- 1Department of Otolaryngology-Head and Neck Surgery, Shanghai Children's Hospital, School of Medicine, Shanghai Jiao Tong University, Shanghai, China
- 2Department of Pathology, Shanghai Children's Hospital, School of Medicine, Shanghai Jiao Tong University, Shanghai, China
Objective: To explore the clinical characteristics and surgical treatment of children with bronchogenic cysts (BCs) in the head and neck region.
Methods: A retrospective study of 10 pediatric patients with BCs in the head and neck region treated in Shanghai Children's Hospital during 2011 to 2022 was performed.
Results: Based on their pathological diagnosis, 10 patients with BCs in the head and neck were identified. The most common location was the neck (8 patients, 80%; 2 midline neck, 6 lateral neck), followed by the ventral tip of tongue (1 patient), and the posterior pharyngeal wall (1 patient). Misdiagnosed as lymphangioma in 5 cases, cyst in 3 cases, thyroglossal duct cyst (TGDC) in 2 cases and congenital pyriform sinus fistula (CPSF) in 1 case preoperative. The median follow-up period after surgery was 4.68 (range, 0.67–9.25) years. All 10 patients underwent complete resection without recurrence or other complications.
Conclusions: Although extremely rare, BCs should be considered in the differential diagnosis of midline and lateral neck masses or intraoral cysts in children. Surgical excision is recommended in BCs, and the diagnosis is definitively confirmed by histopathology.
Introduction
Bronchogenic cysts (BCs) are thought to be formed by small buds of diverticula that separate from the foregut during formation of the tracheobronchial tree (1). BCs are rare congenital diseases with an incidence rate of 1/42,000–68,000 (2). According to the location of the lesion, they can be divided into three types: intrapulmonary type, mediastinal type and ectopic type.
More than 99% of the patients occur in the mediastinum and lungs, while less than 1% affect in the head and neck (1, 3). Preoperative diagnosis of BCs in the head and neck region remain challenging (3). The location of a bronchogenic cyst (BC) varies greatly. Because of its rarity, it is often misdiagnosed as a more common congenital neck cyst (3, 4). Herein, we retrospectively analyzed the clinical features and surgical treatment results of children with head and neck BCs.
