- 1Department of Emergency Medicine, Changhua Christian Hospital, Changhua City, Taiwan
- 2School of Medicine, Chung Shan Medical University, Taichung City, Taiwan
- 3School of Medicine, Kaohsiung Medical University, Kaohsiung City, Taiwan
- 4Department of Emergency Medicine, Kaohsiung Chang Gung Memorial Hospital, Chang Gung University College of Medicine, Kaohsiung City, Taiwan
- 5Department of Leisure and Sports Management, Cheng Shiu University, Kaohsiung City, Taiwan
- 6Department of Biological Science and Technology, National Chiao Tung University, Hsinchu, Taiwan
- 7Department of Nursing, Dayeh University, Changhua City, Taiwan
- 8Department of Nursing, Changhua Christian Hospital, Changhua City, Taiwan
Background: In children with non-shockable out-of-hospital cardiac arrest, early epinephrine (EE) might help to establish the return of spontaneous circulation (ROSC) and be associated with survival. In the present study, we aimed to analyze the effects of EE on outcomes and post-resuscitation hemodynamics in children with non-shockable OHCA.
Methods: This was a retrospective analysis of data from 216 children (<19 years) who had suffered non-traumatic and non-shockable OHCA and received epinephrine for resuscitation (Jan 1, 2006–Dec 31, 2014). Demographics, pre-/in-hospital information, and the time to the first dose of epinephrine were recorded. Early post-resuscitation hemodynamics (the first hour after sustained ROSC), survival and good neurological outcomes (Pediatric Cerebral Performance Category Scales 1 or 2) were analyzed by the time to epinephrine—classified as early (EE): <15 min, intermediate (IE): 15–30 min, or late (LE): >30 min.
Results: Twenty-eight (13.0%) children survived to discharge, but only 17 (7.9%) had good neurological outcomes. In all, 41 (18.9%) children received EE; in comparison to IE and LE, this was significantly associated with tachycardia (73.9%) in the post-resuscitation period (p < 0.05). Tachycardia (OR: 7.41, 95% CI: 1.96–29.31) and hypertension (OR: 6.03, 95% CI: 1.85–13.77) were significantly associated with EE after adjusting for confounding factors. EE was also significantly associated with better overall outcomes than ME and LE (any ROSC, sustained ROSC, survival to the intensive care unit, admission, survival to discharge and good neurological outcomes, all p < 0.05).
Conclusions: EE helped to establish ROSC but was also associated with more tachycardia and hypertension in the early post-resuscitation period. In children with non-traumatic and non-shockable OHCA, EE was associated with a higher survival rate and better neurological outcomes than were ME and LE.
Introduction
The outcomes of children who suffer from non-traumatic out-of-hospital cardiac arrest (OHCA) are very poor (1–3). Only 1 to 19.6% of survivors have been reported as exhibiting good neurological outcomes (4–7). Several factors that could improve the chance of survival have been identified, including bystander cardiopulmonary resuscitation (CPR), initial shockable rhythm, chest compression-only CPR and shorter duration of transportation (3, 5, 7–12). Early epinephrine (EE) administration might be associated with survival, but may also exhibit both beneficial and harmful effects, as has been generally discussed in adult OHCA patients (13–15). Some studies have indicated that EE might help to establish spontaneous circulation during CPR by elevating cardiac output (β-agonist effects, increased heart rate, and contractility). The onset of action appears to be very rapid, with a half-life of only 5–10 min (16–18). However, other studies have suggested that the effect of EE may be limited. It also exhibits an intense α-agonist effect (the non-selective effect of epinephrine), leading to early vasoconstriction, increased tissue oxygen consumption and poor end-organ perfusion (19–23). Some studies have even reported that the harmful effects would be more obvious in end organs [i.e., limbs, brain, intestine, kidney; (19, 24, 25)]. More importantly, these effects would potentially be associated with poor neurological outcomes (21).
Thus, the controversial effects of EE raise several issues for emergency department (ED) physicians treating OHCA patients. Therefore, some large population studies have analyzed the patients' outcomes with different times to epinephrine administration. The overall effects of EE seem to be associated with better survival and neurological outcomes in adult OHCA patients (13, 26, 27). However, in OHCA children, information on the beneficial or harmful effects of EE is still limited. Although a few studies have reported that EE might increase the chance of achieving sustained return of spontaneous circulation (ROSC) and even survival in children with in-hospital cardiac arrest (IHCA), the detailed mechanism of the restoration of spontaneous circulation in early post-resuscitation periods is not clear (28, 29). Furthermore, the detailed effect of EE on post-resuscitation hemodynamics has not been well-addressed in non-traumatic OHCA in children.
It has been demonstrated that early defibrillation can establish spontaneous circulation more effectively than EE in patients with shockable rhythm [ventricular fibrillation (VF) and pulseless ventricular tachycardia (VT)] (13, 30). Therefore, the present study focusses on the effect of EE on non-shockable rhythms [asystole and pulseless electrical activity (PEA)]. We aim to analyze the effects of EE treatment on post-resuscitation hemodynamics in children with non-shockable and non-traumatic OHCA.
Materials and Methods
Study Design
The data of this study were retrospectively collected from the two medical centers—one in central and one in southern Taiwan (January 1, 2006 to December 31, 2014). Children (<19 years) were included who had suffered non-traumatic OHCA and received epinephrine for resuscitation. Patients' outcomes and post-resuscitation hemodynamics were analyzed according to the time to epinephrine treatment (early: <15 min, intermediate 15–30 min, late >30 min). The cut-off time points in this study were determined in accordance with a review of the literature (31–33).
