- 1Pain Rehabilitation Program, Mary Free Bed Rehabilitation Hospital, Grand Rapids, MI, United States
- 2College of Human Medicine, Michigan State University, Grand Rapids, MI, United States
Objectives: Sexual satisfaction is an important aspect of quality of life. Chronic pain, depression and anxiety, and relational problems correspond with higher risk for sexual difficulties. Less is known about how risk factors for sexual dysfunction and other problems—such as medical conditions, pain severity, and medication side effects—affect the sexual satisfaction of people with chronic pain. Using a biopsychosocial framework, this study explored factors related to sexual satisfaction among patients presenting for evaluation of chronic pain.
Methods: Researchers used a hierarchical multiple regression analysis to model potential predictors of sexual satisfaction. Variables analyzed were demographic features, medical history, average pain severity, depressed mood, anxiety, and perceived significant other support. Data collection involved administration of retrospective questionnaires and chart review. The sample included male and female participants (N = 134) presenting for evaluation at a multidisciplinary pain rehabilitation clinic.
Results: Medical history (i.e., medical conditions, surgical history, and medications) and clinical self-report variables (i.e., pain severity, depressed mood, anxiety, and perceived significant other support) were associated with sexual satisfaction. In this sample, antidepressant use and higher pain severity were unique predictors of lower sexual satisfaction. Married marital status and higher levels of perceived significant other support were predictive of greater sexual satisfaction.
Discussion: Findings highlight the importance of understanding the unique impact of biopsychosocial variables on the sexual satisfaction of patients presenting for evaluation at a multidisciplinary pain rehabilitation clinic. Further exploration of protective factors that account for sexual satisfaction among individuals with chronic pain may help inform screening, referrals, and treatment.
Introduction
Sexual satisfaction is an important facet of overall quality of life in adults (1) and is strongly linked to relationship satisfaction (2, 3), physical health (1, 3, 4), mental health, and sexual functioning (3, 4). Sexual satisfaction depends on interactions among biological, psychological, and sociocultural factors (5). Chronic pain affects individuals across these domains (6). Chronic pain and sexual problems are also subjectively related. Of patients having completed a multidisciplinary pain rehabilitation program, 51.5% were shown to have 1 or more areas of sexual dysfunction, and 73% perceived these difficulties as “very much” or “somewhat” related to chronic pain (7). Sexual difficulties like sexual dysfunction and dissatisfaction are common and frequently co-occur with chronic pain. Research tends to focus on the prevalence of such sexual difficulties amid chronic pain. This paper contributes to a growing field of literature that considers biopsychosocial factors that predict sexual satisfaction among patients seeking treatment for chronic pain.
Background
Individuals with chronic pain often have complex medical histories including multiple medical comorbidities [e.g., (8)]. Pain intensity is associated with increased sexual difficulties (9), and may be influenced by comorbid medical conditions. Chronic comorbid medical conditions may also have effects on sexual function due to symptoms, sequelae, and/or required medications associated with the disease. This can be the case with inflammatory bowel diseases like Crohn's disease (10), diabetes mellitus (11), epilepsy (12), cardiovascular and respiratory conditions (13, 14), and hepatic, urinary, and reproductive health conditions (15–17).
Addressing both biological and psychiatric risk factors for sexual difficulties among chronic pain patients can be complicated. On the biological level, the human sexual response entails coordination of numerous systems (e.g., cardiovascular, hormonal). Compromised functioning of these systems can affect libido, orgasm, and arousal-based responses and thus cause sexual dysfunction. Psychiatric problems such as depression and anxiety are prevalent and frequently comorbid with chronic pain. Stress, depression, and anxiety are known individual risk factors of sexual difficulties among people with chronic pain (18–20). Psychosocial and cultural influences may affect how individuals cope with medical (21) and psychiatric (22, 23) conditions, thereby affecting sexual function and perceptions of satisfaction.
