- 1Pediatric Cardiology, Pediatric Heart Center, Department of Surgery, University Children's Hospital Zurich, Switzerland
- 2Children's Research Center, University Children's Hospital Zurich, Switzerland
- 3University of Zurich (UZH), Switzerland
- 4Child Development Center, University Children's Hospital Zurich, Switzerland
Background: Patients with hypoplastic left heart syndrome (HLHS) undergoing staged palliation until Fontan procedure are at risk for impaired neurodevelopmental (ND) outcome. The Hybrid procedure with bilateral pulmonary artery banding, ductal stenting, and balloon atrioseptostomy may offer a less invasive stage I procedure compared to the Norwood stage I procedure avoiding early neonatal cardiopulmonary bypass (CPB) surgery. Despite altered fetal cerebral hemodynamics, the type of stage I procedure may be a covariate influencing ND outcome and functional outcome may also be altered due to postponing neonatal CPB surgery. Within this review, we analyzed ND outcome as well as functional outcome after Hybrid procedure as stage I procedure.
Methods: The review analyzed original publications (OPs) published before March 15, 2022, identified by Cochrane, EMBASE, OVID, Scopus, and Web of science. An OP was included if short-to-long-term neurodevelopment outcome, brain development, somatic, and cardiac outcome in patients for HLHS and variants treated by Hybrid procedure were analyzed. In addition to database searches, we reviewed all references of the analyzed OP to obtain a comprehensive list of available studies. The author, year of publication, demographic characteristics of study population, study design (prospective or retrospective), study assessment, and main findings were summarized.
Results: Twenty-one OPs were included with data of patients with ND outcome and functional cardiac outcome. Overall, there is an impaired mid-term ND outcome in patients with Hybrid procedure as stage I for HLHS. Only slight differences between stage I procedures (Hybrid vs. Norwood) in two comparing studies have been determined affecting right ventricular remodeling, short- and mid-term ND outcome, reduced brain growth until two years of age, sufficient quality of life, and altered hemodynamics influencing brain volumes and cerebral perfusion pattern.
Conclusions: Despite some minor differences regarding the mid-term follow-up in patients with HLHS comparing Hybrid vs. Norwood procedure, its impact on ND outcome seems rather low. This may be explained by the large number of covariates as well as the small study populations and the different selection criteria for patients undergoing Hybrid or Norwood procedure as stage I.
Introduction
Regarding congenital heart disease (CHD) as the most frequent birth defect with an incidence of 0.8% of life birth per year (1), the hypoplastic left heart syndrome (HLHS) is one of the most severe types of CHD accounting for 2%–3% of all CHDs or 2 of 10,000 live births per year (2, 3). Patients with HLHS undergoing staged palliation until Fontan procedure are at risk for impaired neurodevelopmental (ND) outcome (4). Impairment of brain development may start during fetal life in patients with HLHS due to an altered cerebral perfusion, impaired cerebral oxygenation, and reduced nutritional cerebral supply (5). At birth, this often results clinically in a microcephaly associated with a lower birth weight. The microcephaly resembles the clinical surrogate for a delay of brain growth and brain development, which has been determined as a delay of 3–4 weeks of gestational age at term (6, 7). The functional and cardiac outcome including body growth, pulmonary artery development, brain growth, hemodynamic findings, and myocardial function may be also affected in patients undergoing staged palliation for HLHS.
More than 95% of newborns with HLHS die after birth, if untreated. The urgent need for therapy for newborns with HLHS includes medical treatment with prostaglandin E1 for the patency of the ductus arteriosus and surgical palliation with perioperative pediatric ICU care due to early neonatal cardiopulmonary bypass (CPB) surgery. For over three decades, this surgical approach for HLHS started with early neonatal CPB surgery, the Norwood surgery as stage I procedure followed by hemi-Fontan or bidirectional cavopulmonary anastomosis during infancy as stage II (4–6 months), and completed by the Fontan procedure as stage III (2–3 years). However, overall survival of patients with HLHS is still limited with survival of 60%–65% at 5 years and 55% at 10 years, and the cardiac as well as extracardiac (ND outcome) morbidity remains a lifelong matter of concern (2, 3, 8).
In this context, postnatal surgical management appears to be a covariant factor influencing brain development as well as ND outcome (9). While the Norwood procedure is standard of care for the majority of patients with HLHS after birth, the perioperative invasiveness may influence ND outcome in up to 40% affected children including neuromotor ability, visual impairment, hearing loss, epilepsy, and cognitive and functional impairment (4).
As an alternative to Norwood stage I procedure, the Hybrid procedure including bilateral pulmonary artery banding, duct stenting, and balloon atrioseptostomy was developed in the early 1990s to improve outcomes among HLHS patients by providing a bridge to transplantation (10), in view of a still high mortality and morbidity. Pioneers of the Hybrid procedure started in 1993 (10, 11) with further use and modifications until today (12–14).
From the standpoint of impaired ND outcome, the Hybrid procedure was thought to be advantageous by postponing early neonatal CPB surgery to later potentially less invasive time periods in less immature and, therefore, less vulnerable brain structures avoiding overt brain damage (9).
Nowadays, the Hybrid procedure is frequently used in critically ill HLHS patients with associated risk factors such as prematurity, low birth weight, and comorbidity with the opportunity for bridging to Norwood procedure or heart transplantation, later on (15). This has been classified as Norwood alternative, salvage procedure, deferred Norwood procedure, pre-transplantation palliation, or univentricular–biventricular decision deferral (16).
The aim of this review was to provide an overview of the potential impact of Hybrid procedure on ND outcome compared to the Norwood procedure. The second aim was to analyze the functional outcome of the Hybrid procedure including somatic growth, pulmonary artery development, structural brain development, and myocardial function.
