- Department of Pediatric Critical Care Medicine, Xinhua Hospital, Affiliated to Shanghai Jiaotong University School of Medicine, Shanghai, China
Objective: End-of-life(EOL) care decision-making for infants and children is a painful experience. The study aimed to explore the clinical factors influencing the EOL care to withhold/withdraw life-sustaining treatment (WLST) in Chinese pediatric intensive care unit (PICU).
Methods: A 14-year retrospective study (2006–2019) for pediatric patients who died in PICU was conducted. Based on the mode of death, patients were classified into WLST group (death after WLST) and fCPR group (death after full intervention, including cardiopulmonary resuscitation). Intergroup differences in the epidemiological and clinical factors were determined.
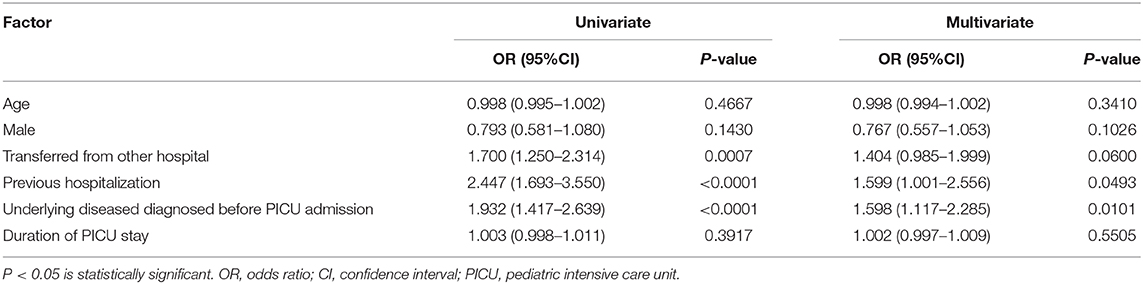
Results: There were 715 patients enrolled in this study. Of these patients, 442 (61.8%) died after WLST and 273 (38.2%) died after fCPR. Patients with previous hospitalizations or those who had been transferred from other hospitals more frequently chose WLST than fCPR (both P < 0.01), and the mean PICU stay duration was significantly longer in the WLST group (P < 0.05). WLST patients were more frequently complicated with chronic underlying disease, especially tumor (P < 0.01). Sepsis, diarrhea, and cardiac attack (all P < 0.05) were more frequent causes of death in the fCPR group, whereas tumor as a direct cause of death was more frequently seen in the WLST group. Logistic regression analysis demonstrated that previous hospitalization and underlying diseases diagnosed before admission were strongly associated with EOL care with WLST decision (OR: 1.6; P < 0.05 and OR: 1.6; P < 0.01, respectively).
Conclusions: Pediatric patients with previous hospitalization and underlying diseases diagnosed before admission were associated with the EOL care to WLST.
Introduction
Most post-neonatal pediatric intensive care unit (PICU) admissions account for majority of pediatric deaths in developed countries, especially in the United States (1, 2). However, recent technological advances in pediatric research have significantly reduced the mortality rates among PICU admissions by prolonging the life of critically ill patients (3–5). Three recent multicenter studies have reported a decline in PICU mortality rates of ~<3% in western countries (6–8). There is no official data of mortality in Chinese PICU.
