- Department of Surgical Sciences, Dentistry, Gynecology and Pediatrics, University of Verona, Verona, Italy
Asthma is the most common chronic respiratory disease in children characterized by airways inflammation, bronchial hyperresponsiveness, recurrent reversible airways obstruction, and respiratory symptoms. The diagnosis of the disease is based on clinical history, airways obstruction at spirometry, and bronchial reversibility. Asthma treatment is aimed to disease control, through the use of controller treatment and monitoring lung function. However, lung function and symptoms not always reflect the underlying airways inflammation and response to the therapy. Objective parameters of asthma inflammation could be important for the clinician in the management of patients with asthma. In the last years, some studies were focused on biomarkers to identify phenotype, inflammation, and pathobiological pathways to help the clinician in the diagnosis and in personalizing the management. Accordingly, clinically feasible tests are represented by the collection of exhaled breath condensate (EBC) and measurement of exhaled nitric oxide (FeNO). Other—methods such as the evaluation of volatile organic compound (VOCs), that reflect airways inflammation and treatment efficacy, are currently used for research purposes For some of these methods, The lack of standardization in pre-collection, collection, post-collection of samples, and interpretation of the results may a problem in clinical practice. Improved these limitations, several biomarkers will be useful to distinguish patients with a different disease condition to personalize the treatment.
Introduction
Asthma is a chronic respiratory disease characterized by inflammation of the airways, bronchial hyperresponsiveness, recurrent reversible airway obstruction, and respiratory symptoms (1). Asthma is the most common chronic respiratory disease in childhood with an incidence between 1 and 18% in people from different countries.
The diagnosis of asthma is based on anamnestic data, clinical evaluation, limitation of the airflow, and bronchial reactivity (1). The goal of asthma treatment is the control of respiratory symptoms with controller daily drugs, reduction of rescue medications needed to maintain a regular daily activity and reaching a normal lung function (1). Though airways inflammation is a pivotal characteristic of the disease, it is not directly related to lung function test or symptoms (2) and with the real response to the therapy (3).
Therefore, objective parameters of airway inflammation should be considered relevant for the treatment choice in asthmatic patients.
The assessment of biomarkers in the exhaled breath of patients with asthma and other lung diseases is a very attractive approach to monitor airways inflammation. Biomarkers are objectively measurable indicators of the biological and pathological processes as well as of the pharmacological responses to the therapeutic intervention (4).
An ideal biomarker should be easy to collect and measure, inexpensive, noninvasive, and feasible in children capable to contribute to the phenotyping of the disease and to the assessment of treatment response (4, 5).
In order to have a clinically useful tool, there are important issues regarding sensibility, reproducibility, and variability of the methods, that need to be evaluated before moving from bench to bedside. In the next future, a number of recently proposed methods are expected to be clinically useful to predict the progression of the disease, to the phenotyping and endotyping of the disease in order to move toward a personalized treatment in asthma (Figure 1).
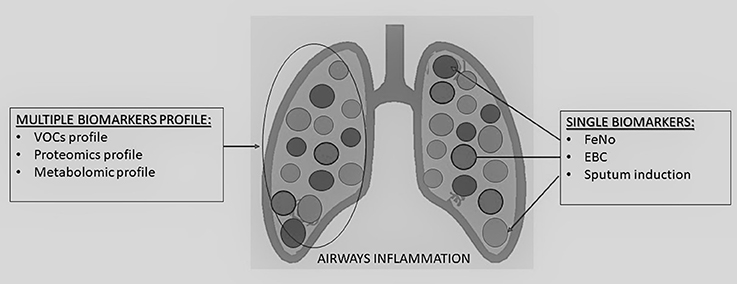
Figure 1. Summary of single and multiple biomarkers detection methods to assess airways inflammation in children.
Bronchoscopy with bronchoalveolar lavage (BAL) and endobronchial biopsy are considered the gold standards for assessing airway inflammation and remodeling in asthma but, being invasive methods, they have a limited use in the clinical setting, in particular in pediatric care (2).
In recent years, therefore, researchers have focused their studies to define surrogate biomarkers to be proposed in the assessment of airway inflammation in asthmatic children and are shortly revised in the following sections (4–6) (Figure 1).
Induced Sputum
The method of induced sputum is a relatively noninvasive diagnostic procedure able to harvest cells and mediators from the lower airway (2) which, however, requires a level of expertise in the collection in order to obtain adequate samples and reliable results. Sputum can be induced in children older than 6 years after inhalation of nebulized hypertonic saline solution at increasing concentration (7, 8).
The procedure to collect sputum is standardized by European Respiratory Society Task Force and is applicable to children older than 8 years (9, 10).
