Commentary: Hematuria as an early sign of multisystem inflammatory syndrome in children: A case report of a boy with multiple comorbidities and a review of the literature
- 1Department of Pediatrics, University Hospital Center Zagreb, Zagreb, Croatia
- 2General Hospital “Dr. Tomislav Bardek”, Koprivnica, Croatia
- 3Department of Pediatrics, School of Medicine, University of Zagreb, Zagreb, Croatia
Introduction: While the clinical course of SARS-CoV-2 infection seems to be milder or asymptomatic within the pediatric population, growing attention has been laid to the rare complication elicited by virus, multisystem inflammatory syndrome in children temporarily associated with COVID-19 (MIS-C). Published definition and criteria of MIS-C include persistent fever, multisystem involvement, and elevated markers of inflammation, without obvious microbial inflammation or other plausible diagnosis. However, the aim of this case report is to emphasize the diversity of symptoms of MIS-C, beyond the defined criteria.
Case Presentation: We present a 10-year-old boy with 8p23.1 microdeletion syndrome and multiple comorbidities who initially came to our attention due to hematuria, persistent fever, rash, and elevated markers of inflammation. Within the next 2 days, his condition worsened despite the broad-spectrum antibiotic therapy. Assuming his past history of SARS-CoV-2 exposure, MIS-C was suspected. A high level of clinical suspicion was further supported by significant clinical features (vomiting, abdominal pain, conjunctivitis, arrhythmia, and mild left ventricular systolic dysfunction with pleural effusion) along with laboratory findings (elevated ESR, CRP, proBNP, D-dimers and fibrinogen, positive IgG SARS-CoV-2 antibodies, and negative microbiological cultures). The patient was given intravenous immunoglobulin (IVIG) and began to show instantaneous clinical and laboratory improvement.
Conclusion: Despite numerous reports of MIS-C cases in children, there are still many uncertainties regarding the clinical presentation and laboratory findings, as well as mechanisms beyond this intriguing disorder. In our case, for the first time hematuria is reported as an early symptom of MIS-C. We strongly believe that reporting various manifestations and outcomes in MIS-C patients will lead to improved diagnosis, treatment, and overall understanding of this novel inflammatory condition.