Nowadays, little attention has been paid to end-of-life (EOL) care, following the ineffectiveness of therapeutic interventions. In collaborative decision-making concerning EOL care for their children, parents are given complete freedom to decide, especially in case of medical futility (9, 10). As a result, the ethical practices of withholding and withdrawing life-sustaining treatments (WLST) in children (11), have become common in PICUs in many countries (2, 12, 13). Consequently, the goals of care get redefined—to ensure support and comfort to the patient's parents rather than providing a cure, and to attend to the psychosocial needs of dying children and their families which will promote optimal EOL care, and thus facilitate a peaceful death (14, 15). Major factors have been shown to strongly influence the decision to WLST including, geographic parameters, religious and cultural beliefs, societal values, race, legal concerns, subjective evaluation of the benefits and burdens of life support, the nature of the underlying disease, the quality of life prior to hospitalization, and the expected suffering secondary to the pathology (12, 16, 17). Thus, the incidence of deaths after WLST vary worldwide (12). Several earlier studies have identified high variability in the prevalence of WLST in the ICU setting (15). Of note, substantial variability exists in WLST across world regions and countries, among individual ICUs within a country, and among individual patients within a single ICU. Moreover, the mean prevalence of deaths after WLST in patients varied from 0 to 84.1% between different studies (SD: 23.7%) whereas the mean prevalence of deaths after withholding also varied from 5.3 to 67.3% (mean: 27.3%, SD: 18.5%) (12). Earlier, studies have reported that ~28–65% of all PICU deaths follow a restriction in care in North America and Europe (11, 18). On the contrary, WLST is less common in South America and some Asian countries, and WLST cases account for ~18–50% of ICU deaths (19, 20).
Although there have been a couple of studies elucidating EOL care in Japanese PICUs (20, 21), to the best of our knowledge, there are no studies evaluating the characteristic factors associated with WLST in EOL care in Chinese PICUs. Therefore, in view of the above, we aimed to document the epidemiologic and clinical characteristics that influence the EOL care to WLST of PICU patients at one of the largest tertiary referral hospitals in China.
Methods
Study Design
This study was performed at Xinhua Hospital, Shanghai, which is one of the largest general hospital with many pediatric subspecialties in China, and is also a tertiary referral center for children with complex pediatric conditions. About 1,000–2,000 pediatric patients were admitted to the PICU every year. The PICU is a comprehensive intensive care facility engaged in the full spectrum of pediatric critical care, including medical/surgical, cardiac and trauma care. This is a 14-year retrospective study that involved post-hoc analysis of data from our previously published study (22). Pediatric patients (n = 715) from 1 month to 11 years of age who died in the PICU between 2006 and 2019 were included.
The study protocol was approved by the Ethics Committees of Xinhua Hospital, Shanghai (XHEC-D-2020-0110), and the need for written informed consent was waived by the committee as all data were used retrospectively and de-identified.
Data Collection
All data used in this study were drawn from the databases of the hospital information services department. These databases prospectively recorded demographic and clinical data of all hospitalized children. The children who died in the emergency department were not included due to incomplete medical records. Data collected included diagnoses, demographic characteristics, hospital units caring for patients, symptoms, diagnosis on PICU admission, source of PICU admission, occurrence and timing of EOL decision-making, mode of death, time and place of death, and information of patients' family members. The immediate cause of death refers to the diagnosis that predominantly and directly played a role in the pathophysiology leading to the occurrence of a life-threatening situation. An underlying chronic disease refers to any complicated chronic disease diagnosed before death. They included congenital abnormalities, immunodeficiency and/or autoimmune diseases, tumors, and other disorders, such as malnutrition, obesity, and hemophilia.
Modes of Death
Since the 1990s, WLST practices have been well-defined in literature (14, 23). We examined WLST status at death based on medical records. All deaths were classified into two groups: WLST group (death after WLST) (14) and fCPR group [death after full intervention, including cardiopulmonary resuscitation (CPR)]. Withdrawal of life-sustaining treatment was defined as discontinuing the life-sustaining intervention/treatment that was already in place. Withholding treatment was defined as the non-initiation or the decision not to escalate a life-sustaining treatment (14, 24, 25). Life-sustaining treatments included CPR, inotropic or vasoactive medication, mechanical ventilation, renal replacement therapy, and extracorporeal membrane oxygenation (ECMO).
These two decisions were made by the parents following the evaluation of patients' prognosis and/or potential quality of life after surviving a critical episode. A poor prognosis indicated an expected poor quality of life after the critical episode. Each patient was evaluated individually by a medical team (including the nurse) together with the family. In this evaluation, the presence of chronic underlying diseases, the prior quality of life, and the expected suffering secondary to the sequelae/pathology were considered. The patient's family was informed in written that the patient was in a life-threaten situation and that death would be the possible outcome. All decisions concerning the WLST status were made during the patients' PICU stay. For families that opted for WLST, Statement of Consent forms required by the standard institutional protocol were signed either by the parents /guardians prior to the procedure.
