- 1Section of Health Care Research and Rehabilitation Research, Faculty of Medicine and Medical Center, University of Freiburg, Freiburg, Germany
- 2Department of Neuropediatrics and Muscle Disorders, Center for Pediatrics, Faculty of Medicine, University of Freiburg, Freiburg, Germany
Background: Integrated care models aim to strengthen the collaboration between healthcare sectors to ensure a higher quality of care for children with chronic conditions. Assessing pediatric healthcare integration through families' experiences, therefore, is essential. Our study aimed to psychometrically test the PICS-D, the first German-language integrated care questionnaire, which is based on the Pediatric Integrated Care Survey (PICS) developed in the USA.
Methods: We examined construct validity using exploratory and confirmatory factor analyses (structural validity). Cronbach's α and McDonald's ωt coefficients explored reliability. Cognitive interviews assessed wording comprehension and item appropriateness.
Results: PICS-D was completed by 204 caregivers of children with chronic conditions (women = 84%; mean age = 41.4 years). Factor analyses identified 3 factors: “Team quality & communication”, “Family impact”, and “Access to care”. The 3-factorial structure showed a satisfying fit to confirmatory classical-test-theory-based models. Due to the insufficient reliability of the third factor, we recommend using only factors 1 and 2 for scoring the PICS-D.
Conclusion: The PICS-D is a 13-item questionnaire to assess family-reported experiences in pediatric care integration, which has good psychometric properties. It may be useful in guiding quality improvement efforts or measuring the impact of a care plan or care model.
Trial registration: German Clinical Trials Register (DRKS): DRKS00018778; Trial registration date 05. December 2019—Retrospectively registered; https://apps.who.int/trialsearch/Trial2.aspx?TrialID=DRKS00018778.
Introduction
One of the most persistent problems in many healthcare systems is the fragmentation between sectors and disciplines, which particularly affects patients with chronic and complex conditions who rely on services from a variety of disciplines (1–6). Integrated care (IC) models aim to strengthen the collaboration between sectors to ensure a higher quality of care (2, 7). The definition of IC varies widely, focusing primarily on adult care (8, 9). Tailoring these definitions to the pediatric setting is essential, as children have different healthcare and social needs (4, 10). By integrating the child's health perspective, Antonelli et al. extend existing definitions and offer the framework upon which this study is based: “Integrated Care is the seamless provision of healthcare services, from the perspective of the patient and family, across entire care continuum. It results from coordinating the efforts of all providers, irrespective of institutional, departmental, or community-based organizational boundaries.” (11–13). This definition implies that patient and family experiences are relevant when assessing IC in pediatric settings (6, 14). To date, evidence on the effectiveness of existing IC models (especially in adult care) has been predominantly specific for certain conditions (4, 8, 15–17). Other pediatric questionnaires, such as the EMPATHIC-30, cover only single facets of care integration (e.g., family-centered care experiences) and are limited to individual pediatric disciplines (18, 19). Generic evaluations often fail to adequately define goals and outcomes, and provide too little information on the availability of established measurement instruments (8, 11–13, 20). The Pediatric Integrated Care Survey (PICS) is a questionnaire for the caregivers of chronically ill children which measures the family-reported experience of pediatric care integration in the US (21). In German-speaking countries, instruments to measure IC currently exist only in the field of adult care (22–26)—a fact highlighting the need for a validated questionnaire to assess how well integrated pediatric healthcare is for families.
Materials and methods
Overview of the pediatric integrated care survey (PICS)
Antonelli et al. at Boston Children's Hospital developed the PICS in 2013. They formed and guided focus groups and interviews with parents of chronically ill children receiving care from multiple medical and non-medical providers (11, 21). It consists of 19 validated (mainly Likert-scaled) core items that form five scales (e.g., Access to care, Family impact, and Team functioning/performance/quality/connectivity). An example item in the “Family impact” scale is as follows: “In the past 12 months, how often have your child's care team members talked with you about how healthcare decisions for your child will affect your whole family?”. The six-point response scale ranges from “never” to “always”. The authors propose a 12-month reference period to evaluate IC. There are supplementary items that have not been validated due to sample size limitations in the Ziniel et al. study, as well as accompanying demographic and healthcare status questions (21). The supplementary items are grouped into so-called “modules” and “supplementary question topics”. Antonelli et al. recommend selecting items in the set of supplementary questions in addition to the validated core items, depending on the focus of use (11).
Research aims
This study is part of the exploratory, prospective, controlled, two-armed SMA-C + -study, developed as an IT-supported Case Management to improve the care of patients with spinal muscular atrophy I and II (27). In this comprehensive project, we use the German version of the PICS to evaluate the Case Management as an IC intervention. Furthermore, we evaluated the questionnaire's psychometric properties by testing construct validity (as factorial/structural validity) and internal consistency. We, therefore, included the set of core items that were already validated in the English version.
