- 1Center for Clinical Research and Education, Region Värmland, Karlstad, Sweden
- 2Faculty of Medicine and Health, School of Health Sciences, Örebro University, Örebro, Sweden
- 3School of Nursing, Faculty of Health, Dalhousie University, Halifax, NS, Canada
- 4MOM-LINC Lab, IWK Health Halifax, Halifax, NS, Canada
Introduction: Research related to parent-led neonatal pain management is increasing, as is the clinical implementation. Skin-to-skin contact, breastfeeding and parents' vocalizations are examples of pain reducing methods that give parents an opportunity to protect their infant from harm while alleviating their anxiety and developing their parenting skills.
Methods: In this paper we will provide a narrative review and describe the current research about parent-led neonatal pain management. Based on this we will discuss clinical challenges, implementation strategies and implications for future research.
Results: Parents express great readiness to embrace opportunities to increase their self-efficacy in their ability to address infant pain. Parent-led pain-reducing methods are effective, feasible, cost-effective, culturally sensitive, and can be individualized and tailored to both the parent's and infant's needs. Both barriers and facilitators of parent-led pain care have been studied in research highlighting structural, organizational, educational, and intra- and interpersonal aspects. For example, health care professionals' attitudes and beliefs on parent-led methods, and their concern that parental presence during a procedure increases staff anxiety. On the other hand, the presence of a local pain champion whose duty is to facilitate the adoption of pain control measures and actively promote parent-professional collaboration, is crucial for culture change in neonatal pain management and nurses have a key role in this change. The knowledge-to-practice gap in parent-led management of infants' procedure-related pain highlight the need for broader educational applications and collaborative professional, parental and research initiatives to facilitate practice change.
Conclusion: Parent-led neonatal pain management is more than simply a humane and compassionate thing to do. The inclusion of parent-led pain care has been scientifically proven to be one of the most effective ways to reduce pain associated with repeated painful procedures in early life and parents report a desire to participate. Focus on enablers across interprofessional, organizational and structural levels and implementation of recommended pediatric pain guidelines can support the provision of optimal evidence-based family-centered neonatal pain management.
Introduction
Although family-centred care was introduced globally in paediatric and neonatal care in the 1990s (1, 2), it was not until the 21st century that many neonatal intensive care units (NICU) started to implement family-centred care welcoming both parents and possibly also siblings in the units, actively involving the parents in the infant's daily care round the clock. Still, accepting parents as active partners in neonatal pain management, is an even more recent and currently ongoing concept across NICUs and healthcare globally. The combined negative effect of repeated pain exposure and maternal separation is a strong stressor with adverse long-term effects (3), which further motivates having the parents at the unit and involving them in the pain management of their infant.
What we do know from previous research is that there is a research-to-practice gap among the NICU team when supporting parent-led pain-reducing methods and a combination of these, for example combined breastfeeding, skin-to-skin contact (SSC) and the parent's live singing during painful procedures (4). Moreover, while it is essential to include parents as active members in the NICUs interprofessional healthcare team since interprofessional collaboration contributes to improved procedural pain management in neonates, few NICUs have fully embraced parent inclusion (5). To what extent and consistency health care professionals promote, support, facilitate and systematically implement parent-led pain management globally, is yet to be ascertained. Nevertheless, engaging parents as key partners which includes promoting parent-led pain-relief and parental involvement in infants' pain assessment, is aligned with best evidence informed infant pain care and should be advanced.
This paper aims to provide a narrative review that describes the current best evidence for parent-led neonatal pain management, as well as address clinical challenges, implementation strategies and implications for future research.
Review
Parent-led pain assessment and management
Parents can play an active role in both assessment and management of neonatal pain (6). Parents who are able to be present with their infant at the hospital can identify signs of pain and discomfort (7–9). However, parents may underestimate their infant's pain, compared to the assessment of health care professionals (10, 11). As such, it is important that parents receive education and support from health care professionals to enable them to perform a valid and reliable pain assessment (12).
Several reviews have demonstrated that parents can be part of the pain management for their infant (4, 13–15) and that this is safe and effective (15). Some of the evaluated methods are almost solely performed by the mother (breastfeeding) or parent (SSC), whereas there are a number of methods that can be performed by the parents, other family members or health care professionals (e.g., facilitated tucking, providing non-nutritive sucking or swaddling) (16). There is moderate to high certainty evidence that skin-to-skin contact, and breastfeeding are effective pain-reducing methods, whereas other interventions should be seen as adjuvant or working best in combination with other (6).
Skin-to-skin contact
SSC, or Kangaroo Care (KC), means placing the baby dressed only in a diaper, and maybe a hat to avoid heat-loss, on the bare chest of the parent. Usually, an upright prone position is used, but side-lying, e.g., during breastfeeding, is also common. There are special tube tops or cloth slings that are used to support maintaining the KC-position over prolonged time.
SSC is probably the most studied parent-led pain relieving method for procedural pain. SSC has been demonstrated to significantly reduce pain intensity scores as measured using validated composite biobehavioral pain indicators (17), with an effect that sustains over repeated episodes of pain exposure (18). Most studies examined heel stick or injections as the source of noxious input (4, 17, 19). Skin-to-skin contact is often combined with other methods such as breastfeeding (20, 21) for an even better effect.
There is also some evidence that continuous or longer periods of SSC may diminish chronic or prolonged pain in infants. Prolonged SSC has been associated with a reduction in chronic pain scores measured using the EDIN pain scale and alteration in neuroendocrine markers suggestive of reduced pain (22). Most notably a decrease in dopamine and cortisol levels, and increase in beta-endorphin and serotonin in salivary and urinary samples. An advantage of promoting prolonged periods of SSC is that the parent and infant are already in position to use this pain-relieving method when a painful procedure is required, reducing the need to transfer the infant immediately prior to the painful event.
Breastfeeding and breast milk
Thirty-six studies examining the efficacy of breastfeeding for procedural pain relief in infants were included in a recent Cochrane review, most evaluated heel stick, intramuscular injection, and venipuncture. Breastfeeding reduced pain indicators such as duration of crying, heart rate increase and the pain scales NIPS, NFCS and DAN (23). As described above, the pain-relieving effect of breastfeeding can be enhanced when combined with skin-to-skin contact but also with maternal holding (21, 24). Giving the infant expressed breastmilk in isolation of the mother however does not appear to effectively reduce pain scores (23, 25), nor does waiting 1–2 h after the breastfeeding before performing the painful procedure (26).
The pain-relieving effect of breastfeeding persists beyond the neonatal period, at least for immunizations up to 12 months age, with a reduction of bio-behavioural pain responses (27).
Parental infant-directed singing and speech
More than a dozen reviews have been published on music-based interventions in neonatal care (28–30), including meta-analyses demonstrating significant positive effects on infant physiological signs, oral feeding volume, stress levels, and maternal anxiety (31, 32). In procedural pain management, previous research with recorded music as well as live lullaby singing carried out by a music therapist, have shown pain relieving and stress reducing effects (33) with a reduction in NIPS pain score (34).
A recent area of research is live or recorded parental infant-directed singing and speech as procedural support (35–43). Infant-directed speech is less effective in reducing distress than infant-directed singing. Parents should therefore sing live to tailor the singing to the infant's state and responses. Parents should sing or hum with a soothing, soft, steady, slow, and constant voice.
Recorded sound of the mother's heartbeats (44–46) or intrauterine sounds (47, 48) may have some effect in reducing physiological and behavioral signs of pain.