Materials and methods
Literature search
Systematic literature search using the terms “hypoplastic left heart syndrome” or “HLHS” and “neurodevelopment” and “hybrid” or “norwood” were performed on five electronic biomedical literature databases including Embase, Ovid, Web of science, Scopus, and Cochrane. During analysis, the reference list of each retrieved paper was further scanned for additional studies according to the selection criteria and publications analyzing functional cardiac outcome were added in the analysis. A second literature research was added by using the term (“Hypoplastic left heart syndrome” or “HLHS”) and hybrid and (neurodevelopmental* or “cerebral imaging” or “brain imaging” or “magnetic resonance imaging” or “MRI” or “ultrasound”).
Selection criteria
Eligible studies for the review included mono- or multicentric original publications (OPs), with retrospective or prospective study design, analyzing short-to-long-term neurodevelopmental outcome after Hybrid procedure as initial stage I palliation in patients with HLHS as well as the functional cardiac outcome as defined above. Hybrid procedure was defined as combined bilateral pulmonary artery banding with ductal stenting or continuous prostaglandin E1 infusion to preserve ductal patency and balloon atrioseptostomy.
Data extraction
Full OPs were extracted and checked critically for appraisal of evidence. Analyzed factors included name of the first author, year of publication, study design, number of patients, time, type and result of ND assessment, number of patients, type of CHD (HLHS/non-HLHS), type of stage I (Hybrid/Norwood), study assessment, and main findings.
Results
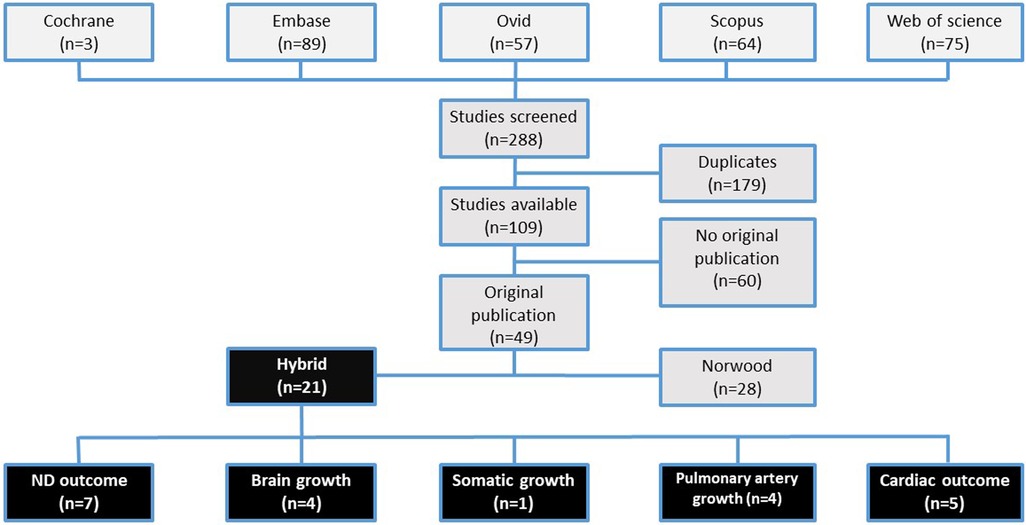
The search was conducted on March 16, 2022, and resulted in 288 data literature records on Cochrane (n = 3), Embase (n = 89), Ovid (n = 57), Scopus (n = 64), and Web of science (n = 75) (Figure 1). After deduplication, a total of 109 publications remained. Sixty papers were further excluded due to their type as reviews (n = 23), conference papers (n = 23), case reports (n = 7), or others including book chapters, clinical trials, or editorials (n = 7). Search results are depicted in Figure 1.
Studies analyzing the ND outcome after Hybrid procedure (n = 7) as well as studies analyzing the outcome beyond ND including brain (n = 4), somatic (n = 1), and pulmonary artery growth (n = 4) and functional cardiac outcome (n = 5) are described in detail in Tables 1 and 2.
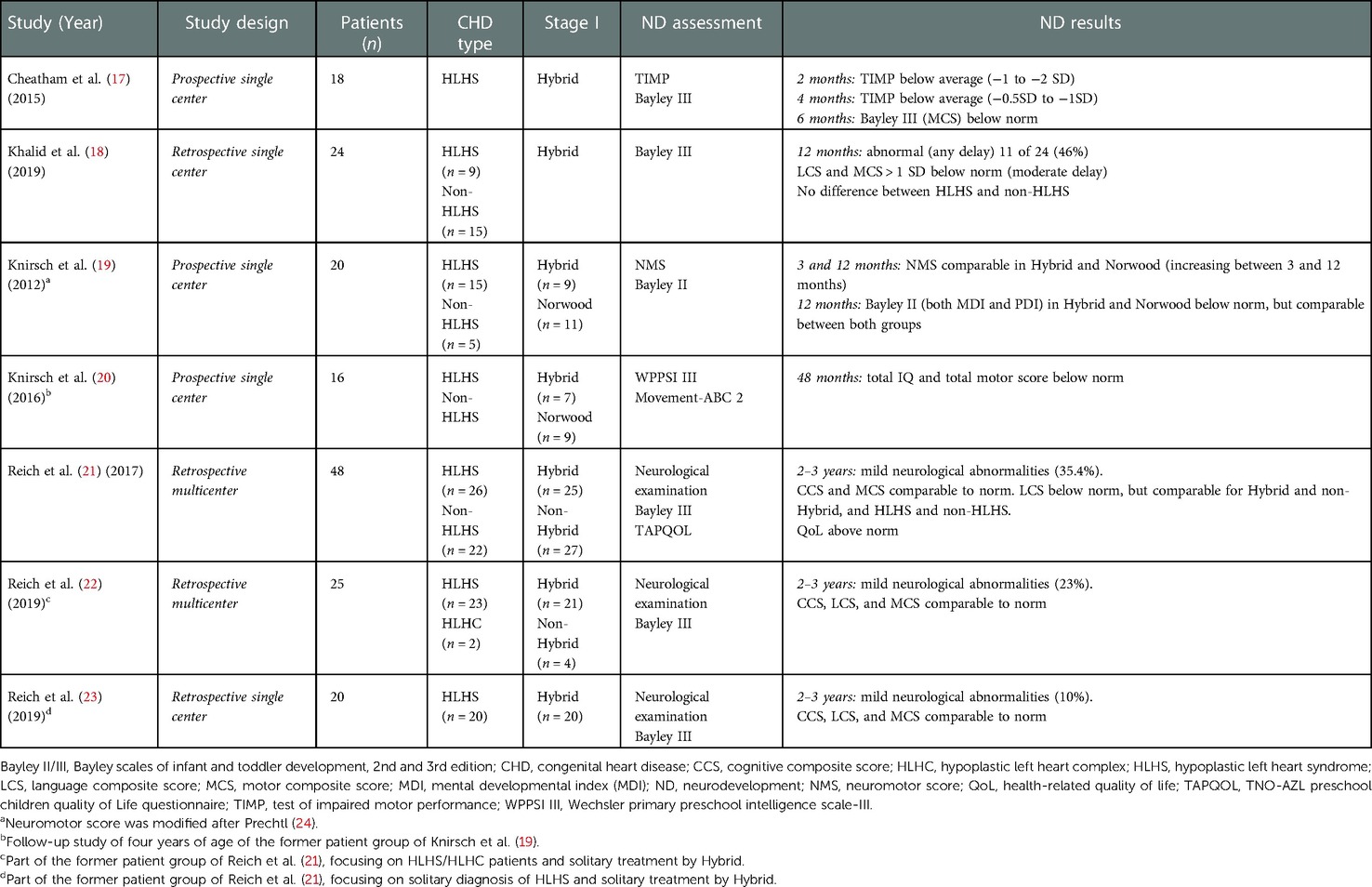
Table 1. Studies on neurodevelopmental outcome in patients with hypoplastic left heart syndrome with Hybrid procedure as stage I.

