- 1International Affairs, Hunan Children's Hospital, Changsha, China
- 2Training and Research, Mnazi Mmoja Hospital, Zanzibar, Tanzania
- 3Nursing School, Hunan University of Chinese Medicine, Changsha, China
- 4Editing Office, Journal of Clinical Pediatric Surgery, Hunan Children's Hospital, Changsha, China
- 5Neonatal Department, Hunan Children's Hospital, Changsha, China
- 6Nursing Department, Hunan Children's Hospital, Changsha, China
- 7Faculty of Health, University of Plymouth, Plymouth, United Kingdom
Background: Neonatal mortality rates remain high in Sub-Saharan African countries. Improving the newborn resuscitation skills of healthcare professionals is important in addressing this challenge. The aim of this study was to evaluate a neonatal resuscitation training programme delivered over a two-year period for healthcare professionals in Zanzibar, Tanzania.
Methods: A pre- and post-intervention study was designed. We delivered neonatal resuscitation training over a 2-day period in 2017 and 2 days of refresher training in 2018. Knowledge was evaluated by a self-designed survey (11 items with a total score of 22) before and after the two training periods, and skills were evaluated by a skills checklist (six domains with 25 items with a total score of 50) completed by the trainers based on their observations. Statistical analysis included differences in the knowledge and skills scores before and after the training sessions and between the two periods.
Results: A total of 23 healthcare professionals participated and completed both neonatal resuscitation training sessions. The knowledge mean scores before and after the training in 2017 increased from 9.60 to 13.60 (95% CI: −5.900; −2.099, p < 0.001), and in 2018, the scores increased from 10.80 to 15.44 (95% CI: −6.062; −3.217, p < 0.001). The mean knowledge scores post-training over time were 13.60 in 2017 and 15.44 in 2018 (95% CI: −3.489; 0.190, p = 0.030). The resuscitation skills performance between the two time periods increased from a mean of 32.26 (SD = 2.35) to a mean of 42.43 (SD = 1.73) (95% CI: −11.402; −8.945, p < 0.001).
Conclusion: The neonatal resuscitation training programme increased the theoretical knowledge and resuscitation skills before and after the two training sessions and over time after a 9-month period. Continuous neonatal resuscitation training based on the local needs in resource-limited countries is essential to provide confidence in healthcare professionals to initiate resuscitation and to improve newborn outcomes.
Introduction
While child mortality has improved globally over the past decades, neonatal mortality rates have remained stagnant in certain areas. The annual estimated range of child mortality decreased from 4.7 to 2.8 million, with a 40% drop between 1990 and 2013 (1, 2). Almost half of neonatal deaths occur in low- and middle-income countries. This is most prevalent in Sub-Saharan countries in Africa, including Tanzania (3). Tanzania has one of the lowest physician-to-population ratios in the world, and neonatal mortality remains high at 21 deaths per 1,000 live births (4). Although significant efforts have been made to fulfill the Sustainable Development Goals, less progress has been shown in the reduction of neonatal mortality rates to at least 12 per 1,000 live births (5, 6). High neonatal mortality is partially influenced by a lack of qualified healthcare professionals with skills in neonatal resuscitation, inadequate training, and insufficient medical resources (7). Therefore, neonatal resuscitation training programmes are a priority to reduce preventable deaths and thereby reduce neonatal mortality (8).
Birth asphyxia and failure to initiate or sustain resuscitation at birth remain the main causes of neonatal deaths worldwide (9). These data are even higher in rural locations, such as in Zanzibar hospitals, where up to 60% of neonatal deaths occur (10, 11). A survey study in five rural districts of southern Tanzania identified 219 neonatal deaths (12). The most common causes of neonatal death were prematurity (n = 72; 33%), birth asphyxia (n = 49; 22%), infection (n = 21; 10%), congenital abnormalities (n = 10; 5%), and 19 other causes (9%) (12).
Several studies have demonstrated that interventions related to improving neonatal resuscitation can increase infant survival (13–15). Furthermore, home delivery is considered a common practice in Zanzibar, and only a few skilled birth attendants are available for home delivery (16). Skilled birth attendants in Zanzibar include midwives and healthcare workers who are trained in normal delivery, pregnancy management, and referral in case of complications. Additionally, a study performed in regions of Africa, Asia and Latin America/Caribbean indicated that a short period of in-service training was significantly associated with decreased neonatal mortality (17).
The retention of knowledge and skills over time is essential in healthcare professional training and has been reported to be a challenge in limited-resource countries (18–20). A systematic review demonstrated that in four included studies, there was no or only a limited drop in knowledge and skills after a refresher newborn resuscitation training over a period between nine months and two years (21). Currently, there is limited evidence of the impact of sustained knowledge and skills as well as the frequency of repeated training and knowledge in resource-limited settings. To address this gap, we explored a strategy to improve the training of healthcare professionals in neonatal resuscitation.