Materials and methods
In the present study, we performed a retrospective review of 10 patients presenting with cystic masses in the head and neck region who were histopathological diagnosed with BCs between January 2011 to January 2022. The children were identified from the Department of Otolaryngology Head and Neck Surgery at Shanghai Children's Hospital. Cases were assessed by parameters including age at diagnosis, gender, clinical symptoms, symptoms duration, misdiagnosis history, infection and treatment history, location and size of the BCs, diagnostic methods, treatment method, operative notes, postoperative complications, histopathological diagnosis, length of the follow-up, and recurrence. All patients with BCs received surgical treatment. This study was approved by our institutional Research Ethics Board (Approval No: 2022R067-E01).
Results
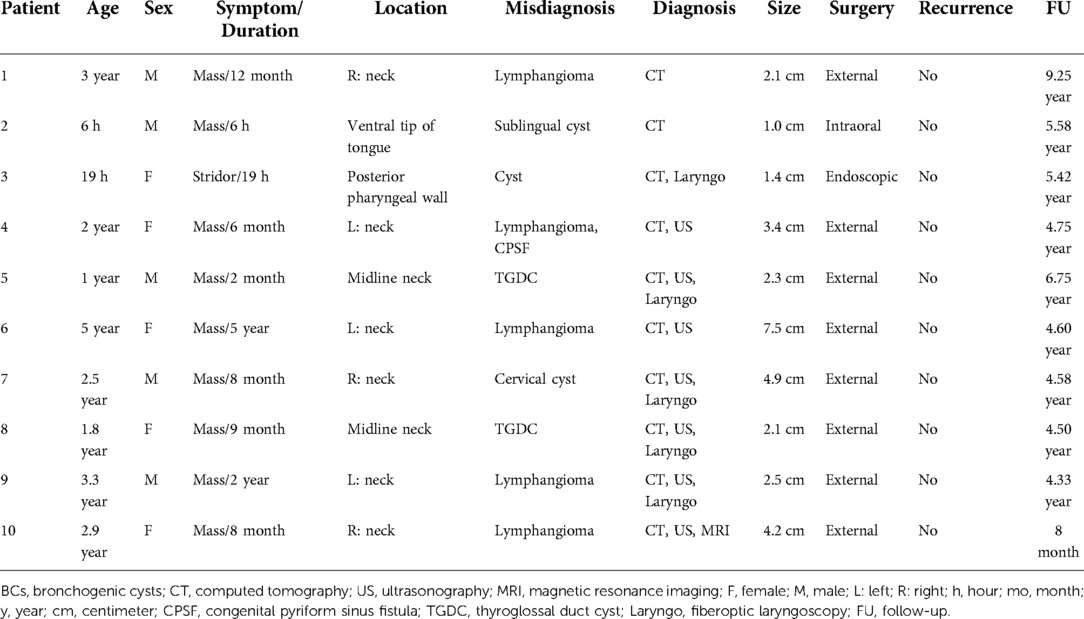
There were 10 patients (5 males and 5 females; age range, 6 h–5 years; median, 2.25 years) in this study (Table 1). Seven patients presented with asymptomatic masses in the neck. One patient (1.8-year-old female) had a history of recurrent infection in the midline neck, and had undergone incision and drainage. One newborn showed stridor after birth, and fiberoptic laryngoscopy revealed a mass in the posterior pharyngeal wall (Figure 1). The remaining 1 patient was incidentally diagnosed by routine physical examination (Figure 2). The duration of symptoms was 6 h to 5years (median, 8 months). Misdiagnosed as lymphangioma in 5 cases, cyst in 3 cases, TGDC in 2 cases and CPSF in 1 case before operation.
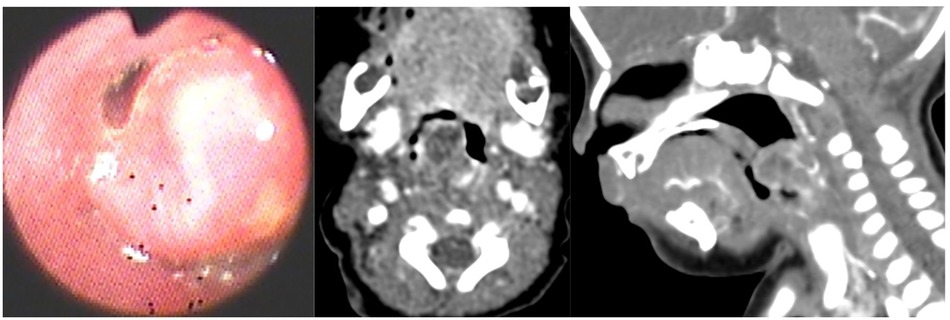
Figure 1. A 19-hour-old female. (A) Fiberoptic laryngoscopy showed a large globular mass (white arrow) with a smooth mucosal surface in the posterior pharyngeal wall. CT revealed a 1.4-cm sized cystic lesion in the posterior pharyngeal wall (red circle): (B) axial contrast-enhanced CT; (C) sagittal contrast-enhanced CT.
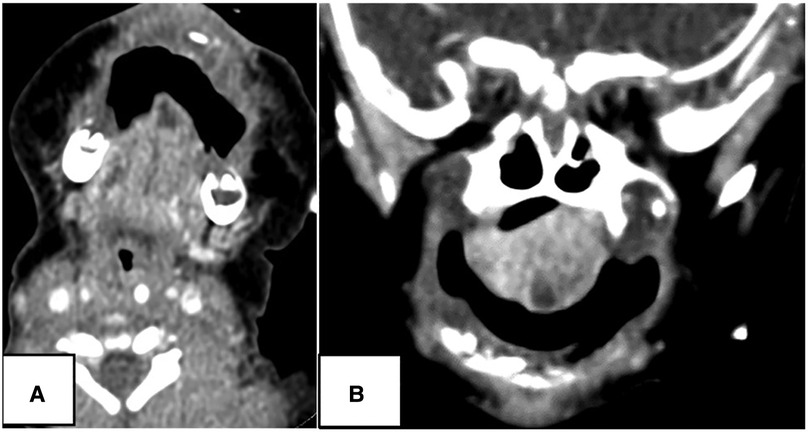
Figure 2. A 6-hour-old Male. CT showed a 1.0-cm sized cystic lesion in the ventral tip of tongue (white arrow): (A) contrast-enhanced axial scan; (B) coronal scan.
