- 1St Mary's Hospital, Imperial College London, London, United Kingdom
- 2Pediatric Critical Care, BC Children's Hospital, Vancouver, BC, Canada
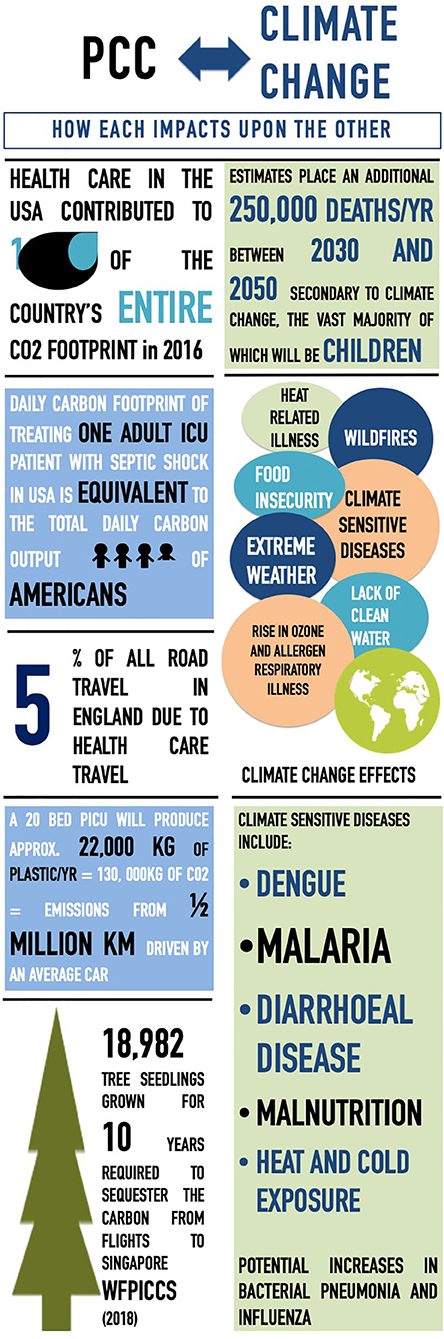
Critical care is perhaps one of the most “climate-intensive” divisions of health care. As greenhouse gas emissions continue to rise, the unprecedented threat of climate change has belatedly prompted an increased awareness of critical care's environmental impact. Within our role as pediatric critical care providers, we have a dual responsibility not only to care for children at their most vulnerable, but also to advocate on their behalf. There are clear, demonstrable effects of our worsening climate on the health of children, with the resultant increased burden of pediatric critical illness and disruption to health care systems. From increasing wildfires and their effect on lung health, to the spread of vector-borne diseases such as dengue, and the increased migration of children due to a changing climate, the effects of a changing climate are here, and we are beginning to see the changing epidemiology of pediatric critical illness. Ensuring that the effects of ongoing changes are minimized, including its future effects on child health, requires a multifaceted approach. As part of this review, we will use the Lancet Countdown on Climate Change indicators to explore the impact of pediatric critical care on climate change and the inevitable influence climate change will have on the future practice of pediatric critical care globally.
Introduction
The world is rapidly changing. Despite the signing of the Paris Agreement in 2015 (1), greenhouse gas emissions have continued to rise (2), and if current trends continue, global warming is likely to reach 1.5°C between 2030 and 2052 (3). The Intergovernmental Panel on Climate Change Working Group 1 in 2013 stated the warming of the climate system is unequivocal and that human influence was the dominant cause (4). With limited progress toward the United Nations Sustainable Development Goal 13 (5), the current and future detrimental effect on health is felt to be irrefutable (6–9), despite the fragmented evidence base, particularly in low-income countries (10). In 2004, ~0.2% of global deaths were attributable to climate change, 85% of which were children (11). Current estimates place an additional 250,000 deaths per year between 2030 and 2050 secondary to climate change, the vast majority of which will be under the age of 5 years (12). Children are projected to bear 88% of the burden of the disease related to climate change (13, 14). With this clear direct impact on children's well-being, many consider the anthropogenic global warming a violation of the rights of future people (15).
Health professionals occupy a privileged position and are ideally placed to not only provide compelling examples of the medical consequences of climate change (16) but also inform policies that aim to mitigate its effects (17, 18). As pediatric intensive care providers, working in perhaps one of the most climate-intensive divisions of health care, we have yet to adequately prepare for the changing burden of critical illness; nor have we taken the appropriate actions to mitigate this eventuality. Our role in advocacy and as ambassadors of change, both within our institutions and across our larger communities, is essential, especially considering the substantial contribution of the health care sector to a nation's greenhouse gas emissions (19–21), the increasing awareness of the environmental impact of critical care (22–25), and the general lack of literature on climate change and health (6). We all have a duty to conserve and improve the planet for future generations. This is something the entire medical community can support, irrespective of their interpretation of the evidence related to climate change.
The direct and indirect impacts of COVID-19 on global child health are likely to be devastating for years to come. The extensive measures imposed, however, during the pandemic have led to dramatic reductions in air pollution in many major cities of the world, and the hope is that this could be a real turning point in tackling climate change. Over the coming months and years, economies will need to be reset, international travel remains restricted compared to previous, and government priorities shifted. An opportune moment therefore exists to promote, advocate, and prioritize local, national, and global efforts to tackle climate change.