Statistical Analyses
All analyses were performed using GraphPad Prism (version 8 for Mac OS, GraphPad Software, La Jolla California USA, www.graphpad.com). Categorical data were expressed in terms of frequency and percentage, and Chi-square test was performed for comparison. Nonparametric continuous variables were expressed as median with interquartile range (IQR). For continuous data, the Mann-Whitney U-test was performed to compare variables between two groups. After conducting these bivariate analyses comparing the patient characteristics and clinical factors in WLST group and fCPR group, we then used a multiple logistic regression analysis to identify the factors that influencing EOL care. The dependent variable was EOL care as WLST. The independent variables were those showed p < 0.05 in the bivariate analysis. A P-value of < 0.05 was considered statistically significant.
Results
Basic Characteristics
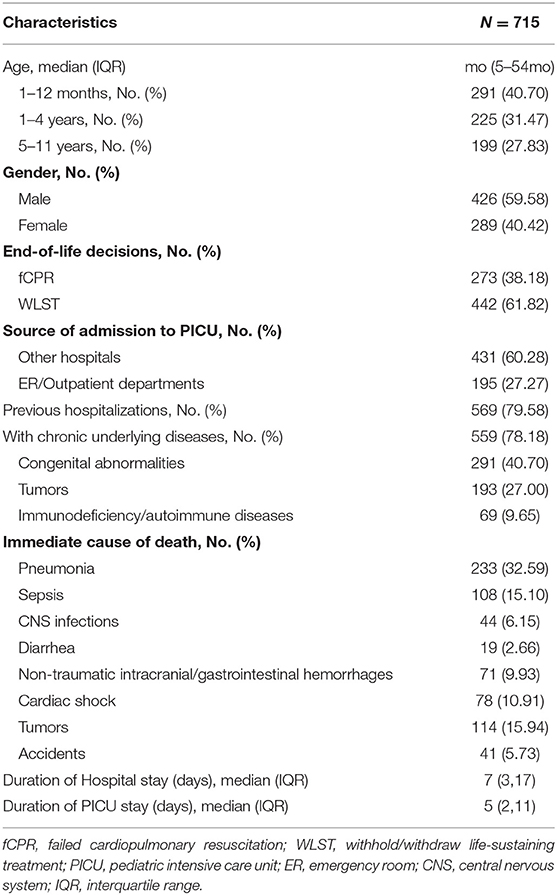
During the 14-year study period, there were a total of 715 (3.6%) patients died among the 19, 813 patients admitted to the PICU. Of these 715 patients, 442 (61.8%) died after WLST and 273 (38.2%) died after fCPR. Approximately 59.6% of pediatric patients who died were male, while 40.4% were female. The median age was 19 months (IQR: 5–54 months). In this study, 72% of the deaths occurred in children below 5 years of age, of whom 40.7% were infants. Children aged 5–11 years accounted for about 28% of the deaths (Table 1).
Clinical Factors Associated With WLST and fCPR
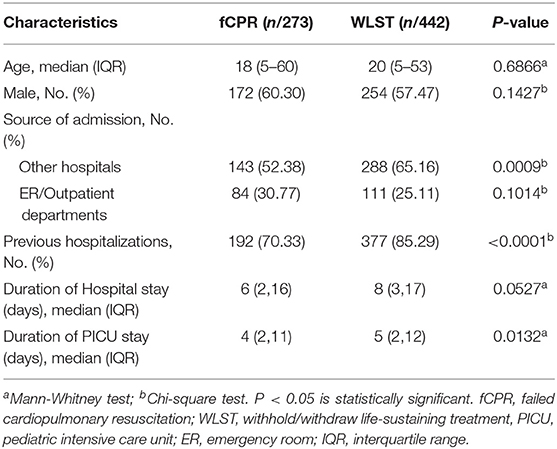
Notably, 79.6% (n = 569) of patients had a history of previous hospitalization, whereas 60.3% (n = 431) were transferred from other hospitals before admission to the PICU (Table 2). The proportion of patients who were transferred from other hospitals and those with previous hospitalizations were significantly higher in the WLST group than the fCPR group (P = 0.0009 and P < 0.0001, respectively). The lengths of hospital and PICU stays of patients in the WLST group were longer than those in the fCPR group (P = 0.0527; P = 0.0132, respectively).
