- 1Pediatric Endocrinology and Diabetes Unit, Dana-Dwek Children's Hospital, Tel Aviv Sourasky Medical Center, Affiliated With the Sackler Faculty of Medicine, Tel Aviv University, Tel Aviv, Israel
- 2Department of Epidemiology and Preventive Medicine, School of Public Health, Sackler Faculty of Medicine, Tel Aviv University, Tel Aviv, Israel
- 3The Nutrition and Dietetics Unit, Dana-Dwek Children's Hospital, Tel Aviv Sourasky Medical Center, Affiliated With the Sackler Faculty of Medicine, Tel Aviv University, Tel Aviv, Israel
- 4The Psychological Services, Tel Aviv Sourasky Medical Center, Affiliated With the Sackler Faculty of Medicine, Tel Aviv University, Tel Aviv, Israel
Introduction: The preventive measures taken in attempt to prevent COVID-19 spread lead to closure of schools and leisure time activities. The impact of the pandemic on pediatric weight status is unclear, reports from around the world predict grave consequences with increasing obesity. We aimed to examine the change in body composition parameters of children and adolescents during the pandemic.
Materials and Methods: An observational study of 220 pediatric subjects (109 boys; mean current age 11.8 ± 3.3 years; 37 with underweight, 123 with normal weight, and 60 with overweight/obesity) who underwent height and body composition measurements by bioelectrical impedance analysis, Tanita MC-780MA, GMON Professional Software before and during the pandemic. Height, body mass index (BMI) and muscle-to-fat ratio (MFR) z-scores were calculated. Data collected from the participants' medical files included home address for socioeconomic position calculation, pubertal stage, and self-reported sleep duration and physical activity performance.
Results: The vast majority of the cohort (81.8%) had stable or improved MFR z-scores during the pandemic. MFR z-scores significantly increased in subjects with underweight (p = 0.05) and normal weight (p = 0.008), but not in subjects with overweight/obesity (p = 0.169). There were significant associations in BMI z-scores (r = 0.961, p < 0.001) and MFR z-scores (r = 0.854, p < 0.001) before and during the pandemic. A multivariate linear regression model identified socioeconomic position, pre-pandemic BMI z-scores, pre-pandemic MFR z-scores, and physical activity levels during the pandemic as predictors for delta MFR z-scores (F = 12.267, p < 0.001). Age, sex, pre-pandemic physical activity, and the time that had elapsed between initiation of the first nationwide lockdown and the BIA assessment during the pandemic did not emerge as predictors for delta MFR z-score.
Conclusions: Our encouraging findings demonstrate improvement in body composition parameters of subjects with underweight and normal weight and stability in subjects with overweight/obesity. Engagement in physical activity during the pandemic predicted improvement, while lower socioeconomic position predicted deterioration.
Introduction
The Coronavirus disease (COVID-19) pandemic continues to demonstrate an enormous impact on morbidity and mortality rates of the entire world population in an age-stratified manner (1–3). On March 15, 2020, the Israeli government declared the first nationwide lockdown, with restriction of non-necessary movement in the public space, and closure of all educational institutions and leisure time activities. The resultant confinement of people to their homes led to lifestyle changes, including diet, sleep, and physical activity. Since then, the Israeli population has been subject to several lockdowns without full restoration of the pre-COVID-19 routine. It has been suggested that this changing reality may have negative implications on metabolic health in adults (4, 5) and in youth (6).
The effect of the COVID-19 pandemic on weight status of children and adolescents remains unclear (7). Reports from around the world predict grave consequences with increasing obesity, especially in predisposed individuals (8–10). Multiple studies are based on lifestyle questionnaires, which subjectively reflect eating behavior and physical activity of adults over a limited time period (11–13), with only a minority of the studies objectively quantitating the effect on the weight status of children (14). Childhood obesity and its future metabolic implications are now of even greater concern than ever with future threats on health economics (15).
Childhood weight status is most widely classified by age- and sex-specific cutoffs for body mass index (BMI) (16). BMI z-scores, however, can not characterize the relationship between fat and muscle (17). Both increased adiposity, especially if centrally located, and decreased skeletal muscle mass have been linked to early-onset metabolic derangements (18–20). Since January 2018, our Pediatric Endocrine Unit implemented the analysis of body composition by means of bioelectrical impedance analysis (BIA) as part of routine assessment of patients referred for endocrine consultation (21). In the current study, we aimed to examine changes in body composition parameters of children and adolescents belonging to different weight status categories (underweight, normal weight, and overweight/obesity), during the COVID-19 pandemic.
Materials and Methods
Study Design
This real-life, observational study was conducted in the Pediatric Endocrine Unit in a tertiary medical center. The clinic's BIA database was searched for children and adolescents (age 5–18 years) with the sole diagnosis of “observation of growth” and/or “observation of puberty” whose body composition parameters were measured during the COVID-19 pandemic (from May 15, 2020 until December 15, 2020). Included were subjects for whom pre-COVID-19 BIA measurements were available. Those BIA data were linked to the subjects' electronic medical records. Excluded from the study were patients who entered puberty and those who initiated medication or underwent bariatric surgery between the two time periods.
Data Collection
Data collected from the participants' medical files included sex, age, home address, perinatal history (mode of conception, number of fetuses, gestational diabetes mellitus, gestational age, and birthweight), anthropometric measurements, systolic (SBP) and diastolic blood pressure (DBP) measurements, pubertal stage, and self-reported sleep duration and physical activity performance.
