
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Pediatr. , 30 September 2020
Sec. Pediatric Urology
Volume 8 - 2020 | https://doi.org/10.3389/fped.2020.00520
This article is part of the Research Topic Hydronephrosis Associated with Ureteropelvic Junction Anomalies: An Ongoing Challenge View all 17 articles
The most common cause of hydronephrosis in the pediatric age group is ureteropelvic junction-type hydronephrosis (UPJHN). Since the advent of widespread maternal ultrasound screening, clinical presentation of hydronephrosis associated with UPJ anomalies has changed dramatically. Today most cases are diagnosed in the prenatal period, and neonates present without signs or symptoms. For those who are not detected at birth, UPJHN eventually presents throughout childhood and even adulthood with various symptoms. Clinical picture of UPJHN highly depends on the presence and severity of obstruction, and whether it affects single or both kidneys. Abdominal or flank pain, abdominal mass, hematuria, kidney stones, urinary tract infections (UTI), and gastrointestinal discomfort are the main symptoms of UPJHN in childhood. Other less common findings in such patients are growth retardation, anemia, and hypertension. UTI is a relatively rare condition in UPJHN cases, but it may occur as pyelonephritis. Vesicoureteric reflux should be kept in mind as a concomitant pathology in pediatric UPJHN that develop febrile UTI. Although many UPJHN cases are known to improve over time, close clinical observation is critical in order to avoid irreversible kidney damage. The most appropriate approach is to follow-up the patients considering the presence of symptoms, the severity of hydronephrosis and the decrease in kidney function and, if necessary, to decide on early surgical intervention.
Widespread use of prenatal ultrasonography (US) gave clinicians the opportunity to diagnose urinary tract abnormalities much earlier and more frequently than the past (1). The approximate varying incidence of 1 per 750–2,000, ureteropelvic junction type hydronephrosis (UPJHN) is the most common cause of childhood hydronephrosis (2). It occurs in 13% of children with prenatally detected renal pelvis dilatation, and is more common on the left side, more common in boys (2:1- male to female), and is rarely seen bilaterally (2–4).
An obstruction at ureteropelvic junction level which is defined as restriction of urine outflow from pelvis renalis to the ureter may result in progressive deterioration or hinder normal renal development (5–8). Over 50% of all cases considered to have kidney abnormalities in the prenatal period are hydronephrosis, but unfortunately there are currently no reliable prenatal diagnostic test that can distinguish obstructive hydronephrosis from non-obstructive (8–10). The differentiation between urinary tract obstruction and dilatation is the most important problem in the management of these patients (6, 11, 12). Since the clinical course are quite diverse, and generalization is rather difficult, the most appropriate approach of UPJHN seen in children would be to evaluate on a patient basis (4, 13–16).
In this review, the purpose is to provide general information about the clinical presentation and symptomatology of hydronephrosis associated with uretero pelvic junction anomalies, as well as discussing the clinical findings through some case examples.
Over the last decades, clinical presentation of patients with UPJHN has shifted from the “symptomatic” patients to the “asymptomatic” neonates who present with prenatal diagnosis (1–4, 15, 16). UPJHN cases without a prenatal diagnosis present with various symptoms such as febrile urinary tract infection (UTI), abdominal masses, pain, pyuria, hematuria, and some gastrointestinal symptoms in the post-natal period or later years. Failure to thrive, anemia, hypertension, and urinary extravasation are much more rare symptoms of UPJHN in childhood (14–16).
Clinical picture of hydronephrosis associated with uretero pelvic junction anomalies highly depends on the presence and severity of obstruction, and whether it affects single or both kidneys. However, most infants with severe hydronephrosis are otherwise asymptomatic and rarely require intervention during follow-up (6, 8, 12). Therefore, parallel to the change in its clinical presentation, the first enthusiasm for early intervention of hydronephrosis associated with UPJ anomalies has turned into a more conservative approach in recent years (11, 15, 17–19). Although there are numerous publications regarding conservative management of UPJ hydronephrosis, and the current trend is to follow the infants through clinical and US findings, the general practice shows a wide variety even today (20–26).
The most accurate answers to the questions of which treatment is better for symptomatic infants, which kidney will benefit from surgery and which patients should be followed up expectantly are still not clear. There are two issues that do not have much discussion during follow-up period of UPJHN patients. First; close monitoring is mandatory for high-grade hydronephrosis managed conservatively; secondly, severe hydronephrosis suggesting an obstruction in solitary kidney is an indisputable condition that requires urgent intervention. An urgent intervention may also be required in patients presenting with urosepsis or acute renal failure (13, 15, 26, 27). In general, the surgical decision in UPJOHN cases is made based on US findings. Therefore, accurate determination of hydronephrosis severity is very important for infants associated with UPJHN. In severe cases of hydronephrosis (SFU 4) with renal parenchymal thinning, clinicians should make a surgical decision without delay, as kidney function may also be impaired in a short time. Based on EAU and ESPU 2019 Guidelines on pediatric urology, surgical indications for UPJHN are impaired renal function (<40%), significant renal functional decrease (>10%) in control scans, poor drainage after furosemide injection, increased AP diameter, and SFU-III/IV (8, 26). Although there are problems with some of these indications, absolute surgical indications in the follow-up of UPJHN cases can be considered as renal parenchymal thinning (<3 mm), contralateral kidney balancing hypertrophy and decreased kidney function. Differential renal uptake on diuretic renography <30% in unilateral cases and <35% in bilateral cases is usually required a surgical intervention. Surgical treatment can also be recommended in children whose SFU3 hydronephrosis continues for 3 years and develops compensated hypertrophy in the contralateral kidney (27). If the main goal during conservative monitoring is to protect the child from the risk of permanent kidney damage, waiting for ultrasonographic or functional deterioration is a cornerstone that must be distinguished very carefully in each case. It should be noted that at this cornerstone, the presence of symptoms such as recurrent UTI, hematuria, kidney stones or pain will speed up the decision of surgical intervention (21, 26, 27).