In 2013, with the proposal of the ‘Belt and Road Initiative', China made a commitment to provide training opportunities to 100,000 professionals in Asian and African countries (22). Initial discussions with officials in Zanzibar revealed a need for neonatal resuscitation training (NRT) for medical and nursing staff because training resources were limited. Colleagues from the USA have already started projects to improve neonatal resuscitation knowledge (11). To meet the needs of the local staff and contribute to the improvement of medical training in Zanzibar, we developed and implemented a NRT programme for healthcare professionals in Zanzibar, Tanzania.
The aim of this study was to evaluate a NRT programme for healthcare professionals in Zanzibar. Specifically, the objective was to evaluate the acquisition and retention of healthcare professionals' neonatal resuscitation knowledge and skills.
Materials and Methods
The study used a pre-post intervention design. The NRT was implemented in Zanzibar, Tanzania, over a 2-day period in September 2017, and nine months later, 2 days of refresher training was repeated in June 2018. Data were collected before and after the training sessions in 2017 and 2018, respectively.
Setting
The study was conducted in the 510-bed Mnazi-Mmoja Hospital on the island of Zanzibar in Tanzania. This tertiary teaching hospital serves a population of nearly 1.4 million. This publicly funded hospital includes a pediatric department with a neonatal department with a 30-bed capacity.
Participants and Recruitment
Study participants were selected by the Zanzibar Ministry of Health. Participants were eligible if they were healthcare staff who voluntarily wanted to participate in the NRT and were able to follow the full training days. In total, 23 professionals from three health sectors participated in both NRT programmes delivered in 2017 and 2018: 14 participants from Mnazi-Mmoja Hospital (three neonatal physicians, five neonatal nurses, six mid-wives), five participants from Makunduchi Primary Healthcare Center (two nurses and three physicians), and four participants from Kivunge Primary Healthcare Center (two physicians and two administrators).
Neonatal Resuscitation Training
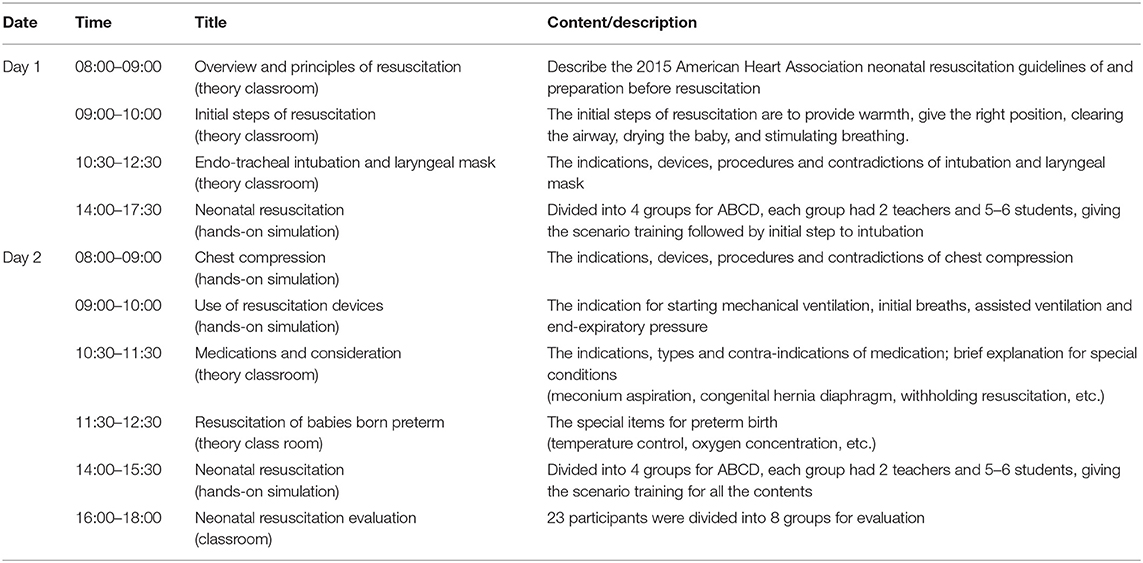
The NRT consisted of theory and hands-on simulation sessions. The training was designed and provided by five neonatal experts with English proficiency from Hunan Children's Hospital in China after exploring the participants' needs and the standard neonatal resuscitation protocols in Zanzibar. The training was based on the American Heart Association guidelines (23, 24). The curriculum of the 2-day training used in 2017 and 2018 is presented in Table 1. The hands-on simulation sessions used a trainer-trainee ratio of 1:5. The same curriculum of the NRT was provided to the same 23 participants in 2017 and 2018. All materials were provided in English, including course materials, handouts, and checklists. Two Kiswahili interpreters supported the 2-day training sessions to assure effective communication. The Chinese trainers were five neonatal physicians who were trained and authorized by the Chinese National Neonatal Resuscitation Program.
Data Collection
Prior to training, each participant completed a demographic questionnaire in 2017 collecting the participants' characteristics: gender, working experience in years, and profession. The knowledge questionnaire and the skills assessment form were designed and validated by 10 neonatal physicians certified by the Chinese National Neonatal Resuscitation Program linked to the Resuscitation Guidelines of the American Heart Association. The questionnaire and assessment form have been used previously in other medical settings in limited-resource countries. These forms were discussed and agreed upon by our colleagues in Zanzibar.
