- Department of Ophthalmology, Weill Cornell Medicine, New York Presbyterian Hospital, New York, NY, United States
Retinopathy of prematurity (ROP) is a leading cause of childhood blindness that occurs due to incomplete development of retinal blood vessels in preterm infants. Glaucoma is an ocular comorbidity in some patients with ROP, and it may be associated with immature anterior chamber development, ROP itself, or the treatment for ROP. There have been a few reports of narrow-angle glaucoma after laser treatment for ROP. In this case report, we describe the course of a female infant born at 24 weeks and 5 days of gestational age with treatment-requiring ROP treated with laser photocoagulation who subsequently developed very elevated intraocular pressure and shallow anterior chambers without pupillary block. The patient required bilateral ab externo trabeculotomy for elevated intraocular pressure, which normalized after the procedure. The patient has remained stable at the last follow-up at 51 weeks postmenstrual age. Differing from previous glaucoma presentations in this setting, we illustrate a case of elevated intraocular pressure and anterior chamber narrowing after laser therapy without pupillary block or synechiae. The possible multifactorial etiology of glaucoma in this patient, including incomplete angle development, ischemia, and laser treatment, highlight the need for glaucoma screening in patients with ROP, both in the short and long term.
Introduction
Retinopathy of prematurity (ROP) is a disorder of incomplete development of retinal blood vessels in preterm infants (1). Although titration of supplemental oxygen, which has been shown to decrease ischemic drive, has decreased the incidence of ROP, this condition remains a leading cause of childhood blindness in the United States (2) and throughout the world (3). The main goals of treatment are to optimize long-term visual outcomes by preventing complications of ROP such as retinal detachment (4). Laser photocoagulation has replaced cryotherapy as the standard of care for treatment-requiring ROP (5, 6), while intravitreal antivascular endothelial growth factor (anti-VEGF) injections are also used with similar efficacy (5), particularly in posterior ROP (6).
Treatment of ROP has known potential complications, including cataract, inflammation, vitreous hemorrhage, choroidal detachment, retinal detachment, and glaucoma (7, 8). Patients with ROP are at increased risk for glaucoma, which can be attributed to retrolental tissue pushing of the lens–iris diaphragm forward (9, 10), as well as pupillary block or neovascularization (11, 12).
The Early Treatment for Retinopathy of Prematurity (ETROP) trial found a 1.67% (12/718) prevalence of glaucoma at 6 years old (9, 10), with 11 out of these 12 children having received laser therapy for high-risk pre-threshold ROP (13). There are few cases reported of narrow angle or angle-closure glaucoma following laser for ROP (14–16).
In this case report, we describe the course of an ex-24-week-old female infant who developed very elevated intraocular pressure and shallow anterior chambers without pupillary block at postmenstrual age of 38 weeks following laser treatment in both eyes for type 1 ROP (zone 2 stage 3 with plus disease). Examination was remarkable for corneal haze that precluded gonioscopy and shallow anterior chambers without pupillary block or neovascularization. Genetic testing for the most common causes of congenital glaucoma was negative. There was significant improvement in the anterior chamber (AC) depth with cycloplegia; however, the patient ultimately required bilateral ab externo trabeculotomy for adequate intraocular pressure control. This case highlights that glaucoma in the setting of ROP may be multifactorial and should be regularly screened for in any at-risk infant.
