- Division of Pediatric Cardiology, Lucile Packard Children's Hospital, Stanford University Medical Center, Palo Alto, CA, United States
Introduction: As we learn more about the novel multisystem inflammatory syndrome in children (MIS-C) associated with COVID-19 infection, the protocols for long-term follow-up have evolved and only some of these protocols have been published. Here, we review the current literature on follow-up guidelines in MIS-C patients.
Methods: We conducted a PUBMED search of all articles published on “MIS-C” and the term “follow-up” between 2020 and 2022. Inclusion criteria were that (1) the study was an observational study or case series, and (2) the study population included pediatric population who met the diagnostic criteria for MIS-C.
Results: There were 206 publications on MIS-C and follow-up in the last 2 years with 11 studies that fit the inclusion criteria. These papers were representing 11 different centers and encompassed a total of 343 participants. Seven of the 11 studies had participants follow-up with their cardiologist within 1 month of discharge. Between 12% and 62% of patients within each study had depressed left ventricular ejection fraction (LVEF) at admission. At the initial follow-up visit, five studies showed a normal LVEF in all patients while the other seven studies showed 2%–13% patients continuing to have depressed LVEF. In eight of the 11 studies, 9%–52% of patients had coronary artery dilation at admission. At their initial follow-up visit, 3%–28% of patients continued to have coronary artery dilation.
Conclusion: There is some institutional variation in the outpatient follow-up protocols in patients diagnosed with MIS-C. A standardized follow-up guidelines might be helpful to monitor long-term prognosis of these patients.
Introduction
Our understanding of multi-inflammatory syndrome in children (MIS-C) associated with COVID-19 infection has grown significantly over the course of the global pandemic. There are many published studies describing the cardiac involvement of MIS-C with elevated markers of myocardial damage (troponin, B-type natriuretic peptide, etc.), ventricular dysfunction, coronary artery dilation, and arrhythmias (1). Many children with MIS-C present with hypotension and shock requiring admission to intensive care unit and have prolonged hospital courses. As these children are discharged, recommendations regarding follow-up visits with pediatric cardiology and timing of echocardiography remains largely institution-dependent with many institutions adopting timelines similar to Kawasaki Disease or myocarditis guidelines (1, 2). Current CDC and AAP guidelines remain largely broad with recommendation to follow-up with pediatric cardiology 2–3 weeks after discharge (3, 4). There are currently several published studies from multiple institutions on their MIS-C population with follow-up cardiology visits and echocardiography results. The purpose of our study is to review the current published data on the cardiology follow up guidelines for MIS-C patients, along with their echocardiography results, to understand the variability in current practice.
Methods
We conducted a PUBMED search with keywords “MIS-C” and “Follow-up” between 2020 and 2022. We selected case series and observational studies that fit our inclusion and exclusion criteria. Studies which met the following criteria were included: (1) the study design was an observational study or case series, (2) the study population included pediatric population (<21 years old) who met the diagnostic criteria for MIS-C as established by Centers for Disease Control and Prevention (4). The following information was extracted: author(s), year of publication, sample size, admission and follow-up echocardiography findings, and timing of follow-up pediatric cardiology visits.