The consequences of a changing climate are here, with implications for all and will only escalate in coming years. The burden, however, will fall heaviest on the vulnerable populations in low- and middle-income countries (LMICs). Compromised air quality from increasing wildfires and their effect on lung health (26), altered patterns of spread of vector-borne diseases such as dengue (27), and food insecurity and lack of clean drinking water (10), the impact of climate change upon global child health is severe. Ensuring that these effects are minimized, including its future impact on child health, requires a multifaceted approach. What can we do therefore as practitioners to not only reduce our input into the climate emergency but also respond to the already initiated changes? The “Lancet Countdown: Tracking Progress on Health and Climate Change” is a global collaboration tracking progress of a number of indicators across five domains relating to health, climate change, and their implications for national governments (6). As part of this review, we will use and highlight those Lancet indicators relevant to the care of critically ill children. The impact of pediatric critical care on climate change will be explored, and the inevitable influence climate change will have on the practice of pediatric critical care globally discussed (Figure 1).
Impact of Pediatric Critical Care on Climate Change.
• 2019 Lancet Countdown Indicator 3.9: mitigation in the health care sector, healthcare sector greenhouse gas emissions.
The health and social care sector of England represented 6.3% of the total nation's carbon footprint emissions in 2017. Almost two-thirds are accounted by supply chain emissions, one-fourth from core (including building's energy use), and one-eighth from the community including patient travel and staff commuting (21). In 2016, health care in the United States contributed to 10% of the country's entire CO2 footprint (19), 7% in Australia (20), and 3.5% in India (28). Globally, health care sectors were responsible for 4.4% of the global total CO2 emissions in 2014 (28). Significant progress can be made, however, with the implementation of legal targets and political will, as evidenced by the reduction in total health and social care emissions by 18.5% in England over the last decade (21, 29).
The total emissions per bed day in a critical care unit were calculated to be approximately equivalent to 9 kg of CO2 (CO2e) (not including heating, travel, or procurement) (30). Prior work has demonstrated the daily carbon footprint of treating one adult intensive care patient (178 kg CO2e) with septic shock in the United States to be equivalent to the total daily carbon output of 3.5 Americans (31). This was predominately accounted for by the heating, ventilation, and air conditioning.
Drug Manufacturing and Its Impact
Twelve percent of health-related carbon emissions in England originate from pharmaceuticals (21), of which critical care is a significant consumer. The majority of morphine's carbon footprint, perhaps the most commonly used pediatric intensive care unit (PICU) medication, was found to derive from sterilization and packaging, with the production of every 100 mg of morphine sulfate having an emission of 204 g CO2, equivalent to that of the emissions of driving 1 km in an average car (32). The overall carbon footprint of pharmaceuticals is high when consideration is given to the chemicals used, the degree of refinement required in factories, transportation costs, and the fact that a large proportion go to waste (33). Potential actionable routes for individual units, hospitals, and governments to take may include an environmental rating for drugs (34) and a preference to use those medications with a lower environmental impact.
Plastic Waste in Intensive Care Units
In the United States, health care is the second highest contributor to landfill and incinerators (24), with ~2.2 kg of waste produced per patient per day (35). A 10-bed Australian intensive care unit (ICU) at a 320-bed hospital produced 5% of total hospital waste, approximately, 44% of which was recyclable, with almost 60% of the ICU general waste suitable for recycling (36). A later audit revealed only 15% of the waste to be recyclable, with almost half (70 kg of 145 kg) actually recycled. The estimated cost was ~$13 per week (37). An average of 3.4 kg of single-use materials per patients per day (31) was used. This predominantly plastic produces, for a 20-bed PICU with 90% occupancy year-round, 22,338 kg of plastic annually, equivalent to 134,028 kg of CO2. For reference, this is approximately equivalent to the emissions from half a million kilometers driven by the average passenger car. Recycling itself is, however, energy-intensive, especially in a health care setting where high reprocessing standards must be met (38), and initial outlay high. Addressing this high initial cost may be difficult to justify, particularly in areas where resources are limited, and finances best diverted to actual patient care.
Theaters
Operating theaters are an appreciable source of greenhouse gas emissions, with the use of anesthetic gases and energy consumption primarily responsible (39). Anesthetic gases represent 1.7% of the carbon footprint for all acute National Health Service organizations (21). The use of desflurane or sevoflurane from modern anesthetic machine for 1 h is the same as 230 or 30 miles traveled in a modern car, respectively (40). Progressive elimination of desflurane led to a 24% reduction in greenhouse gas emissions associated with anesthetic gas use (41).
Travel and Transport
Telemedicine will likely play an increasing role in the care of acutely unwell children in the future (42), including promoting the virtual dissemination of knowledge, such as the well-attended World Sepsis Day virtual congress, up-skilling of local staff, and virtual meetings. It is already playing an increasing role in the fight against recent outbreaks. With health care–related travel accounting for around 5% of all road travels in England each year (21)—patient travel and staff commuting the largest contributory sources—limiting unnecessary travel and promoting work from home needs to be encouraged. There are limitations associated with the use of telemedicine in pediatric critical care, however, including the obvious inability to examine patients, privacy, and security concerns related to patient data and the initial setup cost.
