
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Pediatr. , 28 October 2020
Sec. Pediatric Gastroenterology, Hepatology and Nutrition
Volume 8 - 2020 | https://doi.org/10.3389/fped.2020.545760
Esophageal perforation is a rare but critical emergency that requires early detection and prompt management. In the pediatric population, iatrogenic injury is the most common etiology of esophageal perforation, and the majority of cases come from stricture dilation. Treatment options include medical management, endoscopic therapy, and surgery. Usually, conservative treatment is appropriate in most carefully selected patients, especially in the setting of early diagnosis and with the absence of severe sepsis. A surgical approach is reserved for a large tear with mediastinum contamination, or clinical deterioration after unsuccessful conservative management. With the advancement of the endoscopy technique, endoscopy therapy using esophageal stents is an available choice for adult populations who have a complicated protracted healing course or comorbidities precluding surgical attempts. However, this procedure is seldom implemented in children, especially in young infants, owing to unavailable equipment and experts. We report our successful use of a fully-covered self-expandable metal biliary stent in managing esophageal perforation in a seven-month-old infant. In light of this encouraging achievement, this model can be applied to more children who have the same problem.
Esophageal atresia (EA) is one of the common congenital esophageal malformations in children. EA with and without tracheoesophageal fistula (TEF) is classified into five types: EA without TEF (type A), EA with proximal TEF (type B), EA with distal TEF (type C), EA with both proximal and distal TEF (type D), and TEF without EA (type E, H-type TEF). Type C is the most common form of EA. Standard surgical intervention has been TEF ligation and esophageal end-to-end anastomosis. In the case of H-type TEF, bronchoscopy combined with endoscopy management has also been attempted (1). Although the survival of patients with EA has significantly improved since Haight and Towsley (2) reported their first primary repair in 1944, complications after EA repair remain a continuing challenge. Esophageal anastomotic stricture is the major early complication after the surgery, accounting for up to two-thirds of the patients (3). Endoscopic dilatation with balloon or savary dilators is a suggested procedure to manage post-operative anastomotic stricture with a satisfactory outcome of 79.7% (4). However, repeated esophageal dilation is needed for recurrent and refractory anastomotic stricture (5), which may increase the risk of esophageal perforation.
Esophageal perforation is a serious and potentially life-threatening condition that requires early detection and prompt management. Treatment options include medical management, endoscopic therapy, and surgery. Conservative treatment is appropriate in most carefully selected patients, especially in the setting of early diagnosis and absence of severe sepsis, while a surgical approach is reserved for a large tear with mediastinum contamination and sepsis, or clinical deterioration after unsuccessful conservative management (6–8). In patients with esophageal perforation who have a poor healing process or advanced comorbidities that preclude surgical approach, endoscopic esophageal stenting has been widely applied to adult populations (9). However, endoscopic esophageal stenting in pediatric populations is uncommon due to the limitations of available instruments and techniques. We report our successful use of a fully covered self-expandable metal biliary stent in managing iatrogenic esophageal perforation in a 7-month-old infant.
A female infant weighing 2,942 g was born at 39+4 weeks gestation by vaginal delivery. She was found to have a tracheoesophageal fistula and esophageal atresia (TEF/EA) soon after birth. The right aortic arch with an aberrant left subclavian artery was diagnosed in a complete assessment of the VACTERL association. She temporarily received laparoscopic esophageal banding and gastrostomy one day after birth. The thoracoscopic repair of TEF/EA was conducted when she was 2 months old. However, esophageal anastomotic stricture ensued 2 months later. She cannot tolerate oral feeding smoothly and received serial endoscopic balloon dilation at an interval of 3 weeks. At 7 months old, she received the 6th session of esophageal dilation with a balloon diameter of 9 mm. Five hours after the procedure, the patient became severely tachypneic with labored breathing. Chest auscultation revealed diminished breathing sounds over the left lung field. The respiratory rate was 55 per minute, heart rate was 195 per minute, blood pressure was 103/72 mmHg, and SpO2 was 98% under a simple oxygen face mask. A chest X-ray disclosed left pneumothorax and pneumomediastinum with a mediastinal shift. Emergent pigtail catheter insertion and endotracheal tube intubation were performed. Chest computed tomography revealed a suspected esophageal mucosal injury, pneumopericardium, pneumomediastinum, and left pneumothorax. Under the diagnosis of esophageal perforation, she received conservative treatment, including avoidance of oral intake, nasogastric tube decompression, intravenous broad-spectrum antibiotics, and partial parenteral nutrition. The clinical course was complicated by fever, but the patient soon became hemodynamically stable.
