
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pediatr. , 03 December 2019
Sec. Pediatric Pulmonology
Volume 7 - 2019 | https://doi.org/10.3389/fped.2019.00498
We evaluated the effects of air pollutants, age, allergic history, family allergic history, treatment, treatment steps, and compliance on uncontrolled childhood asthma in Xiamen, China. The clinical data of children with asthma in the pediatric outpatient department of the First Affiliated Hospital of Xiamen University from January 2016 to June 2018 were analyzed retrospectively. According to the assessment of the patients' outcome including well-controlled, partly-controlled and uncontrolled, 7,211 cases of 3,268 patients were selected. Rank sum test and ordered multi-class logistic regression analysis were used. In the rank sum test, age, allergic history, family allergic history, season, treatment, treatment steps and compliance were found associated with uncontrolled rate (all P < 0.001). Logistic regression analysis showed that PM10, NO2, and SO2 raised uncontrolled-asthma rate (aOR 1.311, aOR 1.281, aOR 1.252, respectively). Older children had lower uncontrolled rate (OR = 0.849, 95% CI: 0.758–0.950), children with higher treatment steps had higher uncontrolled rate (OR = 1.227, 95%CI: 1.040–1.448), and children with better treatment compliance have lower uncontrolled rate (OR = 0.374 95% CI: 0.331–0.424). The order of the uncontrolled rate of asthma from high to low was winter, spring, autumn, and summer. PM10, NO2, SO2, age, season, treatment steps, and treatment compliance have significance for predicting the control rate of childhood asthma in Xiamen, China.
Asthma is a common chronic respiratory disease, especially in children. Epidemiological study found that the prevalence of asthma is increasing year by year (1, 2). The control of asthma is closely related to the quality of life of patients.
Children's asthma is related to various factors such as environmental factors, genetic factors, and immunological factors. Environmental pollution plays a part in asthma exacerbation, and there are a few investigations regarding to the relationship between air pollutants and childhood asthma in China. PM1, PM2.5, and PM10 exposure had a negative effect on adolescent respiratory system and was associated with asthma exacerbation (3, 4). NO2, SO2, and CO were risk factors of severe childhood asthma (5–7). However, the research on the air pollution and childhood asthma control is rare in China.
The control of asthma is far from encouraging. In one worldwide survey, the prevalence of severe asthma symptoms (four or more attacks of wheeze, waking at night with asthma symptoms one or more times per week, and/or any episodes of wheeze severe enough to limit the ability to speak) was more than 7.5% in numerous centers in the UK, New Zealand, Brazil and other countries in the preceding 12 months (8). Asthma prevalence varies from 1 to 18% in different part of the world, with the highest prevalence (6.0–12.0%) in developed western countries (9). A global investigation presented that the hospitalized asthma patients are decreasing (8), which indicated that outpatient management of asthma is important. We found some recent studies from China on associations between personal statements and children asthma exacerbation but a few studies on childhood asthma control. Xiang's study found that the risk of uncontrolled asthma was higher in subjects with treatment non-adherence, concomitant allergic rhinitis (AR), disease duration ≥ 1.5 years, and first-degree relatives with AR (10). One study from Beijing found that children with asthma showed significant improvements in control rates and lung function during control-based asthma management (11). Thus, there is a need for more studies on asthma control among children in China in relation to personal statements.
In order to better guide the patients and their family in developing countries to cooperate with doctors, the risk factors of the decreasing asthma control rate in Xiamen were studied. We obtained real-world data of childhood asthma cases from the electronic medical record system of the First Affiliated Hospital of Xiamen University to provide theoretical support for asthma management.
The data of pediatric respiratory diseases from January 1, 2016 to June 30, 2018 were obtained from the pediatric outpatient electronic medical record system of the First Affiliated Hospital of Xiamen University. The data were from urgent care, department of asthma and outpatient. The patients were followed up regularly (every one, 2 or 3 months). At the follow-up, the doctors who work in the First Affiliated Hospital of Xiamen University recorded the patient's condition and judged the control status according to examination, diurnal and nocturnal symptoms. The data included the visit date, the patient ID, the patient's name, age, gender, chief complaint, current medical history, diagnosis, family history, past medical history, etc. All patients were aged between 0 and 14 years old.