Case
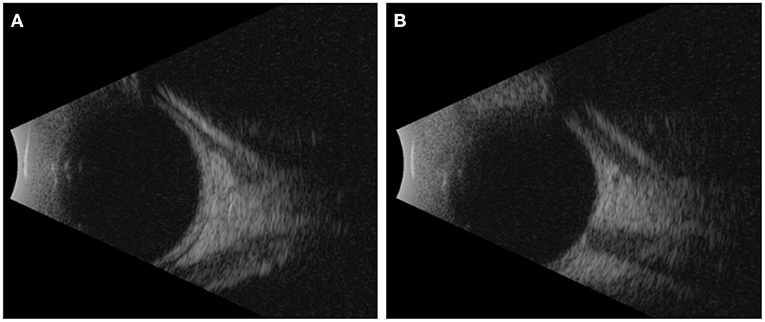
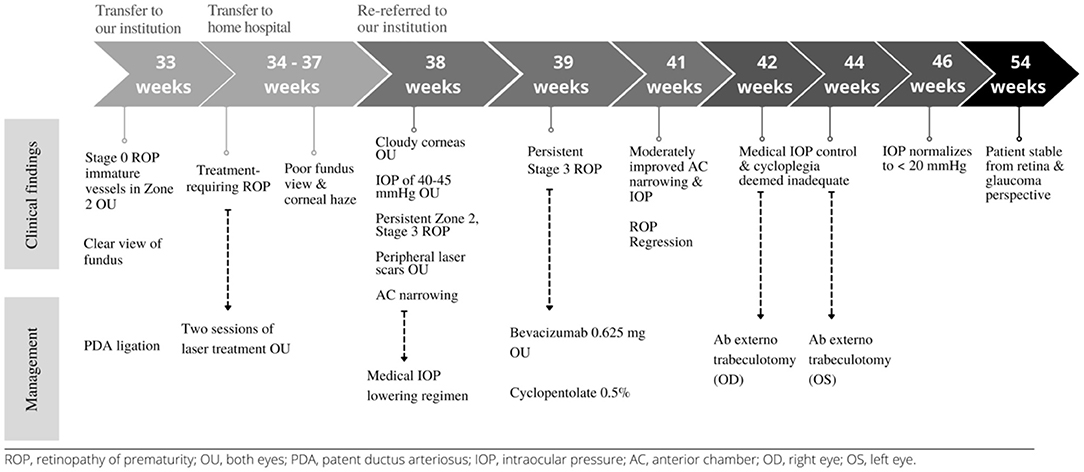
A 450-g female infant was born at 24 weeks and 5 days of gestational age by normal spontaneous vaginal delivery at an outside hospital and transferred to our institution at a postmenstrual age (PMA) of 33 weeks and 2 days for patent ductus arteriosus ligation. At our institution, she underwent an initial ROP screening, which showed stage 0 immature vessels in zone 2 of both eyes. There were clear views of the fundus in both eyes. The patient was then transferred back to the home referring hospital where she underwent two sessions of diode laser in both eyes at 36 and 37 weeks of PMA for treatment-requiring ROP. Due to concern for inadequate laser and poor fundus view with corneal haze, she was re-referred to our institution. Upon reevaluation, she was noted to have cloudy corneas, intraocular pressure (IOP) of 40–45 mmHg, and persistent zone 2, stage 3 ROP, with peripheral laser scars in both eyes (Figure 1).
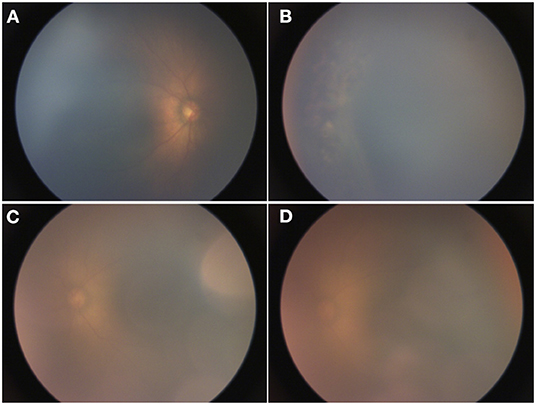
Figure 1. RetCam images taken at 37 weeks of postmenstrual age (PMA). (A) Right eye with zone 2, stage 3 retinopathy of prematurity (ROP), (B) limited view of laser scars in the periphery of the right eye, and (C,D) left eye with zone 2, stage 3 ROP.