She was extubated and started on NG-tube feeding 4 days after the event. However, milk-like fluid drained out from the pigtail catheter after advancing the feeding amount. A chest X-ray after being orally fed with water-soluble contrast revealed contrast leakage with local accumulation over the left lung (Figure 1). Fasting was resumed, along with total parenteral nutrition support. However, follow-up chest X-rays showed progressing left-sided pleural effusion. Persistent esophageal leakage after a 14-day conservative treatment was impressed. She received an esophageal stent placement under endoscopic and fluoroscopic guidance. A stricture in the mid-esophagus and a trivial contrast leak was noticed under the concurrent esophagogram (Figure 2). A fully covered self-expandable metal biliary stent (M-intraductal biliary stent, the middle portion diameter was 8 mm, and the diameter at the both ends was 10 mm) was applied across the esophageal stricture because small-diameter esophageal stents for children were unavailable (Figure 3). Two weeks later, the upward migration of the esophageal stent was noticed. Endoscopic assessment following the removal of the dislodged stent disclosed a lesser degree of the stricture, but there was a small oval wall defect over it. A new fully covered self-expanding metal biliary stent was placed (WallFlex Biliary Stent, diameter 10 mm, length 40 mm; Figure 4). One month later, an esophagogram demonstrated an improvement in the stricture with no more contrast leakage. The esophageal stent was removed. The patient tolerated oral intake smoothly during a 4-month follow-up period.
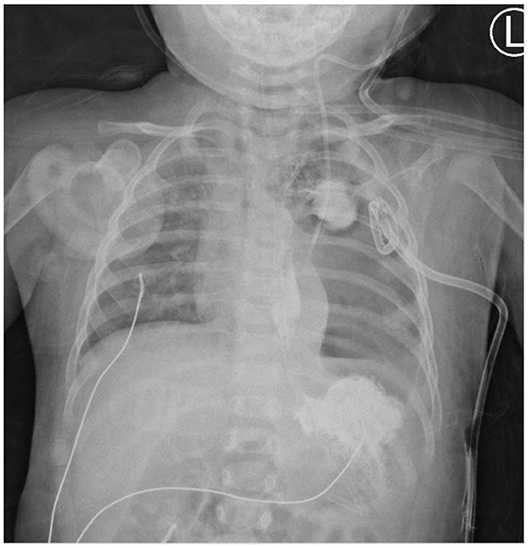
Figure 1. Esophageal perforation with the contrast leak contained in left focal para-mediastinal space.
Esophageal perforation is a potentially life-threatening clinical emergency with a high mortality and morbidity rate. In the pediatric population, iatrogenic injury is the most common etiology of esophageal perforation, and the majority comes from stricture dilation (10). Early diagnosis and intensive medical and/or surgical management promise good outcomes, and successful non-operative management require careful patient selection. The criteria for non-operative management of esophageal perforations had been established, consisting of perforations that are early diagnosed, not in neoplastic tissue or in the abdominal cavity, and the symptoms and signs of septicemia should be absent (6). Since iatrogenic injuries are often diagnosed more quickly and are associated with less extraluminal contamination, most of them are appropriate for non-operative attempts.
However, in patients who fail to respond to conservative management or have a refractory leak, endoscopic esophageal stents provide an alternative with increasing clinical application. Rollins and Barnhart (11) reported three children with esophageal perforations that were managed successfully with covered nitinol esophageal stents, after the perforations failed to close with non-operative management. The stents were introduced 13–29 days after perforation for 3–4 weeks. All of them sealed the perforation successfully. Manfredi et al. (12) also reported a success rate of 80% for closure of esophageal perforations with stent therapy after dilation. A systematic review demonstrated a success rate of 76% using self-expanding esophageal stents for managing esophageal perforation in children (13). The optimal amount of time to leave the stent in place for esophageal perforation remains unclear, and a repeat esophagogram is mandated to document that the perforation has sealed. According to the European Society for Gastrointestinal Endoscopy Guidelines (14), a duration of 6–8 weeks of stent insertion was recommended for benign esophageal stricture and esophageal perforation. In our case, complete healing of perforation and relief of stricture was achieved after 7 weeks of stenting, which conformed with previous studies.