However, the practical use of this method is limited due to technical issues which can make the feasibility at clinical setting difficult to perform for regular assessment of airways inflammation in children (11, 12). In particular, hypertonic saline inhalation may cause bronchoconstriction, especially in asthmatic children, for whom pre-medication with β2-agonist may be necessary. Furthermore, the post-collection analysis needs skilled laboratory personnel for mediator assay and cell specimens to be transferred onto slides and properly stained. Trained physicians are also needed in order to have a correct reading of the results from the specimens.
Several studies demonstrated a strong correlation between cellular elements of BAL and cells collected from in the airways through the induced sputum method.
The dominant cell in sputum from normal children is the macrophages, and the normal ratio for eosinophils in sputum from children is 2.5% (7).
Different inflammatory patterns are being identified from sputum of asthmatic children and adults: eosinophilic, neutrophilic, mixed, and paucigranulocytic types (13).
Sputum eosinophilia is a marker of severity of allergic inflammation in asthma and is characterized by elevated numbers of eosinophils, and eosinophil cationic protein concentration, as well as increased nitric oxide and hydrogen peroxide levels in exhaled breath. The patients with an eosinophilic pattern are expected to have a better response to corticosteroids therapy (14).
Also, children with stable asthma show increased number of eosinophils and bronchial epithelial cells in their sputum (15, 16). During asthma exacerbation, eosinophils and mast cells are more represented in the samples obtained from the airways through the method of induced sputum and eosinophil cationic protein concentrations are higher in the fluid phase of the samples. Some patients have sputum neutrophilia with improved levels of interleukin 8 (17). On the other hand, children with asymptomatic airway hyperresponsiveness are expected to have normal cell counts, whereas patients with cystic fibrosis have sputum neutrophilia (15, 18).
Exhaled Breath Condensate
Exhaled breath condensate (EBC) is a noninvasive method aimed to evaluate volatile markers and inflammatory mediators that may contribute to evaluate asthma pathophysiology.
EBC collects particles from airway lining fluid by the condensation of warm humid breath onto a cold surface in a condensing device.
EBC collection, as described in ATS/ERS guidelines, requires a refrigerated device (19) and patient are requested to breath at tidal volume for 10–15 min. During this time the airways lining fluid undergoes an aerosolization process and the exhaled fraction is condensed in a cooling device (0 to −20°C) (20).
The most frequently evaluated parameters in EBC are pH, exhaled markers of oxidative stress and inflammation.
EBC is composed of water vapor, unstable volatiles such as CO2 and H2O2, inorganic (O2, N2), and organic (CO2) particles, exogenous, and endogenous organic compounds, protein, and cytokines (21). In the respiratory tract, H2O2 may be released from inflamed cells—including neutrophils, macrophages, eosinophils, and epithelial cells. Nitrogen redox forms such as nitrite (NO2 –) and nitrate (NO3 –) are present in the epithelial lining fluid of the human respiratory tract.
High concentrations of NO2 and NO2+NO3 were showed in patients with asthma, CF and bronchiectasis compared with healthy controls (21).
The pH of EBC is a non-specific marker of airway disease being a median normal pH value of 8.0 in children from 0 to 20 years (22). Some studies showed a lower pH in children with stable asthma than healthy controls and a lower pH value in children with severe than mild asthma (23, 24). In addition, asthmatic patients not adequately treated with ICS have been demonstrated to have a lower pH than those properly treated. Patients with acute exacerbation had a higher pH value after the treatment with budesonide (23, 24).
At present, no association has been reported between asthma symptoms, lung function, FeNO, and airway hyperresponsiveness (25, 26).
Biomarkers related to oxidative stress like H2O2, 8-isoprostane, asymmetric dimethylarginine (ADMA), aldehydes, and nitrite/nitrate are important to be evaluated in EBC in a number of airway diseases, including asthma.
Asymmetric dimethylarginine (ADMA) is an EBC marker of oxidative stress which can be assessed by the UPLC-MS/MS technique. It is an analog of L-arginine that reduces the synthesis of NO and increases superoxide from inhibition of NOS. A previous study showed that asthmatic children had higher values of ADMA than healthy ones with no difference with ICS treatment (27).
The oxidation of the phospholipid membrane and polyunsaturated fatty acid produces aldehydes and lipid hydroperoxides. One study showed high levels of glutathione in the EBC of asthmatic children with exacerbation and after 5 days of prednisolone therapy, the malondialdehyde level dropped, while glutathione rose (28). Malondialdehyde levels also correlate with air pollution, lung function and inflammatory markers. These results suggest that during exacerbations there is an imbalance between oxidative and antioxidant agents in the airways.