Sexual dysfunction is a prominent side effect of certain first-line medications for common medical and psychiatric conditions as well as chronic pain. For instance, anticonvulsants (e.g., gabapentin) and antidepressants [e.g., tricyclics, specific serotonin, and serotonin-norepinephrine reuptake inhibitors (SSRIs, SNRIs)] are widely prescribed for chronic pain conditions (24). Antidepressants, anticonvulsants (25), antihypertensives (26), and long-term opiate use (27) have been linked to iatrogenic sexual dysfunction. Surgeries have also evidenced increased risk of sexual dysfunction (11, 28) and may alter or impede sexual engagement with partners.
Relationship factors are particularly relevant when investigating sexual satisfaction. Couples tend to report both reduced sexual and relational satisfaction associated with the onset of chronic pain (29). Conversely, relationship dissatisfaction may act as a long-term contributor to sexual difficulties amid chronic pain (18). Sexual difficulties have been found to predict relationship dissatisfaction among women with chronic pain and vice versa (22). Research has shown that preferences for social support correlate with pain-related disability (30). Perceived significant other support is particularly important for sexual wellbeing (22, 31) but has received less attention in treatment and the relevant literature.
Limitations of research on sexual satisfaction include both limited consideration of biological factors and exclusion of male participants (3). Few studies have examined specific predictors for sexual dissatisfaction in a clinically heterogenous sample of patients with non-malignant chronic pain [e.g., (32)]. However, many studies center a single condition that may be known to be associated with sexual difficulties, such as pelvic pain (33). Sexual satisfaction and chronic pain are complex, biopsychosocial experiences, and there is a deficit in clinical pain-related research that considers all these levels of experience simultaneously (6). This research is needed to elucidate the intricate relationships between sexual satisfaction and chronic pain, which could promote exploration of possible mechanisms of change and inform clinical interventions from a biopsychosocial framework.
The aim of this study was to examine predictors of sexual satisfaction among male and female individuals presenting for chronic pain evaluation. Based on prior research, the following variables were identified as potential risk factors: medical conditions, past surgeries, medication use, and endorsed anxiety and depression. Researchers hypothesized that lower levels of perceived support from significant others and higher levels of pain severity would be associated with higher levels of sexual dissatisfaction. These hypotheses were informed by an earlier study with preliminary data (34).
Materials and methods
Participants and recruitment
This study included retrospective data from both patient self-report questionnaires and chart review. Participants included 134 adults meeting the following inclusion criteria: (1) provided informed consent for study participation, (2) ≥18 years of age, (3) were presenting for a pain psychology evaluation at a multidisciplinary pain rehabilitation clinic, and (4) reported that they were sexually active within the past 30 days. Eligible patients included those seeking treatment at a 10- to 12- week chronic pain rehabilitation program, or seeking pain psychology services alone. Details of the multidisciplinary pain rehabilitation program have been previously described (35). Eligibility criteria are consistent with past studies on sexual function using similar samples (7, 36).
A total of 508 individuals were potentially eligible to participate in this study, 269 (53.0%) of whom consented to participate. Of those who consented, 247 completed measures related to sexual functioning, and 137 endorsed being sexually active. Three participants were excluded due to insufficient chart data to assess medical risk factors (n = 2) or ineligibility due to a presenting problem aside from pain (n = 1).
The Mary Free Bed (MFB) institutional review board (IRB) approved data collection encompassing use of patient self-report questionnaires and retrospective patient chart review. Participants were recruited using an electronic prompt following completion of electronic questionnaires given routinely at evaluation in a multidisciplinary pain rehabilitation clinic. Patients who completed the informed consent form were granted access to research questionnaires including information about sexual health and perceived social support. Patients who endorsed sexual activity alone or with partner(s) within the past 30 days were invited to answer additional questions about their sexual satisfaction during that period. Researchers conducted a patient chart review using electronic medical records of survey participants who were eligible for inclusion in analyses.
Measures
Measures included self-reported pain severity, anxiety, depression, sexual functioning, and perceived social support and patient chart review. Researchers tested measure reliability using Cronbach's alpha coefficient. All measures had good internal consistency.
Self-report questionnaires
Average pain severity
For the last 30 days, patients rated their average pain severity on a single-item, 11-point numeric scale ranging from 0 to 10. Numeric rating scales for pain have relatively good reliability (37), responsiveness, and ease of use (38). Higher scores suggest higher pain severity.
