- 1Division of Neonatology, Department of Pediatrics, Johns Hopkins University School of Medicine, Baltimore, MD, United States
- 2Department of International Health, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, United States
- 3Department of Anesthesia and Critical Care Medicine, Johns Hopkins University School of Medicine, Baltimore, MD, United States
- 4Armstrong Institute for Patient Safety and Quality, Johns Hopkins Medicine, Baltimore, MD, United States
- 5Byramjee-Jeejeebhoy Government Medical College-Johns Hopkins University Clinical Research Site, Pune, India
- 6Department of Pediatrics, Byramjee-Jeejeebhoy Government Medical College, Pune, India
- 7Department of Neonatology, Bharati Vidyapeeth Deemed to Be University Medical College, Pune, India
- 8Department of Pediatrics, Bharati Vidyapeeth Deemed to Be University Medical College, Pune, India
- 9Department of Pediatrics, King Edward Memorial Hospital, Pune, India
- 10Department of Pediatrics, Dr. D. Y. Patil Medical College, Pune, India
- 11Department of Hospital Epidemiology and Infection Control, Johns Hopkins Hospital, Baltimore, MD, United States
- 12Division of Infectious Diseases, Department of Pediatrics, University of Pennsylvania, Philadelphia, PA, United States
- 13Centers for Disease Control and Prevention, Atlanta, GA, United States
- 14Department of Biostatistics, Bloomberg School of Public Health, Johns Hopkins University, Baltimore, MD, United States
- 15Division of Infectious Diseases, Department of Medicine, Johns Hopkins University School of Medicine, Baltimore, MD, United States
- 16Division of Pediatric Infectious Diseases, Department of Pediatrics, Johns Hopkins University School of Medicine, Baltimore, MD, United States
Objective: To implement the Comprehensive Unit-based Safety Program (CUSP) in four neonatal intensive care units (NICUs) in Pune, India, to improve infection prevention and control (IPC) practices.
Design: In this quasi-experimental study, we implemented CUSP in four NICUs in Pune, India, to improve IPC practices in three focus areas: hand hygiene, aseptic technique for invasive procedures, and medication and intravenous fluid preparation and administration. Sites received training in CUSP methodology, formed multidisciplinary teams, and selected interventions for each focus area. Process measures included fidelity to CUSP, hand hygiene compliance, and central line insertion checklist completion. Outcome measures included the rate of healthcare-associated bloodstream infection (HA-BSI), all-cause mortality, patient safety culture, and workload.
Results: A total of 144 healthcare workers and administrators completed CUSP training. All sites conducted at least 75% of monthly meetings. Hand hygiene compliance odds increased 6% per month [odds ratio (OR) 1.06 (95% CI 1.03–1.10)]. Providers completed insertion checklists for 68% of neonates with a central line; 83% of checklists were fully completed. All-cause mortality and HA-BSI rate did not change significantly after CUSP implementation. Patient safety culture domains with greatest improvement were management support for patient safety (+7.6%), teamwork within units (+5.3%), and organizational learning—continuous improvement (+4.7%). Overall workload increased from a mean score of 46.28 ± 16.97 at baseline to 65.07 ± 19.05 at follow-up (p < 0.0001).
Conclusion: CUSP implementation increased hand hygiene compliance, successful implementation of a central line insertion checklist, and improvements in safety culture in four Indian NICUs. This multimodal strategy is a promising framework for low- and middle-income country healthcare facilities to reduce HAI risk in neonates.
Introduction
As facility-based births increase worldwide, low- and middle-income countries (LMIC) increasingly provide care for premature and sick neonates in neonatal intensive care units (NICUs) and special care nurseries (1). Hospitalized neonates are uniquely vulnerable to healthcare-associated infections (HAI) (2, 3). Poor infection prevention and control (IPC) practices augment this risk in many LMIC healthcare facilities (4). The burden of HAI in hospitalized neonates in LMICs exceeds that of facilities in high-income settings (5). The predominance of multi-drug resistant Gram-negative HAIs, which have limited treatment options and are associated with high morbidity and mortality in neonates, underscores the urgency of prevention interventions (6–8).
The World Health Organization (WHO) recommends implementation of multimodal improvement strategies for IPC with the following five elements: (1) system change, (2) training and education, (3) monitoring and feedback, (4) reminders and communication, and (5) culture change (9, 10). The Comprehensive Unit-based Safety Program (CUSP) is a multimodal improvement strategy that has been successfully implemented to improve IPC practices. CUSP has been used to reduce risk of central line-associated bloodstream infections (CLABSIs) and other HAIs in a variety of healthcare settings and populations (11–17). CUSP fosters the creation of a unit-based multidisciplinary team and empowers staff to assume responsibility for change, improving local patient safety culture and compliance with best practices to reduce HAIs and other threats to patient safety (18). While CUSP has been successfully applied internationally in high-income settings, including in Saudi Arabia and the United Arab Emirates, there is limited experience in NICU and LMIC settings (16, 17). Our objective was to assess the performance of CUSP in NICUs in an LMIC setting to guide IPC improvement strategies, reduce HAI risk in hospitalized neonates, and improve patient safety culture.
Methods
In this quasi-experimental study, we implemented CUSP to improve adherence to evidence-based IPC practices in four tertiary care NICUs in Pune, India. Consent was obtained from all healthcare workers (HCWs) who completed surveys. This study was approved by the Johns Hopkins Medicine Institutional Review Board, the ethics committees of all participant sites, and the Indian Health Ministry's Screening Committee. This manuscript uses the SQUIRE 2.0 standards for reporting (19).
Study Sites
All participant sites are tertiary care facilities with high-volume NICUs located in Pune, India, though referral patterns and patient demographics differ. Byramjee Jeejeebhoy Government Medical College (BJGMC) is a government medical college affiliated with Sassoon Hospital, which has a 60-bed NICU. King Edward Memorial (KEM) Hospital is a non-governmental facility run by a charitable trust and has a 46-bed NICU. Dr. D. Y. Patil Medical College is a private medical college and has a 26-bed NICU. Bharati Vidyapeeth Deemed University Medical College is a private medical college and has a 60-bed NICU. All hospitals are delivery centers and admit both inborn and outborn neonates.
CUSP Implementation
CUSP is a validated strategy to empower staff to improve unit-level patient safety and consists of the following steps: (1) educate staff on the science of safety, (2) engage staff in identifying defects, (3) partner with a senior executive, (4) identify and learn from defects, and (5) implement teamwork tools (20). CUSP methodology has previously been described in the literature and the CUSP toolkit is publicly available on the Agency for Healthcare Research and Quality's (AHRQ) website at www.ahrq.gov (11, 20, 21). In this study, CUSP was used to improve HCW adherence to evidence-based IPC practices and reduce HAI risk in the NICU (see conceptual framework, Figure 1). Site staff received training in CUSP methodology and formed multidisciplinary teams led by a CUSP nurse champion and physician champion. Monthly CUSP meetings were attended by CUSP facilitators. Teams were additionally supported by monthly coaching calls.
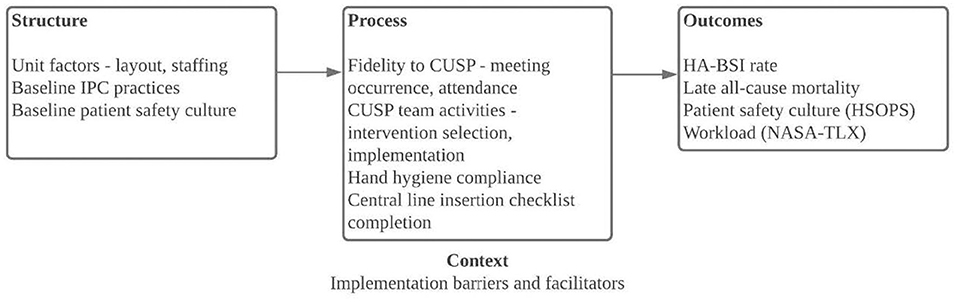
Figure 1. Conceptual framework for CUSP implementation at four tertiary care neonatal intensive care units in Pune, India. CUSP, Comprehensive Unit-based Safety Program; HA-BSI, healthcare-associated bloodstream infections; HSOPS, Hospital Survey on Patient Safety Culture; IPC, infection prevention and control; NASA-TLX, National Aeronautics and Space Administration Task Load Index.