On exam and diagnostic imaging with B-scan ultrasound, there was no rubeosis, and no choroidal or retinal detachments were noted (Figure 2). Clinical examination and ultrasound biomicroscopy (UBM) revealed significant anterior chamber shallowing without pupillary block or synechiae, which improved significantly with topical cycloplegia with cyclopentolate 0.5% (Figure 3). With oral acetazolamide and topical IOP-lowering eyedrops, her pressures improved but were still elevated to the 30- to 35-mmHg range, and the corneal clouding still prevented adequate gonioscopic visualization of angle anatomy. Fundus examination revealed persistent stage 3 ROP with inadequate laser, particularly nasally; however, the view was still somewhat limited for additional laser photocoagulation (Figure 1). She underwent intravitreal injection of bevacizumab 0.625 mg in both eyes at 39 weeks of PMA. In both eyes, regression of ROP after laser and intravitreal bevacizumab was noted by 41 weeks of PMA (2 weeks after injections). Despite moderate improvement in the anterior chamber depth (Figure 3) and IOP, medical treatments were ultimately determined to be inadequate, and the patient required ab externo trabeculotomy in the right eye at 42 weeks of PMA and left eye at 44 weeks of PMA. With parental consent, genetic screening for congenital glaucoma through the Prevention Genetics Glaucoma Panel was obtained and found to be negative.
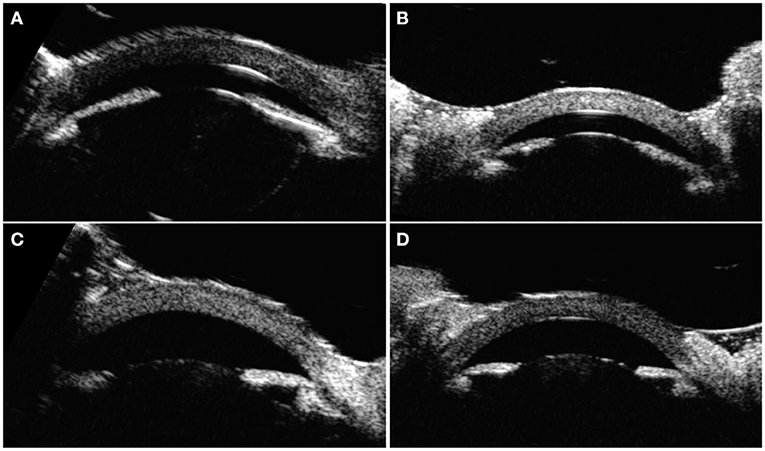
Figure 3. Ultrasound biomicroscopy images taken at 40 and 41 weeks of PMA. (A) Right eye before cyclopegia. (B) Left eye before cyclopegia. (C) Right eye after cyclopegia. (D) Left eye after cyclopegia.
The intraocular pressures normalized to under 20 mmHg by postoperative week 2 after trabeculotomy in both eyes. The patient has remained stable from both a retina and glaucoma perspective at the last follow-up at 51 weeks of PMA in the office. Of note, cycloplegic refraction revealed −8.00 and −2.00 D myopia in the right and left eyes, respectively, for which she was prescribed spectacle correction. The timeline of clinical findings and management of this patient are presented (Figure 4). Written informed consent was obtained from the legal guardian of the minor for the publication of any potentially identifiable images or data included in this article.
Discussion
The pathogenesis of glaucoma in ROP has various proposed mechanisms including incomplete development of the anterior segment and secondary angle closure from ROP or the treatment of ROP. Given the presentation and exam findings of our patient, it is possible that underlying incomplete development of her anterior segment structure, as well as ROP, may have put her at increased risk for glaucoma that was further exacerbated by ROP laser treatment though no effusions or clear sequelae of this were observed.
There are few cases in the literature describing glaucoma in the short-term postoperative period after ROP laser (14–16). The cases requiring surgical intervention presented with shallow or flat AC depth and had documented posterior synechiae with pupillary block in infants with gestational ages ranging from 24 to 29 weeks (14). A report from Australia described the case of a male infant of 24 weeks of gestational age receiving laser therapy for stage 2 zone 3 ROP who was later found to have pupillary block and angle closure in the right eye as well as anatomic narrow angle in the left eye (15). A third report described a female infant of 25 weeks of gestational age who received laser photocoagulation for ROP in both eyes (stage 2, zone 2 with plus disease), after which she developed total posterior synechiae and shallow ACs (16).