An example of a direct contribution pediatric critical care has on climate change is air travel related to the World Federation of Pediatric Intensive and Critical Care Societies (WFPICCS) meetings. The carbon dioxide emissions were calculated for air travel to and from the meeting site for the nations with the 20 leading delegates. Carbon dioxide emissions were calculated according to the universally determined model, incorporating the type of airplane likely used and assuming an average occupancy of the plane. Emissions were calculated for 3,556 delegates for the three meetings (78.7% of the total 4,520 delegates). Total emissions for flying the majority of delegates to the three meetings were 760 tons for Istanbul, 856 tons for Toronto, and 1,148 tons for Singapore (Supplementary Table 1). For the purposes of large conferences, where a stated goal is to build community, virtual meetings likely do not satisfy these goals. Medical conferences will still play a role for advancing our field—research presented at meetings in face-to-face conversations is cited more highly than that which has not (43), and scientific progress in our field has direct impact on the lives of sick children, including those affected by a changing climate. The interpersonal relationships built through face-to-face contact are likely irreplaceable and not quantifiable (44).
Limiting our Climate Change Contribution
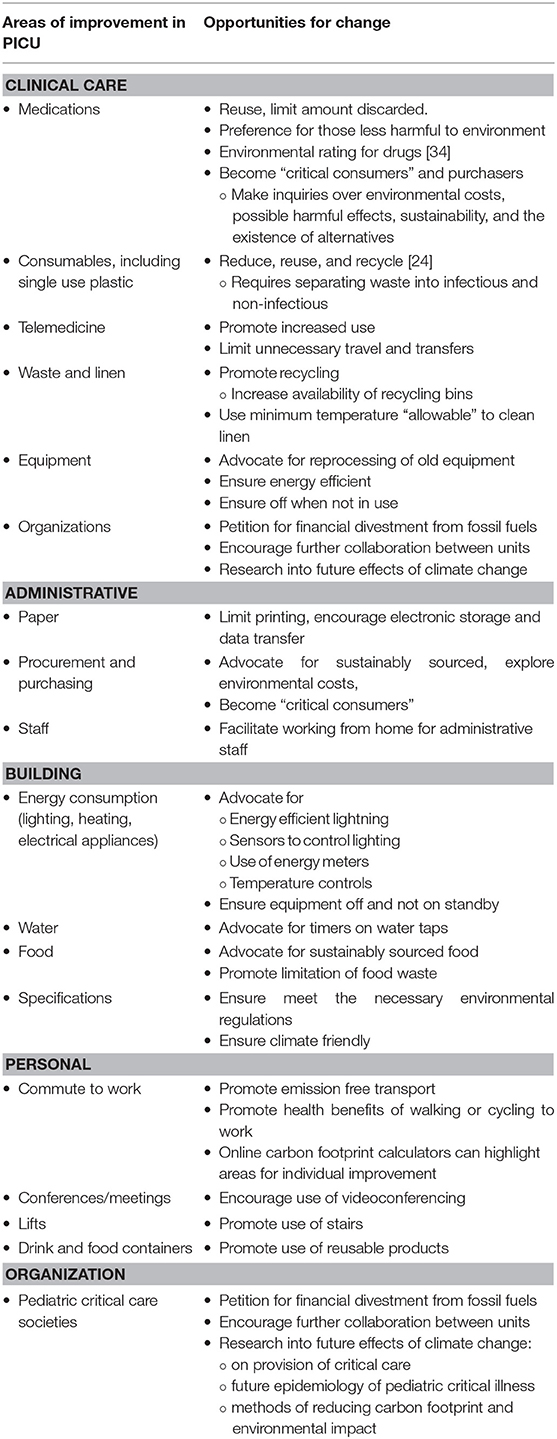
The pediatric critical care community needs to decide how best to lead the health care sector in advocacy and change (Table 1). As stewards of the health of children, our professional careers are directly linked to the future health of the planet, and we have an obligation to serve as role models for other fields. There is a compelling argument for the health sector to lead by example in implementing mitigation measures (45). A number of medical organizations have either passed resolutions calling for financial divestment from fossil fuel companies (46), produced statements on environmental sustainability (47), or written open letters to governments (48). Numerous staff surveys have revealed a willingness to engage in measures to reduce their environmental impact (21, 49, 50). The ability to reduce our dependence on plastic within in critical care is crucial, and we should all encourage recycling and safe reuse of equipment where practical. Local council members or hospital board members can be petitioned to ensure food and other purchases are sustainably sourced (24, 51), and that new building specifications abide by the World Health Organization (WHO) framework for climate-resilient health systems (52) and are climate-friendly (51). Promoting climate change as a health issue may have greater political and public resonance (53) and lead to better staff engagement.
As the costs, both monetary and environmental, of fossils fuels are likely to increase in the coming decades, as too will the costs to the health care sector (38), a significant consumer. The financial impact of climate-sensitive events is also substantial (54). Discussions at a local level will have to evaluate a multitude of factors including a cost-benefit analysis of the initial high startup expense and the long-term return on investment. When compared to the cost savings from the health and social benefits of these policies, however, including combatting health inequalities that will be exacerbated by climate change, the long-term cost of mitigation efforts required to stabilize climate change is thought to be relatively small over the long term (38, 45).
Impact of Climate Change on Pediatric Critical Care
At least seven of the Lancet Countdown indicators are implicated in the care of the critically ill child.
