
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Pediatr., 10 November 2022
Sec. Pediatric Orthopedics
Volume 10 - 2022 | https://doi.org/10.3389/fped.2022.1021981
Objective: To systematically review the current articles to compare the efficacy and safety of 3D navigation-assisted osteotomy of DDH with conventional osteotomy of DDH in children. Study design Databases such as PubMed, Embase, Cochrane Library were searched, from inception to April, 2022, for studies applying 3D navigation-assisted osteotomy in DDH children.
Methods: There were 626 articles identified. According to the search strategy and inclusion criteria, 7 studies were finally included, with a total of 288 cases. Study screening, data extraction, and quality assessment were conducted by two reviewers independently. Data analyses were performed using RevMan 5.4 software.
Results: There were 7 retrospective cohort studies included. Meta-analysis showed that 3D navigation-assisted DDH osteotomy resulted in shorter duration of surgery [I2 = 88%, REM, MD = 22.86, 95%CI (−27.29, −18.43), p < 0.00001], less radiation exposure during surgery [I2 = 53%, REM, MD = 2.76, 95%CI (−3.15, −2.37), p < 0.00001], and less intraoperative bleeding [I2 = 94%, REM, MD = 26.83, 95%CI (−39.24, −14.41), p < 0.0001], compared with conventional DDH osteotomy. There was a significant difference in the number of patients with McKay clinical function graded as poor between the two groups [I2 = 0%, FEM, RR = 0.20, 95%CI (0.05, 0.74), p = 0.02], whereas there were no significantly statistical differences in the corrected acetabular index angle, postoperative leg length discrepancy, and number of patients with Severin x-ray graded as poor between the two groups (p > 0.05).
Conclusion: 3D navigation-assisted pelvis and thighbone osteotomy for DDH children could shorten duration of surgery and reduce intraoperative bleeding and x-ray exposure, presenting definite therapeutic effect.
Systematic Review Registration: https://www.crd.york.ac.uk/PROSPERO/#myprospero, identifier: CRD42022333767.
Developmental dysplasia of the hip (DDH) is the most common type of hip joint deformity in children, with the morbidity of 4–6 per thousand in newborns in developed countries (1, 2). It presents a tough-nut-to-crack in child osteology especially for children aged over 2 years (3). Pelvic osteotomy combined with proximal femur varus, rotation, and shortening is the most commonly applied surgical option for DDH. However, DDH children often have aberrant and complicated anatomical characteristics in their hip joints, which poses a great challenge for surgeons to perform precise osteotomy. Pediatric orthopedists perform osteotomy in pelvic and proximal femur conventionally based on their experience. Any error in preoperative plan-making or intraoperative manipulation would compromise the outcome of the surgery, making it an urgent need for a more precise surgical approach.
3D navigation template technology uses CT data and 3D reconstruction technology to design a rotating and moving orthotic limit navigation template for hip osteotomy, which can achieve accurate osteotomy and accurate displacement of bone blocks. Three-dimensional navigation technology (3D navigation) can help clinicians make precise and individualized surgical scheme and perform surgery simulation so as to facilitate precise osteotomy and internal fixation (4). It has been widely applied in multiple fields such as complicated pelvic, hip, and spinal surgery, bone tumor resection, limb deformity orthotics, and artificial limb-manufacturing (4). However, there are few clinical studies focusing on 3D navigation-assisted hip osteotomy for children with DDH so that evidence of its efficacy and safety remains insufficient, and there is still lack of relevant systematic review and meta-analysis. Therefore, it is of great necessity to conduct a meta-analysis to evaluate the clinical efficacy of 3D navigation-assisted osteotomy for the treatment of DDH in children, so as to provide reference for clinical decision-making.
We aim to systematically review the current articles to compare the efficacy and safety of 3D navigation-assisted osteotomy of DDH with conventional osteotomy of DDH in children.
The protocol for this systematic review was established in advance, documented, and submitted before commencement to PROSPERO (registration number CRD42022333767) on June 15, 2022. This systematic review conformed to the principles detailed in the handbook of the Cochrane Collaboration and the guidelines established by the Preferred Reporting Items for Systematic Reviews and Meta analysis.