Anthropometric Measurements and Pubertal Assessment
The clinical evaluation of the study subjects included measurement of height by a commercial Harpenden stadiometer (Holtain Ltd., Crosswell, United Kingdom) and weight by BIA. BMI was calculated as weight in kilograms divided by height in meters squared. The subjects' height, weight, and BMI values were converted to sex- and age-specific standard deviation scores (z-scores) with PediTools Electronic Growth Chart Calculators, based on CDC growth charts (22). Weight status was categorized as underweight for BMI values ≤ 5th percentile (z-score at or below −1.645), normal for BMI between 5th and 84th percentiles (z-score between −1.645 and 1.036), and overweight and obese for BMI ≥ 85th percentile (z-score at or above 1.036) (23). Corrected birth weight z-scores were calculated with PediTools Electronic Growth Chart Calculators (22). The appropriate for gestational age (AGA) birth weight was defined as corrected birth weight z-scores of −1.88 to 1.88, the small for gestational age (SGA) as birth weight z-scores < −1.88, and the large for gestational age (LGA) as birth weight z-scores > 1.88. BP percentiles were calculated by means of an online age-based pediatric BP calculator (24).
Pubertal stages were graded with Tanner scores for genital status in boys and for breast development in girls (25, 26). Onset of puberty was defined as genitalia Tanner stage 2 with testicular volume > 3 mL in boys and appearance of breast buds in girls, with or without sexual hair. The subject was considered fully pubertal when pubertal signs corresponded to Tanner stage 5.
Body Composition Measurement
Body composition in subjects older than 5 years of age who were able to stand upright was measured by BIA (Tanita Body Composition Analyzer, Tanita MC-780 MA and GMON Professional Software), which has been clinically verified to be accurate and reliable and to provide highly reproducible results (27, 28). The BIA measures both whole body and segmental analysis (trunk, upper, and lower limbs) of fat and muscle. The BIA measurement required the subject to stand barefoot on the analyzer and to grip the handles, and the entire procedure took ~1 min per subject. The BIA report includes the following data: body weight (kilograms), fat percentage (FATP), truncal fat percentage (TFATP), fat mass (kilograms), and muscle mass (kilograms). Calculated variables included: appendicular skeletal muscle mass (ASMM = the sum of muscle mass of four limbs) and muscle-to-fat ratio [MFR = ASMM (kg)/fat mass (kg)]. The z-scores for MFR were calculated according to BIA pediatric reference curves (29). Delta MFR z-scores were calculated as the difference between MFR z-scores during the COVID-19 pandemic and the MFR z-scores preceding the pandemic. Subjects were stratified into three groups according to delta MFR z-scores: better (delta MFR z-score > 0.3), stable (−0.3 ≤ delta-MFR z-score ≤ 0.3), and worse (delta-MFR z-score < −0.3) (29, 30).
Socioeconomic Position
The SEP by home address was analyzed based on the Israel Central Bureau of Statistics' Characterization and Classification of Statistical Areas within Municipalities and Local Councils by the Socio-Economic Level of the Population 2015 (31). The neighborhoods or localities are divided into SEP clusters, with 1 representing the lowest and 10 representing the highest rating. The SEP index is an adjusted calculation of 14 variables that measure social and economic levels in the domains of demographics, education, standard of living, and employment (range from −2.797 to 2.590).
Ethics
The study was approved by the Ethics Committee of the Tel-Aviv Sourasky Medical Center according to the Helsinki Declaration. Informed consent by the participants was waived since the data were retrieved from the subjects' medical records and all personal identification was omitted. The data were handled in accordance with the principles of Good Clinical Practice.
Statistical Analyses
The data were analyzed with Statistical Package for the Social Sciences software version 27 (SPSS Inc., Chicago, IL). All statistical tests were 2-sided. The Kolmogorov-Smirnov test was applied to test the normality of continuous data. The data are expressed as means ± standard deviations (SDs) for normally distributed variables and median and interquartile range (IQR) for skewed distribution or number (percent) for categorical variables. To compare body composition and BP before and during the COVID-19 pandemic stratified according to weight status, the paired-samples t-test or the Wilcoxon matched-pair signed rank-test were used for normal or skewed distributions, respectively. One-way ANOVA analysis and post-hoc Tukey or Kruskal Wallis tests were used to compare between change in the MFR ratio z-score categories and weight-status categories (three categories each) in normal and skewed variables, respectively. A one-sample Wilcoxon signed rank test was performed to test the null hypothesis that the median z-score equals zero. Pearson's correlation test was applied to examine the correlation between two continuous data groups. A multivariate stepwise linear regression model was used to identify predictors for the delta MFR z-score. A p-value of ≤ 0.05 was considered significant.
