- 1Division of Pediatric Infectious Disease, Department of Pediatrics, Kaohsiung Medical University Hospital, Kaohsiung, Taiwan
- 2Division of Pediatric Cardio-Pulmonology, Department of Pediatrics, Kaohsiung Medical University Hospital, Kaohsiung, Taiwan
- 3Department of Pediatrics, E-Da Hospital, Kaohsiung, Taiwan
- 4School of Medicine, I-Shou University, Kaohsiung, Taiwan
- 5Department of Pediatrics, School of Medicine, College of Medicine, Kaohsiung Medical University, Kaohsiung, Taiwan
In December 2019, the first case of coronavirus disease (COVID-19) was first reported in Wuhan, China. As of March 2021, there were more than 120 million confirmed cases of COVID-19 and 2.7 million deaths. The COVID-19 mortality rate in adults is around 1–5%, and only a small proportion of children requires hospitalization and intensive care. Recently, an increasing number of COVID-19 cases in children have been associated with a new multisystem inflammatory syndrome. Its clinical features and laboratory characteristics are similar to those of Kawasaki disease (KD), KD shock syndrome, and toxic shock syndrome. However, this new disorder has some distinct clinical features and laboratory characteristics. This condition, also known as multisystem inflammatory syndrome in children (MIS-C) associated with COVID-19, has been observed mostly in Europe and the United States. This emerging phenomenon has raised the question of whether this disorder is KD triggered by SARS-CoV-2 or a syndrome characterized by multisystem inflammation that mimics KD. This narrative review is to discuss the differences between MIS-C and KD with the aim of increasing pediatricians' awareness of this new condition and guide them in the process of differential diagnosis.
Introduction
In December 2019, the first case of coronavirus disease (COVID-19), caused by the novel human coronavirus severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was first reported in Wuhan, Hubei province, China (1). It rapidly spread to more than 215 countries, including those in Asia, Europe, North America, and South America and has become an emergent health crisis globally. The outbreak of COVID-19 worldwide had been declared as a pandemic. As of March 28, 2021, there were more than 120 million confirmed cases of COVID-19 and 2.7 million deaths. The clinical manifestations of COVID-19 range from asymptomatic to severe pneumonia, respiratory failure, acute respiratory distress syndrome, and fatal outcomes. A systemic review of all COVID-19 literatures published between January 1, 2020 and March 18, 2020, demonstrated that only 1–5% COVID-19 cases have been reported in children (2). The prevalence of laboratory-confirmed COVID-19 cases in children younger than 15 years reported to The European Surveillance System is only 2.1% (3). Compared with adults with COVID-19, children with COVID-19 present milder symptoms and less mortality. Among the 171 laboratory-confirmed COVID-19 pediatric patients treated at Wuhan Children's Hospital, only 1.7% pediatric patients received intensive care support or mechanical ventilation (4). In a large scale study of pediatric COVID-19, only 5.9% of them had hypoxemia, compared with adults with COVID-19 (18.5%), and 0.6% had a life-threatening condition (5).
Recently, a new syndrome characterized by a systemic inflammatory status that seems to be related with SARS-CoV-2 infection has been identified. This syndrome, also known as multisystem inflammatory syndrome in children (MIS-C), seems to significantly overlap with Kawasaki disease (6–8). Although several common symptoms are noticed in both KD and MIS-C, including skin rash, lymphadenopathy, strawberry tongue, and an elevation of inflammatory biomarkers, MIS-C demonstrates unique features. Belhadjer et al. reported the tendency of older onset, prominent gastrointestinal symptoms, and more left ventricular systolic dysfunction (6). Therefore, this narrative review is to discuss differences between MIS-C and KD, and to alert pediatricians about this emergent and aggressive disease, MIS-C, in children with COVID-19.