PubMed, Cochrane Library, and Embase were searched from inception to April 20th, 2022. Other sources, including teaching materials, conference records, national health guidelines, systematic reviews and meta-analyses, clinical trial registrations, and DDH treatment guidelines, were manually searched. We consulted experts in literature search to search for studies that were unidentified in preliminary search. No language restriction was set. Search strategy mainly included: (Developmental Dysplasia of the Hip) AND (3d printing* OR Computer-Aided Design).
Two reviewers (YY and DS) independently browsed the titles and abstracts to identify potential eligible articles, and the full-texts of which were retrieved and read to identify eligible studies to be included. Any disagreement was settled via discussion or, if necessary, by a third reviewer (LY). Consensus was reached after discussion and consultation. A PRISMA flowchart was used to present the overview of study selection process.
(1) Types of study: Observational cohort study regarding osteotomy of DDH in children;
(2) Types of participants: Children receiving hip osteotomy who were recruited in the study after appraisal of the ethics committee and signed informed consent;
(3) Types of intervention: 3D navigation-assisted osteotomy and performing conventional osteotomy for DDH children.
(1) Complications undescribed and diagnosis unclear or unclassified;
(2) Data incomplete or unavailable;
(3) Animal study, case-report, systematic review and meta-analysis, etc.;
(4) Repeated publication, uncomplete study, or study considered to be pointless.
Characteristics of included studies were extracted by two reviewers (YY and DS) independently, which included: name of the first author, journal, publication date, DDH classification, number of hip joint cases in cohort, 3D navigation technology, pelvic and femur osteotomy, mean age and gender distribution of participants, and follow-up. We also extracted the radiographic results, including femur osteotomy angle, postoperative acetabular index, and leg length discrepancy. Clinical outcomes included the postoperative function score (number of reports and detailed description), intraoperative bleeding, duration of surgery, radiation exposure, and postoperative complication. Results of data extraction of the two reviewers were cross-checked to ensure the accuracy. Any discrepancy in recorded values was verified by both the two reviewers to make a final decision. For missing or incomplete data, the reviewers would try to contact the author to obtain the original data. Had they failed to contact the author, the missing or incomplete data would have been removed.
Quality assessment and data extraction of included studies were conducted by two reviewers independently. Quality assessment for retrospective cohort study was based on the Newcastle-Ottawa Scale (NOS). Any disagreement was settled through discussion with the third reviewer. All included studies were assessed in strict accordance with the assessment criteria of Cochrane Handbook 5.1.1.
Consistency between the reviewers was quantified using Kappa statistics, and risk ratio (RR) was applied as pooled statistic for therapeutic effect. Statistical homogeneity was assessed using q test with the significance level of 10%. Heterogeneity test was performed using Higgins I2 statistic. Meta-analysis was performed via RevMan 5.4 software. A fixed-effect model would be applied if no significant heterogeneity was considered among the studies (I2 < 50%), otherwise, a random-effect model would be used. However, we provided extra data fixed- and random-effect models for the groups analyzed to process data comparison. Sensitivity analysis was employed to determine the influence of each individual study on the summary results by repeating random-effects meta-analysis, omitting one study at a time. For outcome measures that could not be quantitatively pooled, a qualitative description would be provided. Publication bias assessment inapplicable in that less than 10 studies were included.
There were 626 articles retrieved, and each article was evaluated independently. There were 548 articles remained after removing 78 duplicates, then 507 relevant articles were excluded after browsing titles and abstracts (animal studies, pharmacological studies, letters, etc.), and 41 remained for full-text reading. Following exclusion of 34 studies failing to meet the inclusion criteria, 7 retrospective cohort studies were finally included in this meta-analysis (Figure 1).
Publication date of included studies ranged from 1978 to 2022, with a total of 288 child participants. All included studies were retrospective cohort design, with similar definition of DDH but different disease classification. Among the 7 studies (5–11), 1 reported the preoperative scheme-making and clinical effect of computer-aided design (CAD) and 3D reconstruction, 2 reported the application and prospect of 3D printing in osteotomy of child DDH, 4 reported the application of 3D technology and navigation template in osteotomy of child DDH (Table 1). All groups of included studies were comparable.
A total of 7 retrospective cohort studies were included. Publication bias assessment was unavailable due to less than 10 studies included. Sensitivity analysis was performed for duration of surgery, x-ray frequency during surgery, and intraoperative bleeding in that few studies reported relevant outcomes. The results were robust after removal of each study one by one, while significant heterogeneity remained (Table 2). Compared with conventional DDH osteotomy, 3D navigation-assisted osteotomy:
All included studies reported duration of surgery, with significant heterogeneity existing among the studies (I2 = 88%), and random-effect model was applied for meta-analysis. The results showed that 3D navigation-assisted osteotomy remarkably decreased the duration of surgery [I2 = 88%, REM, MD = 22.86, 95%CI (−27.29, −18.43), p < 0.00001] (Figure 2A).