More research is needed to confirm the effectiveness of live parental singing and recorded maternal related sounds on infant pain. If used, parents should combine these strategies with other parent-led methods such as SSC and breastfeeding (49).
Positioning and touching
Helping the infant to a comforting position during painful procedures is something that easily can be performed by the parents. Facilitated tucking means gently holding the infant in a side lying flexed posture, supported by the hands of the parents. It has been demonstrated to reduce composite scores of stress and pain (50, 51). Holding the baby in the arms of the mother alone has not been associated with effective pain relief; however, in combination with oral glucose or breastfeeding it has been demonstrated to reduce pain intensity scores (24, 52).
Other adjuvant interventions that parents can provide, though with mixed findings on pain reduction, are comforting touch in a structured way (38, 53), e.g., with Yakson touch (54, 55), or combined with other interventions, i.e., as sensorial saturation (56, 57) or nesting (55). A systematic review showed that massage can reduce pain scores and cry duration (58). It is important to combine comforting touch with more effective parent-led interventions.
Sweet solution and non-nutritive sucking
While not a parent-led intervention, parents can actively participate by offering a pacifier or finger to suck to their infant following administration of a sweet tasting solution. There is moderate certainty of evidence supporting the pain-relieving effect of a small amount of sweet solution that is given in the mouth prior to a painful procedure, as measured with composite pain scores. Sucrose is the most studied substance (59, 51), followed by glucose (60, 61) and comparisons between the effectiveness of the two substances are inconclusive (62). The effectiveness of sweet tasting solutions has been linked with the concentration, i.e., that it is sweet enough (63). Concentrations of sucrose greater than 18% sucrose may be more effective, however, very high concentrations >35% do not seem to provide greater effect (59). Ensuring that the solution is given on the tip (taste receptors) of the tongue enhances the effect. While significant variation in the dosing of sucrose exists, research supports that small amounts as low as 0.1 ml repeated as necessary throughout the procedure to achieve low pain scores are effective (63). The additive effect of non-nutritive sucking has been associated with enhanced pain-relieving effect of sweet solutions (64) but according to a Cochrane-review, the evidence is of low certainty (59). While the combination of sweet tasting solution with skin-to-skin contact did not appear to provide an additive pain reducing effect in preterm infants undergoing heel stick (65), it is uncertain whether the combination may reduce needle related pain scores in full term infants (6).
Interaction between the parent and the infant
Infants seek contingent, companionable interactions with their parent. An infant has an innate capacity to communicate, and share affects, which develops through the close relationship with the parents. Naturalistic parent-infant moment-to-moment communication comprises multimodal actions, including music-like vocalizations, and are present in a healthy regulatory parent-infant interaction (66). Parents communicate with their infant in a multimodal and multisensory way where the communication takes place through the intentions and affects carried by the music-like qualities of the infant-parent joint vocalization in combination with the joint dance-like gestures of their bodies, facial movements, and touch (67).
Mediating factors in parent-led pain management
Most parent-led interventions are multisensorial in nature. Conceptionally, the Neuromatrix Theory, developed by Melzack (68), an extension to his original “gate theory” of pain developed in 1965 with Wall (69) provides an underlying framework to better understand the possible efficacy of non-pharmacologic methods of pain relief. The model outlines the importance of both ascending and descending inputs to the conscious experience of pain and includes additional inputs such as the important contributions of memory and context. Mediating factors, such as context, relationships, competing multisensorial inputs and meaning have been shown to modulate the experience of pain in adults (70–72). Similarly, infants experience the affective dynamics of pain like adults (73–75). When brain regions within the descending pain modulatory system are more functionally connected, infants have a greater ability to regulate their brain activity in response to incoming noxious stimulation (73). It is not yet determined if the descending pain modulatory system operates at birth in a less functionally connected brain, like the preterm infant's immature brain (73). The descending pain modulatory system is fully functional at birth in term born healthy infants, similar to that observed in adults (73). In the context of parent-led pain care, the combination of the parent's, skin, warmth, voice, breathing rhythm, soothing touch, taste, and scent fully match and harmonize with the infants' multisensory, biopsychosocial state of being, which may modulate the affective dynamics of the infant's pain.
Intuitive parental activities, drawn from the naturally occurring patterns of successful parent-infant communication which support the infant to be heard, seen, and nurtured, can be incorporated into the guidelines for procedural pain management to foster the parent-infant relationship. What seems to be most crucial for an infant before, during and after a painful situation as well as for future painful experiences, is the extent to which the parent is emotionally available and stable, capable of noticing and contingently interpreting cues and communications implicit in the infant's behaviour, responding adequately to the infant's distress signals and being able to soothe, regulate and share the infant's states (49).
How involved do parents want to be?
Parents' opinions about active contribution in pain management and membership in an interprofessional team-based collaboration, are unanimous across research (4, 76). Parents want to and need to actively participate in their infant's pain management (4). They want to, because parents have a need to feel validated in their role as their infant's principal protector and it helps them feel in control over the painful situation (76). And they need to, because it relieves the parents' own stress when fulfilling their role (51, 76), resulting in an upward spiral towards emotional availability and responsiveness in the painful context. One reason for the effectiveness of parent-led pain management is something as fundamental as love, a parent's love and empathy (77). Parental presence enables a range of effective parent-led pain reducing interventions such as skin-to-skin contact, breastfeeding, rocking and soothing vocalizations.
Competence and confidence to participate
Parental advocacy addresses parents' perspectives on advocating for themselves to participate in pain management or advocating for their infant to have their pain managed (78). Advocating for their infant's needs, being involved in shared decision making and having opportunities to provide parent-led non-pharmacological measures, empowers parents to take a more active role in the prevention, assessment and management of their infant's pain and discomfort (79). Consequently, prerequisites for parent-led pain management and equal partnership in the infant's pain care, are parental presence in the NICU and proximity to the infant as well as a trusting and updated staff, and access to information and guidance (5, 78–86).
Parents feel they have a vital role in infant pain care, and they want as much involvement as possible. Both mothers and their partners express a strong desire to be present and involved in various painful procedures to comfort their infant (78, 87). Nevertheless, even though a majority of health care professionals [in some estimates, as many as 70% (88),] find it beneficial for the infant with parents present during common painful procedures i.e., nasogastric tube placement, capillary blood sampling, or venepuncture, the parent's role as a bystander increases the more invasive the procedures are (central line insertion, extubation, lumbar puncture, and intubation) (88–90).
Challenges of parent-led pain care
While neonatal pain care is moving in the right direction, the culture of care that facilitates active parental contribution in infants' pain management is challenged by structural, organizational, and intra- and interpersonal barriers (85) (Table 1).
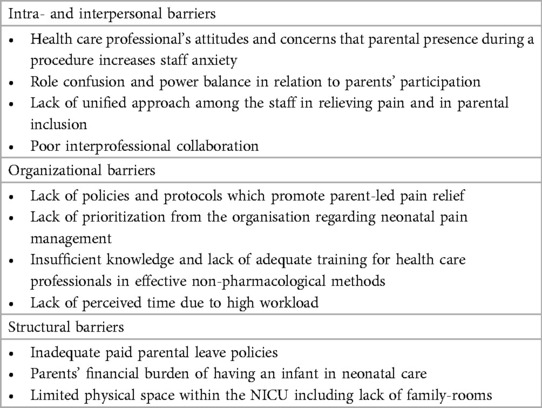
Table 1. Factors defined in the literature that impede implementation of parent-led pain care (5, 76, 80, 85, 88, 91–94).
