- 1Fondazione IRCCS Ca' Granda Ospedale Maggiore Policlinico, NICU, Milan, Italy
- 2Department of Clinical Sciences and Community Health, University of Milan, Milan, Italy
- 3Fondazione IRCCS Ca' Granda Ospedale Maggiore Policlinico, Epidemiology Unit, Milan, Italy
- 4Fondazione IRCCS Ca' Granda Ospedale Maggiore Policlinico, Direzione Professioni Sanitarie, Milan, Italy
Background: The importance of rooming-in in promoting breastfeeding initiation and continuation within the 10 Steps for Successful Breastfeeding is widely acknowledged. However, adherence to this practice by healthcare facilities is lower than that of other Steps. A deeper knowledge of maternal rooming-in experience has been advocated to identify the most effective rooming-in policies, thus enabling mothers to have a positive experience when practicing it in the postpartum period.
Aim: To investigate maternal knowledge of rooming-in and the most frequently encountered barriers and possible facilitators of adherence to the practice, according to their experience.
Study Design and Methods: We enrolled mothers who delivered healthy term or late preterm infants during the month of January 2019 in a tertiary referral center for neonatal care in Milan, Italy. At discharge, a structured interview about mothers' rooming-in experience was administered by healthcare professionals. Basic subjects' characteristics and mode of feeding were recorded.
Results: The enrolled population included 328 mothers and 333 neonates. The great majority of mothers knew of rooming-in and 48.2% practiced it continuously. The 86.3% of mothers was aware of the beneficial effects of rooming-in; promotion of mother-infant bonding, increased confidence in taking care of the baby and ability to recognize baby's feeding cues were the most frequently cited, whereas improving breastfeeding was reported by a limited number of mothers, unless they were asked a specific question about it. The main reported obstacles were fatigue (40.5%) and cesarean section related difficulties (15.5%); night was the most critical time of the day for rooming-in. Strategies suggested by mothers for improving rooming-in were increased assistance to the dyad, organizational and structural changes and the possibility to have a family member during the night. Additionally, mothers who adhered to rooming-in practice continuously during hospital stay had a higher exclusive breastfeeding rate at discharge compared to mothers who did not.
Conclusions: Our study contributes to a deeper knowledge of maternal rooming-in experience in an Italian tertiary maternity. We underline the importance of providing a tailored support to the mother-infant dyad in order to overcome rooming-in barriers perceived by mothers and promote a positive rooming-in experience.
Introduction
The Baby Friendly Hospital Initiative (BFHI), launched by WHO/UNICEF in 1991 (1), is a global Initiative with the specific purpose of implementing evidence-based maternity healthcare services to protect, promote, and support breastfeeding. Since the BFHI began, its implementation has led to an improvement in the rates of initiation, exclusive breastfeeding and breastfeeding duration in many Countries (2–6).
The implementation of the BFHI strongly relies on the application of the Ten Steps for Successful Breastfeeding, first introduced in the 1989 WHO/UNICEF joint statement Protecting, Promoting, and Supporting Breastfeeding (7, 8). The evidence-based impact of the BFHI on breastfeeding (2, 3, 5, 6, 9) has shown a strong correlation with the number of Steps experienced (10), indicating that a collection of maternal practices has a stronger impact on breastfeeding than each one of them taken individually (6). Nonetheless, the degree of application of the 10 Steps varies widely between facilities (11).
Rooming-in is the practice of enabling mothers and their newborn babies to be together after birth day and night, 24 h a day, during hospital stay (8). Rooming-in has a great potential for improving mother-baby bonding, increasing mothers' confidence and decreasing psychological stress (12–14). Furthermore, sharing the room with her baby, a mother learns to recognize and promptly respond to the baby's early feeding cues, thus facilitating initiation and continuation of breastfeeding (15, 16). However, the implementation of this practice by healthcare facilities has been reported as lower than that of other Steps (such as Step 3-antenatal care, 5-breastfeeding support, and 8-responsive feeding) (11).
While organizational factors and negative healthcare professionals' attitude (11, 17) have been identified as barriers to rooming-in implementation, maternal rooming-in experience has not been extensively investigated (18) and attention has shifted from what mothers thought of rooming-in (14, 19) to what they and their babies could gain from it (20, 21). A deeper knowledge of maternal rooming-in experience has been therefore advocated to identify the most effective rooming-in policies, thus enabling mothers to have a positive experience, within a supportive environment, when practicing it in the post-partum period.