Baseline IPC Assessments
Baseline IPC assessments of practices relevant to neonatal care at the facility level and within the Labor & Delivery ward and NICU were conducted in February 2017 and January 2018 using the Infection Control Assessment Tool (ICAT), 2nd version (2009) (22, 23). We supplemented the ICAT with questions specific to neonatal care, such as the storage and preparation of breast milk and formula feeds, umbilical catheter insertion and maintenance, and isolette and radiant warmer cleaning and disinfection. After review of these assessments and discussions with key local stakeholders, we identified three focus areas for CUSP: hand hygiene, aseptic technique for invasive procedures, and medication and intravenous (IV) fluid preparation and administration. For the third focus area, medication and IV fluid preparation and administration, sites were additionally provided an injection safety assessment tool that guided site self-assessment of existing practices (see Supplementary Material).
Selection and Implementation of Interventions
After CUSP teams were formed, unit-level staff selected interventions for the three focus areas, hand hygiene, aseptic technique for invasive procedures, and medication and IV fluid preparation and administration. For each pre-selected focus area, sites completed a two-question Staff Safety Assessment (SSA), adapted from the CUSP toolkit to each focus area in order to elicit staff perceptions of threats to patient safety within each focus area (Supplementary Table 1). After analyzing SSA responses, each CUSP team identified and implemented targeted interventions for each focus area. All sites initiated hand hygiene monitoring and implemented a central line insertion checklist (see Supplementary Material). Other interventions were selected and implemented at sites' discretion (Table 1). For focus area 2, creation of a central line maintenance audit tool was requested; completion of this tool was encouraged but not monitored (see Supplementary Material). For focus area 3, the injection safety assessment tool was used to support site assessments of existing practices and selected of interventions, which included use of multi-dose medication vials with a lower concentration, thereby reducing number of doses per vial, use of dedicated staff for preparation of all medications and IV fluids, and moving medication and IV fluid preparation to a separate space outside of the immediate patient care area (Figure 1). Notably, most medications administered in site NICUs are admixed in the patient care areas, rather than in the hospital's central pharmacy.
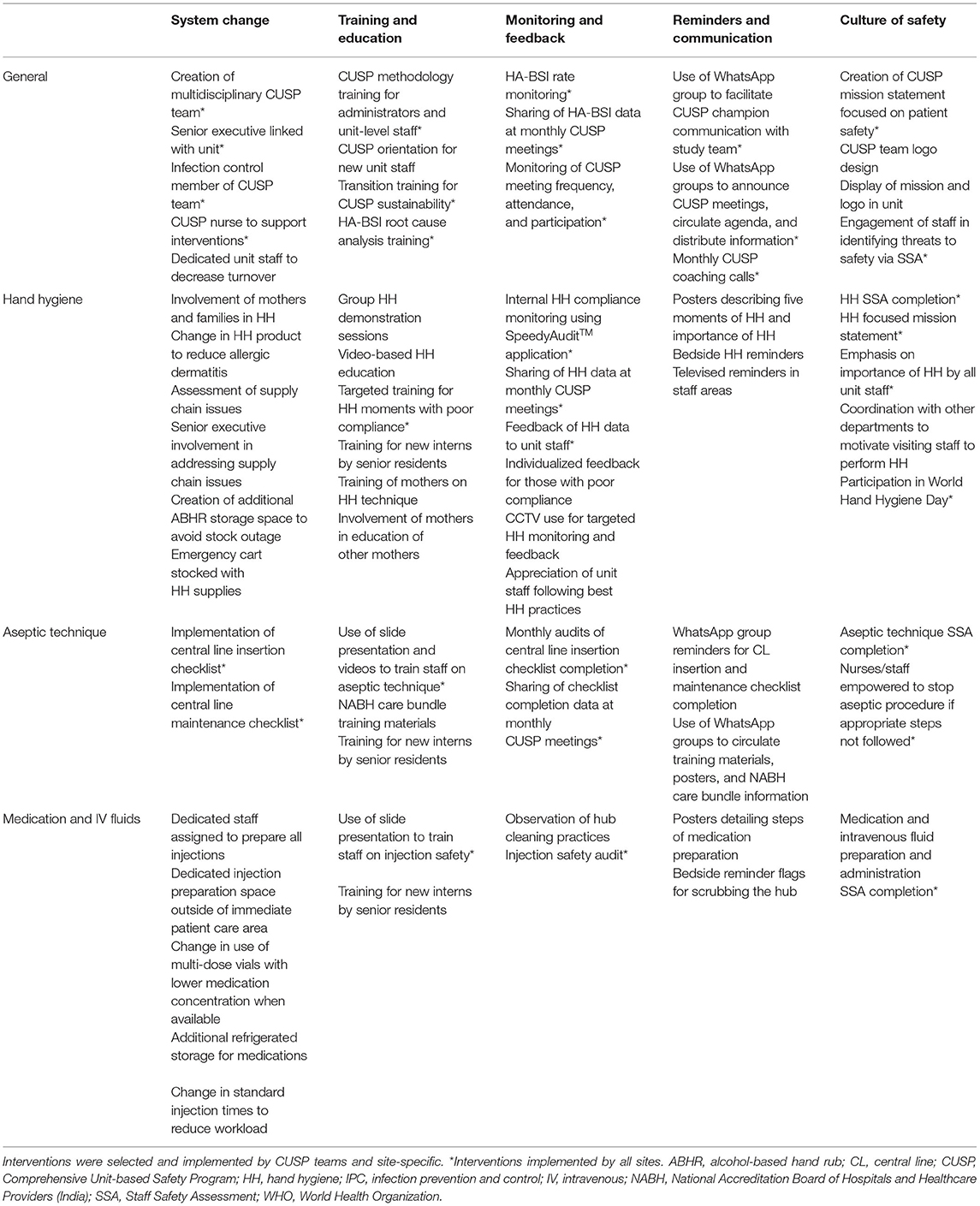
Table 1. CUSP interventions, general and by focus area, categorized by the five elements of the WHO multimodal IPC improvement strategy.
During monthly CUSP coaching calls, study team CUSP coaches and facilitators introduced adapted CUSP tools to support the implementation of interventions, such as the SSA and Patient Safety Rounds (see Supplementary Material) (21).
Outcomes
Process measures included CUSP training participation, monthly meeting occurrence and attendance, hand hygiene compliance, and central line insertion checklist completion. Outcome measures included the rate of healthcare-associated bloodstream infections (HA-BSI), all-cause mortality, patient safety culture, and workload.
Process Measures
CUSP Participation
We recorded attendance of all participants in CUSP training by name, role, and site. Each site recorded attendance of all participants by name and role at each monthly CUSP meeting.
Hand Hygiene Compliance
Hand hygiene compliance was measured by direct observation using trained external observers via the SpeedyAuditTM application (HandyMetrics Corporation, Toronto, Canada). Hand hygiene compliance was recorded by HCW role and the five moments of hand hygiene: (1) before touching a patient; (2) before clean/aseptic procedures; (3) after body fluid exposure risk; (4) after touching a patient; and (5) after touching patient surroundings (24). Hand hygiene data by HCW role and moment of hand hygiene were reported monthly and shared with site CUSP teams and unit staff throughout the study period.