Geographical location of the NICU/hospital as well as the health care professional's age, gender, experience, status, education level, expertise, and confidence, can contribute or hamper parent-led pain management (88, 89, 95). In general, nurses appear to be more in favour of involving the parents in pain management compared with physicians and a north-to-south gradient has been observed in Europe, where barriers to the presence of parents and other family members in European NICUs remain higher in southern European countries (88). Lack of communication and collaboration between physicians and nurses is a significant factor in poor pain management (5).
Enablers of parent-led pain care
Knowledge of providing pain management strategies for their infants empowers parents to take an active role in their infant's pain care, and updated knowledge on parent-led pain-reducing methods is a prerequisite for health care professionals' attitudes towards actively involving parents (76, 80–82, 85, 86, 88–90, 96, 97). Several factors across structural, organizational, and intra- and interpersonal levels have been reported. Research lists numerous factors that can facilitate practice change (Table 2).
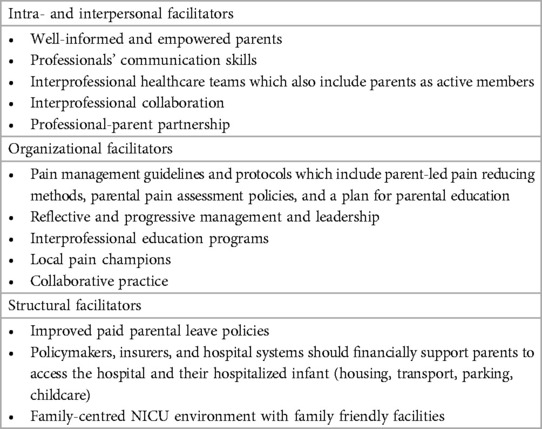
Table 2. Factors defined in the literature that facilitate implementation of parent-led pain care (5, 81, 86, 91–93, 95, 96, 98–101).
Knowledge transfer
Family-centered care is well recognized for its positive influence on family health outcomes, and there has been advocacy towards parents being considered as essential member of the neonatal care team (102). Despite this trend, the concept of fully integrating families in the provision of infant pain care is a relatively new concept, with poor practice uptake. Many parents remain unaware of their capacity to provide pain relief for their infants which contributes to poor practice (4, 103–106). Nurses and physicians who are key figures in driving clinical change, require education and training that support parental participation (95). The development of professional knowledge consists of developing guidelines, continuous presentation of consolidated new research findings, regular evaluation of pain management outcomes, and periodic education for new staff (91). Knowledge sharing is key for clinical change which leads to successful involvement of parents in their infant's pain management and better pain care for the infants.
Parent-targeted education in the neonatal period
Parental education increases parents' knowledge about strategies, self-efficacy and confidence in managing infant pain, and satisfaction with the pain management, and should therefore be incorporated into postnatal care (87). From the parents' point of view, it's a question of timing, framing and content of the knowledge sharing and collaboration. Parents state that they prefer information about pain and pain management to be provided by the staff at a pace directed by the parent and infant, in a calm, supportive and more private environment and without having to ask for it (76, 80). Parents have difficulty absorbing new information during a procedure or in a noisy room with many distractions, and parents might feel hesitant to ask questions or get in the way (76). The initial days of hospitalization are often stressful for NICU parents, but parents express that during the first week of hospitalization it would be optimal for the staff to deliver information on parent-led pain management (78).
Information to increase parent-led strategies needs to be delivered in different formats and in the many languages of our multi-cultural society (83). Research has investigated various knowledge-translational interventions e.g., available on-line videos, educational booklets, pamphlets, dedicated websites, QR codes, educational bundles, customized individual workshop sessions for parents with hands-on guidance in parent-led methods, face-to-face interaction with health care professionals (78, 83, 84, 87, 107–109). Parents (especially low literacy parents) may need better visual aids to fully comprehend the various comfort techniques (107). Even though many parents prefer electronic resources, parents still desire human interaction for learning and favor a health care professional to review the information with them face to face (78).
Co-creation of mutual knowledge is a dynamic process that is important for the establishment of a nurse-parent partnership (110) which increases the sense of equality among parents and helps them feel valued, trusted, respected, and seen as a resource (86). Open and honest communication is the basis for cooperation in pain management (110), including health care professionals' willingness to listen to the parents to find a mutually satisfactory course of action (86). Parents want for example guidance on how to interpret an infant's pain and guidance in pain assessment. A crucial factor is the freedom for the parents to choose and being listened to about how much, and in which way, they want to participate—or not (86).
Online e-health resources for parents
In addition to formal (e.g., healthcare providers) and informal (e.g., peer groups) written and oral resources to advise parents of the importance of their role, there has been a trend towards using online e-health resources to inform and engage parents in pain care. Parents in neonatal care have reported high use and a preference for using the internet or smartphone to access information (111, 112). However, there remains a paucity of quality online resources. An evaluation of websites or mHealth apps targeted to parents of preterm infants found issues related to their credibility and moderate overall quality, with less than 11% providing any information on infant pain (113, 114). While online resources appear to be favoured by parents, parents recognize possible issues regarding the quality of the content. Parents reported that online resources created by institutions with healthcare provider input would reduce this concern.
Additionally, only 11 studies were included in a comprehensive analysis of the impact of parent-targeted eHealth educational interventions about infant procedural pain management on parental (e.g., mental health, knowledge uptake), eHealth (e.g., acceptance, use), and pain management outcomes [e.g., parental involvement, infant pain response (115)]. Findings revealed that short and engaging educational videos may positively impact parents' knowledge, confidence, and desire to be involved in procedural pain management for their infant (109, 116). Key facilitators of e-health related resources include alignment with the Baby-Friendly Hospital Initiative, modeling by Lactation Consultants, and frequent reminders (117). However, there remains a gap in our understanding if the provision of this information to parents leads to a greater parental involvement in clinical practice and subsequent reduction on infant pain. Further work in this area is warranted.
Practice and policy implications
To date, few studies in the neonatal pain context, have investigated parents' experiences of providing parent-led pain management for their infant (4). However, several studies are ongoing. The study “Parents as pain management in Swedish neonatal care (SWEpap)” (118) is a cutting-edge interdisciplinary multi-centre clinical study with mixed methods involving both parents and health professionals. The aim of SWEpap is to investigate parents' and nurses' reflections on experiencing parent-delivered pain management, breastfeeding (when applicable), skin-to-skin contact, and parental infant-directed lullaby singing, during painful procedures in neonatal care. Another on-going study, the British Petal Trial, is examining the pain-relieving effects of parental touching, or more specific strokes in 112 neonates undergoing heel lancing on noxious-evoked brain activity, pain scores, parental anxiety, and parents' reflections on participating in neonatal pain research (119, 120).
In many countries parents have limited possibilities to stay with their newborn infant at hospital, due to social support systems, limited space at the unit or rules and tradition. Therefore, some researchers are trying to develop systems with recorded maternal voices (121, 122) or robots (123, 124) to replace the mother when not there. This “better-than-nothing” approach could however delay efforts to include parents in the hospital care of their infants, especially when resource-saving arguments are being used (125).
Recommendation for guidelines
There has been a considerable movement towards ensuring that parents are included in pain standards and guidelines. The Pediatric Pain Management Standard released in April 2023 by the Health Standards Organization of Canada in partnership with Solutions for Kids in Pain, a government funded national centre for excellence is aimed to support the delivery of equitable evidence informed pain care. The standard consisting of 34 recommendations recognizes that parents are equal members of the team and should be actively involved in decision making and care decisions (126). The standard is well aligned with the Lancet commission call to action to improve pediatric pain care (127). Despite these important inroads, few guidelines issued by a national or international authority, or a professional organization or network specifically recommend or include implementation strategies for parent-led pain management, with even fewer addressing parent-led interventions in low income and low-tech settings (4).
