- 1Department of Pediatric Cardiology, Saarland University Medical Center, Homburg, Germany
- 2Medical School, University of Saarland, Homburg, Germany
- 3Institute for Medical Biometry, Epidemiology and Medical Informatics, Saarland University Medical Center, Homburg, Germany
- 4SPG, Saarpfalz-Gymnasium, Homburg, Germany
- 5Department of Neuropediatrics, Saarland University Medical Center, Homburg, Germany
- 6Department of Anesthesiology, Intensive Care and Pain Therapy, Saarland University Medical Center, Homburg, Germany
- 7Department of Pediatrics and Neonatology, Saarland University Medical Center, Homburg, Germany
Aim: To provide data on the inadequate use of emergency medical transports services (EMTS) in children and underlying contributing factors.
Methods: This was a prospective single-center cohort study (01/2017-12/2017) performed at the Saarland University Children's Hospital, Homburg, Germany. Patients ≤20 years of age transported by EMTS for suspected acute illness/trauma were included and proportion of inadequate/adequate EMTS use, underlying contributing factors, and additional costs were analyzed.
Results: Three hundred seventy-nine patients (mean age: 9.0 ± 6.3 years; 55.7% male, 44.3% female) were included in this study. The three most common reasons for EMTS use were: central nervous system (30.6%), respiratory system affection (14.0%), and traumas (13.2%). ETMS use was categorized as inadequate depending on physician's experience: senior physician (58.8%), pediatrician (54.9%), resident (52.7%). All three physicians considered 127 (33.5%) cases to be medically indicated for transportation by EMTS, and 177 (46.7%) to be medically not indicated. The following parameters were significantly associated with inadequate EMTS use: non-acute onset of symptoms (OR 2.5), parental perception as non-life-threatening (OR 1.7), and subsequent out-patient treatment (OR 4.0). Conversely, transport by an emergency physician (OR 3.5) and first time parental EMTS call (OR 1.7) were associated with adequate use of EMTS. Moreover, a significant relation existed between maternal, respectively, paternal educational status and inadequate EMTS use (each p = 0.01). Using multiple logistic regression analysis, non-acute onset of symptoms (OR 2.2) was associated with inadequate use of EMTS while first time parental EMTS call (OR 1.8), transport by an emergency physician (OR 3.3), and need for in-patient treatment (OR 4.0) were associated with adequate use of EMTS.
Conclusion: A substantial number of pediatric EMTS is medically not indicated. Possibly, specific measures including multifaceted educational efforts may be helpful in reducing unnecessary EMTS use.
Introduction
Overcrowded emergency departments (ED) are a well-known problem in highly-industrialized countries (1, 2). One important reason is the increasing demand for hospital and ED care, but the misuse of emergency medical transport services (EMTS) as a taxi service must be taken into consideration as well. Interestingly, the incidence of life-threatening illness in children is at an all-time low while presentations and admissions to hospital increase (3). Several studies have demonstrated that up to 61% of EMTS are not medically necessary (4–10), thus putting a relevant financial burden on the health-care system.
While pediatric emergencies are rare at an estimated rate of 5–10% of all EMTS (11–14), misuse of the EMTS has been reported for children as well (8, 9, 15). Among a number of contributing factors, parental over-anxiety appears to be one of the most relevant reasons (16). Conversely, rapid assessment of the medical necessity whether or not to use an EMTS in children is challenging for parents and teachers as well as EMTS staff, in part because of poor medical routine in pediatric emergencies.
The aim of this study was to provide current data on the inadequate EMTS use in children in Germany (Saarpfalz region). Secondly, we performed an explorative analysis of potential, underlying factors that may contribute to this problem. Thirdly, an estimation of additional costs secondary to the unnecessary EMTS use was made.
Patients and Methods
After institutional review board approval from the ethics committee of Saarland, Saarbrücken, Germany, this prospective explorative study (PEACE study) was performed at the University Children's Hospital of Saarland, Homburg/Saar, Germany (Saarpfalz region) between 01 January and 31 December 2017. The PEACE study was reported using the STROBE guideline (Supplementary Data Sheet 1) (17).
The pediatric emergency department of the Saarland University Medical Center, Homburg/Saar, Germany, is the largest emergency department in Saarland with ~5,000 visits per year.
The time period of 1 year was considered representative since acute diseases typically occurring at different time points (seasons) were included in this study, generating a convenient and adequate sample size of children using EMTS.