SARS-CoV-2 Related Multisystem Inflammatory Syndrome in Children
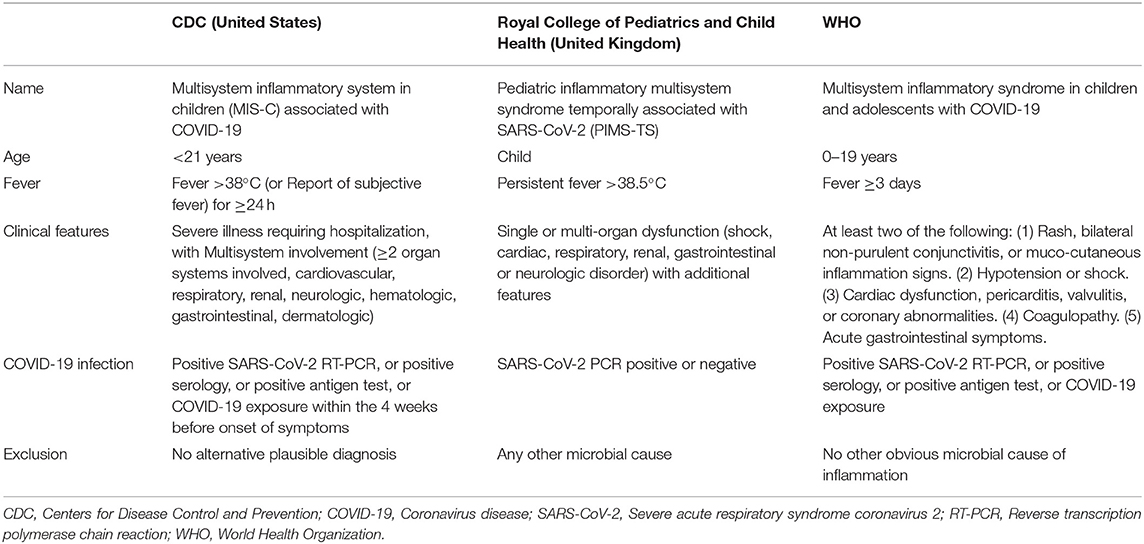
In April 2020, general practitioners in London received a warning from the National Health Service in England to be cautious of increasing numbers of children suffering from a multisystem inflammatory state with overlapping presentations of toxic shock syndrome and atypical KD (9). Despite no direct confirmation of SARS-CoV-2 or exposure history, children with COVID-19 developed fever, hypotension, severe abdominal pain, and cardiac dysfunction (10). Attention should be given to features of the cytokine storm, particularly high serum interleukin-6 levels, and patients generally require inotropic support to increase cardiac output with a rare need for extracorporeal membrane oxygenation (10). In addition, in Bergamo, Italy, KD was diagnosed in 19 children over a short period, roughly equivalent to the total number of cases previously diagnosed over 3 years in that region (8). Similarly, the French Health Minister reported that 16 children with symptoms of KD were hospitalized in Paris hospitals (11). A series of cases involving children with this condition have been reported in the UK (9), Italy (8), Spain (12), France, Switzerland (6), and the United States (13). The Center for Disease Control and Prevention of the United States has developed a case definition and has specifically named the condition MIS-C. To date, three definitions of MIS-C have been proposed, by Center for Disease Control and Prevention of the United States, the Royal College of Pediatrics and Child Health, and the World Health Organization, respectively (14–16). Although there are some discordances between these definitions (Table 1), the common characteristics are fever, evidence of inflammation, multisystem organ involvement, likely contact or evidence of SARS-CoV-2 infection, and exclusion of other microbial causes. Indeed, these definitions may overlap partial criteria for KD (17).
The geographical distribution of MIS-C cases overlaps with that of COVID-19 cases. Most MIS-C pediatric cases in New York and United Kingdom did not have direct evidence of acute COVID-19 infection (18–20). However, most of them had positive serological results, especially IgG, suggesting that MIS-C could represent a delayed immune response to SARS-CoV-2. The hypothesis that MIS-C is a post-infectious manifestation was further supported by a lag time of 4–5 weeks in the epidemic curve of COVID-19, followed by that of MIS-C (18, 21). Therefore, countries with currently ongoing COVID-19 epidemic should consider this rare but critically delayed syndrome in children.
Differences Between MIS-C and KD
Some clinical similarities between MIS-C and KD have been found. The most noteworthy common feature is febrile illness involving inflammation of the blood vessels and possible subsequent consequences of coronary artery aneurysms. In addition, patients with MIS-C may have some similar features of KD including fever, conjunctivitis, rash, and congestion of the oropharynx. However, these non-specific clinical findings could be observed in many pediatric infectious diseases. Therefore, it is unclear whether or to what extent MIS-C and KD may overlap. Indeed, these two syndromes appear to have some distinct differences, including age distribution, racial and ethnic disparities, clinical manifestations, cardiac involvement, inflammatory markers, treatment and outcome (Table 2) (18, 19, 22–25).
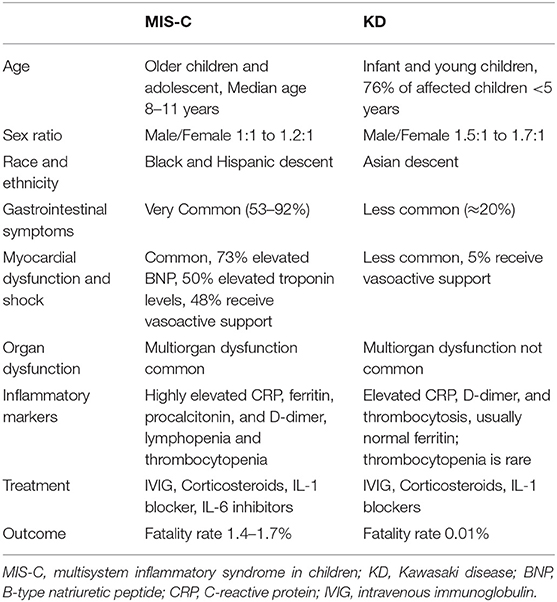
Table 2. Difference between multisystem inflammatory syndrome in children and Kawasaki disease (18, 19, 22–25).