Introduction
The first experience from the beginning of the COVID-19 pandemic showed that children rarely developed severe or critical illness (1) or die from the infection as compared with adults (2, 3). Nevertheless, since the beginning of the pandemic, multisystem inflammatory syndrome in children (MIS-C), a new phenomenon with temporal association with COVID-19, has become a great concern of parents and pediatricians worldwide (4–6).
The pathogenesis of this syndrome remains largely unknown, but immunological mechanisms and vasculopathy have been implied (7). Literature data are growing on this subject, and although a unique definition and criteria have still not been established, prospective studies and case series have described multiorgan involvement, most commonly including the gastrointestinal, mucocutaneous, cardiac, and respiratory systems (8, 9). Renal involvement is a rather rarely reported manifestation of MIS-C, most commonly presented as acute kidney injury (AKI) in children with a complicated disease course, and seldom as hematuria, proteinuria, and pyuria (Table 1) (10–31). With continued pandemic and increasing awareness of this syndrome among clinicians, it is expected that more cases of MIS-C will be diagnosed and unusual presentations are likely to be seen, while, on the other hand, extensive medical and public attention might result in overdiagnosis of MIS-C, which highlights the need for reporting informative cases (32). Therefore, we describe an unusual case of a boy who initially presented with hematuria, persistent fever, rash, and elevated markers of inflammation, while, within the next 2 days he developed multisystem involvement and met the criteria for MIS-C. Moreover, we performed a literature review of MIS-C patients presenting with renal symptoms. The aim of this case report is to emphasize the diversity of symptoms of MIS-C, beyond the defined criteria.
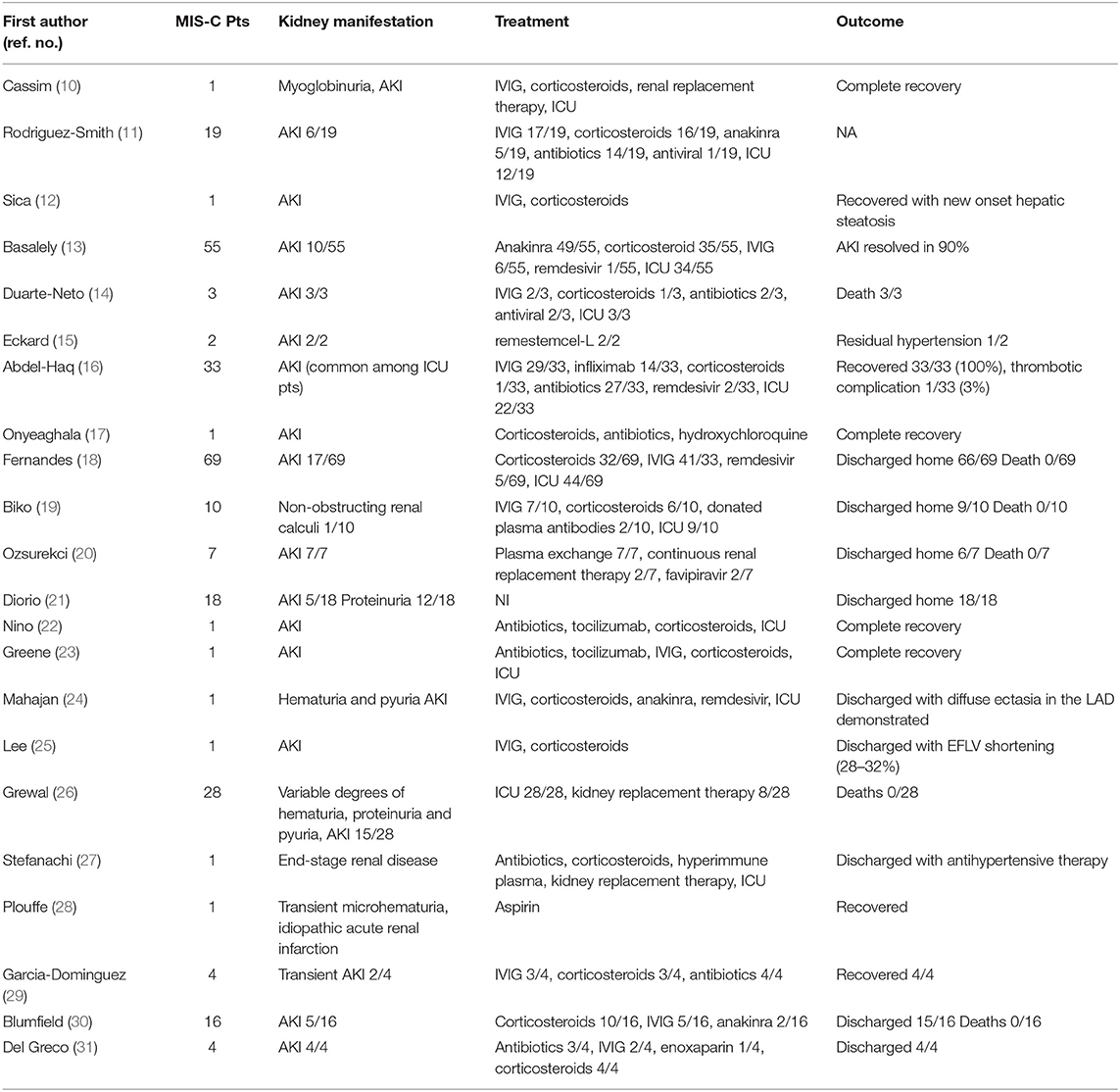
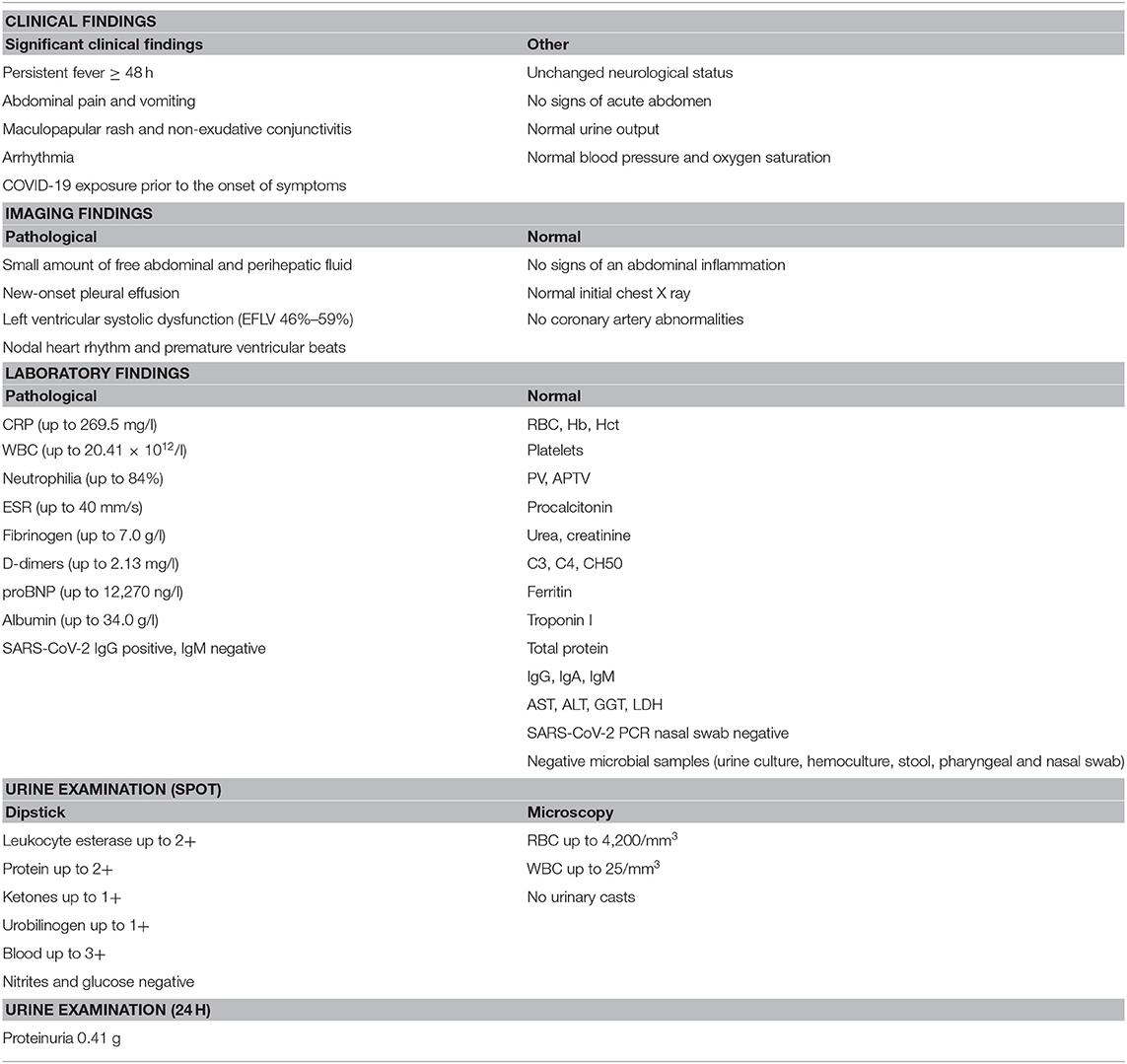
Table 1. Clinical characteristics, treatment modalities, and outcome of MIS-C patients with renal impairment.