As mentioned above, the clinical picture of UPJHN should be evaluated in two different categories, considering that most cases are asymptomatic and diagnosed on routine prenatal US screening; (a) asymptomatic infants who are usually managed conservatively (b) children who present at an older ages with urinary symptoms or as a result of incidental findings during the analysis of unrelated problems.
Symptomatology in a newborn with antenatally diagnosed UPJHN is usually the absence of symptoms. However, the most frequent symptom of UPJHN in neonates and infants was a palpable flank mass in the past. Most of the abdominal masses encountered in the neonatal period are related to hydronephrotic kidneys. Therefore, a palpable abdominal mass may be the first finding to be considered in a physical examination in a newborn with UPJHN.
Since UPJHN is often associated with other congenital anomalies, including imperforated anus, contralateral multicystic kidney, congenital heart disease, VATER syndrome, and esophageal atresia, in a newborn with established prenatal diagnosis, a thorough examination of all systems should be performed (8). Occasionally, UPJHN can also be diagnosed during extended diagnostics of other congenital abnormalities. On the other hand, in all children with a diagnosis of urinary tract infection (UTI) within the early neonatal period, urinary tract obstruction, UPJHN should also be considered.
Children with UPJHN and impaired urinary drainage are considered to be prone to severe UTIs (28, 29). Although UTI is an uncommon presentation in UPJHN cases with an incidence of 1.3–12%, it may be quite severe requiring urgent intervention and drainage (4, 30–35). Previous reports suggest that the risk of UTI increases with the degree of hydronephrosis, and patients with high-grade hydronephrosis have significantly higher UTI rates than those with mild hydronephrosis (13.8 vs. 4.1%) (36–39). Although the studies are not standardized in terms of the use of prophylactic antibiotics, the method of detecting infection or the selection of patients for VCUG, it has been clearly demonstrated that patients with mild or moderate hydronephrosis are at much lower risk of significant UTI than patients with severe hydronephrosis.
When a child with UPJHN applies with a febrile UTI, the possibility of associated VUR is an important issue to consider. Based on the fact that some studies show one-third of cases having a VUR (8, 40, 41); VCUG is often favored by European guidelines for all children with UPJO (42, 43). Before deciding to apply VCUG, an invasive procedure with radiation exposure in UPJHN patients, it should be taken into account that in many cases that are often asymptomatic, VUR may improve over time and the concept of benefit-harm to the patient (44–46).
Madden et al. (47) performed VCUG in more than 80% of their patients with UPJHN and in no case detected VUR. In the same study, it was reported that patients who did not undergo VCUG remained asymptomatic and no imaging was required except for follow-up ultrasounds (47). Given the low rate of UTI reported, it may be considered that antibiotic prophylaxis has a limited role in the management of such patients (13, 47–49), and VCUG screening is considered to be optional (50). However, more aggressive evaluation and intervention, including antibiotic prophylaxis and VCUG are often indicated in those with worsening or high-grade hydronephrosis (47, 51–53). It should be noted that the presence of ureter dilatation is also important to suspect VUR even in severe hydronephrosis cases.
Another issue that can be considered for the prevention UTI in boys with UPJHN may be circumcision. Ellison et al. (54) reported that the risk of UTI in boys with UPJHN decreased significantly when circumcised. Although there may be no direct relationship since the stasis is in renal pelvis away from the external urethral meatus, in clinical practice, circumcision may be recommended for infant boys who have UTI history.
Unlike asymptomatic presentation early in life, older children with UPJHN are often diagnosed due to their specific or non-specific symptoms. A carefully gathered clinical history played a very important role in the diagnosis of patients with UPJHN. These symptoms are usually febrile UTIs, a palpable mass, or unexplained abdominal or flank pain. In addition, UPJHN can be detected during evaluation of stone disease and sudden onset hypertension (8). Another small group ordered for a completely unrelated issue during imaging is diagnosed by chance.
In children with UPJHN/UPJO, pain is primarily the result of dilation, stretching and spasm of the urinary tract, when the urine flow exceeds the capacity to drain properly. The causes of pain are generally muscle spasm, increased proximal peristalsis, local inflammation, irritation and edema at the site of obstruction. It develops through chemoreptor activation and stretching of the submucosal free nerve endings. The severity of pain depends on the individual's pain threshold and perception, and on the speed and degree of changes in hydrostatic pressure within the proximal ureter and renal pelvis. Chronic severe obstruction usually does not cause pain.