Incidence and Epidemiology
The incidence of KD is markedly higher in East Asia, especially in Japan, Korea and Taiwan, but low in Europe and the United States. The annual incidence among children younger than 5 years old was ~240 per 100,000 in Japan and 20 per 100,000 in United States, respectively (24). While the incidence of MIS-C is uncertain, it was mostly reported in Europe (18, 26, 27) and the United States (20, 26). Intriguingly, much fewer cases had been reported in Asian countries, including Iran (28), Korea (29), and India (30). Regardless, MIS-C appears to be a relatively rare complication of COVID-19 in children. According to a study in France, the risk of MIS-C was fewer than 0.2 cases per 100,000 children (3). In addition, another report from United States shows the incidence of MIS-C about 2 per 100,000 children (18).
The epidemiology of KD has been similar worldwide for the past decades, with 50% cases occurring in children younger than 2 years, 80% case younger than 5 years, with a peak incidence at 6–11 months of age (31). There was a significantly higher incidence of KD in boys than in girls. Male patients represented 56–70% of KD patients (24, 32). This contrasts with the epidemiology of MIS-C, which usually affects older children and adolescents. In fact, age distribution in a pediatric study involving 156 MIS-C cases showed a median of 8 years and an interquartile range of 5–11 years (3). The balanced or mild male dominant sex ratio in MIS-C is also different from those observed in KD. A systemic review of 16 case series of total 655 MIS-C cases reported the male to female ratio 1.2:1 (33) and another study of total 270 MIS-C cases reported close to 1:1 (34).
KD apparently shows a predilection in Asian ancestry, even with transmigration (35). A retrospective analysis of KD children in United States demonstrated annual incidence was highest among Asians and Pacific Islander (30 per 100,000), intermediate among non-Hispanic African Americans (17 per 100,000) and Hispanic (16 per 100,000), and lowest among Caucasians (12 per 100,000) (36). In contrast to KD, children of African or Hispanic descent carried higher risk of MIS-C while Asian children accounted for less cases (9). In parallel, two large studies of MIS-C in the US demonstrated that 25–40 percent of patients were black, 31–36% Hispanic and 5% Asian (19, 37). To date, no cases of MIS-C have been reported in China and Japan (38). Thus, the underlying genetic discrepancy might be a factor resulting in these epidemiologic differences.
Physiopathology
KD is an acute self-limited systemic vasculitis. The physiopathology is unclear but is considered to be associated with exposure of a genetically pre-disposed child to an unknown infectious agent (24). This exposure may trigger abnormal immune reactions, leading to increased Th1/Th17-related immunity and a Treg/Th17 imbalance, which ultimately results in the release of large amounts of proinflammatory cytokines and systemic inflammation in all the medium-sized arteries and in multiple organs and tissues (35).
The physiopathology of MIS-C is also not well-understood, but it appears to be a consequence of massive release of inflammatory mediators with exaggerated activation of the immune system like cytokine storm (39). Based on the timing of the increased MIS-C cases relative to the peak of COVID-19 pandemic, post-infectious process is suggested (18, 21). Recently, small bowel mucosal biopsy from a COVID-19 patient with vasculitis demonstrated the presence of SARS-CoV-2 in endothelial cells (40). This finding corroborates that SARS-CoV-2 infection might be a pre-requisite for the development of MIS-C. In addition, detection of autoantibodies in MIS-C patient in mucosal and cardiac tissue, endothelial cells and cytokine molecules have been reported recently (41, 42), similar to patients with KD (43). Autoantibodies engaging with Fcγ receptors on neutrophils and monocytes resulting in formation of immune complexes are probably contributing to disease pathogenesis in both MIS-C and KD (41, 42). However, the underlying mechanisms for hyperinflammation are different between KD and MIS-C. In KD, interleukin-1 (IL-1) has direct inflammatory effects on coronary endothelial cells (35), while in MIS-C, the myocardial dysfunction and higher severity of the SARS-CoV-2 infection is predominantly driven by IL-6 and IL-10 (44).
Clinical Characteristics
Fever is a universal feature in KD patients. Manifestations of oral mucositis, conjunctivitis, extremity change and polymorphous rash are seen in ~90% of cases, while cervical lymphadenopathy in ~30% and diarrhea only in ~20% (45). Shock, ventricular dysfunction and ischemic damage are rarely reported in the acute stage of KD (46). Only <3% of KD patients developed shock (47).
Compared with KD, the clinical features of MIS-C include a higher incidence of gastrointestinal symptoms, multisystem organ involvement, and relatively fewer classical KD symptoms (44). In large case series (18–20, 22, 37), most patients with MIS-C have similar clinical symptoms including fever (100%), gastrointestinal symptoms like abdominal pain, vomiting and diarrhea (53–92%), skin rashes (45–60%), conjunctivitis (29–56%), mucosal change (29–35%) and respiratory involvement (21–63%). A study of 186 MIS-C patients in the US, 71% patients have involvement of at least four organ systems (19). The most common involved organ systems are the gastrointestinal (92%), cardiovascular (80%), hematologic (76%), mucocutaneous (74%), and respiratory systems (70%). Intriguingly, most MIS-C patients present with 5 or more days of fever (78%) and about 40% of patients meet the diagnostic criteria of KD or incomplete KD (19). However, 35–50% MIS-C patients experience hypotension (18, 20), and neurologic symptoms are common. In a report of 616 patients with MIS-C, neurologic involvement was found in 20% (48). Indeed, life-threatening neurologic conditions including severe encephalopathy, stroke, Guillain-Barré syndrome, and acute fulminant cerebral edema were observed in 20 patients (3.2%).