Results
Yield of the search
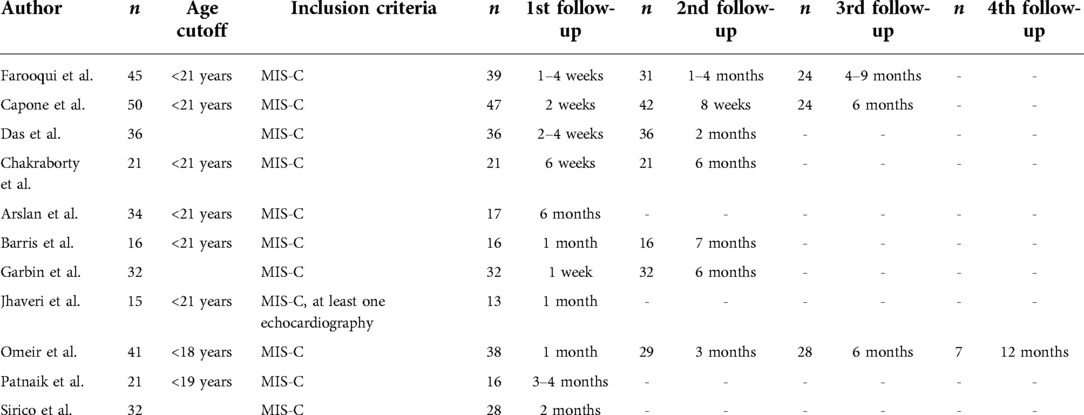
There were 206 publications that resulted with our keyword search on MIS-C and follow-up between 2020 and 2022. Eleven published studies fit the inclusion criteria with a total of 343 participants (5–15). All studies included patients who met criteria for MIS-C per the CDC guidelines (see Figure 1).
First follow-up timeline
We summarize the follow-up timeline of the included studies in Table 1. Seven of the 11 studies had participants follow-up with pediatric cardiology within 1 month of discharge regardless of the hospital course or echocardiography findings during hospital admission. In the other four studies there was variation. Sirico et al. and Chakraborty et al. had patients follow-up within 2 months, Patnaik et al. had patients follow-up at 3–4 months, and Arslan et al. had patients follow-up at 6 months.
Second or further follow-up timeline
Four of these 11 studies did not have data regarding further follow-up visits. Of the seven studies that had second follow-up visit data, the timeline varied between 2 and 6 months. Only three of the 11 studies had data about a third follow-up visit which was around 6 months. Two studies had fourth follow-up visit data which was 1 year from discharge.
Echocardiography results
We only extracted LV function and coronary dilation data for this review due to limited information available from the included publications.
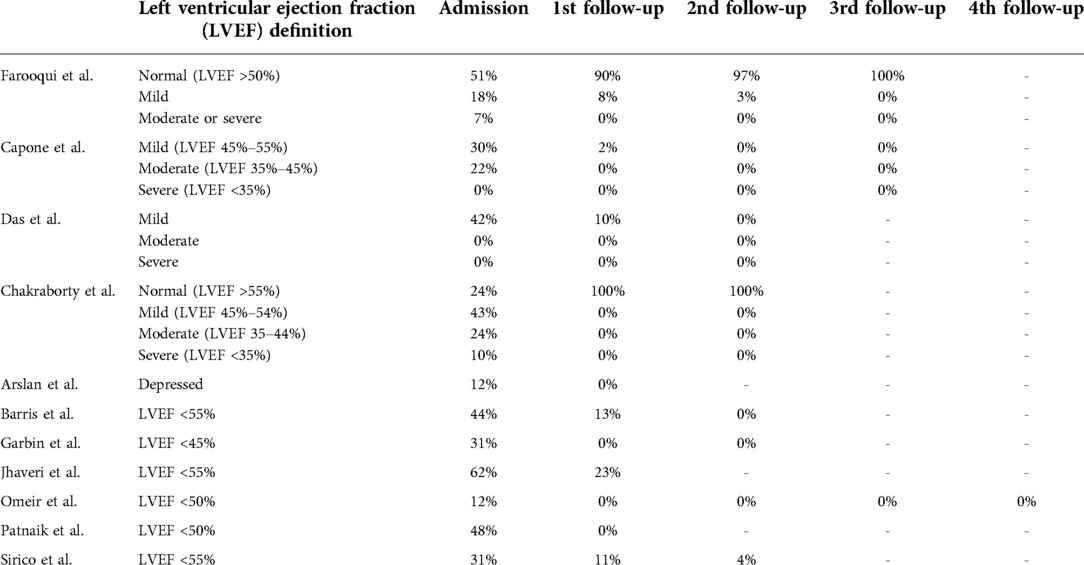
Table 2 summarizes the left ventricular function assessment by ejection fraction (LVEF) results from admission and follow-up that are available from each study being reviewed. In terms of grading the left ventricular systolic function, four of the 11 studies categorized left ventricular function data into normal, mild, moderate, and severe. The other seven studies provided data as normal vs. depressed systolic function. The percentage of patients with depressed LVEF at admission ranged between 12% and 62%.