The aim of this study was to investigate the maternal knowledge of rooming-in and the most frequently encountered barriers and possible facilitators of adherence to the practice according to their experience.
Materials and Methods
Design and Setting
We performed a survey study during the month of January 2019 in the postnatal unit of a tertiary referral center for neonatal care (Fondazione IRCCS Ca' Granda Ospedale Maggiore Policlinico, Milan, Italy) that covers around 6,000 deliveries per year. The Fondazione promotes and supports breastfeeding in all mother-infant dyads throughout the hospital stay, following the principles of the BFHI (1). According to our internal protocol, term (370/7-416/7 weeks) and late preterm (340/7-366/7 weeks) infants with a birth weight ≥1,800 g stay in the same room as the mothers provided that their clinical conditions are stable. To facilitate the stay of mothers and their babies in the same room as continuously as possible, mothers are supported and guided through the following strategies. At admission, all mothers are informed about the importance of rooming-in and the role of the nursery as a place where they can receive help and advice, if needed. Mother-baby contact is encouraged especially at night: healthcare professionals are trained to provide indications and support to mothers to ensure they breastfeed during the night, informing them of the value, both quantity and quality-wise, of night-time feedings, and showing them how to breastfeed while lying down. Partners are allowed in the dyad's room from 8 am to 8 pm, in a family centered care perspective, whereas other family members and friends can visit from 12 pm to 8 pm (with the suggestion of limiting the number of people visiting to a maximum of 2 at a time).
Mothers and other family members are thoroughly informed on newborn safety policies, including the prevention of accidental falls and post-natal collapse. All routine care is performed in the mother-baby room, with the exception of the pre-discharge metabolic screening, which is performed at the nursery, in the presence of at least one parent. Our post-natal unit comprises 32 double rooms and a triple room, which can host a total of 67 mothers; each room has its own private bathroom. The infant's crib is placed beside the mother's bed. The average length of hospital stay, in the absence of maternal or neonatal medical complications, is 72 h after spontaneous deliveries and 96 h after cesarean sections.
The institutional Ethics Committee approved the present study and mothers provided written informed consent.
Sample
Out of the 466 mothers who delivered healthy term and late preterm neonates during the month of January 2019, we enrolled 328 mothers with an adequate oral comprehension of the Italian language. We considered as exclusion criteria any clinical condition of the newborn requiring specific support or the need to be monitored (hospitalization in the neonatal intensive care unit, congenital malformations, genetic conditions, respiratory problems, neurologic diseases, metabolic conditions, or gastrointestinal problems) or any possible maternal condition that would pose an obstacle to rooming-in (diseases or complications requiring attendance in other Units, severe psychiatric conditions, drug abuse).
Data Collection and Procedures
At discharge, enrolled mothers were administered a structured interview, which lasted ~10 min, by two healthcare professionals. The responses were transcribed as mothers answered, but not audio-recorded. The structured interview was previously administered to a sample of 50 Italian mothers and 10 foreign Italian-speaking mothers, whose answers were not included in the analysis, in order to identify any possible issue in the items' comprehension.
