial morphology. This method also has some drawbacks, including errors during manual measurement and needs for storage space. Other 3D measurements such as stereophotogrammetry and laser scanning have been reported to be employed in PNAM therapy to acquire digitalized patients’ dento-maxillofacial structures and customize templates (23–25). Nevertheless, the equipment was not available for many CLP centers. To further validate the efficacy of PNAM, studies with large sample size and long-term follow-up with the application of 3D analysis were highly recommended.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Institutional Review Board of West China Hospital of Stomatology, Sichuan University (No. WCHSIRBD-2016-084R1). Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin. Written informed consent was obtained from the individual(s), and minor(s)' legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article.
JY, SZ, NH and CY designed, wrote, and revised the manuscript. BS and QZ revised the manuscript. All authors contributed to the article and approved the submitted version.
This study was supported by the Research and Develop Program, West China Hospital of Stomatology, Sichuan University grant to HH (YF-4-202112).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Grayson BH, Santiago PE, Brecht LE, Cutting CB. Presurgical nasoalveolar molding in infants with cleft lip and palate. Cleft Palate Craniofac J. (1999) 36(6):486–98. doi: 10.1597/1545-1569_1999_036_0486_pnmiiw_2.3.co_2
2. Liang Z, Yao J, Chen PKT, Zheng C, Yang J. Effect of presurgical nasoalveolar molding on nasal symmetry in unilateral complete cleft lip/palate patients after primary cheiloplasty without concomitant nasal cartilage dissection: early childhood evaluation. Cleft Palate Craniofac J. (2018) 55(7):935–40. doi: 10.1597/14-296
3. Kinouchi N, Horiuchi S, Yasue A, Kuroda Y, Kawai N, Watanabe K, et al. Effectiveness of presurgical nasoalveolar molding therapy on unilateral cleft lip nasal deformity. Saudi Med J. (2018) 39(2):169–78. doi: 10.15537/smj.2018.2.21020
4. Attiguppe PR, Karuna YM, Yavagal C, Naik SV, Deepak BM, Maganti R, et al. Presurgical nasoalveolar molding: a boon to facilitate the surgical repair in infants with cleft lip and palate. Contemp Clin Dent. (2016) 7(4):569–73. doi: 10.4103/0976-237X.194104
5. Mandwe RS, Puri S, Shingane S, Pawar G, Kolhe VR, Alsi A. Presurgical nasoalveolar remodeling - an experience in the journey of cleft lip and palate. Clin Cosmet Investig Dent. (2015) 7:1–7. doi: 10.2147/CCIDE.S70823
6. Al-Rudainy D, Ju X, Stanton S, Mehendale FV, Ayoub A. Assessment of regional asymmetry of the face before and after surgical correction of unilateral cleft lip. J Craniomaxillofac Surg. (2018) 46(6):974–8. doi: 10.1016/j.jcms.2018.03.023
7. Rezende Pucciarelli MG, de Lima Toyoshima GH, Marchini Oliveira T, Marques Honorio H, Sforza C, Soares S. Assessment of dental arch stability after orthodontic treatment and oral rehabilitation in complete unilateral cleft lip and palate and non-clefts patients using 3D stereophotogrammetry. BMC Oral Health. (2020) 20(1):154. doi: 10.1186/s12903-020-01143-1
8. Mancini L, Gibson TL, Grayson BH, Flores RL, Staffenberg D, Shetye PR. Three-Dimensional soft tissue nasal changes after nasoalveolar molding and primary cheilorhinoplasty in infants with unilateral cleft lip and palate. Cleft Palate Craniofac J. (2019) 56(1):31–8. doi: 10.1177/1055665618771427
9. Kimura N, Nozoe E, Okawachi T, Ishihata K, Fuchigami T, Nakamura N. Three-dimensional analyses of nasolabial forms and upper lip surface symmetry after primary lip repair in patients with complete unilateral cleft lip and palate. J Cranio-Maxillofac Surg. (2019) 47(2):245–54. doi: 10.1016/j.jcms.2018.11.035
10. Zheng J, He H, Kuang W, Yuan W. Novel three-dimensional coordinate system to analyze alveolar molding effects of Pre-surgical nasoalveolar molding on infants with non-syndromic unilateral cleft lip and palate. J Craniofac Surg. (2020) 31(3):653–7. doi: 10.1097/SCS.0000000000006148
