- 1Department of Pediatric Surgery and Urology, Necker-Enfants Malades Hospital, APHP, Paris, France
- 2Department of Pediatric Nephrology, Reference Center for Inherited Renal Disease (MARHEA), Necker-Enfants Malades Hospital, APHP, Paris, France
- 3INSERM UMR 1163, Laboratory of Inherited Kidney Diseases, Imagine Institute, Université de Paris, Paris, France
- 4Department of Urology, Tenon Hospital, APHP, Paris, France
- 5Groupe de Recherche Clinique sur la Lithiase Urinaire (GRC no 20), Tenon Hospital, Sorbonne Université, Paris, France
- 6Sorbonne Université, Paris, France
- 7Université de Paris, Paris, France
- 8INSERM U1151-CNRS UMR 8253, Université de Paris, Paris, France
Purpose: Cystinuria is a genetic disorder characterized by a defective reabsorption of cystine and dibasic amino acids leading to development of urinary tract calculi from childhood onward. Cystine lithiasis is known to be resistant to fragmentation. The aim was to evaluate our long-term experience with extracorporeal shockwave lithotripsy (ESWL) used as first-line urological treatment to treat cystine stones in children.
Methods: We retrospectively reviewed the charts of all children who underwent ESWL for cystine stone. We assessed the 3-month stone-free rate, according to age, younger (group 1) or older (group 2) than 2 years old.
Results: Between 2003 and 2016, 15 patients with a median (IQR) age at first treatment of 48 (15–108) months underwent ESWL in monotherapy. Median age was, respectively, 15 and 108 months in each group. The median (IQR) stone burden was 2,620 (1,202–8,265) mm3 in group I and 4,588 (2,039–5,427) mm3 in group II (p = 0.96). Eleven patients had bilateral calculi. ESWL was repeated on average 2.4 times, with a maximum of 4 for patients of group I, and 4.8 times, with a maximum of 9 for group II (p > 0.05). ESWL in monotherapy was significantly more efficient to reach stone-free status for children under 2 years of age: 83% vs. 6.2% (p = 0.040). The median (IQR) follow-up of the study was 69 (42–111) months.
Conclusion: ESWL appears as a valid urological option for the treatment of cystine stones, in young children. Even if cystine stones are known to be resistant to fragmentation, we report 83% of stone-free status at 3 months with ESWL used in monotherapy in children under 2 years old with cystinuria. In older children, the success rate is too low to recommend ESWL as a first line approach.
Introduction
Cystinuria is a rare autosomal recessive genetic disorder characterized by defective reabsorption of cystine and other dibasic amino acids (ornithine, lysine, and arginine) in the renal proximal tubule and intestinal epithelial cells (1). Dysfunction of this transport mechanism is due to mutations in solute carrier genes SLC3A1 or in SLC7A9 (2). Cystinuria is responsible for 5 to 10% of pediatric stones (3) and more than half of patients will develop stones throughout their lifetime, with a higher risk of recurrence, bilaterality (4), and loss of renal function (5–7) than children with non-cystine stones. Although first symptoms often occur during childhood (3), cystinuria can be suspected prenatally, warranting early medical treatment (8–10).
In addition to mandatory medical management, pediatric upper urinary tract stones can be treated using different modalities according to patient's age, stone localization/size, and surgeon's experience: extracorporeal shockwave lithotripsy (ESWL), percutaneous nephrolithotomy (PCNL), retrograde rigid or flexible ureteroscopy (RUS), or open nephrolithotomy (ON) (11). The goal is to reach a stone-free status to avoid recurrence.
Previous reports have demonstrated that ESWL was effective and safe in infants and young children (12, 13) while other techniques (PCNL and RUS) may be more challenging and associated with significant complications, especially in the prepubertal period (14, 15). Cystine stones are known to be particularly resistant to intra- or extracorporeal fragmentation (11) and no consensus has been reached regarding the preferred and age-appropriate technique.
This study's aim was to assess the efficacy of ESWL in treating cystine stones in children according to the age of treatment.
Materials and Methods
With the approval from the Necker-Enfants Malades Hospital's institutional review board, we retrospectively reviewed the data of all children (younger than 16 years old) treated in our center for cystine stones with at least one urological procedure for upper urinary tract stones. We selected those with a diagnosis of cystinuria and at least once treated using ESWL. All patients were diagnosed with cystinuria based on urine analysis (Brandt reaction and/or crystalluria study with infrared spectrophotometry) prior to any urologic or medical treatment. There were no exclusion criteria.
Data collected included age, gender, familial history of cystinuria, parental consanguinity, circumstance of diagnosis, stones' location, medical management, age at first urological treatment, stone burden (mm3), type of procedure (ESWL, PCNL, ON, or RUS), and number of procedures to reach a stone-free status.