Table 2. Studies beyond neurodevelopmental outcome (cerebral, somatic, hemodynamic, and cardiac findings) in patients with hypoplastic left heart syndrome with Hybrid procedure as stage I.
A secondary search conducted on May 3, 2022, using (“Hypoplastic left heart syndrome” or “HLHS”) AND hybrid AND (neurodevelopmental* or “cerebral imaging” or “brain imaging” or “magnetic resonance imaging” or “MRI” or “ultrasound”) did not reveal further studies to be included.
Neurodevelopmental outcome
The ND outcome in patients with HLHS undergoing Hybrid procedure has been determined in retrospective (n = 3), prospective (n = 4), monocentric (n = 3), or multicentric (n = 4) studies (Table 1). The number of analyzed patients per study ranged between 16 and 48, but the patient cohorts analyzed in the different studies were overlapping due to subsequent follow-up study with evaluation at an older age (4 years of age), or patient analysis focusing solitary on HLHS/hypoplastic left heart complex (HLHC) patients or solitary treatment by Hybrid and not comparing with Norwood (19, 21). Some studies additionally included infants with a “non-HLHS” diagnosis of CHD defined as HLHC with left heart hypoplasia according to small left heart structures due to dysbalanced atrioventricular septal defect with left ventricular hypoplasia (Table 1). The ND assessment was conducted at different time points starting at 2 months of age until 4 years of age. Most frequently, Bayley II or III scale was used as primary ND outcome parameter.
Overall, the results of ND assessment after Hybrid procedure as stage I were mildly below normal-referenced data of control subjects.
At 2–4 months of age, mild affection of motor development was found using the Test of Infant Motor Performance (TIMP) (37) with a mean TIMP score at 2 months of age of 63.9 ± 18.1 (−1 to −2 SD) and at 4 months of age of 108.3 ± 14.9 (−0.5 to −1 SD) (17).
At the first half year of life (0–6 months), the neuromotor score [modified after (24) with a scaling of 0–18, i.e., 0 normal to 18 severely abnormal] was median (range) 4 (1–9) (19) after the Hybrid procedure.
At 12 months of age, the Bayley Scales of Infant Development II (Bayley II) were lower than the norm of 100 with median psychomotor development index (PDI) and mental development index (MDI) [PDI 57 (49–99), P < 0.001; MDI 91 (65–109), P = 0.002] (19). At the same age (12 months), Bayley III scores were comparable to the population norm for cognitive composite score (CCS) (95.2 ± 8.14) and 1 SD below the norm for language composite score (LCS) (93.6 ± 9.6) and motor composite score (MCS) (82.1 ± 11.9) (18).
At 2–3 years of age, despite mild neurological abnormalities, the median (range) LCS 97 (68–124) was below norm, while CCS with 100 (65–120) and MCS with 97 (55–124) were comparable to normative data (21) (Table 1).
At 4 years of age, cognitive outcome was determined by Wechsler Primary Preschool Intelligence Scale III (WPPSI III) and the Movement-ABC 2 for children after Hybrid were below the norm with median (range) IQ 88 (76–116) (20).
Comparative studies on ND outcome in children comparing Hybrid and Norwood procedure as stage I did not determine differences between cognitive, motor, or language development, neither using Bayley II scale at 1 year of age (19) nor using Bayley III scale at 2–3 years of age (21) or WPSSI III at 4 years of age (Table 1). Comparing the type of CHD (HLHS vs. non-HLHS) treated by Hybrid of ND outcome until preschool age ND outcome was similar (18, 19, 21).
Cerebral imaging findings
Cerebral imaging findings were analyzed in four studies (Table 2) (17, 25–27). Transcranial Doppler cerebral blood flow (CBF) from the middle cerebral artery (17, 27) and cerebral MRI for assessment of brain volumes (26) showed lower CBF in infants (2–6 months of age) after Hybrid procedure as stage I compared to a control population (27), but showed no correlation with ND outcome at 6 months of age (17). Saiki et al. compared Doppler cerebral blood flow over a longer (chronic) time period between stage I and stage II with reduced oxygenation balance index between lower and upper body in patients after Hybrid procedure. While the total brain volume and total, deep gray, and white matter volumes were reduced in HLHS/C compared to controls at 2–3 years of age, the volume reduction of deep gray and white matter was more reduced after Norwood as stage I procedure compared to Hybrid procedure (26). Of note, intracranial cerebral spinal fluid volume was larger compared to healthy controls before stage III Fontan procedure and correlated with impaired ND outcome (25, 36).