Methods
A systematic literature search was conducted to identify MIS-C patients with renal involvement. The Scopus and MEDLINE/PubMed databases were searched (from November 1, 2019, to August 30, 2021) by entering the following keywords “MIS-C” and “kidney” according to the published guidance on narrative reviews. The following parameters were noted from the studies including MIS-C patients: renal impairment, treatment, and outcome. Twenty-two articles describing 277 patients with renal manifestation of MIS-C were found during the literature search (Supplementary Figure 1).
Case Presentation
We present a 10-year-old boy with 8p23.1 microdeletion syndrome who presented to our pediatric emergency department at the end of February 2021, with dry cough and fever lasting for 2 days. Additional medical problems of the patient, associated with microdeletion syndrome, included psychomotor delay, behavioral complications, and complex congenital heart disease that underwent complete surgical correction in infancy. Despite the variety of comorbidities, his underlying medical conditions have been well controlled. His recent medical history included exposure to SARS-CoV-2 infection. The patient's mother, a nurse in a COVID-19 intensive care unit, tested positive for SARS-CoV-2 after onset of symptoms in January 2021. At that time, our patient remained asymptomatic. In the middle of February, he developed dry cough with subfebrile temperature that resolved over several days, but no test for SARS-CoV-2 was performed.
At physical examination, he was febrile and well appearing. He had erythematous maculopapular rash on the right lower leg, while auscultation revealed decreased breathing sound on the right side. Laboratory tests showed neutrophilic leukocytosis, an elevated C-reactive protein (CRP 149.75 mg/l), and hematuria (135 RBC/μl). Initial chest X-ray showed no obvious consolidation or pleural effusion. He was discharged with a diagnosis of acute respiratory infection and recommended to take amoxicillin/clavulanate orally.
The patient returned to our emergency department the following day due to persistent fever, vomiting, prostration, loss of appetite, and abdominal pain, but without significant guarding or peritoneal signs. Due to further elevation of CRP (222.59 mg/l) and progression of hematuria (4,200 RBC/μl) with proteinuria (2+ by dipstick analysis), the patient was admitted to inpatient care. The preadmission screening polymerase chain reaction (PCR) test of SARS-CoV-2 was negative. An abdominal x-ray showed stool burden, while abdominal ultrasound revealed a small amount of free fluid, with no other specific findings. Acute surgical emergency was ruled out by a pediatric surgeon consultant, and constipation was successfully managed with glycerin suppositories and lactulose solution. Further management included intravenous administration of crystalloid solutions and ceftriaxone, but his condition continued to worsen within the next 2 days. He developed bilateral conjunctivitis and irregular heart rhythm. Electrocardiography detected nodal rhythm with ventricular extrasystoles, while echocardiography revealed pleural effusion and mild left ventricular systolic dysfunction (EFLV 46–59%) without coronary artery abnormalities. Moreover, pro-B-type natriuretic peptide (proBNP) was elevated (12,270 ng/l).
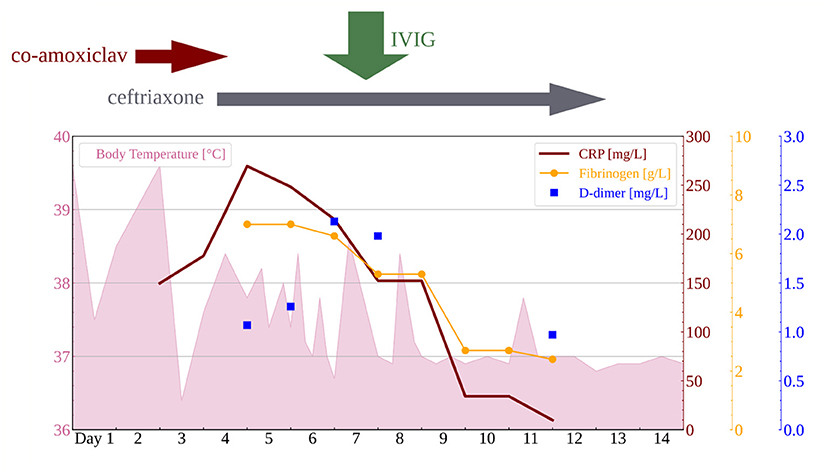
The differential diagnosis at this point included sepsis, myocarditis, and Kawasaki disease. Nevertheless, all three were ruled out by negative blood and urine cultures and normal values of troponin I, creatinine kinase, and platelets, while repeated echocardiography showed no increase of coronary arteries. Assuming his past history of SARS-CoV-2 exposure, MIS-C was finally suspected after 5 days of fever. A high level of clinical suspicion was supported by positive SARS-CoV-2 immunoglobulin G (IgG) and rising erythrocyte sedimentation rate (ESR 40 mm/h), CRP (269.5 mg/l), proBNP (12.270 ng/l), D-dimers (2.13 mg/l), fibrinogen (7.0 g/l), and hypoalbuminemia (34.0 g/l), as shown in Tables 2, 3 and Figure 1.
During this period, hematuria started to resolve, but low-grade proteinuria persisted (24-h urine protein 0.41 g/dU). Global kidney function tests (urea and creatinine), urine output, liver function test, ferritin levels, complement components (C3, C4), and total complement activity (CH50) were within the normal range during the whole course of the disease. There was no cytopenia or decrease in hematological parameters and no casts in urine sediment. Moreover, there were no episodes of hypotension, a decrease in blood oxygen saturation, and no need for inotrope support (Table 2). Finally, on the morning of the seventh day of illness, IVIG was administered in a single dose of 2 g/kg. Therapeutic effects included prompt downtrend of fever, inflammatory markers, and proteinuria, as shown in Figure 1, along with gradual improvement of left ventricular systolic function (EFLV 65–68%) and complete resolution of pleural effusion within the next few days. After 10 days of ceftriaxone therapy, the patient was discharged from the hospital. Outpatient follow-up after 4 weeks revealed complete normalization of clinical and laboratory findings, with no new symptoms and/or signs after 6 months.
