- Section of Orthopaedics and Traumatology, Department of Clinical Science and Traslational Medicine, University of Rome “Tor Vergata”, Rome, Italy
Background: Literature over the last 20 years provides evidence for a surgical treatment of displaced olecranon fractures in children, this is usually obtained with commonly proposed methods, although there is no general agreement about the best recommended technique.
Aim: Identifying the best surgical technique in displaced olecranon fractures in children and the role of associated fractures in the prognosis of these lesions, by analyzing the most relevant studies on this topic.
Methods: A literature search was performed in MEDLINE database and Scopus database. Articles reporting clinical outcomes of pediatric patients affected by olecranon fractures treated surgically were identified.
Results: The initial search produced 111 studies, with 8 fulfilling the eligibility criteria of our study. Selected articles (2002–2022) included 122 patients overall.
Conclusion: Displaced olecranon fractures, occurring during skeletal growth and surgically treated, generally have good results, although we are unable to recommend the best surgical treatment based on our review. In most cases, they are intra-articular fractures; thus, the overall goal is to get an anatomic reduction that in some cases cannot be obtained by percutaneous techniques. Tension band suture is the preferred device, although it is not recommended in adolescence for the high risk of fixation failure. Associated lesions may affect results.
Introduction
Fractures of the olecranon are rare and account for 5% of all elbow fractures during skeletal growth (1). These fractures generally occur between 5 and 10 years of age and the most common mechanism of injury is trauma onto either an outstretched hand or a flexed elbow; they are commonly associated with additional fractures of the radial head or the distal part of the humerus. Fractures with displacement greater than 2 mm generally require surgical treatment (2). In 2002, we reported a long-term follow-up study with an average follow-up of 23.8 years, on 39 cases, the majority of which were treated conservatively. We conclude that the long-term prognosis of olecranon fractures in children is related to the anatomic site of the fracture line, to the interfragmentary displacement and to the presence of an associated lesion that represent a negative prognostic factor (3). Classification