Knowledge was tested by a self-designed questionnaire (Supplementary Material 1). The test included 11 multiple choice questions (only one answer was correct out of the four answer options) related to general knowledge of neonatal resuscitation. For any correct answer, a score of 2 points was given. The total score range of the questionnaire was 0–22.
The skill performance assessment form consisted of six domains with a total of 25 observation items assessing resuscitation procedures (Supplementary Material 2). Every correctly performed item received two points. The total score of the skills assessment was 50 points. Trainers assessed the participant's behavior and completed the skills performance assessment form.
Data were collected by the five trainers who were certified neonatal resuscitation trainers. The five trainers were the same physicians in 2017 and 2018. Each participant completed the knowledge test pre- and post-training in both years. The skills were assessed in a session after the hand-on simulation training.
Data Analysis
Data were analyzed using IBM SPSS version 25.0. Participants' characteristics were descriptively analyzed using frequencies. The item scores of the knowledge questionnaire were calculated and presented as the mean and standard deviation (SD). When comparing the pre- and post-knowledge item scores, the frequency (%) of the total participants with correct answers was calculated, and an independent sample t-test was used. The chi square test and Fisher's exact test were used to evaluate the differences in knowledge in the 2-year period. Finally, the independent sample t-test was used to analyse the domains of neonatal resuscitation skill performance in 2017 and 2018.
Ethics
This study was approved by the Medical Ethics Committee of Hunan Children's Hospital (HCHLL-2018-03). The training programme was supported by the Zanzibar Ministry of Health. The study participants received the study procedures, including neonatal resuscitation training details and questionnaires, before the training. Informed consent was obtained by the participants via verbal informed consent, as written consent was waived by the Medical Ethics Committee of Medical Ethics Committee of Hunan Children's Hospital. All methods were performed in accordance with the relevant guidelines and regulations, including the Declaration of Helsinki.
Results
In total, 23 participants completed both training programmes in 2017 and 2018. Of these, 18 were female, and their professions were physicians (n = 8), nurses (n = 13), and hospital administrators (n = 2). Work experiences were 1 year (n = 10), 2 years (n = 3), 3 years (n = 7), and 4 years (n = 3).
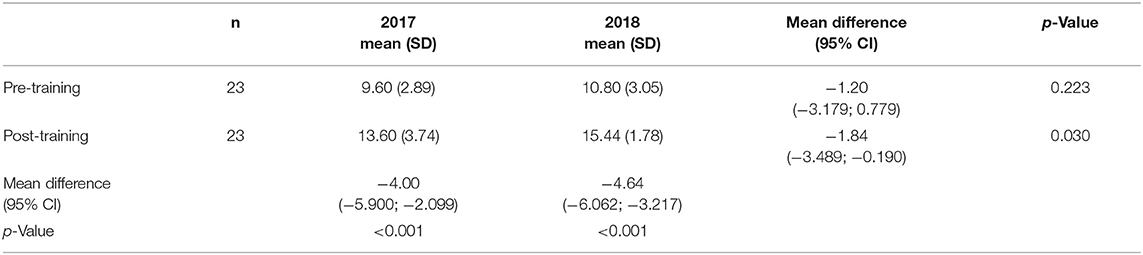
Knowledge was tested before and after both training sessions in 2017 and 2018. In 2017, the mean knowledge scores increased from 9.60 to 13.60 (mean difference −4.00, 95% CI: −5.900; −2.099, p < 0.001), and in 2018, the scores increased from 10.80 to 15.44 (mean difference −4.64, 95% CI: −6.062; −3.217, p < 0.001). Over time, the mean difference in the knowledge scores post-training in 2017 was 13.60 and in 2018 was 15.44 (mean difference −1.84, 95% CI: −3.489; −0.190, p = 0.030) (Table 2).