Somatic and pulmonary artery growth
Chan et al. compared in a small retrospective single-center study the weight-for-age and height-for-age (Z-score) somatic growth in three patient cohorts: Hybrid procedure with an early (within 4–6 weeks) switch to Norwood is defined as four-stage procedure (n = 5), Hybrid procedure with later comprehensive stage I/II is defined as a three-stage procedure (n = 8), and Norwood as stage I procedure (n = 49). The decline of weight-for-age (Z-score) between stage I and II was most distinct in the patient group of four-stage followed by three-stage procedure and the Norwood group (28), while in all three groups, there was a catch-up growth until stage III Fontan procedure (Table 2).
Limited pulmonary artery growth was described by smaller pulmonary artery indices after Hybrid procedure compared to Norwood patients before Fontan procedure at 2–3 years of age (29), while in another study, no differences of the pulmonary artery growth parameters such as McGoon ratio at comprehensive stage II and Fontan procedure in patients after Hybrid procedure were shown (30).
Cardiac findings
Three studies analyzed the myocardial function comparing Hybrid and Norwood procedure using cardiac MRI or echocardiography (31–33). At 2–3 years of age, in cardiac MRI, right ventricle (RV) size was larger after Norwood compared to Hybrid procedure, while in both groups, global RV function was preserved but RV myocardial strain was reduced (32). This was also determined by echocardiography, with no differences until 3 years of age regarding RV size, RV function determined by right ventricular fraction area of change, or calculated global RV radial shortening after Hybrid and Norwood procedure (33) (Table 2).
Discussion
The Hybrid procedure as stage I for the treatment of HLHS with PDA stenting, bilateral pulmonary artery banding combined with balloon atrioseptostomy, was developed as an alternative to the Norwood procedure in 1993 by Gibbs et al. (10), followed by the “Giessen group” in 1998 (11, 38). Further technical modifications of the Hybrid procedure were developed by combining PDA stenting by transpulmonary access immediately after pulmonary artery banding and delaying atrial septostomy to time of hospital discharge (Columbus and Sao Paolo) (12), and by including a reverse modified Blalock–Taussig shunt after pulmonary artery banding before PDA stenting (“Toronto group”) (14), these different technical modifications have been established in some centers for high-risk cases as a bridge to a delayed Norwood procedure (39). Despite less invasiveness of the Hybrid procedure in critical hemodynamic cases, the potential benefit of the Hybrid procedure remains the minimally invasive technique compared to the Norwood procedure by postponing early CPB surgery to a later time point with potential benefit on neurodevelopmental outcome (7). Although data on ND outcome after Hybrid procedure are limited due to small numbers of studies, this review focuses on ND and functional (cardiac) outcomes after Hybrid procedure.
In summary, this review on ND outcome of patients with HLHS after Hybrid procedure as stage I shows two major findings and consecutive challenges regarding this research topic for the future. First, the available data on ND outcome are limited concerning the number of patients being analyzed, comparing both treatment strategies as stage I (Hybrid vs. Norwood) in a prospective study protocol with a predefined neuroimaging follow-up using cerebral MRI with advanced cerebral MR perfusion techniques, volumetric assessment, metabolic, and microstructural (diffusion tensor imaging) assessment as well as a long-term ND outcome follow-up assessment. Second, the ND outcome follow-up assessment should be performed for a longer time period until adolescence and young adulthood and include more sophisticated test batteries for evaluation (executive function) of risk for alterations of brain maturation during development (40).
Neurodevelopmental outcome
In the past, ND outcome of patients treated for HLHS has been analyzed by the single ventricle reconstruction trial of the Pediatric Heart Network Investigators (41). This network was started by enrolling a large population of HLHS patients from a number of centers in North America undergoing Norwood procedure with the primary focus comparing the type of aortopulmonary shunt procedure, i.e., the modified Blalock–Taussig shunt and right ventricular-to-pulmonary artery shunt (42). Nevertheless, the trial also assessed the ND outcome for HLHS after Norwood procedure at 14 months (43). In their study, the mean (SD) PDI (74 ± 19) and MDI (89 ± 18) scores were lower than normative means. Compared to the findings after Hybrid procedure at 1 year of age, PDI trended to be lower, while MDI was comparable after Hybrid procedure [PDI 57 (49–99), P < 0.001; MDI 91 (65–109), P = 0.002] (19). At 3 years of age, they found developmental delay in all domains of the Ages and Stages Questionnaire (ASQ) ranging between 17% and 35%, including communication, gross and fine motor, problem solving, and personal social interaction. Furthermore, behavioral attitudes, quality of life, and functional status were also reduced (44). Our review on ND outcome after Hybrid procedure as stage I for HLHS determines an impaired ND outcome in all domains of early childhood development until 3 years of age, comparable to the findings of the Pediatric Heart Network Investigators for the ND outcome after Norwood procedure as stage I (19–23, 26, 30, 31). This includes mild neurological abnormalities with rates between 10% and 35% (Table 1). A clear difference of ND outcome between Norwood and Hybrid procedure has not been determined, so far. Therefore, long-term ND follow-up studies comparing both procedures for stage I until age of adolescence or early adulthood assessing complete neuropsychological profiles with specific notice on cognitive ND outcome measurements such as memory, executive function, and processing speed are needed (45).
Two decades ago, ND outcome was compared between Norwood patients and primary heart transplantation at school age, showing for both groups an overall lower neurocognitive test results (full scale IQ 86 ± 14) without difference between groups stratified by surgical strategy (46). Nowadays, there are some studies determining lower to normal Bayley Scales III; differences between the Hybrid and Norwood patient groups were not evident as well as between the HLHS and non-HLHS patient groups (Table 1). Therefore, it is recommended that children with complex CHD are regularly monitored in a structured ND follow-up program to identify early developmental delay and introduce early interventions, when needed (47).
