- 1Division of Critical Care Medicine, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States
- 2Department of Pediatrics, Northwestern University Feinberg School of Medicine, Chicago, IL, United States
- 3Stanley Manne Children's Research Institute, Chicago, IL, United States
- 4Data Analytics and Reporting, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States
- 5Division of Autonomic Medicine, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States
Objective: Re-hospitalization after sepsis can lead to impaired quality of life. Predictors of re-hospitalization could help identify sepsis survivors who may benefit from targeted interventions. Our goal was to determine whether low heart rate variability (HRV), a measure of autonomic nervous system dysfunction, is associated with re-hospitalization in pediatric septic shock survivors.
Materials and Methods: This was a retrospective, observational cohort study of patients admitted between 6/2012 and 10/2020 at a single institution. Patients admitted to the pediatric intensive care unit with septic shock who had continuous heart rate data available from the bedside monitors and survived their hospitalization were included. HRV was measured using age-normalized z-scores of the integer HRV (HRVi), which is the standard deviation of the heart rate sampled every 1 s over 5 consecutive minutes. The 24-h median HRVi was assessed on two different days: the last 24 h of PICU admission (“last HRVi”) and the 24-h period with the lowest median HRVi (“lowest HRVi”). The change between the lowest and last HRVi was termed “delta HRVi.” The primary outcome was re-hospitalization within 1 year of discharge, including both emergency department encounters and hospital readmission, with sensitivity analyses at 30 and 90 days. Kruskal-Wallis, logistic regression, and Poisson regression evaluated the association between HRVi and re-hospitalizations and adjusted for potential confounders.
Results: Of the 463 patients who met inclusion criteria, 306 (66%) were re-hospitalized, including 270 readmissions (58%). The last HRVi was significantly lower among re-hospitalized patients compared to those who were not (p = 0.02). There was no difference in the lowest HRVi, but patients who were re-hospitalized showed a smaller recovery in their delta HRVi compared to those who were not re-hospitalized (p = 0.02). This association remained significant after adjusting for potential confounders. In the sensitivity analysis, a smaller recovery in delta HRVi was consistently associated with a higher likelihood of re-hospitalization.
Conclusion: In pediatric septic shock survivors, a smaller recovery in HRV during the index admission is significantly associated with re-hospitalization. This continuous physiologic measure could potentially be used as a predictor of patients at risk for re-hospitalization and lower health-related quality of life.
Introduction
Sepsis is a leading cause of morbidity and mortality worldwide (1–3). Up to 35% of pediatric sepsis survivors experience deterioration in their health-related quality of life (HRQL) for at least 1 year following hospitalization (4–6). Children who experience severe sepsis and septic shock are also more likely to utilize the healthcare system subsequently (7, 8). Certain factors associated with a sepsis admission increase the risk of death or deterioration in HRQL at 3 months, including renal replacement therapy, extracorporeal life support, and cardiopulmonary resuscitation (9). Certain biomarkers (specifically, the PERSEVERE tool which includes C-C chemokine ligand 3 (CCL3), interleukin 8 (IL8), heat shock protein 70 kDa 1B, granzyme B, and matrix metallopeptidase 8) have also been shown to predict HRQL at 3 months (10). While measures of autonomic nervous system (ANS) function have been used to risk-stratify critically ill patients at risk of poor outcomes (11, 12), it is unknown if these measures are associated with risk of readmission or lower HRQL in survivors.
The ANS is a unique system as it regulates functions in all organ systems, maintaining homeostasis when confronted with stressors, including sepsis (13). ANS dysfunction (ANSD) may occur during an imbalanced or maladaptive response to infection, and is often identified as excessive, uncontrolled, or prolonged sympathetic activation, or inappropriate regulation by the parasympathetic nervous system (14). Most of the evidence of ANSD in critical illness is based on measures of heart rate variability (HRV), a non-invasive, continuous physiologic marker of ANS function that is inversely correlated with organ dysfunction and mortality in both adult and pediatric patients (11, 15–17). The goal of this study was to assess whether HRV during an index admission for septic shock was associated with re-hospitalizations within a year in survivors.