Although it is generally thought to have gastrointestinal symptoms, It should be noted that attacks of unexplained recurrent vomiting or abdominal discomfort may be associated with UPJ obstruction in infants (55). Sudden onset of severe abdominal pain, nausea, and vomiting, often in the late evening, is typical in older children with UPJO. This colicky-type pain usually begins in the upper lateral midback over the costovertebral angle and occasionally subcostally. It radiates inferiorly and anteriorly toward the groin. At their initial presentation, this symptomatology is far more common than febrile urinary tract infections or hematuria (8, 56). Pain along with increased diuresis should also raise the level of suspicion for an obstructive process. This usually occurs in children who receive a diuretic challenge during a furosemide renal scan.
It is important to recognize that patients with extrinsic anatomic abnormalities (e.g., lower pole crossing vessels) can present with colicky flank pain, which is sometimes associated with vomiting, and may present misleadingly unremarkable test results during their asymptomatic periods (56, 57). There is no history of hydronephrosis in the neonatal period In 75–100% of children with crossing vessels (57–59). The incidence of colickly pain in pure extrinsic UPJHN has been reported as 71.8–100%, increasing with age (57–59). The average age of patients with a crossing vessel is between 7 and 11 years and is statistically higher than in patients with pure intrinsic obstruction (58–61). An ultrasonography performed in the symptomatic period can prevent delay in diagnosis of extrinsic UPJHN due to crossing vessel.
Hydronephrosis is considered as a risk factor for stone formation in children. Although the etiology of stone formation does not depend solely on the pelvicaliceal anatomy, impaired urinary drainage, decreased or abnormal peristalsis, increased urine transit times and larger pelvicaliceal volumes play a subtle role during the beginning of the nucleation process in UPJHN patients with nephro/urolithiasis (62) (Figure 1).
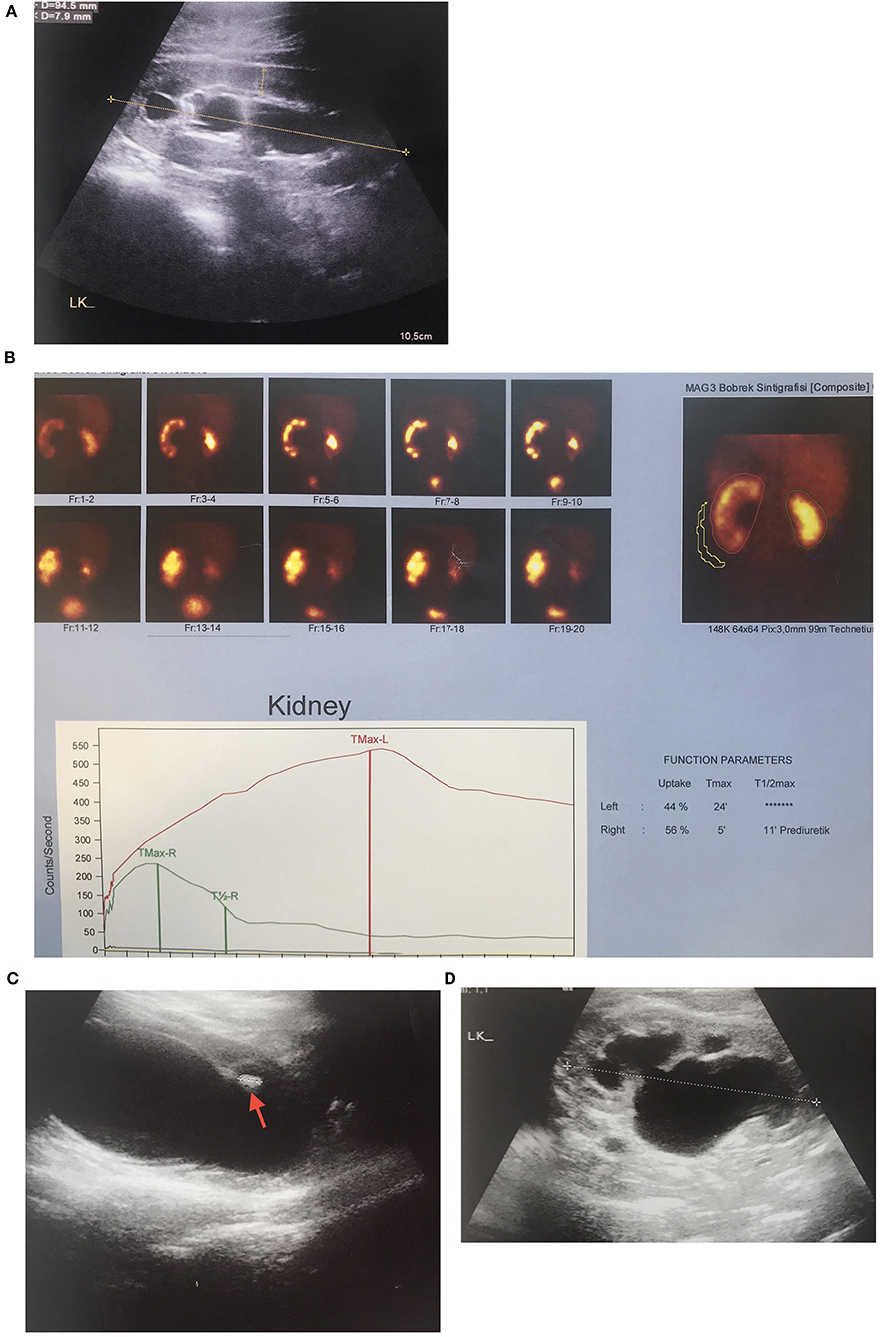
Figure 1. UPJHN in 3 months-old boy with prenatally detected left hydronephrosis (A) Severe hydronephrosis with 2.4 mm paranchymal thickness and 22 mm in AP diameter of pelvis renalis (B) Left obstructive hydronephrosis with 44% of differential function on MAG 3 scintigraphy (C) Mobile hyperechogenic particules in renal pelvis and calyces, hyperechogenicity in the lower calyces which are suggested urinary stone formation (D) Mild hydronephrosis with 8 mm paranchymal thickness and 16 mm in AP diameter of pelvis renalis in 9 years after left pyeloplasty.