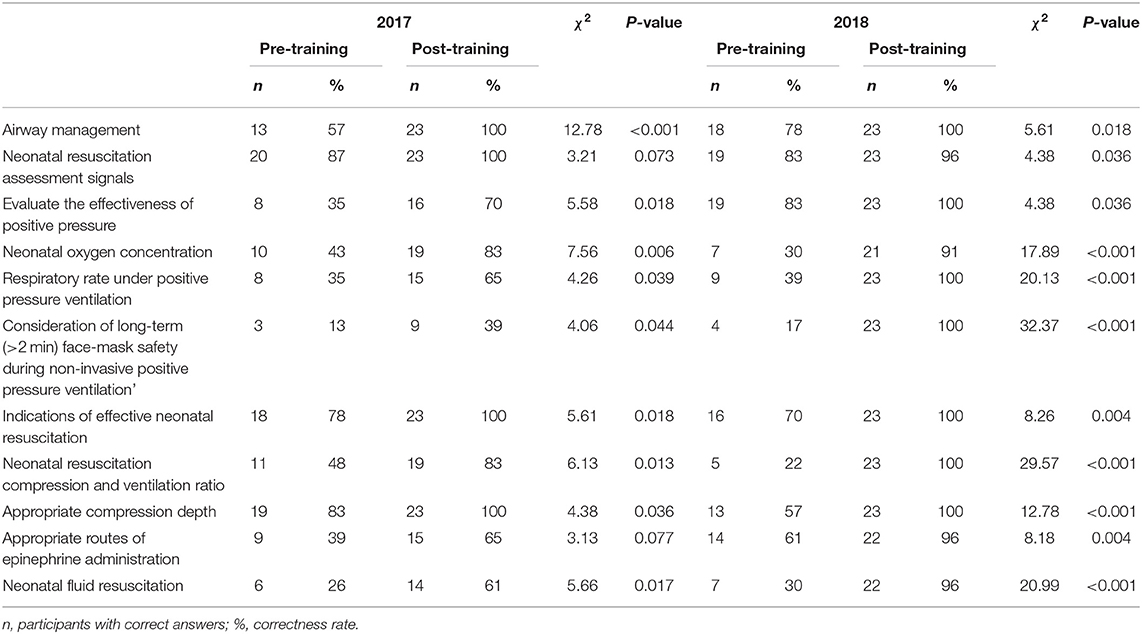
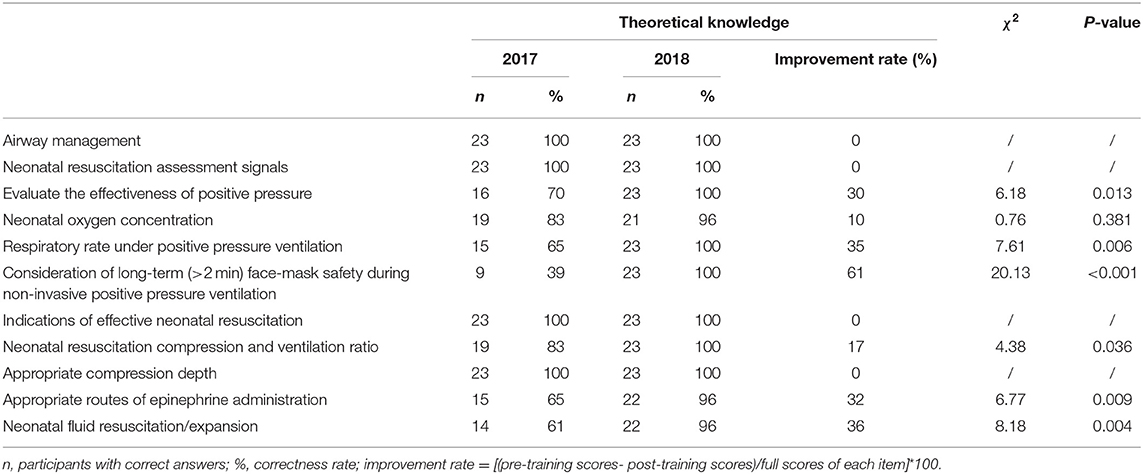
The correct answer ratios and the improvement ratios of the knowledge tests pre- and post-training at the two time points were analyzed. All knowledge items improved from pre- to post-training (Table 3). Over time, the knowledge of four items was sustained at 100%: neonatal resuscitation assessment signals, evaluation of the effectiveness of positive pressure, indications of effective neonatal resuscitation, and appropriate compression depth (Table 4). The correct response to the question on “Consideration of long-term (>2 min) face-mask safety during non-invasive positive pressure ventilation” increased from 13% to 39% in 2017 and from 17% to 100% in 2018 (Table 4). This indicated an improvement of 61% over time (p < 0.001).
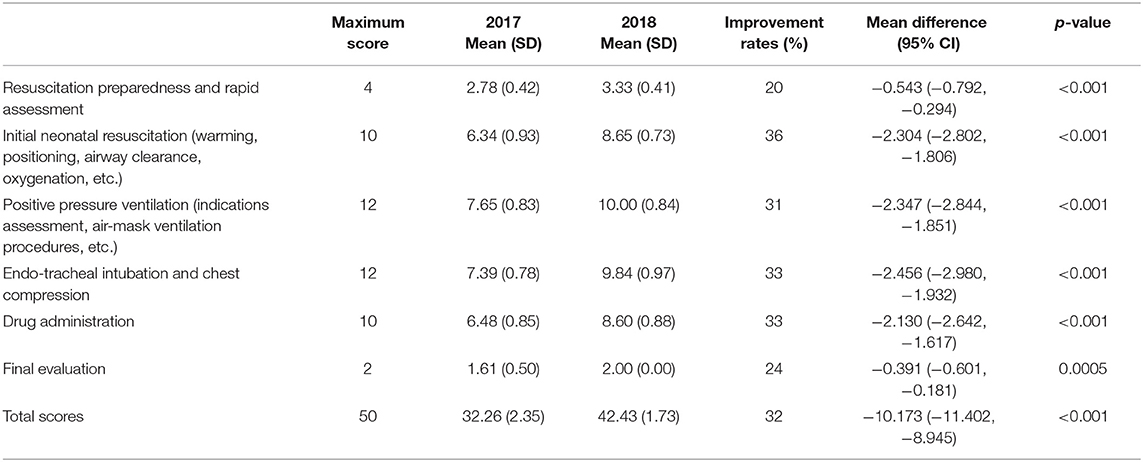
Table 5 presents the scores of the participants' skill performance after the theoretical and hands-on training. Overall, the total mean scores of the six domains increased from 32.26 (SD = 2.35) in 2017 to 42.43 (SD = 1.73) in 2018 (Table 5). Improvement ratios increased most in the domains: initial neonatal resuscitation (36%), endotracheal intubation and chest compression (33%), and drug administration (33%).