• 2019 Lancet Countdown Indicator 1.1: health and heat
• 2019 Lancet Countdown Indicator 1.2: health and extreme weather events
• 2019 Lancet Countdown Indicator 1.3: global health trends in climate-sensitive diseases
• 2019 Lancet Countdown Indicator 1.4: climate-sensitive infectious diseases
• 2019 Lancet Countdown Indicator 1.5: food security and under nutrition
• 2019 Lancet Countdown Indicator 3.3.1: exposure to air pollution in cities
• 2019 Lancet Countdown Indicator 3.3.2: premature mortality from ambient air pollution by sector
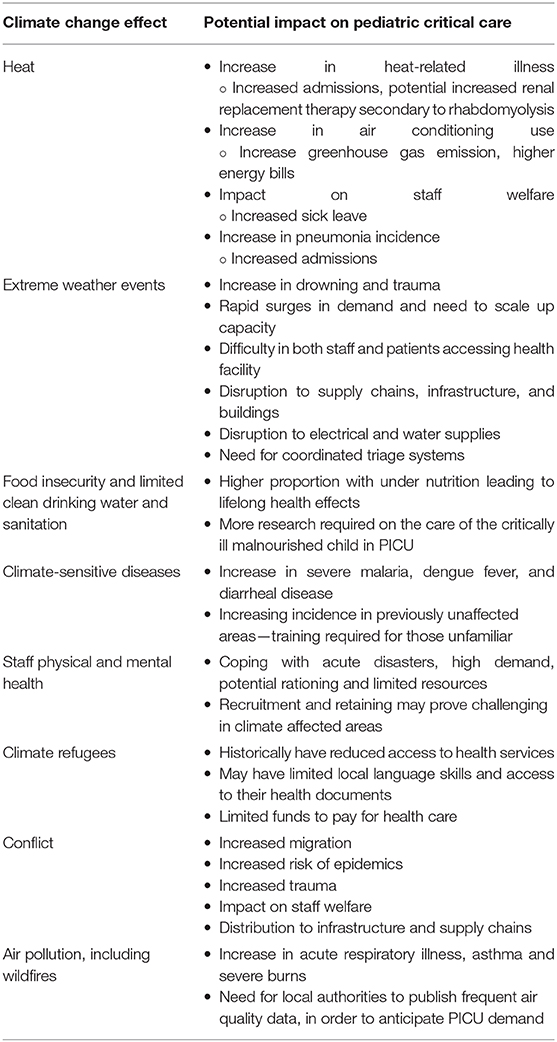
The dire effects of the climate emergency on global child health will impact pediatric critical care units worldwide. The degree to which climate change will alter the current daily running of an ICU is, however, unclear. With limited ability and infrastructure to mitigate the impact of climate change, those working in an LMIC setting will undoubtedly face the greatest challenges, while being the ones least responsible for its causes (Figure 2). The United Nations Environment found that nearly a quarter of all deaths globally in 2012 could be attributed to modifiable environmental risks, with a greater portion occurring in populations in a vulnerable situation and in developing countries (55).
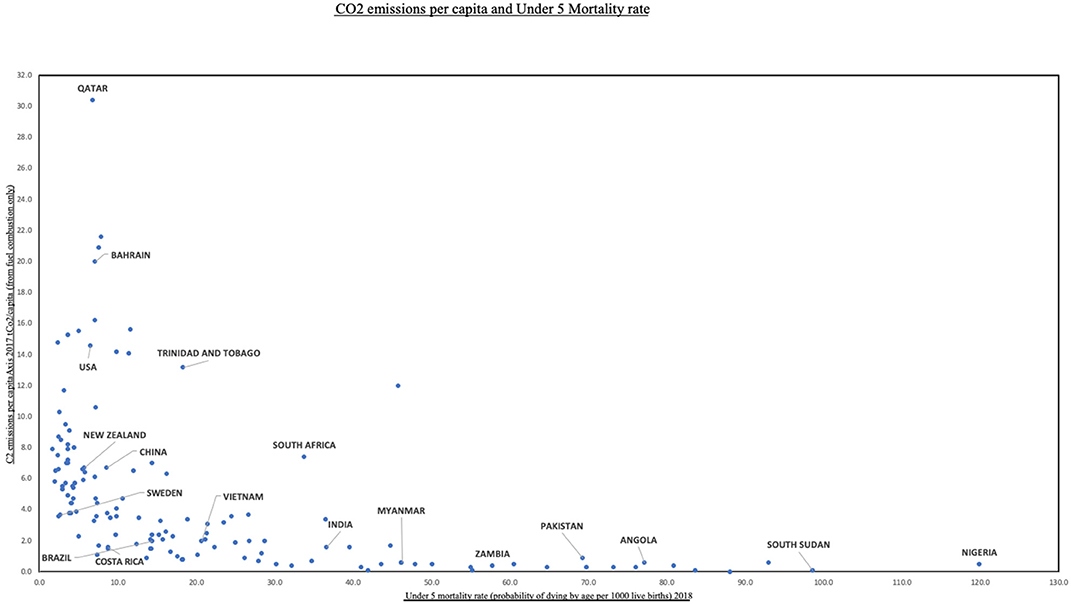
Figure 2. CO2 emissions per capita and under-5 mortality rate. Data from World Bank (https://data.worldbank.org/).