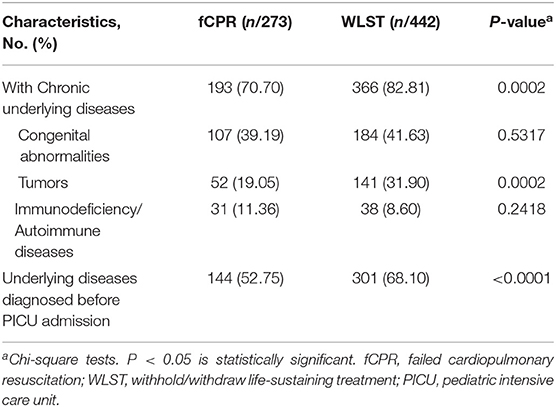
Chronic Underlying Diseases for Different EOL Care
The distribution pattern of chronic underlying diseases for different EOL care was shown in Table 3. Approximately 78.2% of patients presented with chronic underlying diseases, including congenital abnormalities (40.7%), tumors (27%), and immunodeficiency/autoimmune diseases (9.7%). The proportion of patients who had chronic underlying diseases was significantly higher in the WLST group than in the fCPR group (68.1 vs. 52.8%). The proportion of patients pre-existing chronic diseases diagnosed before PICU admission was also significantly higher in the WLST group than in the fCPR group (68.1 vs. 52.8%,). Pediatric patients in the WLST group were more likely to have tumors than patients in the fCPR group (31.9 vs. 19.1%). Although the occurrence of congenital abnormalities was more frequent than the other occurrence of chronic underlying diseases in all patients, no significant differences were observed between the two EOL care groups.
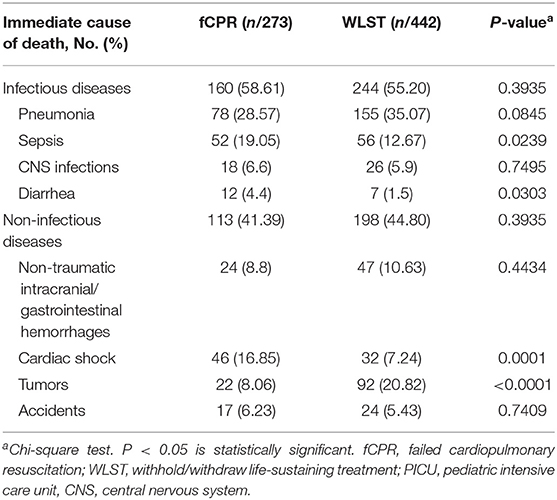
Immediate Causes of Death for Different EOL Care
The distribution of immediate causes of death for different mode of death was shown in Table 4. Infectious diseases caused the majority of the deaths in children. Patients with fCPR decision were more like to have a diagnosis of immediate cause of death as sepsis, diarrhea and cardiac attack, compared with those in the WLST group (P < 0.05). On the contrary, the patients in the WLST group were more likely to have a diagnosis of tumor as the direct cause of death when compared with those in the fCPR group (P < 0.0001).
Multivariable Analysis of Factors Associated With EOL Care
In multivariable analysis, the history of previous hospitalization and the underlying diseases diagnosed before PICU admission significantly associated with WLST decision (OR: 1.599; and OR: 1.598; respectively, Table 5). The source of admission as transferred from other hospitals tended to be an independent factor influencing the WLST decision; however, this did not reach statistical significance (P = 0.06). We selected the independent variables showing significant difference (p < 0.05) in binary analysis (Tables 2–4) for the univariable and multivariable logistic regression test. In the multiple logistic regression analysis, age and gender were remained as covariates. With chronic underlying diseases was eliminated from the model since it was related with underlying diseases diagnosed before PICU admission, while latter showed significant association with EOL care.