Ethics Statement
This study was carried out in accordance with the recommendations of the STROBE statement. The protocol was approved by the institutional review board (IRB) of Changhua Christian Hospital (central Taiwan). Since this is a retrospective chart review study, and outputs were secondarily anonymized data, informed consent was not needed under the IRB permission. Finally, the team members and data collectors also followed the rules of the IRB.
(1) Full name of the ethics committee: Institutional review board (IRB) of Changhua Christian Hospital.
(2) Consent procedure: retrospective chart review; no formal consent necessary.
(3) Any additional considerations of the study in cases where vulnerable populations were involved, for example minors, persons with disabilities or endangered animal species: There were no additional considerations for vulnerable populations under the IRB permission.
Inclusion and Exclusion Criteria
Inclusion
Children (<19 years) who had suffered non-traumatic OHCA and received epinephrine for CPR.
Exclusion
(1) Cardiac arrest caused by trauma, intoxication, drowning, child abuse, or substance abuse.
(2) Absence of epinephrine treatment—either prehospital or ED or during CPR. Patients with a “Do Not Resuscitate” order were also excluded.
(3) Unknown time of collapse or time to first epinephrine.
(4) Incomplete medical records
(5) Initial shockable cardiac rhythm (VF/pulseless VT).
Study Setting and Population
Information on demographics and resuscitation was retrospectively obtained from the medical records (and CPR database). Prehospital information, including duration of prehospital CPR, duration from time of collapse to arrival of emergency medical services (EMS), time from EMS arrival to epinephrine, time from the scene of collapse to hospital, and witness of the arrest were obtained from EMS records or witnesses (i.e., EMS personal, family member, caregiver). The ages of children were classified into groups (infant: <1, toddler: 1–4, preschool children: 5–9, schoolchildren: 10–14, and adolescents: 15–19 years). The possible etiologies of arrest were divided into the following seven major causes: sudden infant death syndrome, cardiovascular diseases, neurological diseases, respiratory diseases, malignancy, infections, and others (including idiopathic causes). The ED resuscitation information included the duration of in-hospital CPR and initial cardiac rhythms. The rhythms included asystole and PEA and were obtained from an electrocardiography (ECG) monitor (on arrival at the ED).
Time to Epinephrine
Information on epinephrine administration was also obtained from the medical and EMS records. The route of the first epinephrine administration was given as intravenous or non-intravenous. Time to epinephrine was defined as the duration from collapse (no pulse, no vital signs, and/or unconsciousness) to the first dose of epinephrine. The time of collapse was decided according to EMS records, witness statements and/or medical records. As given in the exclusion criteria, children were excluded if the time of collapse could not be confirmed. Time to epinephrine was classified as early (<15 min), intermediate (15–30 min), or late (>30 min).
Study Protocol
Primary Outcomes—Utstein Style Reports for All Patients
All patients' outcomes were classified using Utstein style reports [any ROSC, sustained ROSC, survival to admission to intensive care unit (ICU), survival to discharge, good neurological outcomes] (34, 35). The “good neurological outcomes” in this study were considered as Pediatric Cerebral Performance Category Scales (PCPCS) = 1 or 2 on discharge from hospital (36, 37). Outcomes were classified by time to epinephrine.
Secondary Outcomes—Post-resuscitation Hemodynamics (in the First Hour After Achieving Sustained ROSC) in Patients who Survived to ICU Admission
The secondary outcomes were analyzed by time to first treatment with epinephrine.
Post-resuscitation Hemodynamics
Post-resuscitation hemodynamics were recorded in the first hour after achieving sustained ROSC (10, 11). The variables included oxygenation (hypoxia and non-hypoxia), heart rate (tachycardia, normal, bradycardia), heart rhythm (sinus, non-sinus), mean blood pressure (hypertension, normal, hypotension), consciousness level (Glasgow Coma Score, GCS>7, 4–7, = 3), body temperature (pyrexia and non-pyrexia), and urine output (>1, 1–0.5, <0.5 ml/kg/h). In addition, oxygenation was evaluated with ventilator support. The verbal response in patients who received endotracheal intubation was classified as a single score. Pyrexia was defined as over 38 degrees Celsius (°C). The post-resuscitation care protocols in ED or ICU adhered to the recommendations of the American Heart Association (AHA) guidelines during the study period. The protocols included systemic supports (respiratory, cardiovascular, neurological systems), continuous monitoring (blood pressure, cardiac rhythms, and oxygenation), end organ protection (brain and kidney), and aggressive fever control. Temperature was continuously measured. Temperatures of 38°C or more were aggressively treated in all pediatric patients after ROSC (38–40).
Data Analysis
SPSS software version 15.0 (SPSS Inc., Chicago, IL) was used to analyze the data in this study. Descriptive statistics for demographics, pre-/in-hospital resuscitation information, hemodynamics and primary/secondary outcomes are reported as the number, percentage and/or mean ± standard deviation (SD). The relationships between different times to epinephrine and post-resuscitation hemodynamics were analyzed with the chi square test. Multinomial logistic regression analysis was used to determine the effect of EE, taking LE as the reference group, for hemodynamics parameters, pre/in-hospital CPR information, body temperature, and etiology of arrest. Finally, the primary outcomes of patients were also analyzed by the chi square test by different times to epinephrine. p < 0.05 was considered statistically significant.