When written instructions are available in the NICUs about pain assessment with a structure for pain documentation, and the use of non-pharmacological methods including parent-led interventions, the staff reports higher awareness on these matters than units that do not have written local pain management guidelines for everyday work (93). One of the main obstacles leading to inadequate use of non-pharmacological methods is the lack of standards and guidelines. Guidelines are important means to improve the effectiveness and consistency of care. However, the mere existence of guidelines does not guarantee the use of them (128). Adherence depends on for example ongoing training and monitoring of their use (90). Regular rotations of staff means that frequency of teaching needs must be evaluated and prioritized to increase awareness of parent involvement in pain care, pain assessment, assessment tools and parent-led interventions.
Guidelines are usually initiated and implemented in health care through a top-down approach where information filters down through a hierarchical structure. When this approach is combined with dedicated and well-informed nurses and physicians as local pain champions in each NICU, a profound long-lasting change can happen. This will improve the conditions for the pain exposed infant and welcome the parents as partners in neonatal pain management. Local pain facilitators strive to provide health care professionals the opportunity to talk about and reflect on pain management issues and professional limitations and needs (91). Interprofessional discussions will build confidence, maintain skills, and produce living guidelines. One method to support the uptake of practice recommendations, is through quality improvement initiatives, a strategy that has been emphasized in the Canadian Pediatric Standards (126).
Conclusion
Parent-led neonatal pain management is more than simply a humane and compassionate thing to do. The inclusion of parent-led pain care has been scientifically proven to be one of the most effective ways to reduce pain associated with repeated painful procedures in early life and parents report a desire to participate. Focus on enablers across inta- and interprofessional, organizational and structural levels and implementation of recommended pediatric pain guidelines can support the provision of optimal evidence-based family-centered neonatal pain management.
Author contributions
AU: Writing – review & editing, Writing – original draft, Conceptualization. MC-Y: Writing – review & editing, Writing – original draft. ME: Project administration, Writing – review & editing, Writing – original draft, Conceptualization.
Funding
The authors declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Franck LS, O’Brien K. The evolution of family-centered care: from supporting parent-delivered interventions to a model of family integrated care. Birth Defects Res. (2019) 111(15):1044–59. doi: 10.1002/bdr2.1521
2. Roue JM, Kuhn P, Lopez Maestro M, Maastrup RA, Mitanchez D, Westrup B, et al. Eight principles for patient-centred and family-centred care for newborns in the neonatal intensive care unit. Arch Dis Child Fetal Neonatal Ed. (2017) 102(4):F364–F8. doi: 10.1136/archdischild-2016-312180
3. Filippa M, Poisbeau P, Mairesse J, Monaci MG, Baud O, Hüppi P, et al. Pain, parental involvement, and oxytocin in the neonatal intensive care unit. Front Psychol. (2019) 10:715. doi: 10.3389/fpsyg.2019.00715
4. Ullsten A, Andreasson M, Eriksson M. State of the art in parent-delivered pain-relieving interventions in neonatal care: a scoping review. Front Pediatr. (2021) 9:651846. doi: 10.3389/fped.2021.651846
5. Balice-Bourgois C, Zumstein-Shaha M, Simonetti GD, Newman CJ. Interprofessional collaboration and involvement of parents in the management of painful procedures in newborns. Front Pediatr. (2020) 8:394. doi: 10.3389/fped.2020.00394
6. Campbell-Yeo M, Eriksson M, Benoit B. Assessment and management of pain in preterm infants: a practice update. Children. (2022) 9(2):244. doi: 10.3390/children9020244
7. dos Santos MCC, Pereira Gomes MF, Capellini VK, dos Santos Carvalho VC. Maternal assessment of pain in premature infants. Revista da Rede de Enfermagem do Nordeste. (2015) 16(6):842–7. doi: 10.15253/2175-6783.2015000600010
8. Soares MFE, Gomes Chaves A, da Silva Morais AP, da Silva Rabelo MZ, Rodrigues LDN, Camelo Chaves EM. Newborn’s pain under the mother’s perception. Rev Dor São Paulo. (2017) 18(4):338–41. doi: 10.5935/1806-0013.20170126
9. Palomaa AK, Hakala M, Polkki T. Parents’ perceptions of their child’s pain assessment in hospital care: a cross-sectional study. J Pediatr Nurs. (2023) 71:79–87. doi: 10.1016/j.pedn.2023.03.012
10. Tannous Elias LSD, dos Santos AMN, Guinsburg RJBP. Perception of pain and distress in intubated and mechanically ventilated newborn infants by parents and health professionals. BMC Pediatr. (2014) 14(44):1–7. doi: 10.1186/1471-2431-14-44
11. Olsson E, Pettersson M, Eriksson M, Ohlin A. Oral sweet solution to prevent pain during neonatal hip examination: a randomised controlled trial. Acta Paediatr. (2019) 108(4):626–9. doi: 10.1111/apa.14588
12. Pillai Riddell R, Flora DB, Stevens S, Greenberg S, Garfield H. The role of infant pain behaviour in predicting parent pain ratings. Pain Res Manag. (2014) 19(5):e124–32. doi: 10.1155/2014/934831
13. Eissler AB, Zwakhalen S, Stoffel L, Hahn S. Systematic review of the effectiveness of involving parents during painful interventions for their preterm infants. J Obstet Gynecol Neonatal Nurs. (2022) 51(1):6–15. doi: 10.1016/j.jogn.2021.08.100
14. Acharya S, Sethi D. Effectiveness of involving parents during minor invasive procedures of the neonates admitted in neonatal intensive care unit (NICU): a review based on available literature. Int J Innov Res Sci Eng Technol. (2023) 8(7):1781–8. doi: 10.5281/zenodo.8211264
15. Muirhead R, Kynoch K, Peacock A, Lewis PA. Safety and effectiveness of parent- or nurse-controlled analgesia in neonates: a systematic review. JBI Evid Synth. (2022) 20(1):3–36. doi: 10.11124/JBIES-20-00385
16. Pillai Riddell RR, Bucsea O, Shiff I, Chow C, Gennis HG, Badovinac S, et al. Non-pharmacological management of infant and young child procedural pain. Cochrane Database Syst Rev. (2023) 6(6):CD006275. doi: 10.1002/14651858.CD006275.pub4
17. Johnston C, Campbell-Yeo M, Disher T, Benoit B, Fernandes A, Streiner D, et al. Skin-to-skin care for procedural pain in neonates. Cochrane Database Syst Rev. (2017) 2(2):CD008435. doi: 10.1002/14651858.CD008435.pub3