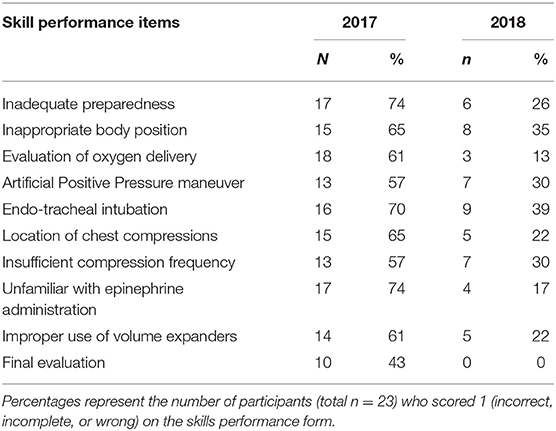
Table 6 presents the 10 key items of inadequate neonatal resuscitation skills in 2017 and 2018. In 2017, 74% of the participants showed poor performance on aspects of “inadequate preparedness” and “unfamiliar with epinephrine administration”, 70% of the participants failed in “endotracheal intubation”, and 65% of the participants failed in the “inappropriate body position” and “location of chest compressions”. However, “endotracheal intubation” and “inappropriate body position” remained common items affecting resuscitation skills in 2018, but these declined to 39% and 35%, respectively.
Discussion
We evaluated the implementation of a NRT programme in the resource-limited setting of Zanzibar and assessed the acquisition and sustainability of neonatal resuscitation competencies among healthcare professionals. Theoretical knowledge and skills performance improved in most categories, which supports the effect of neonatal training over a two-year period. The post-training scores of theoretical knowledge and skill performance in 2018 were higher than those in 2017. This indicates that refresher courses might improve knowledge compared to one course only. Studies from other resource-limited countries, such as Bangladesh and Ethiopia, reported that improvements in knowledge and skills were observed at 1 year and 18 months after newborn health training, respectively (25, 26). Our results are consistent with those of Bang et al. and Drake et al. who documented that ongoing training programmes are more effective and necessitated, as these can improve knowledge and skill retention, especially in resource-limited countries (22, 27). A pre- and post-intervention study testing a long-term newborn training programme in Somalia over a two-and-a-half-year period (including an 18-month follow-up) demonstrated that some skills did not improve (28). Issues such as hand hygiene and discharge education did not improve over time, and the authors suggested that different training approaches were needed to address the local needs. Developing and implementing training in resource-limited settings remains a challenge and should be coordinated collaboratively with colleagues outside these settings.
The interval between the two NRT sessions in our study was nine months. Despite the paucity of evidence for an optimal resuscitation training interval, effective strategies for teaching, assessing, and maintaining knowledge and skills are recommended (29, 30). A recent systematic review looking at the effectiveness of neonatal simulation sessions demonstrated that the long-term retention of skills is related to training time and duration (31). However, the effects of high-fidelity simulation training of healthcare professional skills in real life situations has not yet been demonstrated by rigorous randomized controlled trials (31, 32).
Our study indicated that several competencies in neonatal resuscitation are difficult to maintain over time by healthcare professionals. Hence, we revised and adjusted the training content based on the local practical context and the needs of the local healthcare professionals. The results indicate that ongoing support is needed for local healthcare professionals' skills and work collaboratively together to reach the Sustainable Development Goals in 2030 (5). The main causes of neonatal deaths are prematurity, asphyxia, and sepsis (33, 34). A pre- and post-experimental study of the NRT programme may not directly lead to a decrease in neonatal death. However, full competence and proficiency in neonatal resuscitation might contribute to decreased neonatal mortality and neonatal asphyxia (32, 35).
Neonatal care and resuscitation in Zanzibar have received increasing attention from healthcare professionals from other countries, such as the USA, in delivering the Helping Babies Breathe (HBB) programme to midwives (36). The HBB programme has been implemented with a limited budget and the knowledge and skills of midwives retained over a 6-month post-training time. Our initiative contributed to the knowledge and skills of several different healthcare professionals from different healthcare settings in Zanzibar. It is indeed important to establish a long-term relationship among international colleagues and experts in neonatal resuscitation to work collaboratively toward the target of the Every Newborn Action Plan of the Sustainable Development Goals trying to reduce neonatal mortality to 10 or less per 1,000 live births by 2035 (37). Therefore, successful neonatal resuscitation training programme need to focus on the sustainability of competence and translate the generated knowledge into clinical practice to tackle medical problems and reduce neonatal mortality and morbidity (38). An example is the recently tested Rapid Feedback for quality Improvement in Neonatal rEsuscitation (REFINE) initiative in Nepal to improve resuscitation competencies using the HBB programme (39). This programme is designed with a combination of theory and simulation sessions with real-time feedback via a high-fidelity neonatal mannequin. With our experience in providing the NRT in Zanzibar, we propose that an effective NRT in resource-limited healthcare settings should be developed by exploring local needs and continuing with refresher training sessions and a train-the-trainer programme.