All patients ≤20 years of age who were transported to our ED by EMTS were assessed for potential enrollment in this study. The upper limit of age of ≤20 years was attributed to the fact that patients with complex, pediatric diseases were included. These patients are primarily transferred to our children's hospital by EMTS because of ongoing treatment of these patients in our hospital, e.g., children/adolescents/young adults with complex congenital heart disease, and patients with complex genetic syndromes affecting the central nervous system. Exclusion criteria were: lack of parental informed consent and transfer from another hospital/doctor's office per EMTS, and patients requiring immediate resuscitation, or patient-specific missing data >10%.
Patients' data were collected prospectively from the hand-written and electronic patients' medical charts (SAP, Walldorf, Germany) and included the following information: gender, age, transport by EMTS only or staffed with an emergency physician, suspected diagnosis at admission, time, week-day and month of presentation. Potential underlying risk factors as detailed below were specified a priori.
All participating families were asked to fill out a questionnaire, which included questions with regard to the current and past medical problems and the social status of the family. The following questions were chosen for data analysis:
Questions regarding the emergency:
1) Duration of symptoms: acute = sudden onset of symptoms, non-acute = duration of symptoms for several hours or longer
2) Perception of situation as life-threatening?
3) First-time call of EMTS for your child?
4) If “no,” how often have you used EMTS?
5) Availability of car or access to other transport possibilities (e.g., public transport)?
Questions regarding parental/family status
1) Number of children? Single parent?
2) Parental educational status: low = no graduation, special-needs school, secondary school or middle = middle school, academic high school or higher = university
3) Current occupation: unskilled, skilled, highly skilled, others
4) Parental age: <40 years, 40–60 years, >60 years.
All included cases were evaluated by a senior physician in pediatrics and pediatric emergency medicine (SM), a fully trained pediatrician (MP), and a resident (MB). All three physicians were blinded to each other.
The included medical cases were categorized down into:
1) Yes, EMTS use was medically indicated.
2) No, EMTS use was medically not indicated, including EMTS medically not indicated but considered reasonable because of specific circumstances (e.g., patient at school and transportation by car not feasible).
3) Assessment was not possible because of inadequate medical information.
For final statistical analysis, the assessment by the senior physician was used because his long-standing experience was considered most reliable in providing a correct medical assessment. Inter-rater agreement was calculated using Cohen's Kappa coefficient.
“Medically indicated” was defined as “A sudden and usually unforeseen event that calls for immediate measures to minimize its adverse consequences” (18, 19). Immediate means that 95% of the emergency patients have to be seen by EMTS within 20 min of receipt of emergency call. At time of assessment, all three physicians were unaware of the further medical course (e.g., need for hospital admission etc.) of included patients.
“Medically not indicated” was defined as any clinical condition that did not mandate immediate medical assessment, diagnostic work-up, or treatment.
In the federal state of Saarland, costs for EMTS operations during the study period were [https://www.zrf-saar.de/de/wir_ueber_uns/aufgaben_des_zrf_saar/finanzierung_tarifverhandlungen (accessed 28.12.2019)]:
• 441.00 € for transport by EMTS only
• 870.00 € for transport by accompanying emergency physician.
Data were pseudonymized for statistical analysis. Statistical analysis was performed using IBM SPSS Statistics (IBM Corp., Released 2010; IBM SPSS Statistics for Macintosh, Version 19, Armonk, NY, USA). Data is presented as absolute numbers, percentage, odds ratios (OR), and 95% confidence intervals (95%-CI). Binary logistic regression analysis was computed with forward and backward (Wald) method. In cases of incongruent results, only the results of the backward computed logistic regression are reported. For each variable, univariate logistic regression analysis was performed, and all significant variables were included into the multiple logistic regression analysis. Since the aim of the regression analysis was to identify variables which contributed to the adequate/inadequate EMTS use, the “adequate EMTS use,” respectively, the “inadequate EMTS use” were the dependent variables. The independent variables were the potential, underlying factors that may have contributed to this problem. Comparison between variables was performed using Chi2-test. A p-value of <0.05 was considered statistically significant.
To explore a potential bias, both data from patients with parental consent as well as data where parental consent could not be obtained for the questionnaire were included, and we subsequently analyzed the basic data with regard to demographics and assessment of the adequacy of EMTS use of the two groups (Supplementary Table 1).
Results
In total, 597 pediatric patients brought to our hospital by EMTS from home or non-medical facilities were assessed. After exclusion of patients who did not meet the inclusion criteria (most common cause: lack of parental consent) 379 patients (mean age: 9.0 ± 6.3 years, range: 0–19.2 years; 55.7% male, 44.3% female) were enrolled and subsequently analyzed (Figure 1). Patients' and family characteristics are depicted in Tables 4, 5.
