
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pediatr., 22 December 2022
Sec. Neonatology
Volume 10 - 2022 | https://doi.org/10.3389/fped.2022.1064931
This article is part of the Research TopicSARS-CoV-2: Implications for Maternal-Fetal-Infant and Perinatal Mortality, Morbidity, Pregnancy Outcomes and Well-BeingView all 15 articles
Mother-infant dyads faced many challenges during the COVID-19 pandemic; however, the impact was different depending on socio-economic determinants. This study aims to investigate the impact of the COVID-19 pandemic on maternal provision of mother's own milk (MOM) at neonatal intensive care unit (NICU) discharge among preterm infants. We hypothesized that fewer infants would be discharged home on any MOM during the pandemic period compared to a pre-pandemic period. This is a retrospective analysis of infants born <34 weeks' gestation admitted to the Women and Infant's Hospital NICU. Infants born pre-pandemic (1/1/2019 to 2/29/2020) were compared to infants born during the pandemic (3/1/2020 to 4/30/2021). Maternal and neonatal variables were analyzed by group. The primary outcome was provision of MOM (defined as feeding exclusively MOM, or a combination of MOM and formula) at NICU discharge. Analyses were performed for time periods, and multivariable regression analyses were run for the total cohort and by insurance type. Analysis included 268 infants born pre-pandemic and 262 infants born during the pandemic. Pandemic group mothers vs. pre-pandemic were less likely to be single (27%, 63/233 vs. 38%, 93/243; p = 0.01) and more likely to have a diagnosis of chorioamnionitis (16%, 38/236 vs. 7%, 17/243; p = 0.002). Rates of public insurance were similar (55% pre-pandemic and 50% pandemic). There was no significant change in provision of MOM between time periods. In multivariable analysis, public insurance decreased the odds of MOM at discharge for the entire study period (aOR 0.31, 95% CI: 0.19–0.50; p = 0.0001). On analysis by insurance type, rates of MOM increased from 77% pre-pandemic to 88% during the pandemic (p = 0.03) for mothers with private insurance and remained unchanged for mothers with public insurance (52% pre-pandemic and 53% pandemic; p = 0.86). Mothers with private insurance had twice the odds (aOR 2.02, 95% CI: 1.02–3.97; p = 0.04) of providing MOM during the pandemic vs. pre-pandemic. For those with public insurance, the odds for any MOM provision during the pandemic were unchanged (aOR 0.95, 95% CI: 0.5–1.7; p = 0.86). These differences may be related to health care disparities requiring additional exploration of risk factors and the need for equitable opportunities for all mother-infant dyads.
Mother's own milk (MOM) is the ideal source of nutrition for infants, and in particular for infants born prematurely. MOM is beneficial in decreasing the risks of necrotizing enterocolitis, chronic lung disease, and late onset sepsis, and is associated with improved neurodevelopmental outcomes (1, 2). Yet despite these benefits, fewer preterm infants than term infant receive breast milk. In a recent report published by the Centers for Disease Control and Prevention, among infants born in the United States, 71.3% of preterm infants receive breast milk comparted to 84.6% of term infants (3). Unfortunately, there are known multi-factorial socioeconomic challenges such as poverty, low maternal education, and maternal race and ethnicity that are linked to decreased provision of MOM (4–8). Authors of a recent California cohort study reported a 52% lower odds of breast milk use at Neonatal Intensive Care Unit (NICU) discharge for families with public insurance compared to those with private insurance (8).
The onset of COVID-19 brought about unexpected and swift changes in the NICU environment. Early in the pandemic, NICU visitation policies were restrictive, limiting the number of parents who could visit as well as the frequency of visits. Such changes led to parental reported difficulties with breastfeeding, bringing in milk and supplies, communication and teaching moments, as well as overall decreased wellbeing (9–13). Additionally, many units experienced staffing changes that included scaled-down in-person lactation support (9, 14-16).
Currently, there are limited data published on the early impact of the pandemic on the provision of MOM for high-risk preterm infants, particularly between mothers with different insurance types. The primary aim of this study was to investigate maternal provision of MOM at the time of NICU discharge among preterm infants, and second, MOM provision for mothers with public vs. private insurance. Our primary hypothesis was that fewer infants would be discharged home on any MOM during the pandemic when compared to pre-pandemic.