(Interstage) mortality
According to the comparable results of ND outcome at 2–3 years of age after Hybrid and Norwood procedures, this has been also shown for overall mortality rate (including interstage mortality) comparing both treatment strategies. Lloyd et al. analyzed the preoperative condition and interstage mortality in Norwood and Hybrid procedures for HLHS (48). Although the patients after Hybrid procedure had a significantly higher Aristotle score, there was no difference for mortality at any stage. Yerebakan et al. reported single-center results of surgical mortality at stage I, comprehensive stage II, and Fontan procedure of 2.5%, 4.9%, and 0%, respectively, and an interstage mortality of 14.2% leading to a probability of survival of 77.8% at 10 years (30). Baba et al. compared survival after stage II and Fontan procedure after Hybrid and Norwood procedure as stage I, which were equivalent (14).
Myocardial function
Differences in myocardial function in patients undergoing Hybrid and Norwood as stage I procedure have been analyzed (Table 2). While Kobayashi et al. focused on acute changes of myocardial function undergoing Hybrid procedure, they showed higher right ventricular myocardial performance index (MPI) in Hybrid patients before intervention, followed by a decrease of MPI after Hybrid procedure within 2 weeks (34). For the chronic changes of myocardial function, Grotenhuis et al. described similar indices of RV size over a longer follow-up for systolic and diastolic function throughout all stages of palliation for Norwood and for Hybrid procedure patients (35). In contrast, right ventricular remodeling seems to be altered when analyzing global radial shortening and deformation indices, as determined by the Toronto group (33). While right ventricular fractional area change remained normal until stage III Fontan procedure independent of Hybrid or Norwood procedure, the global radial shortening increases after stage I in both groups due to greater relative RV circumferential contraction and unchanged longitudinal strain until stage III. Nevertheless, the RV remodeling after Norwood and Hybrid procedure were comparable, and the impact of CPB bypass surgery during stage I was limited (33). Within the largest cohort comparative study between stage II and III, Latus et al. showed comparable preserved global RV pump function determined by cardiac MRI, but better RV strain, strain rate, and intraventricular synchrony after Norwood stage I, both factors not influencing all-cause mortality (32).
Growth parameters
Pulmonary artery growth until stage III is more affected after Hybrid compared to Norwood procedure accompanied by a higher number of catheter interventions after Hybrid procedure (Table 2) (14, 18, 30, 32).
Somatic growth (determined as weight-for-age and height-for-age) declines after stage I. This decline continues until stage II and is most prominent for the critical ill neonates, who undergo Hybrid compared to Norwood procedure. Until stage III, Fontan procedure, a moderate increase of body growth follows (28). Nevertheless, after birth restricted body growth has been described for all growth parameters including body weight, body length, and head circumference, determined at birth before stage I, and is followed by a catch-up growth starting after stage II until stage III most prominent for the head circumference which is strongly correlated with the intracranial cerebral spinal fluid volume at 2–3 years of age (25).
On the other hand, brain growth determined for total brain volume and total, deep gray, and white matter volumes is reduced in a mixed population with HLHS and HLHC compared to healthy controls, while deep gray and white matter volumes are more reduced after Norwood stage I compared to Hybrid stage I (26).
Between stage I and stage II, cerebral perfusion determined by transcranial Doppler flow of middle cerebral artery that is either acute within the first week after Hybrid or until stage II is severely impaired after Hybrid (27). Similar findings were found in HLHS patients after Hybrid procedure as stage I with lower cerebral blood flow for 2–6 months compared to controls, but not correlating with ND outcome at 6 months of age (17). The oxygenation balance index between the lower and upper body was lower after Hybrid compared to Norwood procedure as stage I demonstrating impaired cerebral perfusion, which may be due to ongoing retrograde cerebral perfusion after Hybrid procedure as stage I (27). On the other hand, mesenteric perfusion determined by Doppler mesenteric indices improves after Hybrid procedure, which correlates with the potential beneficial effect for the prevention of necrotizing enterocolitis, which is a frequent complication in patients with HLHS by dysbalanced systemic (i.e., cerebral) and pulmonary perfusion (31).
Limitations
No long-term data comparing ND outcome after Hybrid or Norwood procedure as stage I procedure are available so far, although the technique was developed more than two decades ago. The total number of patients studied remains low for risk factor analysis in a highly multifactorial setting.
Conclusions
Overall, for comparing ND and functional outcome after Hybrid procedure, the numbers of studies are rather limited and differences between the two treatment options are rather small. Disadvantages of the Hybrid procedure as stage I include impaired pulmonary artery development, which may contribute to an impaired functional outcome after Fontan (49). Therefore, efforts are needed to enhance pulmonary artery growth as one of the most important prerequisite for later Fontan completion and long-term survival after Fontan completion until adulthood (50). This includes additional surgical procedures promoting symmetric pulmonary artery growth (51, 52) as well as optimizing catheter interventional procedure at different stages of treatment (53). So far, data available for children until preschool age show no clear advantage of Hybrid palliation on ND outcome, but long-term follow-up studies until adolescence or early adulthood are lacking, and the comparison of the two treatment strategies as stage I is still difficult due to a relevant selection bias. Nowadays, Hybrid stage I palliation for HLHS is used as a salvage procedure after birth obtaining hemodynamic stability (54) for high-risk HLHS patients with significant comorbidities (low birth weight or premature newborn or preterms), or is performed as a deferred Norwood procedure or a rapid two-stage Norwood procedure (55). Therefore, the Hybrid procedure for HLHS has become a kind of niche treatment option, and guidelines for the management of neonates and infants with HLHS summarize in most centers with an established Norwood program that Hybrid procedure is primarily used for high-risk neonates and to delay CPB bypass beyond the neonatal period (15).
Author contributions
WK: conceptualized the review, read the original publications, analyzed them, wrote the first draft of the manuscript, and finalized the manuscript after feedback from the coauthors. ADS: did the complete literature research and corrected the manuscript with substantial impact. MvR: wrote parts of the manuscripts and included the part concerning the neurodevelopmental outcome. All authors contributed to the article and approved the submitted version
Funding
This study was supported by the Swiss National Science Foundation (Grant No. 320030_184932) “Altered cerebral growth and development in infants with single ventricle congenital heart disease.”