H2O2 is released from cells in the airways as superoxide anions, an unstable and reactive particle. In the respiratory system, H2O2 can be released from both inflammatory cells—including neutrophils, macrophages, eosinophils—and epithelial cells. In non-asthmatic, non-smoking children, the normal value of this molecule is 0.09 μmol (19). H2O2 was higher in asthmatic children during exacerbations and decreased after ICS treatment, supporting the hypothesis that H2O2 is a marker of airways inflammation (29, 30). However, other studies failed to demonstrate its ability to predict exacerbations (31, 32).
8-isoprostane, a suitable marker of oxidative stress, is a product of arachidonic acid (33). Children and adults with severe asthma or asthma exacerbation have high levels of this 8-isoprostane (34). The concentrations of 8-isoprostane failed to show any correlation with lung function, FeNO, ICS or leukotriene receptor antagonist therapy (35, 36).
Eicosanoids are another group of markers derived from arachidonic acid that play a role in asthmatic inflammation. The presence of these markers in EBC is confirmed by specific enzyme immunoassay and radioimmunoassays (37).
Asthmatic children have high levels of leukotriene B4 (LTB4), cysteinyl leukotrienes (LTC4, LTD4, and LTE4) in EBC (36, 37). The role of cysteinyl leukotrienes (CysLT) in response to ICS therapy is under debate (38–40). Some authors showed a significant reduction of CysLT after a course of oral corticosteroids and after 6 months of ICS therapy, whereas others did not confirm this result. A significant reduction of CysLTs has been reported after montelukast therapy (41).
Several other markers of inflammation and oxidative stress, such as cytokines and adenosine, have been investigated. Asthmatic children showed high Th2 cytokines and low Th1 cytokines in EBC (42, 43). Moreover, children with asthma had a high IL-4/INFγ ratio related to Th2 inflammation (43). IL-4 was high in asthmatic and atopic children as a predictor of asthma condition, whereas IL-5 could predict exacerbations (32).
Fractional Exhaled Nitric Oxide (FeNO)
Nitric oxide in airways is mainly produced by two enzymes: constitutive nitric oxide synthase (cNOS), that produces low quantities of NO, and epithelial inducible NOS (iNOS) that is induced by various inflammatory cytokines (44). FeNO is a marker of eosinophilic airway inflammation, able to evaluate the level of inflammation and the response of anti-inflammatory therapy (45).
FeNO is a noninvasive, repeatable and reproducible method (46) applicable in the pediatric practice. The gold standard technique for cooperative children is the single breath on-line method (47) but also other techniques have been proposed for uncooperative children or in sedated infants (47). Nevertheless, at present, no clear evidence is available regarding the potential clinical application of FeNO measurements in uncooperative children. In this age group, the method deserves additional efforts to standardization because it its potential application to predict asthma (33).
FeNO levels can be influenced by different factors such as patient's age, height, gender, and race, nasal contamination, exhalation flow ambient and air pollution (48). The execution of spirometry or exercise before the measurement, diet or exposure to smoke also need to be considered (48).
The standardization of techniques permits to collect comparable data from different centers in healthy children and subjects with diseases. For this purpose, the first document on FeNO evaluation in children was published in 2002 (47), subsequently revised by ATS/ERS in 2005 (48).
Several studies demonstrated that FeNO correlates with airway hyperresponsiveness, IgE serum levels, bronchodilator response, skin prick tests, asthma symptoms, and lung function (49, 50).
Airway inflammation in allergic asthma results from the activation of Th2-mediated pro-inflammatory cytokine mechanism involving IL-4, IL-5, and IL-13. This mechanism causes the expression of epithelial inducible NO synthase up-regulated via STAT-6, a process which is corticosteroid sensitive (51, 52).
Furthermore, other studies showed that FeNO levels are correlated with serum eosinophilic cation protein, eosinophils in induced sputum, blood eosinophilia, eosinophil infiltration of the airways, and IgE levels in atopic patients (52). High FeNO values characterize Th2-mediated airway inflammation, eosinophilia, and responsiveness to ICS (52).
FeNO is helpful during evaluation of the patients characterizing asthma of the eosinophilic phenotype and predicting asthma exacerbation. In children less than 5-year-old with recurrent coughing and wheezing, increased FeNO levels can predict physician diagnosed asthma at school age (53). Furthermore, increased FeNO levels at the age of 4 years, predict higher risk for wheezing, asthma and need of ICS by school age (54).
The ATS guidelines recommend the use of FeNO for monitoring airway inflammation and for addressing the choice of anti-inflammatory treatment (52, 55, 56). It has been extensively proved a rapid decrease of FeNO values when ICS treatment is started, with a dose-dependent mechanism and a sudden rise when ICS therapy is withdrawn (57). This trend may be helpful in monitoring patient adherence to the therapy (46).
High FeNO values are not always linked to eosinophilic asthma but also to allergic rhinitis, eosinophilic bronchitis and allergen or viral exposure and a correct interpretation is stressed in the ATS/ERS document (55).