Limitation
Our study has several limitations to address. First, our sample of 23 healthcare professionals was small, reducing the generalizability of our findings. Second, we did not collect participants' previous resuscitation experiences and skills that might have influenced the training outcomes. Third, the language barrier might have caused ineffective communication during the courses. Although native speakers facilitated the training, the participants might not have immediately understood relevant statements or instructions by the trainers. This could have led to the loss of potential useful information affecting the evaluation data. Finally, the interval between the first NRT and the refresher training was nine months, which can be considered long. Shorter intervals are recommended. Monthly, quarterly and bi-annual resuscitation refresher courses have been demonstrated to be more effective than longer intervals (40).
Conclusion
Our study demonstrated overall progress and retention of knowledge and skills in neonatal resuscitation training among a small group of pediatric healthcare professionals from resource-limited settings. Continuous neonatal resuscitation training based on the local conditions and participants' needs has been effective and essential for professionals in Zanzibar. Hence, future research should focus on the short-term and long-term effectiveness of a NRT, including the health outcomes of newborns. Ideally, these studies need to include factors that influence infant mortality, such as prematurity, sepsis, birth asphyxia, and malnutrition. Collaborations between pediatric healthcare professionals and governmental support to improve the competencies of neonatal resuscitation performance will benefit the medical staff, infants, and parents, through both a NRT and training of neonatal health promotion and management. These combined efforts might contribute to reaching the Sustainable Development Goals in reducing neonatal mortality to at least 12 per 1,000 live births.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
This study was approved by Medical Ethics Committee of Hunan Children's Hospital (HCHLL-2018-03). Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
XD, LW, MIM, YH, JQ, SL, MZ, LZ, and JML contributed to the design of the study. XD, MIM, JQ, SL, and MZ contributed to the data collection. XD, YH, and JML contributed to the data analysis. XD and JML drafted the first manuscript. LW, MIM, YH, JQ, SL, and LZ provided revisions. All authors contributed to manuscript revision, read, and approved the submitted version.
Funding
This study is funded by a grant from China Hunan Provincial Science and Technology Department (2018WK2062 and 2020WK2021) and partially funded by Resource Development Cooperation Programs in the Framework of China's Foreign Aid Project (2017D1582 and 2018D0188).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We would like to thank the participants, facilitators and trainers. The authors acknowledge the support provided by the Ministry of Commerce of the People's Republic of China, the Consul General of People's Republic of China in Zanzibar, and Ministry of Health in Zanzibar, Tanzania.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2021.693583/full#supplementary-material
References
1. Shiffman J. Issue attention in global health: the case of newborn survival. Lancet. (2010) 375:2045–2049. doi: 10.1016/S0140-6736(10)60710-6
2. Oestergaard MZ, Inoue M, Yoshida S, Mahanani WR, Gore FM, Cousenset S, et al. United Nations Inter-Agency Group for Child Mortality Estimation and the Child Health Epidemiology Reference Group. Neonatal mortality levels for 193 countries in 2009 with trends since 1990: a systematic analysis of progress, projections, and priorities. PLoS Med. (2011) 8:e1001080. doi: 10.1371/journal.pmed.1001080
3. World Health Organization. (2020). Newborns: Improving Survival And Well-Being. Available online at: https://www.who.int/news-room/fact-sheets/detail/newborns-reducing-mortality (accessed, April 4, 2021).
4. Drake M, Bishanga DR, Temu A, Njozi M, Thomas E, Mponzi V, et al. Structured on-the-job training to improve retention of newborn resuscitation skills: a national cohort helping babies breathe study in Tanzania. BMC Pediatr. (2019) 19:51. doi: 10.1186/s12887-019-1419-5
5. Liu L, Johnson HL, Cousens S, Perin J, Scott S, Lawn JE, et al. Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet. (2012) 379:2151–61. doi: 10.1016/S0140-6736(12)61878-9
6. World Health Organization. (2020). Sustainable Development Goal 3: Health. Available online at: www.who.int/topics/sustainable-development-goals/targets/en/ (accessed, April 4, 2021).