According to the “Guidelines for the Diagnosis and Prevention of Childhood Bronchial Asthma” developed by the Department of Respiratory Medicine of the Chinese Medical Association in 2016 (12), 17,835 childhood asthma cases (J45 in ICD10) were selected from the diagnosis results of the medical records (Supplementary Table 1). According to the symptoms and examinations 4 weeks before the patients' visit, the patient's outcome was evaluated as “well-controlled,” “partly-controlled,” and “uncontrolled” (Supplementary Table 2). The treatment was decided based on patients' outcomes (Supplementary Figures 1, 2). After removal 175 patients from other cities, a total of 7,211 cases of 3,268 patients were enrolled. And 35 patients were asked to be admitted after the outpatient visits.
The data of air pollution including PM2.5, PM10, CO, SO2, NO2 were collected at four different sites in the city, with the help of Xiamen Department of Environmental Protection. The concentration of pollutants was measured and we took the average of every site. Meteorological data, such as temperature, wind speed, precipitation and so on, were got from Xiamen Meteorological Bureau. March, April, and May are defined as spring, June, July, and August are summer, September, October, and November are autumn, and December to February are winter.
We used Wilcoxon and Kruskal-Wallis rank sum test to investigate the relationship between control levels and the personal statements containing gender, season, age, family allergic history, allergic history, treatment, and compliance. The variables which showed significant differences were included in multiple logistic regression analysis. The average concentration of air pollutants, including PM2.5, PM10, CO, NO2, and SO2, in the 4 weeks before the patient's visit was included in the ordered multi-class logistic regression analysis. We marked the “well-controlled asthma” as 1, the “partly controlled asthma” as 2 and “uncontrolled asthma” as 3. In order to eliminate the difference of air pollutants, we divided the pollutant concentration by the interquartile range (IQR) to get the adjusted OR (aOR). Statistical significance was set at p < 0.05. Data filter and statistical analysis were conducted in R 3.5 software with the “MASS” package.
We calculated the average of the pollutant concentration and meteorological data in 4 weeks before the visits. The average concentration of PM2.5 was 27.25 μg/m3, the minimum was 10.29 μg/m3, and the maximum was 43.50 μg/m3. The PM10 concentration range was 22.39–72.61 μg/m3 and the annual mean was 47.50 μg/m3. The average concentration of CO was 584.70 μg/m3 and the concentration ranged from 332.10 μg/m3 to 839.30 μg/m3. The average of NO2 was 31.48 μg/m3, and the median was 31.29 μg/m3. The mean of SO2 was 10.84 μg/m3 and the median was 10.64 μg/m3 (Table 1). The study period contains 912 days. According to “Technical Regulation on Ambient Air Quality Index” (13), the standard of PM2.5 is 35 μg/m3 and there were 198 days whose average concentration in the previous 4 weeks exceed the standard; the standard of PM10 is 50 μg/m3 and in 43.09% days the concentration of PM10 exceeds the standard; the standard of CO is 4,000 μg/m3, the concentration of NO2 is 80 μg/m3 and the concentration of SO2 is 50 μg/m3, and all the average concentration was below the standard of “Rank 1” (Figure 1).
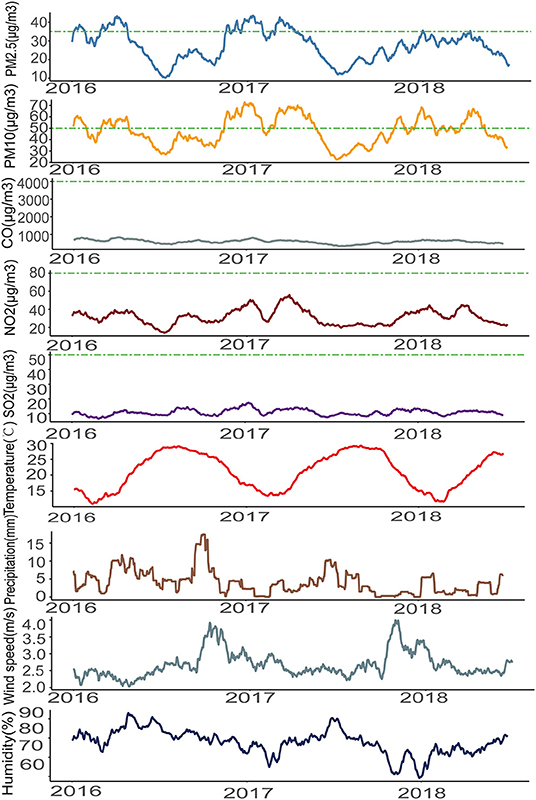
Figure 1. The air pollutants and the meteorological data (mean values of the previous 4 weeks of the visits) during the study period.
