- 1Faculty of Medicine, University of Ottawa, Ottawa, ON, Canada
- 2Department of Pediatrics, University of Ottawa, Children's Hospital of Eastern Ontario, Ottawa, ON, Canada
- 3Neonatal Intensive Care Unit, Children's Hospital of Eastern Ontario, Ottawa, ON, Canada
- 4Parents of Preemies Association, Ottawa, ON, Canada
- 5Health Care Systems Division, Health Canada, Ottawa, ON, Canada
- 6Telfer School of Management, University of Ottawa, Ottawa, ON, Canada
Background: Parental involvement in their newborn's neonatal intensive care reduces stress and helps with the parent-child attachment, transition to home, and future development. However, parents' perspectives are not often sought or considered when adapting family-centered care in neonatal intensive care units (NICUs).
Aim: To identify what parents believe helps or hinders their involvement in their newborn's care when admitted to our Level 3B NICU.
Methods: Between August and October 2018, nine mothers and one father were interviewed during three 60- to 90-min audiotaped focus groups using a semi-structured interview tool. From the content analysis of the verbatims, three reviewers identified key themes that affected how involved parents could be in their newborn's care.
Results: Parents provided examples of factors that facilitated or restricted their involvement. The analysis identified themes: (1) parent-staff interactions, (2) supportive/trustworthy healthcare professionals, (3) consistency in care and caring staff, (4) family, couple, and peer support, (5) newborn status, (6) resources and education for parents, (7) the NICU environment, and (8) academic and research participation.
Conclusion: We identified a conceptual framework to allow our NICU team to prioritize working strategies to strengthen parental involvement in newborn care. In addition to implementing ways to involve parents, we need to address parents' satisfaction with their participation. These findings may help other investigators explore parents' expectations toward their NICU experience.
Introduction
Recent advances in neonatal medicine and medical technology have made neonatal intensive care more accessible to fragile newborns, resulting in increased survival rates and lower limits of gestational age viability (1). But with all the monitoring, machines and equipment surrounding a newborn's fighting for survival, parents often feel lost and frightened and experience extreme stress and anxiety (2, 3), which can affect parent-infant attachments, hospital-to-home transition, and long-term development. Parental involvement with a newborn's day-to-day care in the neonatal intensive care unit (NICU) can reduce the anxieties, strengthen the bonds and ease the transition (4–6).
Family-centered care is a family-professional partnership developed to bring a more holistic and interdisciplinary approach to the care of newborns (3, 7). The newest models emphasize staff and family partnerships to better support infant and parent/infant outcomes (8). Shared governance allows for partnership with parents in co-designing a model of care that places the family unit at the center (9). Although principles of family-centered/integrated care models have been described (10), physical setup, workflow, culture characteristics, and staff experience vary considerably between NICUs (11). So each NICU must adapt their family-centered care models to fit parent's needs, considering the local context, culture, and staff experience, to successfully implement changes (11).
Although the Children's Hospital of Eastern Ontario's (CHEO) Level 3B regional NICU includes family-centered care practices, our internal patients' satisfaction surveys and unit performances to kangaroo care and other transitions, including discharge, showed challenges to parent participation in the care on their newborn during their NICU stay (12). From these observations, we identified the need to better incorporate parents' input to strengthen partnerships according to the model of shared governance (13). For this study, we explored parental perspectives to identify factors that help or hinder their involvement in their newborns' care. The research ethics boards of the CHEO Research Institute (CHEO REB# 18/33X) and the Ottawa Health Sciences Network (OHRI# 20180261-01H) approved the study.
Materials and Methods
Study Design and Setting
We adopted a qualitative descriptive phenomenological framework to explore how individuals interpret an experience (14) to better understand parents' participation in their newborn's care. The recommended guideline ‘Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups' has been used to report this study (15). We conducted this study in a 16-bed surgical tertiary care Level 3B NICU. The clinical care team includes ~17 registered nurses, 10 respiratory therapists, one social worker, one dietician, one pharmacist, and 13 neonatologists.
Participants
We used purposive sampling to recruit parents of high-risk neonates recently discharged from our NICU. The criteria to define high-risk neonates were: (1) infant born ≤29 weeks of gestational age; (2) infant with intraventricular hemorrhage grade III-IV, neonatal stroke and any other type of neonatal encephalopathy that present with seizures; (3) infant with a congenital anomaly in central nervous, respiratory, cardiac and/or digestive systems or genetic syndrome not yet identified who were hospitalized for at least 7 days, and/or (4) infant with hypoxic ischemic encephalopathy requiring therapeutic hypothermia hospitalized for at least 14 days.