Preoperative evaluation of stone diameter was done using kidney–ureter–bladder (KUB) x-ray, ultrasonography (US), and/or computed tomography (CT) scan for right and left upper urinary tract. A spherical shape of the stones was assumed to determine the stone burden for each child, using measurements in coronal, sagittal, and axial planes on KUB x-ray, ultrasound, and/or CT scan.
ESWL procedures were performed as first line/option in the initial surgical management for most patients or as an adjunct after prior urological procedure in some. Sessions were conducted under general anesthesia by the same pediatric urologist (HL), using a Dornier® Compact Delta lithotripter. Ultrasound was mainly used as a targeting system for renal stones. Ultrasound and/or fluoroscopy was used to target ureteral stones. Power was set on 4 for renal stones and 5 for ureteral stones. A maximum of 2,500 shocks on the kidney and 3,500 on the ureter were delivered per site and per session. Stone fragments were analyzed in all patients using a Fourier-transform infrared spectrometer.
Patients were divided into two groups according to age at treatment: ≤ 2 years old (group 1) and >2 years old (group 2). Results were analyzed separately for each group.
Follow-up included KUB and ultrasound at 1 month following urologic procedure for all patients in addition to the nephrologic follow-up. In case of residual fragments, repeat KUB and ultrasound were performed at 3 months. If patients were stone-free, KUB–ultrasound were performed at 6 months and then on a yearly basis. ESWL was considered a monotherapy if no other urological procedure was necessary to achieve a stone-free status per treated site. Success of treatment (stone-free status) was defined for each treated side (right and/or left) as no visible remaining stones on KUB and US, or CT scan 3 months after the end of initial urological treatment. Recurrence was defined as a newly appeared stone during the follow-up period.
The study was conducted in accordance with French legislation, Good Clinical Practices, and the Declaration of Helsinki.
Data were expressed as mean (range) for continuous variables, and as numbers and percentages for categorical variables. Mann–Whitney test or Student's t-test was used to compare continuous variables according to normal distribution (Shapiro–Wilk's test) and chi-square or Fischer's exact test for categorical variables. A p < 0.05 was considered significant.
Results
Between 2003 and 2016, 210 children were treated in our department for upper urinary tract stones. Eighteen children (7%) were diagnosed with cystine stones. Three of them were never treated with ESWL and were therefore excluded from further analysis.
Seven children were younger than 2 years old (group 1) and eight were older than 2 years old (group 2). There were eight boys and seven girls.
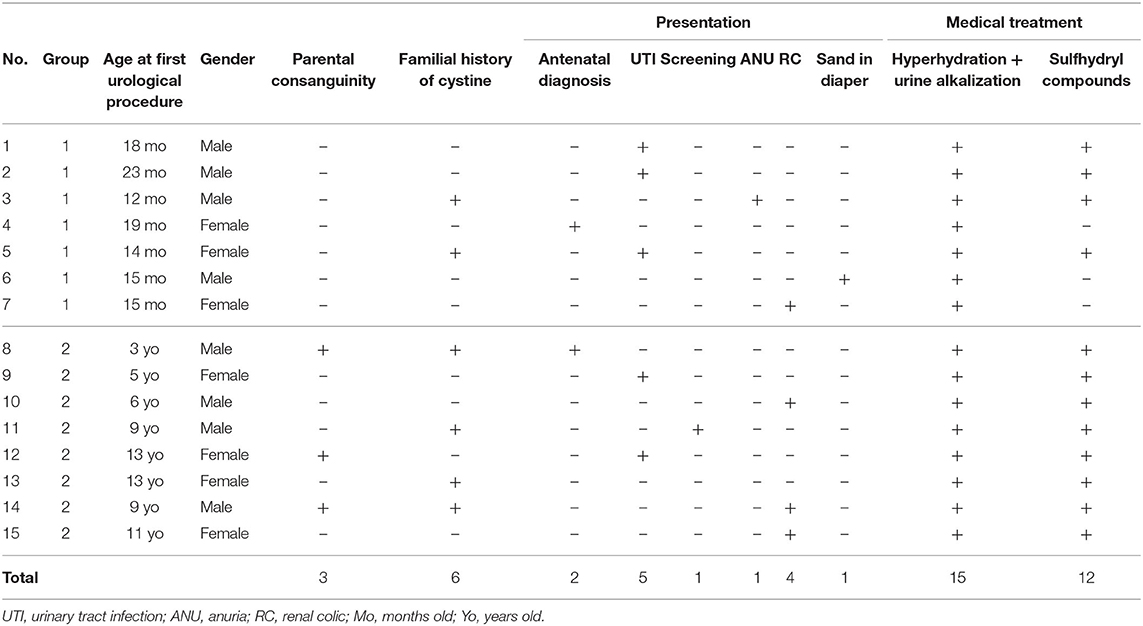
Parental consanguinity was noted in three cases (20%) and a family history of cystine stones in six cases (40%) (Table 1). In two cases (13%), cystinuria was suspected prenatally based on a hyperechoic colon during the third trimester of pregnancy. Symptoms included urinary tract infection (n = 5; 33%), renal colic (n = 4; 31%), anuria (n = 1; 7%), and stone fragments in the diaper (n = 1; 7%). One child was diagnosed through sibling screening of an index case.