Results
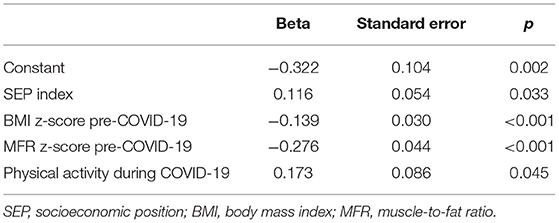
The study cohort was comprised of 220 pediatric subjects (49.5% males) with a mean ± SD current age of 11.8 ± 3.3 years. The median time that had elapsed between BIA assessments (pre-COVID-19 and during COVID-19) was 10.8 months [IQR 7.3, 11.6], and the median time that had elapsed between the initiation of the first nationwide lockdown and the BIA assessment during COVID-19 was 4 months [IQR 3, 5]. The subjects' sociodemographic and perinatal characteristics, pre-COVID-19 anthropometric measurements, BP percentiles, and pubertal status are shown in Table 1. Most of the subjects were conceived spontaneously in a singleton pregnancy and were born at term with birthweight appropriate for gestational age. At the pre-COVID-19 assessment, the median BMI z-score of the cohort was within average (−0.13 [−1.24, 1.14], p = 0.383), 45.4% were pre-pubertal, and 54.6% were in puberty/fully pubertal. The median sleep duration was 9 h (range 5–11 h). Most of the subjects (83%) were engaged in some kind of physical activity during and after school.
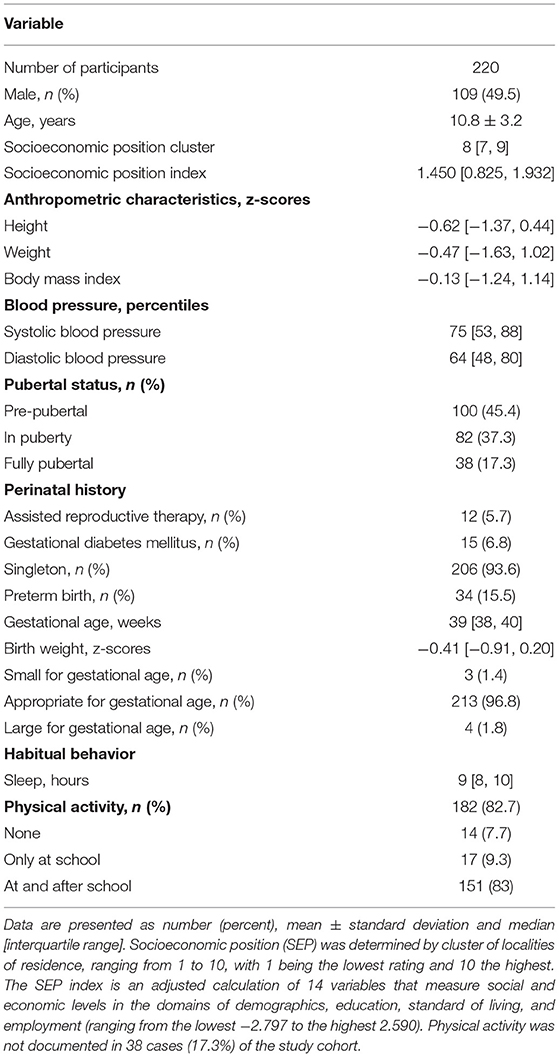
Table 1. Sociodemographic, perinatal, and pre-COVID-19 characteristics of 220 children and adolescents.
At the pre-COVID-19 assessment, the cohort was comprised of 37 (16.8%) subjects with underweight, 123 (55.9%) with normal weight, and 60 (27.3%) with overweight/obesity. Subjects with overweight/obesity had a lower median SEP cluster and SEP index compared to those with normal weight and underweight (8 [6.25, 8.75] vs. 8 [8, 9] and 8 [8, 9]; 1.039 [0.422, 1.636] vs. 1.609 [1.002, 1.955] and 1.553 [1.078, 2.005], respectively, p < 0.001 for both parameters). The distribution of weight status categories differed between sexes [boys: 26 (23.9%) underweight, 60 (55%) normal weight, and 23 (21.1%) overweight/obesity and girls: 11 (10%) underweight, 93 (56.8%) normal weight, and 37 (33.2%) overweight/obesity, respectively, p = 0.009]. The time that had elapsed between the initiation of the first nationwide lockdown and the BIA assessment during the pandemic did not differ between weight categories (p = 0.372). During the COVID-19 assessment the cohort was comprised of 26 (11.8%) subjects with underweight, 137 (62.3%) with normal weight, and 57 (25.9%) with overweight/obesity, the change in distribution of weight status categories did not reach significance (p = 0.244). The body composition parameters of the cohort stratified by pre-COVID-19 weight status are presented in Table 2. Indices of adiposity, FATP, and TFATP did not significantly change during the pandemic. The MFR z-scores of the underweight and normal weight subjects significantly increased during the pandemic (p = 0.05 and p = 0.008, respectively), while it did not change in subjects with overweight/obesity (p = 0.169). Pearson's correlation analysis revealed significant associations between the BMI z-scores of subjects before and during the pandemic (r = 0.961, p < 0.001) (Figure 1A), and between the MFR z-scores of subjects before and during the pandemic (0.854, p < 0.001) (Figure 1B).