On the initial follow-up echocardiography, five studies reported normal LVEF in all the patients they saw in clinic. In the other six studies, 2%–13% of the patients who came in for their first follow-up visit had ongoing depressed LVEF.
In the seven studies that showed second follow-up visit data, 3%–4% of patients showed ongoing depressed LVEF. Farooqui et al. showed that 3% of the patients who had decreased LVEF at their second follow-up had complete recovery of function at the third follow-up visit. Sirico et al. which showed 4% of patients with ongoing depressed LVEF does not have further follow-up data. Capone et al. and Chakraborty et al. notes persistent diastolic dysfunction in a small subset of patients (4%–9.5%) at their 6 month follow-up. All of these patients had LV systolic dysfunction during their hospitalization.
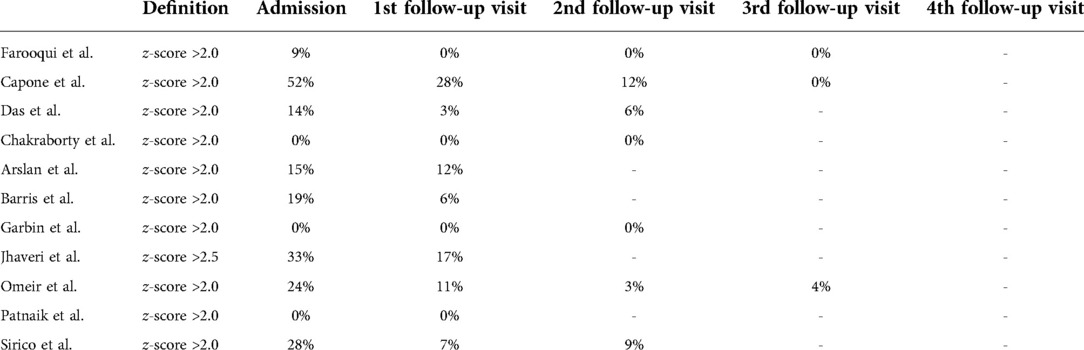
Table 3 summarizes the coronary artery dilation data from each study being reviewed. In terms of coronary artery dilation, three studies showed no coronary artery dilation in patients during admission. Of the other eight studies, there was coronary artery dilation in 9%–52% of patients during admission. There was complete resolution of coronary artery dilation in Farooqui et al. at the first follow-up visit. Others showed ongoing coronary artery dilation in 3%–28% of patients at the first follow-up. Barris et al., Jhaveri et al., and Arslan et al. showed ongoing coronary artery dilation in 6%, 17%, and 12% of patients respectively at the initial follow-up visit and did not have data on further follow-up visits. Four studies showed ongoing coronary artery dilation in 3%–12% of patients at the second follow-up visit. Capone et al. showed complete resolution of coronary artery dilation in all patients at the third follow-up visit. Omeir et al. showed ongoing coronary artery dilation in 4% of patients at the third follow-up visit 6 months later.
Discussion
We reviewed eleven studies that report on follow-up visits and echocardiography findings in patients with MIS-C between 2020 and 2022. Due to the limited available data, we focused mainly on the timing of the follow-up visit, and LVEF and coronary artery dilation in the echocardiography reports.