18. Wang Y, Zhang L, Dong W, Zhang R. Effects of Kangaroo mother care on repeated procedural pain and cerebral oxygenation in preterm infants. Am J Perinatol. (2023) 40(8):867–73. doi: 10.1055/s-0041-1731650
19. Jones L, Laudiano-Dray MP, Whitehead K, Meek J, Fitzgerald M, Fabrizi L, et al. The impact of parental contact upon cortical noxious-related activity in human neonates. Eur J Pain. (2021) 25(1):149–59. doi: 10.1002/ejp.1656
20. Leite AM, Silva ADCTOD, Castral TC, Nascimento LC, Sousa MID, Scochi CGS. Breastfeeding and skin-to-skin contact for pain relief of newborns during hepatitis B vaccination. Revista Eletrônica de Enfermagem. (2015) 17(3):31932. doi: 10.5216/ree.v17i3.31932
21. Marin Gabriel MA, del Rey Hurtado de Mendoza B, Jimenez Figueroa L, Medina V, Iglesias Fernandez B, Vazquez Rodriguez M, et al. Analgesia with breastfeeding in addition to skin-to-skin contact during heel prick. Arch Dis Child Fetal Neonatal Ed. (2013) 98(6):F499–503. doi: 10.1136/archdischild-2012-302921
22. Pavlyshyn H, Sarapuk I. Skin-to-skin contact-an effective intervention on pain and stress reduction in preterm infants. Front Pediatr. (2023) 11:1148946. doi: 10.3389/fped.2023.1148946
23. Shah PS, Torgalkar R, Shah VS. Breastfeeding or breast milk for procedural pain in neonates. Cochrane Database Syst Rev. (2023) 8(8):CD004950. doi: 10.1002/14651858.CD004950.pub4
24. Obeidat HM, Shuriquie MA. Effect of breast-feeding and maternal holding in relieving painful responses in full-term neonates: a randomized clinical trial. J Perinat Neonatal Nurs. (2015) 29(3):248–54. doi: 10.1097/JPN.0000000000000121
25. Gradin M, Finnstrom O, Schollin J. Feeding and oral glucose–additive effects on pain reduction in newborns. Early Hum Dev. (2004) 77(1-2):57–65. doi: 10.1016/j.earlhumdev.2004.01.003
26. Altuntas N, Altuntas S, Nar D, Simsek M, Unsal A, Gungor AA. Does interval between breastfeeding and heel lance affect the perception of pain in newborns? J Coll Physicians Surg Pak. (2022) 32(1):46–50. doi: 10.29271/jcpsp.2022.01.46
27. Harrison D, Reszel J, Bueno M, Sampson M, Shah VS, Taddio A, et al. Breastfeeding for procedural pain in infants beyond the neonatal period. Cochrane Database Syst Rev. (2016) 10(10):CD011248. doi: 10.1002/14651858.CD011248.pub2
28. Mohan A, Gokulakrishnan G, El-Saie A, Brickley A, Hagan J, Pammi M. Music therapy for preterm neonates in the neonatal intensive care unit: an overview of systematic reviews. Acta Paediatr. (2021) 110(12):3180–200. doi: 10.1111/apa.16055
29. Haslbeck FB. Music therapy for premature infants and their parents: an integrative review. Nord J Music Ther. (2012) 21(3):203–26. doi: 10.1080/08098131.2011.648653
30. Costa VS, Bundchen DC, Sousa H, Pires LB, Felipetti FA. Clinical benefits of music-based interventions on preterm infants’ health: a systematic review of randomised trials. Acta Paediatr. (2022) 111(3):478–89. doi: 10.1111/apa.16222
31. Yue W, Han X, Luo J, Zeng Z, Yang M. Effect of music therapy on preterm infants in neonatal intensive care unit: systematic review and meta-analysis of randomized controlled trials. J Adv Nurs. (2021) 77(2):635–52. doi: 10.1111/jan.14630
32. Bieleninik Ł, Ghetti C, Gold C. Music therapy for preterm infants and their parents: a meta-analysis. Pediatrics. (2016) 138(3):e20160971. doi: 10.1542/peds.2016-0971
33. Ullsten A, Hugoson P, Forsberg M, Forzelius L, Klässbo M, Olsson E, et al. Efficacy of live lullaby singing during procedural pain in preterm and term neonates. Music Med. (2017) 9(2):73–85. doi: 10.47513/mmd.v9i2.546
34. Anbalagan S, Velasquez JH, Staufert Gutierrez D, Devagiri S, Nieto D, Ankola P. Music for pain relief of minor procedures in term neonates. Pediatr Res. (2023) 95:679–83. doi: 10.1038/s41390-023-02746-4
35. Jahromi LB, Putnam SP, Stifter CA. Maternal regulation of infant reactivity from 2 to 6 months. Dev Psychol. (2004) 40(4):477–87. doi: 10.1037/0012-1649.40.4.477
36. Johnston CC, Filion F, Campbell-Yeo M, Goulet C, Bell L, McNaughton K, et al. Enhanced Kangaroo mother care for heel lance in preterm neonates: a crossover trial. J Perinatol. (2009) 29(1):51–6. doi: 10.1038/jp.2008.113
37. Johnston CC, Campbell-Yeo M, Filion F. Paternal vs maternal Kangaroo care for procedural pain in preterm neonates: a randomized crossover trial. Arch Pediatr Adolesc Med. (2011) 165(9):792–6. doi: 10.1001/archpediatrics.2011.130
38. Johnston CC, Rennick JE, Filion F, Campbell-Yeo M, Goulet C, Bell L, et al. Maternal touch and talk for invasive procedures in infants and toddlers in the pediatric intensive care unit. J Pediatr Nurs. (2012) 27(2):144–53. doi: 10.1016/j.pedn.2010.12.016
39. Efendi D, Caswini N, Rustina Y, Iskandar RATP. Combination of mother therapeutic touch (MTT) and maternal voice stimulus (MVS) therapies stabilize sleep and physiological function in preterm infants receiving minor invasive procedures. J Neonat Nurs. (2018) 24(6):318–24. doi: 10.1016/j.jnn.2018.08.001
40. Chen Y, Li Y, Sun J, Han D, Feng S, Zhang X. The effect of maternal voice on venipuncture induced pain in neonates: a randomized study. Pain Manag Nurs. (2021) 22(5):668–73. doi: 10.1016/j.pmn.2021.01.002
41. Chirico G, Cabano R, Villa G, Bigogno A, Ardesi M, Dioni E. Randomised study showed that recorded maternal voices reduced pain in preterm infants undergoing heel lance procedures in a neonatal intensive care unit. Acta Paediatr. (2017) 106(10):1564–8. doi: 10.1111/apa.13944
42. Filippa M, Monaci MG, Spagnuolo C, Di Benedetto M, Serravalle P, Grandjean D. Oxytocin levels increase and anxiety decreases in mothers who sing and talk to their premature infants during a painful procedure. Children. (2023) 10(2):334. doi: 10.3390/children10020334
43. Filippa M, Monaci MG, Spagnuolo C, Serravalle P, Daniele R, Grandjean D. Maternal speech decreases pain scores and increases oxytocin levels in preterm infants during painful procedures. Sci Rep. (2021) 11(1):17301. doi: 10.1038/s41598-021-96840-4
44. Rossi A, Molinaro A, Savi E, Micheletti S, Galli J, Chirico G, et al. Music reduces pain perception in healthy newborns: a comparison between different music tracks and recoded heartbeat. Early Hum Dev. (2018) 124:7–10. doi: 10.1016/j.earlhumdev.2018.07.006
45. Rand K, Lahav A. Maternal sounds elicit lower heart rate in preterm newborns in the first month of life. Early Hum Dev. (2014) 90(10):679–83. doi: 10.1016/j.earlhumdev.2014.07.016
46. Kucuk Alemdar D, Guducu Tufekc IF. Effects of maternal heart sounds on pain and comfort during aspiration in preterm infants. Jpn J Nurs Sci. (2018) 15(4):330–9. doi: 10.1111/jjns.12202
47. Alemdar DK, Özdemir FK. Effects of covering the eyes versus playing intrauterine sounds on premature Infants’ pain and physiological parameters during venipuncture. J Pediatr Nurs. (2017) 37:e30–6. doi: 10.1016/j.pedn.2017.06.016