Discussion
Children with clinical and laboratory findings associated with inflammation have always presented a diagnostic challenge in everyday clinical practice. On top of many established immune-mediated disorders, in the era of the COVID-19 pandemic MIS-C needs to be considered as well, especially in children unresponsive to antimicrobial therapy (Table 3). Nevertheless, despite the growing number of reports in the literature, the full extent of the MIS-C manifestations remains unknown. Conversely, a wide range of reported symptoms and signs makes the diagnostic process of this novel syndrome confusing or delayed. Therefore, early recognition and valid interpretation of characteristic features lead to accurate diagnosis and proper treatment, and eventually to elucidation of the underlying mechanisms.
Although an enhanced understanding of the processes beyond the MIS-C is essential for effective treatment, despite many recent efforts they remain inconclusive. Different pathogenesis traits have been proposed, but the predominant theory is the postinfection antibody-mediated disease (7, 33, 34). However, evidence is mounting that vasculopathy has an important role in MIS-C (33, 34). Evidence supporting this theory incorporates the resemblance of MIS-C and Kawasaki disease, a known vasculitis (35–37). Similar features of these two inflammatory disorders include prolonged fever, increased inflammatory markers, rash, non-exudative conjunctivitis, and mucous involvement (cracked lips, strawberry tongue) (33, 35–37). Despite these resemblances, there are also marked differences in clinical manifestations, such as older age of onset, more frequently observed gastrointestinal involvement, and a more severe disease course in MIS-C, as well as dissimilarities in laboratory findings, such as lymphopenia, thrombocytopenia, and elevated D-dimer levels in MIS-C (33, 35, 37). Comparison of inflammatory cells and 180 plasma proteins in patients with MIS-C and Kawasaki disease revealed that both conditions have elements of hyperinflammation and vasculitis but a different cytokine pattern, suggesting different pathogenesis (33). Other noteworthy characteristics of MIS-C implying vasculopathy is the common presence of coagulation disorders (34, 38, 39). Elevated levels of D-dimer and von Willebrand factor are seen in almost all patients with MIS-C, while fibrinogen levels and prothrombin time are also frequently increased (34, 38, 39). In addition, an intriguing case report has been published, describing intestinal ischemia in a patient with MIS-C presenting with severe abdominal pain and pseudoappendicular syndrome, suggesting intestinal vasculitis (40).
Moreover, it has been suggested that MIS-C could be a severe form of acute COVID-19 infection (7, 34). This theory is supported by the fact that children mostly lack respiratory symptoms and therefore a nasal swab positive for COVID should not be expected. Instead, Rowley et al. proposed PCR analysis on stool samples since children mainly have gastrointestinal symptoms (7). On the other hand, the respiratory mucosal epithelium is most commonly the entry point of virus in adults (41), and therefore, it is fair to mark the lung as a “primary battle zone.” Accordingly, the highest levels of SARS-CoV-2 virus per cell were detected within the respiratory tract. Nevertheless, viral particles were also isolated from many other organs, including the kidney, liver, brain, heart muscle, blood, small intestine, and even sweat glands and skin (41). Many studies reported that SARS-CoV-2 was isolated from the kidney in COVID-19 patients with kidney involvement or coexisting chronic kidney disease (42). Multiorgan tropism and its affinity and affection of the kidney especially indicate that AKI might be a consequence of direct viral toxicity (42). However, it remains unclear if the cell invasion is the sole mechanism responsible for kidney manifestations of COVID-19. Angiotensin-converting enzyme 2 (ACE 2) has been identified as the cell entry receptor for SARS-CoV-2, making the tubular cells that harbor ACE2 especially vulnerable and resulting in tubular damage (43). On the contrary, new cases of collapsing glomerulopathy emerged in patients of African ancestry who are homozygous for APOL risk alleles, potentially suggesting other specific molecular mechanisms (44).
The European Renal Association revealed that advanced chronic kidney disease is an independent risk factor for poorer outcome of COVID-19 (45), while de novo kidney disease is commonly seen in hospitalized patients with COVID-19 as well, especially in those critically ill (46). The available literature most commonly describes renal involvement in children with MIS-C as acute renal failure or AKI (4, 39, 47–50). The prevalence of renal involvement varies greatly depending on the studied population (4, 39, 47–49). Two French studies, in which complicated MIS-C cases needing intensive care were enrolled, described a prevalence of 59 and 70%, respectively (4, 48), while a large US cohort of 570 MIS-C patients reported AKI in 18% of patients (42, 47); an Iranian study reported renal failure in 29% of patients (49). In most studies, the course of renal failure was not elaborated in detail (38, 47, 49). In the US study, kidney injury was sought a complication of severe MIS-C (47); in the Iranian study a consequence of high levels of ACE2 in the kidney (49). Since renal failure is present more frequently in COVID and MIS-C patients needing intensive care, circulatory shock may be an important contributor to renal failure development (4, 48, 51).
Additionally, among 277 MIS-C patients with renal involvement identified during our literature search, the most commonly reported manifestation was AKI (Table 1). Compared to patients without AKI, it was more frequent among patients who had cardiac dysfunction, required inotropic support, and ICU admission (26). Accordingly, pathogenesis of AKI appears to be predominantly pre-renal (26). On the other hand, severity of kidney dysfunction in patients with AKI did not correlate with degree of cardiac dysfunction (26). Beside AKI, other renal manifestations or urinalysis results in MIS-C patients were described only in few articles, reporting variable degrees of hematuria, proteinuria, and pyuria (21, 24, 28). Interestingly, abnormal urinalysis as indicator of renal parenchymal injury was present in a significant proportion of AKI patients (21, 24). Furthermore, proteinuria was a predominant symptom in MIS-C patients who also met the clinical criteria for thrombotic microangiopathy (TMA) (21). TMA is a clinical syndrome defined by the presence of hemolytic anemia, thrombocytopenia, and organ dysfunction due to endothelial cell damage and formation of microscopic blood clots in capillaries and small arteries. Soluble C5b9 (Sc5b9), a biomarker of complement activation and TMA, was elevated in patients with SARS-CoV-2 disease, as well as in MIS-C patients (21). Consequently, increased plasma levels of the terminal complement complex (sC5b9) suggest that complement activation and thrombotic microangiopathy are prevalent in COVID-19 and MIS-C patients (21). Although many of the described patients beside IVIG required an additional treatment with glucocorticoids, antibiotics, biological agents, and even plasmapheresis and renal replacement therapy, in many complete recovery was reported (10, 17, 22, 23, 28, 29).