The most common location of BCs was the neck (8 cases, 80%; 2 midline neck, 6 lateral neck), followed by the ventral tip of tongue (1 case, 10%), and the posterior pharyngeal wall (1 case, 10%). The size of the cysts ranged from 1 to 7.5 (median, 2.3) cm. Contrast enhanced computed tomography (CT) was performed in 10 cases, ultrasound (US) in 7 cases, and magnetic resonance imaging (MRI) in 1 case to determine the extent of the cyst and exclude other diseases. Uncooperative patients were given 10% chloral hydrate (0.5 ml/kg) orally prior to the CT examinations.
All 10 patients with head and neck BCs received surgical treatment. Eight cases underwent external cervical approach under general anesthesia. The remaining 2 patients underwent intraoral and endoscopic surgery under general anesthesia. All patients with BCs were confirmed by histopathology.
All cases were cured without complications and no recurrence during follow-up. The median follow-up period after surgery was 4.68 (range, 0.67–9.25) years.
Discussion
At the third week of the embryo, the foregut undergoes dichotomous development. The ventral side forms the respiratory tract, and the dorsal side forms the esophagus, duodenum and stomach. During the development of tracheobronchial trees, developmental defects and abnormal division can lead to the formation of BCs (1, 2). BCs are rare congenital malformations that usually occur in the lung parenchyma or mediastinum (4, 5). However, BCs appear in the neck are particularly rare (2, 6). Previous reports have described that the positions of BCs in the head and neck are variable, from the oral cavity to the midline and lateral neck regions (3, 7). Lee DH (3) reported that clinicians should be aware that BCs in the head and neck may exist in many locations, such as the soft palate, the posterior pharyngeal wall, the floor of the mouth, and the arytenoid cartilage. In our studies, 7 cases were located in the neck, 1 case in the tongue and 1 case in the posterior pharyngeal wall, which was consistent with the literature.
BCs in the head and neck region are usually asymptomatic cystic lesions, and most cases are found during physical examinations (8), unless they are large enough to cause compression of the surrounding tissue or secondarily infected (9). In some individuals, large cysts may cause respiratory distress, wheezing, cough, dyspnea, and dysphagia (8). If the cyst is shallow, it may lead to sinus formation and external drainage of pus. If the cyst is deep, it may lead to abscess formation (1, 10, 11). In our series, 7 cases showed asymptomatic neck mass, 1 case had secondary infection of neck mass and underwent incision and drainage. One case had stridor after birth, and a posterior pharyngeal wall mass was found by fiberoptic laryngoscopy. There was 1 case incidentally diagnosed by physical examination. The clinical symptoms in our study were consistent with the above-mentioned cyst characteristics.
Although physical examination is the most important factor in diagnosis, assistant examination can provide valuable information for the evaluation of congenital cervical masses, especially in children (5). US, CT, and MRI are helpful in the diagnosis of BCs (3, 9). US typically shows a unilocular cystic lesion filled with fluid (4).