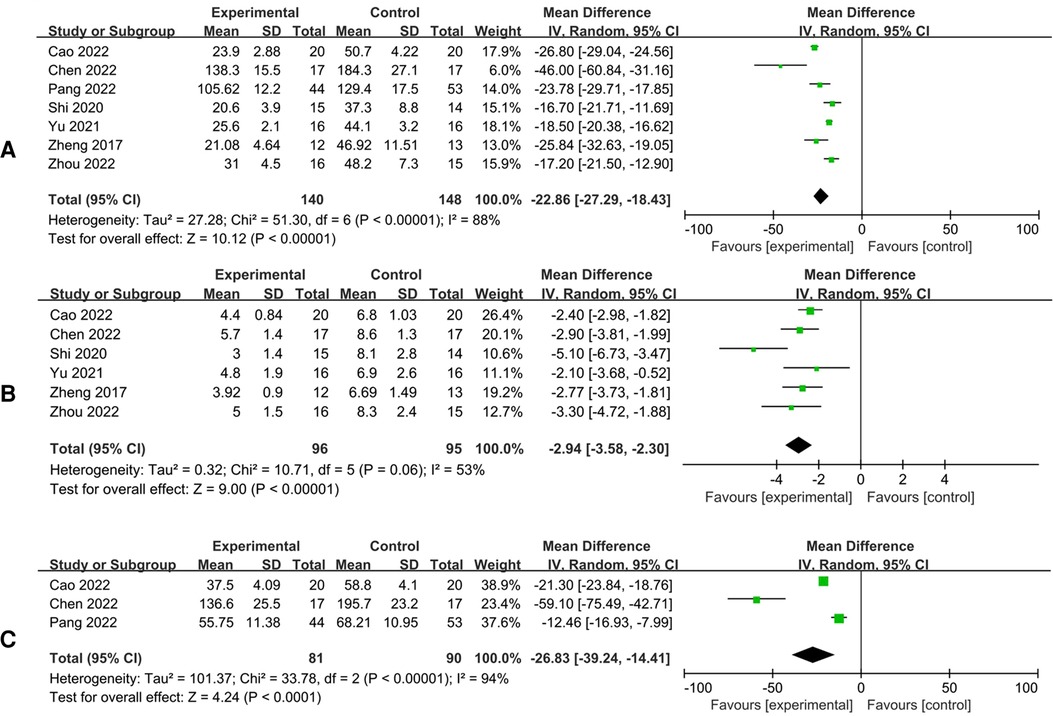
Figure 2. Forest plots of the overall meta-analysis. Operation time (A); Intraoperative fluoroscopy frequency (B). Intraoperative blood loss (C).
There were 6 studies that reported x-ray frequency during surgery, and the results showed that 3D navigation-assisted osteotomy required lower x-ray frequency [I2 = 53%, REM, MD = 2.76, 95%CI (−3.15, −2.37), p < 0.00001], while there was significant heterogeneity among the studies (I2 = 53%) (Figure 2B).
There were 3 studies that reported intraoperative bleeding volume, and the results showed that 3D navigation-assisted osteotomy had less intraoperative bleeding volume [I2 = 94%, REM, MD = 26.83, 95%CI (−39.24, −14.41), p < 0.0001], while there was significant heterogeneity among the studies (I2 = 94%) (Figure 2C).
There were 5 studies that reported numbers of patients with McKay clinical function graded as poor. The results showed that patients receiving 3D navigation-assisted osteotomy has better clinical function [I2 = 0%, FEM, RR = 0.20, 95%CI (0.05, 0.74), p = 0.02]. No significant heterogeneity considered existing among the studies (I2 = 0%) (Figure 3A).