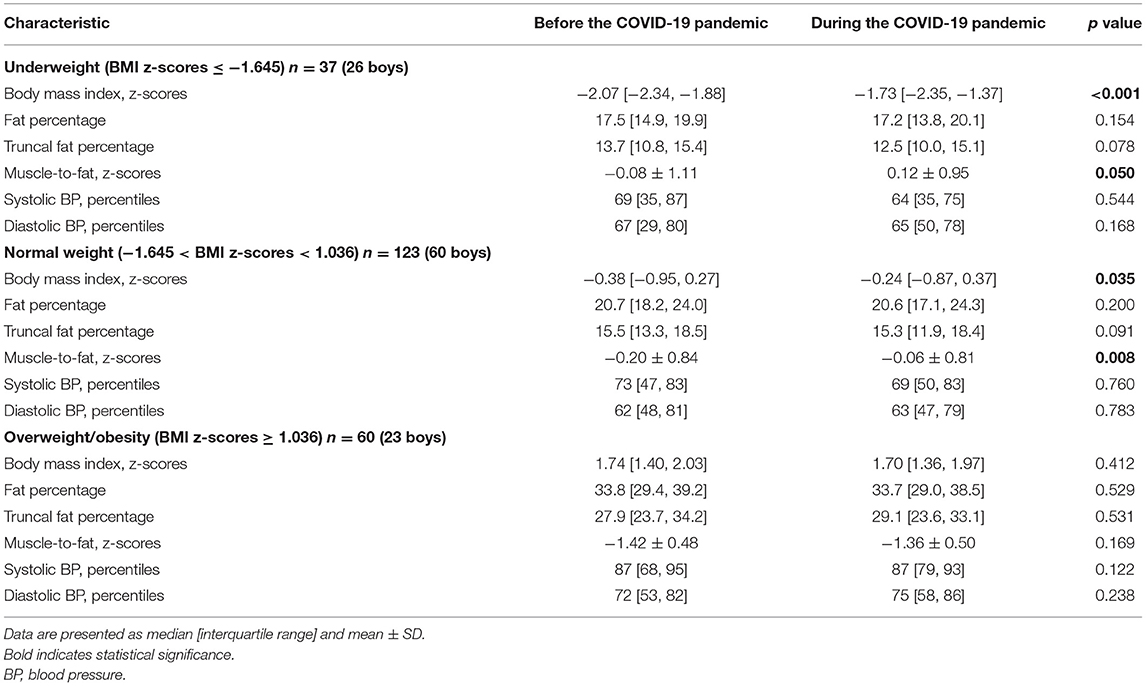
Table 2. Body composition and blood pressure characteristics of 220 children and adolescents before and during the COVID-19 pandemic stratified according to weight status.
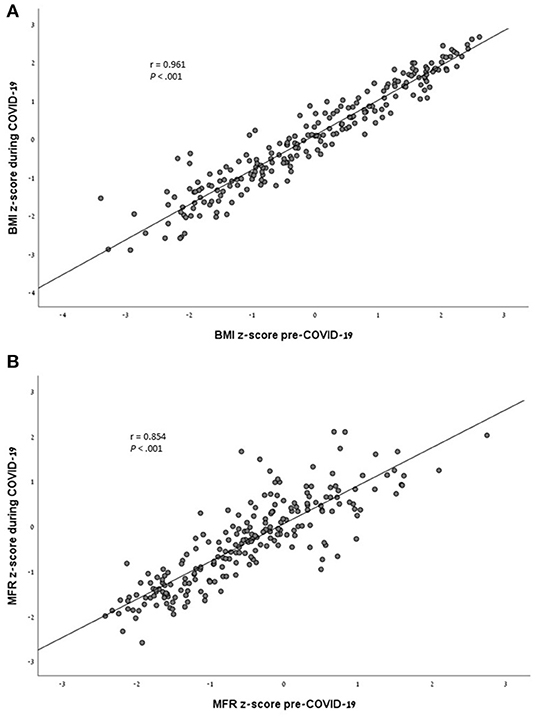
Figure 1. (A) Analysis of the correlation between the BMI z-scores of subjects before and during the COVID-19 pandemic (r = 0.961, P < 0.001). (B) Analysis of the correlation between the MFR z-scores of subjects before and during the COVID-19 pandemic (r = 0.854, P < 0.001).
The vast majority of the cohort (81.8%) had stable or improved MFR z-scores during the pandemic. Sociodemographic, anthropometric, and body composition parameters of the subjects stratified by change in the MFR z-scores (delta MFR z-scores) are presented in Table 3. Sex, age, SEP (cluster and index), and anthropometric parameters did not differ between the delta MFR z-score groups. Subjects whose MFR z-scores worsened during the pandemic had a lower fat percentage, a lower truncal fat percentage, and a higher MFR z-score at baseline (p = 0.05, p = 0.026, and p < 0.001, respectively).
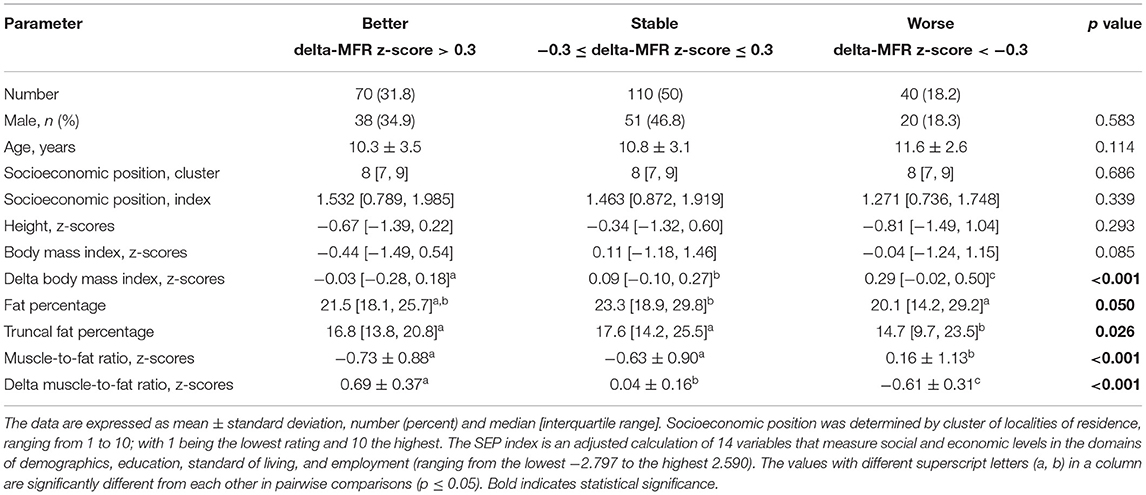
Table 3. Sociodemographic, anthropometric, and body composition parameters of the study cohort before COVID-19 pandemic stratified by change in muscle-to-fat ratio (MFR) z-scores.
