
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pediatr. , 30 November 2021
Sec. Pediatric Cardiology
Volume 9 - 2021 | https://doi.org/10.3389/fped.2021.772138
This article is part of the Research Topic Heart Failure in Pediatrics and Congenital Heart Disease View all 17 articles
 Penghui Yang1,2,3,4†
Penghui Yang1,2,3,4† Zhijun Wu5†
Zhijun Wu5† Zhiyuan Liu1,2,3,4
Zhiyuan Liu1,2,3,4 Jing Zhang1,2,3,4
Jing Zhang1,2,3,4 Hao Zhou6
Hao Zhou6 Xiaojuan Ji2,3,4,7
Xiaojuan Ji2,3,4,7 Qijian Yi1,2,3,4
Qijian Yi1,2,3,4 Mi Li1,2,3,4*
Mi Li1,2,3,4*Objectives: To evaluate the causes and risk factors of unplanned surgery after transcatheter closure of ventricular septal defect (VSD) in children.
Methods: A total of 773 patients with VSD who had the devices transcatheter released between January 2013 and December 2018 in our institution were retrospectively reviewed. Univariate and multivariate analyses were used to identify the risk factors for unplanned surgery.
Results: Twenty four patients (3.1%) underwent unplanned surgery after transcatheter closure of VSD. The most common cause for unplanned surgery was new-onset or worsening aortic regurgitation (14/24; 58.3%), followed by occluder migration (4/24; 16.7%), complete atrioventricular block (2/24; 8.3%), severe hemolysis (2/24; 8.3%), residual shunt (1/24; 4.2%), and occluder edge near the tricuspid valve chordae (1/24; 4.2%). Logistic regression analysis revealed that primary aortic valve prolapse (OR: 5.507, 95%CI: 1.673–18.123, P = 0.005); intracristal VSD (OR: 8.731, 95%CI: 2.274–33.527, P = 0.002); eccentric occluder (OR: 4.191, 95%CI: 1.233–14.246, P = 0.022); larger occluder size (OR: 1.645, 95%CI: 1.331–2.033, P < 0.001); and pulmonary artery systolic pressure ≥45 mmHg (OR: 4.003, 95%CI: 1.073–14.941, P = 0.039) were risk factors for unplanned surgery.
Conclusions: New-onset or worsening aortic regurgitation was the primary cause for unplanned surgery after transcatheter closure of VSD in children. Primary aortic valve prolapse, intracristal VSD, eccentric occluder, larger occluder size, pulmonary artery systolic pressure ≥45 mmHg could increase the risk of unplanned surgery.
Ventricular septal defect (VSD) is the most common form of congenital heart diseases in children, occurring at a rate of ~3 per 1,000 live births (1). Surgical closure has been regarded as the standard treatment strategy. However, since Lock et al. (2) described transcatheter closure of VSD with the Rashkind double umbrella device in 1988, techniques and devices for transcatheter treatment have been continuously evolved and refined in the past decades (3, 4). Currently, transcatheter closure of VSD has been accepted as a valuable alternative to surgical treatment for certain types of VSD, with the benefit of shorter hospitalization time and absence of sternotomy and extracorporeal circulatory support (5, 6). Increasing attention has been paid to the adverse events associated with the transcatheter approach, and a series of studies have reported that its short—and long-term complications are acceptable (7–9). However, unplanned surgery after transcatheter closure has not been well-described. The purpose of this study was to evaluate the causes and corresponding risk factors of unplanned surgery after transcatheter closure of VSD in children in a single-center cohort.
Clinical data of patients with VSD who underwent transcatheter device closure in our institution were retrospectively reviewed from January 2013 to December 2018. All patients fulfilled the following criteria: (1) age <18 years old, (2) VSD diagnosed by standard transthoracic echocardiography (TTE) pre-procedurally, (3) the severity of aortic regurgitation and aortic valve prolapse before the procedure not greater than mild, and (4) intra-procedural implantation of the occluder. Exclusion criteria were: (1) transcatheter closure for residual shunt after VSD surgical repair, and (2) presence of uncontrolled infection. According to whether unplanned surgery was performed, patients were assigned into the unplanned surgery group and the control group. Unplanned surgery refers to surgery performed after the release of the occluder due to new or worsening problems. The study was approved by the Ethics Committee of the Children's Hospital of Chongqing Medical University and complied with the Declaration of Helsinki.