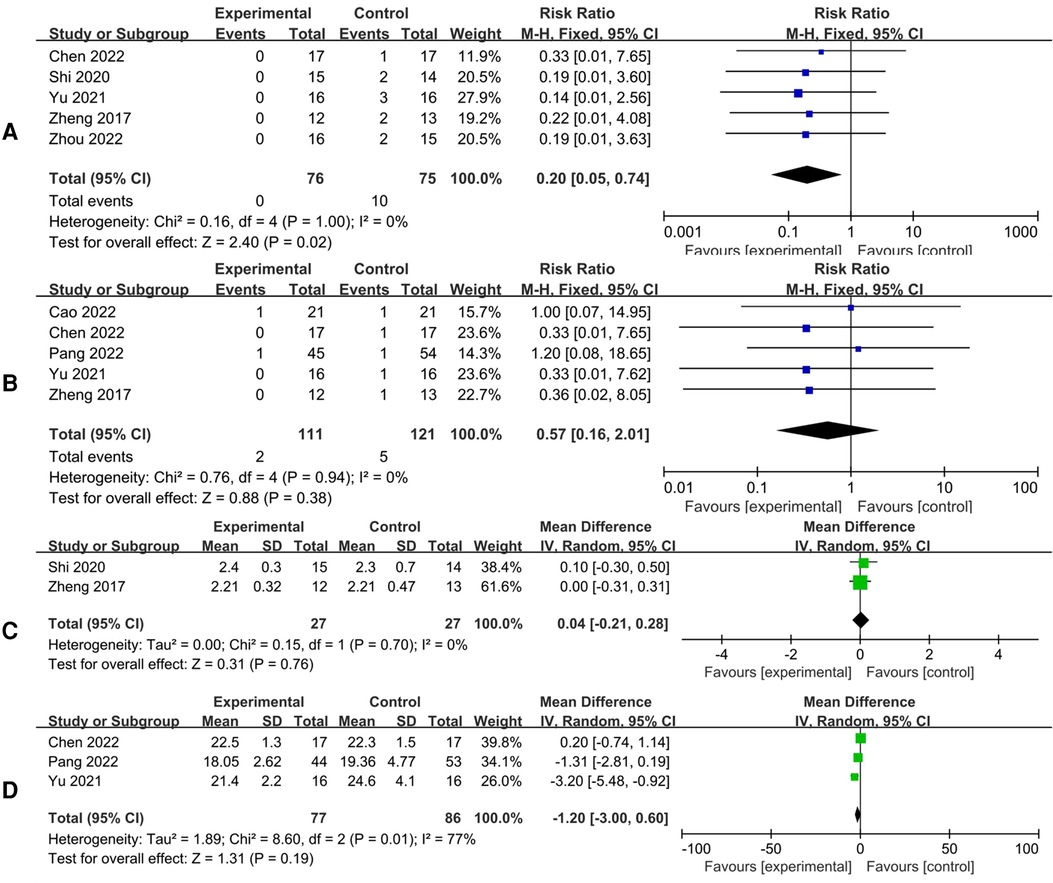
Figure 3. Forest plots of the overall meta-analysis. Poor results of McKay clinical function evaluation (A); poor results of severin X line assessment (B); postoperative lower limb discrepancy (C); postoperative acetabulum indx (D).
There were 5 studies that reported numbers of patients with Severin x-ray graded as poor. There was no significant difference between the two groups [I2 = 0%, FEM, RR = 0.57, 95%CI (0.16, 2.01), p = 0.38]. No significant heterogeneity considered existing among the studies (I2 = 0%) (Figure 3B).
There were 2 studies that reported postoperative leg length discrepancy. There was no significantly statistical difference between the two groups [I2 = 0%, FEM, MD = 0.04, 95%CI (−0.21, 0.28), p = 0.76]. No significant heterogeneity considered existing among the studies (I2 = 0%) (Figure 3C).
There were 3 studies that reported postoperative acetabular index. There was no significant difference between 3D navigation-assisted osteotomy and conventional osteotomy [I2 = 77%, REM, MD = −1.20, 95%CI (−3.00, 0.06), p = 0.03]. There was significant heterogeneity among the studies (I2 = 77%) (Figure 3D).
There were 3 studies that reported postoperative proximal femur osteotomy angle in the two groups. These studies had assessed just 1 of the 3 proximal femur osteotomy angle-related dimensions, which included proximal femur varus, rotation, and shortening, so that this outcome could not be assessed.
This meta-analysis showed that 3D navigation-assisted hip osteotomy could be more effective than conventional hip osteotomy in the treatment of child DDH, and the difference was statistically significant. 3D navigation-assisted osteotomy presented more superior in shortening duration of surgery and reducing intraoperative x-ray frequency and bleeding than conventional osteotomy.