In general, COVID-19 is a self-limited disease in children, and most studies on clinical characteristics of COVID-19 in children do not report features consistent with KD (5, 49, 50). For example, Parri et al. found that fever (>38°C) was present in only 41% of cases, while rash was present in only 3% of cases (49). Therefore, only those COVID-19 children who has prolonged fever and other features of KD should be considered as MIS-C.
Blood Markers
Systemic inflammation is characteristic laboratory finding of KD. Typical manifestations included elevation of C-reactive protein, erythrocyte sedimentation rate, leukocytosis, increased immature neutrophil and thrombocytosis. High ferritin, thrombocytopenia and high triglycerides are seen in macrophage activation syndrome, a rare complication of KD (23).
In MIS-C patients, increased inflammatory markers including C-reactive protein, procalcitonin, ferritin, and serum IL-6, are also widely observed (7, 11, 18, 19, 51, 52). High levels of erythrocyte sedimentation rate and thrombocytopenia were also common (33, 53). Compared to KD, patients with MIS-C usually have lower platelet and lymphocytes, higher ferritin and procalcitonin level (11, 18, 51, 54). MIS-C symptoms have a greater resemblance to those of macrophage activation syndrome, presenting with elevated ferritin, D-dimer, triglyceride levels, with the cytokine storm (44, 52). However, the cytokines underlying the inflammatory mechanisms appear to be distinct in MIS-C and KD. In KD, IL-1 appears to be the main mediator of coronary artery inflammation, while IL-6 and IL-8 are main mediators in MIS-C (55).
Cardiac Manifestations
In KD, the cardiac hallmark is coronary artery abnormalities (44). Coronary artery aneurysms occur in 20–25% of untreated KD children (24). Evidence of mild to moderate ventricular dysfunction, valvular regurgitation and pericardial effusion are commonly seen during the acute stage of KD. Treatment with intravenous immunoglobulin (IVIG) usually restores normal ventricular function rapidly. Shock and severe myocardial dysfunction are rare in KD (46). One study found that only 138 of 9,488 children with KD were complicated by shock (56). Increased risk of heart complications is found particularly in these KD patients with shock. For example, left ventricular systolic dysfunction was detected only in 4% of patients with KD without shock, but in 31% of KD patients with shock (57).
By contrast, cardiac complications of MIS-C are common, including myocardial dysfunction, manifested by imaging and higher B-type natriuretic peptide (BNP) and troponin levels. In fact, left ventricular dysfunction was reported in 35–100% of children with MIS-C (58). Belhadjer et al. reported that 80% of patients with MIS-C who developed acute left ventricular failure required inotropic support, 28% received extracorporeal membrane oxygenation support (6). Unlike classic KD, coronary arteries involvement was less common in MIS-C. In a case series of 503 patients with MIS-C, only 13% of them had coronary artery aneurysms (CAA) (59), and most of these CAA (93%) were mild and there were no large or giant aneurysm.
Diagnostic Criteria
With the overlapping clinical manifestations and the lack of a specific diagnostic test for either MIS-C or KD, distinguishing the two conditions in an individual patient can be challenging. Diagnosis of KD according to the criteria established by Dr. Tomisaku Kawasaki in 1967 is based on the presence of ≥5 days of fever and the presence of ≥4 of the 5 principal clinical features, bulbar conjunctivitis, oral mucous membrane changes, peripheral extremity changes, polymorphous skin rash and cervical lymphadenopathy (24). The criteria used for MIS-C case definition vary between different health agencies (Table 1). Only 25% MIS-C patients' cardiovascular manifestations fulfill criteria for KD (60) and 66% for incomplete KD (61). Thus, MIS-C appears to be a larger group of heterogeneous diseases, including SARS-CoV-2 induced cytokine storm syndrome (CSS), COVID-19 with severe inflammatory responses, and KD concurrent with SARS-CoV-2 infection (20).
Treatment
The recommended initial therapy of KD includes IVIG (2 g/kg) administered as a single infusion and oral aspirin. The use of corticosteroids has been controversial for children with KD. Systemic corticosteroid is additionally added in patients who are at high risk for IVIG resistance (24). Second dose of IVIG, high-dose pulse steroids or monoclonal antibody against TNF-α (infliximab) is considered for IVIG-resistant patients. For treatment of highly refractory KD, human IL-1 receptor antagonist (anakinra), cytotoxic agents, or rarely plasma exchange may be considered (24).
On the other hand, since without widely accepted guidelines, treatment strategies for MIS-C are similar with the standard therapy of KD, including IVIG and corticosteroids (33, 53). For refractory patients of MIS-C, monoclonal antibodies to the IL-6 receptor (tocilizumab), IL-1 receptor antagonist (anakinra), monoclonal antibody against TNF-α (infliximab) or convalescent plasma therapy have been used. In a retrospective study of 111 MIS-C patients, 65% received initial treatment with IVIG alone and 31% received IVIG plus methylprednisolone (62).