There were 1,453 patients who were in step 1, 1,119 in step 2, 2,105 in step 3, 1,330 in step 4, and 35 in step 5 (Figure 2A). In 5,950 visits with complete prescription data, 412 people used leukotriene receptor antagonist (LTRA) alone and 1,453 patients had no medication prescribed. The medication prescribed was shown in Figure 2B. Among the enrolled visits, 4,815 (66.77%) visits were male patients and 2,396 (33.23%) were female patients. The prevalence of asthma in males was higher. The well-controlled rate was 41.20% for males and 41.19% for females. The uncontrolled rate of male patients was 12.88% while the uncontrolled rate of female patients was 12.10%. The gender difference in control was not significant (P = 0.763). According to the age, the patients were divided into three groups: infant (0–3 years old), preschool children (4–6 years old), and school-aged children (7–14 years old). There were 3,412 children in preschool group, accounting for the largest proportion (47.3%), which suggests that preschool children are most susceptible to asthma. Table 2 showed that there were differences in the control rate of the three age groups (P < 0.001).
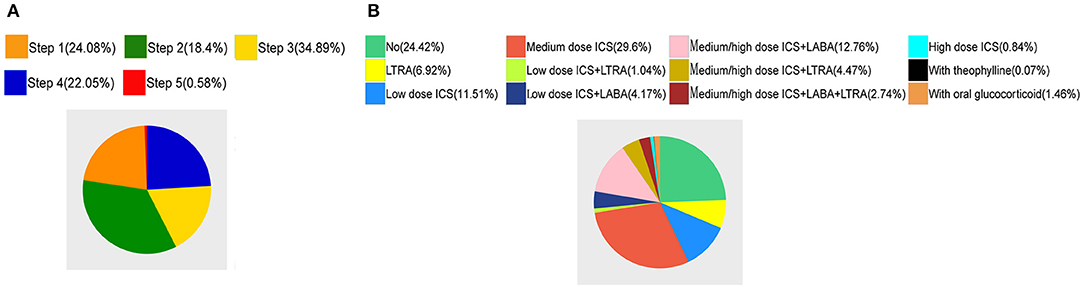
Figure 2. (A) The Pie chart of the treatment steps of the patient. (B) The Pie chart of the medication prescribed.
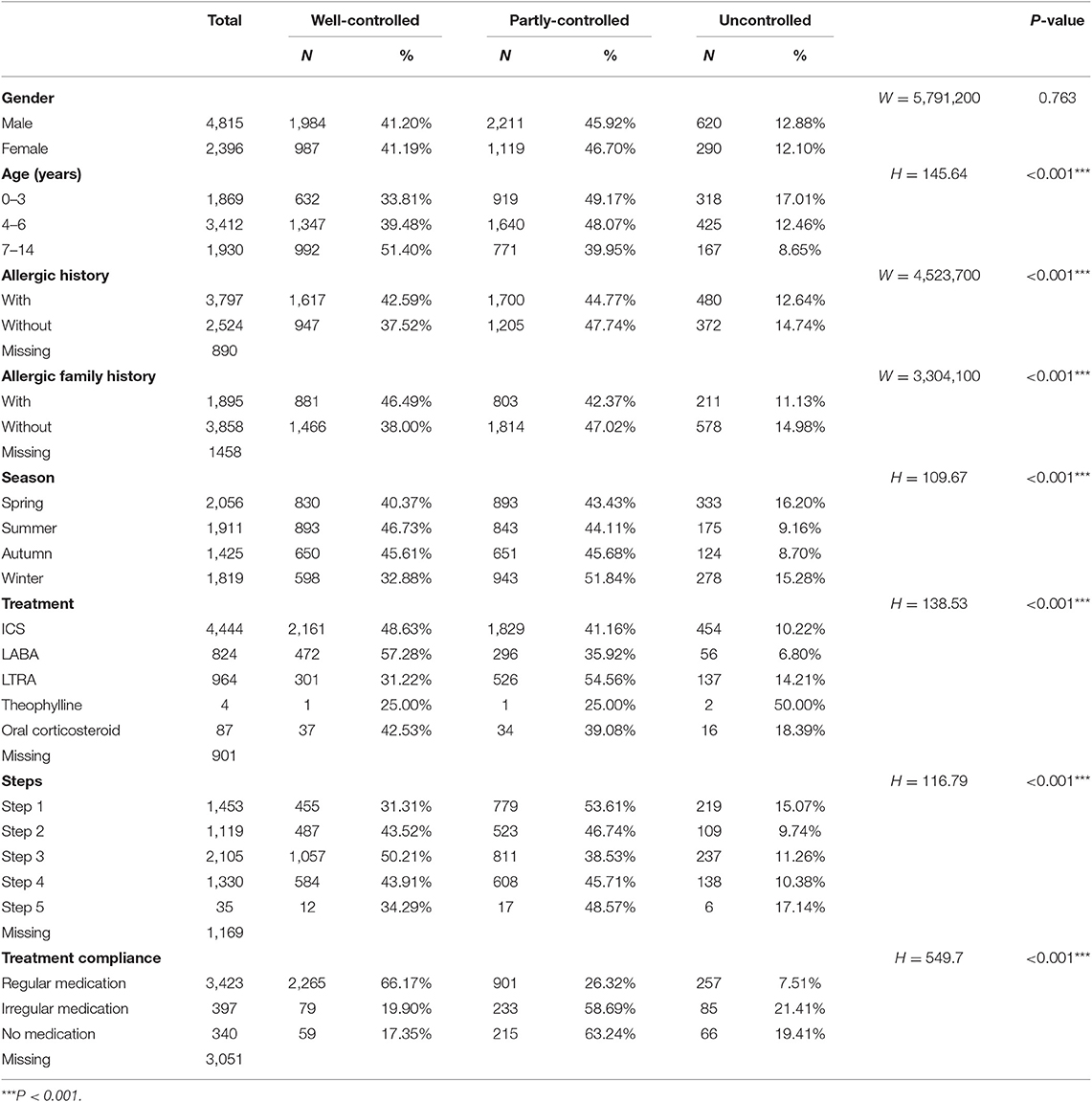
Table 2. Summary of gender, age, allergic history, allergic family history, visit seasons, treatment and compliance, and the assessment of relationship with asthma control from rank sum test.
Among the 6,321 patients with a history record, 3,797 had a history of allergic disease accounting for 60.07%, and 2,524 had no history of allergic disease (Table 2). There was a difference in the control rate between the two groups with or without allergic disease (P < 0.001). Among the 5,753 patients with a family history record, there were 1,895 (32.94%) patients whose three-generation relatives had allergic diseases, and 3,858 (67.06%) patients did not have family allergic history. There was a significant difference between the two groups with or without family allergic history (P < 0.001).