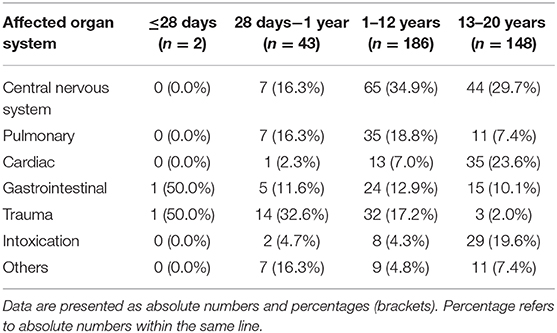
In most cases (n = 330, 87.1%), parents did not contact their family physician, family general physician or a hospital. The three most common reasons for EMTS use were: central nervous system (CNS) (n = 116, 30.6%) and pulmonary system affection (n = 53, 14.0%), and traumas (n = 50, 13.2%). An analysis of the affected organ systems by age is depicted in Table 1.
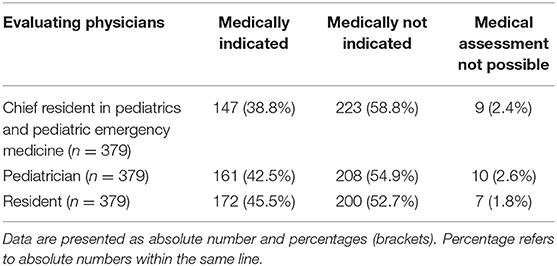
All three physicians considered 127 (33.5%) cases to be medically indicated for transportation by EMTS, and 177 (46.7%) not to be medically indicated. In 75 (19.8%) cases, all three physicians could not agree on the necessity for EMTS. The assessment of inadequate EMTS was depending on the physician's experience: senior physician in pediatrics and emergency medicine: 58.8%; 13.2% of EMTS were medically not indicated, but considered reasonable because of specific circumstances; pediatrician: 54.9%; 20.3% of EMTS medically not indicated, but considered reasonable because of specific circumstances; resident: 52.7%; 12.1% medically not indicated, but considered reasonable because of specific circumstances (Table 2).
The inter-rater agreement was as followed: rater 1 vs. rater 2: Kappa 0.777, p = 0.000, rater 1 vs. rater 3: Kappa 0.747, p = 0.000 and rater 2 vs. rater 3: Kappa 0.770, p = 0.000.
In the group of adequate EMTS, the three most common indications were: CNS affection (n = 56, 38.1%), intoxications (n = 25, 17.0%), and pulmonary disorders (n = 22, 15.0%). In the group of inadequate EMTS, the three most common indications were: CNS (n = 58, 26.0%), gastrointestinal (n = 40, 17.9%), and the cardiovascular system (n = 33, 14.8%). The number of non-acute complaints in the group of inadequate EMTS was almost twice as high as in the group of adequate EMTS (Table 3).
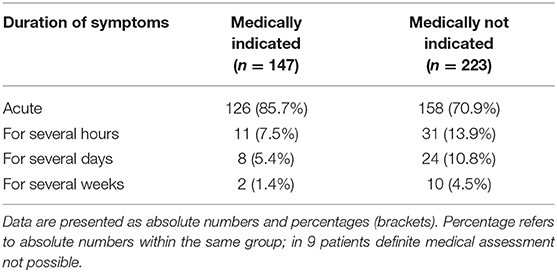