In patient treated with omalizumab, FeNO values, blood eosinophils and BMI can predict the response to the therapy (58).
Authors, for a long time, have been very cautious to support the use of FeNO as coadjutant to standard symptom-based management (59, 60).
However, in recent Cochrane review it has been showed that FeNO guided treatment in asthmatic children was associated with a significant reduction in exacerbation as compared with guideline-based treatment (61). On these bases, the most recent GINA document in 2018 included FeNO guided treatment as a proposed for tailoring treatment to be considered in children (1).
Therefore, FeNO can be regarded a useful method to categorize patients with eosinophilic and Th2-mediated asthma evaluating the response to ICS therapy, predicting exacerbations and the compliance to the therapy.
Exhaled Breath Volatile Organic Compounds (VOCs)
Exhaled breath volatile organic compounds (VOCs) are analyzed by breathomics science and they represent a noninvasive tool to evaluate the lung inflammation. VOCs have a metabolic origin from larger molecules. Airway VOCs originate not only from the upper and lower airways but also from a capillary bed near the alveoli (62). Their concentration in exhaled breath is influenced by blood gas coefficient, cardiac output and alveolar minute volume.
The methodological approach to collect VOCs from exhaled breath requires attention to exclude organic compounds from the ambient air, type of sampling (total vs. alveolar breath), type of collecting materials and other confounding factors (62).
In particular, the collection of airway VOCs needs an inhalation filter to exclude ambient VOCs. The patient is asked to breath into a system which can collect online samples directly via inert tubes into an analyzer or off-line by collecting exhaled air into bags, tubes or syringes. These devices are made of inert materials such as Tedlar bags (63).
Gas chromatography-mass spectrometry (GC-MS) and flame ionization detection (GC-FID) are the most widely used techniques to analyze the samples after collection. These methods can differentiate and quantify VOCs at low concentrations, but they require both qualified technicians and expensive technology (33).
A new non-selective approach to analyze VOCs in exhaled breath is metabolomic profiling that identify and quantify all metabolites in a biological sample without a priori hypothesis.
Metabolomic profiles describe the interaction among environmental exposure, medication, nutrition, and toxic substances, genetic expression and microorganisms (33, 62). This method is an interesting approach to patient characterization and personalized medication (33). This approach simultaneously evaluates many metabolites in a sample and generates a profile capable of discriminating between different groups of individuals characterizing the biochemical processes underway in each biological system.
More recently sensor-based device such as the electronic nose, colorimetric sensor array, and gold nanoparticle sensors have been proposed. They adopt specific sensors with optical, chemical or electronic properties that analyze VOCs in the EB (62). Recently, some studies have demonstrated the clinical application of these instruments in respiratory disease (64, 65). VOCs in the EB discriminate between asthma and healthy and between atopic and non-atopic children (64, 65). VOCs profile in exhaled breath was able to discriminate healthy, transient wheezing and asthmatic children starting from the age of 2-3-year-old (66). In the pediatric field, VOCs can also predict asthma exacerbations (67, 68).
Nevertheless, further studies are necessary to evaluate the clinical utility of VOCs in evaluating asthma severity and monitoring asthma symptoms and response to ICS therapy.
Conclusions
Noninvasive techniques to collect and analyze airways inflammatory biomarkers are helpful in evaluating the airway pathophysiology of asthmatic children.
In clinical practice, FeNO evaluation has been suggested as the only valid and non-invasive technique to test for underlined eosinophilic inflammation, but it would need to be adopted in combination with other useful markers.
The standardization of the new techniques to collect biomarkers in EB and EBC remains problematic. Low reproducibility of exhaled biomarkers and the lack of standardization of the methods of pre-collection, collection, post-collection of the samples, along with the correct interpretation of the results, represent critical issues in clinical practice.
The identification and utilization of ideal and defined biomarkers in asthmatic children remains debated. The reasons for this are the biological aspects of each prospective biomarker, the disease pathobiology, and methods and invasiveness of sample collection. Therefore, the development of novel biomarker with more sensitivity and specificity may lead to prompt diagnosis of severe asthma in future.
Author Contributions
MZ, MP, and LT: drafting of the manuscript; GP, MZ, and LT: critical revision.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention,. Available online at: www.ginasthma.org (2018).