In our case, the initial treatment with topical cycloplegia and IOP-lowering topical and oral medications led to deepening of the anterior chamber as well as moderate, though ultimately insufficient, improvement of the IOP. Normalization of IOP was achieved after ab externo trabeculotomy in both eyes. This points to a possible mixed mechanism of glaucoma in infants with ROP after laser therapy: (1) abnormal angle anatomy from prematurity or underlying genetic predisposition, and (2) ciliary body rotation, possibly exacerbated by laser. In contrast to the previously described cases in the literature (14–16), our case illustrates a presentation of elevated IOP and anterior chamber narrowing after laser therapy without pupillary block or synechiae.
Prematurity itself introduces some structural risks that may contribute to glaucoma. Development of the trabecular meshwork is not complete until late in gestation, after at least 25 weeks, which makes the angle anatomy susceptible to many factors that can potentially influence risk of angle-closure glaucoma (17). Other predisposing anterior segment abnormalities observed in premature children, with and without ROP, include steep corneal curvature, decreased anterior chamber depth, anteriorly displaced iris planes, and increased lens thickness (10, 18–22). Eyes with ROP not requiring treatment as well as ROP-treated eyes have been found to have narrower anterior chamber angles (ACA) than full-term children (22) or preterm monitored eyes (23). These changes may also explain the high prevalence and magnitude of myopia in preterm children (24), and the even higher apparent risk in those with laser-treated ROP (21). It is notable that our patient demonstrated a high degree of myopia in right eye and a moderate degree of myopia in the left eye at just 11 months of PMA.
Premature infants with ROP likely acquire other additional pathologic features that put them at additional risk of glaucoma. The anterior segment changes observed in premature infants with ROP could be further exacerbated by an arrested state of retinal development, such that the local growth signals involved in anterior segment development are altered (24). Additionally, laser treatment is considered to contribute significantly to the development of narrow angles and anterior segment defects in children with ROP (23, 24). More specifically, laser-induced mechanical changes may impair development of the angle by affecting the posterior ciliary nerve, artery, or pars plana (23). While anterior chamber narrowing without closure has been previously described after laser for other conditions, the laser-induced anterior shifting and inward rotation of the ciliary body is typically short lived in older children and adults (25). In a case series of secondary glaucoma in children with ROP, all of the patients had shallow anterior chambers before the onset of glaucoma symptoms, so these patients might have had an initial anatomic compromise of the aqueous outflow subsequently exacerbated by other factors leading to high intraocular pressures (26). Likewise, in another study, shallow anterior chambers were noted to be a feature of most stage 3 ROP eyes, as a result of arrested development of the anterior segment, but with notable higher and more significant prevalence in laser-treated eyes (27). Given the presentation and exam findings of our patient, it is possible that underlying developmental anterior segment abnormalities, as well as ROP, may have put her at increased risk for glaucoma that was further exacerbated after ROP laser treatment. A potential future avenue for research would be to investigate the use of anti-VEGF injections as an alternative to laser in infants with significant narrow-angle glaucoma or anterior segment narrowing.
Laser treatment may induce structural anterior segment changes in infants with ROP and increase their vulnerability to complications, such as secondary glaucoma. Careful anterior segment examination in ROP infants should be undertaken to exclude glaucoma risk factors, such as shallow anterior chambers, rubeosis, and ocular hypertension. In particular, shallow anterior chambers are challenging to assess in premature eyes and can be overlooked unless accompanied by more obvious clinical signs of glaucoma like corneal clouding, enlarged corneal diameters, and blepharospasm (14). Glaucoma poses a vision-threatening risk in infants with ROP, due to premature development of the eye, as well as direct consequences of ROP and ROP treatment. While congenital glaucoma is a possible etiology in any infant with elevated intraocular pressure and cloudy corneas, this case highlights other contributory factors, such as prematurity itself, as well as laser for ROP, that should be considered.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
Written informed consent was obtained from the minors' legal guardian for the publication of any potentially identifiable images or data included in this article.