Anxiety
For the last 7 days, patients rated their anxiety symptoms using the Patient-Reported Outcomes Measurement Information System (PROMIS) Anxiety—Short Form 8a, an 8-item measure with item scales ranging from 1 (never) to 5 (always). Examples of items include “I felt anxious” and “My worries overwhelmed me.” This form has good validity and responsivity (39). For this and other PROMIS measures used in this study, raw total scores were converted to a T-distribution, with a mean (M) of 50 and standard deviation (SD) of 10. Higher t-scores are associated with higher anxiety symptom severity. Internal consistency (Cronbach's α) was high for the current sample (α = .95).
Depression
For the last 7 days, patients rated their depressive symptoms using the PROMIS Depression—Short Form 8a, an 8-item measure with item scales ranging from 1 (never) to 5 (always). Examples of items include “I felt depressed” and “I felt hopeless.” This form has strong validity and reliability (40) and moderate responsivity (41). Higher t-scores suggest higher depression symptom severity. Internal consistency was high (α = .95).
Sexual functioning
To assess domains of sexual wellbeing, the PROMIS Sexual Function and Satisfaction (SexFS) Version 2.0 (v2.0) was used. The PROMIS SexFS v.2.0 has strong validity and reliability (42). Examples of sexual activity assessed by this measure include sexual intercourse, masturbation, and oral sex. For the purposes of this study, satisfaction with one's sex life was used as the primary outcome variable (i.e., Global Satisfaction with Sex Life).
Female sexual function and satisfaction
Female participants completed the Brief Profile Sexual Function and Satisfaction (Female) 2.0. For the past 30 days, female patients rated their overall sexual function and satisfaction on a total 14 items. For the current study, only the Global Satisfaction with Sex Life subscale was used (2 items). Higher scores suggest higher satisfaction with sexual experiences. Internal consistency for this subscale was high in this study (α = .92).
Male sexual function and satisfaction
Male participants also received a sex-specific measure, the Brief Profile Sexual Function and Satisfaction (Male) 2.0, which pertains to sexual function and satisfaction over the past 30 days. This measure consists of 10 items. Only the 2-item Global Satisfaction with Sex Life subscale was used in this study. Internal consistency was high (α = .89).
Social support
The Multidimensional Scale of Perceived Social Support (MSPSS) (43) was used, which was designed to assess perceived social support. The MSPSS has good reliability, validity, and factor structure across multiple populations, including adults and psychiatric patients (44). Previous research has demonstrated a 3-factor structure consistent with its three distinctive subscales, indicative of perceived support from Family, Friends, and a Significant Other (45), respectively. The current study examined only the Significant Other subscale. Examples of items include “There is a special person in my life who cares about my feelings.”
Chart review
The lead author developed a chart review method and trained and oversaw research assistants to ensure integrity of the chart review process. Information sources encompassed medical and pain psychology evaluations, scanned intake paperwork, and relevant chart documentation (e.g., referral forms, problem lists) as appropriate. Risk factors of interest were identified based on literature review. These factors included medications, past surgeries, and number and type of major medical co-morbidities. Demographic information regarding sex, relationship status (e.g., single, married), and living situation (e.g., living with spouse) were also obtained. Please refer to Table 1 for full list of chart review variables. Research assistants logged ambiguous items. To ensure information fidelity, the lead author conducted a secondary review of all charts marked as incomplete, inconsistent, or complex. Chart reviewers also noted conditions that they believed should be considered for statistical analyses, which the lead author reviewed and checked for relevancy. Subsequently, the lead author used a random number generator to select 18 out of 134 (13.43%) charts to assess interrater reliability. Each chart contained 23 categorical or numeric results, totaling 414 response items. Two items were found to have a different result by reviewer, suggesting 99.5% interrater agreement.