A multivariate linear regression model identified SEP index, pre-pandemic BMI z-score, pre-pandemic MFR z-score, and physical activity during the pandemic as predictors for the delta MFR z-score (F = 12.267, p < 0.001). Age, sex, pre-pandemic physical activity, and the time that had elapsed between initiation of the first nationwide lockdown and the BIA assessment during the pandemic did not emerge as predictors for delta MFR z-score and therefore were not included in the model (Table 4).
A univariate analysis performed on the findings of the subjects with underweight, normal weight, and overweight/obesity revealed significant correlations between pre-pandemic MFR z-scores and delta MFR z-scores (r = −0.524, p = 0.001; r = −0.391, p < 0.001 and r = −0.291, p = 0.024, respectively, and p = 0.428 for the comparison between correlations).
Discussion
It could be reasonably expected that the extended period out of school would lead to an increase in sedentary behavior with worsening of body composition. However, the subjects in our select cohort tended to maintain similar BMI and MFR z-scores, and 31.8% even improved their body composition during the COVID-19 pandemic. Improvement in both weight status (BMI z-scores) and body composition (MFR z-scores) was evidenced in subjects with underweight and normal weight, while those with overweight/obesity maintained stable parameters. Engagement in physical activity during the pandemic predicted an improvement in body composition, while lower socioeconomic position predicted deterioration.
The COVID-19 pandemic has had enormous effects on lifestyle that could potentially cause health-related problems. In Israel, most workplaces gradually returned to full activity under strict safety guidance. Schools were the last to resume activity, with limited numbers of schools reopening (kindergartens, grades 1–3 and 11–12) since May 2020. Major COVID-19 outbreaks were reported in schools only a few days after opening, leading to a second unlimited closure of all educational settings (32). The exclusion of the pediatric population from the vaccination program was an obstacle in planning the reopening of school (33). Two studies suggested that the prolonged closure of schools may disproportionately affect activity patterns and weight status of youths (34, 35). Of note, 92.3% of our cohort had been engaged in physical activity during school hours in the pre-pandemic period, and 83% also did so after school hours. Encouragement in participating in physical activity is an integral part of the healthy lifestyle education provided to all the subjects followed at our clinic, regardless of their weight status. Our results could, therefore, be attributed in no small part to the increased awareness of healthy habits and the desirability of maintaining them. Another potential contributor is the increased accessibility and popularity of at-home physical activity through web-based applications (YouTube, Tik-Tok, etc.). Surveys for quantification of physical activity were not part of this observational study.
The extent of change in body composition differed between weight status categories, with the greatest improvement measured in the subjects with underweight. The worse their pre-pandemic body composition, the greater the improvement that had been measured during the pandemic. Children and adolescents with low weight status are considered at increased risk for infectious diseases (36, 37). The pandemic rampage with increasing anxiety of developing severe manifestation might have raised the parental motivation for improving the offspring's nutrition status. In addition, the prolonged stay at home changed familial practices with increased time spent in planning and preparing meals (38). Of note, subjects with underweight did not only improve their BMI z-scores as a result of increased caloric consumption; their body composition improvement may reflect a healthier food selection combined with physical activity. This improvement in muscle mass may decrease the metabolic hazards related to early-onset sarcopenia (39). The combination of sarcopenia with increased adiposity, termed “sarcopenic obesity,” may result in the false impression of slightly elevated BMI while harboring a double jeopardy (40).
The management of pediatric obesity is a daunting challenge, especially since lifestyle interventions have shown only modest effect on weight loss (41). The COVID-19 period further intensified the challenge faced by obese children who were threatened by increased obesity and metabolic health deterioration (42). We were gratified to observe that, on average, weight status, body composition, and BP percentiles of subjects with overweight and obesity were stable. This could not be attributed to any new medication or their having undergone bariatric surgery, since they were study exclusion criteria. A plausible explanation for this welcome achievement could be the preservation of continuity of surveillance in the clinic in spite of the ongoing pandemic. Our multidisciplinary team of physicians, nurse educators, dieticians, and psychosocial workers deliver age-appropriate medical care and healthy lifestyle education to clinic attendees and their families. The continuity of medical care, either in-clinic or by telemedicine, provides a network of support that is crucial in obesity management (43).
A lower socioeconomic position predicted decreased delta MFR z-score during the COVID-19 pandemic. Socioeconomic circumstances are recognized as a major determinant of health conditions in children and adolescents (44). The COVID-19 pandemic has led to an economic crisis, characterized by increasing rates of unemployment and financial insecurity with increasing health inequalities (45). Coping with financial strain may negatively impact health behaviors, such as leading to unhealthy food choices and decreased enthusiasm for physical activity (46). While our society as a whole was not immune to such financial upheavals, our patients were apparently successfully persuaded not to fall victim to such consequences. The metabolic consequences of these will be dealt in the future, as unhealthy lifestyle during childhood has both metabolic and behavioral effects (47). Health care systems should take these findings into consideration in planning contemporary health care strategies.