Pre-data collection methods
The original PICS items' translation followed the six steps in the “Functional Assessment of Chronic Illness Therapy Translation Procedures and Guidelines” (FACIT): First, two native German speakers translated the instrument independently into German. A third native German speaker reviewed the translations and produced a preliminary version. A native English speaker then translated the preliminary version back into English. In subsequent steps, methodological and bilingual experts evaluated and discussed the different versions. In the final revision, the translated instrument is checked orthographically by a bilingual expert (28).
We conducted cognitive semi-structured interviews to assess wording comprehension and the item appropriateness of the preliminary PICS-D from the caregiver's perspective (29). For this purpose, we recruited N = 10 caregivers of chronically ill children in the Clinic of Neuropediatrics and Muscle Disorders of the University Medical Center Freiburg. After seven interviews, we revised problematic items based on their feedback. We then conducted another three interviews.
Pilot testing
We used the PICS-D for a cross-sectional study of family-reported experiences with IC involving caregivers of children with a chronic disease. Taking the original authors' approach, we identified patients with chronic conditions based on their care needs. Patients are categorized as having a chronic condition if at least one of the following criteria is met: regular use of medications, regular use of therapies, use of auxiliary aids, regular counseling, or psychotherapy. We recruited N = 204 caregivers Germany-wide via personal contact from the University Medical Center, Freiburg; the Clinic for Pediatrics I, University Hospital, Essen; and several social pediatric centers (SPC). SPCs are interdisciplinary outpatient clinics that provide multidisciplinary care for children with complex healthcare needs. The participating SPCs are located in Bochum, Bremen, Celle, Freiburg, Lübeck, Rotenburg (Wuemme) and, Stuttgart. Caregivers were approached individually and were given the questionnaire and an information leaflet. In addition, the patient organization “Children's Network Germany” posted an invitation to participate on its website. The “Children's Network” represents pediatric patient organizations in Germany. All participants received a 20 € voucher per completed questionnaire. Exclusion criteria for participating in the questionnaire were not having a chronically ill child, limited German proficiency, or a patient's or caregiver's refusal to participate. Data collection took place between March 2019 and May 2020.
Statistical analyses
The statistical methods applied in psychometrically testing the PICS rely on the procedure described in the original publication and are supplemented by analyzing additional properties (21). Antonelli et al. recommend a top/bottom box scoring (11). The top/bottom boxes are the highest and lowest ratings (most positive/negative rating) on a response scale. Therefore, the item is “transformed” into a binary variable, and the respondent receives a box score of 1 indicating that he/she checked the desirable answer (most positive/negative answer). In contrast, we did not dichotomize the items and considered the response scale as an interval-scaled variable. The original authors indicate that the recommended scoring method is primarily for communicating quality improvement to healthcare institutions/professions, which is not a primary endpoint of our study. We described sample characteristics for children and respondents (caregivers) and assessed distribution properties, structural validity, and internal consistency (Cronbach's α and McDonald's ωt). We performed descriptive analyses of the sample using IBM SPSS® and applied factor analyses in R (30).
Due to the content adjustment of the PICS-D, we refrained from confirmatory testing of the factor structure of the original PICS and conducted two exploratory factor analyses (EFA; extraction method: principal axis factoring after direct oblimin rotation) to identify concepts underlying the IC experience in German pediatric settings. Kaiser-Mayer-Olkin (KMO) coefficient and Bartlett sphericity test were used to analyze the suitability of the data for EFA. We calculated different criteria to determine the number of retained factors [Kaiser-Guttman criterion, parallel analysis and Velicer's MAP (31)]. We excluded three items on goal setting and access to medical records (original items 13, 30, and 31) from the beginning because the response scale deviated from a Likert scale (e.g., yes/no response format). Therefore, we included 16 Likert-scaled experience items (instead of the 19 original items) in the first EFA and 13 Likert-scaled items in the second EFA (another three items were excluded during the analysis process). We recoded response options such as “I don't know.” or “I have no concerns.” as missing values. Because the first EFA was mainly intended to provide exploratory support for selecting items, only the second EFA's results are reported in detail below.
To further analyze the PICS-D structure, we conducted two confirmatory factor analyses (CFA) using confirmatory classical-test-theory-based models. In each case, the CFAs followed an EFA that had been already been performed. We used the first CFA to obtain statistical criteria to exclude further items. The second CFA tested the performance of the final factor structure. Global measures of fit indicate the discrepancy between the data and hypothetical model (CFI, TLI, RMSEA) (32, 33). Bad fit of models may indicate violation of unidimensionality (i.e., item not related to the underlying concept) or insufficient item reliability. To determine the best dimensional structure, we conducted the CFAs on each factor as well as the whole model. Furthermore, we explored each factor's internal consistency via Cronbach's α and McDonald's ωt coefficient.