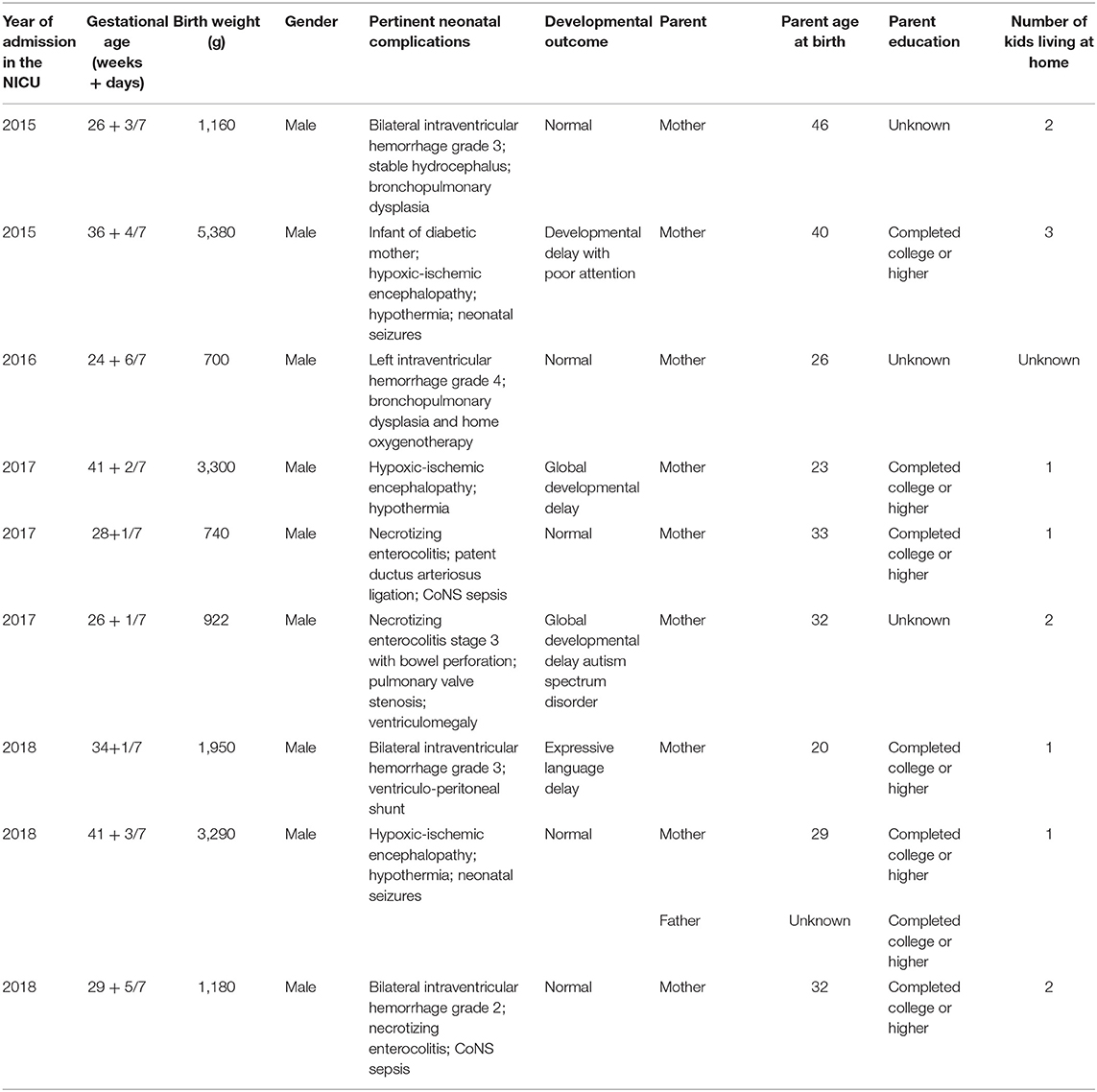
The study design excluded any parents who could not speak English or any family in which parents present in the NICU were not deemed long-standing caregivers (e.g., adoption, foster care). Following pre-identification of the families according to the inclusion criteria and after being invited by the neonatal follow-up clinic nurse, our research assistant approached 21 parents for consent between June and September 2018. Although 15 parents initially consented, nine mothers and one father ultimately participated. The other five parents could not make it for scheduling conflict. Table 1 describes the demographic characteristics of their high-risk newborns, who were admitted between 2015 and 2018, and their parents.
Data Collection
Between August and October 2018, three exploratory meetings with the parents—in groups of two, three, and five—were held at the hospital by one of the principal investigators, a physician with a master's degree (TD) and a researcher in healthcare system evaluation with doctorate degree (MM). Some parents might have interacted with one of the interviewers (TD) prior to the study, being a physician and medical director of the NICU. Interviewers used a semi-structured interview guide (Appendix 1) developed by two authors (TD, MM) who have substantial experience with qualitative research methods and interviews as well as extensive knowledge of NICU environment. We did not include an external review of the topic guide, considering the risk for bias as minimal. However, two principal investigators (TD, MM) revised the questions after each focus group to increase clarity and comprehensiveness and, to reflect the previous focus group's findings.
We asked the parents to identify and describe circumstances and conditions that facilitated or hindered their involvement in their newborn's care. We focused on specific events: medical rounds; critical situations; care of the newborn, including kangaroo care; breastfeeding; transition to home, and decision-making situations. Questions were open-ended and no examples were provided to parents, in order to explore their perspective without directing them toward a specific theme. Although small focus group facilitated symmetrical parents' participation, attention was given to silent parents to encourage them to share their opinion on each subject. To make parents feel more comfortable, they were given the opportunity to introduce themselves and their child at the beginning of the focus group. All the interviews were recorded and transcribed.
Data Analysis
Two independent reviewers (AF, TD) used an inductive and constant comparisons process (16) to perform a qualitative content analysis of the first focus group interview involving five parents. One reviewer (AF) then conducted content analysis of the following two focus groups verbatim. Themes were designated as “facilitators” or “challenges” to parents' involvement. The two reviewers (AF, TD) met twice for a total of 4 h to review the coding and related transcripts and to discuss themes and concepts to create a framework. We counted the number of times parents mentioned examples to provide a relative weight between the themes. As a counter-coding strategy to ensure the validity of the results, the two coders met with a third author (EF) to review the themes and the preliminary classifications. Modifications were made as needed until agreement was reached. We used tables on Microsoft Word to support the analysis and organization of the data.