Published pediatric reports of hypertension obviously caused by hydronephrosis are few, and the numbers of patients included in these reports are very low (63–68). On clinical basis, the number of cases diagnosed with UPJHN/UPJO by referring to the results or symptoms of high blood pressure in the child age group is very few. While the development of clinically significant hypertension or proteinuria is very rare in patients with unilateral hydronephrosis, the same is not the case for bilateral disease (8, 63). Depending on the onset, level, and degree of obstruction as well as the presence of renal parenchymal damage or dysplasia, hypertension may develop during the follow-up.
It has been demonstrated that the function of the hydronephrotic kidney is rather well-preserved in young children, therefore it appears that the intrarenal mechanism leading to hypertension is also reversible (6, 11). The clinical importance of such finding is that surgical management may prevent the development of chronic hypertension and associated comorbidities in patients with severe hydronephrosis (68–70). The pediatric urologist and nephrologist may have to pay more attention to the risk of development of high blood pressure in patients with severe hydronephrosis (Figure 2).
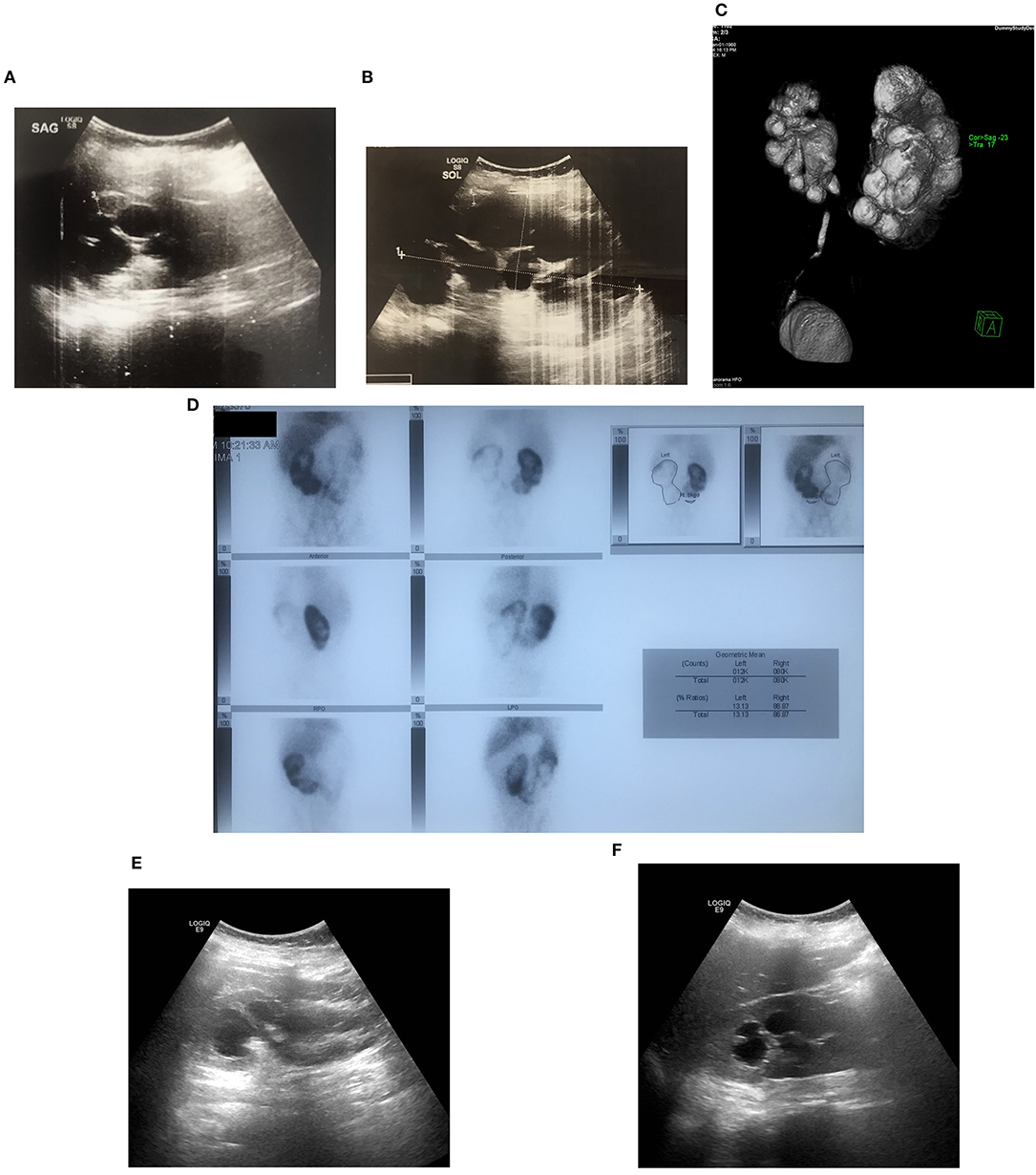
Figure 2. Bilateral UPJHN in 12 years-old boy with prenatally detected bilateral hydronephrosis with no follow-up who presented with severe hypertension and high serum creatinine (1.6 mg/dl) (A,B) pre-operative US images showing right and left severe hydronephrosis (C) Severe renal paranchymal loss on left kidney with 13% of differential function on DMSA scintigraphy (D) bilateral obstructive UPJ type hydronephrosis shown by MR urography (E,F) post-operative (bilaterally pyeloplasty) US image showing a resolution of left and right hydronephrosis, which was followed by resolution serum creatinine (0.67 mg/dl) and hypertension.