results
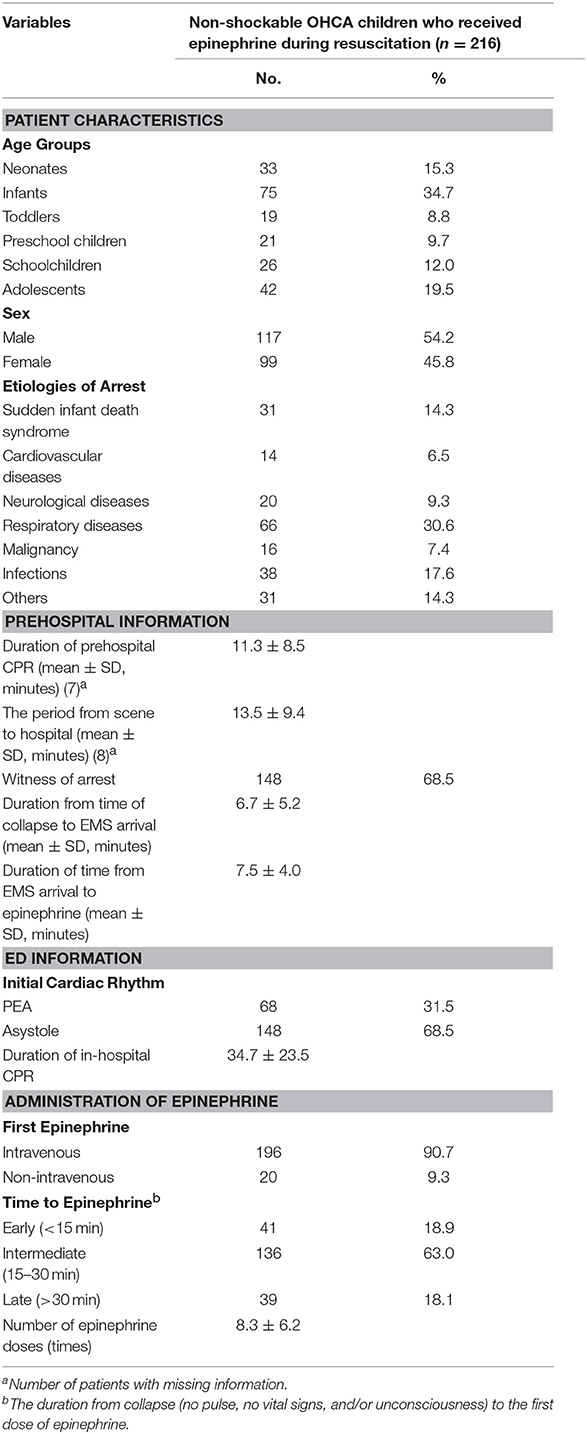
Demographics of Non-traumatic OHCA Children
The final population of this study was 216 children. Demographics and resuscitation information are shown in Table 1. Most patients were infants (n = 75, 34.7%), followed by adolescents (n = 42, 19.5%). The majority of patients were males (n = 117, 54.2%). The most common etiologies of arrest were respiratory diseases (n = 66, 30.6%) and infections (n = 38, 17.6%). Asystole was the most predominant non-shockable cardiac rhythm (n = 148, 68.5%). Finally, most children received the first dose of epinephrine in the intermediate time category (n = 136, 63.0%), followed by early (n = 41, 18.9%), and late (n = 39, 18.1%).
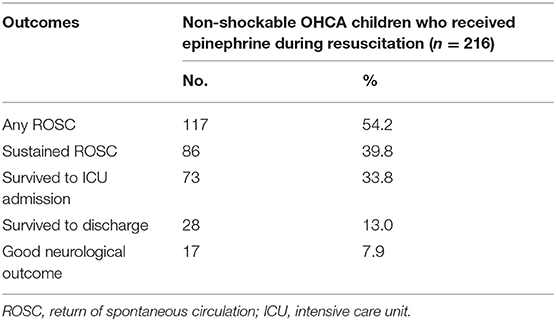
Primary Outcomes and Target Patient Identification
The primary outcomes are shown in Table 2. Among these children, 28 (13.0%) survived to discharge, and only 17 (7.9%) had good neurological outcomes. The number of patients who survived to ICU admission (target patients) was 73 (33.8%).
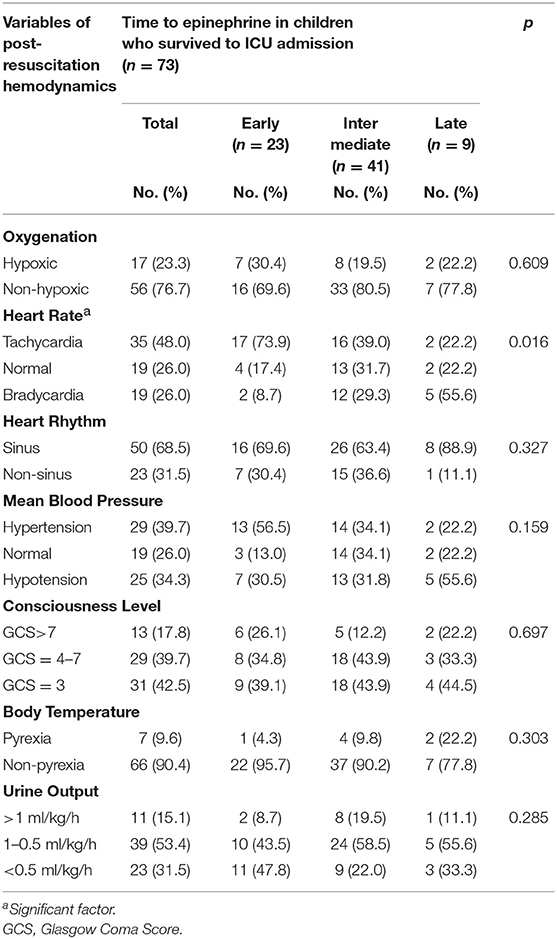
Post-resuscitation Hemodynamics in Target Patients
The post-resuscitation hemodynamics (in the first hour of the post-resuscitation period) of the 73 targeted children are shown in Table 3. During this period, all patients were supported by ventilators. However, 17 (23.3%) of them still suffered hypoxia. Tachycardia (48.0%), sinus rhythm (68.5%), and hypertension (39.7%) were the most common cardiac presentations.