All patients received medical management: hyperhydration and urine alkalization. Most of them received sulfhydryl compounds (n = 12; 80%) at some point.
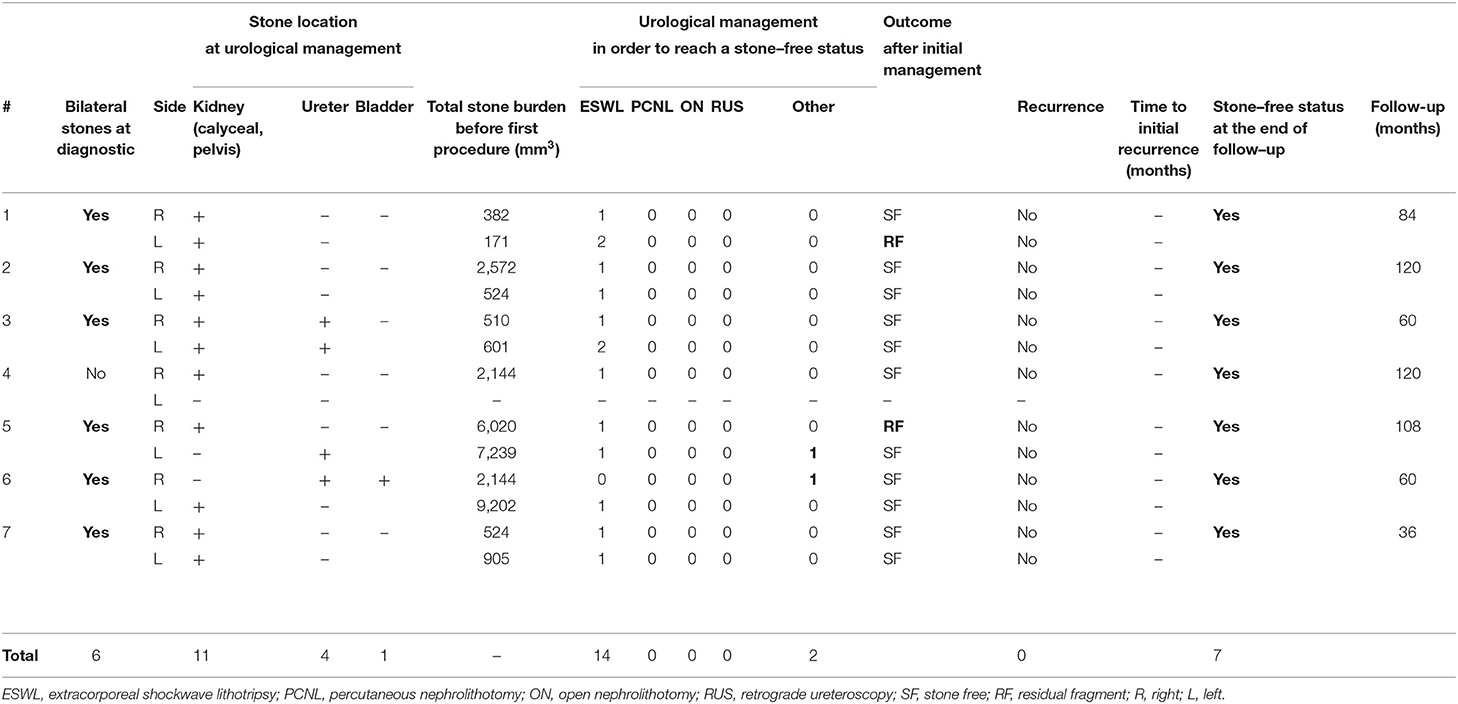
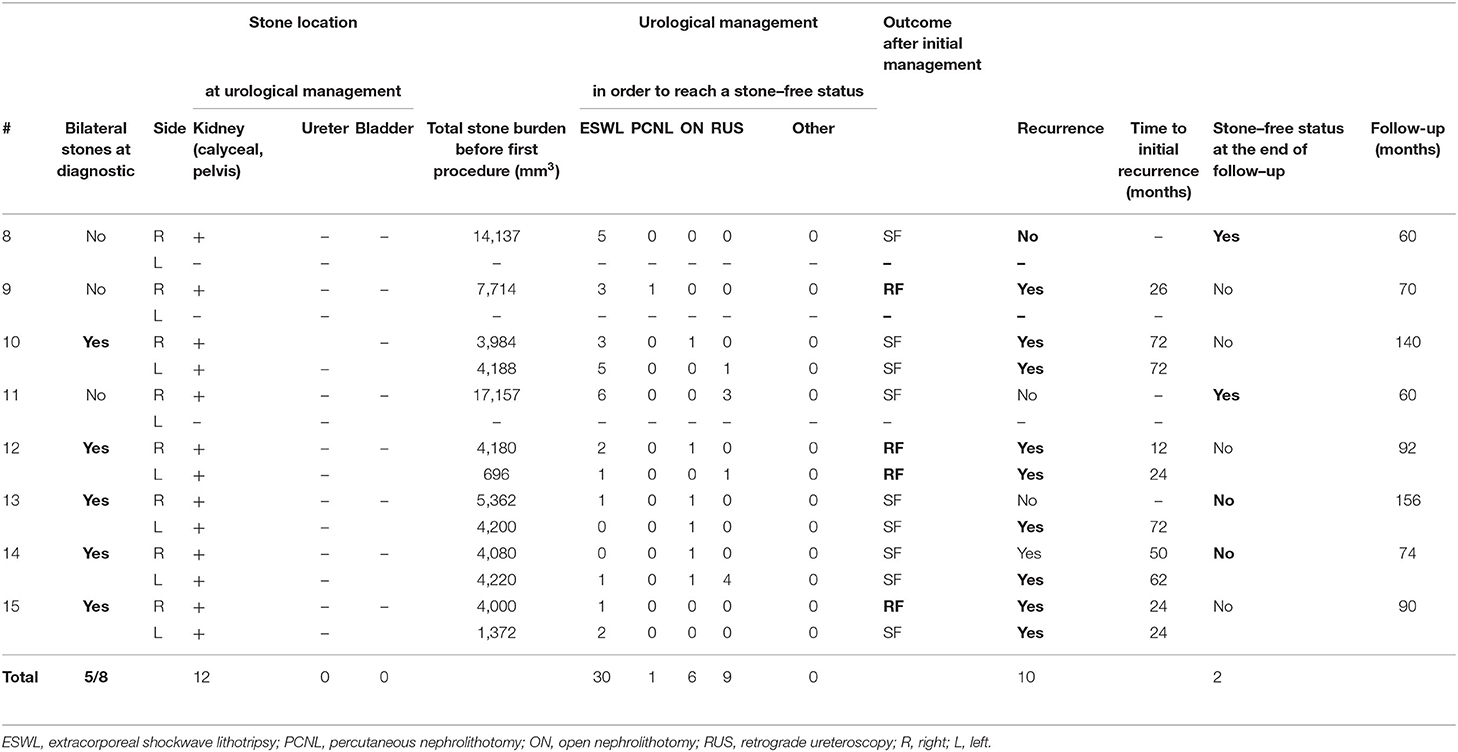
Cystine stones were bilateral in six children in group 1 (86%) and five children in group 2 (62%) (Tables 2, 3). The mean stone burden was 2,533 (171–9,202) mm3 in group 1 and 5,791 (696–17,157) mm3 in group 2 (p = 0.02). The first urological procedure was performed at a mean age of 17 (12–23) months in group 1 and 8.6 (3–13) years in group 2.
A total of 44 ESWL session were performed, 14 in group 1 and 30 in group 2. Overall treatment outcomes are summarized in Tables 2, 3.
In group 1, ESWL was used as a monotherapy to treat at least one side for all children and allowed to reach a stone-free status in all treated cases but two (85%).
In one case, ESWL was followed by a ureteral steinstrasse requiring an ureterotomy to remove an obstructive residual fragment (RF) after RUS failure (case # 5).
During a single general anesthesia, patient #6, from abroad, had ESWL on the left side (caliceal stone) and a ureterotomy and cystotomy to remove a bladder and a large right lower ureteric stone.
The two children (#1 and #5) with RF mobilized their stone after 3 years of medical treatment and required cystotomy and ureteroscopy, respectively.
In group 2, ESWL was successful as a monotherapy to reach a stone-free status in one side in only two patients (#8 and #15). In other sides, either the child had small RF after ESWL or at least one other kind of urological procedure was necessary following ESWL.
In case # 8, ESWL was followed by acute urinary retention because of a fragment obstructing the urethral meatus and was extracted under sedation using small forceps.
ESWL was repeated on an average 1.1 times per side, with a maximum of 2 per side for group 1 patients and an average of 2.7 times per side, with a maximum of 6 for group 2 (p = 0.04).
ESWL used as a monotherapy was significantly more efficient to reach stone-free status per treated side without recurrence in children younger than 2 years old: 85% (n = 11/13) in group 1 against 8% (n = 1/13) in group 2 (p = 0.002).
The median follow-up was 84 (36–156) months. No patient was lost to follow up.
At last follow-up, no recurrence occurred and all children were stone free in group 1. All children with RF recurred and only two children were stone free in group 2.