Central Line Insertion Checklist Completion
The central line insertion checklist was adapted from the Johns Hopkins Hospital Pediatric Central Arterial and Venous Catheter Insertion Checklist with input from local stakeholders (see tools included in Supplementary Material). Sites implemented the central line insertion checklist in January-February 2019; none of the sites had a similar checklist in place prior to the study. Checklist completion was monitored by monthly audit completed by external assessors, with an assessment of central line checklist presence and completion in the medical record of neonates with a central line in place, and reported monthly at CUSP meetings.
Outcome Measures
Healthcare-Associated Bloodstream Infections and All-Cause Mortality
HA-BSI was defined as culture-confirmed BSI on hospital day 3 or greater. The monthly rate of HA-BSI was expressed as cases per 1,000 patient-days. Blood cultures were obtained at the discretion of the clinical teams and processed at site microbiology laboratories. For the primary outcome of HA-BSI, organisms deemed as likely contaminants (per categorization as a common commensal per the Centers for Disease Control and Prevention National Healthcare Safety Network) were excluded, with the exception of coagulase negative Staphylococcus (CONS), one of the most common HA-BSI pathogens in hospitalized neonates (2, 25). All-cause mortality was defined as the number of deaths per 100 admissions among neonates admitted for at least 3 days. HA-BSI and mortality data was collected as part of a concurrent prospective cohort study enrolling all neonates admitted to the NICU in which three sites participated (26). The fourth site reported unit-level HA-BSI and mortality data for outcome ascertainment.
Patient Safety Culture
Patient safety culture was assessed at baseline and follow-up using the Agency for Healthcare Research and Quality (AHRQ) Surveys on Patient Safety Culture (SOPSTM) Hospital Survey (HSOPS) version 1.0 (27). The HSOPS consists of 42 items organized into 12 composite dimensions that assess elements of patient safety culture using a Likert response scale as well as nine items assessing respondent characteristics (Supplementary Table 2). The survey was administered in English, Marathi, or Hindi based on respondent preference. Survey responses were anonymous, and baseline and follow-up survey responses were not linked.
Workload
Workload was assessed at baseline and follow-up using the National Aeronautics and Space Administration Task Load Index (NASA-TLX) (28). The NASA-TLX assesses workload across six domains: mental demand, physical demand, temporal demand, effort, performance, and frustration. Each domain is assessed by a single item on a 20-point continuous scale. The NASA-TLX was administered with the HSOPS; responses were also anonymous and not linked.
Statistical Analysis
Logistic regression models were used to describe trends in hand hygiene compliance after CUSP implementation. The models included month and allowed for comparisons across site and by HCW role. All regression models accounted for potential autoregressive correlation of rates within a site over time; standard errors for the pooled analyses were estimated using robust variance estimates.
Descriptive analyses included summarizing baseline and post-implementation HA-BSI rates and all-cause mortality overall and by site. The site-specific baseline and post-implementation HA-BSI and mortality rates were compared using two-sample Poisson tests. The pooled relative monthly HA-BSI and mortality rates comparing the post-implementation and baseline periods were estimated using Poisson regression models with the number of HA-BSI or deaths as the outcome, main effect for the post-implementation and baseline periods and offset for total exposure time (patient-days or admissions).
For HSOPS analysis, percent positive scores (PPS) by item were calculated by dichotomizing responses and reverse coding scores for negative items. Mean PPS for composite domains were calculated by averaging PPS across items included in each domain. Comparison of baseline and follow-up patient safety culture was performed by site-level analysis of the difference in mean PPS for each composite domain. Confidence intervals (CIs) for the change in the mean PPS for composite domains were generated using a bootstrap procedure. Given that it was not possible to link responses for a respondent who participated in both baseline and follow-up surveys, the bootstrap procedure was used to replicate this potential clustering by resampling respondents with replacement within site and pre- and post-intervention surveys. The reported bootstrap CIs are based on 1000 bootstrap samples and use the bias-corrected and accelerated method.
For NASA-TLX analysis, mean scores were calculated at baseline and follow-up for the six domains of workload. An overall workload score was calculated by summing the six domain scores at baseline and at follow-up, for a maximum score of 120. Baseline and post-intervention means were compared using Student's t-test. A p-value < 0.05 was considered statistically significant.
All statistical analyses were completing using Stata version 15.0 (Stata Corp., College Station, TX) and R version 3.6.1 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Process Measures
CUSP Methodology Training
Across the four sites, 144 HCWs and administrators participated in CUSP methodology training in March 2018. Central training was attended mostly by administrators and senior leadership, as well as physician and nurse champions for each site. Site-based training included primarily unit-based staff as well as infection control staff. By the conclusion of training, all sites identified CUSP team members, including physician and nurse champions, a senior executive partner, infection control staff, and additional unit-based physicians and nurses.
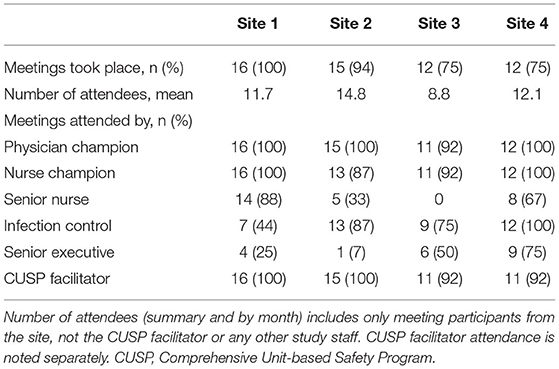
CUSP Meetings and Coaching Calls
CUSP meetings took place monthly at each site over the course of the study period (Table 2). All sites conducted at least 75% of monthly meetings, with average attendance ranging from 8.8 to 14.8 participants per meeting across sites. The proportion of monthly meetings attended was highest among physician and nurse champions (87–100%). Senior executive attendance varied from 7% to 75%.
Hand Hygiene Compliance
There were 8684 hand hygiene observations across the sites over the course of the study period with all four sites collecting hand hygiene observations within 3 months of CUSP implementation (Figure 2). From the pooled analysis of all four sites, the proportion of compliant hand hygiene observations during the month of CUSP implementation was 51% (95% confidence interval (CI) 40-62%) and increased significantly to 56% (95% CI 46–65%), 65% (95% CI 57–72%), and 73% (95% CI 65–81%) by the 3rd, 9th and 15th month, respectively, following CUSP implementation; odds of hand hygiene compliance increased 6% per month, odds ratio (OR) 1.06, 95% CI 1.03–1.10). All sites had a statistically significant increase in the estimated hand hygiene compliance from CUSP implementation to the 15th month thereafter: site 1 from 48 to 67% (OR 1.05, 95% CI 1.04–1.07), site 2 from 52 to 78% (OR 1.08, 95% CI 1.06–1.11), site 3 from 33 to 76% (OR 1.13, 95% CI 1.10–1.16), and site 4 from 61 to 87% (OR 1.10, 95% CI 1.01–1.19). The rate of change of hand hygiene compliance over time did not differ by HCW role (p = 0.988).