Discussion
Our 14-year retrospective observational study described the differences of epidemiologic and clinical characteristics of the pediatric patients with the different decisions of WLST in the PICU in one of the largest tertiary referral hospital in China. The present study showed that WLST decision was commonly associated with PICU deaths and was more frequent in patients with previous hospitalization and underlying diseases diagnosed before admission. Our findings provided a better understanding of factors influencing EOL care decisions, which could help support the decision-making for these family and health care professionals.
As highlighted previously, we found that PICU deaths accounted for most deaths within our tertiary care pediatric hospital (14). A previous study in a Japanese PICU reported the mortality rate to be ~3.3%, which was consistent with that reported in our study (3.6%). In contrast, the mortality rate reported in Western countries have been shown to be <3% (6–8). This difference could be attributed to the differences in geographic parameters, disease distribution, race, and medical systems, which could in turn influence the modes of death among or within countries (19, 26, 27).
Recent prospective, multicenter studies have reported that approximate 70 and 30% of patients died in a PICU setting following WLST and fCPR/brain death, respectively (28). Studies have also showed that a majority of deaths (60–85%) were due to the WLST (8, 26, 29). Similarly, our study found that ~62% and 38.2% of deaths occurred after WLST and fCPR, respectively. Our study findings are also in line with other recent reports from PICUs worldwide (30–32). Over the past decade, WLST decisions have become relatively acceptable in critically ill patients in China, but there is very few research in the this field in China yet.
Similar to a previous study, this study demonstrated that the incidence of deaths in patients with previous hospitalization history and that of patients who were transferred from other hospitals were significantly higher in the WLST group than in the fCPR group (33). Our study also suggested that previous history of hospitalization tend to be an independent factor of influencing WLST decision and source of admission as transferred from another hospital before PICU admission was strongly associated with WLST. These findings indicated that after children being diagnosed at another hospital, the parents of these critical-ill children sought a second opinion and/or alternate hospital to understand the severity and impact of the child's underlying condition before acknowledging the futility of further therapeutic efforts. Therefore, such families, after reaching a consensus with the healthcare professionals involved in their child's care, were more likely to choose WLST as the EOL care for their child.
The present study found that underlying chronic diseases diagnosed before PICU admission tend to be an independent factor of WLST decision. Our results were further corroborated by previous studies that showed that nearly two-thirds of all deaths in PICUs are attributable to chronic or pre-existing diagnoses (2, 31). Cancer is a known predictor for WLST (34). Moreover, parents of patients diagnosed with tumor were aware of the clinical outcome. Therefore, parents of such patients are more likely to choose WLST when treatment efforts fail to avoid prolonged suffering. The lengths of hospital and PICU stays were longer in the WLST group than in the fCPR group, similar to previously reported results (35, 36).
Our study showed that the incidence of infectious diseases was significantly higher than that of non-infectious diseases, suggesting that infectious diseases are the leading cause of death in most PICU patients. Similar to previous reports, our study demonstrated that the most common immediate causes of deaths in hospitalized children were pneumonia, tumors, sepsis, cardiac shock, non-traumatic intracranial and gastrointestinal hemorrhage (37). Although pneumonia was the most common immediate cause of death, it did not influence the EOL decision. Furthermore, the incidences of sepsis, diarrhea, and cardiac shock were significantly more common in the fCPR group than in the WLST group. In contrast, tumors were more commonly observed in the WLST group (21%) than in the fCPR group. The most plausible explanation for this could be that sepsis, diarrhea, and cardiac attack were acute diseases and often present atypical symptoms at the early stages but the conditions could deteriorate dramatically as the disease progresses. In such cases, if the circumstances of cardiac or respiratory arrest were envisaged, the family and the physician would be more willing to believe that the disease was reversible, which in turn might impede the acceptance of EOL decision until fCPR.