Materials and Methods
Study Design and Patient Population
This was a retrospective, observational cohort study from 6/2012 to 10/2020 at a single institution. Patients admitted to the pediatric intensive care unit (PICU) with septic shock who had heart rate data available from bedside monitors were included in the analysis. Septic shock was defined as the need for vasoactive medications in children with confirmed or suspected infection within 72 h of PICU admission. The study was approved with a waiver of consent by Ann & Robert H. Lurie Children's Hospital of Chicago institutional review board (IRB #2020-3868).
HRV Measurement
Continuous heart rate data from the entire PICU stay were extracted from bedside monitors using the BedMaster system (Hillrom, Jupiter, FL) and stored locally in an archiving system within hospital servers. HRV was estimated using the integer HRV (HRVi), which was calculated as the standard deviation of the heart rate sampled every 1 s over 5 consecutive minutes and normalized for age as previously described (11). A minimum of 50% of the heart rate samples in each 5-min interval were needed to be included in the analysis. Within each 5-min interval included, data availability was high, with >90% of intervals including >90% of possible heart rate samples. The median HRVi in 24 h was assessed on two different days: the last 24 h of PICU admission (“last HRVi,” a proxy for the pre-discharge level of ANSD) and the 24-h period with the lowest median HRVi during the PICU admission (“lowest HRVi,” a proxy for the most severe ANSD). The change between the lowest and the last HRVi was also calculated and termed “delta HRVi.”
Outcomes
The primary outcome was all cause re-hospitalization to the same institution within 1 year from the index admission, including emergency department visits and hospital readmissions (both inpatient and PICU). The secondary outcome was the total number of re-hospitalizations (both inpatient and ICUs) within 1 year from the index admission to the same institution.
Confounder Analysis
To address possible confounders of re-hospitalization, we used a multivariable regression analysis to adjust for age, severity of illness on admission using the Pediatric Risk of Mortality (PRISM) III (18), immunocompromised state, and chronic comorbid conditions. Immunocompromised status (defined as an oncologic diagnosis and/or transplantation) and chronic comorbid conditions were classified according to Feudtner's criteria (19). We defined multi-comorbidity as having 2 or more chronic comorbid conditions. We chose these confounders a priori based on common risk factors associated with poor outcomes in children with septic shock that may also influence HRV.
Sensitivity Analysis
To determine if there were differences in the associations based on the timeframe of re-hospitalization, we performed a sensitivity analysis of patients re-hospitalized within 30 days and within 90 days from the index admission.
Statistical Analysis
Data were analyzed using R version 3.6.1 (R Foundation for Statistical Computing, Vienna, Austria) (20). Kruskal-Wallis and chi-square tests, logistic regression (primary outcome), and Poisson regression (secondary outcome) were performed to evaluate the association between HRVi measurements and re-hospitalization.