Current management approach for most children with UPJHN is often considered conservative follow-up because hydronephrosis associated with UPJ anomalies can safely improve over the time. However, it is clear that delayed decision making in the case of obstructive hydronephrosis, which requires surgical intervention, leads to impaired kidney function and long-term morbidity.
It should always be kept in mind that clinical and symptomatological findings, as well as radiological tests, should be carefully evaluated so that the conservative follow-up strategy does not put a single patient at risk for possibly irreversible kidney damage.
Although conservative management algorithms and surgical indications are still an ongoing problem and there is no consensus among different disciplines, it is very important to maintain a long follow-up in both conservatively managed and surgical cases, taking into account negative prognostic factors.
The author confirms being the sole contributor of this work and has approved it for publication.
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Thomas DFM. Prenatal diagnosis: what do we know of long term outcomes? J Pediatr Urol. (2010) 6:204–11. doi: 10.1016/j.jpurol.2010.01.013
2. Woodward M, Frank D. Postnatal management of antenatal hydronephrosis. BJU Int. (2002) 89:149–56. doi: 10.1046/j.1464-4096.2001.woodward.2578.x
3. Nguyen HT, Benson CB, Bromley B, Campbell JB, Chow J, Coleman B, et al. Multidisciplinary consensus on the classification of prenatal an postnatal urinary tract dilation (UTD classification system). J Pediatr Urol. (2014) 10:982–99. doi: 10.1016/j.jpurol.2014.10.002
4. Passerotti CC, Kalish LA, Chow J, Passerotti AM, Recabal P, Cendron M, et al. The predictive value of the first postnatal ultrasound in children with antenatal hydronephrosis. J Pediatr Urol. (2011) 7:128–36. doi: 10.1016/j.jpurol.2010.09.007
5. Whitaker RH. Some observations and theories on the wide ureter and hydronephrosis. Br J Urol. (1975) 47:377–85. doi: 10.1111/j.1464-410X.1975.tb03990.x
6. Koff SA. Requirements for accurately diagnosing chronic partial upper urinary tract obstruction in children with hydronephrosis. Pediatr Radiol. (2008) 38 (Suppl. 1):S41–8. doi: 10.1007/s00247-007-0590-2
7. Chevalier RL, Chung KH, Smith CD, Ficenec M, Gomez RA. Renal apoptosis and clusterin following ureteral obstruction: the role of maturation. J Urol. (1996) 156:1474–9. doi: 10.1097/00005392-199610000-00075
8. Lorenzo AJ, Csaicsich D, Aufricht C, Khoury AE. Obstructive Genitourinary Disorders. Elsevier BV (2008). doi: 10.1016/B978-0-323-04883-5.50043-X
9. Elder JS. Antenatal hydronephrosis. Fetal and neonatal management. Pediatr Clin North Am. (1997) 44:1299–321. doi: 10.1016/S0031-3955(05)70558-7
10. Reddy PP, Mandell J. Prenatal diagnosis. Therapeutic implications. Urol Clin North Am. (1998) 25:171–80. doi: 10.1016/S0094-0143(05)70005-7
11. Ulman I Jayanthi V and Koff SA. The longterm follow-up of newborns with severe unilateral hydronephrosis managed nonoperatively. J Urol. (2000) 164 (3 pt 2):1101–5. doi: 10.1097/00005392-200009020-00046
12. Ransley PG, Dhillon HK, Gordon I, Duffy PG, Dillon MJ, Barrat TM. The postnatal management of hydronephrosis diagnosed by prenatal ultrasound. J Urol. (1990) 144:584–7. doi: 10.1016/S0022-5347(17)39528-9
13. Nguyen HT, Herndon CD, Cooper C, Gatti J, Kirsch A, Kokorowski P, et al. The Society for fetal urology consensus statement on the evaluation and management of antenatal hydronephrosis. J Pediatr Urol. (2010) 6:212–31. doi: 10.1016/j.jpurol.2010.02.205
14. Keays MA, Guerra LA, Mihill J, Raju G, Al-Asheeri NA, Pike J, et al. Reliability assessment of society for fetal urology ultrasound grading system for hydronephrosis. J Urol. (2008) 180:1680–2; discussion 1682–3. doi: 10.1016/j.juro.2008.03.107
15. Herndon A. Antenatal hydronephrosis: differential diagnosis, evaluation, and treatment options. ScientificWorld J. (2006) 6:2345–65. doi: 10.1100/tsw.2006.366
16. Onen A. Treatment and outcome of prenatally detected newborn hydronephrosis. J Pediatr Urol. (2007) 3:469–76. doi: 10.1016/j.jpurol.2007.05.002