of these rare lesions is still debated and to the best of our knowledge, there is no universally accepted classification in the literature. Generally, in all the classification systems reported, the possible presence of the intra-articular displacement more than 2 mm and the presence of associated injuries are considered (4, 5). In our study we proposed a classification in 5 types, on the basis of the anatomic site of the fracture line, the inter-fragmentary displacement and the presence of an associated lesion (3). There is general agreement that undisplaced or minimally displaced (less than 2 mm) fractures may be treated conservatively with good results, while displaced fractures need to be treated surgically. The most common methods of treatment proposed in the last 20 years are open reduction and internal fixation (ORIF) with tension band wiring or suture, open or percutaneous screw fixation and ORIF with plate and screws. The aim of our systematic review was to identify the best method of surgical treatment in displaced olecranon fractures in children and the role of associated fractures in the prognosis of these lesions.
Materials and methods
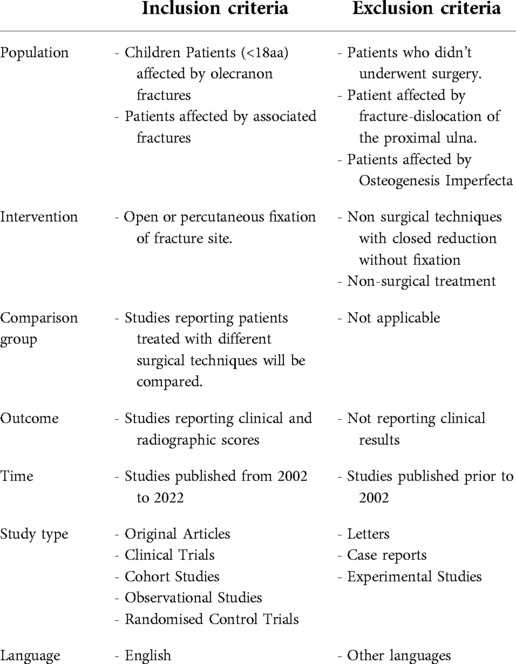
Inclusion and exclusion criteria were formulated according to the population, intervention, comparator, outcome (PICO) method and are summarized in Table 1 (6). Search strategy and sources of information: Authors of this review (PF, FM, GG, DC, AC, and CL) performed a literature search about the topic by querying Medline database, Scopus and Chocrane Library. The search strategy covers PICO and was performed independently by each author in July 2021. Keywords and Medical Subject Headings (MeSH) terms were identified by a preliminary search and selected by discussion. The search was conducted using the following keywords and their synonyms or MeSH Terms assembled in various combinations to obtain most pertinent articles: olecranon, fractures, children. The following is the list of all of the terms used and the Boolean operators used to combine them: ((“olecran*”[Title]) OR ((“olecranon process/injuries”[MeSH Terms] OR “olecranon process/surgery”[MeSH Terms] OR “olecranon process/therapy”[MeSH Terms]))) AND (“fractur”[All Fields] OR “fractural”[All Fields] OR “fracture's”[All Fields] OR “fractures, bone”[MeSH Terms] OR (“fractures”[All Fields] AND “bone”[All Fields]) OR “bone fractures”[All Fields] OR “fracture”[All Fields] OR “fractured”[All Fields] OR “fractures”[All Fields] OR “fracturing”[All Fields]) AND (“Child”[Mesh] OR “Adolescent”[Mesh] OR “Pediatrics”[Mesh] OR “Child*”[Title] OR “Pediatr*”[Title]).