Table 3. Duration of symptoms categorized by medically indicated, respectively, not indicated EMTS (emergency medical transport service).
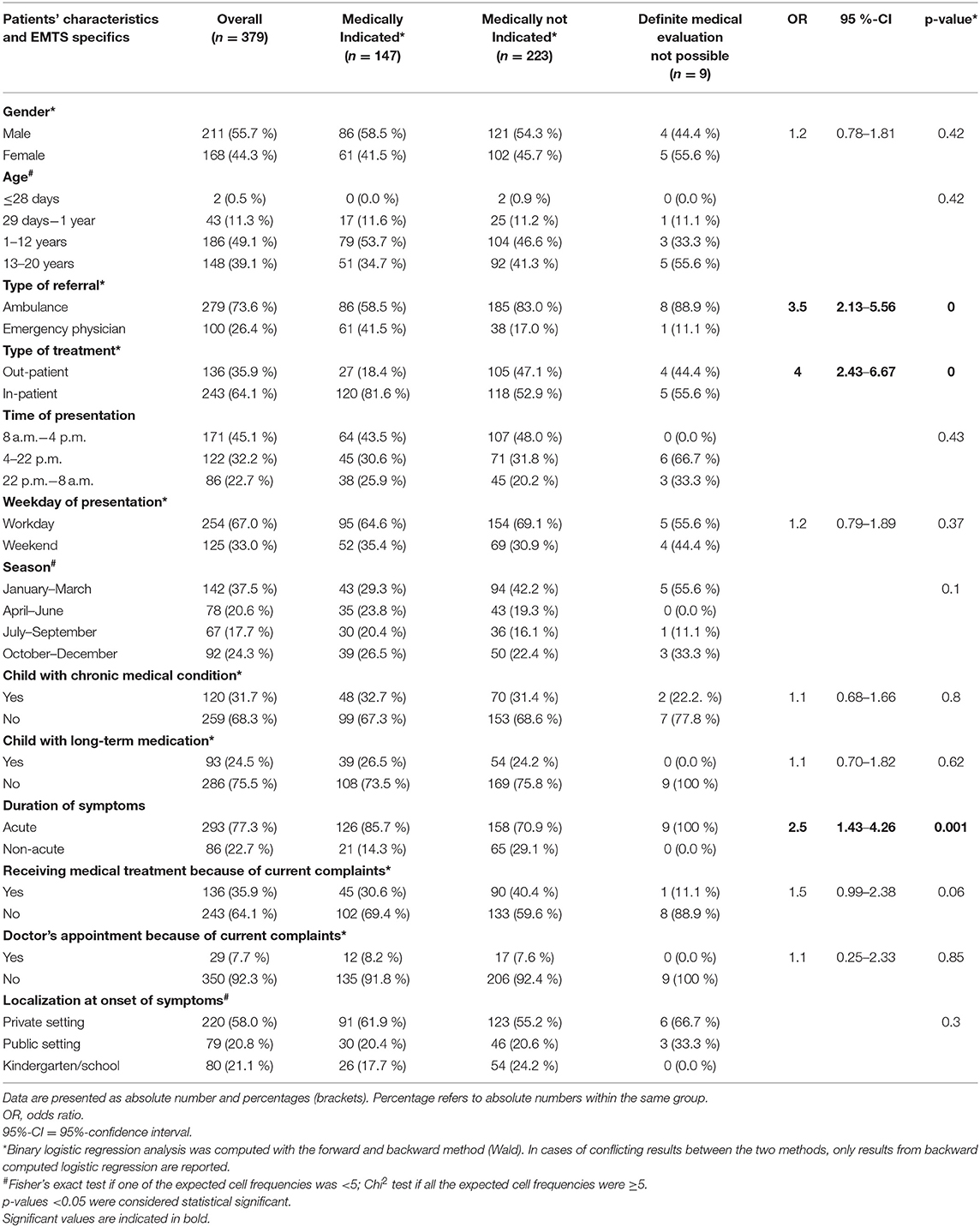
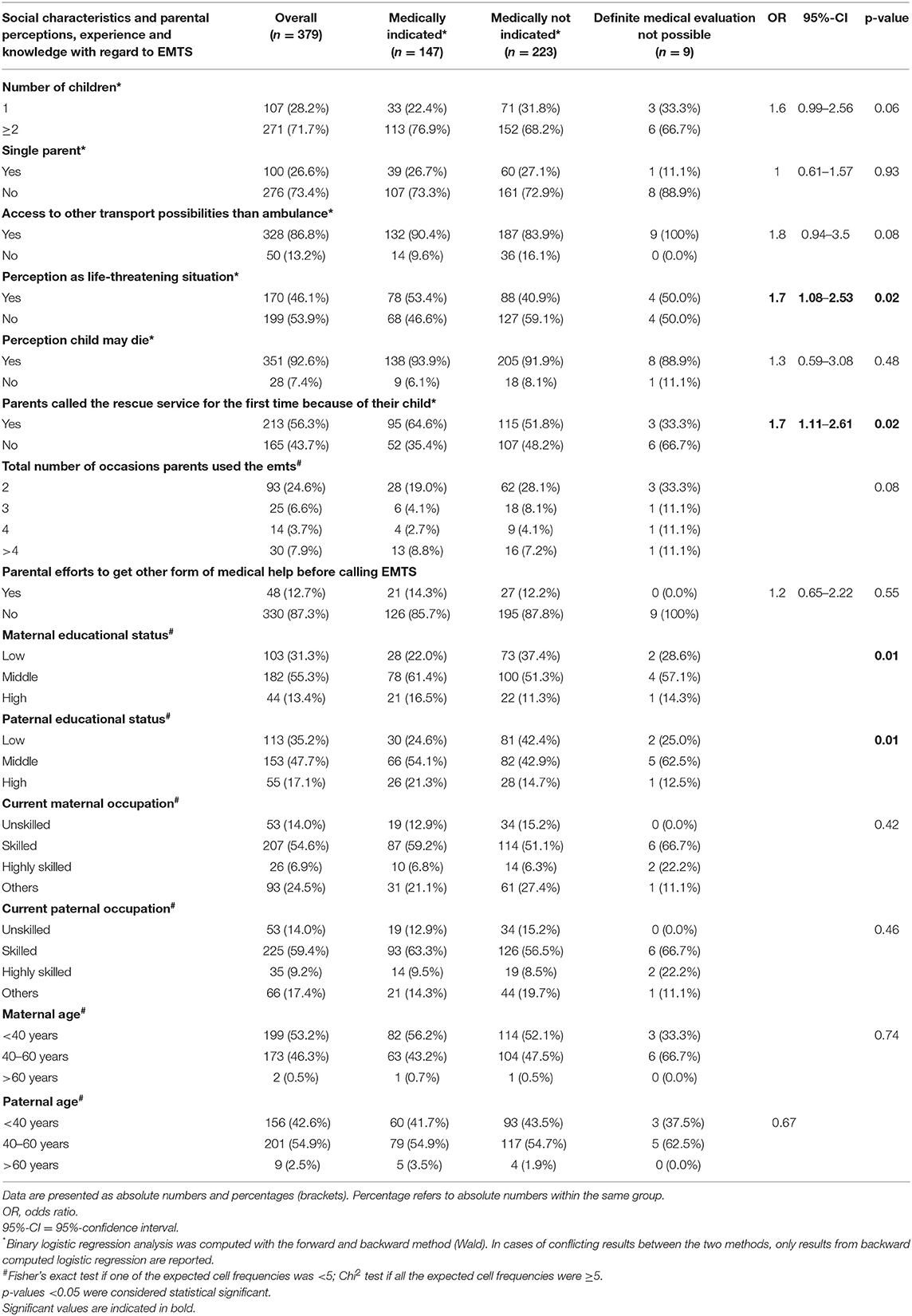
The following parameters were significantly associated with inadequate EMTS use (Tables 4, 5): non-acute onset of symptoms, parental perception as non-life-threatening, and subsequent out-patient treatment. Conversely, transport by an emergency physician and first time parental EMTS-call were associated with adequate use of EMTS. Moreover, a significant relation existed between maternal, respectively, paternal educational status and inadequate EMTS use (each p = 0.01).
Using multiple logistic regression analysis, non-acute onset of symptoms (OR 2.2, 95%-CI [1.20–3.87]) was associated with inadequate use of EMTS, while first time parental EMTS call (OR 1.8, 95%-CI [1.12–2.03]), transport by emergency physician (OR 3.3, 95%-CI [1.95–5.49]), and need for in-patient treatment (OR 4.0, 95%-CI [2.39–6.85]) were associated with adequate use of EMTS.
In total, medical expenditures of 210,039 € incurred in our cohort; 123,039 € related to EMTS use and 87,000 € related to EMTS use operated by emergency physicians. More than half of these costs was secondary to inadequate EMTS use, causing additional costs of 114,645 € (ambulance 81,585 € and emergency physician 33,060 €) per year.
Discussion
In our prospective exploratory PEACE study, a substantial number of EMTS use was medically not indicated (46.7%). We were able to demonstrate that a number of underlying risk factors were contributory to the inadequate use of EMTS, i.e., non-acute onset of symptoms (OR 2.5), parental perception as non-life-threatening (OR 1.7), and subsequent out-patient treatment (OR 4.0), while transport by emergency physician (OR 3.5) and first time parental EMTS-call (OR 1.7) were associated with adequate use of EMTS. The physician's assessment with regard to the adequacy of EMTS use was dependent on the level of clinical experience of the evaluating physician, i.e. the more experienced the physician, the higher the rate of unnecessary use of EMTS.