In 7,211 visits, 2,056 visits were in spring, 1,911 in summer, 1,425 in autumn and 1,819 in winter. There were 893 well-controlled visits in summer, accounting for 46.73% of the visits in summer but there were only 32.88% well-controlled visits in winter. The Kruskal-Wallis rank sum test showed that there were differences in the control of the four groups (Table 2).
We analyzed every drug separately including ICS, long-acting beta2-agonist (LABA), LTRA, theophylline and oral corticosteroid. Among the 6,320 patients with prescription data, 4,444 patients used ICS, and the well-controlled rate was 48.63%. Nine hundred and sixty-four patients had LTRA and the well-controlled rate was 31.22%. The Kruskal-Wallis rank sum test showed that the control of using various drugs were different. The difference of control rates among five steps was statistically significant (P < 0.001). Therefore, we included treatment steps in the logistic regression. Among the 4,160 cases recorded with treatment compliance (regular medication, irregular medication, no medication), 3,423 (82.28%) patients had regular medication and the well-controlled rate was 66.17%. There were 340 (8.17%) patients who did not use the drug prescribed, among whom the well-controlled rate was 17.35%. The difference of distribution of control levels among the three groups was significant (P < 0.001).
The effects of PM2.5, PM10, CO, NO2, and SO2 on asthma control were adjusted by the average temperature, precipitation, wind speed and humidity, respectively. Table 3 indicated that the adjusted OR. The aOR of PM10 was 1.311 (95% CI 1.185–1.449). The aOR of NO2 was 1.281 (P < 0.001). The SO2 augmented the uncontrolled rate (aOR 1.252, 95% CI 1.166–1.344). But PM2.5 concentration was not relative to the asthma control rate (P = 0.273), and the influence of CO on asthma control had no statistical significance either.