Results
Translation and adaptation
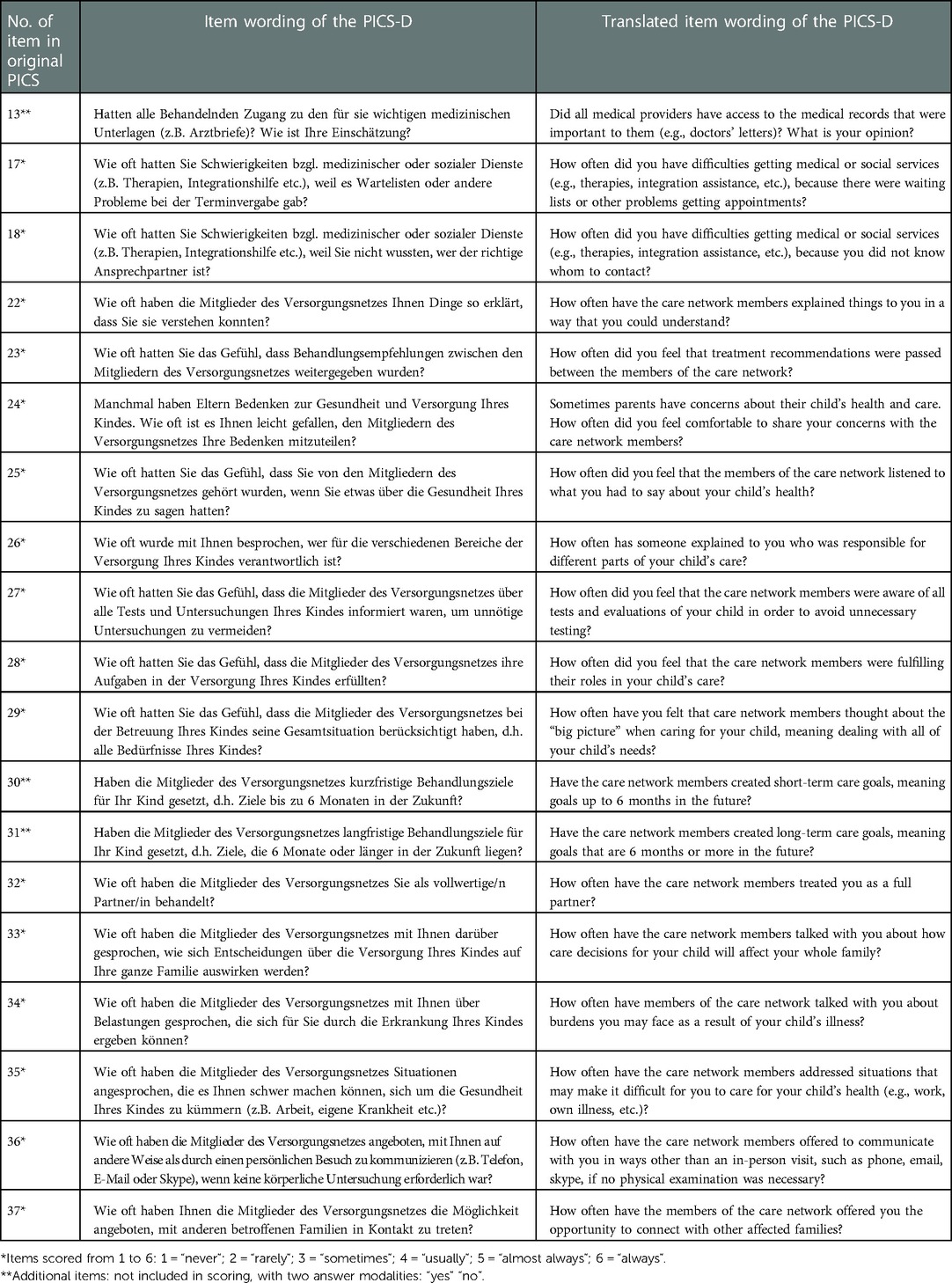
This section describes modifications to the original core items for assessing pediatric care integration in Germany. Table 1 shows the original 19 core items in both German and English translations (note: the latter does not match the wording of the original PICS items due to adaptations to the German health care system). The assignment of the original items, as well as their respective numbering, is found in the PICS “User Manual” (11). Most of the item changes resulted from the need to linguistically simplifying the wording, or adding information (concrete examples) for clarification. To ensure that the originally intended meaning of an item's wording remained intact, we consulted with the original authors at regular intervals. Moreover, cognitive interviews showed that the wording “care team” created confusion between the concepts of a “fixed team”, that works cohesively as a unit and a team that results from different responsibilities within the child's care. Caregivers reported that the care of their children had no “fixed team”. That is why we added an instruction defining the care team as all individuals involved in caring for the chronically ill child in the past 12 months (called the “care network”). After finalizing the questionnaire, we discussed the items with the original authors via videoconference. The translated PICS-version contained 19 core items on experiences (Table 1), a demographic and descriptive section including 32 items, and one open-ended item.