DDH children often have aberrant and complicated anatomical characteristics in their hip joints, bringing multiple difficulties to conventional hip osteotomy (19, 20). We compared the duration of surgery, intraoperative x-ray frequency, intraoperative bleeding, postoperative leg length discrepancy, postoperative acetabular index, number of patients with postoperative McKay clinical function (21) graded poor, and number of patients with Severin x-ray (22) graded as poor. The results revealed statistical significance in the duration of surgery, intraoperative x-ray frequency, intraoperative bleeding, postoperative acetabular index, and number of patients with postoperative McKay clinical function graded poor. There were no significantly statistical differences in the number of patients with Severin x-ray graded as poor and postoperative leg length discrepancy. However, it has been reported by several studies that there is a difference between preoperatively set osteotomy angles and postoperatively measured ones. We failed to further explore this difference due to few studies included. It can be determined that 3D navigation-assisted DDH hip osteotomy appears more advantaged in accuracy, compared with conventional osteotomy. The design of proximal femur osteotomy involves rotation, varus and shortening, which requires accurate osteotomy and proper placement of steel plate so as to achieve satisfied correction (23). Part of included studies reported the advantages of 3D navigation-assisted rotation, varus and shortening, which was also undiscussed in this study due to few studies included.
Most studies indicate that the older the children are, the more likely they are to need further surgical treatment for acetabular residual dysplasia (24–26). For DDH children aged over 2 years, osteotomy presents to be the most preferable option in that increased acetabular index and femoral neck anteversion are important pathological characteristics in DDH (27, 28). The goal of treatment is to achieve reduction of acetabular concentric circles so that to promote the recovery to normal anatomical structure and optimal joint function, which is also crucial for postoperative evaluation (29, 30). Pelvic osteotomy combined with proximal femur osteotomy can facilitate joint reduction, decrease stress on hip joint, correct over-anteversion, and reduce acetabular index, so that to finally restore the nearly normal anatomical structure around the hip joint (31, 32).
Conventional Salter pelvic rotational osteotomy can cause proximal and distal malposition. The supportive triangular bone block needs to be firmly fixed, and the fixation ends of the Kirschner wire should be kept contactless with hip joint, which demands accurate fixation direction (33). Child often has thin ilium, and attempts to fix could induce unfirm fixation and subsequent bone block shift or collapse so that the therapeutic effect would be compromised. Generally, this process is performed by experienced clinicians. Aberrant anatomical characteristics of the hip joint in DDH children (34) increase the difficulty and risk of pelvic and femur osteotomy (35). Conventional osteotomy scheme is made typically based on preoperative pelvic x-ray scan and computed tomography (CT), which is less intuitive so that the osteotomy requires a wealth of experience and exquisite skills of the surgeon.
The pelvis and femur models were reconstructed in three dimensions by importing the original DICOM data of the hip joint into professional software. According to preoperative measurements and compared with the contralateral parameters, design the size of the pelvic bone cutting way, direction, internal fixation, and varus femoral Angle, rotation Angle and length of bone cutting, with reference to the intraoperative use of steel plate pitch, gram parameters such as diameter of needle, the needle was simulated bone cutting plane and into a certain way, navigation template design and the reverse calculation combined with modeling, The surface anatomical and morphological features of pelvis and femur were extracted, and the navigation template three-dimensional model with Kirschner needle path was established. A 1 : 1 hip joint model can be constructed through 3D navigation, which allows orthopedic surgeons to simulate the whole surgical process, make full assessment of the key points during surgery, and select optimal surgical option and scheme. On the other hand, pelvic and femur osteotomy and internal fixation via navigation template can prevent shifting or over-deep implantation to ensure accurate osteotomy and internal fixation. Inexperienced surgeon can also perform the osteotomy with the aid of 3D navigation. The learning curve is shortened (36). In addition, orthopedic surgeons can conduct preoperative communication with patients using 3D printed model, which brings the patients more intuitive understanding of the surgical procedure, enhances their confidence, and increases their satisfaction (13).