Of 7,211 cases, 3,026 cases which had records of age, allergic history, family allergic history, visit date, treatment, steps, and compliance were analyzed by ordered multi-class logistic regression. The results were shown in Table 4. Age was associated with control and older children had lower asthma uncontrolled rate (OR 0.849, 95% CI 0.758–0.950, P = 0.004). The seasons affected childhood asthma control rate (OR 0.818 95% CI 0.768–0.872 P < 0.001). In summer, the control was best. The associations between treatment steps and asthma control remained statistically significant (OR 1.227, 95% CI 1.040–1.448, P = 0.015).Treatment adherence (OR 0.374, 95% CI 0.331–0.424, P < 0.001) was a risk factor in uncontrolled childhood asthma. The drugs the patients used had no effect on the control.
The diagnosis and control assessment of childhood asthma in this study were from Chinese guidelines which was made based on GINA (14). The Chinese doctors, especially in less-developed areas, use stethoscopes frequently, so the description of auscultation is more detailed in Chinese guidelines.
This study showed that, in the 7,211 visits in pediatric outpatients from 2016 to 2018, 2,971 cases were well-controlled, accounting for 41.20, 46.18% were partly-controlled and 12.62% were uncontrolled asthma. Thus, children with asthma in Xiamen are mostly partly-controlled. The asthma control rate in Europe is 55% (15). The US survey found that 55.8% of patients with had at least one asthma attack in the past year (16). In China, 60.0–64.9% of adults with asthma were uncontrolled (17, 18). The rate of uncontrolled childhood asthma in China needs a population-based study. It is suggested that the asthma control situation in Xiamen is consistent with that in other parts of China, but the asthma controlled rate in China is lower than that in developed countries.
We eliminated the effect of other weather conditions such as temperature, wind speed, etc. and concluded that PM10, NO2, and SO2 have a negative effect on childhood asthma control. The association between air pollution and asthma has been studied in different parts of the world. A study from South Africa showed that exposure to PM10, SO2, NO2, and NO is associated with significantly increased occurrence of respiratory symptoms among children (19). A study, in Bradford England, used a newly developed full-chain model to show that 38% of childhood asthma were caused by air pollution, and 6% of which attributed to NO2 and NOx (20). This article provides a detailed explanation of the relationship between asthma control and air pollution within 4 weeks prior to the visits. We collected the air pollution data from four sites in Xiamen but the data did not reflect the exact living environment of the patients.
This study found that there was no effect of PM2.5 on the childhood asthma control. This contrasts with the results from several previous studies that have demonstrated the adverse effect of PM2.5 on asthma in children. A review summarized that children exposure to both PM2.5 and PM10 was associated with the aggravation of asthma symptoms (21). Each increase of 10 μg/m3 in concentrations of PM2.5 was associated with 1–2% increase in risk of wheeze-associated disorders (22). In particular, an earlier study conducted among school children in California found each 8.1 μg/m3 decrease in particulate matter <2.5 μm was associated with a reduction of 1.53 cases per 100 person-years in asthma incidence in their study while examine whether decreasing regional air pollutants were associated with reduced incidence of childhood asthma (23). However, several previous studies also failed to find an association between ambient PM2.5 and asthma in children. Mazenq who performed a study of the effects of air pollution on children in southeastern France, suggested that PM10 increased the risk of emergency asthma-related hospital visits, but PM2.5 were not found to be a risk factor (24). Other epidemiological survey also reported that PM10 is associated with asthma, but not PM2.5 (25). This might be due to the different composition of PM2.5 in different regions.
The Rank Sum Test of age, gender, allergic history, family allergic history, season, treatment, steps, and compliance showed that age, allergic history, family allergic history, season, treatment, steps, and compliance were related to asthma control. And these related factors were included into the logistic regression model. Multi-factor logical regression analysis showed that age, season and treatment steps and compliance were the risk factors of asthma control. The control rate increased with age and the highest control rate presented in children aged 7–14. With the increase of age, children's medication compliance is good, especially using aerosol therapy. They can make full use of the inhaled drugs. And children's immune system is constantly improving (26), which maintains immune balance and alleviates the Th1/Th2 cell imbalance, so that asthma symptoms are relieved (27, 28). Some studies reported that asthma control is related to the season, temperature, humidity and pollen (29–33). The control rate was different in different seasons, but the data of pollen lacked in this study. The impact of pollen and childhood asthma control requires further research. It is a common view that passive smoking is detrimental to respiratory system (34, 35), but there was no data of passive smoking in the study. In our study, treatment compliance had the greatest impact on asthma control. The Global Initiative for Asthma (GINA) guidelines (36) pointed out that management of ICS treatment is an influential factor in asthma control, suggesting that children should pay attention to the medication. In a systematic review, daily ICS appears more effective than daily LTRA for improving symptom control and decreasing exacerbation, when a minimum of 3-month therapy with daily ICS or LTRA was performed (37). However, in this study, the effect of varies of drugs on asthma control was not significant because only 4-weeks medication was observed. It is worth noting that compliance with medical advice and regular use of drugs can alleviate asthma symptoms and greatly improve the quality of life.