Results
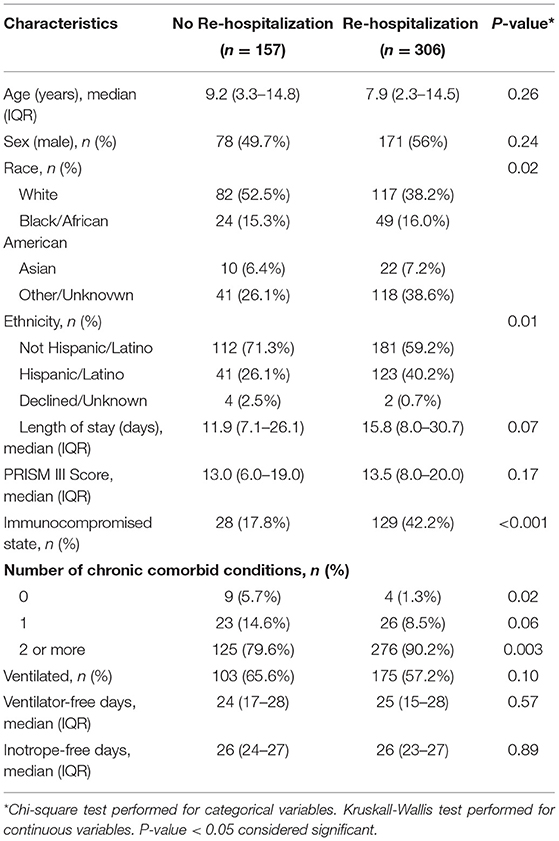
There were 463 patients who met inclusion criteria during the study period. Of those patients, 306 (66%) were re-hospitalized within 1 year, and 270 (58%) were readmitted to an inpatient ward or an ICU. The demographics and clinical characteristics of these patients during their index admission are presented in Table 1. Of all the patients in this cohort, 34% were immunocompromised and 87% had multi-comorbidity. Patients who were re-hospitalized were more likely to be non-white and Hispanic/Latino and more likely to be immunocompromised (42.2 vs. 17.8%). There were no differences in age, sex, PRISM III, technology dependence, length of stay, inotrope-free days, or ventilator-free days at 28 days. Patients who were re-hospitalized had on average 3 re-hospitalizations (IQR 1–6) within the first year after the index admission. Respiratory and infection/sepsis were the main causes of re-hospitalization. Eighty-five (28%) patients were re-hospitalized within 30 days of the index admission, and 207 (68%) were re-hospitalized within 90 days of the index admission (Supplementary Table 1).
Primary Outcome
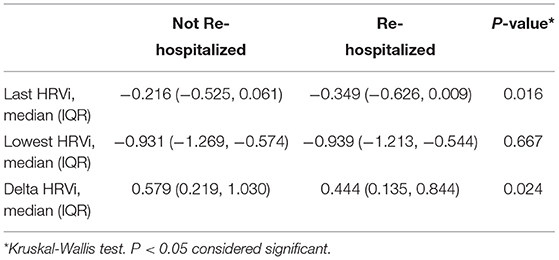
The median last HRVi measurement during the index admission was significantly lower among patients who were re-hospitalized compared to those who were not (p = 0.02, Table 2). The median lowest HRVi measurement during the index admission was not significantly different between patients who were re-hospitalized compared to those who were not (p = 0.67), but patients who were re-hospitalized showed a smaller improvement in their delta HRVi (p = 0.02, Table 2).
After controlling for potential confounders (including age, PRISM III, immunocompromised state, and multi-comorbidity) using logistic regression, the median last and delta HRVi measurements remained significantly associated with re-hospitalization, with higher HRVi measurements associated with a lower adjusted odds ratio of re-hospitalization. The lowest HRVi measurement was not associated with re-hospitalization in the unadjusted or adjusted models (Table 3).
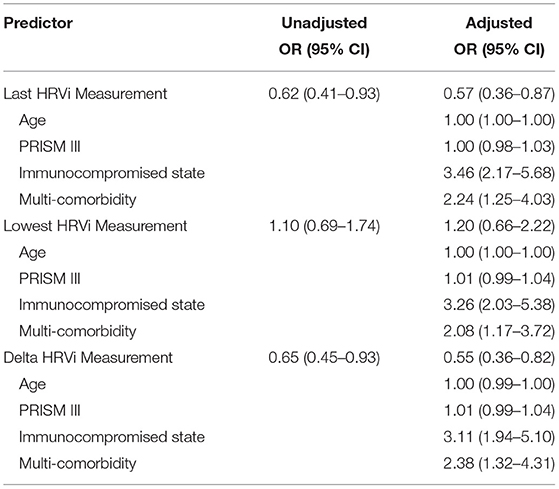
Table 3. Unadjusted and adjusted odds ratios (OR) for re-hospitalizations within 1 year after septic shock admission based on age-normalized HRVi.