2. Vijverberg SJ, Hilvering B, Raaijmakers JA, Lammers JW, Maitland-van der Zee AH, Koenderman L. Clinical utility of asthma biomarkers: from bench to bedside. Biologics.(2013) 7:199–210. doi: 10.2147/BTT.S29976
3. Murugan A, Prys-Picard C, Calhoun WJ. Biomarkers in asthma. Curr Opin Pulm Med. (2009) 15:12–8. doi: 10.1097/MCP.0b013e32831de235
4. Kharitonov SA, Barnes PJ. Exhaled markers of inflammation. Curr Opin Allergy Clin Immunol. (2001) 1:217–24. doi: 10.1097/00130832-200106000-00004
5. Barnes PJ, Chowdhury B, Kharitonov SA, Magnussen H, Page CP, Postma D. Pulmonary biomarkers in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. (2006) 174:6–14. doi: 10.1164/rccm.200510-1659PP
6. Moore WC, Meyers DA, Wenzel SE, Teague WG, Li H, Li X, et al. Identification of asthma phenotypes using cluster analysis in the Severe Asthma Research Program. Am J Respir Crit Care Med. (2010) 181:315–23 doi: 10.1164/rccm.200906-0896OC
7. Gibson PG, Henry RL, Thomas P. Noninvasive assessment of airway inflammation in children: induced sputum, exhaled nitric oxide, and breath condensate. Eur Respir J. (2000) 16:1008–15.
8. Deykin A, Massaro AF, Drazen JM, Israel E. Exhaled nitric oxide as a diagnostic test for asthma: online versus offline techniques and effect of flow rate. Am J Respir Crit Care Med. (2002) 165:1597–601. doi: 10.1164/rccm.2201081
9. Gibson PG, Grootendor DC, Henry RL, Pin I, Rytila PH, Wark P, et al. Sputum induction in children. Eur Respir J Suppl. (2002) 37:44s−6s. doi: 10.1183/09031936.02.00004402
10. Robroeks CM, van Berkel JJ, Dallinga JW, Jobsis Q, Zimmermann LJ, Hendriks HJ, et al. Metabolomics of volatile organic compounds in cystic fibrosis patients and controls. Pediatr Res. (2010) 68:75–80. doi: 10.1203/PDR.0b013e3181df4ea0
11. Wilson NM, Bridge P, Spanevello A, Silverman M. Induced sputum in children: feasibility, repeatability, and relation of findings to asthma severity. Thorax (2000) 55:768–74. doi: 10.1136/thorax.55.9.768
12. Fens N, Zwinderman AH, van der Schee MP, de Nijs SB, Dijkers E, Roldaan AC, et al. Exhaled breath profiling enables discrimination of chronic obstructive pulmonary disease and asthma. Am J Respir Crit Care Med. (2009) 180:1076–82. doi: 10.1164/rccm.200906-0939OC
13. Simpson JL, Scott R, Boyle MJ, Gibson PG. Inflammatory subtypes in asthma: assessment and identification using induced sputum. Respirology (2006) 11:54–61. doi: 10.1111/j.1440-1843.2006.00784.x
14. Haldar P, Pavord ID, Shaw DE, Berry MA, Thomas M, Brightling CE, et al. Cluster analysis and clinical asthma phenotypes. Am J Respir Crit Care Med. (2008) 178:218–24. doi: 10.1164/rccm.200711-1754OC
15. Cai Y, Carty K, Henry RL, Gibson PG. Persistence of sputum eosinophilia in children with controlled asthma when compared with healthy children. Eur Respir J. (1998) 11:848–53. doi: 10.1183/09031936.98.11040848
16. Piacentini GL, Vicentini L, Mazzi P, Chilosi M, Martinati L, Boner AL. Mite-antigen avoidance can reduce bronchial epithelial shedding in allergic asthmatic children. Clin Exp Allergy (1998) 28:561–7. doi: 10.1046/j.1365-2222.1998.00260.x
17. Norzila MZ, Fakes K, Henry RL, Simpson J, Gibson PG. Interleukin-8 secretion and neutrophil recruitment accompanies induced sputum eosinophil activation in children with acute asthma. Am J Respir Crit Care Med. (2000) 161(3 Pt 1):769–74. doi: 10.1164/ajrccm.161.3.9809071
18. Pin I, Radford S, Kolendowicz R, Jennings B, Denburg JA, Hargreave FE, et al. Airway inflammation in symptomatic and asymptomatic children with methacholine hyperresponsiveness. Eur Respir J. (1993) 6:1249–56.ho
19. Horvath I, Hunt J, Barnes PJ, Alving K, Antczak A, Baraldi E, et al. Exhaled breath condensate: methodological recommendations and unresolved questions. Eur Respir J. (2005) 26:523–48. doi: 10.1183/09031936.05.00029705