It remains unknown whether hematuria and proteinuria were really absent in the published cohorts or they were underreported. Although hematuria and proteinuria might have been neglected in MIS-C patients, they are rather common manifestations of adult COVID-19 infection (51–53), ranging from 7 to 63% of patients for proteinuria (51) and 26.7% (52) and 40.9% (53) for hematuria. Histopathological analysis of renal tissue of COVID patients revealed viral fragments in the cytoplasm of proximal tubules as well as podocytes, which could potentially explain proteinuria (51). Another common finding in adults is obstruction of glomerular lumen and peritubular capillaries by erythrocyte aggregates (51). In children, hematuria and SARS-CoV-2 infection were described in a 9-year-old girl who presented with increased temperature, cough, and gross hematuria, which resolved spontaneously (54). SARS-CoV-2 was isolated not only from her nasal swab but also from her urine sample (54). Another case describes a 13-year-old boy who presented with purpuric rashes, mild hematuria, elevation of serum IgA, and biopsy-confirmed leukocytoclastic vasculitis secondary to asymptomatic SARS-CoV-2 infection (55). This is in line with the notion that hematuria is most commonly associated with vasculitis syndromes such as immunoglobulin A (IgA) nephropathy or anti-neutrophil cytoplasmic autoantibody (ANCA)-associated vasculitis (56). Furthermore, recent findings suggest that gross hematuria can damage the glomeruli and lead to AKI (56).
In our patient, there were no signs of kidney function deterioration, hypotension, or need for inotropic support, although a moderate cardiac dysfunction was noted. Moreover, he had no signs of TMA or complement dysfunction. Besides, he had a complete and persistent resolution of all symptoms and signs following only IVIG therapy, without further need for glucocorticoid treatment. Therefore, no additional laboratory tests or invasive procedures were performed. Consequently, limitations of this case presentation are lack of ANA and ANCA screening and lack of kidney biopsy results, which restricts the conclusion about the possible underlying mechanisms in our patient. Nevertheless, of note is that ANCA-associated vasculitis after COVID-19 was described in a few patients presenting with hematuria, proteinuria, and AKI (57, 58). Hence, SARS-CoV-2 infection is suspected to be the trigger of subsequent development of immune-mediated disorders, which prompts a long follow-up in susceptible patients.
In summary, the pathogenesis of renal involvement in COVID-19 is probably multifactorial, and proposed mechanisms include direct infection of renal parenchyma via ACE2 receptors which are highly present in kidney tissue (43, 52, 59), microvascular injury caused by cytokine storm and/or hypercoagulability (25, 43, 51, 59), and circulatory shock (4, 48, 49).
To the best of our knowledge, this is the first detailed case of hematuria and concomitant proteinuria in an MIS-C patient. Since additional investigations and follow-up revealed no other pathological finding, we are confident that hematuria in the presented patient was a part of MIS-C. This is further supported by the fact that our patient had no sign of hypovolemia, which could have potentially caused kidney damage, and prompt response to IVIG therapy. Since proteinuria and hematuria have resolved, we did not proceed with further investigations.
We report this unusual MIS-C case because the COVID-19 pandemic is still ongoing, and the number of MIS-C cases will probably continue to grow. Moreover, it is not false to predict that other possible pandemics in the future might also cause similar symptoms. We strongly believe that unusual and yet undescribed clinical presentations are useful for the practicing clinicians, especially with diseases like MIS-C, where early recognition is essential for treatment and good outcomes. Moreover, detailed clinical reports can also inform further research on pathogenesis and possible treatment options. Finally, we consider our case to be another piece of evidence tipping the scale toward the underlying process in MIS-C.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics Statement
Written informed consent was obtained from the individuals for the publication of any potentially identifiable images or data included in this article.
Author Contributions
LL conceptualized the work. AG and MD drafted this manuscript. IK, KV, and LL revised this manuscript. All authors were involved in the clinical management of the patient and read and approved the manuscript for submission.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2021.760070/full#supplementary-material
Supplementary Figure 1. The schematic overview of the articles on MIS-C patients with renal impairment included in the literature research.
Abbreviations
ACE2, angiotensin-converting enzyme 2; AKI, acute kidney injury; ANCA, anti-neutrophil cytoplasmic autoantibody; COVID-19, coronavirus disease-2019; CRP, C-reactive protein; EFLV, left ventricular ejection fraction; ESC, erythrocyte sedimentation rate; ICU, intensive care unit; IVIG, intravenous immune globulin; IgA, immunoglobulin A; IgG, immunoglobulin G; MIS-C, multisystem inflammatory syndrome in children; proBNP, pro-B-type natriuretic peptide; PCR, polymerase chain reaction; RBC, red blood cell; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; TMA, thrombotic microangiopathy.