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Hoffman JI, Kaplan S. The incidence of congenital heart disease. J Am Coll Cardiol. (2002) 39(12):1890–900. doi: 10.1016/S0735-1097(02)01886-7
2. Barron DJ, Kilby MD, Davies B, Wright JG, Jones TJ, Brawn WJ. Hypoplastic left heart syndrome. Lancet. (2009) 374(9689):551–64. doi: 10.1016/S0140-6736(09)60563-8
3. Feinstein JA, Benson DW, Dubin AM, Cohen MS, Maxey DM, Mahle WT, et al. Hypoplastic left heart syndrome: current considerations and expectations. J Am Coll Cardiol. (2012) 59(1 Suppl):S1–42. doi: 10.1016/j.jacc.2011.09.022
4. Atallah J, Garcia Guerra G, Joffe AR, Bond GY, Islam S, Ricci MF, et al. Survival, neurocognitive, and functional outcomes after completion of staged surgical palliation in a cohort of patients with hypoplastic left heart syndrome. J Am Heart Assoc. (2020) 9(4):e013632. doi: 10.1161/JAHA.119.013632
5. Sun L, Marini D, Saini B, Schrauben E, Macgowan CK, Seed M. Understanding fetal hemodynamics using cardiovascular magnetic resonance imaging. Fetal Diagn Ther. (2020) 47(5):354–62. doi: 10.1159/000505091
6. Miller SP, McQuillen PS, Hamrick S, Xu D, Glidden DV, Charlton N, et al. Abnormal brain development in newborns with congenital heart disease. N Engl J Med. (2007) 357(19):1928–38. doi: 10.1056/NEJMoa067393
7. Licht DJ, Shera DM, Clancy RR, Wernovsky G, Montenegro LM, Nicolson SC, et al. Brain maturation is delayed in infants with complex congenital heart defects. J Thorac Cardiovasc Surg. (2009) 137(3):529–36; discussion 536–7. doi: 10.1016/j.jtcvs.2008.10.025
8. Khairy P, Fernandes SM, Mayer JE Jr., Triedman JK, Walsh EP, Lock JE, et al. Long-term survival, modes of death, and predictors of mortality in patients with Fontan surgery. Circulation. (2008) 117(1):85–92. doi: 10.1161/CIRCULATIONAHA.107.738559
9. Beca J, Gunn JK, Coleman L, Hope A, Reed PW, Hunt RW, et al. New white matter brain injury after infant heart surgery is associated with diagnostic group and the use of circulatory arrest. Circulation. (2013) 127(9):971–9. doi: 10.1161/CIRCULATIONAHA.112.001089
10. Gibbs JL, Wren C, Watterson KG, Hunter S, Hamilton JR. Stenting of the arterial duct combined with banding of the pulmonary arteries and atrial septectomy or septostomy: a new approach to palliation for the hypoplastic left heart syndrome. Br Heart J. (1993) 69(6):551–5. doi: 10.1136/hrt.69.6.551
11. Akintuerk H, Michel-Behnke I, Valeske K, Mueller M, Thul J, Bauer J, et al. Stenting of the arterial duct and banding of the pulmonary arteries: basis for combined Norwood stage I and II repair in hypoplastic left heart. Circulation. (2002) 105(9):1099–103. doi: 10.1161/hc0902.104709
12. Galantowicz M, Cheatham JP, Phillips A, Cua CL, Hoffman TM, Hill SL, et al. Hybrid approach for hypoplastic left heart syndrome: intermediate results after the learning curve. Ann Thorac Surg. (2008) 85(6):2063–70; discussion 2070–1. doi: 10.1016/j.athoracsur.2008.02.009
13. Pizarro C, Derby CD, Baffa JM, Murdison KA, Radtke WA. Improving the outcome of high-risk neonates with hypoplastic left heart syndrome: hybrid procedure or conventional surgical palliation? Eur J Cardiothorac Surg. (2008) 33(4):613–8. doi: 10.1016/j.ejcts.2007.12.042
14. Baba K, Kotani Y, Chetan D, Chaturvedi RR, Lee KJ, Benson LN, et al. Hybrid versus Norwood strategies for single-ventricle palliation. Circulation. (2012) 126(11 Suppl 1):S123–31. doi: 10.1161/CIRCULATIONAHA.111.084616
15. Alphonso N, Angelini A, Barron DJ, Bellsham-Revell H, Blom NA, Brown K, et al. Guidelines for the management of neonates and infants with hypoplastic left heart syndrome: the European Association for Cardio-Thoracic Surgery (EACTS) and the Association for European Paediatric and Congenital Cardiology (AEPC) hypoplastic left heart syndrome guidelines task force. Eur J Cardiothorac Surg. (2020) 58(3):416–99. doi: 10.1093/ejcts/ezaa188
16. Wilder TJ, Caldarone CA. Apples to oranges: making sense of hybrid palliation for hypoplastic left heart syndrome. JTCVS Open. (2020) 4:47–54. doi: 10.1016/j.xjon.2020.10.002
17. Cheatham SL, Carey H, Chisolm JL, Heathcock JC, Steward D. Early results of neurodevelopment following hybrid stage I for hypoplastic left heart syndrome. Pediatr Cardiol. (2015) 36(3):685–91. doi: 10.1007/s00246-014-1065-5
18. Khalid OM, Harrison TM. Early neurodevelopmental outcomes in children with hypoplastic left heart syndrome and related anomalies after hybrid procedure. Pediatr Cardiol. (2019) 40(8):1591–8. doi: 10.1007/s00246-019-02191-3
19. Knirsch W, Liamlahi R, Hug M, Hoop R, von Rhein M, Pretre R, et al. Mortality and neurodevelopmental outcome at 1 year of age comparing hybrid and Norwood procedures. Eur J Cardiothorac Surg. (2012) 42(1):33–9. doi: 10.1093/ejcts/ezr286
20. Knirsch W, Liamlahi R, Dave H, Kretschmar O, Latal B. Neurodevelopmental outcome of children with hypoplastic left heart syndrome at one and four years of age comparing hybrid and Norwood procedure. Ann Thorac Cardiovasc Surg. (2016) 22(6):375–7. doi: 10.5761/atcs.lte.16-00106
21. Reich B, Heye K, Tuura R, Beck I, Wetterling K, Hahn A, et al. Neurodevelopmental outcome and health-related quality of life in children with single-ventricle heart disease before Fontan procedure. Semin Thorac Cardiovasc Surg. (2017). 5:S1043-0679(17)30288–5. doi: 10.1053/j.semtcvs.2017.09.014
22. Reich B, Heye KN, O'Gorman Tuura R, Beck I, Wetterling K, Hahn A, et al. Interrelationship between hemodynamics, brain volumes, and outcome in hypoplastic left heart syndrome. Ann Thorac Surg. (2019) 107(6):1838–44. doi: 10.1016/j.athoracsur.2018.12.012
23. Reich B, Heye KN, Wetterling K, Logeswaran T, Hahn A, Akintürk H, et al. Neurodevelopmental outcome in hypoplastic left heart syndrome after hybrid procedure. Transl Pediatr. (2019) 8(2):94–106. doi: 10.21037/tp.2019.04.05
24. Prechtl HF. The neurologic examination of the full-term newborn infant. 2nd ed. Press CU, editor. London: Mac Keith Press (1977).