CT and MRI are more helpful to detect the extent of the lesion and determine the relationship between the lesion and the surrounding anatomical structure, which also helps to formulate the surgical strategy (3, 9, 12). CT is convenient and fast, while MRI examination takes a long time and costs high. For these reasons, we generally perform enhanced CT scans. BCs are usually round or oval lesions with smooth edges, uniform density, or air-liquid level due to repeated infection. However, there are currently no specific imaging standards for BC (13), although imaging methods are useful in the case of planning the surgery (10). In this study, a 1.8-year-old female and a 1-year-old male, our preoperative diagnosis were TGDC around the hyoid bone (Figure 3). Therefore, the location of BCs cannot be used to make a final diagnosis (3). Due to the low incidence rate, the rates of misdiagnosis and missed diagnosis are high preoperative (8). The differential diagnosis of BCs in the head and neck region contains TGDC, branchial cleft cyst, lymphangioma, dermoid cyst/epidermoid cyst, cervical thymic cyst, and thyroid cyst (3, 10). That is to say, the diagnosis of BC requires exclusion of all cystic masses in the neck. In the present study, 5 cases were misdiagnosed as lymphangioma, 3 cases as cyst, 2 cases as TGDC, and 1 case as CPSF before surgery (Figures 3–5). The head and neck lymphatic malformations (HNLMs) are usually diagnosed within 2 years old, almost half of which occur in neonates, and usually occur in the posterior triangle of the neck (14). CT findings of HNLMs were mostly poorly defined, multilocular and low-density masses (15, 16). Fluid-fluid levels can be seen in some patients with intracystic hemorrhage (17) TGDC usually occurs in the anterior midline of the neck, at the level of the hyoid bone, and connects with it (18). The first branchial cleft anomalies (CFBCAs) often presented with repeated swelling and purulence in Pochet's triangle. CT showed round, tubular or strip-shaped abnormal low-density shadow with unclear boundary in the parotid region, extending outward to the skin surface or EAC (19). The typical CT features of congenital second branchial cleft anomalies (CSBCAs) include isolated and uniform low-density cystic masses surrounded by uniformly thin, smooth walls. CSBCAs are generally located at the anteromedial border of the sternocleidomastoid muscle, posterior to the submandibular gland, and lateral to the carotid sheath (20, 21). The main clinical manifestations of CPSF are recurrent suppurative thyroiditis and neck abscess, predominantly located on the left sided (22). CT revealed the shallower or disappearing pyriform sinus, large cystic lesion with fluid and air, association or obscuration of the left superior thyroid lobe with the neck mass or abscess, tubular structures seen inside the thyroid and air-containing ducts originating from the piriform fossa (23, 24).
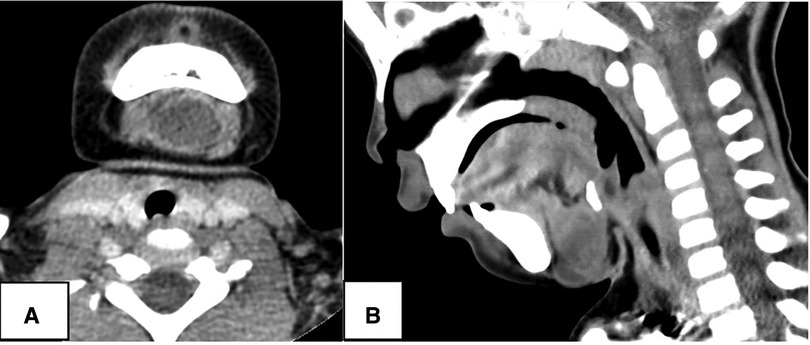
Figure 3. A 1.8-year-old female. CT showed a 2.1-cm sized cystic lesion in the midline neck connecting with hyoid bone (red circle), and misdiagnosed as thyroglossal duct cyst: (A) contrast-enhanced axial scan; (B) sagittal scan.

Figure 4. A 3.3-year-old Male. CT showed a 1.5-cm sized homogeneous, low-density mass in the left neck region (white arrow), and located anterolaterally of thyroid. CT showed that the left thyroid was compressed and deformed. This case was misdiagnosed as lymphangioma preoperative.