The transcatheter procedure was performed following standard domestic guidelines (10). Briefly, heparin was given 100 U/kg during the procedure. Standard left and right cardiac catheterization, left ventriculography, and ascending aorta angiography were performed. An arteriovenous circuit was established through a femoral vein approach. A long sheath was advanced to the position above the aortic valve through the arteriovenous circuit. The delivery sheath was then retrieved into the left ventricle and directed to the apex. The selected device was deployed through the long sheath under fluoroscopic control. The device was completely released when the TTE result was satisfactory. Finally, repeated TTE, left ventriculography, and ascending aortic angiography were performed to assess appropriate device position, residual shunt, and valvular regurgitation. If problems were discovered during the repeated examinations, such as significant aortic regurgitation, occluder migration, complete atrioventricular block (cAVB), and significant residual shunt even using the large-sized occluder, we would attempt to retrieve the occluder percutaneously. When significant aortic regurgitation occurred, we would remove the occluder even if there was no clear evidence of an association with valve impingement because of the potential risk of the valve interference, especially when the edge of the occluder was close to the aortic valve.
The devices used in our study were the modified double-disk VSD occluders (Lifetech Scientific, Shenzhen, China; Shanghai Shape Memory Alloy, Shanghai, China; Starway Medical, Beijing, China). Four subtypes of modified double-disk occluders were used in this study: symmetrical occluder, eccentric occluder, small-waist occluder, and muscular occluder (any of the three companies could manufacture the four subtypes of modified double-disk occluders). All four subtypes of occluders have the same right disk, whose diameter is 4 mm larger than the waist. In the symmetric and muscular occluder, the left disk is symmetric to the right disk, and the diameter of the left disk is 4 mm larger than the waist. In the eccentric occluder, the left disk exceeds the waist by 0 mm on its aortic side and by 6 mm on the opposite side. In the small-waist occluder, the diameter of the left disk is 8 mm larger than the waist. The waist length of the symmetrical, eccentric, and small-waist occluder is 3–4 mm. However, the waist length of the muscular occluder is 5 or 7 mm (Figure 1).
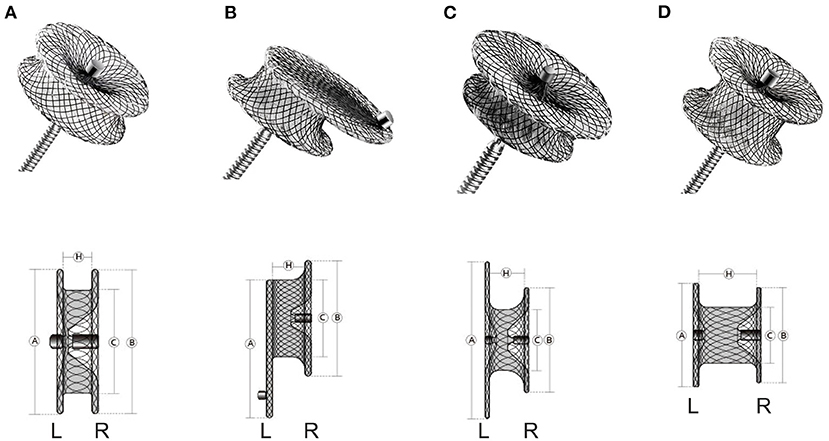
Figure 1. The various occluders and corresponding schematic diagrams. (A), symmetric occluder. (B), eccentric occluder. (C), small-waist occluder. (D), muscular occluder. L, left; R, right.
Patients were discharged from the hospital 5–6 days after the procedure if there were no adverse events. All patients received aspirin (3–5 mg/kg orally daily) for 6 months. Follow-up was performed at 1, 3, 6, and 12 months after the procedure, and yearly thereafter. The follow-up contents included clinical examination, electrocardiogram, and TTE.