25. Heye KN, Knirsch W, Latal B, Scheer I, Wetterling K, Hahn A, et al. Reduction of brain volumes after neonatal cardiopulmonary bypass surgery in single-ventricle congenital heart disease before Fontan completion. Pediatr Res. (2018) 83:63–70. doi: 10.1038/pr.2017.203
26. Knirsch W, Heye KN, Tuura RO, Hahn A, Wetterling K, Latal B, et al. Smaller brain volumes at two years of age in patients with hypoplastic left heart syndrome—impact of surgical approach. Int J Cardiol. (2019) 291:42–4. doi: 10.1016/j.ijcard.2019.03.055
27. Saiki H, Kurishima C, Masutani S, Tamura M, Senzaki H. Impaired cerebral perfusion after bilateral pulmonary arterial banding in patients with hypoplastic left heart syndrome. Ann Thorac Surg. (2013) 96(4):1382–8. doi: 10.1016/j.athoracsur.2013.05.108
28. Chan FTS, Bellsham-Revell HR, Duggan H, Simpson JM, Hulse T, Bell AJ. Interstage somatic growth in children with hypoplastic left heart syndrome after initial palliation with the hybrid procedure. Cardiol Young. (2017) 27(1):131–8. doi: 10.1017/S104795111600024X
29. Dave H, Rosser B, Knirsch W, Hübler M, Prêtre R, Kretschmar O. Hybrid approach for hypoplastic left heart syndrome and its variants: the fate of the pulmonary arteries. Eur J Cardiothorac Surg. (2014) 46(1):14–9. doi: 10.1093/ejcts/ezt604
30. Yerebakan C, Valeske K, Elmontaser H, Yoruker U, Mueller M, Thul J, et al. Hybrid therapy for hypoplastic left heart syndrome: myth, alternative, or standard? J Thorac Cardiovasc Surg. (2016) 151(4):1112–21; 1123.e1–5. doi: 10.1016/j.jtcvs.2015.10.066
31. Cozzi CT, Galantowicz M, Cheatham JP, Nicholson L, Fernandez R, Backes CH, et al. Ultrasound assessment of mesenteric blood flow in neonates with hypoplastic left heart before and after hybrid palliation. Cardiol Young. (2015) 25(6):1074–9. doi: 10.1017/S1047951114001607
32. Latus H, Nassar MS, Wong J, Hachmann P, Bellsham-Revell H, Hussain T, et al. Ventricular function and vascular dimensions after Norwood and hybrid palliation of hypoplastic left heart syndrome. Heart. (2018) 104(3):244–52. doi: 10.1136/heartjnl-2017-311532
33. Mah K, Serrano Lomelin J, Colen T, Tham EB, Lin L, Eckersley L, et al. Right ventricular remodeling in hypoplastic left heart syndrome is minimally impacted by cardiopulmonary bypass: a comparison of Norwood vs. hybrid. Pediatr Cardiol. (2021) 42(2):294–301. doi: 10.1007/s00246-020-02482-0
34. Kobayashi D, Natarajan G, Turner DR, Forbes TJ, Delius RE, Walters HL, et al. Effect of hybrid stage 1 procedure on ventricular function in infants with hypoplastic left heart syndrome. Cardiol Young. (2016) 26(5):867–75. doi: 10.1017/S1047951115001419
35. Grotenhuis HB, Ruijsink B, Chetan D, Dragulescu A, Friedberg MK, Kotani Y, et al. Impact of Norwood versus hybrid palliation on cardiac size and function in hypoplastic left heart syndrome. Heart. (2016) 102(12):966–74. doi: 10.1136/heartjnl-2015-308787
36. Knirsch W, Mayer KN, Scheer I, Tuura R, Schranz D, Hahn A, et al. Structural cerebral abnormalities and neurodevelopmental status in single ventricle congenital heart disease before fontan procedure. Eur J Cardiothorac Surg. (2017) 51(4):740–6. doi: 10.1093/ejcts/ezw399
37. Barbosa VM, Campbell SK, Berbaum M. Discriminating infants from different developmental outcome groups using the test of infant motor performance (TIMP) item responses. Pediatr Phys Ther. (2007) 19(1):28–39. doi: 10.1097/PEP.0b013e31802f65f9
38. Michel-Behnke I, Akinturk H, Schranz D. Fate of the stented arterial duct. Circulation. (2000) 102(22):E178. doi: 10.1161/01.CIR.102.22.e178
39. Karamlou T, Najm HK. Evolution of care pathways for babies with hypoplastic left heart syndrome: integrating mechanistic and clinical process investigation, standardization, and collaborative study. J Thorac Dis. (2020) 12(3):1174–83. doi: 10.21037/jtd.2019.10.75
40. Brossard-Racine M, Panigrahy A. Structural brain alterations and their associations with function in children, adolescents, and young adults with congenital heart disease. Can J Cardiol. (2022) 3:S0828-282X(22)00994–1. doi: 10.1016/j.cjca.2022.10.028
41. Ohye RG, Sleeper LA, Mahony L, Newburger JW, Pearson GD, Lu M, et al. Comparison of shunt types in the Norwood procedure for single-ventricle lesions. N Engl J Med. (2010) 362(21):1980–92. doi: 10.1056/NEJMoa0912461