In Sub-Sahara Africa, total annual expenditure on health is commonly under US $25 per capita and often <3% of the gross domestic product, compared to 8.5% in the United States (56). With limited budgets and challenges accessing international climate finance for health, many nations do not have a national health and climate change strategy, let alone the means to implement it (57). Furthermore, the number of intensive care beds as a percentage of hospital beds is ~1.5% in LMICs compared to 2.5 to 9% in high-income countries (58). Concerns extend to dealing with increased and unexpected acute demand, blackouts caused by disruption to the power supply, increased air conditioning use if present, and coping with extreme heat (59). As the link between climate change and the increasing frequency of natural disasters and variable rainfall continues to be explored, the impact of both acute and longer-term weather events on medical care and societies in LMICs will be devastating. Loss of medical records, damage to water supplies and sanitation, and interruption to medical supply chains from extreme weather events are real and pressing fears (60, 61). In addition, health access for climate refugees may be restricted, and staff and patients experience great difficulties in physically accessing the hospital (62) secondary to natural disasters. At present, 1.6 billion people live in places where protracted crises (including famine, conflict, drought, and population displacement), and weak health care services leave them without access to basic care (63).
Heat and Air Pollution
An inability to care for oneself, the presence of a chronic illness, and certain medications (including diuretics) are all risk factors for heat illness (64, 65). These are clearly relevant to a high proportion of children who are unable to modify their exposure risk and are at a greater risk of dehydration (66). Those with cardiac, respiratory, or renal disorders are at increased risk and will form an increasing proportion of the pediatric critical care population as non-communicable disease rates rise, particularly with a lack of air conditioning for many children in LMICs (65).
With a rise in ambient temperatures and wildfires, levels of ozone, allergens, and other pollutants will increase, potentially triggering acute asthma exacerbations (66–68). Nine out of 10 people already breathe polluted air every day, and in 2019, the WHO deemed air pollution as the greatest environmental risk to health (63). Working on action plans prior to discharge is therefore paramount and may include staying indoors and avoiding unnecessary outdoor activity on poor air quality days (67). Advocating for widespread dissemination of information on air quality, exploring non-polluting methods of inhaler delivery and advance planning for extreme weather events are essential.
Changing Weather and Infectious Diseases
A number of diseases have been deemed climate-sensitive including dengue, malaria, diarrhea, heat and cold exposure, and protein-energy malnutrition. Deaths from malaria, diarrheal disease, and malnutrition are all currently decreasing (6). However, because of changes in vector distribution and environmental suitability (6, 69), vector-borne diseases are emerging in previously unaffected regions. Of particular relevance to pediatric critical care is the rapid increase in dengue fever (6), especially in South East Asia. The incidence and severity of respiratory infections may alter over the coming years, with potential increases in bacterial pneumonia and influenza and a reduction in respiratory syncytial virus during the milder winters (70). Managing this population of high-risk, critically unwell individuals with little physiological reserve in settings with strained health systems due to acute weather events, migration, or conflict will be challenging and require a global coordinated response. In addition to the potentially disrupted medical and utilities infrastructures, a compromised vaccination program and restricted medication availability are all prime breeding grounds for epidemics (71). Higher temperatures and humidity will lead to an increased risk of food and water borne diseases (17).
Responding to Health Impacts of Climate Change
Pediatric critical care practitioners should anticipate a number of variations in their workload as climate change takes a progressive hold. Indeed, a large survey of American Thoracic Society members indicated many had already observed health impacts of climate change among their patients (50), and other reports reveal its current adverse effect on health care and health care systems (8, 9, 54, 72). A rise in demand, with a predominance of heat-related disorders, respiratory illness, and climate-sensitive diseases, interspersed with the direct and indirect effects of extreme weather events on health and infrastructure, will challenge us all (Table 2).
Critical care skills and experience are relevant to each of the WHO's six common “building blocks” for health systems, although importantly critical care is not limited to the ICU. The timely provision of antibiotics to a child with pneumonia is every bit as critical as establishing a periarrest patient on extracorporeal life support (73), and the occurrence of the former will be of vital importance to the vast majority affected by climate change.
Our role in the anticipation and response to current and future health impacts of climate change is essential, as is our involvement in the development of climate-resilient health systems. We have a powerful voice to advocate locally and nationally for change, not only to raise awareness but also to promote partnerships, encourage scientific research, and aid the strengthening of health systems (57). As a field, we need to adapt to this emerging threat and work cohesively with other organizations to first formally recognize the urgent need for action and, second, instigate partnerships and plans to mitigate its effect. We should ensure that staff, our units, hospitals, and local authorities are all aware of the likely impact climate change will have on us all over the coming years and the increased demand on critical care resources and services that will ensue. As a collaboration, tracking PICU-specific Lancet Countdown metrics, both at a local and national level, would inform health care providers and policy holders of progress made toward a sustainable and carbon neutral future, ultimately keeping us accountable to the critically ill children worldwide we strive to care for.
Conclusion
Climate change will have profound, acute, and long-term detrimental effects on the children of today and in the future. As members of the pediatric critical care community, we have a duty to defend and improve upon global child health. Our likely presence at the climate frontier, especially during acute events, demands that we play a pivotal role in mitigating and adapting to the effects of climate change on the critically ill child. Promoting research into climate change and its complex interaction with health is vital, expanding the evidence base and allowing governments and organizations to make informed choices regarding mitigation strategies. Critical care–specific climate studies would allow us as a profession to mitigate, prepare, advocate, and inform future policies. High initial short-term mitigation costs will likely be outweighed by future health benefits. How the current COVID-19 pandemic affects the progression of climate change is as yet unknown, but the reset to society provides an opportune moment to reinvigorate efforts and focus minds once more.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author Contributions
GW and SM were involved in article conception. GW was responsible for the first draft of the manuscript. Both were involved in drafting and editing the final manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2020.00472/full#supplementary-material
References
1. United Nations. Paris Agreement. Paris, France: United Nations Framework Convention on Climate Change (2015).
2. United Nations Development Programme (UNDP). The Heat Is On. Taking stock of Global Climate Ambition. (2019) Available online at: https://unfccc.int/news/the-heat-is-on-taking-stock-of-global-climate-ambition (accessed Nov 1, 2019).