20. Baraldi E, Carraro S. Exhaled NO and breath condensate. Paediatr Respir Rev. (2006) 7 (Suppl. 1):S20–2. doi: 10.1016/j.prrv.2006.04.017
21. Dent AG, Sutedja TG, Zimmerman PV. Exhaled breath analysis for lung cancer. J Thorac Dis. (2013) 5 (Suppl. 5):S540–50. doi: 10.3978/j.issn.2072-1439.2013.08.44
22. Paget-Brown AO, Ngamtrakulpanit L, Smith A, Bunyan D, Hom S, Nguyen A, et al. Normative data for pH of exhaled breath condensate. Chest (2006) 129:426–30. doi: 10.1378/chest.129.2.426
23. Carraro S, Folesani G, Corradi M, Zanconato S, Gaston B, Baraldi E. Acid-base equilibrium in exhaled breath condensate of allergic asthmatic children. Allergy (2005) 60:476–81. doi: 10.1111/j.1398-9995.2005.00718.x
24. Brunetti L, Francavilla R, Tesse R, Fiermonte P, Fiore FP, Lore M, et al. Exhaled breath condensate cytokines and pH in pediatric asthma and atopic dermatitis. Allergy Asthma Proc. (2008) 29:461–7. doi: 10.2500/aap.2008.29.3152
25. Rosias PP, Dompeling E, Dentener MA, Pennings HJ, Hendriks HJ, Van Iersel MP, et al. Childhood asthma: exhaled markers of airway inflammation, asthma control score, and lung function tests. Pediatr Pulmonol. (2004) 38:107–14 doi: 10.1002/ppul.20056
26. Ratnawati Morton J, Henry RL, Thomas PS. Exhaled breath condensate nitrite/nitrate and pH in relation to pediatric asthma control and exhaled nitric oxide. Pediatr Pulmonol. (2006) 41:929–36. doi: 10.1002/ppul.20469
27. Carraro S, Giordano G, Piacentini G, Kantar A, Moser S, Cesca L, et al. Asymmetric dimethylarginine in exhaled breath condensate and serum of children with asthma. Chest (2013) 144:405–10 doi: 10.1378/chest.12-2379
28. Corradi M, Folesani G,reoli R, Manini P, Bodini A, Piacentini G, et al. Aldehydes and glutathione in exhaled breath condensate of children with asthma exacerbation. Am J Respir Crit Care Med. (2003) 167:395–9. doi: 10.1164/rccm.200206-507OC
29. Jobsis Q, Raatgeep HC, Hermans PW, de Jongste JC. Hydrogen peroxide in exhaled air is increased in stable asthmatic children. Eur Respir J. (1997) 10:519–21.
30. Caffarelli C, Calcinai E, Rinaldi L, Povesi Dascola C, Terracciano L, Corradi M. Hydrogen peroxide in exhaled breath condensate in asthmatic children during acute exacerbation and after treatment. Respiration (2012) 84:291–8. doi: 10.1159/000341969
31. Trischler J, Merkel N, Konitzer S, Muller CM, Unverzagt S, Lex C. Fractionated breath condensate sampling: H(2)O(2) concentrations of the alveolar fraction may be related to asthma control in children. Respir Res. (2012) 13:14. doi: 10.1186/1465-9921-13-14
32. Robroeks CM, van Vliet D, Jobsis Q, Braekers R, Rijkers GT, Wodzig WK, et al. Prediction of asthma exacerbations in children: results of a one-year prospective study. Clin Exp Allergy (2012) 42:792–8. doi: 10.1111/j.1365-2222.2012.03992.x
33. Moschino L, Zanconato S, Bozzetto S, Baraldi E, Carraro S. Childhood asthma biomarkers: present knowledge and future steps. Paediatr Respir Rev. (2015) 16:205–12. doi: 10.1016/j.prrv.2015.05.001
34. Baraldi E, Carraro S, Alinovi R, Pesci A, Ghiro L, Bodini A, et al. Cysteinyl leukotrienes and 8-isoprostane in exhaled breath condensate of children with asthma exacerbations. Thorax (2003) 58:505–9. doi: 10.1136/thorax.58.6.505
35. Shahid SK, Kharitonov SA, Wilson NM, Bush A, Barnes PJ. Exhaled 8-isoprostane in childhood asthma. Respir Res. (2005) 6:79. doi: 10.1186/1465-9921-6-79
36. Loukides S, Kontogianni K, Hillas G, Horvath I. Exhaled breath condensate in asthma: from bench to bedside. Curr Med Chem. (2011) 18:1432–43. doi: 10.2174/092986711795328418
37. Thomas PS, Lowe AJ, Samarasinghe P, Lodge CJ, Huang Y, Abramson MJ, et al. Exhaled breath condensate in pediatric asthma: promising new advance or pouring cold water on a lot of hot air? a systematic review. Pediatr Pulmonol. (2013) 48:419–42 doi: 10.1002/ppul.22776