Our study is not without limitations. The cohort was comprised of children and adolescents, both boys and girls, from a wide age range, at various stages of physical growth and development. Cognitive and emotional maturation depends on age and the course of development may vary between the sexes. Therefore, our ability to draw conclusion on health behaviors of a specific age group during the pandemic is limited. In addition, our study did not include questionnaires for evaluating nutritional, behavioral and psychological aspects before and during the COVID-19 pandemic. Since only patients who attended our pediatric endocrine clinic during the pandemic were included, the results may not reflect the body composition of individuals who are not similarly followed by professional medical care providers. Therefore, the generalizability of this study may be limited. Nevertheless, our encouraging findings support the recommendations for global growth surveillance, including a healthy lifestyle education (48). This undertaking is crucial in the current challenging period of spiraling obesity. The major strength of this study is the uniformity of anthropometric, body composition, and BP measurements, together with the calculation of sex- and age-adjusted z-scores/percentiles, allowing for comparisons between subjects.
Conclusion
The weight status and body composition of children and adolescents attending our pediatric endocrine clinic were relatively stable during the COVID-19 pandemic. Subjects with underweight and normal weight had improved body composition parameters, while those with overweight/obesity remained stable. Engagement in physical activity during the pandemic predicted an improvement in body composition, while lower socioeconomic position predicted deterioration. These encouraging findings may well be attributed to the regular growth surveillance and healthy lifestyle education provided to the study participants. We suggest that their availability to the pediatric population at large will produce a similarly rewarding impact on health and far-reaching positive repercussions on health economics.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Tel Aviv Sourasky Medical Center. Written informed consent from the participants' legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author Contributions
EA contributed, analyzed and interpreted the data, wrote the first draft, and revised the manuscript. MY-G performed the statistical analysis, interpreted the data, and critically revised the manuscript. HY, IG, AL, TS, and YW contributed to the data used in this study, contributed to the discussion, and reviewed and edited the manuscript. YL conceived and designed the study, interpreted the data, and revised the manuscript for important intellectual content. AB conceived and designed the study, analyzed and interpreted the data, wrote the first draft and revised the manuscript, incorporating contributions from coauthors (EA, MY-G, HY, IG, AL, TS, YW, and YL), and decided on submission. AB is the guarantor of this work and as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. All authors contributed to the article and approved the submitted version.
Funding
This research was supported by a grant from NovoNordisk (Grant No. 8781).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We wish to thank the subjects who participated in this study. The authors thank Esther Eshkol for editorial assistance.
Abbreviations
ASMM, appendicular skeletal muscle mass; BIA, bioimpedance analysis; BMI, body mass index; FATP, fat percentage; TFATP, truncal fat percentage; MFR, muscle-to-fat ratio; MPHt, mid-parental height; SEP, socioeconomic position.
References
1. Banerjee A, Pasea L, Harris S, Gonzalez-Izquierdo A, Torralbo A, Shallcross L, et al. Estimating excess 1-year mortality associated with the COVID-19 pandemic according to underlying conditions and age: a population-based cohort study. Lancet. (2020) 395:1715–25. doi: 10.1016/S0140-6736(20)30854-0
2. Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. (2020) 382:1199–207. doi: 10.1056/NEJMoa2001316
3. Puig-Domingo M, Marazuela M, Giustina A. COVID-19 and endocrine diseases. A statement from the European Society of Endocrinology. Endocrine. (2020) 68:2–5. doi: 10.1007/s12020-020-02294-5
4. Martinez-Ferran M, de la Guía-Galipienso F, Sanchis-Gomar F, Pareja-Galeano H. Metabolic impacts of confinement during the COVID-19 pandemic due to modified diet and physical activity habits. Nutrients. (2020) 12:1549. doi: 10.3390/nu12061549
5. Wang G, Zhang Y, Zhao J, Zhang J, Jiang F. Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet. (2020) 395:945–7. doi: 10.1016/S0140-6736(20)30547-X
6. An R. Projecting the impact of the coronavirus disease-2019 pandemic on childhood obesity in the United States: a microsimulation model. J Sport Health Sci. (2020) 9:302–12. doi: 10.1016/j.jshs.2020.05.006
7. Cuschieri S, Grech S. COVID-19: a one-way ticket to a global childhood obesity crisis? J Diabetes Metab Disord. (2020) 19:1–4. doi: 10.1007/s40200-020-00682-2