There are several limitations that warrant discussion. First, this study was retrospective and only included deaths that occurred at a tertiary health care facility. Second, we did not examine several patient characteristics known to influence EOL care, including family history, religion, culture, race, and socioeconomic status due to lack of data availability in some patients. The descriptive nature of the study could not fundamentally identify the causal relationship between the observed characteristics and outcomes. Further investigations should be carried out to explore the relationship between a patient's family background and EOL decision. Third, the children who died in the emergency department were not included due to incomplete medical records. Then, this was a single-center study. Thus, our study may not reflect the general practice of PICUs in China. The results of the study should been interpreted bearing in mind that they came from the practice of East Asia. Nevertheless, this study will be the first step forward to reveal and improve EOL care in Chinese PICUs.
Conclusions
The present study showed that WLST was a common practice in EOL care in a Chinese PICU. EOL care of WLST were frequent in patients transferred from other hospitals before admission to PICU, with longer lengths PICU stay and suffered from chronic disease as caner. Patients with fCPR were more common to be diagnosed with sepsis, diarrhea, and cardiac shock as the immediate cause of death. Patients with previous hospitalization and underlying diseases diagnosed before admission were strongly associated with WLST decision for EOL care. A better understanding of these factors associated with decisions to WLST is critical to physicians, policy makers, ethicists, and healthcare leaders to provide optimal EOL care for pediatric patients and improved the quality of life for families.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethics Committees of Xinhua Hospital, Shanghai. Written informed consent from the participants' legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author Contributions
YZ is responsible for the design of this study, patient data analyses, and manuscript preparation. XZ is responsible for the design of this study and interpretation of the results. LX and MD contributed to data collection from the hospital database. MD reviewed the data. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Morell E, Wolfe J, Scheurer M, Thiagarajan R, Morin C, Beke DM, et al. Patterns of care at end of life in children with advanced heart disease. Arch Pediatr Adolesc Med. (2012) 166:745–8. doi: 10.1001/archpediatrics.2011.1829
2. Fontana MS, Farrell C, Gauvin F, Lacroix J, Janvier A. Modes of death in pediatrics: differences in the ethical approach in neonatal and pediatric patients. J Pediatr. (2013) 162:1107–11. doi: 10.1016/j.jpeds.2012.12.008
3. Pollack MM, Patel KM, Ruttimann UE. PRISM III: an updated pediatric risk of mortality score. Crit Care Med. (1996) 24:743–52. doi: 10.1097/00003246-199605000-00004
4. Namachivayam P, Shann F, Shekerdemian L, Taylor A, van Sloten I, Delzoppo C, et al. Three decades of pediatric intensive care: who was admitted, what happened in intensive care, and what happened afterward. Pediatr Crit Care Med. (2010) 11:549–55. doi: 10.1097/PCC.0b013e3181ce7427
5. Aspesberro F, Mangione-Smith R, Zimmerman JJ. Health-related quality of life following pediatric critical illness. Int Care Med. (2015) 41:1235–46. doi: 10.1007/s00134-015-3780-7
6. Typpo KV, Petersen NJ, Hallman DM, Markovitz BP, Mariscalco MM. Day 1 multiple organ dysfunction syndrome is associated with poor functional outcome and mortality in the pediatric intensive care unit. Pediatr Crit Care Med. (2009) 10:562–70. doi: 10.1097/PCC.0b013e3181a64be1