Discussion
Cystinuria is a rare inherited disorder whose first clinical signs can appear during early childhood (3). Treatment is challenging. Children with cystinuria are known to be at higher risk of early surgical management than those with non-cystine stones (16). Prevention of stone formation through medical management is the first line and one of the most important part (17). The aim of the medical management is to decrease urinary cystine concentration using dietary measures and to increase crystals' solubility. Prophylactic measures include proper and permanent hydration with fluid intake (at least 3 L/1.73 m2/day) and urine alkalinization (18, 19). D-Penicillamine or Tiopronine (sulfhydryl compounds) may be added to increase the solubility of cystine up to 50 times (3). However, compliance is difficult to obtain in young patients and side effects may lead to treatment interruption (20, 21).
Cystinuria may be suspected prenatally when an hyperechogenic colon is observed at third-trimester US (8–10). In our study, two patients had a prenatal diagnosis of cystinuria but early medical management could not avoid cystine stone formation. Most patients will require repeat urological procedures during childhood despite proper preventive measures and medical treatment (6, 22). The mean age at first ESWL treatment was 5.2 years in our study. Half of patients received their first procedure before 2 years of age (group 1).
Urological management for cystine stones is challenging. Some authors suggest that ESWL should be restricted to stones smaller than 15 to 25 mm (longest diameter) and prefer PCNL or ON for larger stones (3, 23–25). RUS is preferred for distal ureteral stones (26, 27) and represent a suitable alternative when treating fragments refractory to prior ESWL (3, 14, 28) but remains difficult in young patients. Although cystine stones have always been considered as rather resistant to fragmentation (1), reasonable outcomes have been reported in literature on lithotripters with higher power (29–31). Efficacy and safety of ESWL in the treatment of upper urinary tract stones in children have already been established (12, 23, 32–34). In our study, a total of 62 (16 in group 1, 46 in group 2) urological procedures were performed on 15 patients, and most of them (71%, n = 44/62) were ESWL with an average of three ESWL procedures per child. ESWL was used as a monotherapy to treat at least one side for all patients younger than 2 years old and allowed to reach a stone-free status without recurrence in all cases but one. For children older than 2 years old, monotherapy of ESWL allowed to reach the stone-free status without recurrence in only one treated side. ESWL is a low invasive technique that can be used safely in infants. It requires general anesthesia in children but can be repeated several times for the same patient. The two complications observed were a ureteral steinstrasse requiring an open procedure to remove ureteral stones and an acute urinary retention easily managed without general anesthesia. Moore et al. have recently highlighted the importance to reach a stone-free status after the initial management. According to their results, stone-free patients after their first treatment had lower recurrence rate and fewer procedures during their follow-up (35). Our excellent results of ESWL monotherapy in treating cystine stones in young children (<2 years old) (85% of stone free status) suggest that it could be the reference technique for this age group even for large cystine stones, when combined with proper medical management. Moreover, shockwave transmission is probably better in young children and the ureter is also more compliant to the passage of stone fragments (12). The success of cystine stone fragmentation in younger children may be explained by the greater water content in their tissue and their shorter shockwave transmission path, the fact that the procedure was carried out under general anesthesia, thus minimizing shockwave imprecision due to breathing movements, the lower stone burden as observed in our cohort, the better compliance to medical treatment in young children, or possibly the younger age of the cystine stones (12, 36–38). Conversely, we showed that the older the child is, the poorer the efficacy of ESWL is to reach a stone-free status, with a statistically significative difference. The youngest patient in group 2, aged 3 years, required five ESWL sessions to reach a stone-free status. These findings may be related to a heavier initial stone burden in children aged >2 years old. A lack of observance to medical treatment for school children and adolescents may also contribute to these results, but our study did not address this question.
The advancements in miniaturization of ureteroscopes allow to perform ultra-minimally invasive procedures in children (39–43). These technologies represent new alternative modalities of treatment to ESWL in cystinuria for children but remains challenging, especially for the youngest. A recent systematic review of ureteroscopy for stone disease in the pediatric population highlighted a higher failure and complication rate of RUS in young children (14). Patient's age has been proven to be a strong significant predictor of failure for YAG laser ureteroscopic lithotripsy (44). Considering, on one hand, our good results of ESWL for the treatment of cystine stones for children younger than 2 years old and the higher complication rate of RUS in this population, on the other hand, we suggest an age-dependent urological strategy: a reasonable option is to treat young children with ESWL, particularly infants, whereas RUS and PCNL seem to be more appropriate and accessible to older children.
Although short, our series constitute to our knowledge the largest published pediatric series of nephro-urological management of cystine stones with ESWL, which was the only option besides open surgery for our earliest patients, with a follow-up up to 156 months. Analyzed data did not include the exact caliceal location of the stones, which may have limited our results since location of the stones are potential predictor ESWL success.