Prognosis
The prognosis of KD is better than MIS-C. The mortality rate of MIS-C is 1.7% in the US and 1.4% in Europe (33), which is much higher than 0.01% reported in children with KD in Japan (63). Timely treatment for KD patient reduces the CAAs from 20–25 to 5% or less (24). Overall, 50% of CAAs regress to normal by 1–2 years and CAA regression occurred in 75% of patients by 30 years (64). The long-term prognosis for coronary arterial aneurysm in MIS-C remains unknown but almost all patients with increased cardiac enzymes and left ventricular dysfunction had full recovery (13, 55).
Conclusions
There are both similarities and differences in the epidemiology, manifestations, treatment, and prognosis between MIS-C and KD. The genetic susceptibility resulting in KD and MIS-C remain to be determined, but it will be worthwhile to evaluate in the future. Give with the standard therapies for KD, delays or failures in the diagnosis of KD may lead to unfavorable outcomes related to coronary aneurysms. Thus, MIS-C patients should be closely observed, and correctly distinguishing these two diseases is of the utmost importance to the pediatricians caring children with COVID-19.
Author Contributions
M-SL wrote the first version, complemented by the work of Y-CL and J-HH. J-HH, C-CT, and J-RW revised and performed modifications and lapidating the final work. All authors made substantial contributions to the project, participating in all phases.
Funding
This study was funded by the Grants MOST 109-2314-B-650-010 and MOST 108-2314-B-037-072-MY3 from Ministry of Science and Technology, Taiwan; and the Grant EDPJ109037 from E-Da Hospital/I-Shou University, Kaohsiung, Taiwan.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. (2020) 382:727–33. doi: 10.1056/NEJMoa2001017
2. Ludvigsson JF. Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatr. (2020) 109:1088–95. doi: 10.1111/apa.15270
3. Belot A, Antona D, Renolleau S, Javouhey E, Hentgen V, Angoulvant F, et al. SARS-CoV-2-related paediatric inflammatory multisystem syndrome, an epidemiological study, France, 1 March to 17 May 2020. Euro Surveill. (2020) 25:2001010. doi: 10.2807/1560-7917.ES.2020.25.22.2001010
4. Lu X, Zhang L, Du H, Zhang J, Li YY, Qu J, et al. SARS-CoV-2 Infection in Children. N Engl J Med. (2020) 382:1663–5. doi: 10.1056/NEJMc2005073
5. Dong Y, Mo Xi, Hu Y, Qi X, Jiang F, Jiang Z, et al. Epidemiology of COVID-19 among children in China. Pediatrics. (2020) 145:e20200702. doi: 10.1542/peds.2020-0702
6. Belhadjer Z, Méot M, Bajolle F, Khraiche D, Legendre A, Abakka S, et al. Acute heart failure in multisystem inflammatory syndrome in children in the context of global SARS-CoV-2 pandemic. Circulation. (2020) 142:429–36. doi: 10.1161/CIRCULATIONAHA.120.048360
7. Toubiana J, Poirault C, Corsia A, Bajolle F, Fourgeaud J, Angoulvant F, et al. Kawasaki-like multisystem inflammatory syndrome in children during the covid-19 pandemic in Paris, France: prospective observational study. BMJ. (2020) 369:m2094. doi: 10.1136/bmj.m2094
8. Verdoni L, Mazza A, Gervasoni A, Martelli L, Ruggeri M, Ciuffreda M, et al. An outbreak of severe Kawasaki-like disease at the Italian epicentre of the SARS-CoV-2 epidemic: an observational cohort study. Lancet. (2020) 395:1771–8. doi: 10.1016/S0140-6736(20)31103-X395:1771-1778
9. Riphagen S, Gomez X, Gonzalez-Martinez C, Wilkinson N, Theocharis P. Hyperinflammatory shock in children during COVID-19 pandemic. Lancet. (2020) 395:1607–8. doi: 10.1016/S0140-6736(20)31094-1
10. Schroeder AR, Wilson KM, Ralston SL. COVID-19 and Kawasaki disease: finding the signal in the noise. Hosp Pediatr. (2020) 10:e1–3. doi: 10.1542/hpeds.2020-000356
11. Pouletty M, Borocco C, Ouldali N, Caseris M, Basmaci R, Lachaume N, et al. Paediatric multisystem inflammatory syndrome temporally associated with SARS-CoV-2 mimicking Kawasaki disease (Kawa-COVID-19): a multicentre cohort. Ann Rheum Dis. (2020) 79:999–1006. doi: 10.1136/annrheumdis-2020-217960
12. Cabrero-Hernández M, García-Salido A, Leoz-Gordillo I, Alonso-Cadenas JA, Gochi-Valdovinos A, González Brabin A, et al. Severe SARS-CoV-2 infection in children with suspected acute abdomen: a case series from a tertiary hospital in Spain. Pediatr Infect Dis J. (2020) 39:e195–8. doi: 10.1097/INF.0000000000002777
13. Chiotos K, Bassiri H, Behrens EM, Blatz AM, Chang J, Diorio C, et al. Multisystem inflammatory syndrome in children during the coronavirus 2019 pandemic: a case series. J Pediatric Infect Dis Soc. (2020) 9:393–8. doi: 10.1093/jpids/piaa069
14. Centers for Disease Control and Prevention. Multisystem Inflammatory Syndrome in Children Associated With Coronavirus Disease 2019. (2020). Available online at: https://emergency.cdc.gov/han/2020/han00432.asp (accessed March 28, 2021).