Particularly, parental educational status [maternal (p = 0.01) and paternal educational status (p = 0.01)] had an important impact on the misuse of the EMTS. Interestingly, medium socio-economic status was associated with the lowest percentage of inadequate EMTS use. Although quite speculative, low socio-economic status may possibly be associated with poorer medical knowledge while over-anxiety regarding child's health may be more prevalent in higher socio-economic classes, thus contributing to the inadequate use of EMTS. Conversely, occupational status and parental age were not significantly associated with adequate/inadequate use of EMTS. Interestingly, data from the U.S. (8) demonstrated that the inadequate use of EMTS in children was strongly associated with their medical insurance status (unnecessary use occurred significantly more often in children with Medicaid insurance compared to commercial insurance coverage), indicating that socio-economic factors are contributory to this pattern of misuse.
Owing to today's family structures with small families and many single-parent households, a lack of basic medical knowledge and experience in the proper assessment of children appears to be another contributing factor to the excessive use of EMTS. Therefore, regular visits to the family pediatrician constitute an opportunity to provide families with relevant medical information in order to cut down on the number of inadequate EMTS use. Notably, we were able to demonstrate that families with more children used EMTS that were not medically indicated less frequently; however, this did not reach statistical significance (p = 0.05, OR 1.6, 95%-CI [0.99–2.56]).