Secondary Outcomes—EE Influence on Hemodynamics
Among the target patients, 23 received EE. EE was significantly related to more predominant tachycardia (73.9%) than ME and LE (p < 0.05). However, EE was not significantly related to oxygenation, heart rhythm, blood pressure, level of consciousness, body temperature, or urine output in the early post-resuscitation period (Table 3).
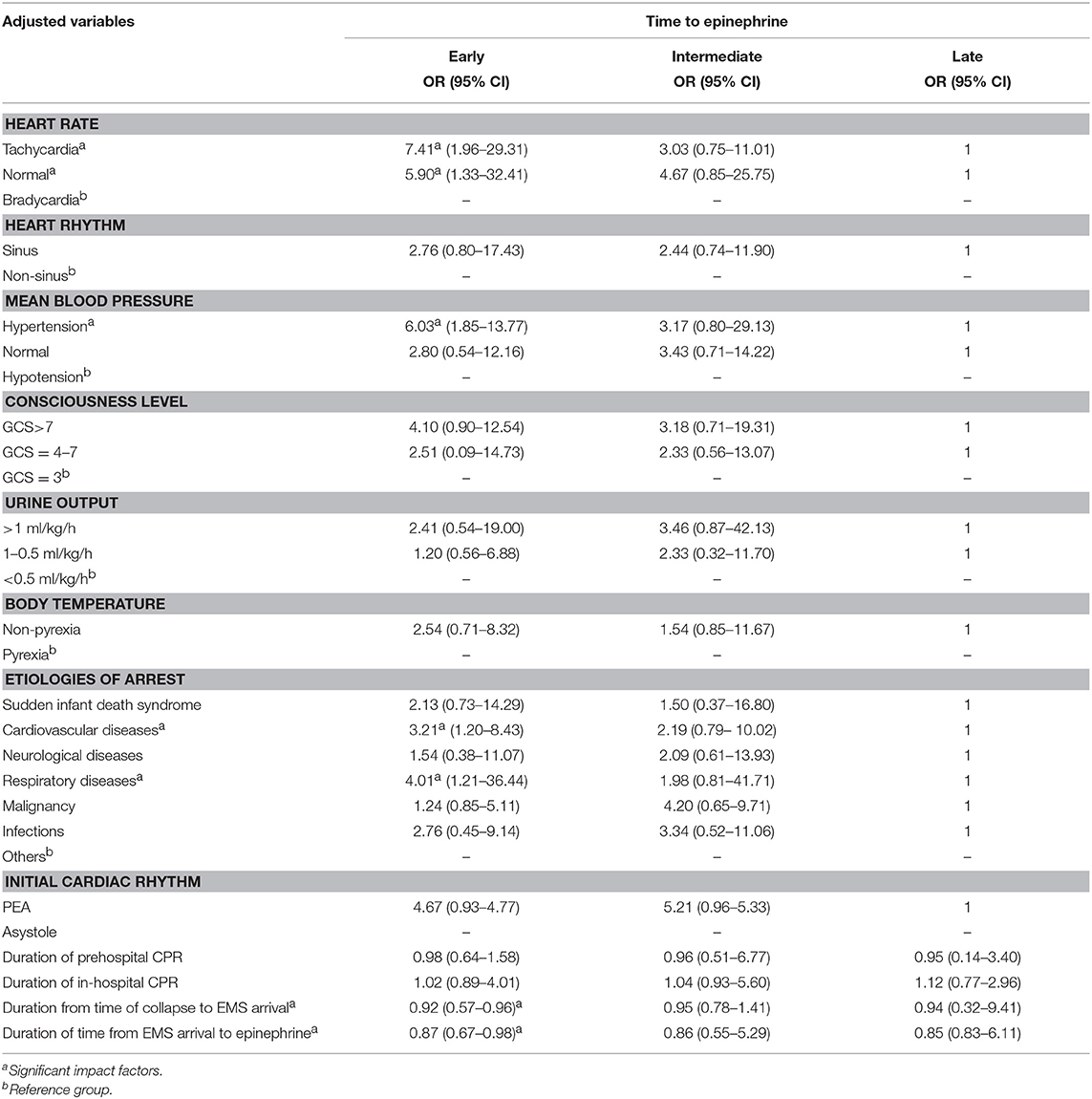
Most Powerful Effects of EE After Correction for Confounding Factors
After correction for the other confounding factors, multinomial logistic regression analysis demonstrated that EE was most closely related to tachycardia (OR: 7.41, 95% CI: 1.96–29.31), hypertension (OR: 6.03, 95% CI: 1.85–13.77), etiology of cardiovascular disease (OR: 3.21, 95% CI: 1.20–8.43), respiratory diseases (OR: 4.01, 95% CI: 1.21–36.44), duration from time of collapse to EMS arrival (OR: 0.92, 95% CI: 0.57–0.96), and duration of time from EMS arrival to epinephrine (OR: 0.87, 95%CI:0.67–0.98) (Table 4).