Timing of follow-up visits
Since there are no standardized protocols for follow-up for children with MIS-C, many institutions have established their internal follow-up guidelines based on Kawasaki disease or myocarditis guidelines. Most studies we reviewed showed an initial cardiology visit within 1 month of discharge, which is similar to the 4–6 weeks recommendation for Kawasaki disease (16). However, unlike Kawasaki disease, there is no risk stratification for MIS-C either based on coronary artery dilation or the degree of ventricular dysfunction. Some institutions, such as ours (see Figure 2), have established follow up schedules based on hospital course and echocardiography findings during admission (1, 2, 17). For studies that had initial follow-up later than 1 month following discharge, it is unclear whether there were other medical visits (general pediatrician, rheumatology, infectious disease etc.) to continue to monitor for symptoms. However, follow-up with pediatric cardiology later than 1 month following discharge might delay evaluation of coronary arteries considering the risk for developing coronary artery dilation in the convalescent phase in patients with MIS-C. At our own institution, we recommend a follow-up with pediatric cardiology at 2 weeks after discharge if patients had coronary or myocardial involvement during admission and four to 6 weeks if patients had no coronary or myocardial involvement (17).
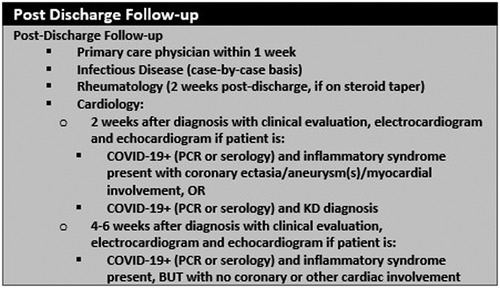
Figure 2. MIS-C follow-up guidelines at Lucile Packard Children's Hospital, Stanford University (17).
Echocardiography findings
The findings of the studies reviewed here are similar to prior studies that have reported LVEF in MIS-C patients (4, 18, 19). There was depressed LVEF in ∼12%–62% of patients during admission in these studies. More than half the patients had normal left ventricular function as early as their initial follow-up echocardiography, which is comparable to myocarditis (20). However, mortality rate is low in MIS-C and there is no reported need for heart transplantation in pediatric population. There are several studies that look at follow-up CMR imaging in patients with LV dysfunction during admission which also shows normalization or improvement in LV function at the follow-up visit (21–23).
In terms of coronary artery dilation, most studies in this review showed 0%–30% of patients with coronary artery dilation with initial follow-up echocardiography within 1 month of discharge reassuringly showing resolution of coronary artery dilation in more than half of the patients. None of the studies note new onset of coronary artery dilation at the follow up visit. These data are important for outpatient pediatric cardiologists who are seeing patients with MIS-C as they are being evaluated for sports clearance and need for ongoing antiplatelet therapy or anticoagulation. Most institutions follow Kawasaki disease guidelines for patients with coronary artery involvement in MIS-C. While much about long-term course of MIS-C remains unknown, collective evaluation of single institutions is paramount to furthering our knowledge about this disease. There is also great anticipation for the MUSIC study which looks at the long term 5 year follow-up for patients with MIS-C to shed further light on this topic (24).
In terms of return to sports participation, only one of the studies reviewed commented on their practice which is to allow for clearance after normalization of inflammatory markers and systolic cardiac function usually around 8 weeks after hospital discharge (7).
Limitations
This mini review is limited to only looking at the follow-up timelines and LV ejection fraction and coronary artery dilation amongst patients with MIS-C. We did not include data regarding laboratory values, valvular involvement, pericardial effusion, cardiac MRI imaging, or arrhythmias in this review. There are also limited information regarding the COVID-19 variants involved in each study.
Conclusion
There is some institutional variation in the follow-up guidance for patients diagnosed with MIS-C. Based on limited publications to date, most institutions appear to have an initial follow-up visit within 1 month of discharge, however the further follow-up timelines vary. Follow-up guidelines based on the severity of initial presentation, hospital course, and echocardiographic findings are needed to provide guidance for physicians caring for patients with MIS-C.
Author contributions
First authorship: JJ conceptualized the review design, conducted search, gathered data, formal analysis, wrote and edited manuscript. Senior authorship: ES conceptualized the review design, supervised search, data gathering, and analysis, reviewed and edited manuscript. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
MIS-C, multisystem inflammatory syndrome in children; LVEF, left ventricular ejection fraction; Echo, echocardiography.