Data analytic strategy
The primary analysis for this study included a hierarchical multiple regression analysis to identify predictors of sexual satisfaction. Categorical variables were coded dichotomously prior to analyses. Sample size was determined appropriate to the analysis for testing individual predictors. Evaluation of statistical assumptions revealed no concerns with multicollinearity after assessing tolerance and variance inflation factors. Demographic features (i.e., age, sex, marital status) were entered in the first step of the analysis to account for variance attributed to these variables. Medical conditions (i.e., cardiac, urological/reproductive, gastrointestinal, respiratory, diabetic, hepatic, and neurological conditions and past surgeries) were entered in the second step; specifically, researchers examined the presence/absence of each medical condition category and total number of medical conditions. Finally, self-reported pain severity, depressed mood, anxiety, and perceived significant other support were entered in the third step. Significance was evaluated using a criterion of p < .05. Analyses were conducted using IBM SPSS version 28. A preliminary analysis was presented (46).
Results
Participant demographic characteristics
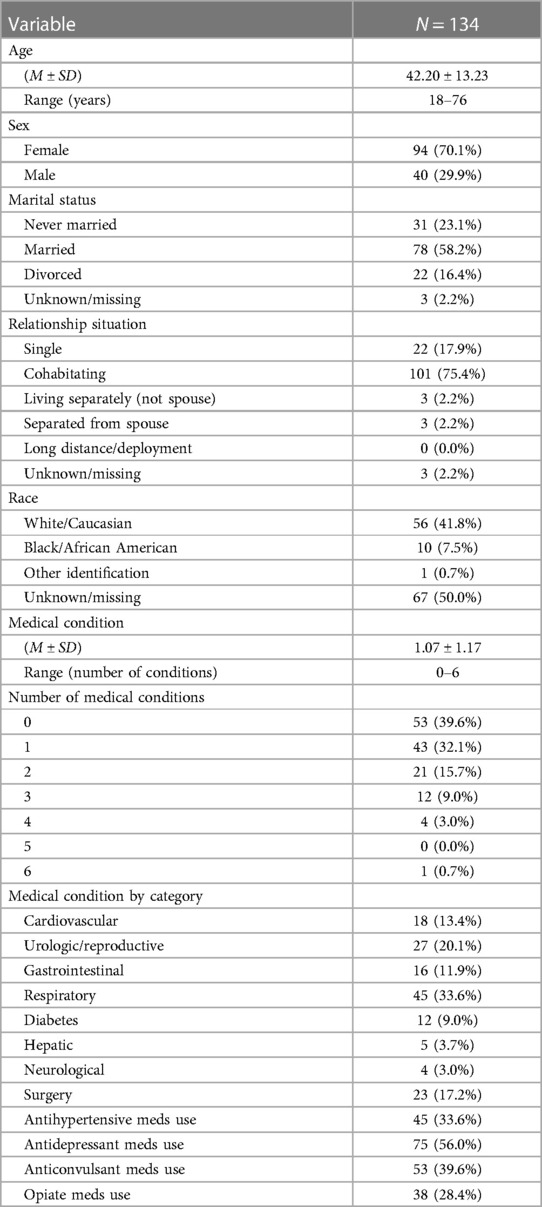
Participant age ranged from 18 to 76 years, with an average of 42.20 ± 13.23. Ninety-four individuals (70.1%) had female sex listed in their medical record, and the remaining 40 (29.9%) were listed as male. Regarding marital status, 78 (58.2%) participants identified as married, 31 (23.1%) as never married, and 22 (16.4%) as divorced. Most participants endorsed cohabitating with a significant other (n = 101, 75.4%) or single status (n = 22, 17.9%). Three (2.2%) participants identified as living separately from a partner (not a spouse), and another 3 (2.2%) indicated being separated from a spouse, respectively. No participants identified as having a long-distance relationship or a significant other deployed due to military service. Three (2.2%) responses to items about marital status and relationship situation were missing. Authors had racial identification information for half the sample, consisting of 67 patients (50%). Of this subsample, 56 (41.8%) were White/Caucasian, 10 (7.5%) were Black/African American, and 1 (0.7%) identified as another race. Table 1 summarizes demographic and clinical characteristics of this sample.