The Impact of EE on Primary Outcomes
The associations between the primary outcomes and different times to epinephrine are shown in Figure 1. EE was associated with a greater chance of achieving any ROSC, sustained ROSC, survival to ICU admission, survival to discharge and good neurological outcomes than ME and LE (all p < 0.05).
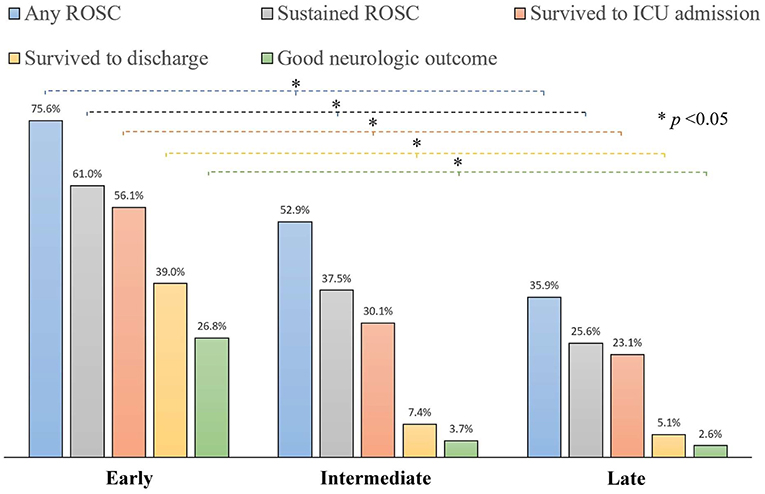
Figure 1. The associations between primary outcomes and different times to epinephrine in non-traumatic OHCA children (comparing EE, ME, and LE using the chi square test).
Discussion
Epinephrine is the first-line CPR medication and is only administered during the first medical contact (41). Thus, the “time to epinephrine” (from collapse to receiving the first dose of epinephrine) might differ significantly among OHCA patients. It is important to understand how patient outcome depends on the time to epinephrine. We suspect that EE might have more intense effects (more beneficial or harmful effects than ME or LE) on a well-established post-resuscitation hemodynamic status. However, this has never been demonstrated. In this study, we first analyzed the effects of EE on post-resuscitation hemodynamics in children with non-traumatic and non-shockable OHCA.
One important parameter influenced by EE is the post-resuscitation heart rate. Some studies have reported that the heart rate of OHCA patients was often increased and more variable during the ROSC period due to several factors, including hypoxia-related baroreceptor stimulation, ischemic/reperfusion response, inflammatory, and cytokine modulation and myocardial injuries (42–45). However, the association between EE and post-resuscitation tachycardia has not been well-addressed, especially in children with OHCA. Aside from other potential harmful effects, EE indeed triggered a greater heart rate in non-traumatic OHCA children.
The second key parameter triggered by EE was post-resuscitation hypertension. Blood pressure is directly associated with vasoconstriction (α-agonist effect) and cardiac output (β-agonist effect) (14, 46, 47). Therefore, we suspected that early administration might maximize the dual effects (α and β agonist effects) of epinephrine and then ROSC would be easier to establish. Increased blood pressure might not inevitably imply better cardiac output, as a higher blood pressure might just be the result of greater systemic vascular resistance (caused by epinephrine).
On the one hand, greater systemic vascular resistance might be detrimental to an end organ by limiting perfusion/cardiac output to that organ. On the other hand, it has been shown that EE provides benefit by increasing coronary artery perfusion pressure, and this might be associated with better outcomes (46, 48). Nevertheless, post-resuscitation oxygenation, rhythm, level of consciousness, body temperature, and urine output were not significantly associated with EE. This is compatible with the idea that EE might not directly improve end organ perfusion. However, more evidence is needed to prove this.
The most important finding was that survival rates and neurological outcomes were better in patients who received EE than in those who received ME or LE. This may be because EE rapidly triggers ROSC and thus immediately enhances blood flow to the brain.
In conclusion, EE not only helps to establish ROSC, but is also associated with cardiovascular effects in the early post-resuscitation period—inducing more tachycardia and hypertension, after correction for confounding factors. EE was associated with a higher survival rate and better neurological outcomes than ME and LE in children with non-traumatic OHCA.
Limitations
There were four major limitations in this study. The first major limitation and a possible source of bias lay in the precise definition of “collapse”—as this could imply anything between full arrest and a low flow state. The second limitation lay in the determination of the true time points of collapse. As the time of collapse was retrospectively obtained from the medical/EMS records, we suspect that several factors (including differences in recording time, different definitions of collapse, and subjective effects of the witness) might influence the risk of bias. The third limitation could be the classification of initial cardiac rhythm. The rhythm seen first by first responders may not be the initial rhythm which caused the arrest. In addition, the initial shockable rhythms (VT/VF) might change to non-shockable (PEA/asystole) before EMS arrived (or even in the ambulance). The final limitation was that the influence of advanced cardiac life support (ALS) was not considered in this study. Because epinephrine was only administered by medical or EMS personnel, EE also indicated early ALS (including early airway management).
Data Availability
The datasets for this manuscript are not publicly available because this is a medical chart review study. Requests to access the datasets should be directed to Yan-Ren Lin,aDYyMTMubGFjQGdtYWlsLmNvbQ==.