Sample characteristics
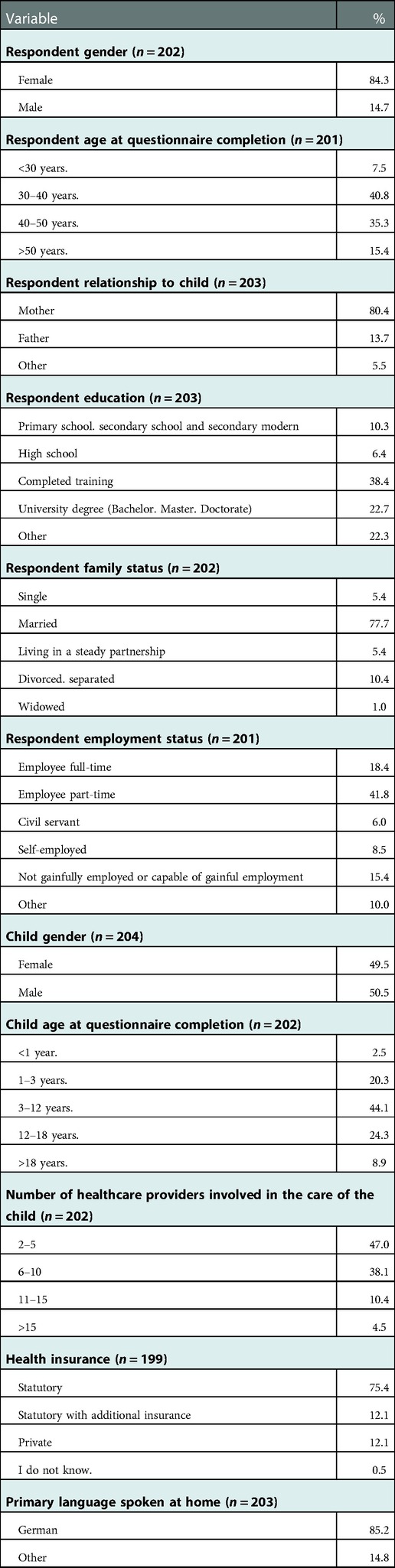
204 caregivers of children with chronic conditions completed the PICS-D, 84.3% of participants were female, 14.7% male. Two-thirds of respondents were between 30 and 50 years old and married. Slightly more than half of the participants were employed either part-time, not employed or not capable of gainful employment. The vast majority of the respondents' chronically ill children were between 1 and 12 years old. In 47% of participants, 2–5 health care providers were involved in the child's care. For around one-third of respondents, their care network even consisted of 6–10 health care providers. Further characteristics are detailed in Table 2.
Structural validity
The KMO coefficient (KMO = .89) and Bartlett sphericity test (χ2 = 1427.29, p < .001) indicated that the data we collected are suitable for the EFA. Parallel analysis and Kaiser-Guttman criterion suggest a three-factor solution, MAP two factors. We compared both EFA models and selected the three-factor solution because of a substantial better fit (RMSA < .08, SRMR < .05) in comparison to the two-factor solution. The three factors solution explained 53% of variance with low factor loadings on item 24 (share concerns with care network) and item 36 (communicate in ways other than an in-person visit). Factor loadings for the two items were item 24: 0.23, 0.19, and 0.10 in factors 1, 2, and 3, respectively and item 36: 0.33, 0.26, and 0.03 in factor 1, 2, and 3, respectively. Cognitive interviews revealed that both items were poorly understood due to their length and complicated syntax and we therefore excluded these items from our analysis. After exclusion, we conducted a first CFA for factor 1 and 2 that revealed high residual correlation within factor 1 for the item 27 with the items 23 and 25. Based on statistical and clinical considerations, we thus eliminated that item and then repeated the EFA and CFA analysis with 13 items.
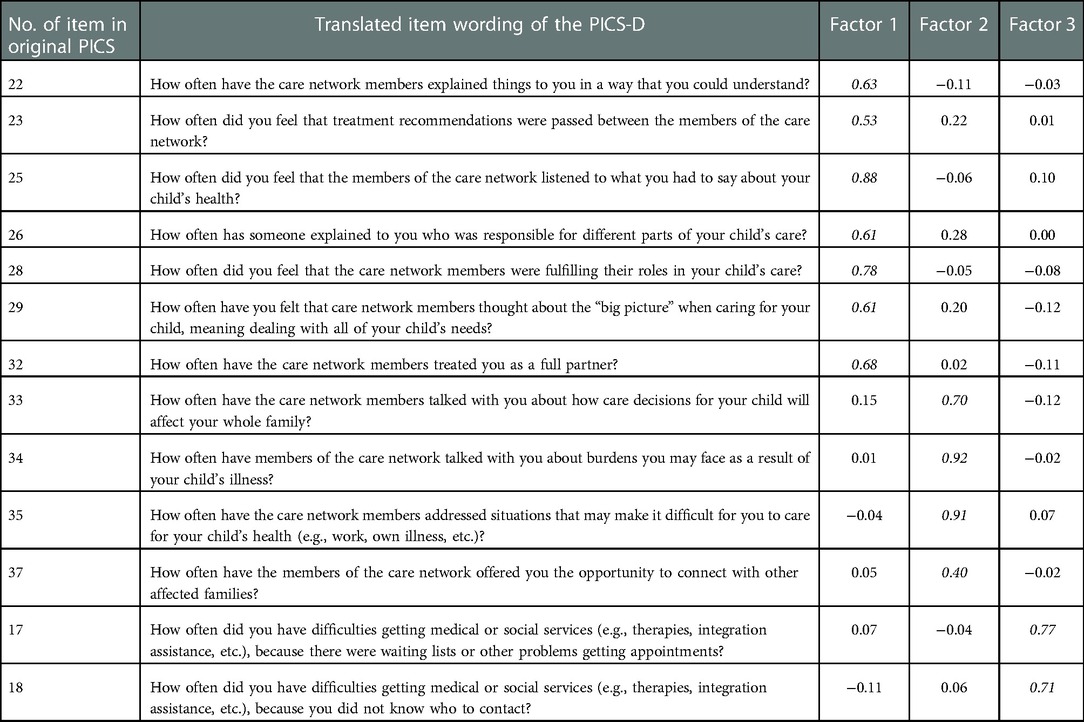
The three factors of the second EFA for the PICS-D items explained 58% of the variance. The items' standardized loadings were ≥0.53 on factor 1 (“Team quality & communication”) for items 22, 23, 25, 26, 28, 29, and 32; ≥0.40 on factor 2 (“Family impact”) for items 33, 34, 35, and 27; and ≥0.71 on factor 3 (“Access to care”) for items 17 and 18. All factor loadings can be found in Table 3.