Secondary Outcome
The total number of re-hospitalizations in the year after the index admission were analyzed as count data. The median last HRVi and delta HRVi measurements were significantly associated with the total number of re-hospitalizations after adjusting for age, PRISM III, immunocompromised state, and multi-comorbidity using Poisson regression, with higher HRVi measurements associated with a lower adjusted incidence rate ratio of a re-hospitalization. The lowest HRVi measurement was also associated with the number of re-hospitalizations with a higher value associated with increased likelihood of more re-hospitalizations (Table 4).
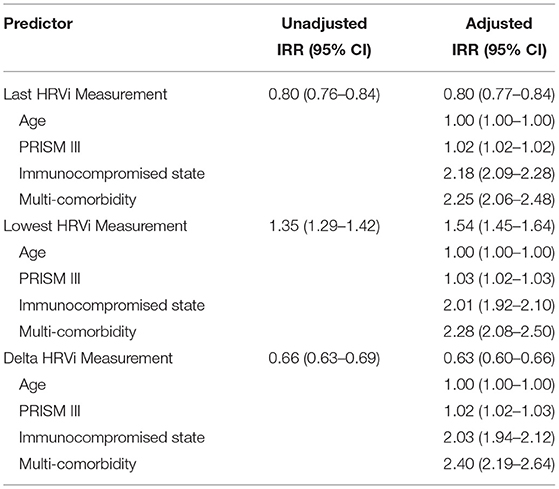
Table 4. Unadjusted and adjusted incidence rate ratios (IRR) for the number of re-hospitalizations within 1 year after septic shock admission based on age-normalized HRVi.
Sensitivity Analysis
In a sensitivity analysis of patients re-hospitalized within 30 or 90 days of the index admission, the delta HRVi remained significantly associated with re-hospitalization, with a higher value associated with a lower likelihood of readmission (p < 0.001). The median last HRVi was not significantly associated with re-hospitalization at 30 days, while the median lowest HRVi had positive, statistically significant association with re-hospitalization at 30 and 90 days (Supplementary Tables 2, 3).
Discussion
In this study we demonstrate that autonomic nervous system dysfunction (ANSD) measured using age-normalized integer heart rate variability (HRVi) is independently associated with re-hospitalization in pediatric septic shock survivors. Specifically, the delta HRVi between the day with the lowest HRVi and the last day of PICU during the index hospitalization was significantly associated with re-hospitalization within 1 year, as well as within 30 and 90 days in sensitivity analysis, with a smaller recovery in the HRVi trajectory associated with higher likelihood of re-hospitalization. This association remained significant after controlling for several potential confounders, including age, PRISM III score, immunocompromised state, and multi-comorbidity. The absolute HRVi mean values on the lowest and last day of PICU stay were inconsistently associated with the outcome across the primary endpoint of readmissions at 1 year and the sensitivity analyses at 30 and 90 days. This suggests that the relative trajectory of recovery of the HRVi at the patient level was more predictive of re-hospitalization than the absolute values at a population level. Furthermore, although commonly considered confounders of poor outcomes, the severity of illness on admission based on PRISM III, patient age, duration of mechanical ventilation and vasoactive-inotrope days did not differ between patients requiring re-hospitalization and those who did not. This lack of association between common physiologic and clinical variables during the index admission and our outcome of interest (re-hospitalizations) makes the independent association between the recovery trajectory of HRVi during PICU admission and re-hospitalization all the more notable.
Readmissions after sepsis are common in children. Our rates of re-hospitalization of 66% and hospital readmission of 58% within a year after septic shock are consistent with prior studies. In a state-wide analysis of pediatric severe sepsis survivors, 47% of children were readmitted within 3 months and 85% of these readmissions were considered urgent or emergent (21). In another multicenter observational cohort study, almost 20% of severe sepsis survivors were readmitted within 30 days, and 30% within 90 days (22). Among children with severe sepsis, those with oncologic, hematologic, immunologic, and neurologic comorbidities were at higher risk of readmission (21). Additionally, children with age <1 year and with cardiovascular, bloodstream and genitourinary infections were at higher risk of readmission (21). In our population, 57% of pediatric septic shock survivors were re-hospitalized with recurrent infection, respiratory illness, or hematologic/oncologic diagnoses.