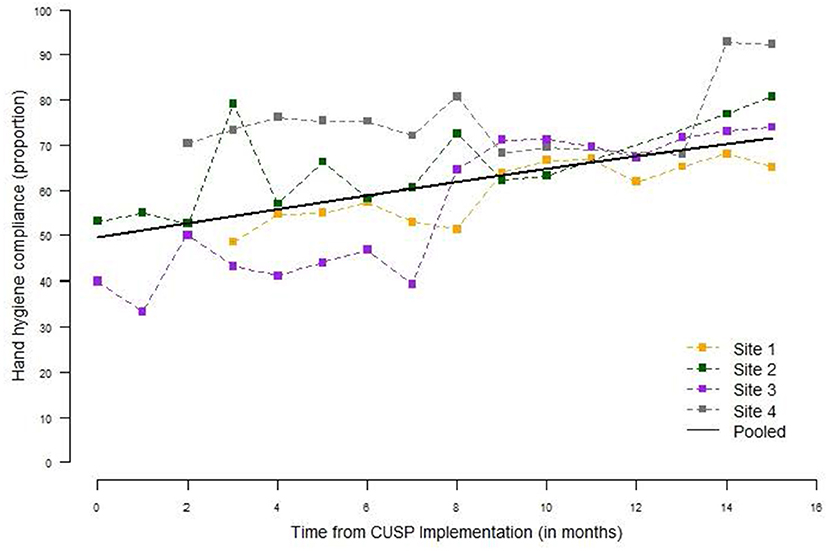
Figure 2. Hand hygiene compliance by site and month, June 2018–September 2019. Monthly hand hygiene compliance was expressed as the proportion of monthly observations compliant, by site for all healthcare worker roles. Hand hygiene was monitored monthly via direct observation by trained observers. There were 8,684 opportunities for hand hygiene across all four sites over the course of the study period. The pooled hand hygiene compliance is based on a logistic regression model for observation compliance as a function of month from CUSP implementation.
Central Line Insertion Checklist Completion
From January 2019 until September 2019, there were 486 neonates who had a central line in place at time of monthly checklist audit. For site 1 (n = 146), 68% of neonates with a central line in place had an insertion checklist present in the medical record; site 2 (n = 166) 100%, site 3 (n = 136) 48%, and site 4 (n = 38) 66%. Site 4's data were only representative of the last 5 months of checklist use; data were collected on checklist presence and completion, but not on the total number of neonates with central lines during the prior 4 months. Among checklists present in the chart (n = 364), 83% were completed (no required fields left blank).
Outcome Measures
Healthcare-Associated Bloodstream Infections
During the baseline period, there were 202 HA-BSI cases, with an HA-BSI rate of 5.99 per 1,000 patient-days (Figure 3). During the post-intervention period, there were 251 HA-BSI cases, with an HA-BSI rate of 6.40 per 1,000 patient-days. Overall, there was no statistically significant change in the monthly HA-BSI rate from baseline to the post-intervention period, with a relative rate (RR) of 0.97 [95% confidence interval (CI) 0.92–1.03] (Figure 3). HA-BSI rates demonstrated seasonality with increased rates over the monsoon period (June-September), which coincided with the start of the post-intervention period. There was no change in monthly HA-BSI rates for sites 1 and 4 (Table 3). Site 2 demonstrated a decrease in monthly HA-BSI rate from baseline to post-intervention (RR 0.52; 95% CI 0.32–0.84), whereas site 3 had an increased monthly HA-BSI rate post-intervention (RR 1.72; 95% CI 1.08–2.74).
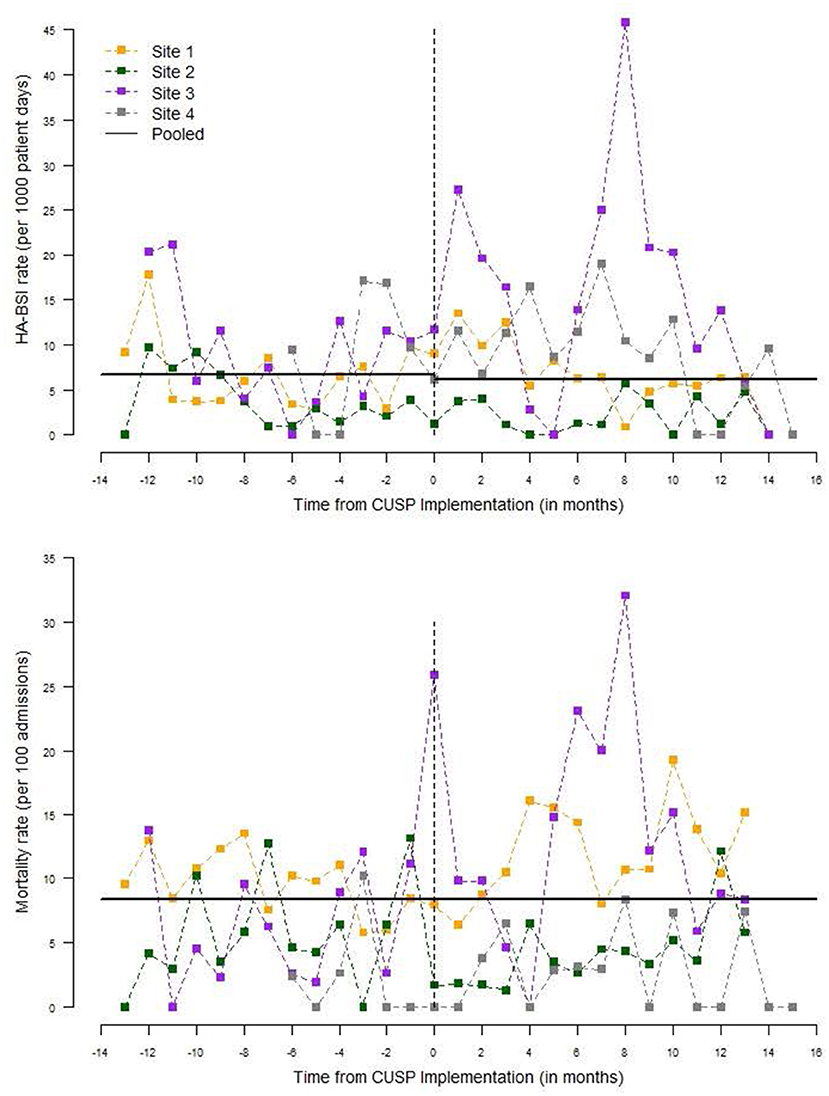
Figure 3. Healthcare-associated bloodstream infection rate and all-cause mortality by site and month. The monthly HA-BSI was expressed as cases per 1,000 patient-days. All-cause mortality was expressed as deaths per 100 admissions among neonates admitted for at least 3 days. The pooled estimates are based on a Poisson regression model for the monthly rate of HA-BSI or mortality as a function of post- vs. pre-CUSP implementation. CUSP, Comprehensive Unit-based Safety Program; HA-BSI, healthcare-associated bloodstream infection.