15. World Health Organization. Multisystem Inflammatory Syndrome in Children and Adolescents Temporally Related to COVID-19. (2020). Available online at: https://www.who.int/news-room/commentaries/detail/multisystem-inflammatory-syndrome-in-children-and-adolescents-with-covid-19 (accessed March 28, 2021)
16. Royal College of Paediatrics and Child Health. Paediatric Multisystem Inflammatory Syndrome Temporally Associated with COVID-19-Guidance for Clinicians. (2020). Available online at: https://www.rcpch.ac.uk/resources/paediatric-multisystem-inflammatory-syndrome-temporally-associated-covid-19-pims-guidance (accessed March 28, 2021)
17. Jiang L, Tang K, Levin M, Irfan O, Morris SK, Wilson K, et al. COVID-19 and multisystem inflammatory syndrome in children and adolescents. Lancet Infect Dis. (2020) 20:e276–88. doi: 10.1016/S1473-3099(20)30651-4
18. Whittaker E, Bamford A, Kenny J, Kaforou M, Jones CE, Shah P, et al. Clinical characteristics of 58 children with a pediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2. JAMA. (2020) 324:259–69. doi: 10.1001/jama.2020.10369
19. Feldstein LR, Rose EB, Horwitz SM, Collins JP, Newhams MM, Son MBF, et al. Multisystem inflammatory syndrome in U.S. children and adolescents. N Engl J Med. (2020) 38:334–46. doi: 10.1056/NEJMoa2021680
20. Godfred-Cato S, Bryant B, Leung J, Oster ME, Conklin L, Abrams J, et al. COVID-19-associated multisystem inflammatory syndrome in children—United States, March-July 2020. MMWR Morb Mortal Wkly Rep. (2020) 69:1074–80. doi: 10.15585/mmwr.mm6932e2
21. Mahase E. Covid-19: cases of inflammatory syndrome in children surge after urgent alert. BMJ. (2020) 369:m1990. doi: 10.1136/bmj.m1990
22. Davies P, Evans C, Kanthimathinathan HK, Lillie J, Brierley J, Waters G, et al. Intensive care admissions of children with paediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2 (PIMS-TS) in the UK: a multicentre observational study. Lancet Child Adolesc Health. (2020) 4:669–77. doi: 10.1016/S2352-4642(20)30215-7
23. Burns JC, Glodé MP. Kawasaki syndrome. Lancet. (2004) 364:533–44. doi: 10.1016/S0140-6736(04)16814-1
24. McCrindle BW, Rowley AH, Newburger JW, Burns JC, Bolger AF, Gewitz M, et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a scientific statement for health professionals from the American Heart Association. Circulation. (2017) 135:e927–99. doi: 10.1161/CIR.0000000000000484
25. Capone CA, Subramony A, Sweberg T, Schneider J, Shah S, Rubin L, et al. Characteristics, cardiac involvement, and outcomes of multisystem inflammatory syndrome of childhood associated with severe acute respiratory syndrome coronavirus 2 infection. J Pediatr. (2020) 224:141–5. doi: 10.1016/j.jpeds.2020.06.044
26. Radia T, Williams N, Agrawal P, Harman K, Weale J, Cook J, et al. Multi-system inflammatory syndrome in children & adolescents (MIS-C): a systematic review of clinical features and presentation. Paediatr Respir Rev. (2020). doi: 10.1016/j.prrv.2020.08.001. [Epub ahead of print].