Results
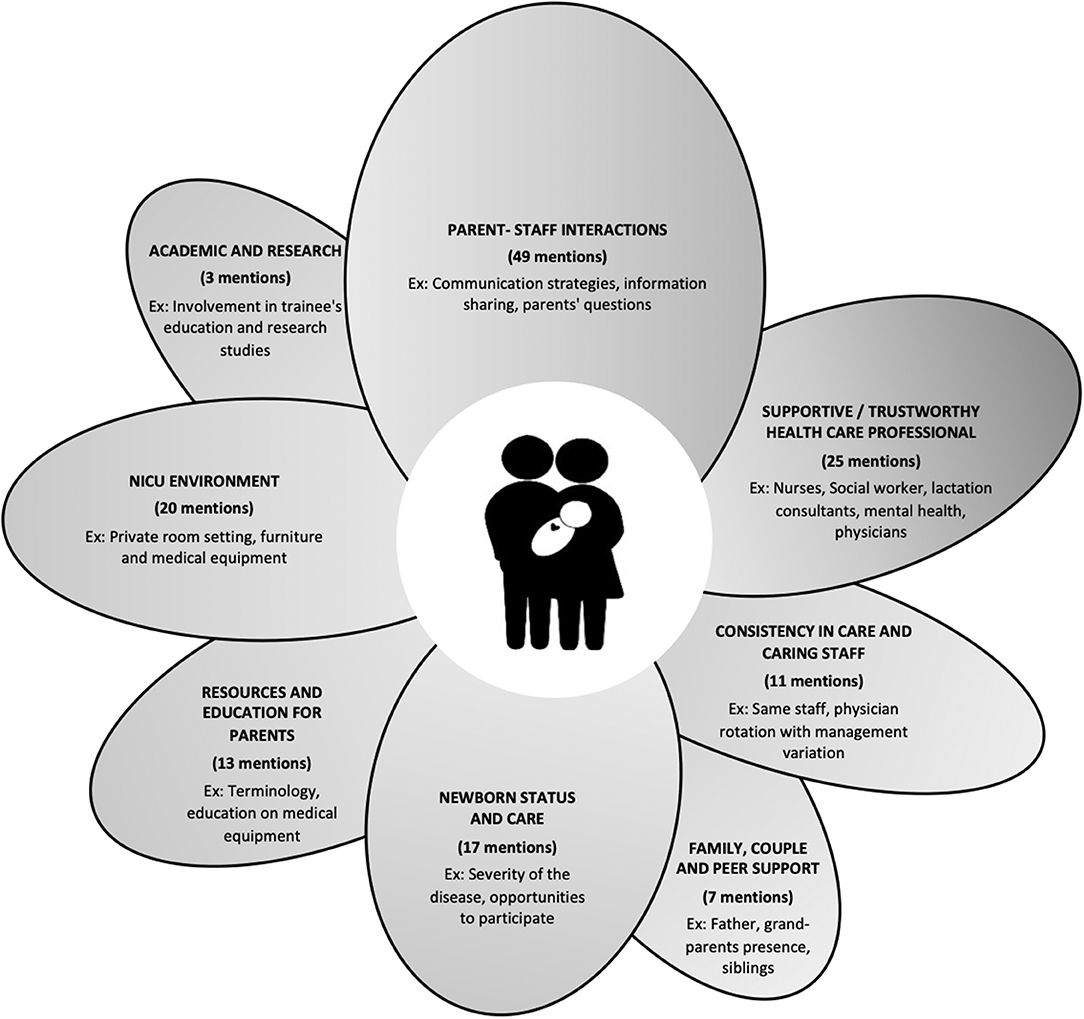
Eight themes were derived from the interviews, outlining factors that influenced parental involvement in their newborn's care during their experience in our NICU. These themes, outlined in Figure 1, include: parent-staff interactions; consistency in care and caring staff; supportive/trustworthy healthcare professional; newborn status and care; family, couple and peer support; resources and education for parents; NICU environment, and participation in academic curriculum and research studies. Tables 2–9 explain the themes and underlying sub-themes with paraphrased comments from the parents. Within the tables, we established each paraphrased comment as either a “facilitator” in white or a “challenge” in gray.
During the interviews and when reading the verbatim, it became obvious that parents weighted some elements more than others. Figure 1 describes how many times each theme was mentioned by parents during the interviews. For example, “parents-staff interactions” was clearly an important element, being mentioned 49 times by parents, while “academic and research participation” was only mentioned three times.
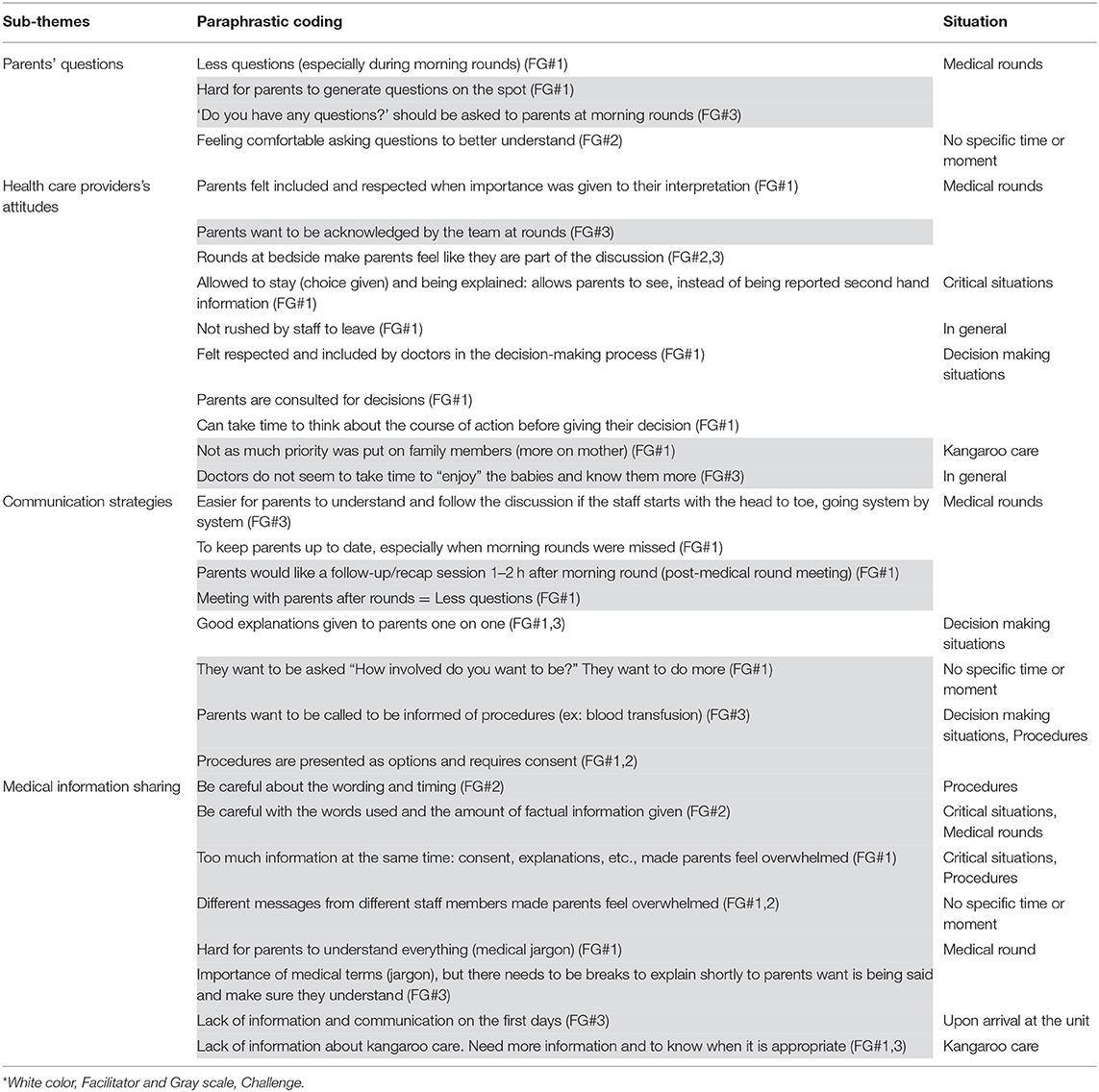
Parent-Staff Interactions (Table 2: 49 Mentions)
Parent-staff interactions clearly influence parental involvement in the NICU care of their newborns. Parents noted the importance of the interactions and communication strategies with the nurses, physicians and social workers, saying they should be considered in daily care, acknowledged by the team and provided time to think when a course of action has to be decided. Morning rounds are a crucial moment for parents as they receive updates about their newborn and an opportunity to ask questions.