A publication date filter was applied to select only articles and review articles from the last 20 years (ranging from 2002 to 2022). Language restriction filter was applied to identify only English articles.
The reviewers (PF, FM, GG, DC, AC, and CL) retrieved the data and independently analyzed each selected study; instances of disagreement were resolved by the senior investigator (PF).
The articles were screened for the presence of the following inclusion criteria: pediatric patients affected by olecranon fractures; patients treated with any surgical technique; studies providing an adequate level of evidence, including retrospective studies; availability of full text. The studies were excluded if they provided information regarding: patients affected by Osteogenesis Imperfecta or affected by fracture-dislocation of the proximal ulna; patients treated with non-surgical techniques or with closed reduction without fixation. Letters, Case reports or Experimental Studies and studies not reporting clinical results were also excluded.
Results
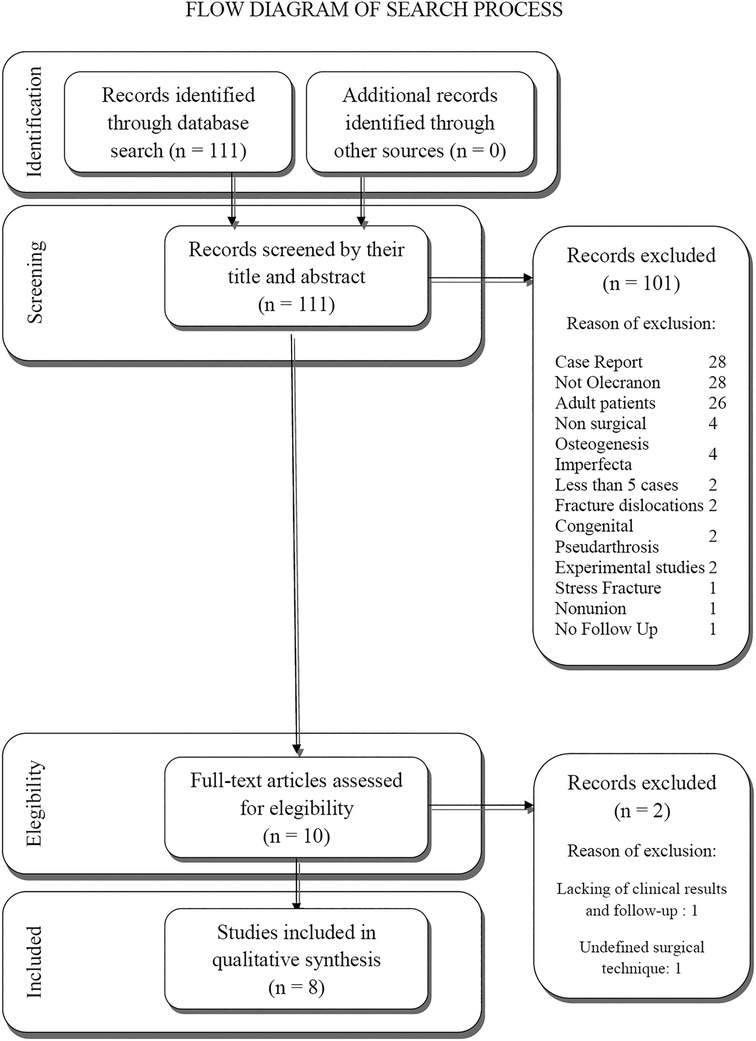
The initial search produced 111 studies. After a first screening, by reading title and abstract and evaluation based on inclusion and exclusion criteria, articles were screened and only 10 studies fulfilled the eligibility criteria of our study. The other studies were excluded for the following reasons: 28 were Case Reports; 28 reported fractures not involving olecranon; 26 were about adult patients; 4 didn't report surgical treatment; 4 reported cases affected by osteogenesis imperfecta; 2 reported less than 5 cases; 2 reported fracture dislocations; 2 reported cases affected by congenital pseudoarthrosis; 2 were experimental studies; 2 reported stress fracture; 1 reported nonunion; 1 didn't report follow-up.
After screening the full text of the remaining 10 articles, we excluded 2 more articles which lacked follow-up measure, clinical outcomes and reported unspecified surgical technique. In conclusion, a total of 8 articles were enrolled in the present review (Figure 1 shows the flowchart for study selection). All the selected articles were published from 2002 to 2022 and included 122 patients overall. Table 2 presents a list of the studies, summarizing the number of patients, classification of fracture, associated lesions, age at surgery, surgical technique performed, length of follow-up, results and conclusions.