Adverse events after esophageal stent placement should be monitored regularly. Migration is one of the most common complications, occurring in up to 56% of the pediatric population (15) and up to 75% of adult patients (16). The risk of migration is associated with the stent location, the presence of strictures, the use of plastic rather than metal stents, and the use of fully covered stents (17). In our case, although we used a fully covered self-expandable metal biliary stent with a middle waist and a cross-wire structure for preventing early migration, upward migration still developed 2 weeks later. Using a fully covered stent could be a factor. However, considering that the uncovered section of partially covered stents may allow tissue embedment, and this may make stent removal difficult and traumatic, we replaced it with a new, fully covered self-expanding metal biliary stent once again.
Hemorrhage due to arterioesophageal fistula after esophageal stent placement has been reported in patients with aberrant subclavian artery (18, 19). Though our case had right aortic arch with an aberrant left subclavian artery, since esophagectomy was challenging in our case, and hemorrhage due to vascular erosion is infrequent in the previous studies (20), the esophageal stent was still applied.
Another challenge of esophageal stenting in the pediatric population is that the size of current commercially available esophageal stents may be inappropriate for small children. Using tracheobronchial stents or self-expanding metal biliary stents as an alternative has been reported in narrow esophageal indications (11, 21–23). Custom dynamic stents, which allow food to pass between the stent and esophageal wall, have also been used (24). Our case demonstrates that biliary stents can be used safely in cases of esophageal perforation in infants. Nevertheless, the development of esophageal stents that are flexible, resist migration, and are available in smaller sizes for the pediatric population desires exploitation in the future.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation, to any qualified researcher.
We obtained informed written consent from the patient's parent authorizing publication of clinical case and images.
M-CL is a resident on the Pediatric Gastroenterology team who drafted the majority of the case report. Y-SW is the gastroenterologist who conducted the endoscopic esophageal stenting procedures. Y-JY is the attending on the Pediatric Gastroenterology team who provided treatment and follow-up for the patient throughout the course of the illness. He also contributed to the editing of the case report and the final manuscript. F-PL is the attending on the Pediatric Gastroenterology team. She contributed to the editing of the case report and the final manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Di Nardo G, Oliva S, Barbato M, Aloi M, Midulla F, Roggini M, et al. Argon plasma coagulator in a 2-month-old child with tracheoesophageal fistula. Surg Endosc. (2012) 26:2678–80. doi: 10.1007/s00464-012-2214-7
2. Haight C, Towsley H A. Congenital atresia of the esophagus with tracheoesophageal fistula: extrapleural ligation of fistula and end to end anastomosis of esophageal ends. Surg Gynecol Obstet. (1943) 76:672–88.
3. Chittmittrapap S, Spitz L, Kiely EM, Brereton RJ. Anastomotic stricture following repair of esophageal atresia. J Pediatr Surg. (1990) 25:508–11. doi: 10.1016/0022-3468(90)90561-M
4. Cabrera Chamorro C, Méndez Manchola C, Molina Ramírez I, Perilla López M, Fierro Avila F. Endoscopic balloon dilatation of esophageal strictures in children. Cir Pediatr. (2013) 26:106–11.
5. Baird R, Laberge JM, Lévesque D. Anastomotic stricture after esophageal atresia repair: a critical review of recent literature. Eur J Pediatr Surg. (2013) 23:204–13. doi: 10.1055/s-0033-1347917
6. Brinster CJ, Singhal S, Lee L, Marshall MB, Kaiser LR, Kucharczuk JC. Evolving options in the management of esophageal perforation. Ann Thorac Surg. (2004) 77:1475–83. doi: 10.1016/j.athoracsur.2003.08.037
7. Søreide JA, Viste A. Esophageal perforation: diagnostic work-up and clinical decision-making in the first 24 hours. Scand J Trauma Resusc Emerg Med. (2011) 19:1–7. doi: 10.1186/1757-7241-19-66
8. Sepesi B, Raymond DP, Peters JH. Esophageal perforation: surgical, endoscopic and medical management strategies. Curr Opin Gastroenterol. (2010) 26:379–83. doi: 10.1097/MOG.0b013e32833ae2d7