7. Pollack MM, Holubkov R, Funai T, Berger JT, Clark AE, Meert K, et al. Simultaneous prediction of new morbidity, mortality, and survival without new morbidity from pediatric intensive care: a new paradigm for outcomes assessment. Crit Care Med. (2015) 43:1699–709. doi: 10.1097/CCM.0000000000001081
8. Burns JP, Sellers DE, Meyer EC, Lewis-Newby M, Truog RD. Epidemiology of death in the PICU at five U.S. teaching hospitals*. Crit Care Med. (2014) 42:2101–8. doi: 10.1097/CCM.0000000000000498
9. Schneiderman LJ, Gilmer T, Teetzel HD, Dugan DO, Blustein J, Cranford R, et al. Effect of ethics consultations on nonbeneficial life-sustaining treatments in the intensive care setting: a randomized controlled trial. JAMA. (2003) 290:1166–72. doi: 10.1001/jama.290.9.1166
10. Weise KL, Okun AL, Carter BS, Christian CW. Guidance on forgoing life-sustaining medical treatment. Pediatrics. (2017) 140:e20171905. doi: 10.1542/peds.2017-1905
11. Plötz FB, van Heerde M, Kneyber MC, Markhorst DG. End-of-life decision in a paediatric intensive care unit: decision making in light of the parents' religious beliefs. Int Care Med. (2008) 34:1355. doi: 10.1007/s00134-008-1115-7
12. Mark NM, Rayner SG, Lee NJ, Curtis JR. Global variability in withholding and withdrawal of life-sustaining treatment in the intensive care unit: a systematic review. Int Care Med. (2015) 41:1572–85. doi: 10.1007/s00134-015-3810-5
13. Oberender F, Tibballs J. Withdrawal of life-support in paediatric intensive care–a study of time intervals between discussion, decision and death. BMC Pediatr. (2011) 11:39. doi: 10.1186/1471-2431-11-39
14. Bobillo-Perez S, Segura S, Girona-Alarcon M, Felipe A, Balaguer M, Hernandez-Platero L, et al. End-of-life care in a pediatric intensive care unit: the impact of the development of a palliative care unit. BMC Palliat Care. (2020) 19:74. doi: 10.1186/s12904-020-00575-4
15. Dryden-Palmer K, Haut C, Murphy S, Moloney-Harmon P. Logistics of withdrawal of life-sustaining therapies in PICU. Pediatr Crit Care Med. (2018) 19(Suppl. 2):S19–25. doi: 10.1097/PCC.0000000000001621
16. Sprung CL, Maia P, Bulow HH, Ricou B, Armaganidis A, Baras M, et al. The importance of religious affiliation and culture on end-of-life decisions in European intensive care units. Int Care Med. (2007) 33:1732–9. doi: 10.1007/s00134-007-0693-0
17. Vincent JL. Forgoing life support in western European intensive care units: the results of an ethical questionnaire. Crit Care Med. (1999) 27:1626–33. doi: 10.1097/00003246-199908000-00042
18. ten Berge J, de Gast-Bakker DA, Plötz FB. Circumstances surrounding dying in the paediatric intensive care unit. BMC Pediatr. (2006) 6:22. doi: 10.1186/1471-2431-6-22
19. Althabe M, Cardigni G, Vassallo JC, Allende D, Berrueta M, Codermatz M, et al. Dying in the intensive care unit: collaborative multicenter study about forgoing life-sustaining treatment in argentine pediatric intensive care units. Pediatr Crit Care Med. (2003) 4:164–9. doi: 10.1097/01.PCC.0000059428.08927.A9
20. Suzuki F, Takeuchi M, Tachibana K, Isaka K, Inata Y, Kinouchi K. Life-sustaining treatment status at the time of death in a japanese pediatric intensive care unit. Am J Hos Palliat Care. (2018) 35:767–71. doi: 10.1177/1049909117743474
21. Seino Y, Kurosawa H, Shiima Y, Niitsu T. End-of-life care in the pediatric intensive care unit: Survey in Japan. Pediatr Int. (2019) 61:859–64. doi: 10.1111/ped.13924
22. Zhu Y, Zhu X, Deng M, Wei H, Zhang M. Causes of death in hospitalized children younger than 12 years of age in a Chinese hospital: a 10 year study. BMC Pediatr. (2018) 18:8. doi: 10.1186/s12887-017-0981-y
23. Mink RB, Pollack MM. Resuscitation and withdrawal of therapy in pediatric intensive care. Pediatrics. (1992) 89(5 Pt 1):961–3.