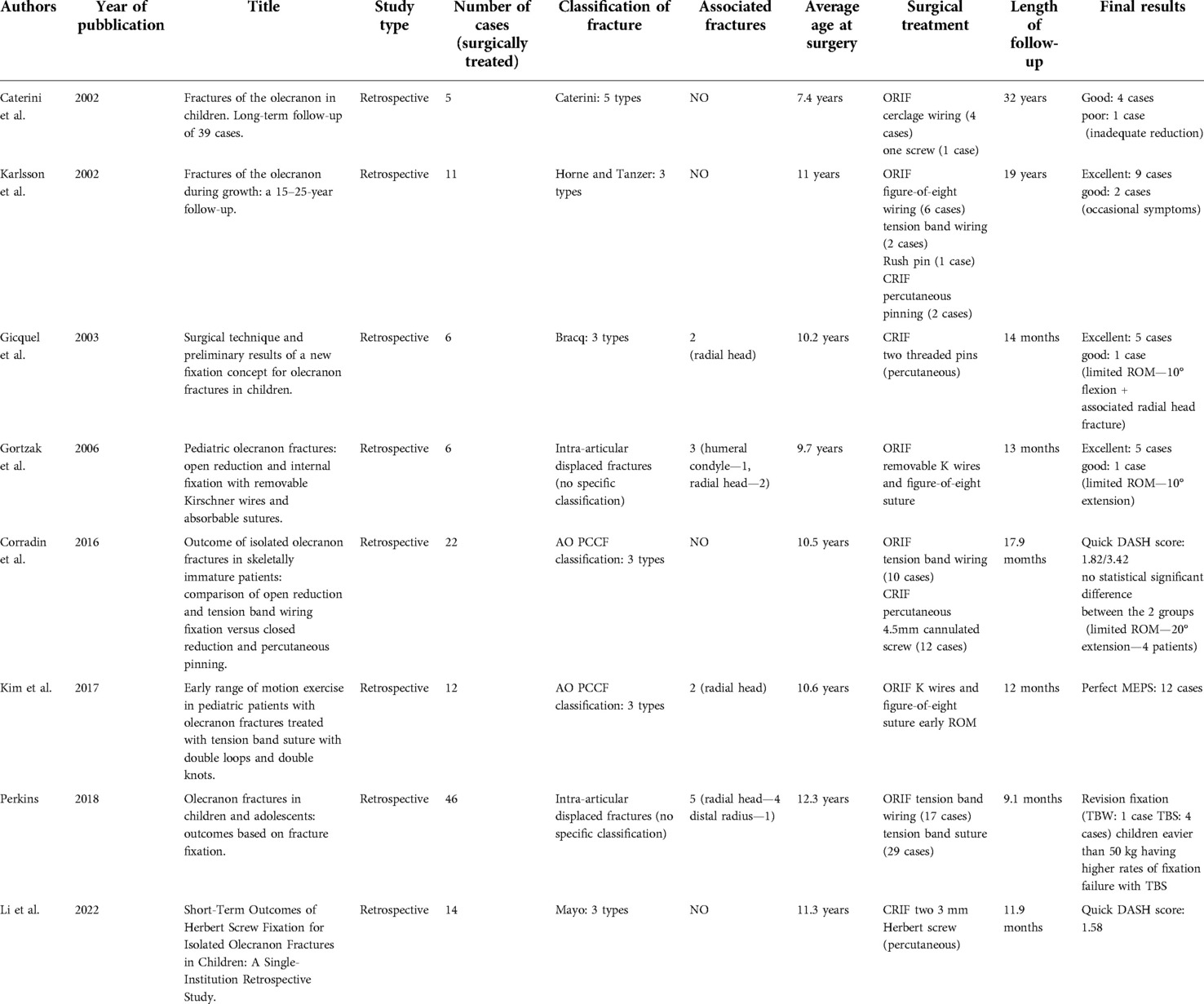
Table 2. This table presents a list of the included studies, summarizing the number of patients, classification of fracture, associated lesions, age at surgery, surgical technique performed, length of follow-up, results and conclusions.
Discussion
Surgical treatment of displaced olecranon fractures in children is still debated. On the contrary, conservative treatment is usually adopted in non-displaced or minimally displaced fractures with good results. Generally, the majority of authors considered minimally displaced olecranon fractures when the interfragmentary gap is more that 2–3 mm.
In this systematic review, we analyzed the clinical and radiological results obtained in 122 children treated surgically, from eight clinical and radiological studies published in the last 20 years. All these studies were retrospective and the majority of them had a short-term follow-up. The surgical techniques commonly reported are open or closed reduction followed by internal fixation using various devices. Tension band wiring (TBW), tension band suture (TBS) and cerclage techniques are the most common devices used after open reduction while screws or pins are generally applied percutaneously after closed reduction.
Usually, the classification systems are proposed to help guide treatment; however, in regards to olecranon fractures in pediatric patients, several classifications have been reported, without any demonstrating superiority over the others. The adopted classifications in our review are the following: Caterini et al. who proposed five different fracture types (3), on the basis of the anatomic site of the fracture line (7), interfragmentary displacement and presence of an associated lesion (5); Horne and Tanzer, who proposed three types, depending on location of the fracture on the olecranon (8); AO PCCF, based on the morphology of the fracture (9) and Mayo classification (10) in three types, described for adults fractures, based on fracture displacement and elbow stability (11). In two papers no specific classification is reported; the authors had surgically treated all intra-articular displaced olecranon fractures. These data confirm that, there is still no classification commonly adopted for olecranon fractures in children that suggests the best treatment to adopt.