Apparently, parents often overestimate the seriousness of their child's disease, which is an important reason for the substantial number of inadequate EMTS use (16, 20). While Camasso-Richardson et al. (9) reported that only 38% of the EMTS occurred during off-hours, about 55% were performed during this time period in our study. This finding is supported by Miller et al. (15) and Seidel et al. (12), who demonstrated a peak in EMTS between 4 and 8 p.m., respectively, noon and 8 p.m. This large number of transports during off-hours may in part be caused by parental subjective assessment that their child may be more severely affected in the evening or at night (21). However, inadequate use of EMTS was not related to day or nighttime in our study.
Miller et al. (15) reported that EMTS use was independent of weekday or season. This is in line with our study, where we did not find any differences with regard to weekdays and seasonal timing on the EMTS use (p = 0.37). Although not significant, a higher number of medically not indicated EMTS occurred during January–March (p = 0.1). During winter-time, the numbers of non-severe, non-life-threatening pulmonary, and gastrointestinal diseases (bronchitis, gastroenteritis) were higher than during summer months, and might have contributed to this finding. In line with previous reports, the most common diagnoses in our cohort were CNS (30.6%) and pulmonary diseases (14.0%), and traumas (13.2%) (9, 15).
In the study by Camasso-Richardson et al. (9), 40% of families had no other possibility to reach the ED, and 86% (79/92) did not contact their pediatrician/general physician prior to calling the emergency number; 71% (40/56) stated that they could have reached the hospital safely by car, bus or taxi (9, 22). These findings are in line with our results, although the number of persons having no access to a car or other transport possibilities was much lower in our cohort (13.2%). This may have been at least in part related to the specific geographic circumstances in our study. Remarkably and in line with the report by Camasso-Richardson et al. (9), most families in our cohort did not contact any medical provider before calling the EMTS (87.1%). One possible reason for the inadequate EMTS use might have been that by using this service immediate medical help is provided with very short waiting times at the ED as demonstrated by Yarris et al. (22) providing adequate medical information may also reduce the number of inadequate EMTS use in patients with recurrent episodes of medical emergencies, e.g., febrile seizures which were generally categorized as clinical situations, which did not mandate the use of EMTS after the first episode. This may open a window for further parental education.
The decision to use EMTS was at the discretion of the medical dispatcher—a well-trained paramedic with extensive experience in emergency medicine. Thus, in addition to parental educational programs, it appears equally important to provide better training in pediatric emergencies for medical personnel. This notion is corroborated by the fact that assessment of a pediatric emergency in our study was subject to physician's experience in this field, and this is also reflected by the fact that in 19.8% of cases, no agreement between the three evaluating physicians could be reached. However, inter-rater agreement was very good in our study. Moreover, non-medical professions (e.g., teachers) should have a basic medical command of emergency situations in order to initiate adequate lay interventions.
Campaigns to inform the public of a reasonable EMTS use bear the potential to reduce the unnecessary use of EMTS. Ohshige (23) reported a reduced utilization of the ambulance in Yokohama by implementing specific public educational programs. However, by using posters in public facilities as well as handouts and public loudspeaker announcements to inform the population of a responsible EMTS use, patients with serious diseases like stroke and myocardial infarction used the EMTS less frequently (23).
In 2012/2013, 14,263,948 EMTS were performed in Germany causing a financial burden of about 7,38 billion euros (24). Thereof, about 5–10% of all EMTS were pediatric emergencies (11–13), which translates into 700,000–1,400,000 pediatric EMTS and costs of about 369–738 million euros. Projecting our data of inadequate EMTS use (annual extra costs of 114,645 euros) to the national level, our analysis would translate into an approximate estimation of extra costs of about 172–344 million euros per year in Germany. Moreover, when looking at these numbers, it is also important to note that a minor percentage required hospitalizations after initial denial of EMTS (25–27).
Possible shortcomings of our study are related to (a) it being a single-center assessment, and (b) the clinical setting of our study. The University Children's Hospital of Saarland is located in a small town in Germany with a more rural environment. Therefore, our numbers may differ from urban or suburban regions, and our data may not be fully transferable to other regions within Germany or to other industrialized countries. However, the ambulance service of the Saarpfalz region provides EMTS for a number of towns with populations ranging from 50,000–85,0000 people as well.
Moreover, about one third of the patients had to be excluded because parental informed consent could not be obtained for full assessment. This might have influenced the significance of different variables. However, no differences with regard to both demographics as well as the use of EMTS were seen between the two groups (Supplementary Table 1).