“It's very easy if they talked at the bedside of the baby, then you're obviously part of the conversation, and they always asked me at the end of their discussion, they asked me if I had any questions and concerns.” (FG#2)
This demonstrates the importance of staff and physicians' attitudes, the type of communication strategies used, and the need for sharing medical information, allowing questions and asking for consent about the procedures used on the newborns.
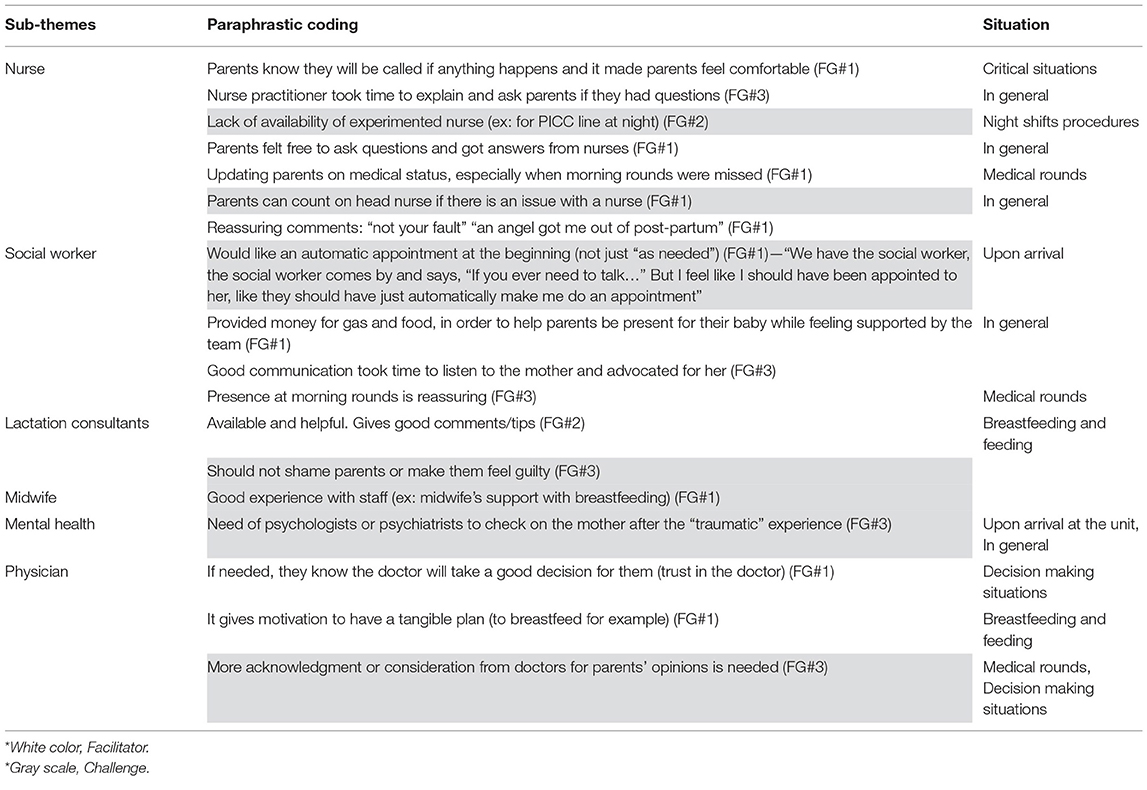
Supportive/Trustworthy Healthcare Professional (Table 3: 25 Mentions)
Parents' description of what influenced their participation in their infant's care reflected staff attitudes to making them feel comfortable.
“One nurse, she snapped me out of my postpartum. Just as — you know, no matter what anybody was saying to me, it was just — it was constant, I was blaming myself. But her, she was like — to me, she was like my angel. She came in, she's like, “No, that's enough. You're doing perfect, that's more than enough.” (FG#1)
Nurses' availability, openness to questions and experience influenced parents' involvement as they felt comfortable asking questions. They could rely on nurses for explanations, updated information and reassurance. In addition, parents identified the lack of experienced nurses on night shifts as a barrier to support.
Parents trusted physicians in making good decisions during critical situations. On the other hand, they would appreciate more consideration from physicians for parents' opinions. “After I got into an argument with one of the doctors. After I had told him like, ‘No, I do not want Puramino or lipid or formula.' He's like, ‘Okay, fine. Then what's going to happen after this then?' I'm like, ‘I don't know what's going to happen after this. Right now, I don't want him to get NEC again.' for, like, the fifth time.” (FG#3)
Social workers were identified as valued in many ways, from helping understand the financial aspects of having a preemie to being present during morning rounds. The social worker was felt to be reassuring, enabling good communication and providing advocacy.