48. Yarahmadi S, Pouralizadeh M, Atrkarroushan Z, Shahroudi P. The effect of the simulated intrauterine sound on behavioral and physiological indices of pain during capillary blood sampling for screening preterm infants: a randomized clinical trial study. BMC Pediatr. (2024) 24(1):110. doi: 10.1186/s12887-024-04604-6
49. Ullsten A, Pölkki T, Ghetti CM. Parents as nurturing resources: a family integrated approach to music therapy for neonatal procedural support. Music Med. (2021) 12(2):98–111. doi: 10.47513/mmd.v13i2.796
50. Hartley KA, Miller CS, Gephart SM. Facilitated tucking to reduce pain in neonates: evidence for best practice. Adv Neonatal Care. (2015) 15(3):201–8. doi: 10.1097/ANC.0000000000000193
51. Axelin A, Salantera S, Lehtonen L. “Facilitated tucking by parents” in pain management of preterm infants-a randomized crossover trial. Early Hum Dev. (2006) 82(4):241–7. doi: 10.1016/j.earlhumdev.2005.09.012
52. Bembich S, Cont G, Causin E, Paviotti G, Marzari P, Demarini S. Infant analgesia with a combination of breast milk, glucose, or maternal holding. Pediatrics. (2018) 142(3):e20173416. doi: 10.1542/peds.2017-3416
53. Nist MD, Robinson A, Harrison TM, Pickler RH. An integrative review of clinician-administered comforting touch interventions and acute stress responses of preterm infants. J Pediatr Nurs. (2022) 67:e113–22. doi: 10.1016/j.pedn.2022.08.020
54. Parashar P, Samuel AJ, Bansal A, Aranka VP. Yakson touch as a part of early intervention in the neonatal intensive care unit: a systematic narrative review. Indian J Crit Care Med. (2016) 20(6):349–52. doi: 10.4103/0972-5229.183897
55. Magor NRE, Ads SEM, Elhalafawy SEH. Effectiveness of nesting positioning and Yakson touch on physiological, behavioral state and pain caused by blood sampling procedures in preterm neonates. J Neonat Nurs. (2024). doi: 10.1016/j.jnn.2024.02.004
56. Fitri SYR, Lusmilasari L, Juffrie M, Bellieni CV. Modified sensory stimulation using breastmilk for reducing pain intensity in neonates in Indonesia: a randomized controlled trial. J Pediatr Nurs. (2020) 53:e199–203. doi: 10.1016/j.pedn.2020.04.004
57. Locatelli C, Bellieni CV. Sensorial saturation and neonatal pain: a review. J Matern Fetal Neonatal Med. (2018) 31(23):3209–13. doi: 10.1080/14767058.2017.1366983
58. Liu J, Fang S, Wang Y, Gao L, Xin T, Liu Y. The effectiveness of massage interventions on procedural pain in neonates: a systematic review and meta-analysis. Medicine. (2022) 101(41):e30939. doi: 10.1097/MD.0000000000030939
59. Yamada J, Bueno M, Santos L, Haliburton S, Campbell-Yeo M, Stevens B. Sucrose analgesia for heel-lance procedures in neonates. Cochrane Database Syst Rev. (2023) 8(8):CD014806. doi: 10.1002/14651858.CD014806
60. Oliveira DJD, Medeiros KS, Sarmento ACA, Oliveira FJD, Costa APF, Souza NL, et al. Use of glucose for pain management in premature neonates: a systematic review and meta-analysis protocol. BMJ Open. (2021) 11(12):e052901. doi: 10.1136/bmjopen-2021-052901
61. Bueno M, Yamada J, Harrison D, Khan S, Ohlsson A, Adams-Webber T, et al. A systematic review and meta-analyses of nonsucrose sweet solutions for pain relief in neonates. Pain Res Manag. (2013) 18(3):153–61. doi: 10.1155/2013/956549
62. Isik U, Ozek E, Bilgen H, Cebeci D. Comparison of oral glucose and sucrose solutions on pain response in neonates. J Pain. (2000) 1(4):275–8. doi: 10.1054/jpai.2000.8919
63. Stevens B, Yamada J, Campbell-Yeo M, Gibbins S, Harrison D, Dionne K, et al. The minimally effective dose of sucrose for procedural pain relief in neonates: a randomized controlled trial. BMC Pediatr. (2018) 18(1):85. doi: 10.1186/s12887-018-1026-x
64. Gao H, Li M, Gao H, Xu G, Li F, Zhou J, et al. Effect of non-nutritive sucking and sucrose alone and in combination for repeated procedural pain in preterm infants: a randomized controlled trial. Int J Nurs Stud. (2018) 83:25–33. doi: 10.1016/j.ijnurstu.2018.04.006
65. Campbell-Yeo M, Johnston CC, Benoit B, Disher T, Caddell K, Vincer M, et al. Sustained efficacy of Kangaroo care for repeated painful procedures over neonatal intensive care unit hospitalization: a single-blind randomized controlled trial. Pain. (2019) 160(11):2580–8. doi: 10.1097/j.pain.0000000000001646
66. Beebe B, Steele M. How does microanalysis of mother-infant communication inform maternal sensitivity and infant attachment? Attach Hum Dev. (2013) 15(5-6):583–602. doi: 10.1080/14616734.2013.841050
67. Ullsten A, Eriksson M, Klässbo M, Volgsten U. Singing, sharing, soothing—biopsychosocial rationales for parental infant-directed singing in neonatal pain management:a theoretical approach. Music & Science. (2018) 1:2059204318780841. doi: 10.1177/2059204318780841
68. Melzack R. From the gate to the neuromatrix. Pain. (1999) (Suppl 6):S121–S6. doi: 10.1016/S0304-3959(99)00145-1
69. Melzack R, Wall PD. Pain mechanisms: a new theory. Science. (1965) 150(3699):971–9. doi: 10.1126/science.150.3699.971
70. Moseley GL. A pain neuromatrix approach to patients with chronic pain. Man Ther. (2003) 8(3):130–40. doi: 10.1016/S1356-689X(03)00051-1
71. Moseley GL. Distorted body image in complex regional pain syndrome. Neurology. (2005) 65(5):773. doi: 10.1212/01.wnl.0000174515.07205.11
72. Trout KK. The neuromatrix theory of pain: implications for selected nonpharmacologic methods of pain relief for labor. J Midwifery Womens Health. (2004) 49(6):482–8. doi: 10.1016/j.jmwh.2004.07.009
73. Goksan S, Baxter L, Moultrie F, Duff E, Hathway G, Hartley C, et al. The influence of the descending pain modulatory system on infant pain-related brain activity. Elife. (2018) 7:e37125. doi: 10.7554/eLife.37125
74. Goksan S, Hartley C, Emery F, Cockrill N, Poorun R, Moultrie F, et al. fMRI reveals neural activity overlap between adult and infant pain. eLife. (2015) 4:e06356. doi: 10.7554/eLife.06356
75. Duff EP, Moultrie F, van der Vaart M, Goksan S, Abos A, Fitzgibbon SP, et al. Inferring pain experience in infants using quantitative whole-brain functional MRI signatures: a cross-sectional, observational study. Lancet Digit Health. (2020) 2(9):e458–e67. doi: 10.1016/S2589-7500(20)30168-0
76. Gates A, Shave K, Featherstone R, Buckreus K, Ali S, Scott SD, et al. Procedural pain: systematic review of parent experiences and information needs. Clin Pediatr. (2018) 57(6):672–88. doi: 10.1177/0009922817733694
77. Anand KJ, Hall RW. Love, pain, and intensive care. Pediatrics. (2008) 121(4):825–7. doi: 10.1542/peds.2007-3828
78. McNair C. Enhancing Parental Role in Managing Pain in Neonates (Doctoral dissertation). Canada: University of Toronto (2023).