Health-related quality of life (HRQL) among pediatric sepsis survivors frequently declines, with 17–35% of sepsis survivors demonstrating more disability at discharge when compared to admission (2, 6). This decline includes functional and neuropsychological disability (23), and in some patients can persist for years (24). A retrospective national cohort study of over 9,000 pediatric patients examined potentially preventable readmissions following hospitalization for severe sepsis and other acute care conditions. They found that preventable readmissions were statistically higher following a severe sepsis admission when compared to other acute care admissions. Additionally, that study found 30-day readmissions were lower in patients with no comorbidities (5.9%) when compared to patients with co-morbidities (26%) (22).
While pre-existing comorbidities have been shown to be a driver of readmission following sepsis, our data support that other measures, such as HRVi, are worth considering. In our study, delta HRVi remained significantly associated with re-hospitalization even after controlling for multi-comorbidity and across sensitivity analyses. HRVi is a continuous, non-invasive physiologic marker of ANS function and can be measured in virtually all critically ill patients with high-frequency data collected from the bedside monitor. HRV has been shown to be predictive of in-hospital mortality in adults with sepsis (25) and in critically ill children (11). Our data now suggest that it can also be used to predict re-hospitalization in pediatric septic shock survivors. Real-time measurement of HRVi throughout the admission, and at discharge, may improve identification of patients who are at highest risk of re-hospitalization and facilitate the implementation of strategies to minimize this risk. Furthermore, because HRVi requires only a lightweight implementation, it is conceivable that this physiologic marker could be monitored in septic shock survivors after they are discharged from the hospital using wearable sensors like smart watches.
Our study has several strengths and limitations. First, this was a single center study and therefore may have limited generalizability. However, we present data on a relatively large cohort of septic shock survivors with available high-frequency physiologic bedside monitor data. Second, our definition of re-hospitalization only included patients who were re-hospitalized to our institution. It is possible that some patients were readmitted to other institutions. Third, we calculated the HRVi using high-frequency integer heart rate data, which is a lightweight proxy of HRV. While this method may be more generalizable than the derivation of HRV from R-R intervals in the electrocardiogram waveform, which is more computationally intense, HRVi may not fully capture the physiologic complexity of the ANS. Of note, we were unable to examine medications or specific conditions that may directly affect the autonomic nervous system. Finally, there may have been bedside monitor data losses during the study period, most commonly due to server downtimes without back-ups. We do not believe these data losses resulted in systematic bias in the study population since they occurred at random.
In conclusion, our data demonstrate a significant association between HRVi recovery and re-hospitalization among survivors of pediatric septic shock. This continuous, non-invasive physiologic marker of ANS function may be useful in the derivation of prediction models to stratify and mitigate the risk of re-hospitalization in survivors of pediatric septic shock.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Ann & Robert H. Lurie Children's Hospital of Chicago Institutional Review Board. Written informed consent from the participants' legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author Contributions
CB and LS-P designed the study and performed the data analysis. All authors made substantial contributions to drafting and final approval of the manuscript and agree to be accountable for the content of the work.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2021.745844/full#supplementary-material
Abbreviations
ANS, autonomic nervous system; ANSD, autonomic nervous system dysfunction; HRQL, health-related quality of life; HRV, heart rate variability; HRVi, integer heart rate variability; PRISM, Pediatric Risk of Mortality.