The majority of papers included in the review are short-term follow-up studies. Gicquel et al. reported the preliminary results of a new percutaneous fixation technique to stabilize six olecranon fractures using two threaded pins introduced by a minimal skin incision with a divergent orientation. Only in two cases, the interfragmentary displacement was more than 2 mm. The authors observed excellent result in all patients but one, which was associated with a radial head fracture and mild limited range of motion of the elbow was present. They concluded that their technique can be used routinely because of its effectiveness and simplicity (12). Recently Li et al. reported another short-term follow-up study on 14 cases treated percutaneously using two cannulated Herbert screws with a different direction (13). All the fractures included in the study had a displacement more than 4 mm that were closed reduced, before percutaneous fixation. The authors observed good functional and radiological results in all patients, evaluated with a quickDASH scoring system. The authors strongly recommend the percutaneous technique, to avoid skin complications and hardware irritation causing persistent joint pain, requiring hardware removal. Moreover they underlined the ease of screws removal performed by small incisions. On the contrary, other authors prefer to perform an open reduction; Gortzak et al. in 2006 (14) and more recently Kim et al. in 2017 (15), reported 6 and 12 olecranon fractures respectively, treated by open reduction and internal fixation with two K-wires and figure-of-eight suture. Both papers reported excellent results at an average of 1 year after treatment, except in one case in which the authors observed a limited elbow extension of 10°. Gortzak et al., suggest leaving the two Kirschner wires out of the skin to perform a quick removal of the devices after fracture healing. The authors emphasize their technique that avoid a reoperation for hardware removal. Kim et al., instead emphasize the early range of motion exercise after stabilization fracture performed by tension band suture with double loops and knots (15). Perkins et al. reported 46 olecranon fractures in children and adolescents comparing 17 patients treated by open reduction and tension band wiring and 29 patients treated by open reduction and tension band suture. The authors, who report the largest series of olecranon fractures included in our review, concluded that tension band suture is contraindicated in patients weighting more than 50 kg; in fact, they observed their failures in older and heavier patients (4 cases) (16). Corradin et al. reported a comparison of open reduction and tension band wiring fixation performed in 10 cases versus closed reduction and percutaneous screw fixation performed in 12. The authors, while reporting a difference regarding the quickDASH score at follow-up between the two groups (1.82 in the open series versus 3.42 in the closed series), concluded that no statistically significant differences were present between the two groups, with equally acceptable clinical and radiological final results and similar rate of complications (17).
Only two papers with a long-term follow-up have been published in the last 20 years. Caterini et al. reported only 5 cases of surgically treated patients and concluded that the long-term prognosis of olecranon fractures in children is related to the anatomic site of the fracture line, to the interfragmentary displacement and to the presence of an associated lesion. They observed only one case with poor result related to an inadequate reduction and fixation (3). Karlsson et al. reported 11 olecranon fractures surgically treated and observed that none of their patient developed nonunion or elbow osteoarthritis, therefore they conclude that olecranon fractures during growth have an excellent long-term results (18).
In four studies of our review associated lesions are reported, most of them are radial head fractures that can affect the final result (3, 14).
In conclusion, based on our review, displaced olecranon fractures occurring during skeletal growth surgically treated with various techniques generally have good results, although we are unable to recommend the best surgical treatment to perform. However, we believe that since they are intra-articular fractures in the majority of cases, the overall goal is to get an anatomic reduction that in some cases cannot be obtained using a percutaneous technique. Regarding the devices, tension band suture is preferred but remains contraindicated in adolescence for the high risk of fixation failure. Associated lesions may affect the final result.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author contributions
FM: data collection, manuscript preparation, data analysis. GG: study conception and design, data collection, manuscript preparation and editing. AC: data analysis, manuscript preparation. CL: data collection, manuscript preparation. DC: data collection, manuscript preparation. PF: study conception and design, manuscript preparation and editing, analysis and interpretation of data. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the Department of Clinical Science and Translational Medicine of University of Roma Tor Vergata.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Landin LA, Danielsson LG, Wattsgard C. Transient synovitis of the hip. Its incidence, epidemiology and relation to perthes’ disease. J Bone Joint Surg Br. (1987) 69(2):238–42. doi: 10.1302/0301-620X.69B2.3818754
2. Andreacchio A, Canavese F, Villa R. The child elbow. Practical approach to traumatic and orthopedic disorders. Como, Italy: Timeo (2020).