References
1. Dong Y, Mo X, Hu Y, Qi X, Jiang F, Jiang Z, et al. Epidemiology of COVID-19 among children in China. Pediatrics. (2020) 145:e20200702. doi: 10.1542/peds.2020-0702
2. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the chinese center for disease control and prevention. JAMA. (2020) 323:1239–42. doi: 10.1001/jama.2020.2648
3. Zimmermann P, Curtis N. Coronavirus infections in children including COVID-19: an overview of the epidemiology, clinical features, diagnosis, treatment and prevention options in children. Pediatr Infect Dis J. (2020) 39:355–68. doi: 10.1097/INF.0000000000002660
4. Pouletty M, Borocco C, Ouldali N, Caseris M, Basmaci R, Lachaume N, et al. Paediatric multisystem inflammatory syndrome temporally associated with SARS-CoV-2 mimicking Kawasaki disease (Kawa-COVID-19): a multicentre cohort. Ann Rheum Dis. (2020) 79:999–1006. doi: 10.1136/annrheumdis-2020-217960
5. Ramcharan T, Nolan O, Lai CY, Prabhu N, Krishnamurthy R, Richter AG, et al. Paediatric inflammatory multisystem syndrome: temporally associated with SARS-CoV-2 (PIMS-TS): cardiac features, management and short-term outcomes at a UK tertiary paediatric hospital. Pediatr Cardiol. (2020) 41:1391–401. doi: 10.1007/s00246-020-02391-2
6. Haslak F, Yildiz M, Adrovic A, Sahin S, Barut K, Kasapcopur O, et al. Recently explored aspect of the iceberg named COVID-19: multisystem inflammatory syndrome in children (MIS-C). Turk Arch Pediatr. (2021) 56:3–9. doi: 10.5152/TurkArchPediatr.2020.20245
7. Rowley AH. Understanding SARS-CoV-2-related multisystem inflammatory syndrome in children. Nat Rev Immunol. (2020) 20:453–4. doi: 10.1038/s41577-020-0367-5
8. Esposito S, Principi N. Multisystem inflammatory syndrome in children related to SARS-CoV-2. Paediatr Drugs. (2021) 23:119–29. doi: 10.1007/s40272-020-00435-x
9. Haslak F, Barut K, Durak C, Aliyeva A, Yildiz M, Guliyeva V, et al. Clinical features and outcomes of 76 patients with COVID-19-related multi-system inflammatory syndrome in children. Clin Rheumatol. (2021) 40:4167–78. doi: 10.1007/s10067-021-05780-x
10. Cassim F, Soni AJ, Murphy S. Severe acute inflammatory myositis and rhabdomyolysis in paediatric SARS-CoV-2-associated MIS-C (multisystem inflammatory syndrome in children). BMJ Case Rep. (2021) 14:e243112. doi: 10.1136/bcr-2021-243112
11. Rodriguez-Smith JJ, Verweyen EL, Clay GM, Esteban YM, de Loizaga SR, Baker EJ, et al. Inflammatory biomarkers in COVID-19-associated multisystem inflammatory syndrome in children, Kawasaki disease, and macrophage activation syndrome: a cohort study. Lancet Rheumatol. (2021) 3:e574–e84. doi: 10.1016/S2665-9913(21)00139-9
12. Sica R, Pennoni S, Penta L, Di Cara G, Verrotti A. New onset of hepatic steatosis post-severe multisystem inflammatory syndrome in children (MIS-C): a case report. Int J Environ Res Public Health. (2021) 18:6961. doi: 10.3390/ijerph18136961
13. Basalely A, Gurusinghe S, Schneider J, Shah SS, Siegel LB, Pollack G, et al. Acute kidney injury in pediatric patients hospitalized with acute COVID-19 and multisystem inflammatory syndrome in children associated with COVID-19. Kidney Int. (2021) 100:138–45. doi: 10.1016/j.kint.2021.02.026
14. Duarte-Neto AN, Caldini EG, Gomes-Gouvea MS, Kanamura CT, de Almeida Monteiro RA, Ferranti JF, et al. An autopsy study of the spectrum of severe COVID-19 in children: From SARS to different phenotypes of MIS-C. EClinicalMedicine. (2021) 35:100850. doi: 10.1016/j.eclinm.2021.100850
15. Eckard AR, Borow KM, Mack EH, Burke E, Atz AM. Remestemcel-L therapy for COVID-19-associated multisystem inflammatory syndrome in children. Pediatrics. (2021) 147:e2020046573. doi: 10.1542/peds.2020-0465
16. Abdel-Haq N, Asmar BI, Deza Leon MP, McGrath EJ, Arora HS, Cashen K, et al. SARS-CoV-2-associated multisystem inflammatory syndrome in children: clinical manifestations and the role of infliximab treatment. Eur J Pediatr. (2021) 180:1581–91. doi: 10.1007/s00431-021-03935-1
17. Onyeaghala C, Alasia D, Eyaru O, Paul N, Maduka O, Osemwegie N, et al. Multisystem inflammatory syndrome (MIS-C) in an adolescent Nigerian girl with COVID-19: A call for vigilance in Africa. Int J Infect Dis. (2021) 105:124–9. doi: 10.1016/j.ijid.2021.02.017
18. Fernandes DM, Oliveira CR, Guerguis S, Eisenberg R, Choi J, Kim M, et al. Severe acute respiratory syndrome coronavirus 2 clinical syndromes and predictors of disease severity in hospitalized children and youth. J Pediatr. (2021) 230:23–31 e10. doi: 10.1016/j.jpeds.2020.11.016
19. Biko DM, Ramirez-Suarez KI, Barrera CA, Banerjee A, Matsubara D, Kaplan SL, et al. Imaging of children with COVID-19: experience from a tertiary children's hospital in the United States. Pediatr Radiol. (2021) 51:239–47. doi: 10.1007/s00247-020-04830-x
20. Ozsurekci Y, Oygar PD, Gurlevik SL, Kesici S, Ozen S, Kurt Sukur ED, et al. Favipiravir use in children with COVID-19 and acute kidney injury: is it safe? Pediatr Nephrol. (2021) 2021:1–6. doi: 10.1007/s00467-021-05111-x