References
1. Weiss SL, Peters MJ, Alhazzani W, Agus MSD, Flori HR, Inwald DP, et al. Surviving sepsis campaign international guidelines for the management of septic shock and sepsis-associated organ dysfunction in children. Pediatr Crit Care Med. (2020) 21:e52–106. doi: 10.1097/PCC.0000000000002444
2. Weiss SL, Fitzgerald JC, Pappachan J, Wheeler D, Jaramillo-Bustamante JC, Salloo A, et al. Global epidemiology of pediatric severe sepsis: the sepsis prevalence, outcomes, and therapies study. Am J Respir Crit Care Med. (2015) 191:1147–57. doi: 10.1164/rccm.201412-2323OC
3. Fleischmann-Struzek C, Goldfarb DM, Schlattmann P, Schlapbach LJ, Reinhart K, Kissoon N. The global burden of paediatric and neonatal sepsis: a systematic review. Lancet Respir Med. (2018) 6:223–30. doi: 10.1016/S2213-2600(18)30063-8
4. Zimmerman JJ, Banks R, Berg RA, Zuppa A, Newth CJ, Wessel D, et al. Trajectory of mortality and health-related quality of life morbidity following community-acquired pediatric septic shock. Crit Care Med. (2020) 48:329–37. doi: 10.1097/CCM.0000000000004123
5. Meert KL, Reeder R, Maddux AB, Banks R, Berg RA, Zuppa A, et al. Trajectories and risk factors for altered physical and psychosocial health-related quality of life after pediatric community-acquired septic shock. Pediatr Crit Care Med. (2020) 21:869–78. doi: 10.1097/PCC.0000000000002374
6. Farris RW, Weiss NS, Zimmerman JJ. Functional outcomes in pediatric severe sepsis: further analysis of the researching severe sepsis and organ dysfunction in children: a global perspective trial. Pediatr Crit Care Med. (2013) 14:835–42. doi: 10.1097/PCC.0b013e3182a551c8
7. Watson RS, Carcillo JA, Linde-Zwirble WT, Clermont G, Lidicker J, Angus DC. The epidemiology of severe sepsis in children in the United States. Am J Respir Crit Care Med. (2003) 167:695–701. doi: 10.1164/rccm.200207-682OC
8. Watson RS, Carcillo JA. Scope and epidemiology of pediatric sepsis. Pediatr Crit Care Med. (2005) 6(3 Suppl.):S3–5. doi: 10.1097/01.PCC.0000161289.22464.C3
9. Zimmerman JJ, Banks R, Berg RA, Zuppa A, Newth CJ, Wessel D, et al. Critical illness factors associated with long-term mortality and health-related quality of life morbidity following community-acquired pediatric septic shock. Crit Care Med. (2020) 48:319–28. doi: 10.1097/CCM.0000000000004122
10. Wong HR, Reeder RW, Banks R, Berg RA, Meert KL, Hall MW, et al. Biomarkers for estimating risk of hospital mortality and long-term quality-of-life morbidity after surviving pediatric septic shock: a secondary analysis of the life after pediatric sepsis evaluation investigation. Pediatr Crit Care Med. (2021) 22:8–15. doi: 10.1097/PCC.0000000000002572
11. Badke CM, Marsillio LE, Carroll MS, Weese-Mayer DE, Sanchez-Pinto LN. Development of a heart rate variability risk score to predict organ dysfunction and death in critically ill children. Pediatr Crit Care Med. (2021) 22:e437–47. doi: 10.1097/PCC.0000000000002707
12. Schmidt H, Muller-Werdan U, Hoffmann T, Francis DP, Piepoli MF, Rauchhaus M, et al. Autonomic dysfunction predicts mortality in patients with multiple organ dysfunction syndrome of different age groups. Crit Care Med. (2005) 33:1994–2002. doi: 10.1097/01.CCM.0000178181.91250.99
13. Badke CM, Marsillio LE, Weese-Mayer DE, Sanchez-Pinto LN. Autonomic nervous system dysfunction in pediatric sepsis. Front Pediatr. (2018) 6:280. doi: 10.3389/fped.2018.00280
14. Dunser MW, Hasibeder WR. Sympathetic overstimulation during critical illness: adverse effects of adrenergic stress. J Intensive Care Med. (2009) 24:293–316. doi: 10.1177/0885066609340519