Bao et al., Bednarek et al., and Ahmadizar et al. found that allergic history and family history of allergies can predict asthma control rate (38–40). In this article, we studied whether allergic history and family allergic history were related to childhood asthma control, but the two characteristics were not risk factors. This happened because of the good economic conditions of patients who have the standardized management of asthma in Xiamen. Although these children have genetic susceptibility, their family pay more attention to collecting information and understand ways to prevent and treat asthma symptoms. We analyzed the relationship between allergic history, family allergic history and medication compliance, and found that these patients had more regular medication. Moreover, we found in the study that patients with a family allergic history have a higher rate of testing allergens. These patients and their family avoid contacting with allergens and pay more attention to home cleanness.
Ordered multi-class logistic regression was used to analyze risk factors of asthma control. Seven variables, including PM10, NO2, SO2, age, season, treatment steps, and compliance, were selected. These factors play an important role in the control and management of childhood asthma in Xiamen.
The data analyzed for this study can be found from the corresponding authors on reasonable request.
This study was approved by the ethical guidance (KY2015–027) of the Ethical Review Board of the First Affiliated Hospital of Xiamen University. As private information including patient ID, residence and contact information is crypted and hashed, the review board agreed to waive the statement of consent.
YZ, JW, and DG acquired the data. YZ analyzed the data and drafted the manuscript. JW and QL revised the manuscript. All authors contributed to conception and design of the research, interpretation of the results, and edited the manuscript.
This research was funded by Natural Science Foundation of Fujian Province (No. 2016 J01644).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
We are grateful to Zhifan Hu, Wanting Huang, Qihong Chen, Yuanmei Lan, Wenliu Qiu, Pengyi Zhang, Ruiqi Chen, Huimin Wang, Zhijia Liao for their contribution to the data collection.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2019.00498/full#supplementary-material
2. The National Cooperative Group on Childhood Asthma. The third nationwide survey of childhood asthma in urban areas of China. China J Pediatr. (2013) 51:729–36.
3. Yang M, Chu C, Bloom MS, Li S, Chen G, Heinrich J, et al. Is smaller worse? New insights about associations of PM1 and respiratory health in children and adolescents. Environ Int. (2018) 120:516–24. doi: 10.1016/j.envint.2018.08.027
4. Liu F, Zhao Y, Liu Y-Q, Liu Y, Sun P, Huang M-M, et al. Asthma and asthma related symptoms in 23,326 Chinese children in relation to indoor and outdoor environmental factors: the Seven Northeastern Cities (SNEC) Study. Sci Total Environ. (2014) 497:10–7. doi: 10.1016/j.scitotenv.2014.07.096
5. Norback D, Lu C, Zhang Y, Li B, Zhao Z, Huang C, et al. Sources of indoor particulate matter (PM) and outdoor air pollution in China in relation to asthma, wheeze, rhinitis and eczema among pre-school children: Synergistic effects between antibiotics use and PM10 and second hand smoke. Environ Int. (2019) 125:252–60. doi: 10.1016/j.envint.2019.01.036
6. Chen J, Jiang X, Shi C, Liu R, Lu R, Zhang L. Association between gaseous pollutants and emergency ambulance dispatches for asthma in Chengdu, China: a time-stratified case-crossover study. Environ Health Prev Med. (2019) 24:20. doi: 10.1186/s12199-019-0773-0
7. Zhang H, Chang Q, Gao S, Wu Q, Zhao Y. The impact of prenatal exposure to air pollution on childhood wheezing and asthma: a systematic review. Environ Res. (2017) 159:519–30. doi: 10.1016/j.envres.2017.08.038
9. Lundback B, Backman H, Lotvall J, Ronmark E. Is asthma prevalence still increasing? Exp Rev Respir Med. (2016) 10:39–51. doi: 10.1586/17476348.2016.1114417
10. Xiang L, Zhao J, Zheng Y, Liu H, Hong J, Bao Y, et al. Uncontrolled asthma and its risk factors in Chinese children: A cross-sectional observational study. J Asthma. (2016) 53:699–706. doi: 10.3109/02770903.2016.1144199
11. Gao Q, Huang H, Zhu K, Liu X, Hou X, Guan H, et al. Clinical course and factors associated with asthma control in children under control-based asthma management: a prospective study. Iran J Allergy Asthma Immunol. (2018) 17:18–28.