38. Csoma Z, Kharitonov SA, Balint B, Bush A, Wilson NM, Barnes PJ. Increased leukotrienes in exhaled breath condensate in childhood asthma. Am J Respir Crit Care Med. (2002) 166:1345–9. doi: 10.1164/rccm.200203-233OC
39. Debley JS, Hallstrand TS, Monge T, Ohanian A, Redding GJ, Zimmerman J. Methods to improve measurement of cysteinyl leukotrienes in exhaled breath condensate from subjects with asthma and healthy controls. J Allergy Clin Immunol. (2007) 120:1216–7. doi: 10.1016/j.jaci.2007.06.029
40. Steiss JO, Rudloff S, Landmann E, Ruckes-Nilges C, Zimmer KP, Lindemann H. Effect of inhaled corticosteroid treatment on exhaled breath condensate leukotriene E(4) in children with mild asthma. Allergy Asthma Proc. (2008) 29:371–5. doi: 10.2500/aap.2008.29.3135
41. Montuschi P, Mondino C, Koch P, Barnes PJ, Ciabattoni G. Effects of a leukotriene receptor antagonist on exhaled leukotriene E4 and prostanoids in children with asthma. J Allergy Clin Immunol. (2006) 118:347–53. doi: 10.1016/j.jaci.2006.04.010
42. Karakoc GB, Yukselen A, Yilmaz M, Altintas DU, Kendirli SG. Exhaled breath condensate MMP-9 level and its relationship with asthma severity and interleukin-4/10 levels in children. Ann Allergy Asthma Immunol. (2012) 108:300–4. doi: 10.1016/j.anai.2012.02.019
43. Shahid SK, Kharitonov SA, Wilson NM, Bush A, Barnes PJ. Increased interleukin-4 and decreased interferon-gamma in exhaled breath condensate of children with asthma. Am J Respir Crit Care Med. (2002) 165:1290–3. doi: 10.1164/rccm.2108082
44. Turner S. Exhaled nitric oxide and the management of childhood asthma–yet another promising biomarker “has been” or a misunderstood gem. Paediatr Respir Rev. (2015) 16:88–96. doi: 10.1016/j.prrv.2014.07.005
45. Kharitonov SA, Yates DH, Barnes PJ. Inhaled glucocorticoids decrease nitric oxide in exhaled air of asthmatic patients. Am J Respir Crit Care Med. (1996) 153:454–7. doi: 10.1164/ajrccm.153.1.8542158
46. Pijnenburg MW, De Jongste JC. Exhaled nitric oxide in childhood asthma: a review. Clin Exp Allergy. (2008) 38:246–59. doi: 10.1111/j.1365-2222.2007.02897.x
47. Baraldi E, de Jongste JC. Measurement of exhaled nitric oxide in children, 2001. Eur Respir J. (2002) 20:223–37. doi: 10.1183/09031936.02.00293102
48. ATS/ERS recommendations for standardized procedures for the online and offline measurement of exhaled lower respiratory nitric oxide and nasal nitric oxide, 2005. Am J Respir Crit Care Med. (2005) 171:912–30. doi: 10.1164/rccm.200406-710ST
49. Covar RA, Szefler SJ, Martin RJ, Sundstrom DA, Silkoff PE, Murphy J, et al. Relations between exhaled nitric oxide and measures of disease activity among children with mild-to-moderate asthma. J Pediatr. (2003) 142:469–75. doi: 10.1067/mpd.2003.187
50. Komakula S, Khatri S, Mermis J, Savill S, Haque S, Rojas M, et al. Body mass index is associated with reduced exhaled nitric oxide and higher exhaled 8-isoprostanes in asthmatics. Respir Res. (2007) 8:32. doi: 10.1186/1465-9921-8-32
51. Ludviksdottir D, Diamant Z, Alving K, Bjermer L, Malinovschi A. Clinical aspects of using exhaled NO in asthma diagnosis and management. Clin Respir J. (2012) 6:193–207. doi: 10.1111/crj.12001
52. Mahr TA, Malka J, Spahn JD. Inflammometry in pediatric asthma: a review of fractional exhaled nitric oxide in clinical practice. Allergy Asthma Proc. (2013) 34:210–9. doi: 10.2500/aap.2013.34.3660
53. Singer F, Luchsinger I, Inci D, Knauer N, Latzin P, Wildhaber JH, Moeller A. Exhaled nitric oxide in symptomatic children at preschool age predicts later asthma. Allergy (2013) 68:531–8. doi: 10.1111/all.12127
54. Caudri D, Wijga AH, Hoekstra MO, Kerkhof M, Koppelman GH, Brunekreef B, Smit HA, de Jongste JC. Prediction of asthma in symptomatic preschool children using exhaled nitric oxide, Rint and specific IgE. Thorax (2010) 65:801–7. doi: 10.1136/thx.2009.126912