15. Ellenby MS, McNames J, Lai S, McDonald BA, Krieger D, Sclabassi RJ, et al. Uncoupling and recoupling of autonomic regulation of the heart beat in pediatric septic shock. Shock. (2001) 16:274–7. doi: 10.1097/00024382-200116040-00007
16. Goldstein B, Fiser DH, Kelly MM, Mickelsen D, Ruttimann U, Pollack MM. Decomplexification in critical illness and injury: relationship between heart rate variability, severity of illness, and outcome. Crit Care Med. (1998) 26:352–7. doi: 10.1097/00003246-199802000-00040
17. Papaioannou VE, Maglaveras N, Houvarda I, Antoniadou E, Vretzakis G. Investigation of altered heart rate variability, nonlinear properties of heart rate signals, and organ dysfunction longitudinally over time in intensive care unit patients. J Crit Care. (2006) 21:95–103. doi: 10.1016/j.jcrc.2005.12.007
18. Pollack MM, Holubkov R, Funai T, Dean JM, Berger JT, Wessel DL, et al. The pediatric risk of mortality score: update 2015. Pediatr Crit Care Med. (2016) 17:2–9. doi: 10.1097/PCC.0000000000000558
19. Feudtner C, Feinstein JA, Zhong W, Hall M, Dai D. Pediatric complex chronic conditions classification system version 2: updated for ICD-10 and complex medical technology dependence and transplantation. BMC Pediatr. (2014) 14:199. doi: 10.1186/1471-2431-14-199
20. Gang Y, Malik M. Heart rate variability in critical care medicine. Curr Opin Crit Care. (2002) 8:371–5. doi: 10.1097/00075198-200210000-00002
21. Czaja AS, Zimmerman JJ, Nathens AB. Readmission and late mortality after pediatric severe sepsis. Pediatrics. (2009) 123:849–57. doi: 10.1542/peds.2008-0856
22. Carlton EF, Kohne JG, Shankar-Hari M, Prescott HC. Readmission diagnoses after pediatric severe sepsis hospitalization. Crit Care Med. (2019) 47:583–90. doi: 10.1097/CCM.0000000000003646
23. Syngal P, Giuliano JS Jr. Health-related quality of life after pediatric severe sepsis. Healthcare. (2018) 6:113. doi: 10.3390/healthcare6030113
24. Buysse CM, Vermunt LC, Raat H, Hazelzet JA, Hop WC, Utens EM, et al. Surviving meningococcal septic shock in childhood: long-term overall outcome and the effect on health-related quality of life. Crit Care. (2010) 14:R124. doi: 10.1186/cc9087
25. Prabhakar SM, Tagami T, Liu N, Samsudin MI, Ng JCJ, Koh ZX, et al. Combining quick sequential organ failure assessment score with heart rate variability may improve predictive ability for mortality in septic patients at the emergency department. PLoS ONE. (2019) 14:e0213445. doi: 10.1371/journal.pone.0213445
Keywords: critical care, pediatrics, sepsis, autonomic nervous system, outcomes
Citation: Badke CM, Swigart L, Carroll MS, Weese-Mayer DE and Sanchez-Pinto LN (2022) Autonomic Nervous System Dysfunction Is Associated With Re-hospitalization in Pediatric Septic Shock Survivors. Front. Pediatr. 9:745844. doi: 10.3389/fped.2021.745844
Received: 22 July 2021; Accepted: 09 December 2021;
Published: 04 January 2022.
Edited by:
Luregn J. Schlapbach, University Children's Hospital Zurich, SwitzerlandReviewed by:
Qalab Abbas, Aga Khan University, PakistanThomas Vincent Brogan, Seattle Children's Hospital, United States
Copyright © 2022 Badke, Swigart, Carroll, Weese-Mayer and Sanchez-Pinto. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Colleen M. Badke, Y2JhZGtlQGx1cmllY2hpbGRyZW5zLm9yZw==
 Colleen M. Badke
Colleen M. Badke Lindsey Swigart
Lindsey Swigart Michael S. Carroll2,4
Michael S. Carroll2,4 Debra E. Weese-Mayer
Debra E. Weese-Mayer