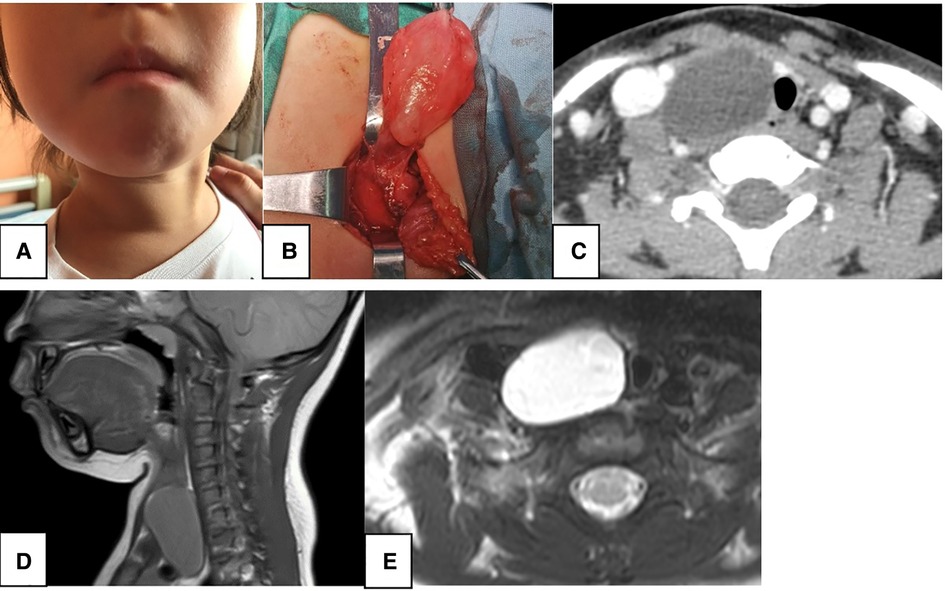
Figure 5. A 2.9-year-old female. CT showed a 4.2-cm sized homogeneous, low-density mass (C, white arrow) with thin walls and smooth borders in the right neck region without enhancement, and misdiagnosed as lymphangioma. The right thyroid was compressed and deformed, and the trachea (C,E, red circle) shifted to the opposite side. MRI showed low signal intensity on T1WI (D, white arrow) and high signal intensity on T2WI (E, white arrow). (A) preoperative neck mass; (B) intraoperative mass; (C) axial contrast-enhanced CT; (D) sagittal T1WI MRI; (E) axial T2WI MRI.
It was difficult to distinguish this disease from other diseases by preoperative imaging alone (8). Therefore, histopathological examination is critical to the final diagnosis of BCs (3, 4, 8, 25). The wall structure of BCs is the same as that of bronchial wall. A typical BC shows ciliated pseudostratified cubic columnar epithelium with underlying fibrous connective walls. Sometimes, variations may occur, such as the presence of cartilage, smooth muscle and seromucous glands (2, 3). The presence of cartilage is a necessary condition for the diagnosis of a BC (1). The cysts are typically filled with clear fluid, air or hemorrhagic secretions (26, 27). In this study, the postoperative pathological analysis was consistent with the above cyst characteristics of BCs (Figure 6).
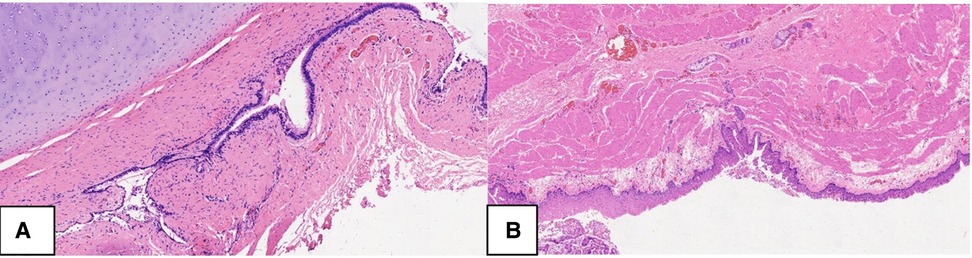
Figure 6. Histopathology of bronchogenic cyst. The inner layer of BC originates from the respiratory system and is covered by pseudostratified columnar ciliated epithelium on the fibrous connective tissue wall, which contains the cartilage plates, (A. HE, 100X), seromucous glands and smooth muscle (B. HE, 50X). pseudostratified columnar ciliated epithelium, PCCE; fibrous connective tissue wall, FCTW; seromucous glands, SG; smooth muscle, SM.
Due to the risk of malignant transformation and complications, surgical resection is the most effective method to treat a BC in the head and neck (8, 9). Once a BC is suspected, surgical excision should be undertaken as soon as possible (8, 28, 29). BCs of the head and neck usually do not recur after complete resection (4). In this study, there was no recurrence or complications resulting from the surgical intervention observed.
However, this study only included a small number of patients, so more cases need to be studied in the future to confirm the study results.
Conclusion
BCs are extremely rare congenital malformations, in addition, they can occur at various sites of the head and neck. As a result, BCs should be considered in the differential diagnosis of lateral and midline cervical masses or intraoral cysts. The definitive diagnosis, however, depends on the histopathological examination. We should perform surgical treatment as soon as possible, as surgery is the most effective method to treat a BC.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics statement
The studies involving human participants were reviewed and approved by Approval Letter of Ethics Review Committee, Children's Hospital of Shanghai/Shanghai Children's Hospital, Shanghai Jiao Tong University (Approval No: 2022R067-E01). Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin. Written informed consent was obtained from the minor(s)' legal guardian/next of kin for the publication of any potentially identifiable images or data included in this article.