A study by Liu et al. (16), found that application of 3D printed pelvic model could increase accuracy and shorten duration of the surgery so that increase the success rate of osteotomy in DDH children and promote their postoperative recovery. Therefore, 3D navigation-assisted pelvic osteotomy can manifest the pelvic deformity of DDH child more intuitively via individualized surgical navigation template so as to help surgeons make accurate measurements, perform surgery simulation, make individualized scheme. It can significantly increase accuracy of the surgery, reduce intraoperative bleeding and radiation exposure, and shorten duration of the surgery. Acetabular index is the most reliable imaging indicator to evaluate the development of DDH (12). This study found that DDH patients receiving 3D navigation-assisted osteotomy had significantly lower postoperative acetabular index than those receiving conventional osteotomy.
Application of 3D navigation promotes the development of orthopedic surgery, while it also needs further improvement (17). The increased surgery costs may restrict the popularization and application of this technology (14, 15). Additionally, the 3D printing equipment is too expensive and the skill requirement is too complicated to be afforded by many hospitals (18). The surgical scheme-making by 3D navigation requires long enough time so that it may be only applicable for patients receiving selective surgery. The contribution of 3D navigation to the decrease of postoperative complications has yet been revealed due to few relevant studies. Meta-analysis based on more clinical trials is needed to robustly support its application.
The results of this meta-analysis are reliable in that the study selection is based on strict inclusion criteria, and the conclusion is drawn via standard meta-analysis process. However, several limitations do exist: firstly, few studies have included, and some of them had limited sample size, resulting in bias of the results. Reliability of the conclusion should be further validated; Secondly, multiple factors could affect the performance of DDH hip osteotomy. Although heterogeneity across sensitivity analyses was stable across all analyses, the large heterogeneity still calls for caution in interpreting the results. The source of heterogeneity may be related to the few included literatures and sample size, different included population, different age, and different application methods of 3D navigation technology. More randomized and large-sample clinical studies are needed in the future. The reviewers have conduct strict screening and selection during data extraction but have failed to perform subgroup analysis. More detailed data should be collected for follow-up studies.
3D navigation-assisted pelvis and thighbone osteotomy for DDH children could shorten duration of surgery and reduce intraoperative bleeding and x-ray exposure, presenting definite therapeutic effect. As for postoperative outcomes, 3D navigation-assisted hip osteotomy is demonstrated to be more effective than conventional osteotomy. The conclusion of this meta-analysis needs to be further validated and updated by more RCTs with remarkable quality. Expanding application of 3D navigation-assisted hip osteotomy presents a great trend in future orthopedic surgery.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
All authors contributed to the study conception and design. YL: Conceptualization, Methodology, Software, Writing—Original draft, Data curation, Visualization, Funding acquisition were performed; YY and SD: Investigation, Writing—Original Draft, Writing—Reviewing and Editing were performed. All authors contributed to the article and approved the submitted version.
Supported by the Ningbo Medical Key Supporting Discipline (grant number 2022-F25).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Pollet V, Percy V, Prior HJ. Relative risk and incidence for developmental dysplasia of the hip. J Pediatr. (2017) 181:202–7. doi: 10.1016/j.jpeds.2016.10.017
2. Woodacre T, Ball T, Cox P. Epidemiology of developmental dysplasia of the hip within the UK: refining the risk factors. J Child Orthop. (2016) 10(6):633–42. doi: 10.1007/s11832-016-0798-5