3. Masson-Delmotte V, Zhai P, Pörtner HO, Roberts D, Skea J, Shukla PR, et al. Summary for Policymakers. In: Global Warming of 1.5°C. An IPCC Special Report on the Impacts of Global Warming of 1.5°C Above Pre-Industrial Levels and Related Global Greenhouse Gas Emission Pathways, in the Context of Strengthening the Global Response to the Threat of Climate Change, Sustainable Development, and Efforts to Eradicate Poverty.
4. IPCC. Climate change 2013: the physical science basis. In: Stocker TF, Qin D, Plattner G-K, Tignor M, Allen SK, Boschung J, M. Midgley, et al. editors. Contribution of Working Group I To The Fifth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge, United Kingdom, New York, NY: Cambridge University Press (2013). p. 1535.
5. United Nations. Report of the Secretary-General on SDG Progress. Special Edition. World Health Organization (2019). Available online at: https://sustainabledevelopment.un.org/sdg13 (accessed July 4, 2020).
6. Watts N, Amann M, Arnell N, Ayeb-Karlsson S, Belesova K, Boykoff M, et al. The 2019 report of the lancet countdown on health and climate change: ensuring that the health of a child born today is not defined by a changing climate. Lancet. (2019) 394:1836–78. doi: 10.1016/S0140-6736(19)32596-6
7. McMichael A, Woodruf R, Hales S. Climate change and human health: present and future risks. Lancet. (2006) 367:859–69. doi: 10.1016/S0140-6736(06)68079-3
8. Ebi KL, Ogden NH, Semenza JC, Woodward detecting A and attributing health burdens to climate change. Environ Health Perspect. (2017) 125:085004. doi: 10.1289/EHP1509
9. Mitchell DM, Heaviside C, Vardoulakis S, Huntingford C, Masato G, Guillod BP, et al. (2016). Attributing human mortality during extreme heat waves to anthropogenic climate change. Environ Res Lett. 11:074006 doi: 10.1088/1748-9326/11/7/074006
10. Haines A, Ebi K. The imperative for climate action to protect health. N Engl J Med. (2019) 380:263–73. doi: 10.1056/NEJMra1807873
11. World Health Organization. Global Health Risks: Mortality and Burden of Disease Attributable To Selected Major Risks. Geneva: World Health Organization (2009).
12. World Health Organization. Quantitative Risk Assessment of the Effects of Climate Change on Selected Causes of Death, 2030s and 2050s. Geneva: World Health Organization. (2014)
13. Zhang Y, Bi P, Hiller JE. Climate change and disability-adjusted life years. J Environ Health. (2007) 70:32–6.
14. Patz JA, Gibbs HK, Foley JA, Rogers JV, Smith KR. Climate change and global health: quantifying a growing ethic. EcoHealth. (2007) 4:397–405. doi: 10.1007/s10393-007-0141-1
15. Amnesty International (n.d.). Climate change. Available online at: https://www.amnesty.org/en/what-we-do/climate-change (accessed March 29, 2019).
16. Chivian E. Why doctors and their organisations must help tackle climate change: an essay by Eric Chivian. BMJ. (2014) 348:g2407. doi: 10.1136/bmj.g2407
17. Patz JA, Frumkin H, Holloway T, Vimont DJ, Haines A. Climate change: challenges and opportunities for global health. JAMA. (2014) 312:1565–80. doi: 10.1001/jama.2014.13186
18. Haines A, Dora C. How the low carbon economy can improve health. BMJ. (2012) 344:e1018. doi: 10.1136/bmj.e1018
19. Eckelman M, Sherman J. Estimated global disease burden from US health care sector greenhouse gas emissions. Am J Public Health. (2017) 108:S120–22. doi: 10.2105/AJPH.2017.303846
20. Malik A, Lenzen M, McALister S, McGain F. The carbon footprint of Australian health care. Lancet Planet Health. (2018) 2:e27–35. doi: 10.1016/S2542-5196(17)30180-8
21. NHS Sustainable Development Unit. NHS carbon footprint. (2018) Available online at: https://www.sduhealth.org.uk/policy-strategy/reporting/nhscarbon-footprint.aspx (accessed November 2, 2019).