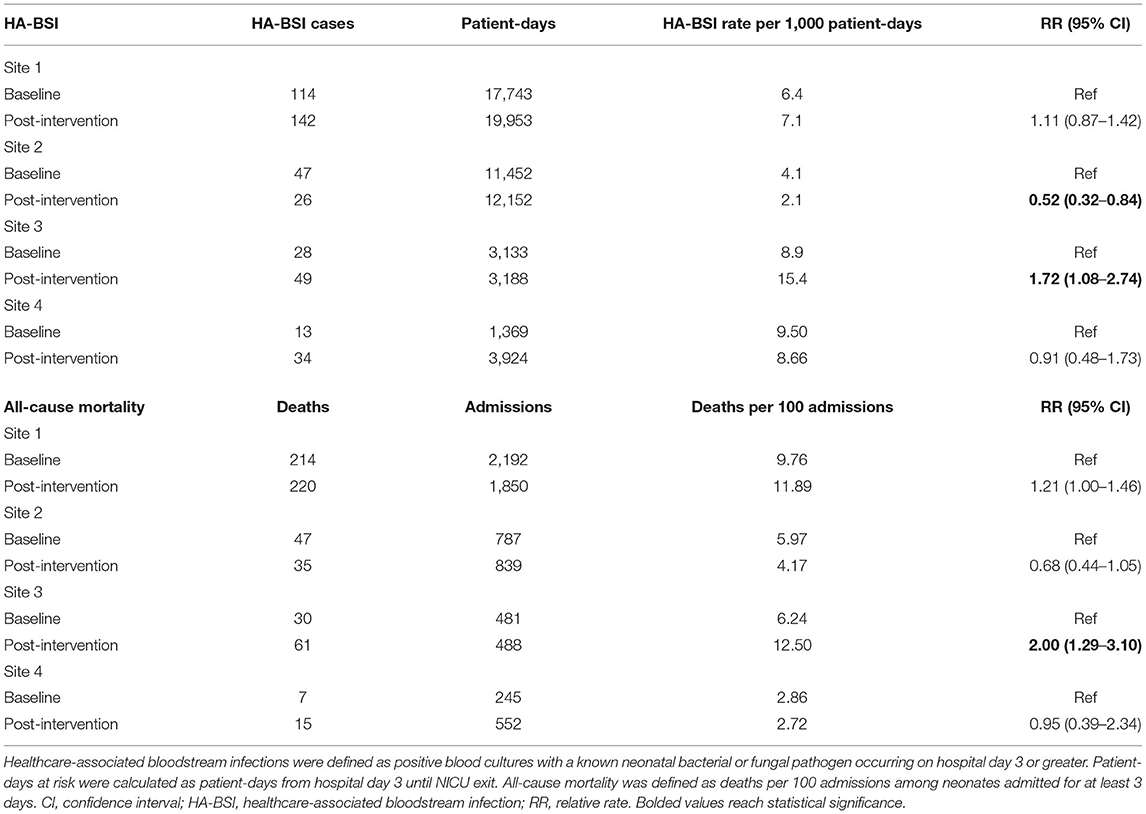
Table 3. Healthcare-associated bloodstream infection rate and all-cause mortality at baseline and post-intervention, by site.
All-Cause Mortality
Monthly all-cause mortality was unchanged from baseline to the post-intervention period across the four sites (RR 1.00, 95% CI 0.69–1.46) (Figure 3). Sites 1, 2, and 4 had no change in monthly all-cause mortality, whereas site 3 had an increase from baseline to post-intervention (RR 2.00; 95% CI 1.29–3.10) (Table 3).
Patient Safety Culture
Respondent Characteristics
The baseline HSOPS was completed by 182 respondents (response rate 85.8%). The follow-up HSOPS was completed by 212 respondents (response rate 99.1%) (Table 4). The majority of respondents were nurses, 163 (89.6%) at baseline and 182 (85.0%) at follow-up. All respondents identified as having direct patient contact.
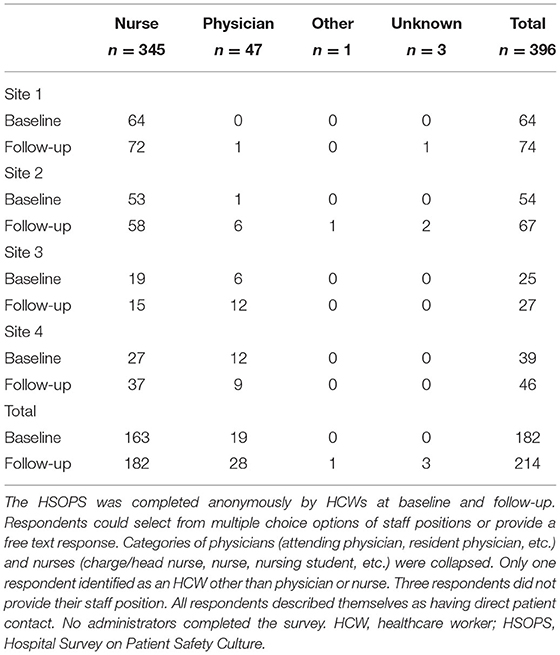
Table 4. Hospital Survey on Patient Safety Culture respondents by healthcare worker role at baseline and follow-up, by site.
Survey Results
High-scoring dimensions at baseline included teamwork within units (mean PPS 81.7% across all sites), supervisor/manager expectations and actions promoting patient safety (78.0%), organizational learning—continuous improvement (85.9%), and patient safety grade (81.8%). Improvements in mean PPS were seen in key dimensions of patient safety culture, with the largest increases in management support for patient safety (+7.6%), teamwork within units (+5.3%), management support for patient safety (+4.7%), and supervisor/manager expectations and actions promoting patient safety (+3.4%). Notably, there was a decrease in communication openness (−10.8%) and patient safety grade (−5.2%).
Survey responses varied by site (Table 5; Supplementary Figures 1a–m). For site 1, the largest gains were in frequency of event reporting (+30.3%), teamwork within units (+15.7%), teamwork across units (+11.9%), and management support for patient safety (+11.1%). For site 2, the composite domains with the greatest increases were non-punitive response to errors (+8.8%), organizational learning—continuous improvement (+8.4%), management support for patient safety (+6.6%), and staffing (+4.2%). For site 3, the largest gains were in supervisor/manager expectations & actions promoting patient safety (+11.7%), teamwork within units (+10.8%), non-punitive response to errors (+8.1%), and handoffs and transitions (+6.2%). For site 4, the greatest improvement was seen in management support for patient safety (+9.9%), patient safety grade (+4.9%), staffing (+3.8%), and organizational learning—continuous improvement (+2.8%).
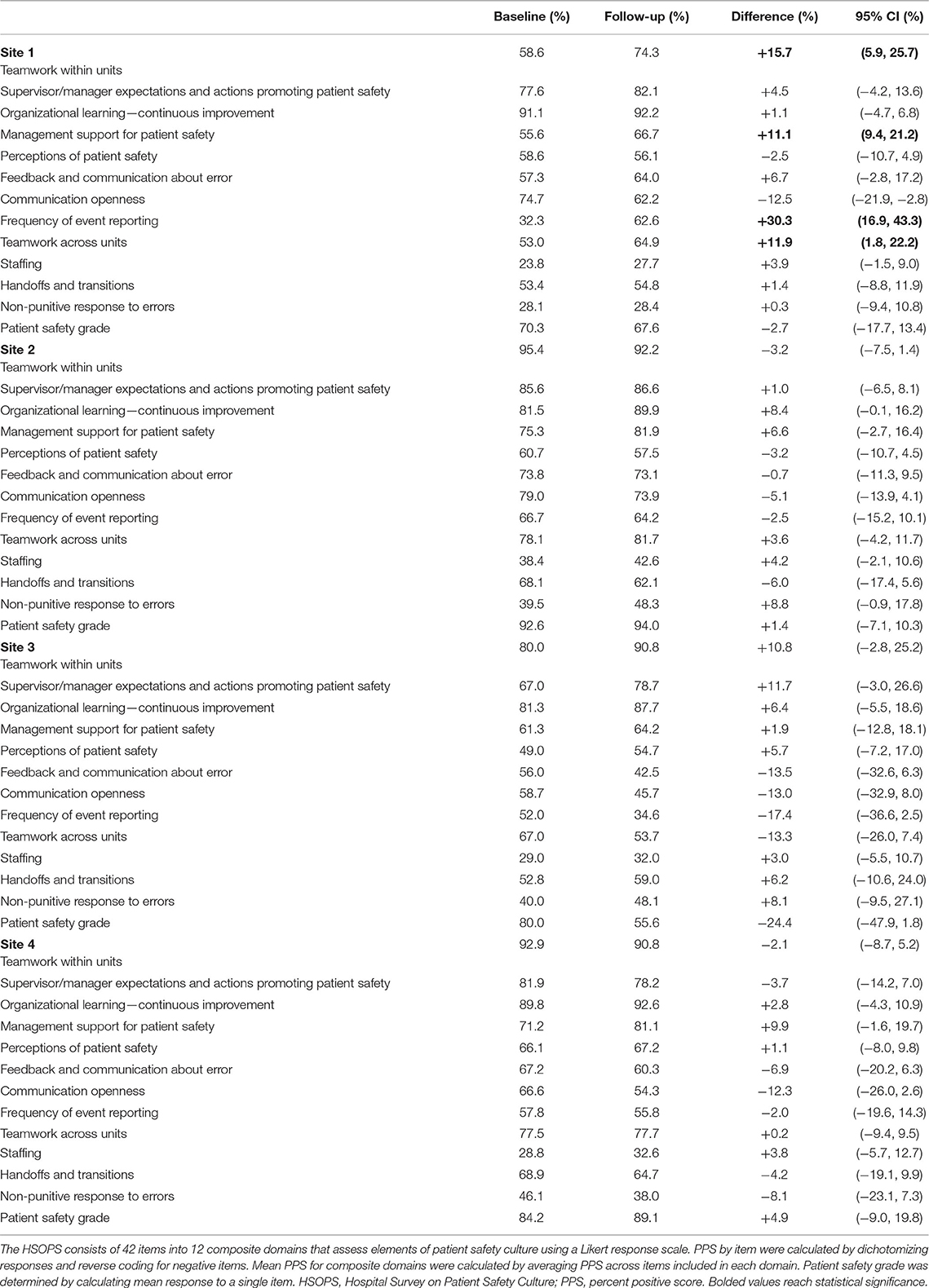
Table 5. Mean percent positive scores by composite dimension, baseline and follow-up Hospital Survey on Patient Safety Culture by site.