This is a single center, retrospective, observational study of preterm infants born <34 weeks gestational age (GA) at Women and Infant's Hospital (WIH) between January 2019 and April 2021 and who survived to NICU discharge. Exclusion criteria included infants with a congenital syndrome and infants who were transferred prior to discharge. The study protocol was approved by the WIH Institutional Review Board and informed consent was waived due to the retrospective nature of the study.
There were two comparison groups: infants born pre-pandemic (January 2019–February 2020), and infants born during the pandemic (March 2020-April 2021). March 2020 was selected as the start date of data collection for the pandemic group as per the World Health Organization (WHO) definition (17).
Maternal and infant data were collected from the electronic medical record and included the following variables: maternal age, marital status, insurance type (public vs. private), parity, multiple gestation, mode of delivery, presence of prenatal care, race, ethnicity, education level, and medical complications during pregnancy including maternal hypertensive disorders (inclusive of gestational hypertension, preeclampsia and eclampsia), gestational diabetes, placental abruption, and clinical chorioamnionitis. Infant variables included GA at birth, birth weight, sex, inborn status, discharge weight, length of hospital stay, and medical complications including sepsis (defined by a positive blood culture), bronchopulmonary dysplasia (defined as oxygen at 36 weeks), necrotizing enterocolitis (defined as Bell stage ≥2), and presence of a gastrostomy tube.
The primary outcome of this study was MOM at NICU discharge, which was defined as either feeding exclusively MOM or a combination of MOM and formula. All breast milk that infants received was MOM, as a donor human milk program was not in place at WIH during the study period.
The WIH lactation support program is an in-person service that is available seven days per week, eight hours per day, and this availability was unchanged during the pandemic time period. The lactation support team is comprised of three Certified Lactation Counselors (CLCs), including a native Spanish speaker, and two nurse International Board Certified Lactation Consultants (IBCLCs). The team assists all NICU mothers in three main areas: milk expression, preparing to breastfeed, and breastfeeding. Additionally, the lactation support team provides post-NICU support, including phone consultations and as needed outpatient lactation appointments. The IBCLCs create unit breastfeeding/lactation guidelines, lead the NICU Breastfeeding Committee, and provide education for the NICU staff.
The WIH NICU visitation policy was modified during the pandemic. The initial change restricted visitation to parents and grandparents only, with universal masking required. Within a week, visitation was further limited to two designated visitors per patient or set of multiples (typically the mother, and their partner/support person). The two designated visitors could be modified under extenuating circumstances, and exceptions were made, pending approval by hospital administration, for critically ill or dying infants. Each visitor was allowed only one visit per day of unlimited duration.
If a designated visitor had any symptoms of COVID-19, they were asked not to visit the hospital and to receive polymerase chain reaction (PCR) testing. If a designated visitor was exposed to someone positive for COVID-19, they were asked to quarantine for 10 days and a negative PCR test after quarantine was required to visit the hospital. If a designated visitor was positive for COVID-19, they were asked to quarantine for 10 days. If a baby was born to a mother positive for COVID-19, they could not visit the baby in the NICU for 10 days after symptom onset, or positive PCR test if asymptomatic. All cases of COVID-19 symptoms, exposure and positive testing were reviewed by the hospital pediatric infectious disease specialist who advised on testing and quarantine requirements.
Maternal and infant characteristics were compared in bivariate analysis by using the t test or Wilcoxon test for continuous variables, and χ2 test for categorical variables. A multivariable logistic regression model was created to identify factors associated with the primary outcome of MOM at discharge. The model was adjusted for multiples, and pre-identified variables known to be confounders in the relationships of provision of MOM including maternal age, marital status, parity, race, education, and insurance status. Length of hospital stay was included to reflect infant health status. Models were run with clinical chorioamnionitis as it was significantly different between the time periods, however, was not retained as it did not contribute to the main regression model. Adjustment for multiple births was done using generalized estimating equations with an exchangeable correlation structure. Adjusted odds ratios were calculated with 95% confidence intervals. Secondary analyses were also conducted to study the relationship of insurance type and MOM at discharge. A p-value of <0.05 was considered statistically significant. All statistical analyses were conducted using SAS version 9.4 (SAS Institute).