Author contributions
All authors contributed to the article and approved the submitted version.
Funding
Shanghai Shenkang Hospital Development Center Municipal Hospital Clinical Research Cultivation Project (SHDC12019X21).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Aldawood Z, Moyer DJ, Woo SB. A bronchogenic cyst masquerading as a tongue mass. Head Neck Pathol. (2021) 15:1404–8. doi: 10.1007/s12105-021-01303-x
2. Cohn JE, Rethy K, Prasad R, Mae Pascasio J, Annunzio K, Zwillenberg S. Pediatric bronchogenic cysts: a case series of six patients highlighting diagnosis and management. J Invest Surg. (2020) 33:568–73. doi: 10.1080/08941939.2018.1527419
3. Lee DH, Yoon TM, Lee JK, Lim SC. Bronchogenic cyst in the head and neck region. J Craniofac Surg. (2017) 28:e303–e5. doi: 10.1097/SCS.0000000000003508
4. Kiralj A, Vuckovic N, Mijatov I. Congenital cervical bronchogenic cyst: a case report. Srp Arh Celok Lek. (2015) 143:317–21. doi: 10.2298/sarh1506317k
5. Wang Y, Kvit AA, Li X. Foregut duplication cysts in the head and neck: a case report and literature review. Clin Pediatr. (2016) 55:1248–51. doi: 10.1177/0009922815614356
6. Al-Balushi Z, Ehsan MT, Al Sajee D, Al Riyami M. Scapular bronchogenic cyst: a case report and literature review. Oman Med J. (2012) 27:161–3. doi: 10.5001/omj.2012.33
7. Mattingly JK, Arganbright JM, Lovell MA, Chan KH. Cervical bronchogenic cysts: case report and review of the literature. Am J Otolaryngol. (2014) 35:655–7. doi: 10.1016/j.amjoto.2014.06.015
8. Xu Y, Han F, Seng D, Jiang L, Wang S, Ni X, et al. A clinical analysis of pharyngeal bronchogenic cysts in the pharynx of children. Front Pediatr. (2021) 9:629009. doi: 10.3389/fped.2021.629009
9. Liu Z, Tian Z, Zhang C, He Y. Ectopic congenital bronchogenic cyst accompanied by infection appearing in the cervical region of an elderly female patient: a case report. Oncol Lett. (2016) 11:1065–8. doi: 10.3892/ol.2015.4022
10. Mumtaz A, Dhanani R, Faisal M, Maqbool H, Iqbal Khan A. Bronchogenic cyst in the cervical region: a rare entity - A case report and review of the literature. Cureus. (2021) 13:e14413. doi: 10.7759/cureus.14413
11. Huang CM, Huang FL, Chien YL, Chen PY. Deep neck infections in children. J Microbiol Immunol Infect. (2017) 50:627–33. doi: 10.1016/j.jmii.2015.08.020
12. Bian B, Yu M, Liu S, Li S, Wei Y, Zhang B. A suprasellar bronchogenic cyst: a case report. Medicine. (2019) 98:e16650. doi: 10.1097/MD.0000000000016650
13. Li Y, Wang S, Tai J, Zhang J, He L, Zhang N, et al. Surgical experiences of pediatric cervical bronchogenic cysts: a case series of 6 patients. Ear Nose Throat J. (2021):145561320982194. doi: 10.1177/0145561320982194
14. Thorburn C, Price D. Expectant management of pediatric lymphatic malformations: a 30-year chart review. J Pediatr Surg. (2022) 57:883–7. doi: 10.1016/j.jpedsurg.2021.12.053
15. Scuglia M, Conforti A, Valfre L, Totonelli G, Iacusso C, Iacobelli BD, et al. Operative management of neonatal lymphatic malformations: lesson learned from 57 consecutive cases. Front Pediatr. (2021) 9:709223. doi: 10.3389/fped.2021.709223
16. Demirag Evman M, Aydin S. A giant cervical lymphangioma. J Craniofac Surg. (2019) 30:e275–e6. doi: 10.1097/SCS.0000000000005363