Ethics Statement
This study was carried out in accordance with the recommendations of STROBE statement. The protocol was approved by the institutional review board (IRB) of Changhua Christian Hospital. Since this is a retrospective chart-review study, and outputs were secondary deidentified data, informed consent were not needed under the IRB permission. Finally, the team members and data collector also followed the rules of the IRB.
(1) Full name of the ethics committee: Institutional review board (IRB) of Changhua Christian Hospital.
(2) Consent procedure used for human participants or for animal owners: retrospective chart-review review.
(3) Any additional considerations of the study in cases where vulnerable populations were involved, for example minors, persons with disabilities or endangered animal species: Although we focused on OHCA children; however, this study only retrospectively obtained information from chart review (output data were also secondary deidentified). No additional considerations for vulnerable population under IRB permission.
Author Contributions
W-LC, T-YC, C-JL, and Y-RL conceived the study. Y-RL and C-FC managed the data, including quality control. Y-RL, C-CH, and T-HL provided statistical advice on the study design and analyzed the data. C-JL, Y-RL, and C-CC chaired the data oversight committee. Y-RL and H-WH drafted the manuscript. H-YH and M-CY made a great contribution in 2nd and 3rd paper revisions. H-WH and W-LC assumed responsibility for the paper as a whole. All of the authors read and approved the final manuscript and contributed substantially to its revision.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Jayaram N, McNally B, Tang F, Chan PS. Survival after out-of-hospital cardiac arrest in children. J Am Heart Assoc. (2015) 4:e002122. doi: 10.1161/JAHA.115.002122
2. Munoz MG, Beyda DH. An ethical justification for termination of resuscitation protocols for pediatric patients. Pediatr Emerg Care. (2017) 33:505–15. doi: 10.1097/PEC.0000000000001191
3. Zhang X, Zhang W, Wang C, Tao W, Dou Q, Yang Y. Chest-compression-only versus conventional cardiopulmonary resuscitation by bystanders for children with out-of-hospital cardiac arrest: a systematic review and meta-analysis. Resuscitation. (2018) 134:81–90. doi: 10.1016/j.resuscitation.2018.10.032
4. Chen CY, Lin YR, Zhao LL, Wu YK, Chang YJ, Yang WC, et al. Epidemiology and outcome analysis of children with traumatic out-of-hospital cardiac arrest compared to nontraumatic cardiac arrest. Pediatr Surg Int. (2013) 29:471–7. doi: 10.1007/s00383-013-3302-z
5. Chia MY, Lu QS, Rahman NH, Doctor NE, Nishiuchi T, Leong BS, et al. Characteristics and outcomes of young adults who suffered an out-of-hospital cardiac arrest (OHCA). Resuscitation. (2017) 111:34–40. doi: 10.1016/j.resuscitation.2016.11.019
6. Forrest A, Butt WW, Namachivayam SP. Outcomes of children admitted to intensive care after out-of-hospital cardiac arrest in Victoria, Australia. Crit Care Resusc. (2017) 19:150–8.
7. Goto Y, Funada A, Nakatsu-Goto Y. Neurological outcomes in children dead on hospital arrival. Crit Care. (2015) 19:410. doi: 10.1186/s13054-015-1132-1
8. Goto Y, Funada A, Goto Y. Conventional versus chest-compression-only cardiopulmonary resuscitation by bystanders for children with out-of-hospital cardiac arrest. Resuscitation. (2018) 122:126–34. doi: 10.1016/j.resuscitation.2017.10.015
9. Riou M, Ball S, Whiteside A, Bray J, Perkins GD, Smith K, et al. 'We're going to do CPR': a linguistic study of the words used to initiate dispatcher-assisted CPR and their association with caller agreement. Resuscitation. (2018) 133:95–100. doi: 10.1016/j.resuscitation.2018.10.011
10. Lin YR, Li CJ, Wu TK, Chang YJ, Lai SC, Liu TA, et al. Post-resuscitative clinical features in the first hour after achieving sustained ROSC predict the duration of survival in children with non-traumatic out-of-hospital cardiac arrest. Resuscitation. (2010) 81:410–7. doi: 10.1016/j.resuscitation.2010.01.006
11. Lin YR, Wu HP, Chen WL, Wu KH, Teng TH, Yang MC, et al. Predictors of survival and neurologic outcomes in children with traumatic out-of-hospital cardiac arrest during the early postresuscitative period. J Trauma Acute Care Surg. (2013) 75:439–47. doi: 10.1097/TA.0b013e31829e2543
12. Lin YR, Wu HP, Huang CY, Chang YJ, Lin CY, Chou CC. Significant factors in predicting sustained ROSC in paediatric patients with traumatic out-of-hospital cardiac arrest admitted to the emergency department. Resuscitation. (2007) 74:83–9. doi: 10.1016/j.resuscitation.2006.11.022
13. Hansen M, Schmicker RH, Newgard CD, Grunau B, Scheuermeyer F, Cheskes S, et al. Time to epinephrine administration and survival from nonshockable out-of-hospital cardiac arrest among children and adults. Circulation. (2018) 137:2032–40. doi: 10.1161/CIRCULATIONAHA.117.033067
14. Kempton H, Vlok R, Thang C, Melhuish T, White L. Standard dose epinephrine versus placebo in out of hospital cardiac arrest: a systematic review and meta-analysis. Am J Emerg Med. (2019) 37:511–7. doi: 10.1016/j.ajem.2018.12.055
15. Shao H, Li CS. Epinephrine in out-of-hospital cardiac arrest: helpful or harmful? Chin Med J. (2017) 130:2112–6. doi: 10.4103/0366-6999.213429
16. Fitzgerald GA, Barnes P, Hamilton CA, Dollery CT. Circulating adrenaline and blood pressure: the metabolic effects and kinetics of infused adrenaline in man. Eur J Clin Invest. (1980) 10:401–6. doi: 10.1111/j.1365-2362.1980.tb00052.x
17. Manole MD, Kochanek PM, Bayir H, Alexander H, Dezfulian C, Fink EL, et al. Brain tissue oxygen monitoring identifies cortical hypoxia and thalamic hyperoxia after experimental cardiac arrest in rats. Pediatr Res. (2014) 75:295–301. doi: 10.1038/pr.2013.220
18. Nachar RA, Booth EA, Friedlich P, Borzage M, Soleymani S, Wider MD, et al. Dose-dependent hemodynamic and metabolic effects of vasoactive medications in normotensive, anesthetized neonatal piglets. Pediatr Res. (2011) 70:473–9. doi: 10.1203/PDR.0b013e31822e178e
19. Hardig BM, Gotberg M, Rundgren M, Gotberg M, Zughaft D, Kopotic R, et al. Physiologic effect of repeated adrenaline (epinephrine) doses during cardiopulmonary resuscitation in the cath lab setting: a randomised porcine study. Resuscitation. (2016) 101:77–83. doi: 10.1016/j.resuscitation.2016.01.032
20. Patanwala AE, Slack MK, Martin JR, Basken RL, Nolan PE. Effect of epinephrine on survival after cardiac arrest: a systematic review and meta-analysis. Minerva Anestesiol. (2014) 80:831–43.