We collected the following information from the hospital's electronic medical record system: (1) demographic information: age, sex, weight (2) preoperative data: VSD size, VSD type, whether combined with arrhythmia, whether combined with aortic regurgitation, whether combined with primary aortic valve prolapse (3) intra- and post-operative data: VSD size, pulmonary artery systolic pressure (PASP), pulmonary artery mean pressure (PAMP), occluder size, occluder type, sheath in-out time, residual shunt, arrhythmia, aortic regurgitation, tricuspid regurgitation, hemolysis, occluder migration, and whether unplanned surgery was performed.
Continuous variables were expressed as mean ± SD or median and interquartile range and categorical variables were expressed as number and percentage. The Shapiro-Wilk test was used to verify whether the variables were normally distributed. To compare the differences between the two groups, the independent t-tests were used for normally distributed continuous variables, Mann–Whitney U-tests for non-normally distributed continuous variables, and chi-square tests or Fisher exact tests for categorical variables. Univariate and multivariate logistic regression analyses were performed to investigate the risk factors associated with unplanned surgery after transcatheter closure of VSD. Factors with statistical significance by univariate regression analysis were further analyzed by multivariate regression, and the forward LR method was used. Finally, the statistically significant factors were considered as independent risk factors. PAMP and PASP were converted to categorical variables according to clinically meaningful cut-off values before logistic regression analysis. All statistical tests were two-sided, and P < 0.05 was considered significant. All statistical analyses were performed with SPSS version 22.0 (SPSS, Chicago, IL).
Based on the inclusion and exclusion criteria, a total of 773 patients were included in the study. During a median follow-up of 5 years, 24 patients (3.1%) underwent unplanned surgery, all of which were performed at a median of 4 days (IQR 3–5 days) after the transcatheter procedure. The characteristics of the entire cohort are shown in Table 1.
Among the causes of unplanned surgery, new or increased aortic regurgitation ranked first, accounting for 58.3% (14/24), followed by occluder migration at 16.7% (4/24), cAVB at 8.3% (2/24), severe hemolysis at 8.3% (2/24), residual shunt at 4.2% (1/24), and occluder edge near the tricuspid valve chordae at 4.2% (1/24) (Figure 2). Five unplanned surgical procedures occurred after early successful transcatheter closure procedures, all of which occurred in patients with perimembranous VSD. A 3-year-old girl (VSD size: 9 mm; device used: 10 mm symmetric occluder) developed cAVB 24 h after transcatheter closure and did not get improved after intravenous methylprednisolone. She underwent open heart surgery and the heart returned to sinus rhythm after removing the device. Two 2-year-old girls (VSD size: 10 and 8.7 mm, respectively; devices used: 12 mm symmetric occluder and 11 mm eccentric occluder, respectively) experienced severe hemolysis after transcatheter closure. Both of them received sodium bicarbonate, methylprednisolone, blood transfusion, fluid rehydration therapy, and removal of the device as well as the reparation of VSD under cardiopulmonary bypass 48 h after the transcatheter procedure. A 3-year-old girl (VSD size: 9.1 mm; device used: 11 mm symmetric occluder) and a 4-year-old boy (VSD size 6.9 mm; device used: 10 mm symmetric occluder) underwent device removal and VSD repair under cardiopulmonary bypass on day 3 after transcatheter closure because of new onset and worsening aortic regurgitation, respectively. The remaining unplanned surgical procedures occurred in the following situations: problems were discovered during the repeated examinations performed immediately after the release of the device, the device was subsequently retrieved percutaneously, and finally, the patient was sent for surgery (Table 2).
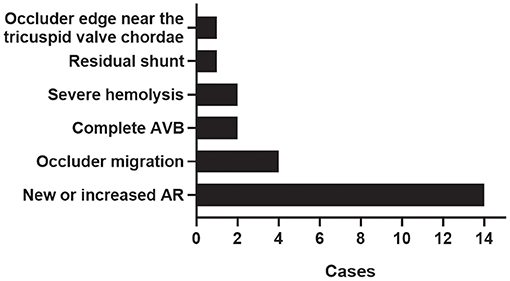
Figure 2. Causes for unplanned surgery. AVB, complete atrioventricular block; AR, aortic regurgitation.