“So I found CHEOs family-centered approach, and the […] social worker was making sure we were okay as a couple and as a family. That made us stronger than ever.” (FG#3)
Parents said they would appreciate an automatic appointment with a social worker at the beginning of their stay instead of only if needed.
Lactation support was also seen as beneficial. One mother mentioned that additional access to mental health support from a psychologist or psychiatrist would have been helpful to cope with this traumatic experience.
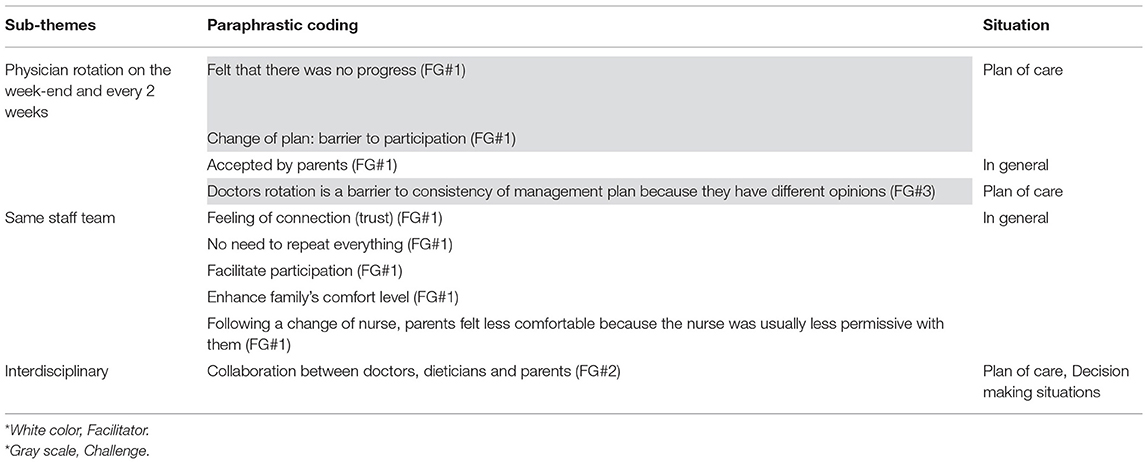
Consistency in Care and Caring Staff (Table 4: 11 Mentions)
Consistency in care is an important concept for the parents. In fact, parents preferred to have the same staff to better participate in the care and be comfortable with and trust the care team. The physician rotation on weekends and after every 2 weeks was perceived as a barrier to the parents' involvement. They noted little to no progress over the weekend and perceived significative changes in care plans with physician rotation, which made their involvement more difficult.
“If the same physician was in for two weeks, you get momentum going and you would kind of be — you'd have a plan, more of a long-term plan. When someone would come in on the weekend, sometimes they would totally switch gears on you. And then, whoever was there would come back the next week, it would sometimes shift again.” (FG#3)
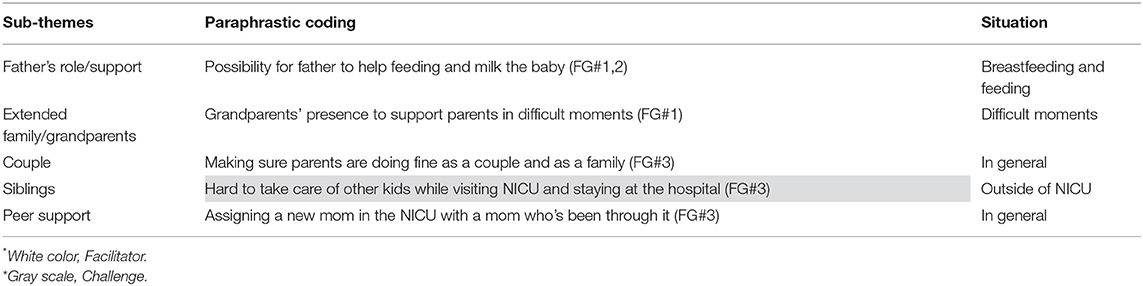
Family, Couple, and Peer Support (Table 5: 7 Mentions)
The presence of family members is significant. The parents noted the importance of their own wellness and indicated the difficulty in caring for the newborn's siblings as well as visiting the NICU, resulting in pressures that can damage the couple's relationship.
“When your husband and yourself […] are under a time of stress, you can say the nastiest things to each other, and relationships can falter away.” (FG#3)
Family members' presence can play a crucial role in supporting the parents' involvement with the newborn's care.
They also mentioned the need for peer support and the opportunity of a new mother to be paired with another parent whose newborn was admitted to the NICU.
“Peer support, so just like assigning one mom with, like, a new mom in the NICU with a mom who's been through it.” (FG#3)
Newborn Status and Care (Table 6: 17 Mentions)
Parents want to be taught about various care procedures so they can gain independence and confidence leading to the infant's eventual discharge. Providing opportunities to breastfeed and have skin-to-skin contact could improve parental involvement if associated with adequate teaching support at the bedside. Skin-to-skin contact is “[…] very important. It just encourages the mother to attach.” (FG#2)
Resources and Education for Parents (Table 7: 13 Mentions)
Parents would benefit from a variety of targeted resources. For example, they said a course or resources for medical terminology, basics of the NICU, and an informative session on their first day at the NICU would be helpful.
“There should be some sort of way to present to parents, this is the NICU, this is what you can expect kind of thing, like, just one information session. Parents should be invited to one information session.” (FG#3)
Education about the medical equipment (e.g., monitors, nasogastric tubes, etc.) and medications should also be offered to build their confidence. Parents wished for more hands-on experiences to gain confidence in caring for their newborn. It allows parents to feel closer to their newborn and facilitates their discharge from the unit because they feel more ready.