12. The Subspecialty Group of Respirology. (2016). The Society of Pediatrics, Chinese Medical Association guidelines for the diagnosis and prevention of asthma in children. Chin J Pediatr. (2016). 54:167–81. doi: 10.3760/ema.j.issn.0578-1310.2016.03.003
13. Ministry of Environmental Protection of P. R. C. Technical requirements for environmental air quality index (AQI) (for Trial Implementation). J China Environ Manag Cadre Coll. (2012) 22:44.
14. The Global Strategy for Asthma Management and Prevention. Global Initiative for Asthma (GINA) (2016). http://www.ginasthma.org/
15. Price D, Fletcher M, van der Molen T. Asthma control and management in 8,000 European patients: the REcognise Asthma and LInk to Symptoms and Experience (REALISE) survey. NPJ Prim Care Respir Med. (2014) 24:14009. doi: 10.1038/npjpcrm.2014.9
16. Zhang YY. (2008). Assessment of Asthma Control of Shi Jiazhuang City and the Multiplicity of the Risk Factors (Master's thesis). Hebei Medical University, Shijiazhuang, China.
17. Cheng XM, Huang ZS, Zhang YQ, Wang B, Ma QL, Zhang Q, et al. Re-survey on current status of treatment and control in asthmatic outpatients. Chin J Asthma. (2011) 31:810–3.
18. Slejko JF, Ghushchyan VH, Sucher B, Globe DR, Lin S-L, Globe G, et al. Asthma control in the United States, 2008-2010: indicators of poor asthma control. J Allergy Clin Immunol. (2014) 133:1579–87. doi: 10.1016/j.jaci.2013.10.028
19. Mentz G, Robins TG, Batterman S, Naidoo RN. Acute respiratory symptoms associated with short term fluctuations in ambient pollutants among schoolchildren in Durban, South Africa. Environ Pollut. (2018) 233:529–39. doi: 10.1016/j.envpol.2017.10.108
20. Khreis H, de Hoogh K, Nieuwenhuijsen MJ. Full-chain health impact assessment of traffic-related air pollution and childhood asthma. Environ Int. (2018) 114:365–75. doi: 10.1016/j.envint.2018.03.008
21. Oliveira M, Slezakova K, Delerue-Matos C, Pereira MC, Morais S. Children environmental exposure to particulate matter and polycyclic aromatic hydrocarbons and biomonitoring in school environments: A review on indoor and outdoor exposure levels, major sources and health impacts. Environ Int. (2019) 124:180–204. doi: 10.1016/j.envint.2018.12.052
22. Luong LMT, Sly PD, Thai PK, Phung D. Impact of ambient air pollution and wheeze-associated disorders in children in Southeast Asia: a systematic review and meta-analysis. Rev Environ Health. (2019) 34:125–39. doi: 10.1515/reveh-2018-0079
23. Garcia E, Berhane KT, Islam T, McConnell R, Urman R, Chen Z, et al. Association of changes in air quality with incident asthma in children in California, 1993-2014. JAMA. (2019) 321:1906–15. doi: 10.1001/jama.2019.5357
24. Mazenq J, Dubus J-C, Gaudart J, Charpin D, Nougairede A, Viudes G, et al. Air pollution and children's asthma-related emergency hospital visits in southeastern France. Eur J Pediatr. (2017) 176:705–11. doi: 10.1007/s00431-017-2900-5
25. Rojas-Rueda D, Vrijheid M, Robinson O, Marit AG, Grazuleviciene R, Slama R, et al. Environmental burden of childhood disease in Europe. Int J Environ Res Public Health. (2019) 16:1084. doi: 10.3390/ijerph16061084
26. Johansson K, McSorley HJ. Interleukin-33 in the developing lung-Roles in asthma and infection. Pediatr Allergy Immunol. (2019) 30:503–10. doi: 10.1111/pai.13040
27. Unuvar S, Erge D, Kilicarslan B, Bag HGG, Catal F, Girgin G, et al. Neopterin levels and indoleamine 2,3-dioxygenase activity as biomarkers of immune system activation and childhood allergic diseases. Ann Lab Med. (2019) 39:284–90. doi: 10.3343/alm.2019.39.3.284
28. Qiu YY, Zhang YW, Qian XF, Bian T. MiR-371, miR-138, miR-544, miR-145, and miR-214 could modulate Th1/Th2 balance in asthma through the combinatorial regulation of Runx3. Am J Transl Res. (2017) 9:3184–99.