In our patients who underwent unplanned surgery due to aortic regurgitation, primary aortic valve prolapse and intracristal VSD were present in 12 cases and absent in only two cases. During the transcatheter procedure performed on these 12 patients, six patients experienced repeated press of the delivery sheath, three patients had right coronary valve interference by the left disk of the occluder, and three patients had repeated adjustment of the eccentric occluder. The remaining two cases of aortic regurgitation occurred in a 2-year-old boy after placement of a 7 mm symmetric occluder to occlude a 5.6 mm perimembranous defect and in a 3-year-old girl after placement of an 11 mm symmetric occluder to occlude a 9.1 mm perimembranous defect. The mechanism of aortic regurgitation in these two patients may be associated with the impingement of the occluder on the valve leaflets.
Compared with the control group, more patients who underwent unplanned surgery had a higher proportion of preoperative aortic regurgitation (41.7 vs. 9.3%), a higher proportion of primary aortic valve prolapse (62.5 vs. 17.6%), a higher proportion of intracristal VSD (29.2 vs. 2.0%), a higher proportion of eccentric occluder (50.0 vs. 5.6%), larger VSD size, higher PASP, larger occluder size, and longer sheath in-out time (all P < 0.001). Patients who did not undergo unplanned surgery had a higher proportion of perimembranous VSD (97.6 vs. 66.6%) and a higher proportion of symmetric occluder (93.1 vs. 41.7%) than patients who underwent unplanned surgery (all P < 0.001).
The results of univariate and multivariate logistic regression analyses are shown in Table 3. In univariate analysis, preoperative aortic regurgitation; primary aortic valve prolapse; intracristal VSD; VSD size; PASP ≥45 mmHg; PAMP ≥25 mmHg; eccentric occluder; occluder size; and sheath in-out time were associated with unplanned surgery. In multivariate analysis, we found that primary aortic valve prolapse (OR: 5.507, 95%CI: 1.673–18.123, P = 0.005); intracristal VSD (OR: 8.731, 95%CI: 2.274–33.527, P = 0.002); eccentric occluder (OR: 4.191, 95%CI: 1.233–14.246, P = 0.022); larger occluder size (OR: 1.645, 95%CI: 1.331–2.033, P < 0.001); and PASP ≥45 mmHg (OR: 4.003, 95%CI: 1.073–14.941, P = 0.039) were associated with increased odds of unplanned surgery after transcatheter closure of VSD in children.

Table 3. Univariate and multivariate logistic analyses of risk factors for unplanned surgery after transcatheter closure of VSD.
Transcatheter closure of specific types of VSD has been widely performed, especially in developing countries, with encouraging follow-up results (11). Nevertheless, unplanned surgery may occur, which requires sufficient attention. To our knowledge, this is the first detailed study to describe unplanned surgery after transcatheter closure of VSD in children.
The present study showed that 3.1% of patients (24/773) underwent unplanned surgery after successful attempt of transcatheter VSD closure. In our cohort, the most common cause of unplanned surgery was new-onset or worsening aortic regurgitation (14/24).
Aortic regurgitation implies aortic valve incompetence with a risk of developing left ventricular dysfunction, heart failure, and even death (12). Aortic regurgitation is one of the major considerations in the transcatheter closure of VSD (13). Surgery performed because of aortic regurgitation that occurred during or after the transcatheter procedure has been reported (13, 14). In our study, 14 patients underwent unplanned surgery due to aortic regurgitation after occluder implantation, accounting for 58.3% of the total number of unplanned surgery. Therefore, it is important to pay enough attention to aortic regurgitation.
The possible cause of aortic regurgitation is the edema or damage of the aortic valve caused by the guidewire, delivery sheath, or occluder, especially in patients with intracristal VSD or primary aortic valve prolapse (15). Aortic valve prolapse is intimately linked to the occurrence or worsening of aortic regurgitation (16). This is because the distal part of the delivery sheath is difficult to press into the left ventricle, and the process of repeatedly pressing the distal part of the delivery sheath into the left ventricle and establishing arteriovenous track would increase the risk of aortic valve injury. Furthermore, if the distal part of the delivery sheath fails to press into the left ventricle, the left disc of the occluder will be released in the ascending aorta, thereby increasing the possibility of aortic valve damage. Most importantly, significant aortic regurgitation after device implantation may be related to the failure to accurately estimate the size and location of the defect due to prolapse of the aortic valve into the defect site. The left disk of the larger sized occluder may interfere with the right coronary valve and cause aortic regurgitation. For patients with intracristal VSD, the location of the defect is high, the upper rim of the defect is adjacent to the aortic valve. Even though the eccentric occluder is preferred in these patients to avoid aortic regurgitation, aortic regurgitation still occasionally occurs. The underlying mechanism may include the following. Objectively, the deployment of the eccentric occluder is technically difficult, because it is necessary to ensure that the eccentric surface of the occluder keeps toward the apex. The repeated adjustment process undoubtedly increases the possibility of aortic valve injury. Additionally, the unextended left disk of the eccentric occluder toward the aorta forms a wider platform, and the junction of the aortic root and valve body is supported by the platform, which may affect valvular activity. Finally, intracristal VSD often coexists with aortic prolapse, which also leads to an increased chance of aortic injury.