79. Muirhead R, Kynoch K, Peacock A, Birch P, Lewis PA. Developing a model of neonatal nurse-controlled analgesia: a delphi study. J Adv Nurs. (2023):1–10. doi: 10.1111/jan.15972
80. Palomaa AK, Korhonen A, Polkki T. Factors influencing parental participation in neonatal pain alleviation. J Pediatr Nurs. (2016) 31(5):519–27. doi: 10.1016/j.pedn.2016.05.004
81. Pierrat V, Marchand-Martin L, Durrmeyer X, Vasante L, Burguet A, Cambonie G, et al. Perceived maternal information on premature infant’s pain during hospitalization: the French EPIPAGE-2 national cohort study. Pediatr Res. (2020) 87(1):153–62. doi: 10.1038/s41390-019-0422-8
82. Hassankhani H, Negarandeh R, Abbaszadeh M, Jabraeili M. The role of mothers during painful procedures on neonates: a focused ethnography. J Neonat Nurs. (2020) 26(6):340–3. doi: 10.1016/j.jnn.2020.03.002
83. Jyoti J, Laing S, Spence K, Griffiths N, Popat H. Parents’ perspectives on their baby’s pain management in a surgical neonatal intensive care unit: the parents’ awareness and involvement in pain management (PAIN-PAM) study—part 2. J Neonat Nurs. (2023) 29(6):839–45. doi: 10.1016/j.jnn.2023.06.007
84. Nejadghanat S, Neshat H, Jabraeili M, Mousavi S. Effect of educational booklet and role-playing on the mothers’ knowledge and self-efficacy in newborn pain management: a quasi-experimental study. J Neonat Nurs. (2023) 30(2):171–5. doi: 10.1016/j.jnn.2023.08.005
85. Neshat H, Hassankhani H, Jabraeili M, Negarandeh R. Organisational challenges of pain management in neonatal intensive care unit: a qualitative study. BMJ Open. (2023) 13(9):e072695. doi: 10.1136/bmjopen-2023-072695
86. Maki-Asiala M, Axelin A, Polkki T. Parents’ experiences with interprofessional collaboration in neonatal pain management: a descriptive qualitative study. J Clin Nurs. (2023) 32(21-22):7860–72. doi: 10.1111/jocn.16857
87. McNair C, Chirinian N, Uleryk E, Stevens B, McAllister M, Franck LS, et al. Effectiveness of parental education about pain in the neonatal period on knowledge, attitudes, and practices: a systematic review and meta-analysis. Paediatr Child Health. (2022) 27(8):454–63. doi: 10.1093/pch/pxac050
88. Ponthier L, Ensuque P, Guigonis V, Bedu A, Bahans C, Teynie F, et al. Parental presence during painful or invasive procedures in neonatology: a survey of healthcare professionals. Arch Pediatr. (2020) 27(7):362–7. doi: 10.1016/j.arcped.2020.06.011
89. Palomares Gonzalez L, Hernandez Caravaca I, Gomez Garcia CI, Sanchez-Solis de Querol M. Parental presence during invasive pediatric procedures: what does it depend on? Rev Lat Am Enfermagem. (2023) 31:e3828. doi: 10.1590/1518-8345.6101.3828
90. Rubinstein R, Akinnusi F, Ho J, Bose J, Khashu M, Gallagher K, et al. Neonatal staff perceptions and attitudes towards family integrated care and fathers: a multi-site survey. J Neonat Nurs. (2023). doi: 10.1016/j.jnn.2023.11.004
91. Marfurt-Russenberger K, Axelin A, Kesselring A, Franck LS, Cignacco E. The experiences of professionals regarding involvement of parents in neonatal pain management. J Obstet Gynecol Neonatal Nurs. (2016) 45(5):671–83. doi: 10.1016/j.jogn.2016.04.011
92. Lewis TP, Andrews KG, Shenberger E, Betancourt TS, Fink G, Pereira S, et al. Caregiving can be costly: a qualitative study of barriers and facilitators to conducting Kangaroo mother care in a US tertiary hospital neonatal intensive care unit. BMC Pregnancy Childbirth. (2019) 19(1):227. doi: 10.1186/s12884-019-2363-y
93. Treiman-Kiveste A, Polkki T, Kalda R, Kangasniemi M. Nurses’ perceptions of infants’ procedural pain assessment and alleviation with non-pharmacological methods in Estonia. J Pediatr Nurs. (2022) 62:e156–e63. doi: 10.1016/j.pedn.2021.09.006
94. Benoit B, Campbell-Yeo M, Johnston C, Latimer M, Caddell K, Orr T. Staff nurse utilization of Kangaroo care as an intervention for procedural pain in preterm infants. Adv Neonatal Care. (2016) 16(3):229–38. doi: 10.1097/ANC.0000000000000262
95. Kjellsdotter A, Lantz B, Ottosson C. Healthcare professionals’ views on parental participation in the neonatal intensive care units. J Pediatr Nurs. (2017) 41:3–8. doi: 10.1016/j.pedn.2017.09.008
96. Gallagher K, Franck L. Ten lessons from 10 years of research into parental involvement in infant pain management. Infant. (2012) 8(3):78–80.