55. Dweik RA, Boggs PB, Erzurum SC, Irvin CG, Leigh MW, Lundberg JO, et al. An official ATS clinical practice guideline: interpretation of exhaled nitric oxide levels (FENO) for clinical applications. Am J Respir Crit Care Med. (2011) 184:602–15. doi: 10.1164/rccm.9120-11ST
56. Taylor DR. Advances in the clinical applications of exhaled nitric oxide measurements. J Breath Res. (2012) 6:047102. doi: 10.1088/1752-7155/6/4/047102
57. van Rensen EL, Straathof KC, Veselic-Charvat MA, Zwinderman AH, Bel EH, Sterk PJ. Effect of inhaled steroids on airway hyperresponsiveness, sputum eosinophils, and exhaled nitric oxide levels in patients with asthma. Thorax (1999) 54:403–8. doi: 10.1136/thx.54.5.403
58. Sorkness CA, Wildfire JJ, Calatroni A, Mitchell HE, Busse WW, O'Connor GT, et al. Reassessment of omalizumab-dosing strategies and pharmacodynamics in inner-city children and adolescents. J Allergy Clin Immunol Pract. (2013) 1:163–71. doi: 10.1016/j.jaip.2013.01.011
59. Petsky HL, Cates CJ, Lasserson TJ, Li AM, Turner C, Kynaston JA, et al. A systematic review and meta-analysis: tailoring asthma treatment on eosinophilic markers (exhaled nitric oxide or sputum eosinophils). Thorax (2012) 67:199–208. doi: 10.1136/thx.2010.135574
60. Jartti T, Wendelin-Saarenhovi M, Heinonen I, Hartiala J, Vanto T. Childhood asthma management guided by repeated FeNO measurements: a meta-analysis. Paediatr Respir Rev. (2012) 13:178–83. doi: 10.1016/j.prrv.2011.11.002
61. Petsky HL1, Kew KM, Chang AB. Exhaled nitric oxide levels to guide treatment for children with asthma. Cochrane Database Syst Rev. (2016) 11:CD011439. doi: 10.1002/14651858.CD011439.pub2
62. van Mastrigt E, de Jongste JC, Pijnenburg MW. The analysis of volatile organic compounds in exhaled breath and biomarkers in exhaled breath condensate in children - clinical tools or scientific toys? Clin Exp Allergy (2015) 45:1170–88. doi: 10.1111/cea.12454
63. Barker M, Hengst M, Schmid J, Buers HJ, Mittermaier B, Klemp D, et al. Volatile organic compounds in the exhaled breath of young patients with cystic fibrosis. Eur Respir J. (2006) 27:929–36. doi: 10.1183/09031936.06.00085105
64. Dallinga JW, Robroeks CM, van Berkel JJ, Moonen EJ, Godschalk RW, Jobsis Q, et al. Volatile organic compounds in exhaled breath as a diagnostic tool for asthma in children. Clin Exp Allergy (2010) 40:68–76.
65. Caldeira M, Barros AS, Bilelo MJ, Parada A, Camara JS, Rocha SM. Profiling allergic asthma volatile metabolic patterns using a headspace-solid phase microextraction/gas chromatography based methodology. J Chromatogr A (2011) 1218:3771–80. doi: 10.1016/j.chroma.2011.04.026
66. Smolinska A, Klaassen EM, Dallinga JW, van de Kant KD, Jobsis Q, Moonen EJ, et al. Profiling of volatile organic compounds in exhaled breath as a strategy to find early predictive signatures of asthma in children. PLoS ONE (2014) 9:e95668. doi: 10.1371/journal.pone.0095668
67. Robroeks CM, van Berkel JJ, Jobsis Q, van Schooten FJ, Dallinga JW, Wouters EF, et al. Exhaled volatile organic compounds predict exacerbations of childhood asthma in a 1-year prospective study. Eur Respir J. (2013) 42:98–106. doi: 10.1183/09031936.00010712
Keywords: biomarkers, inflammation, FeNO, exhaled breath condensate, exhaled breath volatile compounds
Citation: Tenero L, Zaffanello M, Piazza M and Piacentini G (2018) Measuring Airway Inflammation in Asthmatic Children. Front. Pediatr. 6:196. doi: 10.3389/fped.2018.00196
Received: 29 April 2018; Accepted: 18 June 2018;
Published: 06 July 2018.
Edited by:
Mario Barreto, Sapienza Università di Roma, ItalyReviewed by:
Iulia Ioan, Hôpital d'Enfants, FranceZuzana Rennerova, Pneumo-Alergo centrum, Slovakia
Copyright © 2018 Tenero, Zaffanello, Piazza and Piacentini. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Laura Tenero, bGF1cmEudGVuZXJvQHVuaXZyLml0
 Laura Tenero
Laura Tenero Marco Zaffanello
Marco Zaffanello Michele Piazza
Michele Piazza Giorgio Piacentini
Giorgio Piacentini