Cystinuria remains a rare disease, explaining the limited number of patients and the large study period. Further prospective and multicenter studies with a large number of patients are required to determine adequate urological treatment strategies in cystine stones in children.
Conclusion
ESWL appears to be a valid urological option for the treatment of cystine stones, in infants and toddlers. Even if cystine stones are known to be resistant to fragmentation, we report excellent results achieved with ESWL used as a monotherapy in children younger than 2 years old. For older patients, results achieved with ESWL as a first-line approach are poorer and another treatment strategy should be preferred.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Necker-Enfants Malades Institutional Review Board. Written informed consent from the participants' legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author Contributions
NV: data analysis, manuscript drafting, and manuscript revision. AK and PL: data collection, data analysis, and manuscript drafting. LH, NB, OT, and OB: critical revision and manuscript review. TB: data collection, data analysis, critical revision, and manuscript drafting. HL: study design, manuscript drafting, critical revision, and manuscript review. All authors contributed to the study conception and design and read and approved the final manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
ESWL, Extracorporeal shockwave lithotripsy; PCNL, Percutaneous nephrolithotomy; RUS, Retrograde ureteroscopy; ON, Open nephrolithotomy; KUB, Kidney–ureter–bladder; US, Ultrasonography; CT, Computed tomography; RF, Residual fragments.
References
1. Saravakos P, Kokkinou V, Giannatos E. Cystinuria: current diagnosis and management. Urology. (2014) 83:693–9. doi: 10.1016/j.urology.2013.10.013
2. Wong KA, Mein R, Wass M, Flinter F, Pardy C, Bultitude M, et al. The genetic diversity of cystinuria in a UK population of patients. BJU Int. (2015) 116:109–16. doi: 10.1111/bju.12894
3. Knoll T, Zöllner A, Wendt-Nordahl G, Michel MS, Alken P. Cystinuria in childhood and adolescence: recommendations for diagnosis, treatment, and follow-up. Pediatr Nephrol. (2005) 20:19–24. doi: 10.1007/s00467-004-1663-1
4. Claes DJ, Jackson E. Cystinuria: mechanisms and management. Pediatr Nephrol. (2012) 27:2031–38. doi: 10.1007/s00467-011-2092-6
5. Assimos DG, Leslie SW, Ng C, Streem SB, Hart LJ. The impact of cystinuria on renal function. J Urol. (2002) 168:27–30. doi: 10.1016/S0022-5347(05)64824-0
6. Worcester EM, Coe FL, Evan AP, Parks JH. Reduced renal function and benefits of treatment in cystinuria vs other forms of nephrolithiasis. BJU Int. (2006) 97:1285–90. doi: 10.1111/j.1464-410X.2006.06169.x
7. Prot-Bertoye C, Lebbah S, Daudon M, Tostivint I, Bataille P, Bridoux F, et al. CKD and its risk factors among patients with cystinuria. Clin J Am Soc Nephrol. (2015) 10:842–51. doi: 10.2215/CJN.06680714
8. Rasseur-Daudruy M, Garel C, Brossard V, Broux F, Heckettsweiler B, Eurin D. Hyper-echogenic colon: a prenatal sign of cystinuria? Prenat Diagn. (2006) 26:1254–5. doi: 10.1002/pd.1597
9. Benoist JF, Imbard A, Dreux S, Garel C, Haddad G, Hoffet M, et al. Antenatal biochemical expression of cystinuria and relation to fetal hyperechogenic colon. Clin Chem. (2007) 53:149–50. doi: 10.1373/clinchem.2007.080705
10. Amat S, Czerkiewicz I, Benoist JF, Eurin D, Fontanges M, Muller F. Isolated hyperechoic fetal colon before 36 weeks' gestation reveals cystinuria. Ultrasound Obstet Gynecol. (2011) 38:543–7. doi: 10.1002/uog.8917
12. Lottmann HB, Archambaud F, Traxer O, Mercier-Pageyral B, Helal B. The efficacy and parenchymal consequences of extracorporeal shock wave lithotripsy in infants. BJU Int. (2000) 85:311–5. doi: 10.1046/j.1464-410x.2000.00475.x
13. Griffin SJ, Margaryan M, Archambaud F, Sergent-Alaoui A, Lottmann HB. Safety of shock wave lithotripsy for treatment of pediatric urolithiasis: 20-year experience. J Urol. (2010) 183:2332–6. doi: 10.1016/j.juro.2010.02.030