27. Moraleda C, Serna-Pascual M, Soriano-Arandes A, Simó S, Epalza C, Santos M, et al. Multi-inflammatory syndrome in children related to SARS-CoV-2 in Spain. Clin Infect Dis. (2021) 72:e397–401. doi: 10.1093/cid/ciaa1042
28. Mamishi S, Movahedi Z, Mohammadi M, Ziaee V, Khodabandeh M, Abdolsalehi MR, et al. Multisystem inflammatory syndrome associated with SARS-CoV-2 infection in 45 children: a first report from Iran. Epidemiol Infect. (2020) 148:e196. doi: 10.1017/S095026882000196X
29. Kim H, Shim JY, Ko JH, Yang A, Shim JW, Kim DS, et al. Multisystem inflammatory syndrome in children related to COVID-19: the first case in Korea. J Korean Med Sci. (2020) 35:e391. doi: 10.3346/jkms.2020.35.e391
30. Jain S, Sen S, Lakshmivenkateshiah S, Bobhate P, Venkatesh S, Udani S, et al. Multisystem inflammatory syndrome in children with COVID-19 in Mumbai, India. Indian Pediatr. (2020) 57:1015–9. doi: 10.1007/s13312-020-2026-0
31. Nakamura Y, Yashiro M, Uehara R, Sadakane A, Chihara I, Aoyama Y, et al. Epidemiologic features of Kawasaki disease in Japan: results of the 2007-2008 nationwide survey. J Epidemiol. (2010) 20:302–7. doi: 10.2188/jea.JE20090180
32. Huang WC, Huang LM, Chang IS, Chang LY, Chiang BL, Chen PJ. Epidemiologic features of Kawasaki disease in Taiwan, 2003-2006. Pediatrics. (2009) 123:e401-5. doi: 10.1542/peds.2008-2187
33. Kaushik A, Gupta S, Sood M, Sharma S, Verma S. A systematic review of multisystem inflammatory syndrome in children associated with SARS-CoV-2 infection. Pediatr Infect Dis J. (2020) 39:e340–6. doi: 10.1097/INF.0000000000002888
34. Tang Y, Li W, Baskota M, Zhou Q, Fu Z, Luo Z, et al. Multisystem inflammatory syndrome in children during the coronavirus disease 2019 (COVID-19) pandemic: a systematic review of published case studies. Transl Pediatr. (2021) 10:121–35. doi: 10.21037/tp-20-188
35. Rife E, Gedalia A. Kawasaki disease: an update. Curr Rheumatol Rep. (2020) 22:75. doi: 10.1007/s11926-020-00941-4
36. Holman RC, Belay ED, Christensen KY, Folkema AM, Steiner CA, Schonberger LB. Hospitalizations for Kawasaki syndrome among children in the United States, 1997-2007. Pediatr Infect Dis J. (2010) 29:483–8. doi: 10.1097/INF.0b013e3181cf8705
37. Dufort EM, Koumans EH, Chow EJ, Rosenthal EM, Muse A, Rowlands J, et al. Multisystem inflammatory syndrome in children in New York state. N Engl J Med. (2020) 383:347–58. doi: 10.1056/NEJMoa2021756
38. Xu S, Chen M, Weng J. COVID-19 and Kawasaki disease in children. Pharmacol Res. (2020) 159:104951. doi: 10.1016/j.phrs.2020.104951
39. Alunno A, Carubbi F, Rodríguez-Carrio J. Storm, typhoon, cyclone or hurricane in patients with COVID-19? Beware of the same storm that has a different origin. RMD Open. (2020) 6:e001295. doi: 10.1136/rmdopen-2020-001295
40. Carnevale S, Beretta P, Morbini P. Direct endothelial damage and vasculitis due to SARS-CoV-2 in small bowel submucosa of COVID-19 patient with diarrhea. J Med Virol. (2021) 93:61–3. doi: 10.1002/jmv.26119
41. Gruber CN, Patel RS, Trachtman R, Lepow L, Amanat F, Krammer F, et al. Mapping systemic inflammation and antibody responses in multisystem inflammatory syndrome in children (MIS-C). Cell. (2020) 183:982–95.e14. doi: 10.1016/j.cell.2020.09.034
42. Consiglio CR, Cotugno N, Sardh F, Pou C, Amodio D, Rodriguez L, et al. The immunology of multisystem inflammatory syndrome in children with COVID-19. Cell. (2020) 183:968–81.e7. doi: 10.1016/j.cell.2020.09.016
43. Sakurai Y. Autoimmune aspects of Kawasaki disease. J Investig Allergol Clin Immunol. (2019) 29:251–61. doi: 10.18176/jiaci.0300
44. Shulman ST. Pediatric coronavirus disease-2019-associated multisystem inflammatory syndrome. J Pediatric Infect Dis Soc. (2020) 9:285–6. doi: 10.1093/jpids/piaa062
45. Wang CL, Wu YT, Liu CA, Kuo HC, Yang KD. Kawasaki disease: infection, immunity and genetics. Pediatr Infect Dis J. (2005) 24:998–1004. doi: 10.1097/01.inf.0000183786.70519.fa
46. Gatterre P, Oualha M, Dupic L, Iserin F, Bodemer C, Lesage F, et al. Kawasaki disease: an unexpected etiology of shock and multiple organ dysfunction syndrome. Intensive Care Med. (2012) 38:872–8. doi: 10.1007/s00134-012-2473-8
47. Kanegaye JT, Wilder MS, Molkara D, Frazer JR, Pancheri J, Tremoulet AH, et al. Recognition of a Kawasaki disease shock syndrome. Pediatrics. (2009) 123:e783-9. doi: 10.1542/peds.2008-1871
48. LaRovere KL, Riggs BJ, Poussaint TY, Young CC, Newhams MM, Maamari M, et al. Neurologic involvement in children and adolescents hospitalized in the United States for COVID-19 or multisystem inflammatory syndrome. JAMA Neurol. (2021) 78:536–47. doi: 10.1001/jamaneurol.2021.0504