Medical conditions and medication use
Of the full sample, 81 (60.4%) participants were found to have at least one major medical condition. The average number of major medical conditions was 1.07 ± 1.17, with a range of 0–6. In brief, 45 (33.6%) of participants had a respiratory condition, with asthma being the most common. Urologic/reproductive conditions were the second most common listed problem, affecting 27 (20.1%) participants. Additionally, 23 (17.2%) participants had had at least 1 surgery affecting urologic/reproductive health, with hysterectomy being predominant procedure documented. Less frequent conditions included major cardiovascular/cardiac conditions (n = 18, 13.4%), diabetes (n = 12, 9.0%), gastrointestinal conditions (n = 16, 11.9%), hepatic conditions (n = 5, 3.7%), and epilepsy or other listed major neurological issue (n = 4, 3.0%). Supplemental Materials show specific medical conditions by frequency and medications included in these analyses.
Regarding antidepressant use, 62 (46.3%) of participants had one prescription listed, and another 9.7% had more than one antidepressant category documented (e.g., SSRI, SNRI). Anticonvulsants were the second most common prescribed drug class, with 53 (39.6%) participants having at least one prescription. Antihypertensive drugs were third most common, with 45 (33.6%) of participants having at least one prescription listed, and 17 (12.7%) of the total sample had multiple hypertensive drugs prescribed for concurrent use. Over one-in-four patients (n = 38, 28.4%) had a current prescription for opiates.
Self-report measures
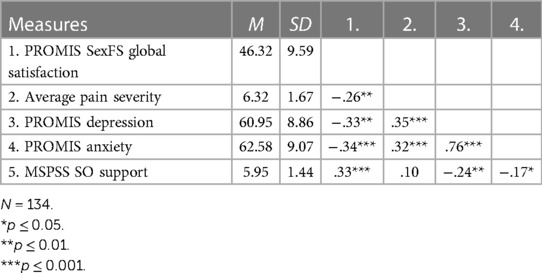
On the PROMIS Global Satisfaction with Sex Life subscale, the average t-score among female and male participants was 46.32 ± 9.59, with a range of 30.67–65.60. These data suggest that most patients indicated some sexual dissatisfaction, with 20.1% participants (n = 27) obtaining scores indicative of clinical levels of sexual dissatisfaction indicated by a score 1 SD below the mean (i.e., ≤40 T). Participants’ average depression rating was 60.95 ± 8.86, ranging from 37.1 ± 81.1, and average anxiety ratings were 62.58 ± 9.07, ranging from 37.10 to 83.00. These scores suggest participant endorsement of recent depression and anxiety symptom ranging from within normal limits (i.e., ≤55 T) up to severe (i.e., ≥70 T), with average ratings falling in the moderate range. Patients’ ratings of average pain ranged from 1 to 10, with an average of 6.32 ± 1.67. Average ratings on the MSPSS significant other subscale were 5.95 ± 1.44, with a range of 1–7. Correlations among measures are included in Table 2.
Predictors of sexual satisfaction
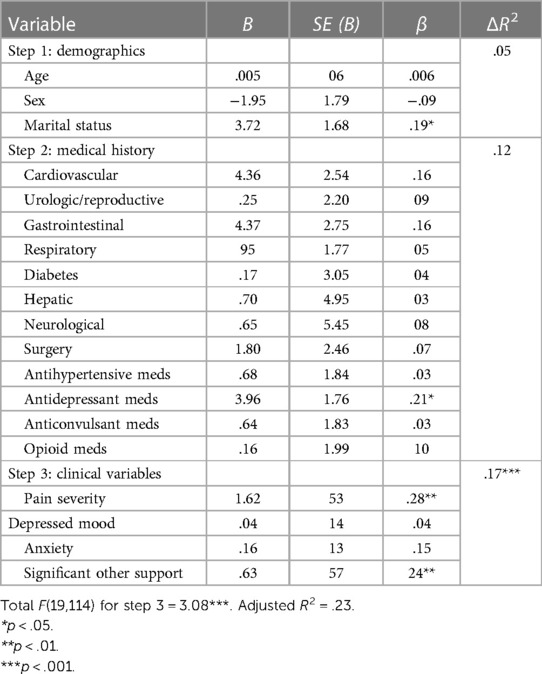
Results of the multiple hierarchical regression indicated that demographic variables (i.e., age, sex, marital status) accounted for 2.3% of the variance in the prediction of sexual satisfaction scores, F(3,130) = 2.05 p = .11. Medical history variables (i.e., medical conditions, surgical history, and medications) were entered on the next step. The addition of these variables added another 12.4% of accounted variance, F(15,118) = 1.60, p = .09. In the final step, clinical self-report variables were entered (i.e., pain severity, depressed mood, anxiety, significant other support), adding another 17.1% of explained variance, F(19,114) = 3.09, p < .001. Once all variables were entered, the final model accounted for 23.0% of the variance in sexual satisfaction scores. In the final model, the final variables were significant unique predictors of sexual satisfaction: marital status (β = .17, p = .04), antidepressant medication (β = −.19, p = .03), pain severity (β = −.28, p = .003), and perceived significant other support (β = .25, p = .01). Note that the direction of the relationships suggests that being married and having higher levels of significant other support was related to increased sexual satisfaction, whereas being on an antidepressant medication and having higher pain levels was associated with lower levels of sexual satisfaction. See Table 3.