In exploring overall trends, all four sites demonstrated improvements in the following composite domains: organizational learning—continuous improvement, management support for patient safety, and staffing. Communication openness was the only composite domain that had decreased follow-up scores at all sites.
Workload
Workload increased across all six domains from baseline to post-intervention periods (Table 6). Mental demand increased from a mean of 7.44 ± 4.35 to 11.16 ± 5.20 (p < 0.0001), physical demand from 7.57 ± 4.41 to 11.95 ± 4.85 (p < 0.0001), temporal demand from 7.55 ± 4.47 to 10.60 ± 4.25 (p < 0.0001), effort from 8.15 ± 4.06 to 11.10 ± 4.37 (p < 0.0001), performance from 10.07 ± 12.15 (p < 0.0001), and frustration from 5.50 ± 2.94 to 8.11 ± 4.45 (p < 0.0001). Overall workload increased from 46.28 ± 16.97 to 65.07 ± 19.05 (p < 0.0001).

Table 6. Workload among neonatal intensive care unit staff at baseline and post-intervention, as measured by NASA-TLX.
Discussion
Our study fostered the creation of multidisciplinary CUSP teams that collaboratively selected and implemented interventions to improve IPC practices in three focus areas, hand hygiene, aseptic technique for invasive procedures, and medication and IV fluid preparation and administration. CUSP enabled sites to pursue multimodal IPC improvement strategies that included a focus on patient safety culture, as championed by the WHO (29). This intervention led to an increase in hand hygiene but did not reduce HA-BSI or all-cause mortality during the study period. While one site did have a reduction in HA-BSI rate, another site experienced an increase in both HA-BSI and mortality, which was largely driven by an outbreak that occurred during the post-intervention period. The CUSP team was instrumental in developing an outbreak response and focusing on appropriate IPC interventions, including a heightened focus on the importance of hand hygiene.
CUSP did lead to process improvements known to reduce infection risk, including a marked improvement in hand hygiene and successful implementation of a central line insertion checklist. The success of CUSP implementation can also be measured by the observed culture change and practice changes. Over the course of the study period, it was evident that nurses became empowered to speak up in front of leadership and advocate for patient safety and nurses attending CUSP meetings increasingly felt ownership and pride in the interventions they were leading. Furthermore, monthly coaching calls facilitated sharing of strategies and dissemination of interventions among sites, serving as a new forum for collaboration among NICUs facing similar challenges.
All sites demonstrated improved hand hygiene over the course of the study period. Implementing a program of hand hygiene compliance monitoring along with feedback of data to CUSP teams and unit staff, constituted a powerful intervention. While all sites previously employed some form of hand hygiene compliance monitoring by infection control, there was no consistent feedback or sharing of data with unit-level staff prior to CUSP implementation. Monthly hand hygiene data provided direct feedback to CUSP teams regarding the impact of their interventions and provided an opportunity to tailor interventions to specific HCW roles and moments of hand hygiene as needed. At the end of the study, sites committed to continue hand hygiene compliance monitoring and feedback of data.
Implementation of a central line insertion checklist are evidence-based practices that represented a paradigm shift in patient safety for these NICUs (30, 31). Prior to CUSP, none of the participant NICUs used pre-operative or pre-procedural checklists. Sites readily adapted its use into daily medical practice, with gradual increases in appropriate completion of checklists used. With checklist implementation, the importance of having an observer or assistant present for central line insertion was highlighted, which can be challenging in a resource-limited setting. The checklist also empowered nurses or other HCWs serving in the observer/assistant role to intervene if steps of appropriate aseptic technique were not followed. By site request, a central line maintenance audit tool was created by the study team, though its completion was not audited by study staff. Both the insertion checklist and the maintenance audit tool fit well into the existing healthcare system at our four sites, with checklists used for a variety of other indications.
During our baseline IPC assessments, we noted opportunities for improvement at all sites for practices related to medication and IV fluid preparation and administration. In a resource-limited setting, challenges to injection safety include reliance on multi-dose vials, reuse of single-dose vials, and large stock bottles of IV fluid solutions and topical antiseptics including alcohol and betadine, as well as preparation of medications and IV fluids within the immediate patient care area (32, 33). While it was not possible to transition to exclusive use of single-dose vials and eliminate use of large stock bottles, CUSP teams focused on how to improve injection safety by including IPC considerations in adapting existing workflow.
Multiple studies have demonstrated that improving patient safety culture across HSOPS domains is associated with lower HAI rates (34, 35). Sites demonstrated gains in key HSOPS domains of patient safety, including teamwork within units, supervisor/manager expectations and actions promoting patient safety, organizational learning—continuous improvement, and management support for patient safety. In considering the elements of the CUSP intervention, these are the domains in which one would expect improvement. Most gains did not reach statistical significance which likely reflects a relatively fixed sample size of HCWs employed within each unit. Our response rates for both baseline and follow-up surveys were excellent and we hope to explore whether these trends continue and assess generalizability of our findings by recruiting more sites.
We did not expect to improve other domains, such as staffing and teamwork across units, which were outside of the scope of our intervention. The notable decrease in communication openness across all sites should be explored further and addressed in moving CUSP forward. We did not see a significant improvement in patient safety grade, which consists of a single item asking respondents to assign a letter grade to their unit's patient safety. It is not surprising that respondents are more critical of patient safety after an intervention that raises knowledge and awareness of IPC practices and their impact on patient safety.
As measured by NASA-TLX across six domains, workload increased from baseline to the post-intervention period. To our knowledge, NASA-TLX assessment of workload has not previously been used in the context of CUSP implementation. Tubbs-Cooley et al. previously measured overall workload among neonatal, pediatric, and adult intensive care nurses using NASA-TLX; among NICU nurses who participated in this multi-center cross-sectional study, the mean overall workload was similar to that reported on our study, roughly midway between our baseline and post-intervention scores (36). CUSP implementation required a comprehensive unit-level shift in the approach to IPC and patient safety. While CUSP activities were led by the physician and nurse champions in conjunction with the CUSP team, selected interventions within the three focus areas required participation and commitment by all unit staff, especially those providing direct patient care. CUSP may have contributed to the increase in workload seen over the course of this study, though other unmeasured factors such as staffing changes or more complex patient load could have also contributed. Effect of CUSP activities on perceived workload should be monitored closely, given the association of increased NASA-TLX scores with HCW burnout (37). Furthermore, a single-center study in a United States NICU described an association between increased nursing workload with missed nursing care (38). CUSP should prioritize interventions that lighten workload by making work more efficient and less burdensome, though advocating for improved staffing may also be a critical CUSP activity.