8. Pietrobelli A, Pecoraro L, Ferruzzi A, Heo M, Faith M, Zoller T, et al. Effects of COVID-19 lockdown on lifestyle behaviors in children with obesity living in Verona, Italy: a longitudinal study. Obesity. (2020) 28:1382–5. doi: 10.1002/oby.22861
9. Robinson E, Boyland E, Chisholm A, Harrold J, Maloney NG, Marty L, et al. Obesity, eating behavior and physical activity during COVID-19 lockdown: a study of UK adults. Appetite. (2021) 156:104853. doi: 10.1016/j.appet.2020.104853
10. Rundle AG, Park Y, Herbstman JB, Kinsey EW, Wang YC. COVID-19-related school closings and risk of weight gain among children. Obesity. (2020) 28:1008–9. doi: 10.1002/oby.22813
11. Reyes-Olavarría D, Latorre-Román PÁ, Guzmán-Guzmán IP, Jerez-Mayorga D, Caamaño-Navarrete F, Delgado-Floody P. Positive and negative changes in food habits, physical activity patterns, and weight status during COVID-19 confinement: associated factors in the Chilean population. Int J Environ Res Public Health. (2020) 17:5431. doi: 10.3390/ijerph17155431
12. Sidor A, Rzymski P. Dietary choices and habits during COVID-19 lockdown: experience from Poland. Nutrients. (2020) 12:1–13. doi: 10.3390/nu12061657
13. Kriaucioniene V, Bagdonaviciene L, Rodríguez-Pérez C, Petkeviciene J. Associations between changes in health behaviours and body weight during the COVID-19 quarantine in Lithuania: the Lithuanian COVIDiet study. Nutrients. (2020) 12:3119. doi: 10.3390/nu12103119
14. Tester JM, Rosas LG, Leung CW. Food insecurity and pediatric obesity: a double whammy in the era of COVID-19. Curr Obes Rep. (2020) 9:442–50. doi: 10.1007/s13679-020-00413-x
15. Ogden CL, Fryar CD, Hales CM, Carroll MD, Aoki Y, Freedman DS. Differences in obesity prevalence by demographics and urbanization in US children and adolescents, 2013-2016. JAMA. (2018) 319:2410–8. doi: 10.1001/jama.2018.5158
16. Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. (2000) 320:1240–3. doi: 10.1136/bmj.320.7244.1240
17. Maynard LM, Wisemandle W, Roche AF, Chumlea WC, Guo SS, Siervogel RM. Childhood body composition in relation to body mass index. Pediatrics. (2001) 107:344–50. doi: 10.1542/peds.107.2.344
18. Kyle UG, Earthman CP, Pichard C, Coss-Bu JA. Body composition during growth in children: limitations and perspectives of bioelectrical impedance analysis. Eur J Clin Nutr. (2015) 69:1298–305. doi: 10.1038/ejcn.2015.86
19. Maffeis C, Morandi A. Body composition and insulin resistance in children. Eur J Clin Nutr. (2018) 72:1239–45. doi: 10.1038/s41430-018-0239-2
20. Steene-Johannessen J, Anderssen SA, Kolle E, Andersen LB. Low muscle fitness is associated with metabolic risk in youth. Med Sci Sports Exerc. (2009) 41:1361–7. doi: 10.1249/MSS.0b013e31819aaae5
21. Brener A, Peleg I, Rosenfeld T, Kern S, Uretzky A, Elkon-Tamir, et al. Beyond body mass index - body composition assessment by bioimpedance in routine endocrine practice. Endocr Pract. (2021) 27:419–25. doi: 10.1016/j.eprac.2020.10.013
22. Chou JH, Roumiantsev S, Singh R. PediTools electronic growth chart calculators: applications in clinical care, research, and quality improvement. J Med Internet Res. (2020) 22:e16204. doi: 10.2196/16204
23. Barlow SE, Expert Committee. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. (2007) 120 (Suppl. 4):S164–92. doi: 10.1542/peds.2007-2329C
24. Shypailo RJ. Age-Based Pediatric Blood Pressure Reference Charts. Retrieved 1/5/2021 from the Baylor College of Medicine, Children's Nutrition Research Center, Body Composition Laboratory. (2018). Available online at: http://www.bcm.edu/bodycomplab/BPappZjs/BPvAgeAPPz.html (accessed April 6, 2021).
25. Marshall WA, Tanner JM. Variations in pattern of pubertal changes in girls. Arch Dis Child. (1969) 44:291–303. doi: 10.1136/adc.44.235.291
26. Marshall WA, Tanner JM. Variations in the pattern of pubertal changes in boys. Arch Dis Child. (1970) 45:13–23. doi: 10.1136/adc.45.239.13
27. Lee SY, Gallagher D. Assessment methods in human body composition. Curr Opin Clin Nutr Metab Care. (2008) 11:566–72. doi: 10.1097/MCO.0b013e32830b5f23
28. Shypailo RJ, Motil KJ. The use of bioimpedance in pediatric health, nutrition, and disease. J Pediatr Gastroenterol Nutr. (2018) 67:435–6. doi: 10.1097/MPG.0000000000002068
29. McCarthy HD, Samani-Radia D, Jebb SA, Prentice AM. Skeletal muscle mass reference curves for children and adolescents. Pediatr Obes. (2014) 9:249–59. doi: 10.1111/j.2047-6310.2013.00168.x
30. Mei Z, Grummer-Strawn LM. Standard deviation of anthropometric Z-scores as a data quality assessment tool using the 2006 WHO growth standards: a cross country analysis. Bull World Health Organ. (2007) 85:441–8. doi: 10.2471/BLT.06.034421
31. Israel Central Bureau of Statistics (CBS); 2019. Characterization and Classification of Geographical Units by the Socio-Economic Level of the Population. (2015). Available online at: https://www.cbs.gov.il/he/publications/DocLib/2019/1765_socio_economic_2015/e_print.pdf (accessed March 1, 2021).