Discussion
The aim of this study was to identify predictors of sexual satisfaction among sexually active patients presenting for a pain psychology evaluation in a multidisciplinary pain rehabilitation clinic setting. Findings demonstrated that antidepressant use and higher pain severity were unique predictors of lower sexual satisfaction. Being married and having greater levels of perceived significant other support were predictive of higher sexual satisfaction. These results demonstrate the significance of both biological and psychosocial risk factors for this aspect of sexual health among individuals presenting for evaluation of chronic pain. Consistent with prior literature, concurrent major medical conditions and elevated anxiety and depressive symptoms were common in this study population (10, 18, 19); however, these were not unique predictors of sexual satisfaction after controlling for other variables.
Antidepressant use stood out as an independent predictor among medical conditions, surgical history, and medications, jointly accounting for 12.1% of the variance in sexual satisfaction in this sample. This finding is remarkable given the high prevalence of antidepressant use in this sample (i.e., 46.3%), in contrast to 13.2% of US adults reporting use in the general community (47). This finding illustrates the importance of clinical assessment and education about the potential side effect profiles of antidepressants when prescribing them for pain control and/or psychiatric reasons in chronic pain populations. Notably, the prevalence of co-occurring medical and psychiatric conditions and polypharmacy may complicate approaches of offsetting sexual side effects (e.g., adjunctive medications) when working with patients with chronic pain.
As hypothesized, average pain intensity predicted sexual dissatisfaction. It is well established that pain severity is associated with risk for sexual difficulties in individuals with chronic pain. It is uncertain how effective pain treatment is for addressing multifactorial sexual dissatisfaction. Some research has demonstrated that reducing pain intensity is associated with improvements in sexual functioning (29). When pain is the primary problem affecting sexual activity, as may be the case in vulvodynia, pain reductions associated with medications have been shown to improve overall sexual function (48). A biopsychosocial approach involving a multidisciplinary pain rehabilitation team may best address concurrent chronic pain and sexual dissatisfaction in some cases.
Yet, best practices remain unclear. One study found that an interdisciplinary pain rehabilitation program (IPRP) resulted in self-reported improvement in sexual functioning for women with pelvic pain (49), while another suggested that an IPRP may be insufficient to improve sexual functioning in a sample of patients with heterogeneous pain conditions (7), despite prior evidence that IPRPs yield clinically significant reductions in pain and emotional distress [e.g., (50)]. Education and group interventions specific to sexual functioning have shown promising results (51). More research is needed to tailor sexual health interventions to individuals and relationships affected by chronic pain in multidisciplinary pain rehabilitation treatment settings.
This study shows an association between perceived significant other support and sexual satisfaction. Findings demonstrate that perceived significant other support may be associated with less emotional distress and more sexual satisfaction among individuals with chronic pain, regardless of pain severity. Prior studies demonstrated that less perceived support in a marriage is associated with more pain-related catastrophizing in individuals with long-term pain (31), and factors like empathic accuracy may be relevant to individuals’ evaluation of significant other support (52). How perceived significant other support relates to other relevant constructs, including relationship satisfaction [e.g., (32)], is not well understood. Overall, this study lends support to the view that relational factors and sexual satisfaction are critical to consider conjointly and adds to the literature in this area. Future research investigating significant other support, relationship satisfaction, and other partner dynamics is needed to elucidate the mechanisms that account for their association with sexual difficulties in populations with chronic pain.