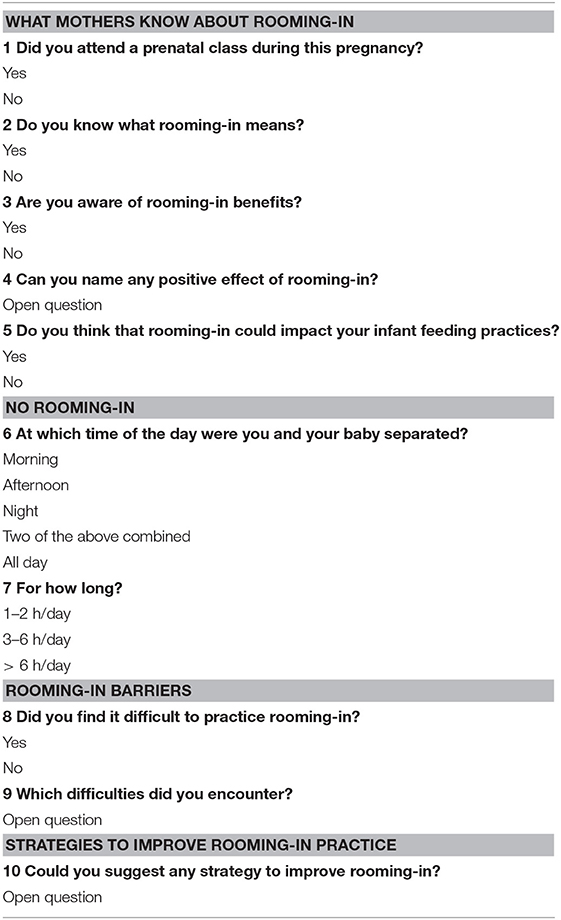
Specifically, the interview consisted of 10 items, both closed-ended and open-ended questions (Table 1). The first 3 items investigated maternal attendance to prenatal classes, their knowledge of rooming-in [as defined by United Nations Children's Fund & World Health Organization (8)] and awareness of its benefits [as described by UNICEF (22)]. Item number 4 asked to state the positive effects of this practice and item number 5 explicitly inquired if mothers were aware of the impact of rooming-in on their infant feeding practices. Items 6 and 7 investigated which time of the day mothers preferred not to practice rooming-in and for how long. Item number 8 asked if mothers had encountered any kind of difficulties during rooming-in practice, and item number 9 asked to specify which those problems were. Finally, in item number 10 mothers were encouraged to suggest strategies to improve rooming-in practice. Infants' computerized medical charts (Neocare, i & t Informatica e Tecnologia Srl, Italy) and obstetric charts were used to collect the basic characteristics of newborns and mothers (i.e., gestational age and birth weight, ethnicity, maternal age and education, parity), mode of feeding and rooming-in duration. Hospital staff keeps daily records of rooming-in time in infants' medical charts. According to the WHO definitions (23, 24) we considered exclusive breastfeeding the administration of no other food or drink, not even water, except breastmilk, and rooming-in the practice of enabling mothers and infants to be together 24 h a day during hospital say. Going to the nursery to ask for help or advice was not considered “no rooming-in.”
Statistical Analysis
Categorical variables were expressed as numbers (frequencies) and compared using the χ2 test. Continuous variables were expressed as mean ± standard deviation (SD) and tested between subgroups with the independent samples t-test and non-parametric tests, as appropriate. The subgroups analyzed were: Italian mothers vs. foreign mothers, primiparous vs. multiparous, mothers ≤34 vs. >34 years (mean age of the population), maternal years of education ≤13 (primary school, secondary school or high school diploma) vs. >13 years (university degree). A p < 0.05 was considered statistically significant.
The data reported in the open-ended questions (4, 9, 10) items were categorized by content analysis into similar ones.
Statistical analysis was performed with SPSS version 21 statistic software package (SPSS Inc., Chicago, IL, USA).
Results
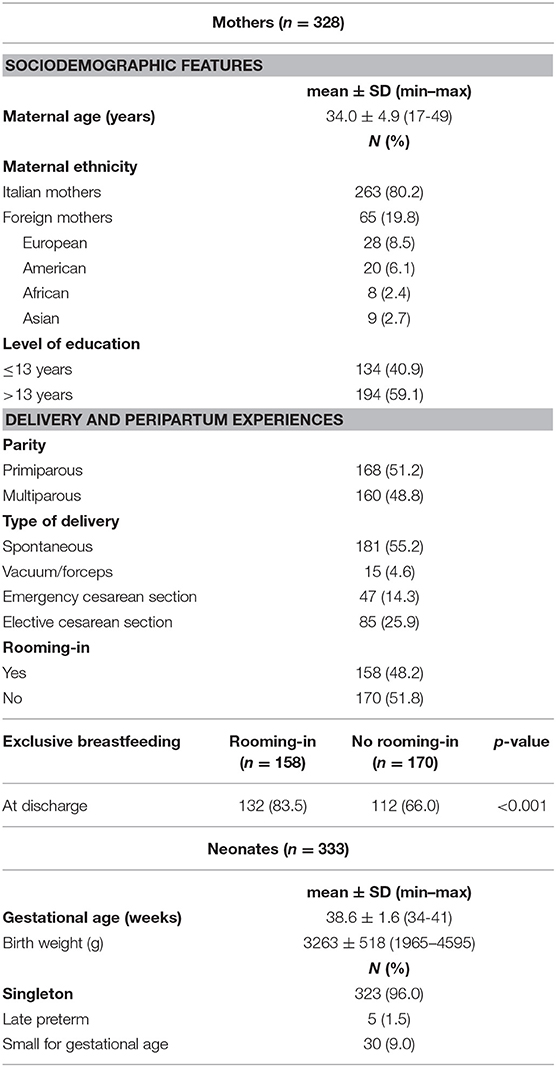
The enrolled population included 328 mothers and 333 neonates with 10 pairs of twins. Of the eligible population (466 mothers), 38 mothers declined participation to the study and 100 mothers were excluded according to the exclusion criteria. The basic characteristics of the mother-infant dyads are summarized in Table 2. The majority of the study population was Italian and had a high educational level. Over half of the mothers were primiparous and had a spontaneous delivery. With regards to the infants' population, a very limited number of newborns were late preterms.