A total of 479 mothers and 530 infants met inclusion criteria and were compared by pre-pandemic (n = 243 mothers and n = 268 infants) and pandemic (n = 236 mothers and n = 262 infants) time periods. Table 1 presents maternal characteristics. In the pandemic group, there were significantly fewer mothers who identified as single (27% vs. 38%, p = 0.01), and more cases of clinical chorioamnionitis (16% vs. 7%, p = 0.002) than pre-pandemic. Maternal social determinants of health including race, ethnicity, and education less than high school were similar between the two time periods. No differences were seen for public insurance pre-pandemic vs. pandemic (55% vs. 50%, p = 0.30). Table 2 presents infant characteristics. Infants born during the pandemic had a higher birth weight (1,481 g ± 528 g vs. 1,617 g ± 507 g, p = 0.005). This difference decreased but remained significant when controlling for GA (p = 0.02). Infant characteristics of medical complications, discharge weight, and length of NICU stay were similar between groups. For the primary outcome of any MOM at NICU discharge, analyzed by pre-pandemic vs. pandemic time periods, no significant differences (63% vs. 71%, p = 0.07) were seen for the total cohort. However, provision of any MOM at NICU discharge increased for mothers with private insurance during the pandemic (77% pre-pandemic vs. 88% pandemic, p = 0.03), while there was no change between time periods for mothers with public insurance (52% pre-pandemic vs. 53% pandemic, p = 0.86).
Table 3 presents the multivariable regression models to predict any MOM at NICU discharge. For the total cohort, there was no effect of the pandemic on maternal provision of any MOM at NICU discharge (aOR 1.3, 95% CI: 0.84–1.95; p = 0.26). However, public insurance was an independent risk factor for lower odds of MOM provision (aOR 0.31, 95% CI: 0.19–0.50; p = 0.0001), and lower maternal education was associated with a 50% lower odds of MOM provision (aOR 0.5, 95% CI: 0.2–0.9; p = 0.03). In addition, for every 10 days in the NICU, there was a 13% decreased odds of MOM provision (aOR 0.87, 95% CI: 0.83–0.91; p = 0.0001).
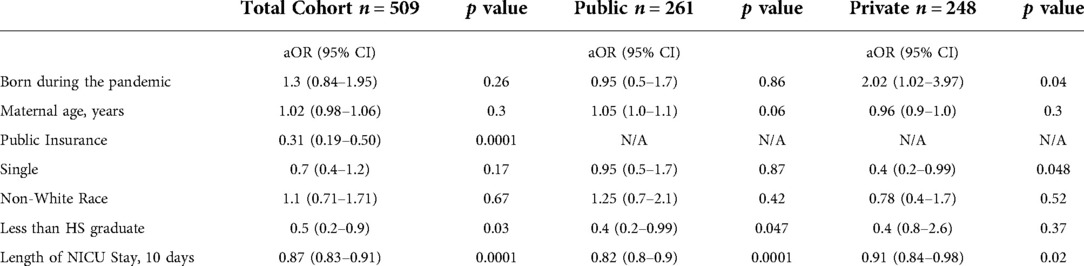
Table 3. Logistic regressions of maternal & infant characteristics to predict MOM at discharge for the entire study period.
Separate regression models (Table 3) were estimated to predict any MOM at discharge by insurance type. During the pandemic, the odds of any MOM at discharge for mothers with public insurance remained unchanged (aOR 0.95, 95% CI: 0.5–1.7; p = 0.86), with a 18% decrease in odds of any MOM (aOR 0.82, 95% CI: 0.8–0.9; p = 0.0001) for every 10 additional days in the NICU. Mothers with private insurance had twice the odds of providing any MOM at NICU discharge (aOR 2.02, 95% CI: 1.02–3.97; p = 0.04), with a 9% decrease in odds of any MOM (aOR 0.91, 95% CI: 0.84–0.98; p = 0.02) for every 10 additional days in the NICU. Being single was associated with lower odds (aOR 0.4, 95% CI: 0.2–0.99; p = 0.048) of providing MOM at discharge for the private insurance group. Lower maternal education was marginally associated with lower odds (aOR 0.4, 95% CI: 0.2–0.99; p = 0.047) of providing MOM for the public insurance group only.
In this study, we report on the provision of MOM, comparing pre-pandemic and pandemic time periods for preterm infants discharged from the NICU. There was no association found between provision of MOM and the COVID-19 pandemic for the total cohort of preterm mother-infant dyads. However, after adjusting for covariates that predict MOM provision, a strong association was noted between private insurance and increased provision of MOM. These findings highlight a disparity between insurance types, especially as it relates to changes during the COVID-19 pandemic.