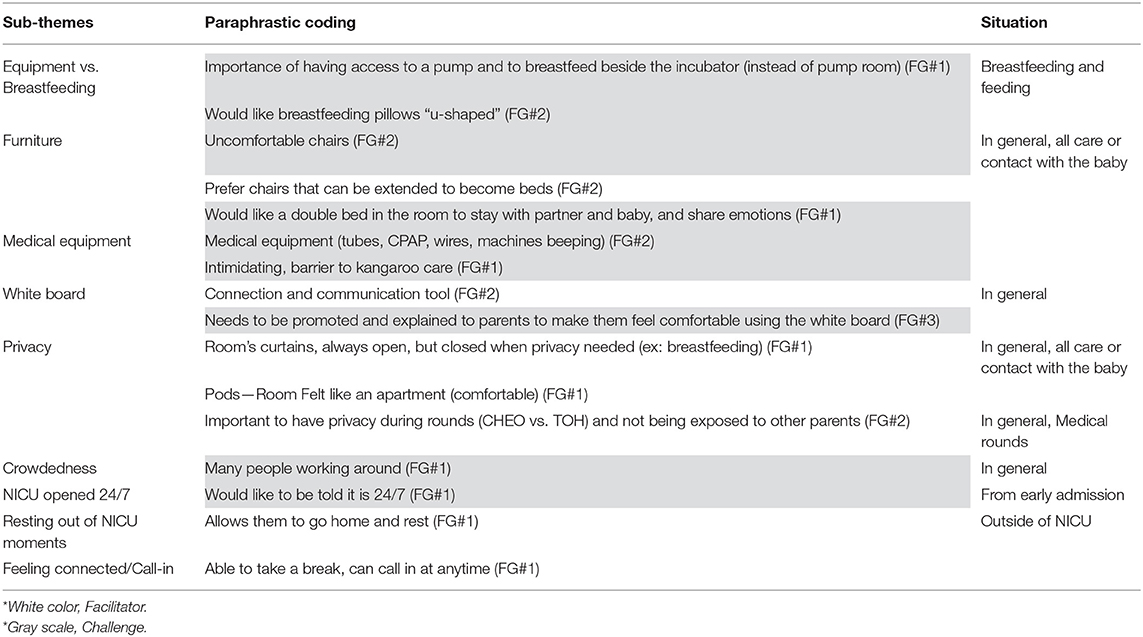
NICU Environment (Table 8: 20 Mentions)
Parents appreciated comfortable chairs that extend to become beds and, as privacy is an important factor, curtains and a quieter environment. They suggested breastfeeding could be improved by u-shaped pillows and good accessibility to breastfeeding pumps beside the incubator. Parents need to be comfortable in order to better participate in the care.
“The chairs are horrible, and the nurses were trying to put a pillow and make me comfortable. […] So as much as I wanted to stay there all day long, I was not comfortable.” (FG#2)
White boards in the rooms where parents and staff can exchange messages facilitate communication and are appreciated as a connection tool but need to be promoted and explained to make the parents feel comfortable using them.
They appreciated that they could call the unit at any time, saying it let them take breaks when needed, or to go home and rest, and still feel connected to their newborns at all times.
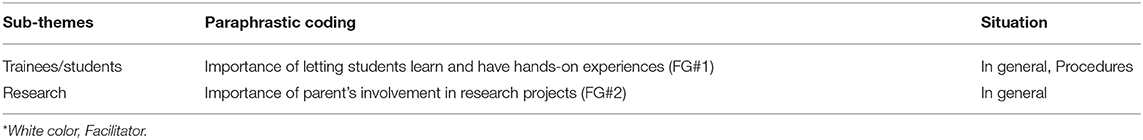
Academic and Research Participation (Table 9: 3 Mentions)
Although less often mentioned, some parents brought up the importance of being able to decide whether to be involved in research projects, with some saying it is gratifying to participate in the development of the next generation of treatments to help future families and fragile newborns. They also appreciated the chance to participate in the education of future staff by allowing students to have hands-on experiences. It gave parents the sense of being “part of the medical team or part of the healthcare team.” (FG#2)
Discussion
From parents' testimony about their involvement in the care of newborns admitted in the NICU, we identified eight themes that influenced their satisfaction. Parent-staff interactions were significant in developing trust. Examples of the situations discussed range from admission to the NICU, medical rounds, breastfeeding, kangaroo care, decision-making processes and transition to home. The wide variation of examples given by parents demonstrates the need for flexibility when implementing a framework within an NICU to facilitate parents' involvement in the care of their newborn.
Research on family-centered care on pediatric wards happened well before Harrison published, in 1993, principles for NICUs. Back then, allowing parents to have a say, negotiating with them, involving them in decision-making and overall parent involvement was perceived as complex (17). There is still resistance from NICU staff about parents' participation in the decision-making process and care of the newborns (18) but we believe use of the themes identified in our study to educate our staff will help alleviate resistance. Studies have shown that the resistance may be related to the lack of knowledge about parents' perceptions about their involvement in newborn care (19).
The importance for the healthcare professional to understand and believe in the philosophy of improving parental participation is not new. Early in the 1990s, Palmer et al. reported that the success of parental involvement in their child's care was conditional on the parents' and staff's attitudes and willingness to work together (19). The authors described the importance of good understanding of parental role in the hospital and the importance of the emotional support to families. Although their recommendations were aimed at pediatric wards, the results of our study would support similar approaches for NICUs. For example, the stress on a couple of having a newborn in intensive care can result in lack of intimacy and communication, depression, anxiety and increased risk of marital dissolution (20). The team should acknowledge possible adjustments needed for the couple to help in the care of their newborn. Peer-to-peer support was also mentioned by our participants. This support program foster feelings of safety and comfort (21) and encourage them to better advocate for their newborns (22).
More than 25 years ago, Harrison stated the importance of an open and honest communication between parents and professionals (17). Our findings on the importance of the parent-staff interactions are aligned with this description. Lopez-Maestro et al. (6) described a framework to improve parental involvement and parent-infant interactions, called “infant and family-centered developmental care.” It identified seven themes: 24-h parental access; psychological support for parents; pain prevention, assessment and treatment; supportive environment; postural support; skin-to-skin contact; sleep protection, and breastfeeding and lactation support. Although our classifications are different, we found many similarities with their findings. The difference is explained in part by the higher level of categorizations in our study. One of the major differences we found is the prime importance of parent-staff interactions. Enabling parental participation is largely influenced by the nurse acknowledgment of the parents as the main caregiver and awareness of the benefits of family-centered care philosophy and skin-to-skin care (11). The healthcare team's attitude may be influenced by unit policies about inviting parents to medical rounds (23). Our category about availability and supportive staff reflects that important factor. Family-centered care should be viewed as a philosophy aiming to improve parental participation (24, 25). The acknowledgment of this view is a first step to modifying parent-staff interactions to positively influence parents' involvement in the care of newborns. Although themes could have been amalgamated, such as “parents-staff interaction” and “Supportive/trustworthy healthcare professional,” we identified these themes based on their pertinence for elements to guide future improvements in developing our family-centered care model.