During hospitalization, nearly half of the mothers practiced continuous rooming-in as defined by UNICEF/WHO. Rooming-in rates were significantly higher in non-Italian mothers compared to Italian ones and in multiparous mothers compared to primiparous ones (62.5% vs. 44.0%, p = 0.012, and 53.5% vs. 41.6%, p = 0.032, respectively), whereas no difference in rooming-in rates was found according to age (48.6% vs. 46.5%, p = 0.73) and years of education (42.2 % vs. 45.5%, p = 0.61). As for mode of delivery, rooming-in rates were significantly higher in mothers who delivered vaginally than in mothers who underwent a cesarean section (56.3% vs. 34.4%, p < 0.001).
At discharge, the exclusive breastfeeding rate was higher in the dyads who practiced rooming-in (83.5% vs. 66%, p < 0.001).
The answers to the items assessed in the interview are shown in Table 3. Most mothers attended prenatal classes and were aware of rooming-in practice and its benefits. Among the reported positive effects of rooming-in, promotion of mother-infant bonding, increased confidence in taking care of the baby and ability to recognize baby's feeding cues were the most frequently cited. Improving breastfeeding was reported as a positive effect of rooming-in by a limited number of mothers, but when asked as a specific question the majority of them stated that they thought rooming-in could impact their infant's feeding practices.
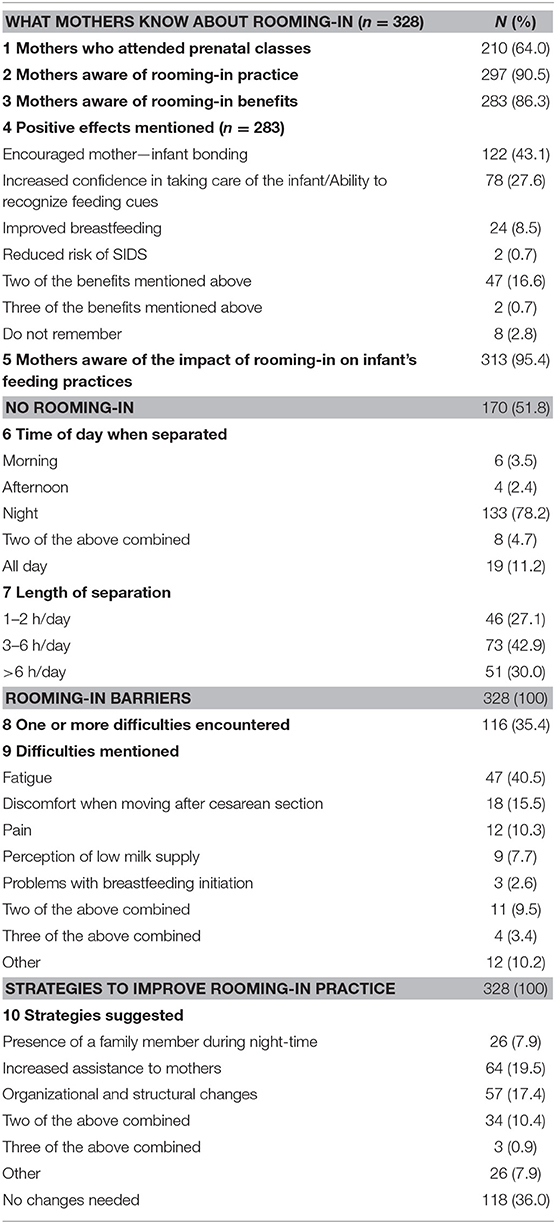
Table 3. Answers to the interview investigating maternal knowledge of rooming-in, barriers, and strategies.