Author Contributions
TL, NL, and AO contributed to the conception and design of the report. TL, AO, VR, KK, and SV participated in the patient's care. TL and NL wrote the first draft of the manuscript. VR, KK, SV, and AO wrote sections of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The handling Editor declared a past collaboration with one of the authors TL.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Hellström A, Smith LEH, Dammann O. Retinopathy of prematurity. Lancet. (1991) 337:83. doi: 10.1016/0140-6736(91)90742-8
2. Kong L, Fry M, Al-Samarraie M, Gilbert C, Steinkuller PG. An update on progress and the changing epidemiology of causes of childhood blindness worldwide. J AAPOS. (2012) 16:501–7. doi: 10.1016/j.jaapos.2012.09.004
3. Sommer A, Taylor HR, Ravilla TD, West S, Lietman TM, Keenan JD, et al. Challenges of ophthalmic care in the developing world. J Am Med Assoc Ophthalmol. (2014) 132:640–4. doi: 10.1001/jamaophthalmol.2014.84
4. DeJonge MH, Ferrone PJ, Trese MT. Diode laser ablation for threshold retinopathy of prematurity: short- term structural outcome. Arch Ophthalmol. (2000) 118:365–7. doi: 10.1001/archopht.118.3.365
5. Hwang CK, Hubbard GB, Hutchinson AK, Lambert SR. Outcomes after intravitreal bevacizumab versus laser photocoagulation for retinopathy of prematurity: a 5-year retrospective analysis. Ophthalmology. (2015) 122:1008–15. doi: 10.1016/j.ophtha.2014.12.017
6. Mintz-Hittner H, Kennedy K, Chuang A. Efficacy of intravitreal bevacizumab for stage 3+ retinopathy of prematurity. N Engl J Med. (2011) 364:1007374. doi: 10.1056/NEJMoa1007374
8. Salgado C, Celik Y, VanderVeen D. Anterior segment complications after diode laser photocoagulation for prethreshold retinopathy of prematurity. Am J Ophthalmol. (2010) 150:17. doi: 10.1016/j.ajo.2009.12.017
9. Pollard ZF. Secondary angle-closure glaucoma in cicatricial retrolental fibroplasia. Am J Ophthalmol. (1980) 89:651–3. doi: 10.1016/0002-9394(80)90282-2
10. Hittner HM, Rhodes LM, McPherson AR. Anterior segment abnormalities in cicatricial retinopathy of prematurity. Ophthalmology. (1979) 86:803–16. doi: 10.1016/S0161-6420(79)35437-9
11. Smith J, Shivitz I. Angle-closure glaucoma in adults with cicatricial retinopathy of prematurity. Arch Ophthalmol. (1984) 102:371–2. doi: 10.1001/archopht.1984.01040030289020
12. Michael AJ, Pesin SR, Katz LJ, Tasman WS. Management of late-onset angle-closure glaucoma associated with retinopathy of prematurity. Ophthalmology. (1991) 98:1093–8. doi: 10.1016/S0161-6420(91)32172-9
13. Bremer DL, Rogers DL, Good W V, Tung B, Hardy RJ, Fellows R. Glaucoma in the Early Treatment for Retinopathy of Prematurity (ETROP) study. J AAPOS. (2012) 16:449. doi: 10.1016/j.jaapos.2012.06.011
14. Trigler L, Grey Weaver R, O'Neil JW, Barondes MJ, Freedman SF. Case series of angle-closure glaucoma after laser treatment for retinopathy of prematurity. J AAPOS. (2005) 9:17–21. doi: 10.1016/j.jaapos.2004.10.007
15. Lee GA, Lee LR, Gole GA. Angle-closure glaucoma after laser treatment for retinopathy of prematurity. J AAPOS. (1998) 2:383–4. doi: 10.1016/S1091-8531(98)90042-8
16. Uehara A, Kurokawa T, Gotoh N, Yoshimura N, Tokushima T. Angle closure glaucoma after laser photocoagulation for retinopathy of prematurity. Br J Ophthalmol. (2004) 88:1099–100. doi: 10.1136/bjo.2003.037994