In this study, marital status was a significant independent predictor of sexual satisfaction. Results are consistent with another study including a probability sample representative of the US adult population (n = 3,159) that found nonmarried women and men had significantly higher odds of sexual dysfunction when compared to married individuals (53). Most married participants in our sample identified as cohabitating with a spouse. This arrangement likely yields increased availability of a familiar sexual partner. Of note, the timing of this study corresponded with the ongoing COVID-19 pandemic, which may have affected partner availability, sexual behaviors, and sexual satisfaction for some [see (54, 55)]. Understanding reasons for sexual inactivity—whether due to personal preference, pain-related disability, etc.—would add valuable context to this study. It follows that research examining the prevalence of and reasons for sexual inactivity in a similar population may help interpret our findings.
More research using a strengths-based approach to sexual satisfaction among people with chronic pain would also be valuable. Prior research using similar samples found that participants presenting for this multidisciplinary pain rehabilitation clinic differed regarding primary presenting concern and program type (e.g., fibromyalgia, headache, complex regional pain syndrome, pain psychology only) (36). Most patients who completed a multidisciplinary pain rehabilitation program endorsed one or more areas of sexual dysfunction (7). Yet, 4 out of 5 patients in this sample did not report clinical levels of sexual dissatisfaction. This discrepancy suggests the existence of significant protective factors against sexual dissatisfaction amidst sexual dysfunction and various types of chronic pain. Our findings demonstrate that perceived significant other support may be one of those important protective factors.
Regarding sexual satisfaction, more research is needed to understand how patients seeking evaluation in a multidisciplinary pain rehabilitation clinic may differ from one another and the general population. Few studies have used the PROMIS SexFS to compare clinical and nonclinical populations [e.g., (56)]. Nonetheless, previous research has found that sexual satisfaction is linked to individual, partner, and relationship factors in the general community (57). This aligns with our findings that antidepressant use, marital status, and perceived significant other support are significant to sexual satisfaction in this sample. Comparing community samples with clinical pain populations may help clarify how pain intensity relates to these variables.
Age and sex were not independent predictors of sexual satisfaction in this sample. Yet, previous research has found gender, sex, and age relevant to sexual difficulties among individuals with chronic pain. In one study, lower sexual satisfaction was associated with higher pain severity, pain-related life interference, depression, and anxiety in female but not male participants (36). Another study found that women who reported higher depression, less relationship satisfaction, and older age reported lower sexual function, whereas age was the only significant correlate for sexual function in men (32). The current study included more biological variables than these investigations. Findings highlight the importance of accounting for biological, psychological, and social variables simultaneously while investigating demographic differences in sexual satisfaction among individuals with chronic pain.
Further research is needed to explore differences in sexual satisfaction among patients with diverse backgrounds seeking evaluation at a multidisciplinary pain rehabilitation clinic. Gender role expectations negatively affect pain perception and the quality of pain treatment for women (58). Race- and size-based oppression are correlated with higher pain intensity (59). How transgender and nonbinary patients with chronic pain define and achieve sexual satisfaction may differ from cisgender patients (60). Sexual orientation should be assessed in research given evidence of between-group differences in sexual satisfaction (61) and reported pain prevalence (62). Understanding the needs and experiences of marginalized and oppressed people can help address healthcare and pain disparities [e.g., (63–65)].
Strengths and limitations
Strengths of this study include consideration of specific patient medical conditions, surgeries, and drug classes, which helps to inform understanding of the prevalence and complex relationships between these variables and sexual satisfaction in a sample of patients presenting for evaluation of chronic pain. This research also adds to the chronic pain literature considering individual psychological (i.e., depression, anxiety), pain-related (i.e., average pain severity) and relationship factors (i.e., marital status, relationship situation, significant other support) in the context of sexual satisfaction of individual chronic pain patients. These factors, most of which are subjective, accounted for more variance (i.e., 16.9%) than listed problems and medications in patients’ medical charts. Results highlight the importance of psychosocial variables regarding sexual satisfaction and suggest helpful directions for future research using a biopsychosocial approach to chronic pain and sexual satisfaction.