We tested the model fit of the congeneric model for factors 1 and 2. The congeneric model is the least restrictive model of classical test theory, in which all items belong to one latent dimension. The fit indices suggested a good fit between the model and the data for factor 1 (CFI = 0.96, TLI = 0.94, RMSEA = 0.10) and a reasonable fit for factor 2 (CFI = 0.99, TLI = 0.96, RMSEA = 0.12). Since factor 3 consists of only two items, we used a parallel model to test unidimensionality because less restrictive models require more items. The parallel model combines the characteristics of the congeneric model with the assumption that correlations and measurement errors should be the same above all items. The fit indices suggested a good fit between the model and data for factor 3 (CFI = 1.00, TLI = 1.00, RMSEA < 0.01). Examining the entire three-factorial model, the fit indices suggested a good fit between the model and the data (CFI = 0.95, TLI = 0.94, RMSEA = 0.07).
Looking at the content of the items loading on factor 1, we observed that the focus was primarily on the interaction between families and health care providers. Simultaneously, factor 1 included items on the quality of communication in the care network. Therefore, we named factor 1 “Team quality & communication”. Items that loaded on factor 2 mainly addressed the impact of care (decisions) on families' daily lives. For this reason, we designated factor 2 “Family impact”. Factor 3 consisted of two items that concerned the access to care, so we named this factor “Access to care”.
Reliability
Cronbach's α was 0.89 and 0.84 in factors 1 and 2, respectively. Due to the absence of essential tau-equivalence in the model test, Cronbach's α is not interpretable as a reliability measure. We thus also report McDonald's ωt. McDonald's ωt was 0.93 and 0.88 in factors 1 and 2, respectively. Since factor 3 contains only two items, we could not calculate Cronbach's α or McDonald's ωt. As the inter-item correlation with r = 0.55 can be used as a reliability value, this factor shows insufficient reliability.
Discussion
In this study, we developed and psychometrically tested a German version of the Pediatric Integrated Care Survey (PICS), the so-called PICS-D. We can provide evidence that the PICS-D is a reliable and valid instrument by which to assess the experiences of IC as reported by the caregivers of chronically ill children. It takes a multidimensional approach and explores several crucial aspects of IC, categorized into three factors. Factor 1 “Team quality & communication” reflects the perceived quality of care and the cooperation within the care network (between all persons involved in caring for the chronically ill child in the last 12 months at the time of reporting), e.g., exchange of treatment recommendations, fulfillment of tasks involved in the care (2). Moreover, factor 1 analyzes the experiences concerning the communication between healthcare professionals and caregivers and the degree of the caregiver's involvement in decisions concerning the child's health, e.g., the feeling of being treated as a full partner (6, 22). Factor 2 “Family impact” evaluates the influence of care decisions and interventions on the entire family, e.g., burdens arising from the child's illness, opportunities for networking with other affected families (34, 35). Factor 3 “Access to care” investigated key elements of access to care, e.g., difficulties coordinating appointments (4, 36). Due to the insufficient reliability of the third PICS-D factor, we recommend using only factors 1 and 2 for scoring the PICS-D. To address this issue, it is necessary to develop a new associated item pool to re-examine this factor via factor analysis. More than four items would be desirable to perform in-depth statistical analyses. To obtain a rudimentary comparison with the psychometric properties of the original PICS, we used Cronbach's α for the two respective largest factors (21). The first PICS-D factor's internal consistency (“Team quality & communication”; Cronbach's α = 0.89) is slightly higher compared to the first original PICS factor (“Communication between health care provider and parent”; Cronbach's α = 0.80). In addition, the second PICS-D factor's internal consistency (“Family impact”; Cronbach's α = 0.84) is higher compared to the second original PICS factor (“Family impact”, Cronbach's α = 0.72).