References
1. Alsaied T, Tremoulet AH, Burns JC, Saidi A, Dionne A, Lang SM, et al. Review of cardiac involvement in multisystem inflammatory syndrome in children. Circulation. (2021) 143(1):78–88. doi: 10.1161/CIRCULATIONAHA.120.049836
2. Son MB, Freidman K. COVID-19: multisystem inflammatory syndrome in children (MIS-C) management and outcome. Available at: https://www.uptodate.com/contents/covid-19-multisystem-inflammatory-syndrome-in-children-mis-c-management-and-outcome#H999319060.
3. AAP. Multisystem inflammatory syndrome in children (MIS-C interim guidance. Available at: https://www.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/clinical-guidance/multisystem-inflammatory-syndrome-in-children-mis-c-interim-guidance/.
4. CDC. Multisystem inflammatory syndrome (MIS) (2021). Available at: https://www.cdc.gov/mis/hcp/index.html.
5. Farooqi KM, Chan A, Weller RJ, Mi J, Jiang P, Abrahams E, et al. Longitudinal outcomes for multisystem inflammatory syndrome in children. Pediatrics. (2021) 148(2):e2021051155. doi: 10.1542/peds.2021-051155
6. Barris DM, Keelan J, Ahluwalia N, Jhaveri S, Cohen J, Stern K, et al. Midterm outcomes and cardiac magnetic resonance imaging following multisystem inflammatory syndrome in children. J Pediatr. (2022) 241:237–241.e1. doi: 10.1016/j.jpeds.2021.10.009
7. Capone CA, Misra N, Ganigara M, Epstein S, Rajan S, Acharya SS, et al. Six month follow-up of patients with multi-system inflammatory syndrome in children. Pediatrics. (2021) 148(4):e2021050973. doi: 10.1542/peds.2021-050973
8. Das N, Hill R, Trivedi M, Kenkre TS, Alsaied T, Feingold B, et al. Longitudinal assessment of cardiac function following multisystem inflammatory syndrome in children associated with COVID-19. Pediatr Cardiol. (2022). doi: 10.1007/s00246-022-02972-3. [Epub ahead of print]
9. Garbin M, Raso I, Piersanti A, Gianolio L, De Silvestri A, Calcaterra V, et al. Advanced echocardiographic analysis in medium-term follow-up of children with previous multisystem inflammatory syndrome. Children (Basel). (2022) 9(6):917. doi: 10.3390/children9060917
10. Jhaveri S, Ahluwalia N, Kaushik S, Trachtman R, Kowalsky S, Aydin S, et al. Longitudinal echocardiographic assessment of coronary arteries and left ventricular function following multisystem inflammatory syndrome in children. J Pediatr. (2021) 228:290–293.e1. doi: 10.1016/j.jpeds.2020.08.002
11. Aziz OA, Sadiq M, Qureshi AU, Hyder N, Kazmi U, Batool A, et al. Short to midterm follow-up of multi-system inflammatory syndrome in children with special reference to cardiac involvement. Cardiol Young. (2022):1–9. doi: 10.1017/S1047951122000828. [Epub ahead of print]35321771
12. Patnaik S, Jain MK, Ahmed S, Dash AK, Ram Kumar P, Sahoo B, et al. Short-term outcomes in children recovered from multisystem inflammatory syndrome associated with SARS-CoV-2 infection. Rheumatol Int. (2021) 41(11):1957–62. doi: 10.1007/s00296-021-04932-1
13. Sirico D, Basso A, Sabatino J, Reffo E, Cavaliere A, Biffanti R, et al. Evolution of echocardiographic and cardiac magnetic resonance imaging abnormalities during follow-up in patients with multisystem inflammatory syndrome in children. Eur Heart J Cardiovasc Imaging. (2022) 23(8):1066–74. doi: 10.1093/ehjci/jeac096
14. Chakraborty A, Philip R, Santoso M, Naik R, Merlocco A, Johnson JN. Cardiovascular magnetic resonance in children with multisystem inflammatory syndrome in children (MIS-C) associated with COVID-19: institutional protocol-based medium-term follow-up study. Pediatr Cardiol. (2022) 43(8):1879–87. doi: 10.1007/s00246-022-02927-8
15. Arslan SY, Bal ZS, Bayraktaroglu S, Ozenen GG, Bilen NM, Levent E, et al. Cardiac assessment in children with MIS-C: late magnetic resonance imaging features. Pediatr Cardiol. (2022) 1–10. doi: 10.1007/s00246-022-02977-y. [Epub ahead of print]35916926
16. McCrindle BW, Rowley AH, Newburger JW, Burns JC, Bolger AF, Gewitz M, et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a scientific statement for health professionals from the American Heart Association. Circulation. (2017) 135:927–99. doi: 10.1161/CIR.0000000000000484
17. Kache S, Schwenk H, Mathew R, Gerstbacher D, Ivancie R, Lo C, et al. Multisystem inflammatory syndrome in children (MIS-C) pathway exclusion criteria: multisystem inflammatory syndrome in children (MIS-C) pathway determine patient disposition based on initial presentation and work-up (2020).