14. Ishii H, Griffin S, Somani BK. Ureteroscopy for stone disease in the paediatric population: a systematic review. BJU Int. (2015) 115:867–73. doi: 10.1111/bju.12927
15. Patil N, Javali T, Hamsa V, Nagaraj HK. A single centre experience of percutaneous nephrolithotomy in infants and its long-term outcomes. J Pediatr Urol. (2021). 31:S1477-5131(21)00364-8. doi: 10.1016/j.jpurol.2021.07.026
16. Zu'bi F, Sidler M, Harvey E, Lopes RI, Hojjat A, Naoum N, et al. Stone growth patterns and risk for surgery among children presenting with hypercalciuria, hypocitraturia and cystinuria as underlying metabolic causes of urolithiasis. J Pediatr Urol. (2017) 13:357.e1–7. doi: 10.1016/j.jpurol.2017.06.022
17. Tkaczyk M, Gadomska-Prokop K, Załuska-Leśniewska I, Musiał K, Zawadzki J, Jobs K, et al. Clinical profile of a Polish cohort of children and young adults with cystinuria. Ren Fail. (2021) 43:62–70. doi: 10.1080/0886022X.2020.1860089
18. Servais A, Thomas K, Dello Strologo L, Sayer JA, Bekri S, Bertholet-Thomas A, et al. Cystinuria: clinical practice recommendation. Kidney Int. (2021) 99:48–58. doi: 10.1016/j.kint.2020.06.035
19. Eisner BH, Goldfarb DS, Baum MA, Langman CB, Curhan GC, Preminger GM, et al. Evaluation and medical management of patients with cystine nephrolithiasis: a consensus statement. J Endourol. (2020) 34:1103–10. doi: 10.1089/end.2019.0703
20. Jaffe IA. Adverse effects profile of sulfhydryl compounds in man. Am J Med. (1986) 80:471–6. doi: 10.1016/0002-9343(86)90722-9
21. Prot-Bertoye C, Lebbah S, Daudon M, Tostivint I, Jais JP, Lillo-Le Louët A, et al. French Cystinuria Group. Adverse events associated with currently used medical treatments for cystinuria and treatment goals: results from a series of 442 patients in France. BJU Int. (2019) 124:849–61. doi: 10.1111/bju.14721
22. Varda BK, Johnson EK, Johnson KL, Rosoklija I, Baum MA, Nelson CP. Imaging and surgical utilization for pediatric cystinuria patients: a single-institution cohort study. J Pediatr Urol. (2016) 12:106.e1–7. doi: 10.1016/j.jpurol.2015.08.019
23. Slavković A, Radovanović M, Sirić Z, Vlajković M, Stefanović V. Extracorporeal shock wave lithotripsy for cystine urolithiasis in children: outcome and complications. Int Urol Nephrol. (2002) 34:457–61. doi: 10.1023/a:1025694230131
24. Gofrit ON, Pode D, Meretyk S, Katz G, Shapiro A, Golijanin D, et al. Is the pediatric ureter as efficient as the adult ureter in transporting fragments following extracorporeal shock wave lithotripsy for renal calculi larger than 10 mm.? J Urol. (2001) 166:1862–4. doi: 10.1016/S0022-5347(05)65707-2
25. Ahmed K, Khan MS, Thomas K, Challacombe B, Bultitude M, Glass J, et al. Management of cystinuric patients: an observational, retrospective, single-centre analysis. Urol Int. (2008) 80:141–4. doi: 10.1159/000112603
26. Thomas K, Wong K, Withington J, Bultitude M, Doherty A. Cystinuria-a urologist's perspective. Nat Rev Urol. (2014) 11:270–7. doi: 10.1038/nrurol.2014.51
27. Skolarikos A, Laguna MP, Alivizatos G, Kural AR, de la Rosette JJ. The role for active monitoring in urinary stones: a systematic review. J Endourol. (2010) 24:923–30. doi: 10.1089/end.2009.0670
28. Delakas D, Daskalopoulos G, Metaxari M, Triantafyllou T, Cranidis A. Management of ureteral stones in pediatric patients. J Endourol. (2001) 15:675–80. doi: 10.1089/08927790152596226
29. Dretler SP. Stone fragility–a new therapeutic distinction. J Urol. (1988) 139:1124–7. doi: 10.1016/S0022-5347(17)42801-1
30. Williams JC Jr, Saw KC, Paterson RF, Hatt EK, McAteer JA, Lingeman JE. Variability of renal stone fragility in shock wave lithotripsy. Urology. (2003) 61:1092–6; discussion 1097. doi: 10.1016/S0090-4295(03)00349-2
31. Kim SC, Burns EK, Lingeman JE, Paterson RF, McAteer JA, Williams JC Jr. Cystine calculi: correlation of CT-visible structure, CT number, and stone morphology with fragmentation by shock wave lithotripsy. Urol Res. (2007) 35:319–24. doi: 10.1007/s00240-007-0117-1