17. King L. Fetal hydronephrosis: what is the urologist to do? Urology. (1993) 42:229–31. doi: 10.1016/0090-4295(93)90609-E
18. Koff SA. Postnatal management of antenatal hydronephrosis using an observational approach. Urology. (2000) 55:609–11. doi: 10.1016/S0090-4295(00)00459-3
19. Perez L, Friedman R, King L. The case for relief of ureteropelvic junction in neonates and young children at time of diagnosis. Urology. (1991) 38:195–201. doi: 10.1016/S0090-4295(91)80343-6
20. Weitz M, Schmidt M, Laube G. Primary non surgical management of unilateral ureteropelvic junction obstruction in children: a systematic review. Pediatr Nephrol. (2017) 32:2203–13. doi: 10.1007/s00467-016-3566-3
21. Braga LH, Ruzhynsky V, Pemberton J, Farrokhyar F, Demeira J, Lorenzo AJ. Evaluating practice patterns in postnatal management of antenatal hydronehrosis: a national survey of Canadian pediatric urologists and nephrologists. Urology. (2014) 83:909–14. doi: 10.1016/j.urology.2013.10.054
22. Williams B, Tareen B, Resnick MI. Pathophysiology and treatment of ureteropelvic junction obstruction. Curr Urol Rep. (2007) 8:111–7. doi: 10.1007/s11934-007-0059-8
23. Ingraham SE, McHugh KM. Current perspectives on congenital obstructive nephropathy. Pediatr Nephrol. (2011) 26:1453–61. doi: 10.1007/s00467-011-1799-8
24. Chertin B, Rolle U, Farkas A, Puri P. Does delaying pyeloplasty affect renal function in children with prenatal diagnosis of pelvi-ureteric juction obstruction? BJU Int. (2002) 90:72–5. doi: 10.1046/j.1464-410X.2002.02829.x
25. Onen A, Jayanthi VR, Koff SA. Long-term follow-up of prenatally detected severe bilateral newborn hydronephrosis initially managed non operatively. J Urol. (2002) 168:1118–20. doi: 10.1016/S0022-5347(05)64604-6
26. Radmayr C, Bogaert G, Dogan HS, Kocvara R, Nijman JM, Stein R, et al. EAU Guidelines on Pediatric Urology. European Society for Paediatric Urology and European Association of Urology (2020). p. 59–61. Arnhem: EAU Guidelines Office. Available online at: http://uroweb.org/guidelines/compilations-of-all-guidelines/
27. Onen A. Grading of hydronephrosis: an ongoing challenge. Front. Pediatr. (2020). doi: 10.3389/fped.2020.00458
28. Riccabona M, Sorantin E, Hausegger K. Imaging guided interventional procedures in pediatric urradiology- a case based overview. Eur J Radiol. (2002) 43:167–79. doi: 10.1016/S0720-048X(02)00110-9
29. Khan A, Jhaveri R, Seed PC, Arshad M. Update on associated risk factors, diagnosis, and management of recurrent urinary tract infections in children. J Pediatric Infect Dis Soc. (2019) 8:152–9. doi: 10.1093/jpids/piy065
30. Yang Y, Hou Y, Niu ZB, Wang CL. Long-term follow-up and management of prenatally detected, isolated hydronephrosis. J Pediatr Surg. (2010) 45:1701–6. doi: 10.1016/j.jpedsurg.2010.03.030
31. Sidhu G, Beyene J, Rosenblum ND. Outcome of isolated antenatal hydronephrosis: a systematic review and meta-analysis. Pediatr Nephrol. (2006) 21:218–24. doi: 10.1007/s00467-005-2100-9
32. Lee RS, Cendron M, Kinnamon DD, Nguyen HT. Antenatal hydronephrosis as a predictor of postnatal outcome: a meta-analysis. Pediatrics. (2006) 118:586–93. doi: 10.1542/peds.2006-0120
33. Tombesi MM, Alconcher LF. Short-term outcome of mild isolated antenatal hydronephrosis conservatively managed. J Pediatr Urol. (2012) 8:129–33. doi: 10.1016/j.jpurol.2011.06.009
34. Estrada CR, Peters CA, Retik AB, Nguyen HT. Vesicoureteral reflux and urinary tract infection in children with a history of prenatal hydronephrosis–should voiding cystourethrography be performed in cases of postnatally persistent grade II hydronephrosis? J Urol. (2009) 181:801–6; discussion 806–7. doi: 10.1016/j.juro.2008.10.057
35. Coelho GM, Bouzada MC, Lemos GS, Pereira AK, Lima BP, Oliveira EA. Risk factors for urinary tract infection in children with prenatal renal pelvic dilatation. J Urol. (2008) 179:284–9. doi: 10.1016/j.juro.2007.08.159
36. Timberlake MD, Herndorn A. Mild to moderate postnatal hydronephrosis- grading systems and management. Nat Rev Urol. (2013) 10:649–56. doi: 10.1038/nrurol.2013.172
37. Coelho GM, Bouzada MC, Pereira AK, Figueiedo BF, Leite MR, Oliveira DS, et al. Outcome of isolated antenatal hydronephrosis: a prospective cohort study. Pediatr Nephrol. (2007) 22:1727–34. doi: 10.1007/s00467-007-0539-6