For our total cohort, maternal and infant characteristics and medical complications were similar between time periods, except for a few differences. There were more mothers with a clinical diagnosis of chorioamnionitis during the pandemic period. This finding is similar to the reports of other investigators. In a Canadian cohort, authors reported a 1.24 increased risk of clinical chorioamnionitis during the COVID-19 lockdown period compared to a corresponding 2015–2019 period (18). Despite the significant group difference identified in our data set, clinical chorioamnionitis did not have an impact on our primary outcome. However, several maternal medical complications during pregnancy that prevent early NICU visitation could potentially delay the initiation of expressing breast milk. In contrast, factors that enhance breast feeding, such as kangaroo care, could be explored further in the setting of pandemics (19).
An additional finding for our cohort was mothers were more likely to report being single during the pandemic. This may be related to COVID-19 isolation and social distancing guidelines, as marriages were often postponed during the pandemic (20). In our private insurance regression model, single status was associated with decreased odds of MOM provision at discharge. This finding may be partially explained by the importance of partner support for lactating mothers, particularly in times of overwhelming pandemic-related stress.
Another difference seen between time periods was infant birth weight, infants born during the pandemic were larger. There are conflicting reports on birthweight in pre-pandemic vs. pandemic time periods (21, 22). The magnitude of the difference decreased, though significance was retained when adjusting for GA. These findings may be a reflection that fewer infants were born at younger GA during the pandemic time period; the mean GA was one week greater in the pandemic time period. Although we interpret this finding with caution as GA differences were not statistically significant, Alshaikh et al. also report that GA and birth weight were higher in infants admitted to the NICU during the lockdown period (18).
While provision of MOM was similar between time periods, it was not until we explored rates by insurance type that clear group differences were identified. There was a significant increase in MOM for the private insurance group. A recent United Kingdom study by Hamid et al. that assessed poverty utilizing an index of multiple deprivation index (IMD) found similar results. Specifically that during the pandemic, women in the higher IMD (least deprived) quintiles were 2–4 times more likely to be feeding breast milk at NICU discharge than those in lower quintiles (23). It is possible that the mothers with private insurance have more opportunities to be present in the NICU, subsequently leading to increased exposure to supportive services and environments. Kelleher et al. reported patients with private insurance were able to spend more hours at the bedside per visit (5.7 h vs. 3.5 h), and an average of one more day per week in the NICU than patients with public insurance (24). Services such as in person lactation support, opportunities for skin-to-skin, participation in bedside care, and collaboration with the medical care team all facilitate successful breast milk production (25, 26). However, careful attention to not only the availability, but the accessibility of such services and opportunities for all groups of mothers is critical.
It was encouraging that provision of MOM did not significantly decrease for our mothers with public insurance. This may be a testament to mother's resiliency. Challenges that low-income mothers with public insurance may have faced during the pandemic include limited time off from work-place responsibilities, particularly if they were frontline or essential workers. In the United States, many essential workers, including those employed in public transit, nursing homes and food manufacturing plants, are reliant on public insurance (27, 28). Additional potential barriers low-income families may have encountered include limited access to transportation to the hospital, or problems finding care for children at home. NICU families with transportation difficulties are known to have decreased breast milk use at discharge (8). While data on maternal job status, available transportation, and home child care were not available for this cohort, they all relate to health care disparities and should be considered when supporting families of high-risk neonates.
Prolonged hospital stays provided a significant negative impact on MOM provision at discharge for our total cohort and separately for both insurance groups, which is not surprising as length of stay is a known risk factor for decreased MOM provision (29). One difficulty with maintaining breast milk provision is the amount of time needed for milk expression prior to each feed. For infants with prolonged hospital stay, mothers may need to return to work, challenging the ability to adequately express milk. Type of work has also been shown to have an impact on sustained provision of MOM which could relate to insurance status (30). Mothers in service/labor occupations have been reported to have the shortest breastfeeding duration (5.9 months average duration) as compared to non-working mothers or those in professional/managerial occupations (7.3–7.4 months average duration) (30). As longer hospital stays are correlated with illness severity among preterm infants, addressing disparities is critical.
Strengths of the study include a large cohort of high-risk preterm infants. To our knowledge, this is the first study in the United States to examine associations between the pandemic and provision of MOM for preterm infants and the differential effects of insurance type. Findings from our study are timely, as several pandemic-related policies are still in effect at hospitals, and may provide opportunity for modifications if needed. We recognize the limitations of this study, including the lack of data pertaining to confounders such as parental visitation, time spent with lactation team, and quantity of MOM available at discharge. Additionally, we did not collect data on maternal COVID positivity status, which may have impacted mother's ability to visit her neonate, and provide breast milk.