11. Fuchigami T, Kimura N, Kibe T, Tezuka M, Amir MS, Suga H, et al. Effects of pre-surgical nasoalveolar moulding on maxillary arch and nasal form in unilateral cleft lip and palate before lip surgery. Orthod Craniofac Res. (2017) 20(4):209–15. doi: 10.1111/ocr.12199
12. Fuchigami T, Kimura N, Tezuka M, Kibe T, Subhan Amir M, Tsujii T, et al. Comparison of short-term effects of presurgical nasoalveolar molding and Hotz's Plate on maxillary arch form in unilateral cleft lip and palate. J Oral Maxillofac Surg Med Pathol. (2019) 31(1):25–30. doi: 10.1016/j.ajoms.2018.08.008
13. Zhang M, Hattori M, Akiyama M, Elbashti ME, Liu R, Sumita YI. Three-dimensional evaluation of the dental arch in cleft lip and palate after prosthetic treatment. J Prosthodont Res. (2022). doi: 10.2186/jpr.JPR_D_21_00033
14. Rubin MS, Clouston S, Ahmed MM, Lowe KM, Shetye PR, Broder HL, et al. Assessment of presurgical clefts and predicted surgical outcome in patients treated with and without nasoalveolar molding. J Craniofac Surg. (2015) 26(1):75–9. doi: 10.1097/SCS.0000000000001233
15. Patel PA, Rubin MS, Clouston S, Lalezaradeh F, Brecht LE, Cutting CB, et al. Comparative study of early secondary nasal revisions and costs in patients with clefts treated with and without nasoalveolar molding. J Craniofac Surg. (2015) 26(4):1229–33. doi: 10.1097/SCS.0000000000001729
16. Zuhaib M, Bonanthaya K, Parmar R, Shetty PN, Sharma P. Presurgical nasoalveolar moulding in unilateral cleft lip and palate. Indian J Plast Surg. (2016) 49(1):42–52. doi: 10.4103/0970-0358.182235
17. Chou PY, Hallac RR, Ajiwe T, Xie XJ, Liao YF, Kane AA, et al. The role of nasoalveolar molding: a 3D prospective analysis. Sci Rep. (2017) 7(1):9901. doi: 10.1038/s41598-017-10435-6
18. Nayak T, Bonanthaya K, Parmar R, Shetty PN. Long-Term comparison of the aesthetic outcomes between nasoalveolar molding- and non-nasoalveolar molding-treated patients with unilateral cleft lip and palate. Plast Reconstr Surg. (2021) 148(5):775e–84e. doi: 10.1097/PRS.0000000000008463
19. Bhutiani N, Tripathi T, Verma M, Bhandari PS, Rai P. Assessment of treatment outcome of presurgical nasoalveolar molding in patients with cleft lip and palate and its postsurgical stability. Cleft Palate Craniofac J. (2020) 57(6):700–6. doi: 10.1177/1055665620906293
20. Zhang S, Yang C, Wu M, Yin J, Zeng N, Shi B, et al. Application of a novel nasal clip for nostril retention after primary unilateral cleft rhinoplasty. Cleft Palate Craniofac J. (2022) 10556656221083812. doi: 10.1177/10556656221083812
21. Zhang S, Wu M, Chen J, Yin J, Sakran KA, Wang Y, et al. The necessity of nostril retention application after secondary unilateral cleft rhinoplasty. Laryngoscope. (2022). doi: 10.1002/lary.30451
22. Shi B, Huang H. Computational technology for nasal cartilage-related clinical research and application. Int J Oral Sci. (2020) 12(1):21. doi: 10.1038/s41368-020-00089-y
23. Ahsanuddin S, Ahmed M, Slowikowski L, Heitzler J. Recent advances in nasoalveolar molding therapy using 3D technology. Craniomaxillofac Trauma Reconstr. (2021) 15(4):387–96. doi: 10.1177/19433875211044622
24. Nur Yilmaz RB, Germec Cakan D. Nasolabial morphology following nasoalveolar molding in infants with unilateral cleft lip and palate. J Craniofac Surg. (2018) 29(4):1012–6. doi: 10.1097/SCS.0000000000004427
Keywords: nasoalveolar molding (NAM), cleft lip and palate, anthropometry, nasal deformity, short time observation
Citation: Yin J, Zhang S, Huang N, Shi B, Zheng Q and Yang C (2022) Short-term surgical outcomes in patients with unilateral complete cleft lip and palate after presurgical nasoalveolar molding therapy: A three-dimensional anthropometric study. Front. Pediatr. 10:1101184. doi: 10.3389/fped.2022.1101184
Received: 17 November 2022; Accepted: 30 November 2022;
Published: 30 December 2022.
Edited by:
Juan Du, Capital Medical University, ChinaReviewed by:
Rui Li, First Affiliated Hospital of Zhengzhou University, China© 2022 Yin, Zhang, Huang, Shi, Zheng and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chao Yang Mjg2MTE3MzZAMTYzLmNvbQ==
Specialty Section: This article was submitted to Pediatric Surgery, a section of the journal Frontiers in Pediatrics
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.