22. Sneyd JR, Montgomery H, Pencheon D. The anaesthetist and the environment. Anaesthesia. (2010) 65:435–7. doi: 10.1111/j.1365-2044.2010.06332.x
23. Sherman J, McGain F. Environmental sustainability in anesthesia. Adv Anesth. (2016) 34:47–61. doi: 10.1016/j.aan.2016.07.004
25. Huffling K, Schenk E. Environmental sustainability in the intensive care unit: challenges and solutions. Crit Care Nurs Q. (2014) 37:235–50. doi: 10.1097/CNQ.0000000000000028
26. Kunzli N, Avol E, Wu J, Gauderman WJ, Rappaport E, Millstein J, et al. Health effects of the 2003. Southern California wildfires on children. Am J Respir Crit Care Med. (2006) 174:1221–8. doi: 10.1164/rccm.200604-519OC
27. Campbell LP, Luther C, Moo-Llanes D, Ramsey JM, Danis-Lozano R, Peterson AT. Climate change influences on global distributions of dengue and chikungunya virus vectors. Philos Trans R Soc Lond B Biol Sci. (2015) 370:1665. doi: 10.1098/rstb.2014.0135
28. Pichler P, Jaccard I, Weisz U, Weisz H. International comparison of health care carbon footprints. Environ Res Lett. (2019) 14:064004. doi: 10.1088/1748-9326/ab19e1
30. Pollard AS, Paddle JJ, Taylor TJ, Tillyard A. The carbon footprint of acute care: how energy intensive is critical care? Public Health. (2014) 128:771–6. doi: 10.1016/j.puhe.2014.06.015
31. McGain F, Burnham JP, Lau R, Aye L, Kollef MH, McAlister S. The carbon footprint of treating patients with septic shock in the intensive care unit. Crit Care Resusc. (2018) 20:304–12.
32. McAlister S, Ou Y, Neff E, Hapgood K, Story D, Mealey P, et al. The environmental footprint of morphine: a life cycle assessment from opium poppy farming to the packaged drug. BMJ Open. (2016) 6:e013302. doi: 10.1136/bmjopen-2016-013302
34. Pierce JMT, Bourton L. Doctors need an environmental rating system for drugs. BMJ. (2019) 367:l6208. doi: 10.1136/bmj.l6208
35. Tudor TL, Marsh CL, Butler S, Van Horn JA, Jenkin LE. Realising resource efficiency in the management of healthcare waste from the Cornwall National Health Service (NHS) in the UK. Waste Manag. (2008) 28:1209–18. doi: 10.1016/j.wasman.2007.04.004
36. McGain F, Story D, Hendel S. An audit of intensive care unit recyclable waste. Anaesthesia. (2009) 64:1299–302. doi: 10.1111/j.1365-2044.2009.06102.x
37. Kubicki MA, McGain F, O'Shea CJ, Bates S. Auditing an intensive care unit recycling program. Crit Care Resusc. (2015) 17:135–40.
38. Jameton A. Medicine's role in mitigating the effects of climate change. Virtual Mentor. (2009) 11:465–9. doi: 10.1001/virtualmentor.2009.11.6.msoc1-0906
39. MacNeill AJ, Lillywhite R, Brown CJ. The impact of surgery on global climate: a carbon footprinting study of operating theatres in three health systems. Lancet Planet Health. (2017) 1:e381–8. doi: 10.1016/S2542-5196(17)30162-6
40. Ryan SM, Nielsen CJ. Global warming potential of inhaled anesthetics: application to clinical use. Anesth Analg. (2010) 111:92–8. doi: 10.1213/ANE.0b013e3181e058d7
41. Kaiser Permanente. Climate Action. (2019) Available online at: https://about.kaiserpermanente.org/community-health/news/greener-anesthesia-making-a-difference (accessed November 12, 2019).
42. Holmner A, Ebi KL, Lazuardi L, Nilsson M. Carbon footprint of telemedicine solutions–unexplored opportunity for reducing carbon emissions in the health sector. PLoS ONE. (2014) 9:e105040. doi: 10.1371/journal.pone.0105040
43. de Leon Fernanda LL, Mcquillin B. The Role of Conferences on the Pathway to Academic Impact: Evidence From a Natural Experiment. (2018) Available online at: https://ssrn.com/abstract=2507361 (accessed March 20, 2018).
44. Lee K, Brownstein JS, Mills RG, Kohane IS. Does collocation inform the impact of collaboration? PLoS ONE. (2010) 5:e14279 doi: 10.1371/journal.pone.0014279
45. World Health Organization. Promoting Health While Mitigating Climate Change. (2015) Available online at: https://www.who.int/globalchange/publications/briefing-health-mitigating/en/ (accessed May 25, 2020).
46. Arabena K, Armstrong F, Berry H, Brooks P, Capon T, Crabb B, et al. Australian health professionals' statement on climate change and health. Lancet. (2018) 392:2169–70. doi: 10.1016/S0140-6736(18)32610-2
47. McGain F, Ma SC, Burrell RH, Percival VG, Roessler P, Weatherall AD, et al. Why be sustainable? the Australian and New Zealand College of anaesthetists professional document ps64: statement on environmental sustainability in anaesthesia and pain medicine practice and its accompanying background paper. Anaesth Intensive Care. (2019) 47:413–22. doi: 10.1177/0310057X19884075
48. Jones B. Doctors sign open letter demanding government action on climate change. BMJ. (2019) 366:l4696. doi: 10.1136/bmj.l4696
49. Petre MA, Bahrey L, Levine M, van Rensburg A, Crawford M, Matava C. A national survey on attitudes and barriers on recycling and environmental sustainability efforts among Canadian anesthesiologists: an opportunity for knowledge translation. Can J Anaesth. (2019) 66:272–86. doi: 10.1007/s12630-018-01273-9
50. Sarfaty M, Bloodhart B, Ewart G, Thurston GD, Balmes JR, Guidotti TL, et al. American Thoracic Society member survey on climate change and health. Ann Am Thorac Soc. (2015) 12:274–8. doi: 10.1513/AnnalsATS.201410-460BC
51. World Health Organization. Reducing the Carbon Footprint of Hospital-Based Care. Healthy Hospitals, Healthy Planet, Healthy People: Addressing Climate Change in Healthcare Settings. WHO (2009) Available online at: www.who.int/globalchange/publications/ climatefootprint_report.pdf (accessed November 10, 2019).