3. Sewell MD, Eastwood DM. Screening and treatment in developmental dysplasia of the hip-where do we go from here? Int Orthop. (2011) 35(9):1359–67. doi: 10.1007/s00264-011-1257-z
4. Duan X, Wang B, Yang L, Kadakia AR. Applications of 3d printing technology in orthopedic treatment. BioMed Res Int. (2021) 2021:9892456. doi: 10.1155/2021/9892456
5. Zhou W, Guo H, Duan R, Shi Q. Visualized simulative surgery in preoperative planning for proximal femoral varus osteotomy of Ddh. BMC Musculoskelet Disord. (2022) 23(1):295. doi: 10.1186/s12891-022-05219-7
6. Cao J, Gao C, Sun JH, Zheng HJ, Zhu HY, Zhong ZP, et al. Effect of 3d printing technology in proximal femoral osteotomy in children with developmental dysplasia of the hip. Dis Markers. (2022) 2022:1291996. doi: 10.1155/2022/1291996
7. Yu J, Shi Q. Efficacy evaluation of 3d navigational template for salter osteotomy of ddh in children. BioMed Res Int. (2021) 2021:8832617. doi: 10.1155/2021/8832617
8. Shi Q, Sun D. Efficacy and safety of a novel personalized navigation template in proximal femoral corrective osteotomy for the treatment of ddh. J Orthop Surg Res. (2020) 15(1):317. doi: 10.1186/s13018-020-01843-y
9. Zheng P, Xu P, Yao Q, Tang K, Lou Y. 3d-Printed navigation template in proximal femoral osteotomy for older children with developmental dysplasia of the hip. Sci Rep. (2017) 7:44993. doi: 10.1038/srep44993
10. Pang H, Wang Y, Fan M, Liu Y, Qiang L, Wang J, et al. Application of three-dimensional printed individualized navigation template in developmental dysplasia during hip surgery. Chin J Pediatr Surg. (2022) 43(4):365–72. doi: 10.3760/cma.j.cn421158-20210303-00101
11. Chen C, Qu G, Tang Y, Zhuang W. Three-dimensional printing technique assisted salter osteotomy in the treatment of develop-mental dysplasia of the hip. J Clin Orthop. (2022) 25(1):53–7. doi: 10.3969/j.issn.1008-0287.2022.01.016
12. Nie Y, Wang H, Huang Z, Shen B, Kraus VB, Zhou Z. Radiographic underestimation of in vivo cup coverage provided by total hip arthroplasty for dysplasia. Orthopedics. (2018) 41(1):e46–51. doi: 10.3928/01477447-20171114-01
13. Kim SJ, Jo YH, Choi WS, Lee CH, Lee BG, Kim JH, et al. Biomechanical properties of 3-dimensional printed volar locking distal radius plate: comparison with conventional volar locking plate. J Hand Surg Am. (2017) 42(9):747.e1–.e6. doi: 10.1016/j.jhsa.2017.05.009
14. Chana-Rodríguez F, Mañanes RP, Rojo-Manaute J, Gil P, Martínez-Gómiz JM, Vaquero-Martín J. 3d Surgical printing and pre contoured plates for acetabular fractures. Injury. (2016) 47(11):2507–11. doi: 10.1016/j.injury.2016.08.027
15. Wan SX, Meng FB, Zhang J, Chen Z, Yu LB, Wen JJ. Experimental study and preliminary clinical application of mini-invasive percutaneous internal screw fixation for scaphoid fracture under the guidance of a 3d-printed guide plate. Curr Med Sci. (2019) 39(6):990–6. doi: 10.1007/s11596-019-2133-0
16. Liu K, Li Z, Ma Y, Lian H. 3d-Printed Pelvis model is an efficient method of osteotomy simulation for the treatment of developmental dysplasia of the hip. Exp Ther Med. (2020) 19(2):1155–60. doi: 10.3892/etm.2019.8332
17. Inge S, Brouwers L, van der Heijden F, Bemelman M. 3d Printing for corrective osteotomy of malunited distal radius fractures: a low-cost workflow. BMJ Case Rep. (2018) 2018. doi: 10.1136/bcr-2017-223996. https://casereports.bmj.com/content/2018/bcr-2017-223996.long. https://casereports.bmj.com/content/2018/bcr-2017-223996.long30042099
18. Jinsihan N, Jin G. Recent developments of 3d-printing technique assisted surgery in the management of complex fractures. Int J Clin Exp Med. (2018) 11(11):11578–83. ISSN:1940-5901; IJCEM0078892
19. Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br Vol. (2005) 87(7):1012–8. doi: 10.1302/0301-620x.87b7.15203
20. Pfirrmann CW, Mengiardi B, Dora C, Kalberer F, Zanetti M, Hodler J. Cam and pincer femoroacetabular impingement: characteristic Mr arthrographic findings in 50 patients. Radiology. (2006) 240(3):778–85. doi: 10.1148/radiol.2403050767