17. Hosaka F, Rodríguez-Vázquez JF, Abe H, Murakami G, Fujimiya M, Ohguro H. Qualitative changes in fetal trabecular meshwork fibers at the human iridocorneal angle. Anat Cell Biol. (2013) 46:49. doi: 10.5115/acb.2013.46.1.49
18. Wu W, Lin R, Shih C, Wang N, Chen Y, Chao A, et al. Visual acuity, optical components, and macular abnormalities in patients with a history of retinopathy of prematurity. Ophthalmology. (2012) 119:1907–16. doi: 10.1016/j.ophtha.2012.02.040
19. Chen T, Tsai T, Shih Y, Yeh P, Yang C, Hu F, et al. Long-term evaluation of refractive status and optical components in eyes of children born prematurely. Invest Ophthalmol Vis Sci. (2010) 51:6140–8. doi: 10.1167/iovs.10-5234
20. Fledelius H, Fledelius C. Eye size in threshold retinopathy of prematurity, based on a Danish preterm infant series: early axial eye growth, pre- and postnatal aspects. Invest Ophthalmol Vis Sci. (2012) 53:4177–84. doi: 10.1167/iovs.12-9516
21. Yang C, Wang A, Shih Y, Hsu W. Long-term biometric optic components of diode laser-treated threshold retinopathy of prematurity at 9 years of age. Acta Ophthalmol. (2013) 91:aos12053. doi: 10.1111/aos.12053
22. Chang SHL, Lee YS, Wu SC, See LC, Chung CC, Yang ML, et al. Anterior chamber angle and anterior segment structure of eyes in children with early stages of retinopathy of prematurity. Am J Ophthalmol. (2017) 179:46–54. doi: 10.1016/j.ajo.2017.04.010
23. Lenis TL, Gunzenhauser RC, Fung SSM, Dhindsa YK, Sarraf D, Pineles SL, et al. Myopia and anterior segment optical coherence tomography findings in laser-treated retinopathy of prematurity eyes. J AAPOS. (2020) 24:86.e1–7. doi: 10.1016/j.jaapos.2020.01.007
24. Geloneck MM, Chuang AZ, Mintz-Hittner HA, Clark WL, Clark WL, Hunt MG, et al. Refractive outcomes following bevacizumab monotherapy compared with conventional laser treatment: a randomized clinical trial. J Am Med Assoc Ophthalmol. (2014) 132:1327–33. doi: 10.1001/jamaophthalmol.2014.2772
25. Mensher JH. Anterior chamber depth alteration after retinal photocoagulation. Arch Ophthalmol. (1977) 95:113–6. doi: 10.1001/archopht.1977.04450010113011
26. Kushner BJ, Sondheimer S. Medical treatment of glaucoma associated with cicatricial retinopathy of prematurity. Am J Ophthalmol. (1982) 94:313–7. doi: 10.1016/0002-9394(82)90356-7
Keywords: retinopathy of prematurity (ROP), glaucoma, anti-VEGF (vascular endothelial growth factor), laser retinal photocoagulation, myopia, case report
Citation: Lenis TL, Ledesma Vicioso N, Reddy V, Kovacs KD, Van Tassel SH and Orlin A (2021) Case Report: Glaucoma in an Infant With Retinopathy of Prematurity. Front. Pediatr. 9:786327. doi: 10.3389/fped.2021.786327
Received: 30 September 2021; Accepted: 10 November 2021;
Published: 16 December 2021.
Edited by:
Irena Tsui, University of California, Los Angeles, United StatesReviewed by:
Simone Pratesi, Careggi University Hospital, ItalyViral Jain, University of Alabama at Birmingham, United States
Copyright © 2021 Lenis, Ledesma Vicioso, Reddy, Kovacs, Van Tassel and Orlin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Anton Orlin, YW5vOTAyOEBtZWQuY29ybmVsbC5lZHU=
 Tamara Lee Lenis
Tamara Lee Lenis Nahomy Ledesma Vicioso
Nahomy Ledesma Vicioso Varun Reddy
Varun Reddy