The project team reviewed the items excluded from the analyses at both methodological and content levels. They seem to be well captured by the other items' content in the factors. A possible explanation for misunderstanding an item's wording could be the translation: In German, items tend to be longer and less commonly used, possibly triggering different latent constructs. However, the recovered factor structure in PICS-D appears to be topically similar to the original PICS’ factor structure (except for the excluded items) (11, 21). Factors 2 and 3 consist of identical items such as the “Access to care”- and “Family impact”-factors in the original PICS. Factor 1 represents a composite of the original factors “Communication between health care provider and parent” and “Team functioning/performance/quality/connectivity”.
Several strengths must be underlined. As far as we know, the PICS-D is the first and currently only German instrument by which to assess the perceived IC quality reported by caregivers of chronically ill children. This study examined its psychometric properties using a relevant nationwide sample. Our project provides compelling support for the critical importance of the role of patients and families in the design of health care delivery models, and in the evaluation of the performance of those models (37). The PICS-D is an initial step toward evaluating possible IC interventions to improve care for chronically ill children and increase caregivers' involvement in the care process. We used rigorous pre- and post-data collection procedures to enable the PICS' transferability to the German healthcare context (extensive translation process; two phases of cognitive interviews with intermittent and final revisions of the PICS-D; multiple virtual meetings with original authors to ensure original meanings of items; combining methodological and qualitative considerations in excluding items, etc.).
Our study has some limitations. Our sample size is at the lower limit of feasibility for psychometric testing. However, through intensive data management, we were able to ensure that the number of missing values was kept to a minimum to guarantee the feasibility of all our statistical analyses. Our assessment of the questionnaire's additional psychometrically important properties (e.g., other facets of construct validity, criterion validity, test-retest reliability, etc.) requires further methodological efforts. It is therefore essential to replicate the questionnaire's structure working with other samples, especially with regard to the factor structure, since factors with only two items are statistically problematic and should only interpreted with care (38, 39). The original PICS was developed in the US healthcare system context by relying on interviews and focus groups with patients and caregivers. The scanned literature contained various definitions of care integration (2, 4, 6, 8, 11–13, 20, 21, 37). Although these are similar in essence, we could not rule out that different latent IC facets are triggered when answering the PICS-D. To design a valid measurement instrument, it is essential to develop a profound theoretical basis. Further psychometric testing in other countries is needed to refine a theoretical IC framework in pediatric settings by considering different experiences in international health contexts. Our study may support the further development of just such a framework.
Conclusion
The PICS-D is the first German-language questionnaire to assess the integration of pediatric care. Thanks to this study's positive findings, we can recommend the use of the PICS-D. Ziniel and co-authors describe a broad range of applications for the original PICS (21). Accordingly, the PICS-D can also be used to identify gaps in care delivery, guide quality improvement efforts, or measure the impact of a care plan or care model. Used under consideration of its framework, the results generated from our study reveal benefits for researchers, decision-makers, and field practitioners alike.
Principal axis factoring after direct oblimin rotation. Item information was summarized in 3 factors: Team quality & communication (factor 1), Family impact (factor 2), and Access to care (factor 3). Values are standardized factor loading: a higher value indicates a strong correlation with the corresponding factor. Values greater or equal 0.40 are in italics.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics statement
The studies involving human participants were reviewed and approved by Ethik-Kommission, Albert-Ludwigs-Universität Freiburg. The patients/participants provided their written informed consent to participate in this study.
Author contributions
Initiation, conception, design of the research project was done by TL and EFG. Coordination of the research project was done by TL, EFG and JW. Material preparation, data collection and analysis were performed by all authors. The first draft of the manuscript was written by JW and all authors commented on previous versions of the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This study is being funded by the Innovationsausschuss of the Gemeinsamer Bundesausschuss, Wegelystraße 8, 10623 Berlin (grant number: 01VSF18005). The funding body was not involved in any aspect of the study's design, in collecting study data, in writing the manuscript, or in the decision to submit this article for publication.
Acknowledgments
We are grateful for the open exchange and helpful comments from the original authors of the PICS survey Richard Antonelli and Sonja Ziniel throughout the study. We also would like to thank Michaela Ruf for her assistance and valuable discussions in planning and developing this study. We acknowledge support by the Open Access Publication Fund of the University of Freiburg.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
CFA, confirmatory factor analysis; CFI, comparative fit index; EFA, exploratory factor analysis; FACIT, functional assessment of chronic illness therapy translation procedures and guidelines; IC, integrated care; KMO, kaiser-mayer-olkin coefficient; PICS, pediatric integrated care survey; PICS-D, german version of the pediatric integrated care survey; RMSEA, root mean square error of approximation; SMA-C+, name of the overall project in which the study took place (“SMA” for spinal muscular atrophy; “C” for CM; “+” for adding an IT component to CM); TLI, Tucker–Lewis index; Velicer's MAP, Velicer's minimum average partial.
References
1. Gerlach FM, Schaeffer D, Greiner W, Thürmann PA, Wille E, Haubitz M, et al. Wettbewerb an der schnittstelle zwischen ambulanter und stationärer gesundheitsversorgung. Bericht des sachverständigenrates zur begutachtung der entwicklung im gesundheitswesen. Bonn: NOMOS; 2012 (2012).