7. Wang YP, Liang WJ, Yang HW, Cao G, Fan XD, Jin N, et al. Ideology and practice of development assistance for health in China. Chin J Health Policy. (2015) 8:37–43. doi: 10.3969/j.issn.1674-2982.2015.05.007
8. Sousa S, Mielke JG. Does resuscitation training reduce neonatal deaths in low-resource communities? a systematic review of the literature. Asia Pac J Public Health. (2015) 27:690–704. doi: 10.1177/1010539515603447
9. Moshiro R, Mdoe P, Perlman JM. A global view of neonatal asphyxia and resuscitation. Front Pediatr. (2019) 7:489. doi: 10.3389/fped.2019.00489
10. Msemo G, Massawe A, Mmbando D, Rusibamayila N, Manji K, Kidanto HL, et al. Newborn mortality and fresh stillbirth rates in Tanzania after helping babies breathe training. Pediatrics. (2013);131:e353–60. doi: 10.1542/peds.2012-1795
11. Wilson GM, Ame AM, Khatib MM, Rende EK, Hartman AM, Blood SJ. Helping babies breathe implementation in Zanzibar, Tanzania. Int J Nurs Pract. (2017) 23:e12561. doi: 10.1111/ijn.12561
12. Mrisho M, Schellenberg D, Manzi F, Tanner M, Mshinda H, Shirima K, et al. Neonatal deaths in rural southern Tanzania: care-seeking and causes of death. ISRN Pediatr. (2012) 2012:953401. doi: 10.5402/2012/953401
13. Pammi M, Dempsey EM, Ryan CA, Barrington KJ. Newborn resuscitation training programmes reduce early neonatal mortality. Neonatology. (2016);110:210–24. doi: 10.1159/000443875
14. Vail B, Spindler H, Morgan MC, Cohen SR, Christmas A, Sah P, et al. Care of the mother-infant dyad: a novel approach to conducting and evaluating neonatal resuscitation simulation training in Bihar, India. BMC Pregnancy Childbirth. (2017) 17:252. doi: 10.1186/s12884-017-1434-1
15. Makene CL, Plotkin M, Currie S, Bishanga D, Ugwi P, Louis H, et al. Improvements in newborn care and newborn resuscitation following a quality improvement program at scale: results from a before and after study in Tanzania. BMC Pregnancy Childbirth. (2014) 14:381. doi: 10.1186/s12884-014-0381-3
16. Arlington L, Kairuki AK, Isangula KG, Meda RA, Thomas E, Temu A, et al. Implementation of “Helping Babies Breathe”: a 3-year experience in Tanzania. Pediatrics. (2017) 139:e20162132. doi: 10.1542/peds.2016-2132
17. Singh K, Brodish P, Suchindran C. A regional multilevel analysis: can skilled birth attendants uniformly decrease neonatal mortality? Matern Child Health J. (2014) 18:242–249. doi: 10.1007/s10995-013-1260-7
18. Zhao Y, Hu Y, Liang J, Xu Q. A pilot study on the simulation-based training for Ethiopia skilled birth attendants. Nurse Educ Pract. (2019) 34:130–138. doi: 10.1016/j.nepr.2018.12.001
19. Woods J, Gagliardi L, Nara S, Phally S, Varang O, Viphouet N, et al. An innovative approach to in-service training of maternal health staff in Cambodian hospitals. Int J Gynaecol Obstet. (2015) 129:178–83. doi: 10.1016/j.ijgo.2014.10.034
20. Eblovi D, Kelly P, Afua G, Agyapong S, Dante S, Pellerite M. Retention and use of newborn resuscitation skills following a series of helping babies breathe trainings for midwives in rural Ghana. Glob Health Action. (2017) 10:1387985. doi: 10.1080/16549716.2017.1387985
21. Reisman J, Arlington L, Jensen L, Louis H, Suarez-Rebling D, Nelson BD. Newborn resuscitation training in resource-limited settings: A systematic literature review. Pediatrics. (2016) 138:e20154490. doi: 10.1542/peds.2015-4490
22. Fan XD, Wang YP, Yang HW, Lu LH, Jin N. Health human resource development cooperation in China's foreign aid: situation analysis and improvement strategies. Chin J Health Policy. (2017) 10:68–75. doi: 10.3969/j.issn.1674-2982.2017.08.013
23. Wyckoff MH, Aziz K, Escobedo MB, Kapadia VS, Kattwinkel J, Perlman JM, et al. Part 13: neonatal resuscitation: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. (2015) 132:S543–60. doi: 10.1161/CIR.0000000000000267
24. Ye HM, Yu RJ, Wang DH, Feng Q, Wang LX, Jian M, et al. Chinese neonatal resuscitation guideline. Chin J Appl Clin Pediatr. (2017) 32:1058–1062. doi: 10.3760/cma.j.issn.2095-428X.2017.14.005
25. Gobezayehu AG, Mohammed H, Dynes MM, Desta BF, Barry D, Aklilu Y, et al. Knowledge and skills retention among frontline health workers: community maternal and newborn health training in rural Ethiopia. J Midwifery Womens Health. (2014) 59 :S21–31. doi: 10.1111/jmwh.12146
26. Dynes M, Rahman A, Beck D, Moran A, Rahman A, Pervin J, et al. Home-based life saving skills in Matlab, Bangladesh: a process evaluation of a community-based maternal child health programme. Midwifery. (2011) 27:15–22. doi: 10.1016/j.midw.2009.07.009