Regression analysis of our total cohort identified the importance of the contribution of public health insurance to our outcome of MOM provision. In the separate adjusted regressions by insurance, rates of MOM provision for mothers with public insurance remained unchanged during the two time periods, whereas mothers with private insurance were twice as likely to provide MOM during the pandemic. In summary, during the pandemic, type of health insurance impacted on provision of MOM. The study findings can be leveraged to support the need for hospitals to continually monitor and evaluate outcomes to ensure equal and equitable opportunity for all families.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to Lauren Boudreau,bGJvdWRyZWF1QHdpaHJpLm9yZw==.
LB: conceptualized and designed the study, identified variables for data collection, collected data, drafted the initial manuscript, and reviewed and revised the manuscript. BV and EM: designed the study, identified variables for data collection, and critically reviewed the manuscript for important intellectual content. RT: coordinated and supervised data collection, carried out data analysis, and reviewed and revised the manuscript. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Parker MG, Stellwagen LM, Noble L, Kim JH, Poindexter BB, Puopolo KM. Promoting human milk and breastfeeding for the very low birth weight infant. Pediatrics. (2021) 148(5):1–9. doi: 10.1542/peds.2021-054272
2. Vohr BR, Poindexter BB, Dusick AM, McKinley LT, Wright LL, Langer JC, et al. Beneficial effects of breast milk in the neonatal intensive care unit on the developmental outcome of extremely low birth weight infants at 18 months of age. Pediatrics. (2006) 118(1):e115–23. doi: 10.1542/peds.2005-2382
3. Chiang KV, Sharma AJ, Nelson JM, Olson CK, Perrine CG. Receipt of breast milk by gestational age – United States, 2017. MMWR Morb Mortal Wkly Rep. (2019) 68:489–93. doi: 10.15585/mmwr.mm6822a1
4. Patel AL, Schoeny ME, Hoban R, Johnson TJ, Bigger H, Engstrom JL, et al. Mediators of racial and ethnic disparity in mother’s own milk feeding in very low birth weight infants. Pediatr Res. (2019) 85(5):662–70. doi: 10.1038/s41390-019-0290-2
5. Lee HC, Gould JB. Factors influencing breast milk versus formula feeding at discharge for very low birth weight infants in California. (2009) (1097–6833 (Electronic)).
6. Patel AL, Johnson TJ, Meier PP. Racial and socioeconomic disparities in breast milk feedings in US neonatal intensive care units. Pediatr Res. (2021) 89(2):344–52. doi: 10.1038/s41390-020-01263-y
7. Jones KM, Power ML, Queenan JT, Schulkin J. Racial and ethnic disparities in breastfeeding. (1556–8342 (Electronic)).
8. Sankar MN, Weiner Y, Chopra N, Kan P, Williams Z, Lee HC. Barriers to optimal breast milk provision in the neonatal intensive care unit. J Perinatol. (2021) 42:1–7. doi: 10.1038/s41372-021-01275-4
9. Darcy Mahoney A, White RD, Velasquez A, Barrett TS, Clark RH, Ahmad KA. Impact of restrictions on parental presence in neonatal intensive care units related to coronavirus disease 2019. J Perinatol. (2020) 40(Suppl 1):36–46. doi: 10.1038/s41372-020-0753-7
10. Garfield H, Westgate B, Chaudhary R, King M, O'Curry S, Archibald SJ. Parental and staff experiences of restricted parental presence on a neonatal intensive care unit during COVID-19. Acta Paediatr. (2021) 110(12):3308–14. doi: 10.1111/apa.16085
11. Muniraman H, Ali M, Cawley P, Hillyer J, Heathcote A, Ponnusamy V, et al. Parental perceptions of the impact of neonatal unit visitation policies during COVID-19 pandemic. BMJ Paediatr Open. (2020) 4(1):e000899. doi: 10.1136/bmjpo-2020-000899
12. Carter BS, Willis T, Knackstedt A. Neonatal family-centered care in a pandemic. J Perinatol. (2021) 41(5):1177–9. doi: 10.1038/s41372-021-00976-0
13. Vance AJ, Malin KJ, Miller J, Shuman CJ, Moore TA, Benjamin A. Parents’ pandemic NICU experience in the United States: a qualitative study. BMC Pediatr. (2021) 21(1):558. doi: 10.1186/s12887-021-03028-w
14. Brown A, Shenker N. Experiences of breastfeeding during COVID-19: lessons for future practical and emotional support. Matern Child Nutr. (2021) 17(1):e13088. doi: 10.1111/mcn.13088
15. Spatz DL, Davanzo R, Müller JA, Powell R, Rigourd V, Yates A, et al. Promoting and protecting human milk and breastfeeding in a COVID-19 world. Front Pediatr. (2020) 8:633700. doi: 10.3389/fped.2020.633700
16. Merritt L, Verklan MT. The implications of COVID-19 on family-centered care in the NICU. Neonatal Netw. (2022) 41(1):45–50. doi: 10.1891/NN-2021-0012
17. WHO Director-General's opening remarks at the media briefing on COVID-19 - 11 March 2020. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19-11-march-2020.