2. Sterly C, Hassler M. Integrierte versorgung. In: Thielscher CH, editors. Medizinökonomie. Wiesbaden: Gabler Verlag | Springer Fachmedien (2012). p. S.483–504.
4. Wolfe I, Lemer C, Cass H. Integrated care: a solution for improving children's Health? Arch Dis Child. (2016) 101(11):992–7. doi: 10.1136/archdischild-2013-304442
5. World Health Organisation. Integrated care models: An overview. Geneva, Switzerland: World Health Organisation (2016). Verfügbar unter: www.euro.who.int/__data/assets/pdf_file/0005/322475/Integrated-caremodels- overview.pdf
6. Singer SJ, Burgers J, Friedberg M, Rosenthal MB, Leape L, Schneider E. Defining and measuring integrated patient care: promoting the next frontier in health care delivery. Med Care Res Rev. (2011) 68(1):112–27. doi: 10.1177/1077558710371485
7. Goodwin N. Understanding integrated care. Int J Integr Care. (2016) 16(4):1–4. doi: 10.5334/ijic.2530. Verfügbar unter: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5354214/
8. Wolfe I, Satherley RM, Scotney E, Newham J, Lingam R. Integrated care models and child health: a meta-analysis. Pediatrics. (2020) 145(1):1–12. doi: 10.1542/peds.2018-3747. Verfügbar unter: https://pediatrics.aappublications.org/content/145/1/e20183747
9. Armitage GD, Suter E, Oelke ND, Adair CE. Health systems integration: state of the evidence. Int J Integr Care. (2009) 9(2):1–11. doi: 10.5334/ijic.316. Verfügbar unter: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2707589/
10. Schor EL. American Academy of pediatrics task force on the family. Family pediatrics: report of the task force on the family. Pediatrics. (2003) 111(6 Pt 2):1541–71.12777595
11. Antonelli R. Pediatric integrated care survey 1.0 user manual. Boston: Boston Children's Hospital (2015).
12. Antonelli R, Mcallister J, Popp J. Making care coordination a critical component of the pediatric health system: a multidisciplinary framework (2009). Verfügbar unter: https://www.commonwealthfund.org/publications/fund-reports/2009/may/making-care-coordination-critical-component-pediatric-health
13. Turchi R, Antonelli R, Norwood K, Adams R, Brei T. Burke R. Patient-and family-centered care coordination: a framework for integrating care for children and youth across multiple systems. Pediatrics. (2014) 133:E1451–60.24777209
14. Eikötter T, Greiner W. Instrumente zur messung der versorgungsqualität in der integrierten versorgung. Gesundheitsökonomie Qualitätsmanagement. (2008) 13(1):25–31. doi: 10.1055/s-2007-963333
15. Wolfe I. Health services for children with long-term conditions and non-communicable diseases. In: Wolfe I, McKee M, Herausgeber , editors. European Child health services and systems: lessons without borders. Maidenhead: Open University Press (2013). p. S.63–93.
16. Weatherly JN, Lägel R, Herausgeber . Neue versorgungsansätze in der psychiatrie, neurologie und psychosomatik. Berlin: Medizinisch Wissenschaftliche Verlagsgesellschaft (2009).
17. Asarnow JR, Rozenman M, Wiblin J, Zeltzer L. Integrated medical-behavioral care compared with usual primary care for child and adolescent behavioral health: a meta-analysis. JAMA Pediatr. (2015) 169(10):929–37. doi: 10.1001/jamapediatrics.2015.1141
18. Latour JM, Duivenvoorden HJ, Tibboel D, Hazelzet JA, EMPATHIC Study Group. The shortened EMpowerment of PArents in THe intensive care 30 questionnaire adequately measured parent satisfaction in pediatric intensive care units. J Clin Epidemiol. (2013) 66(9):1045–50. doi: 10.1016/j.jclinepi.2013.02.010
19. Girch A, Rippe RCA, Latour JM, Jönebratt Stocker M, Blendermann M, Hoffmann K. The German EMPATHIC-30 questionnaire showed reliability and convergent validity for use in an intermediary/general pediatric cardiology unit: a psychometric evaluation. Front Cardiovasc Med. (2022) 9:901260. doi: 10.3389/fcvm.2022.901260
20. Cohen E, Coller RJ. Evaluating integrated care for children: a clarion call or a call for clarity? Pediatrics. (2020) 145(1):1–2. doi: 10.1542/peds.2019-3282. Verfügbar unter: https://pediatrics.aappublications.org/content/145/1/e20193282
21. Ziniel SI, Rosenberg HN, Bach AM, Singer SJ, Antonelli RC. Validation of a parent-reported experience measure of integrated care. Pediatrics. (2016) 138(6):1–11. doi: 10.1542/peds.2016-0676
22. Noest S, Ludt S, Klingenberg A, Glassen K, Heiss F. Ose D. Involving patients in detecting quality gaps in a fragmented healthcare system: development of a questionnaire for Patients’ experiences across health care sectors (PEACS). Int J Qual Health Care. (2014) 26(3):240–9. doi: 10.1093/intqhc/mzu044
23. Hildebrandt H, Pimperl A, Schulte T, Hermann C, Riedel H. Schubert I. Triple aim—evaluation in der integrierten versorgung gesundes kinzigtal—gesundheitszustand, versorgungserleben und wirtschaftlichkeit. Bundesgesundheitsbl. (2015) 58(4):383–92. doi: 10.1007/s00103-015-2120-y
24. Klingenberg A, Bahrs O, Szecsenyi J. How do patients evaluate general practice? German results from the European project on patient evaluation of general practice care (EUROPEP). Zeitschrift für ärztliche Fortbildung und Qualitätssicherung. (1999) 93:437–45.