Our intervention coincided with an increased focus on patient safety by the Indian Ministry of Health. Multiple sites underwent accreditation or government official visits during the study period. Our intervention aligned well with this mission, especially with regard to monitoring of hand hygiene compliance and use of a central line insertion checklist. Senior executive support of CUSP-driven interventions led to spread beyond the NICU, with adaptation of some interventions throughout the hospital.
Strengths of this study include use of a multidisciplinary team that worked together in an iterative process that allows for learning and is firmly grounded in creation of local patient safety culture to reduce HAI risk. This study demonstrated the ready adaptation of an existing toolkit that has proven success to a resource-limited setting. The selected focus areas included high-yield IPC practices, optimization of which has been linked to reduction of HA-BSI in a variety of healthcare settings. Site-driven selection of interventions, rather than a prepackaged IPC bundle, yielded locally appropriate solutions to IPC gaps that are more likely to be sustainable than financially burdensome interventions.
Limitations of this study include its duration and small sample size. A 16-month study period limited our capacity to assess the impact of the intervention on HA-BSI rates and mortality, especially given seasonality of infections in this setting, with higher rates seen during monsoon season. Additionally, the final focus area, medication and IV fluid preparation and administration, was introduced only 3 months prior to study end, limiting our capacity to assess the impact of selected interventions on outcomes of interest. However, improved hand hygiene and gains seen in patient safety culture are promising measures of success of this intervention. Though the advent of the coronavirus disease 2019 pandemic disrupted CUSP activities, sites have committed to sustaining the CUSP intervention. We intend to complete a follow-up assessment of the impact of CUSP, which will provide important information about CUSP sustainability in this setting.
CUSP is a promising multimodal strategy for healthcare facilities in resource-limited settings that encompasses key aspects of the WHO's IPC improvement strategy, including culture of safety. Our study outlines an approach to CUSP that can be readily adapted to NICUs in an LMIC setting and is feasible. Next steps include assessment of sustainability and generalizability of our findings.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Johns Hopkins Medicine Institutional Review Board, Byramjee-Jeejeebhoy Government Medical College Ethics Committee, Dr. D. Y. Patil Medical College Ethics Committee, King Edward Memorial Hospital Ethics Committee, Bharati Vidyapeeth Medical College Ethics Committee. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
BR and AKa supported data collection. JJ and EC analyzed the data. JJ drafted the initial manuscript. All authors conceptualized and designed the study and contributed to the manuscript revision.
Funding
This study was supported by the United States Centers for Disease Control and Prevention (Safe Healthcare, Epidemiology, and Prevention Research Development Program Domain 7, Contract 200-2016-91781). JJ receives support from the National Institutes of Health (K23HD100594). MR receives support from the National Institutes of Health (UM1AI104681). VM receives support from the National Institutes of Health (UM1AI069465-13, 1R01AI43748-01A1). AG receives support from the National Institutes of Health (UM1AI069465, UM1AI068632, and UM1AI068636). AM receives support from the National Institutes of Health (K24AI141580).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors wish to thank the NICU staff who participated in this study.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2021.794637/full#supplementary-material
References
1. World Health Organization. Survive and Thrive: Transforming Care for Every Small and Sick Newborn. (2019). Available online at: https://https://www.who.int/maternal_child_adolescent/documents/care-small-sick-newborns-survive-thrive/en/ (accessed October 13, 2021).
2. Polin RA, Denson S, Brady MT. Epidemiology and diagnosis of health care-associated infections in the NICU. Pediatrics. (2012) 129:e1104–9. doi: 10.1542/peds.2012-0147
3. Hooven TA, Polin RA. Healthcare-associated infections in the hospitalized neonate: a review. Early Hum Dev. (2014) 90(Suppl. 1):S4–6. doi: 10.1016/S0378-3782(14)70002-7
4. Storr J, Twyman A, Zingg W, Damani N, Kilpatrick C, Reilly J, et al. Core components for effective infection prevention and control programmes: new WHO evidence-based recommendations. Antimicrob Resist Infect Control. (2017) 6:6. doi: 10.1186/s13756-016-0149-9
5. Zaidi AK, Huskins WC, Thaver D, Bhutta ZA, Abbas Z, Goldmann DA. Hospital-acquired neonatal infections in developing countries. Lancet. (2005) 365:1175–88. doi: 10.1016/S0140-6736(05)71881-X
6. Tsai MH, Chu SM, Hsu JF, Lien R, Huang HR, Chiang MC, et al. Risk factors and outcomes for multidrug-resistant Gram-negative bacteremia in the NICU. Pediatrics. (2014) 133:e322–9. doi: 10.1542/peds.2013-1248
7. Hsu AJ, Tamma PD. Treatment of multidrug-resistant Gram-negative infections in children. Clin Infect Dis. (2014) 58:1439–48. doi: 10.1093/cid/ciu069
8. Laxminarayan R, Matsoso P, Pant S, Brower C, Rottingen JA, Klugman K, et al. Access to effective antimicrobials: a worldwide challenge. Lancet. (2016) 387:168–75. doi: 10.1016/S0140-6736(15)00474-2
9. World Health Organization. Guide to Implementation: a Guide to the Implementation of the WHO Multimodal Hand Hygiene Improvement Strategy. (2009). Available online at: https://www.who.int/gpsc/5may/Guide_to_Implementation.pdf (accessed October 13, 2021).
10. World Health Organization. WHO multimodal improvement strategy. Available online at: https://www.who.int/infection-prevention/publications/ipc-cc-mis.pdf?ua=1 (accessed October 13, 2021).
11. Pronovost P, Needham D, Berenholtz S, Sinopoli D, Chu H, Cosgrove S, et al. An intervention to decrease catheter-related bloodstream infections in the ICU. N Engl J Med. (2006) 355:2725–32. doi: 10.1056/NEJMoa061115
12. Hsu YJ, Marsteller JA. Influence of the comprehensive unit-based safety program in ICUs: evidence from the keystone ICU project. Am J Med Qual. (2016) 31:349–57. doi: 10.1177/1062860615571963
13. Hong AL, Sawyer MD, Shore A, Winters BD, Masuga M, Lee H, et al. Decreasing central-line-associated bloodstream infections in Connecticut intensive care units. J Healthc Qual. (2013) 35:78–87. doi: 10.1111/j.1945-1474.2012.00210.x
14. Lin DM, Weeks K, Holzmueller CG, Pronovost PJ, Pham JC. Maintaining and sustaining the on the CUSP: stop BSI model in Hawaii. Jt Comm J Qual Patient Saf. (2013) 39:51–60. doi: 10.1016/S1553-7250(13)39008-4
15. Sood G, Caffrey J, Krout K, Khouri-Stevens Z, Gerold K, Riedel S, et al. Use of implementation science for a sustained reduction of central-line-associated bloodstream infections in a high-volume, regional burn unit. Infect Control Hosp Epidemiol. (2017) 38:1306–11. doi: 10.1017/ice.2017.191
16. Latif A, Kelly B, Edrees H, Kent PS, Weaver SJ, Jovanovic B, et al. Implementing a multifaceted intervention to decrease central line-associated bloodstream infections in SEHA (Abu Dhabi Health Services Company) intensive care units: the Abu Dhabi experience. Infect Control Hosp Epidemiol. (2015) 36:816–22. doi: 10.1017/ice.2015.70
17. Khan RM, Aljuaid M, Aqeel H, Aboudeif MM, Elatwey S, Shehab R, et al. Introducing the comprehensive unit-based safety program for mechanically ventilated patients in Saudi Arabian intensive care units. Ann Thorac Med. (2017) 12:11–6. doi: 10.4103/1817-1737.197765
18. Pitts SI, Maruthur NM, Luu NP, Curreri K, Grimes R, Nigrin C, et al. Implementing the Comprehensive Unit-Based Safety Program (CUSP) to improve patient safety in an academic primary care practice. Jt Comm J Qual Patient Saf. (2017) 43:591–7. doi: 10.1016/j.jcjq.2017.06.006
19. Ogrinc G, Davies L, Goodman D, Batalden P, Davidoff F, Stevens D, et al. 2. 0 (Standards for QUality Improvement Reporting Excellence): revised publication guidelines from a detailed consensus process. BMJ Qual Safety. (2016) 25:986–92. doi: 10.1136/bmjqs-2015-004411
20. Weaver SJ, Lofthus J, Sawyer M, Greer L, Opett K, Reynolds C, et al. A collaborative learning network approach to improvement: the CUSP learning network. Jt Comm J Qual Patient Saf. (2015) 41:147–59. doi: 10.1016/S1553-7250(15)41020-7
21. Helder OK, Brug J, Looman CW, van Goudoever JB, Kornelisse RF. The impact of an education program on hand hygiene compliance and nosocomial infection incidence in an urban neonatal intensive care unit: an intervention study with before and after comparison. Int J Nurs Stud. (2010) 47:1245–52. doi: 10.1016/j.ijnurstu.2010.03.005
22. Huskins C, Ross-Degnan D, Goldmann DA. Improving infection control in developing countries: the infection control assessment tool. BMC Proc. (2011) 5:O18. doi: 10.1186/1753-6561-5-S6-O18
23. Strengthening Pharmaceutical Systems. Infection Control Assessment Tool. 2nd ed. Arlington, VA: Management Sciences for Health (2009).