18. Alshaikh B, Cheung PY, Soliman N, Brundler MA, Yusuf K. Impact of lockdown measures during COVID-19 pandemic on pregnancy and preterm birth. Am J Perinatol. (2022) 39(3):329–36. doi: 10.1055/s-0041-1739357
19. Mekonnen AA-O, Yehualashet SS, Bayleyegn AD. The effects of kangaroo mother care on the time to breastfeeding initiation among preterm and LBW infants: a meta-analysis of published studies. (1746–4358 (Print)).
20. Manning WA-O, Payne KA-O. Marriage and Divorce Decline during the COVID-19 Pandemic: A Case Study of Five States. LID. (2378-0231 (Print)). doi: 10.1177/23780231211006976
21. Adhikari EH, Moreno W, Zofkie AC, MacDonald L, McIntire DD, Collins RRJ, et al. Pregnancy outcomes among women with and without severe acute respiratory syndrome Coronavirus 2 infection. (2574–3805 (Electronic)).
22. Wei SQ, Bilodeau-Bertrand M, Liu S, Auger N. The impact of COVID-19 on pregnancy outcomes: a systematic review and meta-analysis. (1488–2329 (Electronic)).
23. Hamid HA-OX A, Szatkowski L, Budge H, Ojha S. Impact of the coronavirus disease 2019 pandemic on breastfeeding during and at discharge from neonatal care: An observational cohort study. LID. (2574–2272 (Electronic)). doi: 10.1002/ped4.12337.
24. Kelleher J, Dempsey J, Takamatsu S, Paul JJ, Kent E, Dempsey AG. Adaptation of infant mental health services to preterm infants and their families receiving neonatal intensive care unit services during the COVID-19 pandemic. Infant Ment Health J. (2022) 43(1):100–10. doi: 10.1002/imhj.21961
25. Gharib S, Fletcher M, Tucker R, Vohr B, Lechner BE. Effect of dedicated lactation support services on breastfeeding outcomes in extremely-low-birth-weight neonates. J Hum Lact. (2018) 34(4):728–36. doi: 10.1177/0890334417741304
26. Campbell-Yeo ML, Disher TC, Benoit BL, Johnston CC. Understanding kangaroo care and its benefits to preterm infants. (1179–9927 (Print)).
27. US Census Bureau. Week 39 household pulse survey: September 29 – October 11. (2022). Available at: https://www.census.gov/data/tables/2021/demo/hhp/hhp39.html.
28. Monte LM, Laughlin L. Essential, frontline, and high risk: How COVID-19 prioritized low-wage workers while heightening their disadvantage. (2022). https://www.census.gov/library/working-papers/2022/demo/SEHSD-WP2022-08.html.
Keywords: mother's own milk, neonatal intensive care unit (NICU), preterm (birth), coronavirus disease 2019 (COVID-19), pandemic, insurance, breast milk
Citation: Boudreau LE, Vohr BR, Tucker R and McGowan EC (2022) Provision of mother's own milk for preterm infants during the COVID-19 pandemic: Differential effect of insurance. Front. Pediatr. 10:1064931. doi: 10.3389/fped.2022.1064931
Received: 8 October 2022; Accepted: 29 November 2022;
Published: 22 December 2022.
Edited by:
Steven M. Barlow, University of Nebraska-Lincoln, United StatesReviewed by:
Hercília Guimarães, University of Porto, Portugal© 2022 Boudreau, Vohr, Tucker and McGowan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Elisabeth C. McGowan ZW1jZ293YW5Ad2locmkub3Jn
Specialty Section: This article was submitted to Neonatology, a section of the journal Frontiers in Pediatrics
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.