97. Pölkki T, Korhonen A, Laukkala H. Nurses’ perceptions of pain assessment and management practices in neonates: a cross-sectional survey. Scand J Caring Sci. (2017) 32(2):725–33. doi: 10.1111/scs.12503
98. Latimer MA, Johnston CC, Ritchie JA, Clarke SP, Gilin D. Factors affecting delivery of evidence-based procedural pain care in hospitalized neonates. J Obstet Gynecol Neonatal Nurs. (2009) 38(2):182–94. doi: 10.1111/j.1552-6909.2009.01007.x
99. Axelin A, Anderzen-Carlsson A, Eriksson M, Polkki T, Korhonen A, Franck LS. Neonatal intensive care nurses’ perceptions of parental participation in infant pain management: a comparative focus group study. J Perinat Neonatal Nurs. (2015) 29(4):363–74. doi: 10.1097/JPN.0000000000000136
100. Lehtonen L, Axelin A. Medical champions can make a difference in initiating culture change. Acta Paediatr. (2016) 105(9):994–5. doi: 10.1111/apa.13482
101. McNair C, Chinian N, Shah V, McAllister M, Franck LS, Stevens B, et al. Metasynthesis of factors that influence parents’ participation in pain management for their infants in the NICU. J Obstet Gynecol Neonatal Nurs. (2020) 49(3):263–71. doi: 10.1016/j.jogn.2020.02.007
102. van Veenendaal NR, Auxier JN, van der Schoor SRD, Franck LS, Stelwagen MA, de Groof F, et al. Development and psychometric evaluation of the CO-PARTNER tool for collaboration and parent participation in neonatal care. PLoS One. (2021) 16(6):e0252074. doi: 10.1371/journal.pone.0252074
103. Christensen J, Fatchett D. Promoting parental use of distraction and relaxation in pediatric oncology patients during invasive procedures. J Pediatr Oncol Nurs. (2002) 19(4):127–32. doi: 10.1177/104345420201900404
104. Corlett J, Twycross A. Negotiation of parental roles within family-centred care: a review of the research. J Clin Nurs. (2006) 15(10):1308–16. doi: 10.1111/j.1365-2702.2006.01407.x
105. Parvez E, Stinson J, Boon H, Goldman J, Shah V, Taddio A. Mothers’ beliefs about analgesia during childhood immunization. Paediatr Child Health. (2010) 15(5):289–93. doi: 10.1093/pch/15.5.289
106. Taddio A, Manley J, Potash L, Ipp M, Sgro M, Shah V. Routine immunization practices: use of topical anesthetics and oral analgesics. Pediatrics. (2007) 120(3):e637–43. doi: 10.1542/peds.2006-3351
107. Franck LS, Oulton K, Nderitu S, Lim M, Fang S, Kaiser A. Parent involvement in pain management for NICU infants: a randomized controlled trial. Pediatrics. (2011) 128(3):510–8. doi: 10.1542/peds.2011-0272
108. Bueno M, Nogueira Costa R, de Camargo PP, Costa T, Harrison D. Evaluation of a parent-targeted video in Portuguese to improve pain management practices in neonates. J Clin Nurs. (2017) 27(5-6):1153–9. doi: 10.1111/jocn.14147
109. Campbell-Yeo M, Dol J, Disher T, Benoit B, Chambers CT, Sheffield K, et al. The power of a parent’s touch: evaluation of reach and impact of a targeted evidence-based YouTube video. J Perinat Neonatal Nurs. (2017) 31(4):341–9. doi: 10.1097/JPN.0000000000000263
110. Brodsgaard A, Pedersen JT, Larsen P, Weis J. Parents’ and nurses’ experiences of partnership in neonatal intensive care units: a qualitative review and meta-synthesis. J Clin Nurs. (2019) 28(17-18):3117–39. doi: 10.1111/jocn.14920
111. Orr T, Campbell-Yeo M, Benoit B, Hewitt B, Stinson J, McGrath P. Smartphone and internet preferences of parents: information needs and desired involvement in infant care and pain management in the NICU. Adv Neonatal Care. (2017) 17(2):131–8. doi: 10.1097/ANC.0000000000000349
112. Monaghan J, Kim T, Dol J, Orovec A, Campbell-Yeo M. Parents’ learning needs and preferences in a neonatal intensive care unit: a desire for enhanced communication and eHealth technology. J Neonat Nurs. (2020) 26(2):101–5. doi: 10.1016/j.jnn.2019.09.001
113. Dol J, Richardson B, Boates T, Campbell-Yeo M. Learning to parent from google? Evaluation of available online health evidence for parents of preterm infants requiring neonatal intensive care. Health Informatics J. (2019) 25(4):1265–77. doi: 10.1177/1460458217752564
114. Richardson B, Benoit B, Rutledge K, Dol J, Misener RM, Latimer M, et al. The impact of parent-targeted eHealth educational interventions on infant procedural pain management: a systematic review protocol. JBI Database System Rev Implement Rep. (2019) 17(8):1589–99. doi: 10.11124/JBISRIR-D-19-00007
115. Richardson BHN, Benoit B, Rutledge K, Dol J, Martin-Misener R, Latimer M, et al. Impact of parent-targeted eHealth educational interventions on infant procedural pain management: a systematic review. JBI Evid Synth. (2023) 21(4):669–712. doi: 10.11124/JBIES-21-00435
116. Korki de Candido L, Harrison D, Ramallo Veríssimo MDLÓ, Bueno M. Effectiveness of a parent-targeted video on neonatal pain management: nonrandomized pragmatic trial. Paediatr Neonatal Pain. (2020) 2(3):74–81. doi: 10.1002/pne2.12023
117. Larocque C, Venegas CL, Dunn S, Campbell-Yeo M, Gilmore L, Harrold J, et al. Exploring implementation processes of a parent-targeted educational video for improving newborn pain treatment: a sequential exploratory mixed-methods study. J Child Health Care. (2023):13674935231176888. doi: 10.1177/13674935231176888
118. Olsson E, Carlsen Misic M, Dovland Andersen R, Ericson J, Eriksson M, Thernstrom Blomqvist Y, et al. Study protocol: parents as pain management in Swedish neonatal care—SWEpap, a multi-center randomized controlled trial. BMC Pediatr. (2020) 20(1):474. doi: 10.1186/s12887-020-02356-7
119. Cobo MM, Moultrie F, Hauck AGV, Crankshaw D, Monk V, Hartley C, et al. Multicentre, randomised controlled trial to investigate the effects of parental touch on relieving acute procedural pain in neonates (petal). BMJ Open. (2022) 12(7):e061841. doi: 10.1136/bmjopen-2022-061841
120. van der Vaart M, Hauck AGV, Mansfield R, Adams E, Bhatt A, Cobo MM, et al. Parental experience of neonatal pain research while participating in the parental touch trial (petal). Pain. (2024). doi: 10.1097/j.pain.0000000000003177
121. Chorna OD, Slaughter JC, Wang L, Stark AR, Maitre NL. A pacifier-activated music player with mother’s voice improves oral feeding in preterm infants. Pediatrics. (2014) 133(3):462–8. doi: 10.1542/peds.2013-2547
122. Standley JM, Cassidy J, Grant R, Cevasco A, Szuch C, Nguyen J, et al. The effect of music reinforcement for non-nutritive sucking on nipple feeding of premature infants. Pediatr Nurs. (2010) 36(3):138–45.20687305
123. Holsti L, MacLean K, Oberlander T, Synnes A, Brant R. Calmer: a robot for managing acute pain effectively in preterm infants in the neonatal intensive care unit. Pain Rep. (2019) 4(2):e727. doi: 10.1097/PR9.0000000000000727
124. Chen W, Oetomo SB, Tetteroo D, Versteegh F, Mamagkaki T, Pereira MS, et al. Mimo pillow–an intelligent cushion designed with maternal heart beat vibrations for comforting newborn infants. IEEE J Biomed Health Inform. (2015) 19(3):979–85. doi: 10.1109/JBHI.2014.2349153
125. Ullsten A, Eriksson M, Axelin A. O parent, where art thou? Paediatr Neonatal Pain. (2019) 1(2):53–5. doi: 10.1002/pne2.12010
127. Eccleston C, Fisher E, Howard RF, Slater R, Forgeron P, Palermo TM, et al. Delivering transformative action in paediatric pain: a lancet child & adolescent health commission. Lancet Child Adolesc Health. (2021) 5(1):47–87. doi: 10.1016/S2352-4642(20)30277-7
Keywords: parent, newborn, infant, neonate, procedural pain, pain management, family-centered
Citation: Ullsten A, Campbell-Yeo M and Eriksson M (2024) Parent-led neonatal pain management—a narrative review and update of research and practices. Front. Pain Res. 5:1375868. doi: 10.3389/fpain.2024.1375868
Received: 24 January 2024; Accepted: 2 April 2024;
Published: 16 April 2024.
Edited by:
Anthony Herbert, Queensland University of Technology, AustraliaReviewed by:
Lorenzo Fabrizi, University College London, United KingdomPoh-Heng Chong, HCA Hospice Care, Singapore
Mary Ghazawy, Townsville University Hospital, Australia
© 2024 Ullsten, Campbell-Yeo and Eriksson. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mats Eriksson bWF0cy5oLmVyaWtzc29uQG9ydS5zZQ==
 Alexandra Ullsten
Alexandra Ullsten Marsha Campbell-Yeo
Marsha Campbell-Yeo Mats Eriksson
Mats Eriksson