Nearly half of the mothers who did not practice continuous rooming-in declared that the duration of the separation was 3–6 h, while one third of them kept the baby at the nursery for more than 6 h. The majority of mothers who did not continuously room-in with their babies indicated that separation from their babies occurred during night. The occurrence of rooming-in barriers was reported by 35.4% of mothers, with fatigue after delivery being the most important difficulty encountered, followed by discomfort when moving after cesarean section and pain after delivery, respectively.
Among the strategies proposed by mothers to improve rooming-in practice, increasing support to mothers, the need for organizational and structural changes, such as the possibility to have the bathroom and the changing table inside their room, more comfortable beds, a closer nursery, the reduction of visiting hours and the presence of a family member during night were the most frequently suggested. The 10.4% of mothers indicated two or more of these strategies combined whereas 36% of mothers did not consider any changes to be necessary.
Discussion
The present findings indicate that, although the mothers enrolled in the present study were familiar with the concept of rooming-in, they lacked a thorough understanding of its importance and associated benefits, and showed a suboptimal adherence to it in almost half of the cases. We also found that fatigue and cesarean section related difficulties were the most frequently reported barriers to rooming-in, with night being the most critical time of the day for this practice. The main strategy suggested for improving rooming-in was increasing assistance to mothers.
It is recommended that mothers' education on the basics of newborn care begins during pregnancy and continue in the immediate post-partum period (25). In our population, more than half of the mothers attended prenatal classes and almost all of them knew the UNICEF/WHO definition of rooming-in. Nevertheless, consistently with previous data published in the literature (26), less than half of them continuously practiced it. Previous studies have noted a similar discrepancy between knowledge and practice, which results in a suboptimal application of the information provided (27, 28). The time gap between the lessons attended and the birth of the baby has been suggested as one possible cause of this phenomenon (27). The results of the present study underline the lack of mothers' deep understanding of rooming-in, especially with regards to its associated benefits, which could have further negatively contributed to the suboptimal adherence to rooming-in. On the basis of the present findings, it is therefore desirable that healthcare professionals promote rooming-in to mothers highlighting its evidence-based benefits, focusing on the major role played by rooming-in in promoting breastfeeding initiation and continuation (21, 29). Consistently, a positive relationship between rooming-in and exclusive breastfeeding rates initiation was found also in our population.
When promoting rooming-in to mothers, it is important to take many aspects into consideration, both at a sociocultural and individual level. Previous studies have addressed the issue of how cultural background can influence the perception of rooming-in and the choice and modality of practicing it (30, 31), as well as impact the implementation of the BFHI itself (31). Accordingly, in our study, non-Italian mothers practiced rooming-in more than their Italian counterparts, confirming the importance of the cultural background within this context. Moreover, in the Italian subgroup we found no association between the choice to room-in and maternal age or level of education, suggesting a cross-sectional tendency not to room-in among these women.
With regards to individual factors, it is important to identify the most vulnerable women, who may need additional guidance and support in the peri-partum period. Operators should be able to acknowledge obstacles, both physical and psychological, limiting adherence to rooming-in and act in order to limit their impact. Possible physical difficulties are usually related to delivery mode and resulting maternal conditions (32, 33). Fatigue, pain due to surgery and movement difficulties, especially frequent after a cesarean section, can limit a mother's ability to take care of her newborn, thus being perceived as barriers in the practice of rooming-in. Moreover, attention should be focused also on first time mothers since primiparae have higher post-partum levels of anxiety than multiparae (34), with inexperience possibly exacerbating what already is an emotionally challenging situation for most women (35). Accordingly, in our population, first time mothers practiced rooming-in less than multiparous women. These results further underline the importance of providing additional guidance to primiparae in their transition to motherhood.
In line with the findings of the present study, mothers usually preferred to leave their infants at the nursery during the night. These results could be at least partially explained by an anticipated fear of disturbed sleep as highlighted in previous studies (36, 37). Nevertheless, it has been demonstrated that mothers who leave their babies at the nursery during the night do not have a longer or better sleep (38), while babies who room-in have a less indeterminate, more quiet sleep than those left at the nursery (39). It is therefore advisable for healthcare professionals to underline this aspect when addressing the issue of rooming-in with mothers. Increased staff attention toward the limitation of unnecessary maternal sleep interruptions due to night-time assessments and medical care has also been suggested (18).