32. Stein-Zamir C, Abramson N, Shoob H, Libal E, Bitan M, Cardash T, et al. A large COVID-19 outbreak in a high school 10 days after schools' reopening, Israel, May 2020. Euro Surveill. (2020) 25:2001352. doi: 10.2807/1560-7917.ES.2020.25.29.2001352
33. Dagan N, Barda N, Kepten E, Miron O, Perchik S, Katz MA, et al. BNT162b2 mRNA Covid-19 vaccine in a nationwide mass vaccination setting. N Engl J Med. (2021) 384:1412–23. doi: 10.1056/NEJMoa2101765
34. Yang S, Guo B, Ao L, Yang C, Zhang L, Zhou J, et al. Obesity and activity patterns before and during COVID-19 lockdown among youths in China. Clin Obes. (2020) 10:e12416. doi: 10.1111/cob.12416
35. Jia P, Zhang L, Yu W, Yu B, Liu M, Zhang D, et al. Correction: impact of COVID-19 lockdown on activity patterns and weight status among youths in China: the COVID-19 impact on lifestyle change survey (COINLICS). Int J Obes. (2021) 45:920. doi: 10.1038/s41366-020-00736-8
36. Walson JL, Berkley JA. The impact of malnutrition on childhood infections. Curr Opin Infect Dis. (2018) 31:231–236. doi: 10.1097/QCO.0000000000000448
37. Mertens E, Peñalvo JL. The burden of malnutrition and fatal COVID-19: a global burden of disease analysis. Front Nutr. (2021) 7:619850. doi: 10.3389/fnut.2020.619850
38. Philippe K, Chabanet C, Issanchou S, Monnery-Patris S. Child eating behaviors, parental feeding practices and food shopping motivations during the COVID-19 lockdown in France: (How) did they change? Appetite. (2021) 161:105132. doi: 10.1016/j.appet.2021.105132
39. Ooi PH, Thompson-Hodgetts S, Pritchard-Wiart L, Gilmour SM, Mager DR. Pediatric sarcopenia: a paradigm in the overall definition of malnutrition in children? J Parenter Enteral Nutr. (2020) 44:407–18. doi: 10.1002/jpen.1681
40. Cauley JA. An overview of sarcopenic obesity. J Clin Densitom. (2015) 18:499–505. doi: 10.1016/j.jocd.2015.04.013
41. Kumar S, Kelly AS. Review of childhood obesity: from epidemiology, etiology, and comorbidities to clinical assessment and treatment. Mayo Clin Proc. (2017) 92:251–65. doi: 10.1016/j.mayocp.2016.09.017
42. Nogueira-de-Almeida CA, Del Ciampo LA, Ferraz IS, Del Ciampo IRL, Contini AA, Ued FDV. COVID-19 and obesity in childhood and adolescence: a clinical review. J Pediatr. (2020) 96:546–58. doi: 10.1016/j.jped.2020.07.001
43. O'Hara VM, Johnston SV, Browne NT. The paediatric weight management office visit via telemedicine: pre- to post-COVID-19 pandemic. Pediatr Obes. (2020) 15:e12694. doi: 10.1111/ijpo.12694
44. Moreno-Maldonado C, Ramos P, Moreno C, Rivera F. Direct and indirect influences of objective socioeconomic position on adolescent health: the mediating roles of subjective socioeconomic status and lifestyles. Int J Environ Res Public Health. (2019) 16:1637. doi: 10.3390/ijerph16091637
45. Wright L, Steptoe A, Fancourt D. Are we all in this together? Longitudinal assessment of cumulative adversities by socioeconomic position in the first 3 weeks of lockdown in the UK. J Epidemiol Community Health. (2020) 74:683–8. doi: 10.1136/jech-2020-214475
46. Beenackers MA, Oude Groeniger J, van Lenthe FJ, Kamphuis CBM. The role of financial strain and self-control in explaining health behaviours: the GLOBE study. Eur J Public Health. (2018) 28:597–603. doi: 10.1093/eurpub/ckx212
47. Wang J, Geng L. Effects of socioeconomic status on physical and psychological health: lifestyle as a mediator. Int J Environ Res Public Health. (2019) 16:281. doi: 10.3390/ijerph16020281
Keywords: body composition, bioimpedance, BMI, children and adolescents, COVID-19, muscle-to-fat ratio, overweight and obesity, weight status
Citation: Azoulay E, Yackobovitch-Gavan M, Yaacov H, Gilboa I, Lopez A, Sheppes T, Waksman Y, Lebenthal Y and Brener A (2021) Weight Status and Body Composition Dynamics in Children and Adolescents During the COVID-19 Pandemic. Front. Pediatr. 9:707773. doi: 10.3389/fped.2021.707773
Received: 10 May 2021; Accepted: 07 June 2021;
Published: 05 July 2021.
Edited by:
Andrea Enzo Scaramuzza, Istituti Ospitalieri di Cremona, ItalyReviewed by:
Sudip Datta Banik, Centro de Investigaciones y Estudios Avanzados, Instituto Politécnico Nacional de México (CINVESTAV), MexicoZbigniew Kułaga, Children's Memorial Health Institute (IPCZD), Poland
Copyright © 2021 Azoulay, Yackobovitch-Gavan, Yaacov, Gilboa, Lopez, Sheppes, Waksman, Lebenthal and Brener. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Avivit Brener, YXZpdml0YkB0bHZtYy5nb3YuaWw=
 Erez Azoulay1
Erez Azoulay1 Yael Lebenthal
Yael Lebenthal Avivit Brener
Avivit Brener