Some NICU family-centered care approaches are developed from healthcare professionals' opinion agreed or adapted by selected parents (10). Such models could have been implemented in our unit, but some of the proposed strategies—such as giving report, basic charting and maintaining a diary or providing focused medical care—are professionally goal-oriented and may not be appropriate for all parents (10). More recently, Skene et al. demonstrated the importance of understanding the unique context of the NICU to support cultural changes (11). In accordance with our results, they identified similar areas of changes, including providing family support and educational programs.
Our study on the perspective of the parents will support change in the philosophy and creation of educational programs to improve attitudes toward parents' participation in newborn care. We will use the examples brought by the parents to guide discussions during interviews with NICU staff. By exploring parental testimony and identifying strategies, we will facilitate parental participation in the care of newborns in different situations.
As Skene et al. mentioned, we needed to better understand the unique context of our NICU before discussing family-centered care with our staff (11). Although some of the themes we found are potentially specific to our unique environment, the higher level of abstraction of our findings into the themes identified is broad enough to be adapted to other NICUs. In addition, the situations identified by parents—early admission in the NICU, medical rounds, critical situations, decisions making and planning of care, breastfeeding, skin-to-skin, kangaroo care to transition to home—are similar between NICUs, which could facilitate the use of our findings for their benefit (26).
Although the impact of parents' participation in the care of their newborn was not our primary goal, the parents explained many potential benefits, including improving milk production, bonding with the newborn, and developing a sense of competence and confidence. These complementary findings are supported by the literature (27).
The results of our study were discussed by our Family Partnership in NICU Care advisory committee and, in 2019, up to three parents were included to help design approaches to improve parental participation in newborn care.
Study Limitations
Although the sample size was small, at 10 participants, the qualitative design of the study allowed in-depth exploration of parents' experience that covered a range of perspectives, echoing the findings of Russell and Gregory in 2003 (28). The participation of parents who experienced the life in the NICU over a large period, 2015 to 2018, and parents' detailed description of their experiences obtained after three focus groups, provided a good understanding of the themes that influenced their participation in the care of their newborn, using the concepts of saturation outlined by Hennink et al. in 2019 (29). The focus groups were held in English, which may have been a language barrier for parents from different origins or cultures. Understanding of cultural impact is limited by the small number of parents, which did not include the indigenous population among the parents. The participation of only one father precludes any conclusion based on gender. Although similarities in parenting role exist among diverse cultures and religions, the concept of “care” might vary (30). The influence of parental gender, ethnicity, culture and beliefs will need to be explored in future studies.
The focus groups were led by a lead consultant on the ward, who may have previously interacted with parents. Therefore, a potential bias exists if parents felt unable to sincerely answer questions or express their perceptions and concerns. The interview guide not being externally reviewed could be considered a limitation, however strong experience of the interviewers with the environment and specific attention to use open-ended questions without suggestive examples or answer choices mitigated this risk. The analysis process maybe criticized, but the involvement of a third coder as a counter-coding strategy alleviates this caveat (28). Participants did not provide feedback on the transcripts or on the findings as our methodology did not include a triangulation process. Follow-up with the parents to confirm whether our findings reflected their experiences or if parents had new information to add was not possible. Despite the limitations, we believe that the themes identified may be of use to NICU leaders exploring their own environments.
Conclusion
This study provided eight themes in which a wide variety of examples could be used to guide improvements for parental involvement in the care of their newborn in our NICU. As such, a personalized approach focused on each parent's specific needs is an innovative approach to enhance care delivery. Parents' insight should facilitate practice improvements. To implement new approaches that will include these themes, the next step would be to investigate the perspective of healthcare professionals in light of our findings. The goal would be to strengthen partnership between healthcare professional and families to provide individualized support to families of newborns admitted in the NICU.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Children's Hospital of Eastern Ontario Research Institute Research Ethics Board. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
AF, TD, and MS conceptualized and designed the study with significant contributions of EF, KC, CJ, and NM. AF, TD, and EF performed the analysis. KC, CJ, MS, and NM reviewed the analysis for final approval. AF wrote the first draft of the manuscript under the supervision of TD. EF, KC, CJ, MS, and NM reviewed the manuscript, figures, and tables. All authors contributed to manuscript revision, read, and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The research team wishes to thank all the parents who participated in the focus groups. We also thank Francesca de Vries for her assistance and Joan Ramsay medical editor for her contribution to the manuscript.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2021.721835/full#supplementary-material
Appendix 1. Exploratory Focus groups with parents—semi-structured interview guide.
References
1. Rutkowska M. [Newborn at the limit of viability. Part 1: ethical dilemmas, international recommendations]. Med Wieku Rozwoj. (2011) 1:349–55.