18. McCrindle BW, Manlhiot C. SARS-CoV-2-related inflammatory multisystem syndrome in children. J Am Med Assoc. (2020) 324(3):246–8. doi: 10.1001/jama.2020.10370
19. Kabeerdoss J, Rakesh PK, Karkhele R, Sathish Kumar T, Danda D, Singh S, et al. Severe COVID-19, multisystem inflammatory syndrome in children, and Kawasaki disease: immunological mechanisms, clinical manifestations and management. Rheumatol Int. (2021) 41:19–32. doi: 10.1007/s00296-020-04749-4
20. Law YM, Lal AK, Chen S, Čiháková D, Cooper LT, Deshpande S, et al. Diagnosis and management of myocarditis in children: a scientific statement from the American Heart Association. Circulation. (2021) 144(6):E123–35. doi: 10.1161/CIR.0000000000001001
21. Aeschlimann FA, Misra N, Hussein T, Panaioli E, Soslow JH, Crum K, et al. Myocardial involvement in children with post-COVID multisystem inflammatory syndrome: a cardiovascular magnetic resonance based multicenter international study—the CARDOVID registry. J Cardiovasc Magn Reson. (2021) 23(1):1–10. doi: 10.1186/s12968-021-00841-1
22. Webster G, Patel AB, Carr MR, Rigsby CK, Rychlik K, Rowley AH, et al. Cardiovascular magnetic resonance imaging in children after recovery from symptomatic COVID-19 or MIS-C: a prospective study. J Cardiovasc Magn Reson. (2021) 23(1):1–7. doi: 10.1186/s12968-021-00786-5
23. Bartoszek M, Małek ŁA, Barczuk-Falęcka M, Brzewski M. Cardiac magnetic resonance follow-up of children after pediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2 with initial cardiac involvement. J Magn Reson Imaging. (2022) 55(3):883–91. doi: 10.1002/jmri.27870
Keywords: MIS-C, COVID-19, follow-up, echocardiography, outpatient MIS-C: multisystem inflammatory syndrome in children, LVEF: left ventricular ejection fraction, echo: echocardiography, coronary artery dilation
Citation: Jose JT and Selamet Tierney ES (2022) Outpatient monitoring of patients with multisystem inflammatory syndrome (MIS-C): A mini review. Front. Pediatr. 10:1069632. doi: 10.3389/fped.2022.1069632
Received: 14 October 2022; Accepted: 17 November 2022;
Published: 7 December 2022.
Edited by:
Marianna Fabi, Sant'Orsola University Hospital, ItalyReviewed by:
Mehdi Oualha, The Necker -Enfants Malades Hospital, France© 2022 Jose and Selamet Tierney. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jerin Tresa Jose anRqMTdAYWx1bW5pLnV0c3cuZWR1
Specialty Section: This article was submitted to Pediatric Cardiology, a section of the journal Frontiers in Pediatrics
 Jerin Tresa Jose
Jerin Tresa Jose Elif Seda Selamet Tierney
Elif Seda Selamet Tierney