17. Li W, Xu H, Zhao L, Li X. The management of giant cerviofacial lymphatic malformations in children. J Craniofac Surg. (2019) 30:e553–e5. doi: 10.1097/SCS.0000000000005520
18. Frauenfelder C, Shelmerdine SC, Simcock IC, Hall A, Hutchinson JC, Ashworth MT, et al. Micro-CT imaging of pediatric thyroglossal duct cysts: a prospective case series. Front Pediatr. (2021) 9:746010. doi: 10.3389/fped.2021.746010
19. Liu W, Chen M, Liu B, Zhang J, Ni X. Clinical analysis of type II first branchial cleft anomalies in children. Laryngoscope. (2021) 131:916–20. doi: 10.1002/lary.29049
20. Kawaguchi M, Kato H, Aoki M, Kuze B, Hara A, Matsuo M. CT And MR imaging findings of infection-free and benign second branchial cleft cysts. Radiol Med. (2019) 124:199–205. doi: 10.1007/s11547-018-0959-3
21. Adams A, Mankad K, Offiah C, Childs L. Branchial cleft anomalies: a pictorial review of embryological development and spectrum of imaging findings. Insights Imaging. (2016) 7:69–76. doi: 10.1007/s13244-015-0454-5
22. Ishinaga H, Kobayashi M, Qtsu K, Nishida K, Sakaida H, Kitano M, et al. Endoscopic electrocauterization of pyriform sinus fistula. Eur Arch Otorhinolaryngol. (2017) 274:3927–31. doi: 10.1007/s00405-017-4713-6
23. Chen W, Chen J, Chen F, Wu J, Zhao L, Xu H, et al. Endoscopic coblation treatment for congenital pyriform sinus fistula in children. Medicine. (2021) 100:e25942. doi: 10.1097/MD.0000000000025942
24. Li L, Zhao DJ, Yao TY, Xiang YH, Liu H, Ma QH, et al. Imaging findings in neonates with congenital pyriform sinus fistula: a retrospective study of 45 cases. Front Pediatr. (2021) 9:721128. doi: 10.3389/fped.2021.721128
25. Farid M, Michael P. Bronchogenic cyst-a rare case mimicking a laryngocoele. J Surg Case Rep. (2017) 2017:rjx055. doi: 10.1093/jscr/rjx055
26. McAdams HP, Kirejczyk WM, Rosado-de-Christenson ML, Matsumoto S. Bronchogenic cyst: imaging features with clinical and histopathologic correlation. Radiology. (2000) 217:441–6. doi: 10.1148/radiology.217.2.r00nv19441
27. Lu D, Yu R, Yang H, Liu J. A bronchogenic cyst of the larynx: a case report. Exp Ther Med. (2017) 14:5523–6. doi: 10.3892/etm.2017.5237
28. Stewart B, Cochran A, Iglesia K, Speights VO, Ruff T. Unusual case of stridor and wheeze in an infant: tracheal bronchogenic cyst. Pediatr Pulmonol. (2002) 34:320–3. doi: 10.1002/ppul.10129
Keywords: bronchogenic cysts, children, head, neck, surgery
Citation: Chen W, Xu M, Wang Q, Xu H, Chen J and Li X (2022) Pediatric bronchogenic cysts in the head and neck region: A study of 10 surgical cases and a review of the literature. Front. Pediatr. 10:1030692. doi: 10.3389/fped.2022.1030692
Received: 29 August 2022; Accepted: 13 October 2022;
Published: 3 November 2022.
Edited by:
Zhengqing Hu, Wayne State University, United StatesReviewed by:
Simmi K. Ratan, University of Delhi, IndiaNikolaos Zavras, University General Hospital Attikon, Greece
Erkan Kaba, Istanbul Florence Nightingale Hospital, Turkey
© 2022 Chen, Xu, Wang, Xu, Chen and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jiarui Chen ZHJjaGVuamlhcnVpQDE2My5jb20= Xiaoyan Li Y2hoc2hlbnRzQDE2My5jb20=
Specialty Section: This article was submitted to Pediatric Otolaryngology, a section of the journal Frontiers in Pediatrics
 Wei Chen1
Wei Chen1 Jiarui Chen
Jiarui Chen Xiaoyan Li
Xiaoyan Li