At present, transcatheter occlusion for patients with aortic prolapse or intracristal VSD is constantly being tried (15, 17–19), while the efficacy and safety remain controversial. By reviewing patients with prolapse and intracristal VSD in our cohort, we summarized the following experiences. The delivery sheath with a curved and soft distal part can be easier pressed into the left ventricle. Secondly, left ventriculography at 60–90°left anterior oblique and 20–30° cranial projection can clearly show the relationship between the defect and the aortic valve. The left ventricular angiography performed after establishing the arteriovenous track and placing the sheath can better reflect the size of the defect because the sheath holds up the aortic valve. Of course, the measurements from various views by TTE and the diameter of the sheath can help to evaluate the size of the defect. Finally, to make the “0” edge of the occluder oriented toward the aorta, the long edge should point to the 5–7 o'clock direction when the eccentric occluder is inserted into the long sheath.
Occluder migration and significant residual shunt caused by the smaller sized occluder; cAVB and the possibility of tricuspid chordae rupture caused by the larger sized occluder; and severe hemolysis caused by the larger defect, larger sized occluder, persistent residual shunt, and higher pulmonary artery pressure also accounted for unplanned surgery in our patients. Thus, selecting the appropriate device is crucial.
Recognizing the associated risk factors will be helpful for better prevention for the occurrence of unplanned surgery. Our univariate and multivariate analyses showed the association between unplanned surgery and multiple risk factors, including primary aortic valve prolapse, intracristal VSD, eccentric occluder, occluder size, and PAS ≥ 45 mmHg.
As mentioned in the preceding text, primary aortic valve prolapse, intracristal VSD, and eccentric occluder are related to aortic regurgitation. In addition, because the intracristal VSD is usually partially covered by the right coronary valve, the true size of the defect is usually underestimated, resulting in the small occluder (the vast majority are eccentric occluder) being selected, causing residual shunt and even occluder migration (17). According to the experience of our center, for these patients, the occluder selected for closure could be 2–4 mm larger than the defect diameter measured by angiography. If the defect was ≥ 5 mm, the occluder that was 4–6 mm larger than the maximum size of the defect measured by angiography could be chosen.
Our study indicated that larger occluder size was associated with unplanned surgery. The large-sized occluders were associated with postprocedural arrhythmia, which has been reported by previous studies (20, 21). The larger the size of the occluder, the more serious compression of the ventricular septum and conduction system. In our series, the occluder size of the 2 patients who underwent unplanned surgery for cAVB was 8 and 10 mm, respectively. Further, the larger the occluder, the closer its edge is to the valve, which may result in valve regurgitation (22).
The presence of massive intracardiac left-to-right shunt causes an overflow in the pulmonary circulation. Bergersen et al. (23) found that elevated PASP was a risk factor for adverse events related to transcatheter procedures. Similarly, our study showed that PASP ≥ 45 mmHg was an independent risk factor for unplanned surgery. Therefore, intervention before PASP ≥ 45 mmHg in VSD patients may reduce the occurrence of unplanned surgery, whereas, for VSD patients with excessive PASP, initial pharmacological reduction of pulmonary artery pressure followed by transcatheter therapy could be considered.
Some limitations of the present study should be acknowledged. First, it was a single-center retrospective study. This not only lead to restrictions in the sample size, but it also limited the generalizability of the findings. Second, our analysis of risk factors for unplanned surgery was also limited because we only explored preoperative and selected intraoperative factors. As such, additional intraoperative factors and postoperative management may contribute to the prognosis of patients.