29. Kim H, Kim H, Lee J-T. Assessing the cold temperature effect on hospital visit by allergic rhinitis in Seoul, Korea. Sci Total Environ. (2018) 633:938–45. doi: 10.1016/j.scitotenv.2018.03.166
30. Kutlug S, Kilic M, Bilgici B, Paksu S, Yildiran A, Sancak R. An evaluation of vitamin D levels in children with seasonal allergic rhinitis during pollen season. Pediatr Allergy Immunol. (2017) 28:446–51. doi: 10.1111/pai.12728
31. Moesges R, Bachert C, Panzner P, Calderon MA, Haazen L, Pirotton S, et al. Short course of grass allergen peptides immunotherapy over 3weeks reduces seasonal symptoms in allergic rhinoconjunctivitis with/without asthma: a randomized, multicenter, double-blind, placebo-controlled trial. Allergy. (2018) 73:1842–50. doi: 10.1111/all.13433
32. Braido F, Brusselle G, Guastalla D, Ingrassia E, Nicolini G, Price D, et al. Determinants and impact of suboptimal asthma control in Europe: the INTERNATIONAL CROSS-SECTIONAL AND LONGITUDINAL ASSESSMENT ON ASTHMA CONTROL (LIAISON) study. Resp Res. (2016) 17:51. doi: 10.1186/s12931-016-0374-z
33. Gao ZS, Fu WY, Sun YM, Gao BY, Wang HY, Liu ML, et al. Artemisia pollen allergy in China: component-resolved diagnosis reveals allergic asthma patients have significant multiple allergen sensitization. Allergy. (2019) 74:284–93. doi: 10.1111/all.13597
34. Bobrowska-Korzeniowska M, Stelmach I, Brzozowska A, Jerzynska J, Mital M, Stelmach W. The effect of passive smoking on exhaled nitric oxide in asthmatic children. Nitric Oxide-Biol Chem. (2019) 86:48–53. doi: 10.1016/j.niox.2019.01.012
35. Solet JL, Raherison-Semjen C, Mariotti E, Le Strat Y, Gallay A, Bertrand E, et al. A cross sectional survey to estimate prevalence and associated factors of asthma on Reunion Island, Indian Ocean. BMC Public Health. (2019) 19:9. doi: 10.1186/s12889-019-7031-7
36. Bousquet J, Clark TJH, Hurd S, Khaltaev N, Lenfant C, O'Byrne P, et al. GINA guidelines on asthma and beyond. Allergy. (2007) 62:102–12. doi: 10.1111/j.1398-9995.2006.01305.x
37. Castro-Rodriguez JA, Rodriguez-Martinez CE, Ducharme FM. Daily inhaled corticosteroids or montelukast for preschoolers with asthma or recurrent wheezing: a systematic review. Pediatr Pulmonol. (2018) 53:1670–7. doi: 10.1002/ppul.24176
38. Bao Y, Chen Z, Liu E, Xiang L, Zhao D, Hong J. Risk factors in preschool children for predicting asthma during the preschool age and the early school age: a systematic review and meta-analysis. Curr Allergy Asthma Rep. (2017) 17:85. doi: 10.1007/s11882-017-0753-7
39. Bednarek A, Bodajko-Grochowska A, Bartkowiak-Emeryk M, Klepacz R, Ciolkowski J, Zarzycka D, et al. Demographic and medical factors affecting short-term changes in subjective evaluation of asthma control in adolescents. Postep Dermatol Alergol. (2018) 35:259–66. doi: 10.5114/ada.2018.76221
Keywords: childhood asthma, disease control rate, risk factors, allergic history, air quality
Citation: Zhu Y, Zhong T, Ge D, Li Q and Wu J (2019) Multi-Factor Analysis of Single-Center Asthma Control in Xiamen, China. Front. Pediatr. 7:498. doi: 10.3389/fped.2019.00498
Received: 18 August 2019; Accepted: 18 November 2019;
Published: 03 December 2019.
Edited by:
Kostas N. Priftis, National and Kapodistrian University of Athens, GreeceReviewed by:
Aroonwan Preutthipan, Mahidol University, ThailandCopyright © 2019 Zhu, Zhong, Ge, Li and Wu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qiyuan Li, cWl5dWFuLmxpQHhtdS5lZHUuY24=; Jinzhun Wu, MTkyMzczMTIwMUBxcS5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.