27. Bang A, Patel A, Bellad R, Gisore P, Goudar SS, Esamai F, et al. Helping Babies Breathe (HBB) training: what happens to knowledge and skills over time? BMC Pregnancy and Childbirth. (2016) 16:364. doi: 10.1186/s12884-016-1141-3
28. Amsalu R, Morris CN, Hynes M, Had HJ, Seriki JA, Meehan K, et al. Effectiveness of clinical training on improving essential newborn care practices in Bossaso, Somalia: a pre and post intervention study. BMC Pediatr. (2020) 20:215. doi: 10.1186/s12887-020-02120-x
29. Chaudhury S, Arlington L, Shelby B, Kairuki AK, Meda AR, Isangula KG, et al. Cost analysis of large-scale implementation of the 'Helping Babies Breathe' newborn resuscitation-training program in Tanzania. BMC Health Serv Res. (2016) 16:681. doi: 10.1186/s12913-016-1924-2
30. Yoon HB, Shin JS, Bouphavanh K, Kang YM. Evaluation of a continuing professional development training program for physicians and physician assistants in hospitals in Laos based on the Kirkpatrick model. J Educ Eval Health Prof . (2016) 13:21. doi: 10.3352/jeehp.2016.13.21
31. Huang J, Tang Y, Tang J, Shi J, Wang H, Xiong T, et al. Educational efficacy of high-fidelity simulation in neonatal resuscitation training: a systematic review and meta-analysis. BMC Med Educ. (2019) 19:323. doi: 10.1186/s12909-019-1763-z
32. Patel A, Khatib MN, Kurhe K, Bhargava S, Bang A. Impact of neonatal resuscitation trainings on neonatal and perinatal mortality: a systematic review and meta-analysis. BMJ Paediatr Open. (2017) 1:e000183. doi: 10.1136/bmjpo-2017-000183
33. Muhe LM, McClure EM, Nigussie AK, Mekasha A, Worku B, Worku A, et al. Major causes of death in preterm infants in selected hospitals in Ethiopia (SIP): a prospective, cross-sectional, observational study. Lancet Glob Health. (2019) 7:e1130–38. doi: 10.1016/S2214-109X(19)30220-7
34. Owais A, Faruque AS, Das SK, Ahmed S, Rahman S, Stein AD. Maternal and antenatal risk factors for stillbirths and neonatal mortality in rural Bangladesh: a case-control study. PLoS ONE. (2013) 8:e80164. doi: 10.1371/journal.pone.0080164
35. Tan W, Ding XP, Zhou JL, Liu H, Zhu FY, Tang WY, et al. Clinical effectiveness evaluation of Neonatal Resuscitation Procedure. Chin J Neonatology. (2013) 28:37–43. doi: 10.3969/j.issn.1673-6710.2013.04.011
36. Wilson GM, Ame AM, Khatib MM, Khalfan BS, Thompson J, Blood-Siegfried J. Helping Babies Breathe (2nd edition) implementation on a shoestring budget in Zanzibar, Tanzania. Matern Health Neonatol Perinatol. (2020) 6:3. doi: 10.1186/s40748-020-00117-z
37. Day LT, Ruysen H, Gordeev VS, Gore-Langton GR, Boggs D, Cousens S, et al. “Every Newborn-BIRTH” protocol: observational study validating indicators for coverage and quality of maternal and newborn health care in Bangladesh, Nepal and Tanzania. J Glob Health. (2019) 9:010902. doi: 10.7189/jogh.09.010902
38. Kc A, Wrammert J, Nelin V, Clark RB, Ewald U, Peterson S, et al. Evaluation of Helping Babies Breathe Quality Improvement Cycle (HBB-QIC) on retention of neonatal resuscitation skills six months after training in Nepal. BMC Pediatr. (2017) 17:103. doi: 10.1186/s12887-017-0853-5
39. Gurung R, Gurung A, Basnet O, Eilevstjønn J, Myklebust H, Girnary S, et al. REFINE (Rapid Feedback for quality Improvement in Neonatal rEsuscitation): an observational study of neonatal resuscitation training and practice in a tertiary hospital in Nepal. BMC Pregnancy Childbirth. (2020) 20:756. doi: 10.1186/s12884-020-03456-z
Keywords: newborn, neonatal resuscitation, training, knowledge, skills, healthcare professionals, mortality
Citation: Ding X, Wang L, Msellem MI, Hu Y, Qiu J, Liu S, Zhang M, Zhu L and Latour JM (2021) Evaluation of a Neonatal Resuscitation Training Programme for Healthcare Professionals in Zanzibar, Tanzania: A Pre-post Intervention Study. Front. Pediatr. 9:693583. doi: 10.3389/fped.2021.693583
Received: 11 April 2021; Accepted: 03 June 2021;
Published: 28 June 2021.
Edited by:
Paolo Biban, Integrated University Hospital Verona, ItalyReviewed by:
Yee Hui Mok, KK Women's and Children's Hospital, SingaporePeter Paul Roeleveld, Leiden University Medical Center, Netherlands
Copyright © 2021 Ding, Wang, Msellem, Hu, Qiu, Liu, Zhang, Zhu and Latour. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lihui Zhu, ODc3ODQ1Mzc1QHFxLmNvbQ==
 Xiang Ding1
Xiang Ding1 Lihui Zhu
Lihui Zhu Jos M. Latour
Jos M. Latour