We conclude that—as in many other industrialized countries—a substantial number of EMTS use is medically not indicated (4–10, 28). In addition to previous reports, our study provides an analysis of possible contributing risk factors. The inadequate use of EMTS causes substantial extra costs per year. Reasonable EMTS use is needed, requiring continuing multifaceted education of parents, families, and teachers as well as of EMTS staff.
Data Availability Statement
All datasets generated for this study are included in the article/Supplementary Material.
Ethics Statement
Full name of the ethics committee that approved the study: Ethics committee of Saarland, Saarbrücken, Germany. Consent procedure used for human participants or for animal owners: This study was carried out in accordance with the recommendations of name of guidelines, name of committee; with written informed consent from all subjects. All subjects gave written informed consent in accordance with the Declaration of Helsinki. The protocol was approved by the name of committee. Any additional considerations of the study in cases where vulnerable populations were involved (for example minors, persons with disabilities or endangered animal species: not applicable.
Author Contributions
MP was responsible for study design, data analysis, and writing of the manuscript. MB was responsible for study design, data analysis, and critical review of the manuscript. SW was responsible for statistical analysis and critical review of the manuscript. BZ was responsible for data compilation. HS was responsible for data analysis and critical review of the manuscript. MFB was involved in patient care and was responsible for critical review of the manuscript. UG was responsible for critical review of the manuscript. MZ was responsible for critical data analysis and review of the manuscript. SM was chief investigator and responsible for study design, data analysis, and writing of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank all participating families who made this work possible. We thank Dagmar Sauer for important linguistic revisions of the manuscript.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2019.00442/full#supplementary-material
References
1. Schneider S, Zwemer F, Doniger A, Dick R, Czapranski T, Davis E. Rochester, New York: a decade of emergency department overcrowding. Acad Emerg Med. (2001) 8:1044–50. doi: 10.1111/j.1553-2712.2001.tb01113.x
2. Olshaker JS, Rathlev NK. Emergency Department overcrowding and ambulance diversion: the impact and potential solutions of extended boarding of admitted patients in the Emergency Department. J Emerg Med. (2006) 30:351–6. doi: 10.1016/j.jemermed.2005.05.023
3. Neill S, Roland D, Thompson M, Tavaré A, Lakhanpaul M. Why are acute admissions to hospital of children under 5 years of age increasing in the UK? Arch Dis Child. (2018) 103:917–9. doi: 10.1136/archdischild-2017-313958
4. Gardner GJ. The use and abuse of the emergency ambulance service: some of the factors affecting the decision whether to call an emergency ambulance. Emerg Med J. (1990) 7:81–9. doi: 10.1136/emj.7.2.81
5. Richards JR, Ferrall SJ. Inappropriate use of emergency medical services transport: comparison of provider and patient perspectives. Acad Emerg Med. (1999) 6:14–20. doi: 10.1111/j.1553-2712.1999.tb00088.x
6. Morris DL, Cross AB. Is the emergency ambulance service abused? BMJ. (1980) 281:121–3. doi: 10.1136/bmj.281.6233.121
7. Billittier AJ, Moscati R, Janicke D, Lerner EB, Seymour J, Olsson D. A multisite survey of factors contributing to medically unnecessary ambulance transports. Acad Emerg Med. (1996) 3:1046–50. doi: 10.1111/j.1553-2712.1996.tb03352.x
8. Kost S, Arruda J. Appropriateness of ambulance transportation to a suburban pediatric emergency department. Prehospital Emerg Care. (1999) 3:187–90. doi: 10.1080/10903129908958934
9. Camasso-Richardson K, Wilde JA, Petrack EM. Medically unnecessary pediatric ambulance transports: a medical taxi service? Acad Emerg Med. (1997) 4:1137–41. doi: 10.1111/j.1553-2712.1997.tb03696.x
10. Hjälte L, Suserud BO, Herlitz J, Karlberg I. Why are people without medical needs transported by ambulance? A study of indications for pre-hospital care. Eur J Emerg Med. (2007) 14:151–6. doi: 10.1097/MEJ.0b013e3280146508
11. Ramgopal S, Elmer J, Escajeda J, Martin-Gill C. Differences in prehospital patient assessments for pediatric versus adult patients. J Pediatr. (2018) 199:200–5.e6. doi: 10.1016/j.jpeds.2018.03.069
12. Seidel JS, Henderson DP, Ward P, Wayland BW, Ness B. Pediatric prehospital care in urban and rural areas. Pediatrics. (1991) 88:681–90.