21. McKay DW. A comparison of the innominate and the pericapsular osteotomy in the treatment of congenital dislocation of the hip. Clin Orthop Relat Res. (1974) 98:124–32. doi: 10.1097/00003086-197401000-00013
22. Ward WT, Vogt M, Grudziak JS, Tümer Y, Cook PC, Fitch RD. Severin classification system for evaluation of the results of operative treatment of congenital dislocation of the hip. A study of intraobserver and interobserver reliability. J Bone Joint Surg Am Vol. (1997) 79(5):656–63. doi: 10.2106/00004623-199705000-00004
23. Cherkasskiy L, Caffrey JP, Szewczyk AF, Cory E, Bomar JD, Farnsworth CL, et al. Patient-specific 3d models aid planning for triplane proximal femoral osteotomy in slipped capital femoral epiphysis. J Child Orthop. (2017) 11(2):147–53. doi: 10.1302/1863-2548-11-170277
24. Salter RB, Dubos JP. The first fifteen year's personal experience with innominate osteotomy in the treatment of congenital dislocation and subluxation of the hip. Clin Orthop Relat Res. (1974) 98:72–103. doi: 10.1097/00003086-197401000-00009
25. Schulze A, Tingart M. Salter innominate osteotomy: indications, surgical technique, results.. Der Orthopade. (2016) 45(8):659–65. doi: 10.1007/s00132-016-3290-5
26. Vaquero-Picado A, González-Morán G, Garay EG, Moraleda L. Developmental dysplasia of the hip: update of management. EFORT Open Rev. (2019) 4(9):548–56. doi: 10.1302/2058-5241.4.180019
27. Baghdadi T, Bagheri N, Khabiri SS, Kalantar H. The outcome of salter innominate osteotomy for developmental hip dysplasia before and after 3 years old. Arch Bone Jt Surg. (2018) 6(4):318–23. doi: 10.22038/abjs.2017.24277.1639
28. Kotlarsky P, Haber R, Bialik V, Eidelman M. Developmental dysplasia of the hip: what has changed in the last 20 years? World J Orthop. (2015) 6(11):886–901. doi: 10.5312/wjo.v6.i11.886
29. Wyles CC, Vargas JS, Heidenreich MJ, Mara KC, Peters CL, Clohisy JC, et al. Natural history of the dysplastic hip following modern periacetabular osteotomy. J Bone Joint Surg Am Vol. (2019) 101(10):932–8. doi: 10.2106/jbjs.18.00983
30. Thawrani D, Sucato DJ, Podeszwa DA, DeLaRocha A. Complications associated with the bernese periacetabular osteotomy for hip dysplasia in adolescents. J Bone Joint Surg Am Vol. (2010) 92(8):1707–14. doi: 10.2106/jbjs.I.00829
31. Sankar WN, Young CR, Lin AG, Crow SA, Baldwin KD, Moseley CF. Risk factors for failure after open reduction for ddh: a matched cohort analysis. J Pediatr Orthop. (2011) 31(3):232–9. doi: 10.1097/BPO.0b013e31820c9b31
32. Wells J, Nepple JJ, Crook K, Ross JR, Bedi A, Schoenecker P, et al. Femoral morphology in the dysplastic hip: three-dimensional characterizations with ct. Clin Orthop Relat Res. (2017) 475(4):1045–54. doi: 10.1007/s11999-016-5119-2
33. Tukenmez M, Tezeren G. Salter innominate osteotomy for treatment of developmental dysplasia of the hip. J Orthop Surg. (2007) 15(3):286–90. doi: 10.1177/230949900701500308
34. Jia J, Li L, Zhang L, Zhao Q, Liu X. Three dimensional-ct evaluation of femoral neck anteversion, acetabular anteversion and combined anteversion in unilateral Ddh in an early walking age group. Int Orthop. (2012) 36(1):119–24. doi: 10.1007/s00264-011-1337-0
35. Schmidutz F, Roesner J, Niethammer TR, Paulus AC, Heimkes B, Weber P. Can salter osteotomy correct late diagnosed hip dysplasia: a retrospective evaluation of 49 hips after 6.7 years? Orthop Traumatol Surg Res. (2018) 104(5):637–43. doi: 10.1016/j.otsr.2018.05.004
Keywords: child DDH, hip osteotomy, 3D navigation, auxiliary, meta-analysis
Citation: Liu Y, Yang Y and Ding S (2022) Application of 3D navigation for osteotomy of DDH in children: A systematic review and meta-analysis. Front. Pediatr. 10:1021981. doi: 10.3389/fped.2022.1021981
Received: 18 August 2022; Accepted: 19 October 2022;
Published: 10 November 2022.
Edited by:
Pablo Castañeda, National Autonomous University of Mexico, MexicoReviewed by:
Pengfei Zheng, Nanjing Children's Hospital, China© 2022 Liu, Yang and Ding. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yunlong Liu MTM5NTc0MDMxMjZAMTYzLmNvbQ==
Specialty Section: This article was submitted to Pediatric Orthopedics, a section of the journal Frontiers in Pediatrics
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.