3. Caterini R, Farsetti P, D'Arrigo C, Ippolito E. Fractures of the olecranon in children. Long-term follow-up of 39 cases. J Pediatr Orthop B. (2002) 11(4):320–8. doi: 10.1097/00009957-200210000-00010
4. Matthews J. Fractures of the olecranon in children. Injury. (1980) 12(3):207–12. doi: 10.1016/0020-1383(80)90009-1
5. Evans MC, Graham HK. Olecranon fractures in children: part 1: a clinical review: part 2: a new classification and management algorithm. J Pediatr Orthop. (1999) 19(5):559. doi: 10.1097/00004694-199909000-00001
6. Riva JJ, Malik KM, Burnie SJ, Endicott AR, Busse JW. What is your research question? An introduction to the PICOT format for clinicians. J Can Chiropr Assoc. (2012) 56(3):167–71.22997465
7. Bracq H. Fractures of the olecranon. Rev Chir Orthop Reparatrice Appar Mot. (1987) 73(6):469–71.3432642
8. Horne J, Tanzer T. Olecranon fractures: a review of 100 cases. J Trauma. (1981) 21(6):469–72.7230301
10. BF M. Current concepts in the treatment of fractures of the radial head, the olecranon, and the coronoid. JBJS. (1995) 77(2):316–27. doi: 10.2106/00004623-199502000-00019
11. Cabanela M, Morrey B. The elbow and its disorders. Fractures of the proximal ulna and olecranon. 2nd ed. Philadelphia: WB Sauners Co. (1993). 405–8.
12. Gicquel P, Giacomelli MC, Karger C, Clavert JM. Surgical technique and preliminary results of a new fixation concept for olecranon fractures in children. J Pediatr Orthop. (2003) 23(3):398–401.12724609
13. Li Y, Wang K, Sun D, Liu Y, Wang Z, Li A. Short-Term outcomes of herbert screw fixation for isolated olecranon fractures in children: a single-institution retrospective study. Indian J Orthop. (2022) 56(7):1174–80. doi: 10.1007/s43465-022-00609-4
14. Gortzak Y, Mercado E, Atar D, Weisel Y. Pediatric olecranon fractures: open reduction and internal fixation with removable kirschner wires and absorbable sutures. J Pediatr Orthop. (2006) 26(1):39–42. doi: 10.1097/01.bpo.0000187988.86892.a2
15. Kim TH, Lee DH, Han KJ, Choi WS, Cho JH. Early range of motion exercise in pediatric patients with olecranon fractures treated with tension band suture with double loops and double knots. J Shoulder Elbow Surg. (2017) 26(7):e227–e31. doi: 10.1016/j.jse.2017.03.004
16. Perkins CA, Busch MT, Christino MA, Axelrod J, Devito DP, Fabregas JA, et al. Olecranon fractures in children and adolescents: outcomes based on fracture fixation. J Child Orthop. (2018) 12(5):497–501. doi: 10.1302/1863-2548.12.180029
17. Corradin M, Marengo L, Andreacchio A, Paonessa M, Giacometti V, Samba A, et al. Outcome of isolated olecranon fractures in skeletally immature patients: comparison of open reduction and tension band wiring fixation versus closed reduction and percutaneous screw fixation. Eur J Orthop Surg Traumatol. (2016) 26(5):469–76. doi: 10.1007/s00590-016-1774-y
Keywords: olecranon, fracture, children, surgery, upper limb, surgical procedures, surgical treament, pediatric
Citation: De Maio F, Gorgolini G, Caterini A, Luciano C, Covino D and Farsetti P (2022) Treatment of olecranon fractures in childhood: A systematic review. Front. Pediatr. 10:1046243. doi: 10.3389/fped.2022.1046243
Received: 16 September 2022; Accepted: 24 October 2022;
Published: 18 November 2022.
Edited by:
Federico Canavese, Centre Hospitalier Regional et Universitaire de Lille, FranceReviewed by:
Giulio Maccauro, Agostino Gemelli University Polyclinic (IRCCS), ItalyNicola Portinaro, University of Milan, Italy
© 2022 De Maio, Gorgolini, Caterini, Luciano, Covino and Farsetti. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Pasquale Farsetti ZmFyc2V0dGlAdW5pcm9tYTIuaXQ=
Specialty Section: This article was submitted to Pediatric Orthopedics, a section of the journal Frontiers in Pediatrics
 Fernando De Maio
Fernando De Maio Pasquale Farsetti
Pasquale Farsetti