21. Diorio C, McNerney KO, Lambert M, Paessler M, Anderson EM, Henrickson SE, et al. Evidence of thrombotic microangiopathy in children with SARS-CoV-2 across the spectrum of clinical presentations. Blood Adv. (2020) 4:6051–63. doi: 10.1182/bloodadvances.2020003471
22. Nino-Taravilla C, Espinosa-Vielma YP, Otaola-Arca H, Poli-Harlowe C, Tapia LI, Ortiz-Fritz P. Pediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2 treated with tocilizumab. Pediatr Rep. (2020) 12:142–8. doi: 10.3390/pediatric12030029
23. Greene AG, Saleh M, Roseman E, Sinert R. Toxic shock-like syndrome and COVID-19: multisystem inflammatory syndrome in children (MIS-C). Am J Emerg Med. (2020) 38:2492.e5–e6. doi: 10.1016/j.ajem.2020.05.117
24. Mahajan N, Chang HT, Leeman R, Manalo R, Glaberson WR. Case of multisystem inflammatory syndrome in children presenting as fever and abdominal pain. BMJ Case Rep. (2020) 13:e237306. doi: 10.1136/bcr-2020-237306
25. Lee M, Hilado M, Sotelo S, Opas LM, Im DD. Acute kidney injury in multisystem inflammatory syndrome in children (MIS-C): a case report. SN Compr Clin Med. (2020) 2020:1–4. doi: 10.1007/s42399-020-00647-9
26. Grewal MK, Gregory MJ, Jain A, Mohammad D, Cashen K, Ang JY, et al. Acute kidney injury in pediatric acute SARS-CoV-2 infection and multisystem inflammatory syndrome in children (MIS-C): is there a difference? Front Pediatr. (2021) 9:692256. doi: 10.3389/fped.2021.692256
27. Stefanachi F, Benetti E, Longo G, Parolin M, Bonardi CM, Meneghesso D. SARS-CoV2 related multi system inflammatory syndrome in a child with chronic kidney disease: case report. SN Compr Clin Med. (2021) 2021:1–3. doi: 10.1007/s42399-021-01004-0
28. Plouffe B, Van Hooren T, Barton M, Nashid N, Demirkaya E, Norozi K, et al. Renal infarcts-a perplexing case in the middle of the COVID-19 pandemic. Front Pediatr. (2021) 9:669453. doi: 10.3389/fped.2021.669453.eCollection2021
29. Garcia-Dominguez M, Angeles-Meneses Y, Lares-Payan A, Velazquez-Rios CA, Tostado Morales E, Perez-Gaxiola G. Multisystemic inflammatory syndrome in children associated with SARS-CoV-2 infection: a case series report in a pediatric center in Mexico. J Med Cases. (2020) 11:375–8. doi: 10.14740/jmc3584
30. Blumfield E, Levin TL, Kurian J, Lee EY, Liszewski MC. Imaging findings in multisystem inflammatory syndrome in children (MIS-C) associated with coronavirus disease (COVID-19). AJR Am J Roentgenol. (2021) 216:507–17. doi: 10.2214/AJR.20.24032
31. Del Greco G, Brady K, Clark B, Park HA. Novel pediatric multisystem inflammatory syndrome during the COVID-19 pandemic. Pediatr Emerg Care. (2020) 36:500–4. doi: 10.1097/PEC.0000000000002229
32. Levi H, Ruben VP, Filomeen H. Multisystem inflammatory syndrome in children related to COVID-19: a systematic review. Eur J Pediatr. (2021) 2021:1–16. doi: 10.1007/s00431-021-03993-5
33. Consiglio CR, Cotugno N, Sardh F, Pou C, Amodio D, Rodriguez L, et al. The immunology of multisystem inflammatory syndrome in children with COVID-19. Cell. (2020) 183:968–81.e7. doi: 10.1016/j.cell.2020.09.016
34. McMurray JC, May JW, Cunningham MW, Jones OY. Multisystem inflammatory syndrome in children (MIS-C), a Post-viral myocarditis and systemic vasculitis-a critical review of its pathogenesis and treatment. Front Pediatr. (2020) 8:626182. doi: 10.3389/fped.2020.626182
35. Loke YH, Berul CI, Harahsheh AS. Multisystem inflammatory syndrome in children: Is there a linkage to Kawasaki disease? Trends Cardiovasc Med. (2020) 30:389–96. doi: 10.1016/j.tcm.2020.07.004
36. Nelson C, Ishimine P, Hayden SR, Correia M, Wardi G. Multisystem inflammatory syndrome in children (MIS-C) in an adolescent that developed coronary aneurysms: a case report and review of the literature. J Emerg Med. (2020) 59:699–704. doi: 10.1016/j.jemermed.2020.09.008
37. Otar Yener G, Pac Kisaarslan A, Ulu K, Atalay E, Haslak F, Ozdel S, et al. Differences and similarities of multisystem inflammatory syndrome in children, Kawasaki disease and macrophage activating syndrome due to systemic juvenile idiopathic arthritis: a comparative study. Rheumatol Int. (2021) 2021:1–11. doi: 10.1007/s00296-021-04980-7
38. Lee PY, Day-Lewis M, Henderson LA, Friedman KG, Lo J, Roberts JE, et al. Distinct clinical and immunological features of SARS-CoV-2-induced multisystem inflammatory syndrome in children. J Clin Invest. (2020) 130:5942–50. doi: 10.1172/JCI141113
39. Lima-Setta F, Magalhaes-Barbosa MC, Rodrigues-Santos G, Figueiredo E, Jacques ML, Zeitel RS, et al. Multisystem inflammatory syndrome in children (MIS-C) during SARS-CoV-2 pandemic in Brazil: a multicenter, prospective cohort study. J Pediatr (Rio J). (2021) 97:354–61. doi: 10.1016/j.jped.2020.10.008
40. Khesrani LS, Chana K, Sadar FZ, Dahdouh A, Ladjadj Y, Bouguermouh D. Intestinal ischemia secondary to Covid-19. J Pediatr Surg Case Rep. (2020) 61:101604. doi: 10.1016/j.epsc.2020.101604