Ultimately, mothers need more assistance, as the majority of our study population suggested. This can come either from the healthcare personnel or from the family. Staff shortage is one of the recognized barriers to the implementation of the BFHI (11, 40). A skewed healthcare professional:dyad ratio inevitably limits the time to dedicate to mothers and the problems they report. On the other hand, visits in the post-natal unit can be a double edged weapon: while partners are much needed to support and help mothers, having too many people around may affect the establishment of a new family routine.
The strength of the present study was that it addressed a relatively large number of mothers, who received the same modality of support. However, our data were collected from a single Italian tertiary center, thus these results may not be generalizable to all post-partum mothers. Moreover, we acknowledge that oral interviews could imply potential bias in comparison to written anonymous self-administered questionnaires.
Conclusions
Our study contributes to a deeper knowledge of maternal rooming-in experience in an Italian tertiary maternity.
We underline the importance of providing a tailored support to the mother-infant dyad in order to overcome rooming-in barriers perceived by mothers and promote a positive rooming-in experience.
Data Availability Statement
Access to the dataset generated and analyzed for this study is restricted to protect patient confidentiality and participant privacy. The data are available upon request to the corresponding author, with permission of the third party.
Ethics Statement
The study was reviewed and approved by the Ethics Committee of the Fondazione IRCCS Ca' Granda Ospedale Maggiore Policlinico, Milan, Italy. Written informed consent to participate in this study was provided by all participants.
Author Contributions
AC contributed to the design of the study and drafted the initial manuscript. BC and JC contributed to the interpretation of results and drafted the initial manuscript. DM contributed to the interpretation of results and reviewed and revised the manuscript. MD collected the data and contributed to the interpretation of results. MB contributed to the interpretation of results, reviewed, and revised the manuscript. DC carried out the statistical analysis and contributed to the interpretation of results. LC and LZ contributed to design the study, supervised the data collection, and reviewed the manuscript. EB, PS, FM, and LP contributed to design the study and reviewed and revised the manuscript. MG contributed to design the study, supervised data collection, contributed to the interpretation of results, reviewed and revised the manuscript. All authors approved the final manuscript as submitted.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors would like to thank all the nurses and neonatologists of the post-natal unit of the Fondazione IRCCS Ca' Granda Ospedale Maggiore Policlinico, alongside all the mothers who participated in the study.
References
1. Baby-Friendly Hospital Initiative: Revised, Updated and Expanded for Integrated Care. Geneva: World Health Organization (2009). Available online at: http://www.ncbi.nlm.nih.gov/books/NBK153471/
2. Saadeh RJ. The Baby-Friendly Hospital Initiative 20 years on: facts, progress, and the way forward. J Hum Lact. (2012) 28:272–5. doi: 10.1177/0890334412446690
3. Broadfoot M, Britten J, Tappin DM, MacKenzie JM. The Baby Friendly Hospital Initiative and breast feeding rates in Scotland. Arch Dis Child Fetal Neonatal Ed. (2005) 90:F114–16. doi: 10.1136/adc.2003.041558
4. Gianni ML, Bezze EN, Sannino P, Baro M, Roggero P, Muscolo S, et al. Maternal views on facilitators of and barriers to breastfeeding preterm infants. BMC Pediatr. (2018) 18:283. doi: 10.1186/s12887-018-1260-2
5. DiGirolamo AM, Grummer-Strawn LM, Fein S. Maternity care practices: implications for breastfeeding. Birth. (2001) 28:94–100. doi: 10.1046/j.1523-536X.2001.00094.x
6. Patterson JA, Keuler NS, Olson BH. The effect of maternity practices on exclusive breastfeeding rates in U.S. hospitals. Matern Child Nutr. (2019) 15:e12670. doi: 10.1111/mcn.12670
7. World Health Organization, UNICEF. WHO | Protecting, Promoting and Supporting Breast-Feeding. The Special Role of Maternity Services. (1989). Available online at: https://www.who.int/nutrition/publications/infantfeeding/9241561300/en/ (accessed May 26, 2019).
8. United Nations Children's Fund & World Health Organization. Protecting, Promoting and Supporting Breastfeeding in Facilities Providing Maternity and Newborn Services: The Revised Baby-Friendly Hospital Initiative. Geneva: UNICEF and WHO (2018).
9. Saadeh R, Akré J. Ten steps to successful breastfeeding: a summary of the rationale and scientific evidence. Birth. (1996) 23:154–60.