38. Szymanski KM, Al-Said AN, Pippi Salle JL, Capolicchio JP. Do infants with mild prenatal hydronephrosis benefit from screening for vesicouretral reflux? J Urol. (2012) 188:576–81. doi: 10.1016/j.juro.2012.04.017
39. Stein R, Dogan HS, Hoebeke P, Kočvara R, Nijman RJ, Radmayr C, et al. European association of urology; european society for pediatric urology. Eur Urol. (2015) 67:546–58. doi: 10.1016/j.eururo.2014.11.007
40. Woo HH, Farnsworth RH. Vesico-ureteric reflux and surgically treated pelvi-ureteric junction obstruction in infants under the age of 12 months. Aust N Z J Surg. (1996) 66:824–5. doi: 10.1111/j.1445-2197.1996.tb00758.x
41. Perrelli L, Calisti A, Pintus C, D'Errico G. Management of pelviureteric junction obstruction in the first six months of life. Z Kinderchir. (1985) 40:158–62. doi: 10.1055/s-2008-1059736
42. Beetz R, Bokenkamp A, Brandis M, Hoyer P, John U, Kemper MJ, et al. Diagnosis of congenital dilatation of the urinary tract. Consensus Group of the Pediatric Nephrology Working Society in cooperation with the pediatric urology working Group of the German Society of urology and with the pediatric urology working Society in the Germany Society of pediatric surgery. Urologe A. (2001) 40:495–507; quiz 508–499. doi: 10.1007/s001200170015
43. Silay MS, Undre S, Nambiar AK, Dogan HS, Kocvara R, Nijman RJM, et al. Role of antibiotic prophylaxis in antenatal hydronephrosis: a systematic review from the European Association of Urology/European Society for Paediatric Urology Guidelines Panel. J Pediatr Urol. (2017) 13:306–15. doi: 10.1016/j.jpurol.2017.02.023
44. Weitz M, Schmidt M. To screen or not to screen for vesicoureteral reflux in children with ureteropelvic junction obstruction: a systematic review. Eur J Pediatr. (2017) 176:1–9. doi: 10.1007/s00431-016-2818-3
45. Williams G, Fletcher JT, Alexander SI, Craig JC. Vesicoureteral Reflux. J Am Soc Nephrology. (2008) 19:847–62. doi: 10.1681/ASN.2007020245
46. Stratton KL, Pope JC, Adams MC, Brock JW III, Thomas JC. Implications of ionizing radiation in the pediatric urology patient. J Urol. (2010) 183:2137–42. doi: 10.1016/j.juro.2010.02.2384
47. Madden JM, Wiener JS, Routh JC, Ross SS. Resolution rate of isolated low-grade hydronephrosis diagnosed within the first year of life. J Pediatr Urol. (2014) 10:639–44. doi: 10.1016/j.jpurol.2014.07.004
48. Lee JH, Choi HS, Kim JK, Won HS, Kim KS, Moon DH, et al. Nonrefluxing neonatal hydronephrosis and the risk of urinary tract infection. J Urol. (2008) 179:1524–8. doi: 10.1016/j.juro.2007.11.090
49. Skoog SJ, Peters CA, Arant BS Jr, Copp HL, Elder JS, Hudson RG, et al. Pediatric vesicoureteral reflux guidelines panel summary report: clinical practice guidelines for screening siblings of children with vesicoureteral reflux and neonates/infants with prenatal hydronephrosis. J Urol. (2010) 184:1145–51. doi: 10.1016/j.juro.2010.05.066
50. Nicolau N, Renkama KY, Bongers EM, Giles RH, Knoers NV. Genetic, environmental and epigenetic factors involved in CAKUT. Nat Rev Nephrol. (2015) 11:720–31. doi: 10.1038/nrneph.2015.140
51. Shaikh N, Ewing AL, Bhatnagar S, Hoberman A. Risk of renal scarring in children with a first urinary tract infection: a systematic review. Pediatrics. (2010) 126:1084–91. doi: 10.1542/peds.2010-0685
52. Zanetta VC, Rosman BM, Bromley B, Shipp TD, Chow JS, Campbell JB, et al. Variations in management of mild prenatal hydronephrosis among maternal-fetal medicine obstetricians, and pediatric urologists and radiologists. J Urol. (2012) 188:1935–9. doi: 10.1016/j.juro.2012.07.011
53. Docimo SG, Silver RI. Renal ultrasonography in newborns with prrenatally detected hydronephrosis: why wait? J Urol. (1997) 157:1387–9. doi: 10.1016/S0022-5347(01)64996-6
54. Ellison JS, Geolani W, Fu BC, Holt SK, Gore JL, Merguerian PA Neonatal circumcision and urinary tract infections in infants with hydronephrosis. Pediatrics. (2018) 142:1–7. doi: 10.1542/peds.2017-3703
55. Mergener K, Weinerth JL, Baillie J. Dietl's crisis: a syndrome of episoodic abdominal pain of urologic origin that may present to gastroenterologist. Am J Gastroenterol. (1997) 92:2289–91.