21. Perkins GD, Ji C, Deakin CD, Quinn T, Nolan JP, Scomparin C, et al. A randomized trial of epinephrine in out-of-hospital cardiac arrest. N Engl J Med. (2018) 379:711–21. doi: 10.1056/NEJMoa1806842
22. Ristagno G, Tang W, Huang L, Fymat A, Chang YT, Sun S, et al. Epinephrine reduces cerebral perfusion during cardiopulmonary resuscitation. Crit Care Med. (2009) 37:1408–15. doi: 10.1097/CCM.0b013e31819cedc9
23. Sicherer SH, Simons FER, SECTION ON ALLERGY AND IMMUNOLOGY. Epinephrine for first-aid management of anaphylaxis. Pediatrics. (2017) 139:e20164006. doi: 10.1542/peds.2016-4006
24. Dumas F, Bougouin W, Geri G, Lamhaut L, Bougle A, Daviaud F, et al. Is epinephrine during cardiac arrest associated with worse outcomes in resuscitated patients? J Am Coll Cardiol. (2014) 64:2360–7. doi: 10.1016/j.jacc.2014.09.036
25. Donnino MW, Salciccioli JD, Howell MD, Cocchi MN, Giberson B, Berg K, et al. Time to administration of epinephrine and outcome after in-hospital cardiac arrest with non-shockable rhythms: retrospective analysis of large in-hospital data registry. BMJ. (2014) 348:g3028. doi: 10.1136/bmj.g3028
26. Ueta H, Tanaka H, Tanaka S, Sagisaka R, Takyu H. Quick epinephrine administration induces favorable neurological outcomes in out-of-hospital cardiac arrest patients. Am J Emerg Med. (2017) 35:676–80. doi: 10.1016/j.ajem.2016.12.066
27. Tomio J, Nakahara S, Takahashi H, Ichikawa M, Nishida M, Morimura N, et al. Effectiveness of prehospital epinephrine administration in improving long-term outcomes of witnessed out-of-hospital cardiac arrest patients with initial non-shockable rhythms. Prehosp Emerg Care. (2017) 21:432–41. doi: 10.1080/10903127.2016.1274347
28. Andersen LW, Berg KM, Saindon BZ, Massaro JM, Raymond TT, Berg RA, et al. Time to epinephrine and survival after pediatric in-hospital cardiac arrest. JAMA. (2015) 314:802–10. doi: 10.1001/jama.2015.9678
29. Fukuda T, Kondo Y, Hayashida K, Sekiguchi H, Kukita I. Time to epinephrine and survival after paediatric out-of-hospital cardiac arrest. Eur Heart J Cardiovasc Pharmacother. (2018) 4:144–51. doi: 10.1093/ehjcvp/pvx023
30. Hunt EA, Duval-Arnould JM, Bembea MM, Raymond T, Calhoun A, Atkins DL, et al. Association between time to defibrillation and survival in pediatric in-hospital cardiac arrest with a first documented shockable rhythm. JAMA Netw Open. (2018) 1:e182643. doi: 10.1001/jamanetworkopen.2018.2643
31. Fukuda T, Ohashi-Fukuda N, Matsubara T, Gunshin M, Kondo Y, Yahagi N. Effect of prehospital epinephrine on out-of-hospital cardiac arrest: a report from the national out-of-hospital cardiac arrest data registry in Japan, 2011-2012. Eur J Clin Pharmacol. (2016) 72:1255–64. doi: 10.1007/s00228-016-2093-2
32. Xue JK, Leng QY, Gao YZ, Chen SQ, Li ZP, Li HP, et al. Factors influencing outcomes after cardiopulmonary resuscitation in emergency department. World J Emerg Med. (2013) 4:183–9. doi: 10.5847/wjem.j.issn.1920-8642.2013.03.005
33. Ono Y, Hayakawa M, Wada T, Sawamura A, Gando S. Effects of prehospital epinephrine administration on neurological outcomes in patients with out-of-hospital cardiac arrest. J Intensive Care. (2015) 3:29. doi: 10.1186/s40560-015-0094-3
34. Jacobs I, Nadkarni V, Bahr J, Berg RA, Billi JE, Bossaert L, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries. A statement for healthcare professionals from a task force of the international liaison committee on resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, Inter American Heart Foundation, Resuscitation Council of Southern Africa). Resuscitation. (2004) 63:233–49. doi: 10.1016/j.resuscitation.2004.09.008
35. Perkins GD, Jacobs IG, Nadkarni VM, Berg RA, Bhanji F, Biarent D, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update of the Utstein Resuscitation Registry Templates for Out-of-Hospital Cardiac Arrest: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian and New Zealand Council on Resuscitation, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern Africa, Resuscitation Council of Asia); and the American Heart Association Emergency Cardiovascular Care Committee and the Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation. Circulation. (2015) 132:1286–300. doi: 10.1161/CIR.0000000000000144