In summary, we found that the rate of unplanned surgery in our center after transcatheter closure of VSD in children was 3.1%, and the main cause of unplanned surgery was new-onset or worsening aortic regurgitation. Risk factors for unplanned surgery include primary aortic valve prolapse, intracristal VSD, eccentric occluder, larger occluder size, and PASP ≥ 45 mmHg.
The original contributions presented in the study are included in the article/supplementary materials, further inquiries can be directed to the corresponding author/s.
The studies involving human participants were reviewed and approved by Ethics Committee of the Children's Hospital of Chongqing Medical University. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin. Written informed consent was obtained from the individual(s), and minor(s)' legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article.
PY, ZW, ZL, and ML: study design. ZW, ZL, and JZ: data collection. PY, ZW, ZL, JZ, and HZ: analysis and interpretation of data. PY and ZW: drafting of the manuscript. XJ, QY, and ML: critical revision of the manuscript for important intellectual content. All authors contributed to the article and approved the submitted version.
This study was supported by the Key Project of Medical Research Program of Chongqing Municipal Health Committee (2016ZDxm018).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Minette MS, Sahn DJ. Ventricular septal defects. Circulation. (2006) 114:2190–7. doi: 10.1161/CIRCULATIONAHA.106.618124
2. Lock JE, Block PC, McKay RG, Baim DS, Keane JF. Transcatheter closure of ventricular septal defects. Circulation. (1988) 78:361–8. doi: 10.1161/01.CIR.78.2.361
3. Haddad RN, Daou LS, Saliba ZS. Percutaneous closure of restrictive-type perimembranous ventricular septal defect using the new KONAR multifunctional occluder: midterm outcomes of the first middle-eastern experience. Catheter Cardiovasc Interv. (2020) 96:E295–302. doi: 10.1002/ccd.28678
4. Haddad RN, Daou L, Saliba Z. Device closure of perimembranous ventricular septal defect: choosing between amplatzer occluders. Front Pediatr. (2019) 7:300. doi: 10.3389/fped.2019.00300
5. Arora R, Trehan V, Kumar A, Kalra GS, Nigam M. Transcatheter closure of congenital ventricular septal defects: experience with various devices. J Interv Cardiol. (2003) 16:83–91. doi: 10.1046/j.1540-8183.2003.08006.x
6. Yang J, Yang L, Yu S, Liu J, Zuo J, Chen W, et al. Transcatheter versus surgical closure of perimembranous ventricular septal defects in children: a randomized controlled trial. J Am Coll Cardiol. (2014) 63:1159–68. doi: 10.1016/j.jacc.2014.01.008
7. Li H, Shi Y, Zhang S, Ren Y, Rong X, Wang Z, et al. Short- and medium-term follow-up of transcatheter closure of perimembranous ventricular septal defects. BMC Cardiovasc Disord. (2019) 19:222. doi: 10.1186/s12872-019-1188-y
8. Bergmann M, Germann CP, Nordmeyer J, Peters B, Berger F, Schubert S. Short- and long-term outcome after interventional VSD closure: a single-center experience in pediatric and adult patients. Pediatr Cardiol. (2021) 42:78–88. doi: 10.1007/s00246-020-02456-2
9. Mandal KD, Su D, Pang Y. Long-term outcome of transcatheter device closure of perimembranous ventricular septal defects. Front Pediatr. (2018) 6:128. doi: 10.3389/fped.2018.00128
10. Congenital Heart Disease Expert Committee of Pediatricians Branch of Chinese Medical Doctor Association Cardiovascular Group of Chinese Medical Pediatrics Association Editorial Board of Chinese Journal of Pediatrics. Expert consensus on the interventional treatment of common congenital heart diseases in children. Chin J Pediatr. (2015) 53:17–24. doi: 10.3760/cma.j.issn.0578-1310.2015.01.004
11. Haddad RN, Rizk C, Saliba Z, Farah J. Percutaneous closure of ventricular septal defects in children: key parameters affecting patient radiation exposure. Am J Cardiovasc Dis. (2021) 11:65–72.