52. World Health Organization. Operational Framework for Building Climate Resilient Health Systems. Geneva: World Health Organization. (2015).
53. Wang H, Horton R. Tackling climate change: the greatest opportunity for global health. Lancet. (2015) 386:1798–9. doi: 10.1016/S0140-6736(15)60931-X
54. Limaye VS, Max W, Constible J, Knowlton K. Estimating the health-related costs of 10 climate-sensitive U.S. events during 2012. GeoHealth. (2019) 3:245–65. doi: 10.1029/2019GH000202
55. UN Environment. Global Environment Outlook – GEO-6: Summary for Policymakers. Cambridge, GB: Cambridge University Press (2019).
56. World Health Organization. Domestic general government health expenditure (GGHE-D) as percentage of gross domestic product (GDP) (%) Data by country, 2015. Available online at: http://apps.who.int/gho/data/node.main.GHEDGGHEDGDPSHA2011?lang=en (accessed July 4, 2020).
57. World Health Organization. Who Health And Climate Change Survey Report: Tracking Global Progress. Geneva: World Health Organization (2019).
58. Murthy S, Leligdowicz A, Adhikari NK. Intensive care unit capacity in low-income countries: a systematic review. PLoS ONE. (2015) 10:e0116949. doi: 10.1371/journal.pone.0116949
59. Kjellstrom T, Holmer I, Lemke B. Workplace heat stress, health and productivity - an increasing challenge for low and middle-income countries during climate change. Glob Health Action. (2009) 2. doi: 10.3402/gha.v2i0.2047
60. World Health Organization. Available online at: https://www.who.int/activities/making-health-facilities-safe-in-emergencies (accessed November 3, 2019).
61. Paterson J, Berry P, Ebi K, Varangu L. Health care facilities resilient to climate change impacts. Int J Environ Res Public Health. (2014) 11:13097–116. doi: 10.3390/ijerph111213097
62. Lancet Oncology. Climate change and non-communicable diseases. Lancet Oncol. (2016) 17:1. doi: 10.1016/S1470-2045(15)00568-9
63. World Health Organization. Available online at: https://www.who.int/news-room/feature-stories/ten-threats-to-global-health-in-2019 (accessed January 10, 2020).
64. Hajat S, O'Connor M, Kosatsky T. Health effects of hot weather: from awareness of risk factors to effective health protection. Lancet. (2010) 375:856–63. doi: 10.1016/S0140-6736(09)61711-6
65. Kovats RS, Hajat S. Heat stress and public health: a critical review. Annu Rev Public Health. (2008) 29:41–55. doi: 10.1146/annurev.publhealth.29.020907.090843
66. Philipsborn RP, Chan K. Climate change and global child health. Pediatrics. (2018) 141:e20173774. doi: 10.1542/peds.2017-3774
67. Guarnieri M, Balmes JR. Outdoor air pollution and asthma. Lancet. (2014) 383:1581–92. doi: 10.1016/S0140-6736(14)60617-6
68. Guan WJ, Zheng XY, Chung KF, Zhong NS. Impact of air pollution on the burden of chronic respiratory diseases in China: time for urgent action. Lancet. (2016) 388:1939–51. doi: 10.1016/S0140-6736(16)31597-5
69. Medlock JM, Leach SA. Effect of climate change on vector-borne disease risk in the UK. Lancet Infect Dis. (2015) 15:721–30. doi: 10.1016/S1473-3099(15)70091-5
70. Mirsaeidi M, Motahari H, Taghizadeh Khamesi M, Sharifi A, Campos M, Schraufnagel DE. Climate change and respiratory infections. Ann Am Thorac Soc. (2016) 13:1223–30. doi: 10.1513/AnnalsATS.201511-729PS
71. Watts N, Adger WN, Agnolucci P, Blackstock J, Byass P, Cai W, et al. Health and climate change: policy responses to protect public health. Lancet. (2015) 386:1861–914. doi: 10.1016/S0140-6736(15)60854-6
72. USGCRP. The impacts of climate change on human health in the United States. In: Crimmins A, Balbus J, Gamble JL, Beard CB, Bell JE, Dodgen D, et al. editors. A Scientific Assessment. Washington, DC: US Global Change Research Program (2016). p. 312.
Keywords: climate change, pediatric critical care, global health, global warming, pediatric emergencies
Citation: Wooldridge G and Murthy S (2020) Pediatric Critical Care and the Climate Emergency: Our Responsibilities and a Call for Change. Front. Pediatr. 8:472. doi: 10.3389/fped.2020.00472
Received: 30 April 2020; Accepted: 06 July 2020;
Published: 20 August 2020.
Edited by:
Ndidiamaka L. Musa, University of Washington, United StatesReviewed by:
Robert Kelly, Children's Hospital of Orange County, United StatesAsha N. Shenoi, University of Kentucky, United States
Copyright © 2020 Wooldridge and Murthy. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gavin Wooldridge, Z2Z3b29sZHJpZGdlQGdtYWlsLmNvbQ==
 Gavin Wooldridge
Gavin Wooldridge Srinivas Murthy
Srinivas Murthy