2. Dudek-Shriber L. Parent stress in the neonatal intensive care unit and the influence of parent and infant characteristics. J Occup Ther. (2004) 58:509–20. doi: 10.5014/ajot.58.5.509
3. Kenner C, Press J, Ryan D. Recommendations for palliative and bereavement care in the NICU: a family-centered integrative approach. J Perinatol. (2015) 35:S19–23. doi: 10.1038/jp.2015.145
4. Hagen IH, Iversen VC, Nesset E, Orner R, Svindseth MF. Parental satisfaction with neonatal intensive care units: a quantitative cross-sectional study. BMC Health Serv Res. (2019) 19:37. doi: 10.1186/s12913-018-3854-7
5. Purdy IB, Craig JW, Zeanah P. NICU discharge planning and beyond: recommendations for parent psychosocial support. J Perinatol. (2015) 35:S24–8. doi: 10.1038/jp.2015.146
6. Lopez-Maestro M, De la Cruz J, Perapoch-Lopez J, Gimeno-Navarro A, Vazquez-Roman S, Alonso-Diaz C, et al. Eight principles for newborn care in neonatal units: findings from a national survey. Acta Paediatr. (2019) 109:1361–8. doi: 10.1111/apa.15121
7. Vetcho S, Cooke M, Ullman AJ. Family-centred care in dedicated neonatal units: an integrative review of international perspectives. J Neonatal Nurs. (2019) 26: 73–92. doi: 10.1016/j.jnn.2019.09.004
8. Hall SL, Hynan MT, Phillips R, Lassen S, Craig JW, Goyer E, et al. The neonatal intensive parenting unit: an introduction. J Perinatol. (2017) 37:1259–64. doi: 10.1038/jp.2017.108
9. O'Connor S, Brenner M, Coyne I. Family-centred care of children and young people in the acute hospital setting: a concept analysis. J Clin Nurs. (2019) 28 3353–67. doi: 10.1111/jocn.14913
10. O'Brien K, Bracht M, Robson K, Ye XY, Mirea L, Cruz M, et al. Evaluation of the Family Integrated Care model of neonatal intensive care: a cluster randomized controlled trial in Canada and Australia. BMC Pediatr. (2015) 15:210. doi: 10.1186/s12887-015-0527-0
11. Skene C, Gerrish K, Price F, Pilling E, Bayliss P, Gillespie S. Developing family-centred care in a neonatal intensive care unit: an action research study. Intensive Crit Care Nurs. (2019) 1:54–62. doi: 10.1016/j.iccn.2018.05.006
12. Manogaran M. Managing transitions of care: an examination of parents' and providers' perspectives on the transitions of care of neonatal patients from the neonatal intensive care unit (Thesis). Ottawa, ON: Université d'Ottawa/University of Ottawa (2017).
13. Rhoney S. “Share the Wealth”: shared governance in the neonatal intensive care unit. J Obstet Gynecol Neonatal Nurs. (2012) 41:S110–1. doi: 10.1111/j.1552-6909.2012.01361_86.x
14. Creswell JW. Research Design: Qualitative and Quantitative Approaches. Thousand Oaks, CA: Sage Publications (1994). p. 143–72.
15. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. (2007) 19:349–57. doi: 10.1093/intqhc/mzm042
16. Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. (2005) 15:1277–88. doi: 10.1177/1049732305276687
18. Trajkovski S, Schmied V, Vickers M, Jackson D. Neonatal nurses' perspectives of family-centred care: a qualitative study. J Clin Nurs. (2012) 21:2477–87. doi: 10.1111/j.1365-2702.2012.04138.x
19. Palmer SJ. Care of sick children by parents: a meaningful role. J Adv Nurs (1993) 18:185–91. doi: 10.1046/j.1365-2648.1993.18020185.x
20. Manning AN. The NICU Experience: How Does It Affect the Parents' Relationship? (2012). Available online at: https://oce-ovid-com.proxy.bib.uottawa.ca/article/00005237-201210000-00014/HTML (accessed July 12, 2021).
21. Jarrett MH. Parent partners: a parent-to-parent support program in the NICU. Part II: program implementation. Pediatr Nurs. (1996) 22:142–4, 149.
22. Hall SL, Ryan DJ, Beatty J, Grubbs L. Recommendations for peer-to-peer support for NICU parents. J Perinatol. (2015) 35:S9–13. doi: 10.1038/jp.2015.143
23. Aija A, Toome L, Axelin A, Raiskila S, Lehtonen L. Parents' presence and participation in medical rounds in 11 European neonatal units. Early Hum Dev. (2019) 130:10–6. doi: 10.1016/j.earlhumdev.2019.01.003
24. Coyne IT. Parent participation: a concept analysis. J Adv Nurs. (1996) 23:733–40. doi: 10.1111/j.1365-2648.1996.tb00045.x
25. Oude Maatman SM, Bohlin K, Lilliesköld S, Garberg HT, Uitewaal-Poslawky I, Kars MC, et al. Factors influencing implementation of family-centered care in a neonatal intensive care unit. Front Pediatr. (2020) 8:222. doi: 10.3389/fped.2020.00222
26. Flacking R, Lehtonen L, Thomson G, Axelin A, Ahlqvist S, Moran VH, et al. Closeness and separation in neonatal intensive care. Acta Paediatr. (2012) 101:1032–7. doi: 10.1111/j.1651-2227.2012.02787.x
27. Cooper LG, Gooding JS, Gallagher J, Sternesky L, Ledsky R, Berns SD. Impact of a family-centered care initiative on NICU care, staff and families. J Perinatol. (2007) 27:S32–7. doi: 10.1038/sj.jp.7211840
28. Russell CK, Gregory DM. Evaluation of qualitative research studies. Evid Based Nurs. (2003) 6:36–40. doi: 10.1136/ebn.6.2.36
29. Hennink MM, Kaiser BN, Weber MB. What influences saturation? Estimating sample sizes in focus group research. Qual Health Res. (2019) 29:1483–96. doi: 10.1177/1049732318821692
Keywords: NICU, parental involvement, partnership, family-centered care, newborn care, parental perspectives
Citation: Ferreira A, Ferretti E, Curtis K, Joly C, Sivanthan M, Major N and Daboval T (2021) Parents' Views to Strengthen Partnerships in Newborn Intensive Care. Front. Pediatr. 9:721835. doi: 10.3389/fped.2021.721835
Received: 07 June 2021; Accepted: 16 August 2021;
Published: 27 September 2021.
Edited by:
Jos M. Latour, University of Plymouth, United KingdomReviewed by:
Katie Gallagher, University College London, United KingdomFranco Baldoni, University of Bologna, Italy
Copyright © 2021 Ferreira, Ferretti, Curtis, Joly, Sivanthan, Major and Daboval. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Thierry Daboval, dGRhYm92YWxAY2hlby5vbi5jYQ==
 Alexie Ferreira
Alexie Ferreira Emanuela Ferretti2,3
Emanuela Ferretti2,3 Krista Curtis
Krista Curtis Cynthia Joly
Cynthia Joly Myuri Sivanthan
Myuri Sivanthan Thierry Daboval
Thierry Daboval