24. Vose L, Nelson R. Ethical issues surrounding limitation and withdrawal of support in the pediatric intensive care unit. J Int Care Med. (1999) 14:220–30. doi: 10.1177/088506669901400502
25. Truog RD, Cist AF, Brackett SE, Burns JP, Curley MA, Danis M, et al. Recommendations for end-of-life care in the intensive care unit: the ethics committee of the society of critical care medicine. Crit Care Med. (2001) 29:2332–48. doi: 10.1097/00003246-200112000-00017
26. Lee KJ, Tieves K, Scanlon MC. Alterations in end-of-life support in the pediatric intensive care unit. Pediatrics. (2010) 126:e859–64. doi: 10.1542/peds.2010-0420
27. Devictor DJ, Nguyen DT. Forgoing life-sustaining treatments in children: a comparison between Northern and Southern European pediatric intensive care units. Pediatr Crit Care Med. (2004) 5:211–5. doi: 10.1097/01.PCC.0000123553.22405.E3
28. Suttle ML, Jenkins TL, Tamburro RF. End-of-life and bereavement care in pediatric intensive care units. Pediatr Clin North Am. (2017) 64:1167–83. doi: 10.1016/j.pcl.2017.06.012
29. Garros D, Rosychuk RJ, Cox PN. Circumstances surrounding end of life in a pediatric intensive care unit. Pediatrics. (2003) 112:e371. doi: 10.1542/peds.112.5.e371
30. Moore P, Kerridge I, Gillis J, Jacobe S, Isaacs D. Withdrawal and limitation of life-sustaining treatments in a paediatric intensive care unit and review of the literature. J Paediatr Child Health. (2008) 44:404–8. doi: 10.1111/j.1440-1754.2008.01353.x
31. Meert KL, Keele L, Morrison W, Berg RA, Dalton H, Newth CJ, et al. End-of-life practices among tertiary care PICUs in the United States: a multicenter study. Pediat Crit Care Med. (2015) 16:e231–8. doi: 10.1097/PCC.0000000000000520
32. Sands R, Manning JC, Vyas H, Rashid A. Characteristics of deaths in paediatric intensive care: a 10-year study. Nurs Crit Care. (2009) 14:235–40. doi: 10.1111/j.1478-5153.2009.00348.x
33. Williamson T, Ryser MD, Ubel PA, Abdelgadir J, Spears CA, Liu B, et al. Withdrawal of life-supporting treatment in severe traumatic brain injury. JAMA Surg. (2020) 155:723–31. doi: 10.1001/jamasurg.2020.1790
34. Lobo SM, De Simoni FHB, Jakob SM, Estella A, Vadi S, Bluethgen A, et al. Decision-making on withholding or withdrawing life support in the ICU: a worldwide perspective. Chest. (2017) 152:321–9. doi: 10.1016/j.chest.2017.04.176
35. Pollack MM, Holubkov R, Reeder R, Dean JM, Meert KL, Berg RA, et al. PICU length of stay: factors associated with bed utilization and development of a benchmarking model. Pediatr Crit Care Med. (2018) 19:196–203. doi: 10.1097/PCC.0000000000001425
36. Kanthimathinathan HK, Plunkett A, Scholefield BR, Pearson GA, Morris KP. Trends in long-stay admissions to a UK paediatric intensive care unit. Arch Dis Childhood. (2020) 105:558–62. doi: 10.1136/archdischild-2019-317797
Keywords: clinical decision-making, pediatric intensive care units, withdrawing care, withholding treatment, withdrawing treatment, end-of-life care
Citation: Zhu Y, Zhu X, Xu L and Deng M (2021) Clinical Factors Influencing End-of-Life Care in a Chinese Pediatric Intensive Care Unit: A Retrospective, post-hoc Study. Front. Pediatr. 9:601782. doi: 10.3389/fped.2021.601782
Received: 01 September 2020; Accepted: 15 March 2021;
Published: 07 April 2021.
Edited by:
Brenda M. Morrow, University of Cape Town, South AfricaReviewed by:
Asha N. Shenoi, University of Kentucky, United StatesSaul Flores, Texas Children's Hospital, United States
Copyright © 2021 Zhu, Zhu, Xu and Deng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaodong Zhu, emh1eGlhb2RvbmdAeGluaHVhbWVkLmNvbS5jbg==
 Yueniu Zhu
Yueniu Zhu Xiaodong Zhu
Xiaodong Zhu Lili Xu
Lili Xu