42. Ohye RG, Gaynor JW, Ghanayem NS, Goldberg CS, Laussen PC, Frommelt PC, et al. Design and rationale of a randomized trial comparing the Blalock-Taussig and right ventricle-pulmonary artery shunts in the Norwood procedure. J Thorac Cardiovasc Surg. (2008) 136(4):968–75. doi: 10.1016/j.jtcvs.2008.01.013
43. Newburger JW, Sleeper LA, Bellinger DC, Goldberg CS, Tabbutt S, Lu M, et al. Early developmental outcome in children with hypoplastic left heart syndrome and related anomalies: the single ventricle reconstruction trial. Circulation. (2012) 125(17):2081–91. doi: 10.1161/CIRCULATIONAHA.111.064113
44. Pasquali SK, Ohye RG, Lu M, Kaltman J, Caldarone CA, Pizarro C, et al. Variation in perioperative care across centers for infants undergoing the Norwood procedure. J Thorac Cardiovasc Surg. (2012) 144(4):915–21. doi: 10.1016/j.jtcvs.2012.05.021
45. Bergemann A, Hansen JH, Rotermann I, Voges I, Scheewe J, Otto-Morris C, et al. Neuropsychological performance of school-aged children after staged surgical palliation of hypoplastic left heart syndrome. Eur J Cardiothorac Surg. (2015) 47(5):803–11. doi: 10.1093/ejcts/ezu299
46. Mahle WT, Visconti KJ, Freier MC, Kanne SM, Hamilton WG, Sharkey AM, et al. Relationship of surgical approach to neurodevelopmental outcomes in hypoplastic left heart syndrome. Pediatrics. (2006) 117(1):e90–7. doi: 10.1542/peds.2005-0575
47. Ware J, Butcher JL, Latal B, Sadhwani A, Rollins CK, Brosig Soto CL, et al. Neurodevelopmental evaluation strategies for children with congenital heart disease aged birth through 5 years: recommendations from the cardiac neurodevelopmental outcome collaborative. Cardiol Young. (2020) 30(11):1609–22. doi: 10.1017/S1047951120003534
48. Lloyd DFA, Cutler L, Tibby S, Vimaleswaran S, Qureshi S, Rosenthal E, et al. Analysis of pre-operative condition and interstage mortality in Norwood and hybrid procedures for hypoplastic left heart syndrome using the Aristotle scoring system. Cardiol Young. (2013) 23:S35–6. doi: 10.1017/S1047951112000376
49. Baek JS, Bae EJ, Kim GB, Kim WH, Lee JR, Kim YJ, et al. Pulmonary artery size and late functional outcome after Fontan operation. Ann Thorac Surg. (2011) 91(4):1240–6. doi: 10.1016/j.athoracsur.2010.12.002
50. Gewillig M, Brown SC. The Fontan circulation after 45 years: update in physiology. Heart. (2016) 102(14):1081–6. doi: 10.1136/heartjnl-2015-307467
51. Seaman CS, d'Udekem Y, Jones BO, Brizard CPR, Cheung MMH. Augmentation of pulmonary arterial growth in single ventricle patients by interim selective shunts. Semin Thorac Cardiovasc Surg. (2021) 33(2):483–9. doi: 10.1053/j.semtcvs.2020.09.007
52. Agematsu K, Okamura T, Takiguchi Y, Yoneyama F, Harada Y. Rapid growth of pulmonary artery after intrapulmonary artery septation. Asian Cardiovasc Thorac Ann. (2018) 26(6):479–81. doi: 10.1177/0218492318782821
53. Chaszczewski KJ, Huang J, Fuller S, Smith CL, Dori Y, Glatz AC, et al. Impact of transcatheter pulmonary artery intervention following superior cavopulmonary connection on pulmonary artery growth. World J Pediatr Congenit Heart Surg. (2021) 12(5):635–42. doi: 10.1177/21501351211033238
54. Haller C, Caldarone CA. The evolution of therapeutic strategies: niche apportionment for hybrid palliation. Ann Thorac Surg. (2018) 106(6):1873–80. doi: 10.1016/j.athoracsur.2018.05.048
Keywords: congenital heart disease, outcome, HLHS, hypoplastic left heart syndrome, Hybrid
Citation: Knirsch W, De Silvestro A and von Rhein M (2023) Neurodevelopmental and functional outcome in hypoplastic left heart syndrome after Hybrid procedure as stage I. Front. Pediatr. 10:1099283. doi: 10.3389/fped.2022.1099283
Received: 15 November 2022; Accepted: 14 December 2022;
Published: 16 January 2023.
Edited by:
Milan Prsa, Centre Hospitalier Universitaire Vaudois (CHUV), SwitzerlandReviewed by:
Jan Hansen, University Medical Center Schleswig-Holstein, GermanyJochen Grohmann, Heart and Diabetes Center North Rhine-Westphalia, Germany
© 2023 Knirsch, De Silvestro and von Rhein. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Walter Knirsch d2FsdGVyLmtuaXJzY2hAa2lzcGkudXpoLmNo
Specialty Section: This article was submitted to Pediatric Cardiology, a section of the journal Frontiers in Pediatrics
 Walter Knirsch
Walter Knirsch Alexandra De Silvestro1,2,3
Alexandra De Silvestro1,2,3