10. Chien L-Y, Tai C-J, Chu K-H, Ko Y-L, Chiu Y-C. The number of Baby Friendly hospital practices experienced by mothers is positively associated with breastfeeding: a questionnaire survey. Int J Nurs Stud. (2007) 44:1138–46. doi: 10.1016/j.ijnurstu.2006.05.015
11. Semenic S, Childerhose JE, Lauzière J, Groleau D. Barriers, facilitators, and recommendations related to implementing the Baby-Friendly Initiative (BFI): an integrative review. J Hum Lact. (2012) 28:317–34. doi: 10.1177/0890334412445195
12. Bystrova K, Ivanova V, Edhborg M, Matthiesen A-S, Ransjö-Arvidson A-B, Mukhamedrakhimov R, et al. Early contact versus separation: effects on mother-infant interaction one year later. Birth. (2009) 36:97–109. doi: 10.1111/j.1523-536X.2009.00307.x
13. Dumas L, Lepage M, Bystrova K, Matthiesen A-S, Welles-Nyström B, Widström A-M. Influence of skin-to-skin contact and rooming-in on early mother-infant interaction: a randomized controlled trial. Clin Nurs Res. (2013) 22:310–36. doi: 10.1177/1054773812468316
14. Greenberg M, Rosenberg I, Lind J. First mothers rooming-in with their newborns: its impact upon the mother. Am J Orthopsychiatry. (1973) 43:783–88. doi: 10.1111/j.1939-0025.1973.tb00850.x
15. Jaafar SH, Lee KS, Ho JJ. Separate care for new mother and infant versus rooming-in for increasing the duration of breastfeeding. Cochrane Database Syst Rev. (2012) CD006641. doi: 10.1002/14651858.CD006641.pub2
16. Cohen SS, Alexander DD, Krebs NF, Young BE, Cabana MD, Erdmann P, et al. Factors associated with breastfeeding initiation and continuation: a meta-analysis. J Pediatr. (2018) 203:190–6.e21. doi: 10.1016/j.jpeds.2018.08.008
17. Merewood A. Rooming-in-are you really? J Hum Lact. (2014) 30:268–9. doi: 10.1177/0890334414538931
18. Theo LO, Drake E. Rooming-in: creating a better experience. J Perinat Educ. (2017) 26:79–84. doi: 10.1891/1058-1243.26.2.79
19. Jackson EB. General reactions of mothers and nurses to rooming-in. Am J Public Health Nations Health. (1948) 38:689–95. doi: 10.2105/AJPH.38.5_Pt_1.689
20. Mc Loughlin G. Rooming-in for new mother and infant versus separate care for increasing the duration of breastfeeding. Int J Nurs Pract. (2019) 25:e12731. doi: 10.1111/ijn.12731
21. Crenshaw JT. Healthy birth practice #6: keep mother and baby together- it's best for mother, baby, and breastfeeding. J Perinat Educ. (2014) 23:211–17. doi: 10.1891/1058-1243.23.4.211
22. UNICEF. Guida All'applicazione dei Passi. (2016). Available online at: https://www.unicef.it/Allegati/Guida_applicazione_dei_Passi_ed2016_19mag17.pdf (accessed October 20, 2019).
23. WHO Exclusive Breastfeeding for Optimal Growth, Development and Health of Infants. WHO. Available online at: http://www.who.int/elena/titles/exclusive_breastfeeding/en/ (accessed May 25, 2019).
24. WHO | Ten Steps to Successful Breastfeeding,. (2018). WHO. Available online at: http://www.who.int/nutrition/bfhi/ten-steps/en/ (accessed May 25, 2019).
25. Su L-L, Chong Y-S, Chan Y-H, Chan Y-S, Fok D, Tun K-T, et al. Antenatal education and postnatal support strategies for improving rates of exclusive breast feeding: randomised controlled trial. BMJ. (2007) 335:596. doi: 10.1136/bmj.39279.656343.55
26. Barrera CM, Nelson JM, Boundy EO, Perrine CG. Trends in rooming-in practices among hospitals in the United States, 2007-2015. Birth. (2018) 45:432–9. doi: 10.1111/birt.12359
27. Nasir NM, Amran Y, Nakamura Y. Changing knowledge and practices of mothers on newborn care through mother class: an intervention study in Indonesia. J Trop Pediatr. (2017) 63:440–6. doi: 10.1093/tropej/fmx010
28. Khadduri R, Marsh DR, Rasmussen B, Bari A, Nazir R, Darmstadt GL. Household knowledge and practices of newborn and maternal health in Haripur district, Pakistan. J Perinatol. (2008) 28:182–7. doi: 10.1038/sj.jp.7211903
29. Yamauchi Y, Yamanouchi I. The relationship between rooming-in/not rooming-in and breast-feeding variables. Acta Paediatr Scand. (1990) 79:1017–22. doi: 10.1111/j.1651-2227.1990.tb11377.x
30. Rice PL. Rooming-in and cultural practices: choice or constraint? J Reprod Infant Psychol. (2000) 18:21–32. doi: 10.1080/02646830050001654
31. Edwards G, Abdulali J, Kumar RR. Meeting the challenge: implementing the Baby Friendly Hospital Initiative in a culturally diverse country. Pract Midwife. (2011) 14:12, 14–16.