9. van Halsema EE, Kappelle WFW, Weusten BLAM, Lindeboom R, van Berge Henegouwen MI, Fockens P, et al. Stent placement for benign esophageal leaks, perforations, and fistulae: a clinical prediction rule for successful leakage control. Endoscopy. (2018) 50:98–108. doi: 10.1055/s-0043-118591
10. Rentea RM, St Peter SD. Neonatal and pediatric esophageal perforation. Semin Pediatr Surg. (2017) 26:87–94. doi: 10.1053/j.sempedsurg.2017.02.005
11. Rollins MD, Barnhart DC. Treatment of persistent esophageal leaks in children with removable, covered stents. J Pediatr Surg. (2012) 47:1843–7. doi: 10.1016/j.jpedsurg.2012.05.001
12. Manfredi MA, Jennings RW, Anjum MW, Hamilton TE, Smithers CJ, Lightdale JR. Externally removable stents in the treatment of benign recalcitrant strictures and esophageal perforations in pediatric patients with esophageal atresia. Gastrointest Endosc. (2014) 80:246–52. doi: 10.1016/j.gie.2014.01.033
13. Tandon S, Burnand KM, De Coppi P, McLaren CA, Roebuck DJ, Curry JI. Self-expanding esophageal stents for the management of benign refractory esophageal strictures in children: a systematic review and review of outcomes at a single center. J Pediatr Surg. (2019) 54:2479–86. doi: 10.1016/j.jpedsurg.2019.08.041
14. Spaander MC, Baron TH, Siersema PD, Fuccio L, Schumacher B, Escorsell À, et al. Esophageal stenting for benign and malignant disease: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. (2016) 48:939–48. doi: 10.1055/s-0042-114210
15. Fallon BP, Overman RE, Geiger JD, Jarboe MD, Kunisaki SM. Efficacy and risk profile of self-expandable stents in the management of pediatric esophageal pathology. J Pediatr Surg. (2019) 54:1233–38. doi: 10.1016/j.jpedsurg.2019.02.025
16. García-Cano J. Dilation of benign strictures in the esophagus and colon with the polyflex stent: a case series study. Dig Dis Sci. (2008) 53:341–6. doi: 10.1007/s10620-007-9864-7
17. Sharma P, Kozarek R. Practice Parameters Committee of American College of Gastroenterology. Role of esophageal stents in benign and malignant diseases. Am J Gastroenterol. (2010) 105:258–73. doi: 10.1038/ajg.2009.684
18. Merlo A, Farber M, Ohana E, Pascarella L, Crowner J, Long J. Aberrant right subclavian artery to esophageal fistula: a rare case and its management. Ann Thorac Surg. (2020) 110:E85–86. doi: 10.1016/j.athoracsur.2019.12.045
19. Hosn MA, Haddad F, El-Merhi F, Safadi B, Hallal A. Repair of an aberrant subclavian arterioesophageal fistula following esophageal stent placement. World J Gastrointest Surg. (2014) 6:117. doi: 10.4240/wjgs.v6.i6.117
20. Wang MQ, Sze DY, Wang ZP, Wang ZQ, Gao YA, Dake MD. Delayed complications after esophageal stent placement for treatment of malignant esophageal obstructions and esophagorespiratory fistulas. J Vasc Interv Radiol. (2001) 12:465–74. doi: 10.1016/S1051-0443(07)61886-7
21. Slater BJ, Pimpalwar A, Wesson D, Olutoye O, Pimpalwar S. Esophageal stents in children: bridge to surgical repair. Indian J Radiol Imaging. (2018) 28:242–6. doi: 10.4103/ijri.IJRI_313_17
22. Pang M, Bartel MJ, Clayton DB, Brahmbhatt B, Woodward TA. Selective application of fully covered biliary stents and narrow-diameter esophageal stents for proximal esophageal indications. Endoscopy. (2019) 51:169–73. doi: 10.1055/a-0650-4588
23. Ruthmann O, Richter S, Fischer A, Ruckauer KD, Hopt UT, Schrag HJ. Biliary stenting of an iatrogenic esophageal perforation following corrosive esophagitis in a 5-year-old child. Endoscopy. (2009) 41(Suppl 2):E325–6. doi: 10.1055/s-0029-1214939
Keywords: endoscopic balloon dilation, esophageal perforation, endoscopic therapy, esophageal stent, pediatrics—infants, biliary stent
Citation: Liu M-C, Wang Y-S, Yang Y-J and Lai F-P (2020) Case Report: Successful Use of Biliary Stent for Iatrogenic Esophageal Perforation Following Balloon Dilation in a 7-Month-Old Infant. Front. Pediatr. 8:545760. doi: 10.3389/fped.2020.545760
Received: 26 March 2020; Accepted: 06 October 2020;
Published: 28 October 2020.
Edited by:
Luigi Dall'Oglio, Bambino Gesù Children Hospital (IRCCS), ItalyReviewed by:
Francesco Valitutti, Ospedali Riuniti San Giovanni di Dio e Ruggi d'Aragona, ItalyCopyright © 2020 Liu, Wang, Yang and Lai. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fu-Ping Lai, bWFydmVsb3VzMzkxOEBnbWFpbC5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.