49. Parri N, Lenge M, Buonsenso D. Children with Covid-19 in pediatric emergency departments in Italy. N Engl J Med. (2020) 383:187–90. doi: 10.1056/NEJMc2007617
50. Bialek S, Gierke R, Hughes M, McNamara LA, Pilishvili T, Skoff T. Coronavirus disease 2019 in children—United States, February 12-April 2, 2020. MMWR Morb Mortal Wkly Rep. (2020) 69:422–6. doi: 10.15585/mmwr.mm6914e4
51. Carlin RF, Fischer AM, Pitkowsky Z, Abel D, Sewell TB, Landau EG, et al. Discriminating multisystem inflammatory syndrome in children requiring treatment from common febrile conditions in outpatient settings. J Pediatr. (2021) 229:26–32.e2. doi: 10.1016/j.jpeds.2020.10.013
52. Samprathi M, Jayashree M. Biomarkers in COVID-19: an up-to-date review. Front Pediatr. (2021) 8:607647. doi: 10.3389/fped.2020.607647
53. Carter MJ, Shankar-Hari M, Tibby SM. Paediatric inflammatory multisystem syndrome temporally-associated with SARS-CoV-2 infection: an overview. Intensive Care Med. (2021) 47:90–3. doi: 10.1007/s00134-020-06273-2
54. Felsenstein S, Willis E, Lythgoe H, McCann L, Cleary A, Mahmood K, et al. Presentation, treatment response and short-term outcomes in paediatric multisystem inflammatory syndrome temporally associated with SARS-CoV-2 (PIMS-TS). J Clin Med. (2020) 9:3293. doi: 10.3390/jcm9103293
55. Riollano-Cruz M, Akkoyun E, Briceno-Brito E, Kowalsky S, Reed J, Posada R, et al. Multisystem inflammatory syndrome in children related to COVID-19: a New York city experience. J Med Virol. (2021) 93:424–33. doi: 10.1002/jmv.26224
56. Lin MT, Fu CM, Huang SK, Huang SC, Wu MH. Population-based study of Kawasaki disease shock syndrome in Taiwan. Pediatr Infect Dis J. (2013) 32:1384–6. doi: 10.1097/INF.0b013e31829efae6
57. Gamez-Gonzalez LB, Moribe-Quintero I, Cisneros-Castolo M, Varela-Ortiz J, Muñoz-Ramírez M, Garrido-García M, et al. Kawasaki disease shock syndrome: unique and severe subtype of Kawasaki disease. Pediatr Int. (2018) 60:781–90. doi: 10.1111/ped.13614
58. Sperotto F, Friedman KG, Son MBF, VanderPluym CJ, Newburger JW, Dionne A. Cardiac manifestations in SARS-CoV-2-associated multisystem inflammatory syndrome in children: a comprehensive review and proposed clinical approach. Eur J Pediatr. (2021) 180:307–22. doi: 10.1007/s00431-020-03766-6
59. Feldstein LR, Tenforde MW, Friedman KG, Newhams M, Rose EB, Dapul H, et al. Characteristics and outcomes of US children and adolescents with multisystem inflammatory syndrome in children (MIS-C) compared with severe acute COVID-19. JAMA. (2021) 325:1074–87. doi: 10.1001/jama.2021.2091
60. Lee PY, Day-Lewis M, Henderson LA, Friedman KG, Lo J, Roberts JE, et al. Distinct clinical and immunological features of SARS-CoV-2-induced multisystem inflammatory syndrome in children. J Clin Invest. (2020) 130:5942–50. doi: 10.1172/JCI141113
61. Diorio C, Henrickson SE, Vella LA, McNerney KO, Chase J, Burudpakdee C, et al. Multisystem inflammatory syndrome in children and COVID-19 are distinct presentations of SARS-CoV-2. J Clin Invest. (2020) 130:5967–75. doi: 10.1172/JCI140970
62. Ouldali N, Toubiana J, Antona D, Javouhey E, Madhi F, Lorrot M, et al. Association of intravenous immunoglobulins plus methylprednisolone vs. immunoglobulins alone with course of fever in multisystem inflammatory syndrome in children. JAMA. (2021) 325:855–64. doi: 10.1001/jama.2021.0694
63. Makino N, Nakamura Y, Yashiro M, Ae R, Tsuboi S, Aoyama Y, et al. Descriptive epidemiology of Kawasaki disease in Japan, 2011-2012: from the results of the 22nd nationwide survey. J Epidemiol. (2015) 25:239–45. doi: 10.2188/jea.JE20140089
Keywords: coronavirus disease 2019, multisystem inflammatory syndrome in children, pediatric multisystem inflammatory syndrome temporally associated with SARS-CoV-2, Kawasaki disease, difference
Citation: Lee M-S, Liu Y-C, Tsai C-C, Hsu J-H and Wu J-R (2021) Similarities and Differences Between COVID-19-Related Multisystem Inflammatory Syndrome in Children and Kawasaki Disease. Front. Pediatr. 9:640118. doi: 10.3389/fped.2021.640118
Received: 10 December 2020; Accepted: 19 May 2021;
Published: 18 June 2021.
Edited by:
Paolo Biban, Integrated University Hospital Verona, ItalyReviewed by:
Francesca Sperotto, Boston Children's Hospital and Harvard Medical School, United StatesNiccolò Parri, University of Florence, Italy
Copyright © 2021 Lee, Liu, Tsai, Hsu and Wu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jiunn-Ren Wu, jirewu@gmail.com; Jong-Hau Hsu, jhh936@yahoo.com.tw
 Min-Sheng Lee
Min-Sheng Lee Yi-Ching Liu2
Yi-Ching Liu2 Jong-Hau Hsu
Jong-Hau Hsu Jiunn-Ren Wu
Jiunn-Ren Wu