32. Casonato M, Cefalà F, Albasi C. Women and post-natal care: analysis of a rooming-in facility. Recenti Prog Med. (2017) 108:425–432. doi: 10.1701/2802.28355
33. Lai Y-L, Hung C-H, Stocker J, Chan T-F, Liu Y. Postpartum fatigue, baby-care activities, and maternal-infant attachment of vaginal and cesarean births following rooming-in. Appl Nurs Res. (2015) 28:116–20. doi: 10.1016/j.apnr.2014.08.002
34. Maes M, Bosmans E, Ombelet W. In the puerperium, primiparae exhibit higher levels of anxiety and serum peptidase activity and greater immune responses than multiparae. J Clin Psychiatry. (2004) 65:71–6. doi: 10.4088/JCP.v65n0112
35. Zanardo V, Gasparetto S, Giustardi A, Suppiej A, Trevisanuto D, Pascoli I, et al. Impact of anxiety in the puerperium on breast-feeding outcomes: role of parity. J Pediatr Gastroenterol Nutr. (2009) 49:631. doi: 10.1097/MPG.0b013e31819e6446
36. Waldenström U, Swenson A. Rooming-in at night in the postpartum ward. Midwifery. (1991) 7:82–9. doi: 10.1016/S0266-6138(05)80232-3
37. Svensson K, Matthiesen A-S, Widström A-M. Night rooming-in: who decides? An example of staff influence on mother's attitude. Birth. (2005) 32:99–106. doi: 10.1111/j.0730-7659.2005.00352.x
38. Keefe MR. The impact of infant rooming-in on maternal sleep at night. J Obstet Gynecol Neonatal Nurs. (1988) 17:122–6. doi: 10.1111/j.1552-6909.1988.tb00522.x
39. Keefe MR. Comparison of neonatal night time sleep-wake patterns in nursery versus rooming-in environments. Nurs Res. (1987) 36:140–4. doi: 10.1097/00006199-198705000-00002
Keywords: rooming-in, maternal knowledge, barriers, facilitators, breastfeeding
Citation: Consales A, Crippa BL, Cerasani J, Morniroli D, Damonte M, Bettinelli ME, Consonni D, Colombo L, Zanotta L, Bezze E, Sannino P, Mosca F, Plevani L and Giannì ML (2020) Overcoming Rooming-In Barriers: A Survey on Mothers' Perspectives. Front. Pediatr. 8:53. doi: 10.3389/fped.2020.00053
Received: 17 November 2019; Accepted: 05 February 2020;
Published: 21 February 2020.
Edited by:
Hans Fuchs, Freiburg University Medical Center, University of Freiburg, GermanyReviewed by:
Georg Schmolzer, University of Alberta, CanadaElizabeth Foglia, Children's Hospital of Philadelphia, United States
Copyright © 2020 Consales, Crippa, Cerasani, Morniroli, Damonte, Bettinelli, Consonni, Colombo, Zanotta, Bezze, Sannino, Mosca, Plevani and Giannì. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Alessandra Consales, YWxlc3NhbmRyYS5jb25zYWxlc0BnbWFpbC5jb20=
 Alessandra Consales
Alessandra Consales Beatrice Letizia Crippa1,2
Beatrice Letizia Crippa1,2 Jacopo Cerasani
Jacopo Cerasani Daniela Morniroli
Daniela Morniroli Martina Damonte
Martina Damonte Maria Enrica Bettinelli
Maria Enrica Bettinelli Patrizio Sannino
Patrizio Sannino Maria Lorella Giannì
Maria Lorella Giannì