24. World Health Organization. WHO Guidelines on Hand Hygiene in Health Care. (2009). Available online at: https://apps.who.int/iris/bitstream/handle/10665/44102/9789241597906_eng.pdf?sequence=1 (accessed October 13, 2021).
25. Centers for Disease Control Prevention. NHSN Patient Safety Component Manual. (2020). Available online at: https://www.cdc.gov/nhsn/pdfs/pscmanual/pcsmanual_current.pdf (accessed October 13, 2021).
26. Johnson J, Robinson ML, Rajput UC, Valvi C, Kinikar A, Parikh TB, et al. High burden of bloodstream infections associated with antimicrobial resistance and mortality in the neonatal intensive care unit in Pune, India. Clin Infect Dis. (2021) 73:271–80. doi: 10.1093/cid/ciaa554
27. Harnoss JC, Dancer SJ, Kaden CF, Baguhl R, Kohlmann T, Papke R, et al. Hand antisepsis without decreasing efficacy by shortening the rub-in time of alcohol-based handrubs to 15 seconds. J Hosp Infect. (2020) 104:419–24. doi: 10.1016/j.jhin.2019.09.004
28. National Aeronautics Space Administration. NASA-TLX. Available online at: https://humansystems.arc.nasa.gov/groups/tlx/publications.php (accessed October 13, 2021).
29. World Health Organization. Guidelines on Core Components of Infection Prevention and Control Programmes at the National and Acute Health Care Facility Level. Geneva: World Health Organization (2016).
30. Marschall J, Mermel LA, Fakih M, Hadaway L, Kallen A, O'Grady NP, et al. Strategies to prevent central line-associated bloodstream infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol. (2014) 35:753–71. doi: 10.1086/676533
31. Blot K, Bergs J, Vogelaers D, Blot S, Vandijck D. Prevention of central line-associated bloodstream infections through quality improvement interventions: a systematic review and meta-analysis. Clin Infect Dis. (2014) 59:96–105. doi: 10.1093/cid/ciu239
32. Curless MS. RC, Thompson E, Trexler PA, editors. Infection Prevention and Control: Reference Manual for Health Care Facilities with Limited Resources. Baltimore, MD: Jhpiego (2018).
33. World Health Organization. WHO Best Practices for Injections and Related Procedures Toolkit. Geneva: WHO Press (2010). Available online at: https://apps.who.int/iris/bitstream/handle/10665/44298/9789241599252_eng.pdf?sequence=1 (accessed October 13, 2021).
34. Weaver SJ, Weeks K, Pham JC, Pronovost PJ. On the CUSP: stop BSI: evaluating the relationship between central line-associated bloodstream infection rate and patient safety climate profile. Am J Infect Control. (2014) 42(10 Suppl.):S203–8. doi: 10.1016/j.ajic.2014.05.020
35. Fan CJ, Pawlik TM, Daniels T, Vernon N, Banks K, Westby P, et al. Association of safety culture with surgical site infection outcomes. J Am Coll Surg. (2016) 222:122–8. doi: 10.1016/j.jamcollsurg.2015.11.008
36. Tubbs-Cooley HL, Mara CA, Carle AC, Gurses AP. The NASA task load index as a measure of overall workload among neonatal, paediatric and adult intensive care nurses. Intensive Crit Care Nurs. (2018) 46:64–9. doi: 10.1016/j.iccn.2018.01.004
37. Harry E, Sinsky C, Dyrbye LN, Makowski MS, Trockel M, Tutty M, et al. Physician task load and the risk of burnout among US physicians in a national survey. Jt Comm J Qual Patient Saf. (2021) 47:76–85. doi: 10.1016/j.jcjq.2020.09.011
Keywords: neonate, healthcare-associated infection, patient safety, hand hygiene, aseptic technique, patient safety culture, multimodal strategy, bloodstream infection
Citation: Johnson J, Latif A, Randive B, Kadam A, Rajput U, Kinikar A, Malshe N, Lalwani S, Parikh TB, Vaidya U, Malwade S, Agarkhedkar S, Curless MS, Coffin SE, Smith RM, Westercamp M, Colantuoni E, Robinson ML, Mave V, Gupta A, Manabe YC and Milstone AM (2022) Implementation of the Comprehensive Unit-Based Safety Program to Improve Infection Prevention and Control Practices in Four Neonatal Intensive Care Units in Pune, India. Front. Pediatr. 9:794637. doi: 10.3389/fped.2021.794637
Received: 13 October 2021; Accepted: 13 December 2021;
Published: 06 January 2022.
Edited by:
Shi Yuan, Children‘s Hospital of Chongqing Medical University, ChinaReviewed by:
Tuuli Metsvaht, University of Tartu, EstoniaShan He, The First People's Hospital of Yunnan Province, China
Copyright © 2022 Johnson, Latif, Randive, Kadam, Rajput, Kinikar, Malshe, Lalwani, Parikh, Vaidya, Malwade, Agarkhedkar, Curless, Coffin, Smith, Westercamp, Colantuoni, Robinson, Mave, Gupta, Manabe and Milstone. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Julia Johnson, ampvaG4yNDVAamhtaS5lZHU=
 Julia Johnson
Julia Johnson Asad Latif
Asad Latif Bharat Randive
Bharat Randive Abhay Kadam
Abhay Kadam Uday Rajput6
Uday Rajput6 Aarti Kinikar
Aarti Kinikar Nandini Malshe
Nandini Malshe Tushar B. Parikh
Tushar B. Parikh Sudhir Malwade
Sudhir Malwade Melanie S. Curless
Melanie S. Curless Susan E. Coffin
Susan E. Coffin Rachel M. Smith
Rachel M. Smith Matthew Westercamp
Matthew Westercamp Matthew L. Robinson
Matthew L. Robinson Vidya Mave
Vidya Mave Amita Gupta
Amita Gupta Yukari C. Manabe
Yukari C. Manabe Aaron M. Milstone
Aaron M. Milstone