41. Puelles VG, Lutgehetmann M, Lindenmeyer MT, Sperhake JP, Wong MN, Allweiss L, et al. Multiorgan and renal tropism of SARS-CoV-2. N Engl J Med. (2020) 383:590–2. doi: 10.1056/NEJMc2011400
42. Braun F, Lütgehetmann M, Pfefferle S, Wong MN, Carsten A, Lindenmeyer MT, et al. SARS-CoV-2 renal tropism associates with acute kidney injury. Lancet. (2020) 396:597–8. doi: 10.1016/S0140-6736(20)31759-1
43. Batlle D, Soler MJ, Sparks MA, Hiremath S, South AM, Welling PA, et al. Acute kidney injury in COVID-19: emerging evidence of a distinct pathophysiology. J Am Soc Nephrol. (2020) 31:1380–3. doi: 10.1681/ASN.2020040419
44. Izzedine H, Brocheriou I, Arzouk N, Seilhean D, Couvert P, Cluzel P, et al. COVID-19-associated collapsing glomerulopathy: a report of two cases and literature review. Intern Med J. (2020) 50:1551–8. doi: 10.1111/imj.15041
45. Council E-E, Group EW. Chronic kidney disease is a key risk factor for severe COVID-19: a call to action by the ERA-EDTA. Nephrol Dial Transplant. (2021) 36:87–94. doi: 10.1093/ndt/gfaa314
46. Vijayan A, Humphreys BD. SARS-CoV-2 in the kidney: bystander or culprit? Nat Rev Nephrol. (2020) 16:703–4. doi: 10.1038/s41581-020-00354-7
47. Godfred-Cato S, Bryant B, Leung J, Oster ME, Conklin L, Abrams J, et al. COVID-19-associated multisystem inflammatory syndrome in children—United States, March–July 2020. MMWR Morb Mortal Wkly Rep. (2020) 69:1074–80. doi: 10.15585/mmwr.mm6932e2
48. Grimaud M, Starck J, Levy M, Marais C, Chareyre J, Khraiche D, et al. Acute myocarditis and multisystem inflammatory emerging disease following SARS-CoV-2 infection in critically ill children. Ann Intensive Care. (2020) 10:69. doi: 10.1186/s13613-020-00690-8
49. Mamishi S, Movahedi Z, Mohammadi M, Ziaee V, Khodabandeh M, Abdolsalehi MR, et al. Multisystem inflammatory syndrome associated with SARS-CoV-2 infection in 45 children: a first report from Iran. Epidemiol Infect. (2020) 148:e196. doi: 10.1017/S095026882000196X
50. Sethi SK, Rana A, Adnani H, McCulloch M, Alhasan K, Sultana A, et al. Kidney involvement in multisystem inflammatory syndrome in children: a pediatric nephrologist's perspective. Clin Kidney J. (2021) 14:2000–11. doi: 10.1093/ckj/sfab073
51. Gabarre P, Dumas G, Dupont T, Darmon M, Azoulay E, Zafrani L. Acute kidney injury in critically ill patients with COVID-19. Intensive Care Med. (2020) 46:1339–48. doi: 10.1007/s00134-020-06153-9
52. Cheng Y, Luo R, Wang K, Zhang M, Wang Z, Dong L, et al. Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney Int. (2020) 97:829–38. doi: 10.1016/j.kint.2020.03.005
53. Nadim MK, Forni LG, Mehta RL, Connor MJ Jr, Liu KD, Ostermann M, et al. COVID-19-associated acute kidney injury: consensus report of the 25th Acute Disease Quality Initiative (ADQI) Workgroup. Nat Rev Nephrol. (2020) 16:747–64. doi: 10.1038/s41581-020-00356-5
54. Almeida FJ, Olmos RD, Oliveira DBL, Monteiro CO, Thomazelli LM, Durigon EL, et al. Hematuria associated with SARS-CoV-2 infection in a child. Pediatr Infect Dis J. (2020) 39:e161. doi: 10.1097/INF.0000000000002737
55. Kumar G, Pillai S, Norwick P, Bukulmez H. Leucocytoclastic vasculitis secondary to COVID-19 infection in a young child. BMJ Case Rep. (2021) 14:e242192. doi: 10.1136/bcr-2021-242192
56. Moreno JA, Sevillano A, Gutierrez E, Guerrero-Hue M, Vazquez-Carballo C, Yuste C, et al. Glomerular hematuria: cause or consequence of renal inflammation? Int J Mol Sci. (2019) 20:2205. doi: 10.3390/ijms20092205
57. Izci Duran T, Turkmen E, Dilek M, Sayarlioglu H, Arik N. ANCA-associated vasculitis after COVID-19. Rheumatol Int. (2021) 41:1523–9. doi: 10.1007/s00296-021-04914-3
58. Fireizen Y, Shahriary C, Imperial ME, Randhawa I, Nianiaris N, Ovunc B. Pediatric P-ANCA vasculitis following COVID-19. Pediatr Pulmonol. (2021) 56:3422–424. doi: 10.22541/au.162055806.69831997
Keywords: hematuria, multisystem inflammatory syndrome in children (MIS-C), SARS-CoV-2, kidney, Kawasaki disease
Citation: Generalić A, Davidović M, Kos I, Vrljičak K and Lamot L (2021) Hematuria as an Early Sign of Multisystem Inflammatory Syndrome in Children: A Case Report of a Boy With Multiple Comorbidities and Review of Literature. Front. Pediatr. 9:760070. doi: 10.3389/fped.2021.760070
Received: 17 August 2021; Accepted: 09 September 2021;
Published: 27 October 2021.
Edited by:
Ozgur Kasapcopur, Istanbul University-Cerrahpasa, TurkeyReviewed by:
Rabia Miray Kisla Ekinci, Adana City Training and Research Hospital, Ministry of Health, TurkeyAmra Adrovic, Istanbul University-Cerrahpasa, Turkey
Copyright © 2021 Generalić, Davidović, Kos, Vrljičak and Lamot. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Maša Davidović, lavic7@gmail.com
 Ana Generalić
Ana Generalić Maša Davidović
Maša Davidović Ivanka Kos
Ivanka Kos Kristina Vrljičak1
Kristina Vrljičak1 Lovro Lamot
Lovro Lamot