56. Cain MP, Rink RC, Thomas AC, Austin PF, Kaefer M, Casale AJ. Symptomatic ureteropelvic junction obstruction in children in the era of prenatal sonography- is there a higher incidence of crossing vessels? Urology. (2001) 57:338–41. doi: 10.1016/S0090-4295(00)00995-X
57. Polok M, Toczewski K, Borselle D, Apoznanski W, Jedrzejuk D, Patkowski D. Hydronephrosis in children caused by lower pole crossing vessels—how to choose the proper method of treatment? Front Pediatr. (2019) 7:1–4. doi: 10.3389/fped.2019.00083
58. Esposito C, Bleve C, Escolino M, Caione P, GerocarniNappo S, Farina A, et al. Laparoscopic transposition of lower pole crossing vessels (vascular hitch) in children with pelviureteric junction obstruction. Transl Pediatr. (2016) 5:256–61. doi: 10.21037/tp.2016.09.08
59. Weiss D, Kadakia S, Kurzweil R, Srinivasan A, Darge K, Shukla A. Detection of crossing vessels in pediatric ureteropelvic junction obstruction: clinical patterns and imaging findings. J Pediatr Urol. (2015) 11:173.e1–5. doi: 10.1016/j.jpurol.2015.04.017
60. Chiarenza S, Bleve C, Fasoli L, Battaglino F, Bucci V, Novek S, et al. Ureteropelvic junction obstruction in children by polar vessels. Is laparoscopic vascular hitching procedure a good solution? Single center experience on 35 consecutive patients. J Pediatr Surg. (2016) 51:310–4. doi: 10.1016/j.jpedsurg.2015.10.005
61. Schneider A, Ferreira CG, Delay C, Lacreuse I, Moog R, Becmeur F. Lower pole vessels in children with pelviureteric junction obstruction: laparoscopic vascular hitch or dismembered pyeloplasty? J Pediatr Urol. (2013) 9:419–23. doi: 10.1016/j.jpurol.2012.07.005
62. Khan SR, Pearle MS, Robertson WG, Gambaro G, Canales BK, Doizi S, et al. Kidney Stones. Nat Rev Dis Primers. (2016) 2:16008. doi: 10.1038/nrdp.2016.8
63. Farnham SB, Adams MC, Brock JW, Pope JC. Pediatric urologogical causes of hypertension. J Urol. (2005) 173:697–704. doi: 10.1097/01.ju.0000153713.46735.98
64. Abramson M, Jackson B. Hypertension and unilateral hydronephrosis. J Urol. (1984) 132:746–8. doi: 10.1016/S0022-5347(17)49855-7
65. Wanner C, Luscher TF, Schollmeyer P, Vetter W. Unilateral hydronephrosis and hypertension: cause or coincidence? Nephron. (1987) 45:236–41. doi: 10.1159/000184125
66. Carlström M, Wåhlin N, Sällström J, Skøtt O, Brown R, Persson AE. Hydronephrosis causes salt-sensitive hypertension in rats. J Hypertens. (2006) 24:1437–43. doi: 10.1097/01.hjh.0000234126.78766.00
67. Mizuiri S, Amagasaki Y, Hosaka H, Fukasawa K, Nakayama K, Nakamura N, et al. Hypertension in unilateral atrophic kidney secondary to ureteropelvic junction obstruction. Nephron. (1992) 61:217–9. doi: 10.1159/000186876
68. Chalisey A, Karim M. Hypertension and hydronephrosis: rapid resolution of high blood pressure following relief of bilateral ureteric obstruction. J Gen Intern Med. (2013) 28:478–81. doi: 10.1007/s11606-012-2183-5
69. Al-Mashhadi A, Häggman M, Läckgren G, Ladjevardi S, Nevéus T, Stenberg A, et al. Changes of arterial pressure following relief of obstruction in adults with hydronephrosis. Ups J Med Sci. (2018) 123:216–24. doi: 10.1080/03009734.2018.1521890
Keywords: ureteropelvic junction, hydronephrosis, urinary tract infection, pain, children
Citation: Bilge I (2020) Symptomatology and Clinic of Hydronephrosis Associated With Uretero Pelvic Junction Anomalies. Front. Pediatr. 8:520. doi: 10.3389/fped.2020.00520
Received: 28 February 2020; Accepted: 22 July 2020;
Published: 30 September 2020.
Edited by:
Abdurrahman Onen, Onen Pediatric Urology Center, TurkeyReviewed by:
Baran Tokar, Eskişehir Osmangazi University, TurkeyCopyright © 2020 Bilge. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ilmay Bilge, aWJpbGdlQGt1LmVkdS50cg==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.