25. Braun S, Kreimeier S, Greiner W. Messung der patientenzufriedenheit in der integrierten versorgung—eine pilotstudie mit dem modifizierten ZAP-fragebogen. Zeitschrift für evidenz. Fortbildung und Qualität im Gesundheitswesen. (2010) 104(2):106–12. doi: 10.1016/j.zefq.2009.12.001
26. Bethge M, Bartel S, Streibelt M, Lassahn C, Thren K. Verbesserte behandlungsqualität durch integrierte versorgung bei knie- und hüftgelenkersatz: ergebnisse einer kontrollierten studie. Rehabilitation. (2011) 50(2):86–93. doi: 10.1055/s-0030-1265144
27. Willems J, Farin-Glattacker E, Langer T. Evaluation of a case management to support families with children diagnosed with spinal muscular atrophy—protocol of a controlled mixed-methods study. Front Pediatr. (2021) 9:614512. doi: 10.3389/fped.2021.614512
28. Eremenco SL, Cella D, Arnold BJ. A comprehensive method for the translation and cross-cultural validation of health status questionnaires. Eval Health Prof. Juni. (2005) 28(2):212–32. doi: 10.1177/0163278705275342
29. Willis GB. Cognitive interviewing: a tool for improving questionnaire design. California, USA: SAGE Publications (2004). 375 S.
30. R Core Team. R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing (2020). Verfügbar unter: https://www.R-project.org/
31. Velicer WF. Determining the number of components from the matrix of partial correlations. Psychometrika. (1976) 41:321–7. doi: 10.1007/BF02293557
32. Hooper D, Coughlan J, Mullen M. Structural equation modeling: guidelines for determining model fit. Electron J Bus Res Methods. (2007) 30:6.
33. Hu Lt, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling Multidiscip J. (1999) 6(1):1–55. doi: 10.1080/10705519909540118
34. Hjorth E, Kreicbergs U, Sejersen T, Jeppesen J, Werlauff U, Rahbek J. Bereaved parents more satisfied with the care given to their child with severe spinal muscular atrophy than nonbereaved. J Child Neurol. (2019) 34(2):104–12. doi: 10.1177/0883073818811544
35. Mastellos N, Gunn L, Harris M, Majeed A, Car J, Pappas Y. Assessing patients’ experience of integrated care: a survey of patient views in the north west London integrated care pilot. Int J Integr Care. (2014) 14:1–9. doi: 10.5334/ijic.1453
36. Altman L, Zurynski Y, Breen C, Hoffmann T, Woolfenden S. A qualitative study of health care providers’ perceptions and experiences of working together to care for children with medical complexity (CMC). BMC Health Serv Res. (2018) 18(1):70. doi: 10.1186/s12913-018-2857-8
37. Bautista MAC, Nurjono M, Lim YW, Dessers E, Vrijhoef HJ. Instruments measuring integrated care: a systematic review of measurement properties. Milbank Q. (2016) 94(4):862–917. doi: 10.1111/1468-0009.12233
38. Marsh HW, Hau KT, Balla JR, Grayson D. Is more ever too much? The number of indicators per factor in confirmatory factor analysis. Multivariate Behav Res. (1998) 33(2):181–220. doi: 10.1207/s15327906mbr3302_1
Keywords: chronic condition, reported outcome measures, integrated care, psychometric properties, chronic disease
Citation: Willems J, Bablok I, Sehlbrede M, Farin-Glattacker E and Langer T (2022) The German pediatric integrated care survey (PICS-D): Translation, adaptation, and psychometric testing. Front. Pediatr. 10:1057256. doi: 10.3389/fped.2022.1057256
Received: 29 September 2022; Accepted: 7 December 2022;
Published: 23 December 2022.
Edited by:
Nan Luo, National University of Singapore, Singapore© 2022 Willems, Bablok, Sehlbrede, Farin-Glattacker and Langer. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jana Willems amFuYS53aWxsZW1zQHVuaWtsaW5pay1mcmVpYnVyZy5kZQ==
†These authors share last authorship
Specialty Section: This article was submitted to Children and Health, a section of the journal Frontiers in Pediatrics
 Jana Willems
Jana Willems Isabella Bablok1
Isabella Bablok1 Thorsten Langer
Thorsten Langer