36. de Caen AR, Kleinman ME, Chameides L, Atkins DL, Berg RA, Berg MD, et al. Part 10: Paediatric basic and advanced life support: 2010 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Resuscitation. (2010) 81(Suppl. 1):e213–59. doi: 10.1016/j.resuscitation.2010.08.028
37. Michiels E, Quan L, Dumas F, Rea T. Long-term neurologic outcomes following paediatric out-of-hospital cardiac arrest. Resuscitation. (2016) 102:122–6. doi: 10.1016/j.resuscitation.2016.01.010
38. Marino BS, Tabbutt S, MacLaren G, Hazinski MF, Adatia I, Atkins DL, et al. Cardiopulmonary resuscitation in infants and children with cardiac disease: a scientific statement from the American Heart Association. Circulation. (2018) 137:e691–782. doi: 10.1161/CIR.0000000000000524
39. Duff JP, Topjian A, Berg MD, Chan M, Haskell SE, Joyner BL Jr, et al. 2018 American Heart Association Focused Update on Pediatric Advanced Life Support: an update to the American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. (2018) 138:e731–9. doi: 10.1161/CIR.0000000000000612
40. de Caen AR, Berg MD, Chameides L, Gooden CK, Hickey RW, Scott HF, et al. Part 12: pediatric advanced life support: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. (2015) 132:S526–42. doi: 10.1161/CIR.0000000000000266
41. Brasted ID, Dailey MW. Basic life support access to injectable epinephrine across the United States. Prehosp Emerg Care. (2017) 21:442–7. doi: 10.1080/10903127.2017.1294224
42. Fletcher EC. Effect of episodic hypoxia on sympathetic activity and blood pressure. Respir Physiol. (2000) 119:189–97. doi: 10.1016/S0034-5687(99)00114-0
43. Iordanova B, Li L, Clark RSB, Manole MD. Alterations in cerebral blood flow after resuscitation from cardiac arrest. Front Pediatr. (2017) 5:174. doi: 10.3389/fped.2017.00174
44. Randhawa VK, Grunau BE, Debicki DB, Zhou J, Hegazy AF, McPherson T, et al. Cardiac intensive care unit management of patients after cardiac arrest: now the real work begins. Can J Cardiol. (2018) 34:156–67. doi: 10.1016/j.cjca.2017.11.013
45. Hassager C, Nagao K, Hildick-Smith D. Out-of-hospital cardiac arrest: in-hospital intervention strategies. Lancet. (2018) 391:989–98. doi: 10.1016/S0140-6736(18)30315-5
46. Turkseven CH, Pekoglu E, Buyukakilli B. Hemodynamic effects of epinephrine in rats: evaluation by impedance cardiography. Bratisl Lek Listy. (2017) 118:613–7. doi: 10.4149/BLL_2017_118
47. Maas JJ, Pinsky MR, de Wilde RB, de Jonge E, Jansen JR. Cardiac output response to norepinephrine in postoperative cardiac surgery patients: interpretation with venous return and cardiac function curves. Crit Care Med. (2013) 41:143–50. doi: 10.1097/CCM.0b013e318265ea64
Keywords: epinephrine, children, OHCA, survival, non-shockable, time, early, outcome
Citation: Lin Y-R, Li C-J, Huang C-C, Lee T-H, Chen T-Y, Yang M-C, Chou C-C, Chang C-F, Huang H-W, Hsu H-Y and Chen W-L (2019) Early Epinephrine Improves the Stabilization of Initial Post-resuscitation Hemodynamics in Children With Non-shockable Out-of-Hospital Cardiac Arrest. Front. Pediatr. 7:220. doi: 10.3389/fped.2019.00220
Received: 27 February 2019; Accepted: 15 May 2019;
Published: 06 June 2019.
Edited by:
Aristomenis K. Exadaktylos, Bern University Hospital, SwitzerlandReviewed by:
Vijay Srinivasan, Children's Hospital of Philadelphia, United StatesRobert Kelly, Children's Hospital of Orange County, United States
Copyright © 2019 Lin, Li, Huang, Lee, Chen, Yang, Chou, Chang, Huang, Hsu and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hsi-Wen Huang, Njg5NTZAY2NoLm9yZy50dw==; Hsiu-Ying Hsu, MTQ2NTFAY2NoLm9yZy50dw==; Wen-Liang Chen, d2VudXJlYUB5YWhvby5jb20udHc=
 Yan-Ren Lin1,2,3
Yan-Ren Lin1,2,3 Wen-Liang Chen
Wen-Liang Chen