13. Shah MN, Cushman JT, Davis CO, Bazarian JJ, Auinger P, Friedman B. The epidemiology of emergency medical services use by children: an analysis of the national hospital ambulatory medical care survey. Prehospital Emerg Care. (2008) 12:269–76. doi: 10.1080/10903120802100167
14. Schlechtriemen T, Masson R, Burghofer K, Lackner CK, Altemeyer KH. Pädiatrische Notfälle in der präklinischen Notfallmedizin. Anaesthesist. (2006) 55:255–62. doi: 10.1007/s00101-005-0922-2
15. Miller MK, Denise Dowd M, Gratton MC, Cai J, Simon SD. Pediatric out-of-hospital emergency medical services utilization in Kansas city, Missouri. Acad Emerg Med. (2009) 16:526–31. doi: 10.1111/j.1553-2712.2009.00418.x
16. Bauchner H, McCarthy PL, Sznajderman SD, Baron MA, Fink HD, Forsyth B, et al. Do mothers overestimate the seriousness of their infants' acute illnesses? J Dev Behav Pediatr. (1987) 8:255–9.
17. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg. (2014) 12:1495–9. doi: 10.1016/j.ijsu.2014.07.013
18. Fuchs S, Terry M, Adelgais K, Bokholdt M, Brice J, Brown KM, et al. Definitions and assessment approaches for emergency medical services for children. Pediatrics. (2016) 138:e20161073. doi: 10.1542/peds.2016-1073
19. Project R. Glossary of Humanitarian Terms. (2008). Available online at: www.reliefweb.int (accessed January 19, 2019).
20. McCarthy PL, Sznajderman SD, Lustman-Findling K, Baron MA, Fink HD, Czarkowski N, et al. Mothers' clinical judgment: a randomized trial of the Acute Illness Observation Scales. J Pediatr. (1990) 116:200–6. doi: 10.1016/S0022-3476(05)82875-6
21. Meyer S, Grundmann U, Reinert J, Gortner L. Notfälle im Kindesalter. Med Klin Intens Notfallmed. (2015) 110:633–43. doi: 10.1007/s00063-015-0104-1
22. Yarris LM, Moreno R, Schmidt TA, Adams AL, Brooks HS. Reasons why patients choose an ambulance and willingness to consider alternatives. Acad Emerg Med. (2006) 13:401–5. doi: 10.1197/j.aem.2005.11.079
23. Ohshige K. Reduction in ambulance transports during a public awareness campaign for appropriate ambulance use. Acad Emerg Med. (2008) 15:289–293. doi: 10.1111/j.1553-2712.2008.00044.x
24. Gesundheitsberichterstattung des Bundes. Available online at: http://www.gbe-bund.de (accessed January 19, 2019).
25. Haines CJ, Lutes RE, Blaser M, Christopher NC. Paramedic initiated non-transport of pediatric patients. Prehospital Emerg Care. (2006) 10:213–9. doi: 10.1080/10903120500541308
26. Pringle RP, Carden DL, Xiao F, Graham DD. Outcomes of patients not transported after calling 911. J Emerg Med. (2005) 28:449–54. doi: 10.1016/j.jemermed.2004.11.025
27. Snooks H, Kearsley N, Dale J, Halter M, Redhead J, Cheung WY. Towards primary care for non-serious 999 callers: results of a controlled study of “Treat and Refer” protocols for ambulance crews. Qual Saf Health Care. (2004) 13:435–43. doi: 10.1136/qhc.13.6.435
Keywords: ambulance, emergency medical transport service, misuse, pediatric emergency, public health
Citation: Poryo M, Burger M, Wagenpfeil S, Ziegler B, Sauer H, Flotats-Bastardas M, Grundmann U, Zemlin M and Meyer S (2019) Assessment of Inadequate Use of Pediatric Emergency Medical Transport Services: The Pediatric Emergency and Ambulance Critical Evaluation (PEACE) Study. Front. Pediatr. 7:442. doi: 10.3389/fped.2019.00442
Received: 30 March 2019; Accepted: 10 October 2019;
Published: 25 October 2019.
Edited by:
Martin Chalumeau, Université Paris Descartes, FranceReviewed by:
Mehdi Oualha, Hôpital Necker-Enfants Malades, FranceChristèle Gras-Le Guen, Centre Hospitalier Universitaire (CHU) de Nantes, France
Fernando José Abelha, São João University Hospital Center, Portugal
Copyright © 2019 Poryo, Burger, Wagenpfeil, Ziegler, Sauer, Flotats-Bastardas, Grundmann, Zemlin and Meyer. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Martin Poryo, bWFydGluLnBvcnlvQHVrcy5ldQ==
†These authors have contributed equally to this work
 Martin Poryo
Martin Poryo Martin Burger2†
Martin Burger2† Harald Sauer
Harald Sauer Marina Flotats-Bastardas
Marina Flotats-Bastardas Michael Zemlin
Michael Zemlin Sascha Meyer
Sascha Meyer