12. Borer JS, Supino PG, Herrold EMcM, Innasimuthu A, Hochreiter C, Krieger K, et al. Survival after aortic valve replacement for aortic regurgitation: prediction from preoperative contractility measurement. Cardiology. (2018) 140:204–12. doi: 10.1159/000490848
13. Han Y, Li H, Zhu H, Sun G, Yin Q, Gu C. Aortic regurgitation after closure of ventricular septal defect by transcatheter device: the long-term complication. Cardiol Young. (2020) 30:577–9. doi: 10.1017/S1047951120000414
14. Yang J, Yang L, Wan Y, Zuo J, Zhang J, Chen W, et al. Transcatheter device closure of perimembranous ventricular septal defects: mid-term outcomes. Eur Heart J. (2010) 31:2238–45. doi: 10.1093/eurheartj/ehq240
15. Jiang D, Han B, Zhao L, Yi Y, Zhang J, Fan Y, et al. Transcatheter device closure of perimembranous and intracristal ventricular septal defects in children: medium- and long-term results. J Am Heart Assoc. (2021) 10:e020417. doi: 10.1161/JAHA.120.020417
16. Saleeb SF, Solowiejczyk DE, Glickstein JS, Korsin R, Gersony WM, Hsu DT. Frequency of development of aortic cuspal prolapse and aortic regurgitation in patients with subaortic ventricular septal defect diagnosed at <1 year of age. Am J Cardiol. (2007) 99:1588–92. doi: 10.1016/j.amjcard.2007.01.034
17. Chen F, Li P, Liu S, Du H, Zhang B, Jin X, et al. Transcatheter closure of intracristal ventricular septal defect with mild aortic cusp prolapse using zero eccentricity ventricular septal defect occluder. Circ J. (2015) 79:2162–8. doi: 10.1253/circj.CJ-15-0301
18. Chen GL, Li HT, Li HR, Zhang ZW. Transcatheter closure of ventricular septal defect in patients with aortic valve prolapse and mild aortic regurgitation: feasibility and preliminary outcome. Asian Pac J Trop Med. (2015) 8:315–8. doi: 10.1016/S1995-7645(14)60337-0
19. Zhang W, Wang C, Liu S, Zhou L, Li J, Shi J, et al. Safety and efficacy of transcatheter occlusion of perimembranous ventricular septal defect with aortic valve prolapse: a six-year follow-up study. J Interv Cardiol. (2021) 2021:6634667. doi: 10.1155/2021/6634667
20. Zhao LJ, Han B, Zhang JJ, Yi YC, Jiang DD, Lyu JL. Postprocedural outcomes and risk factors for arrhythmias following transcatheter closure of congenital perimembranous ventricular septal defect: a single-center retrospective study. Chin Med J (Engl). (2017) 130:516–21. doi: 10.4103/0366-6999.200551
21. Wu Z, Yang P, Xiang P, Ji X, Tian J, Li M. Left anterior fascicular block after transcatheter closure of ventricular septal defect in children. Front Cardiovasc Med. (2021) 8:609531. doi: 10.3389/fcvm.2021.609531
22. Yang L, Tai BC, Khin LW, Quek SC A systematic review on the efficacy and safety of transcatheter device closure of ventricular septal defects (VSD). J Interv Cardiol. (2014) 27:260–72. doi: 10.1111/joic.12121
Keywords: ventricular septal defect, transcatheter closure, unplanned surgery, causes and risk factors, children
Citation: Yang P, Wu Z, Liu Z, Zhang J, Zhou H, Ji X, Yi Q and Li M (2021) Unplanned Surgery After Transcatheter Closure of Ventricular Septal Defect in Children: Causes and Risk Factors. Front. Pediatr. 9:772138. doi: 10.3389/fped.2021.772138
Received: 07 September 2021; Accepted: 08 November 2021;
Published: 30 November 2021.
Edited by:
Dimpna Calila Albert-Brotons, King Faisal Specialist Hospital & Research Centre, Saudi ArabiaReviewed by:
Raymond Nagi Haddad, Hôpital Necker-Enfants Malades, Assistance Publique Hopitaux de Paris, FranceCopyright © 2021 Yang, Wu, Liu, Zhang, Zhou, Ji, Yi and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mi Li, bG1fZGhtQDE2My5jb20=
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.