32. Brinkmann OA, Griehl A, Kuwertz-Bröking E, Bulla M, Hertle L. Extracorporeal shock wave lithotripsy in children. Efficacy, complications and long-term follow-up. Eur Urol. (2001) 39:591–7. doi: 10.1159/000052509
33. Landau EH, Shenfeld OZ, Pode D, Shapiro A, Meretyk S, Katz G, et al. Extracorporeal shock wave lithotripsy in prepubertal children: 22-year experience at a single institution with a single lithotriptor. J Urol. (2009) 182:1835–9. doi: 10.1016/j.juro.2009.04.084
34. Muslumanoglu AY, Tefekli A, Sarilar O, Binbay M, Altunrende F, Ozkuvanci U. Extracorporeal shock wave lithotripsy as first line treatment alternative for urinary tract stones in children: a large scale retrospective analysis. J Urol. (2003) 170(Pt. 1):2405–8. doi: 10.1097/01.ju.0000096422.72846.80
35. Moore SL, Somani BK, Cook P. Journey of a cystinuric patient with a long-term follow-up from a medical stone clinic: necessity to be SaFER (stone and fragments entirely removed). Urolithiasis. (2019) 47:165–70. doi: 10.1007/s00240-018-1059-5
36. Asi T, Dogan HS, Bozaci AC, Citamak B, Altan M, Tekgul S. A single center's experience in pediatric cystine stone disease management: what changed over time? Urolithiasis. (2020) 48:493–9. doi: 10.1007/s00240-020-01200-y
37. Dogan HS, Altan M, Citamak B, Bozaci AC, Karabulut E, Tekgul S. A new nomogram for prediction of outcome of pediatric shock-wave lithotripsy. J Pediatr Urol. (2015) 11:84.e1–6. doi: 10.1016/j.jpurol.2015.01.004
38. Tekin A, Tekgul S, Atsu N, Sahin A, Bakkaloglu M. Cystine calculi in children: the results of a metabolic evaluation and response to medical therapy. J Urol. (2001) 165(Pt. 2):2328–30. doi: 10.1016/S0022-5347(05)66196-4
39. Atar M, Sancaktutar AA, Penbegul N, Soylemez H, Bodakci MN, Hatipoglu NK, et al. Comparison of a 4.5 F semi-rigid ureteroscope with a 7.5 F rigid ureteroscope in the treatment of ureteral stones in preschool-age children. Urol Res. (2012) 40:733–8. doi: 10.1007/s00240-012-0489-8
40. Atar M, Bodakci MN, Sancaktutar AA, Penbegul N, Soylemez H, Bozkurt Y, et al. Comparison of pneumatic and laser lithotripsy in the treatment of pediatric ureteral stones. J Pediatr Urol. (2013) 9:308–12. doi: 10.1016/j.jpurol.2012.03.004
41. Inoue T, Watanabe M, Shimada S, Kinoshita H, Matsuda T. Successful ultra-minimally invasive endoscopic intrarenal surgery for 2-year-old boy with bilateral cystine kidney stones over 2 cm. J Endourol Case Rep. (2018) 4:101–4. doi: 10.1089/cren.2018.0042
42. Kocaoglu C, Ozkan KU. The effectiveness of 4.5F ultrathin semirigid ureteroscope in the management of ureteral stones in prepubertal children: is there a need for any ureteral dilatation? Urology. (2014) 84:202–5. doi: 10.1016/j.urology.2014.03.027
43. Bleve C, Chiarenza SF. Endourologic and retroperitoneoscopic combined mininvasive management of cystine urolithiasis in an infant of 13 months of life. J Endourol Case Rep. (2020) 6:49–52. doi: 10.1089/cren.2019.0072
Keywords: cystinuria, cystine stone, extracorporeal shockwave lithotripsy, pediatric nephrolithiasis, stone free
Citation: Vinit N, Khoury A, Lopez P, Heidet L, Botto N, Traxer O, Boyer O, Blanc T and Lottmann HB (2021) Extracorporeal Shockwave Lithotripsy for Cystine Stones in Children: An Observational, Retrospective, Single-Center Analysis. Front. Pediatr. 9:763317. doi: 10.3389/fped.2021.763317
Received: 23 August 2021; Accepted: 15 October 2021;
Published: 16 November 2021.
Edited by:
Alberto Parente, Consultant, Madrid, SpainReviewed by:
Hans-Göran Tiselius, Karolinska Institutet (KI), SwedenSerdar Tekgul, Hacettepe University, Turkey
Copyright © 2021 Vinit, Khoury, Lopez, Heidet, Botto, Traxer, Boyer, Blanc and Lottmann. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Henri B. Lottmann, aGVucmkubG90dG1hbm5AYXBocC5mcg==
 Nicolas Vinit
Nicolas Vinit Antoine Khoury
Antoine Khoury Pauline Lopez
Pauline Lopez Laurence Heidet
Laurence Heidet Nathalie Botto1
Nathalie Botto1 Olivia Boyer
Olivia Boyer Thomas Blanc
Thomas Blanc Henri B. Lottmann
Henri B. Lottmann