This study has several limitations. First, study generalizability is limited by characteristics of sample size and patient demographic characteristics (i.e., most were White/Caucasian, female, married, and all resided in the Midwestern United States). Unfortunately, race/ethnicity information was missing from 50% of the charts analyzed. Medications, specific pain conditions, and psychological conditions associated with increased odds of sexual dysfunction (e.g., antipsychotic drugs, serotonin antagonists and reuptake inhibitors) were not considered due to sample size. Relevant medication factors, including dosage and length of time of use, were also not considered for this reason. Because antihypertensive agents were a factor of interest in this study, hypertension itself was not analyzed as a potential risk factor due to the likely interaction of these variables; however, hypertension is known to contribute to sexual dysfunction (4).
These limitations may be addressed in future research to increase understanding of how these variables may relate to sexual satisfaction in patients with chronic pain. In addition, causality in these relationships cannot be established based on current findings, nor do these results rule-out the possibility of mediator or moderator variables. Future research examining the process by which marital status, perceived significant other support, antidepressant use, and pain intensity relate to sexual satisfaction would be a valuable addition to the literature in this area.
Conclusions
Researchers conducted this study to investigate biopsychosocial variables accounting for sexual satisfaction among sexually active adult patients presenting for evaluation at a multidisciplinary pain rehabilitation clinic. About 1 in 5 participants obtained scores in the clinical range of sexual dissatisfaction. Relationship factors, antidepressant use, and pain intensity accounted for more variance in sexual satisfaction than noted comorbid medical issues. Findings highlight the importance of a biopsychosocial approach to research, clinical screening, and interventions to promote sexual satisfaction among patients with chronic pain presenting for evaluation. More research is needed to understand how best to address patient sexual dissatisfaction in a multidisciplinary pain rehabilitation clinic setting while accounting for the risk factors highlighted in this study. Research exploring how diversity factors and experiences of societal oppression relate to sexual satisfaction amidst chronic pain may be particularly valuable given known healthcare and pain disparities. Strengths-based research focused on factors such as perceived significant other support may also be helpful in gaining a comprehensive understanding of sexual satisfaction among individuals with chronic pain.
Data availability statement
The datasets presented in this article are not readily available because of the nature of the research. Where applicable, raw, anonymized data that support the findings of this study may be available from co-author Dr. JC, by reasonable request. Requests to access the datasets should be directed toanVsaWEuY3JhbmVyQG1hcnlmcmVlYmVkLmNvbQ==.
Ethics statement
The studies involving humans were approved by Mary Free Bed (MFB) Research Institutional Review Board (IRB). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
AB: Writing – original draft, Writing – review & editing. KM: Writing – original draft, Writing – review & editing. LF: Writing – original draft, Writing – review & editing. EA: Writing – original draft, Writing – review & editing. KK: Writing – original draft, Writing – review & editing. JC: Methodology, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
Authors extend warm thanks to Sarah Kim for assistance with chart review and data collection and to Dr. Jory Catalpa for writing suggestions.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpain.2024.1375546/full#supplementary-material
References
1. Flynn KE, Lin L, Bruner DW, Cyranowski JM, Hahn EA, Jeffery DD, et al. Sexual satisfaction and the importance of sexual health to quality of life throughout the life course of U. S. adults. J Sex Med. (2016) 13(11):1642–50. doi: 10.1016/j.jsxm.2016.08.011
2. McNulty JK, Wenner CA, Fisher TD. Longitudinal associations among relationship satisfaction, sexual satisfaction, and frequency of sex in early marriage. Arch Sex Behav. (2016) 45(1):85–97. doi: 10.1007/s10508-014-0444-6
3. Rausch D, Rettenberger M. Predictors of sexual satisfaction in women: a systematic review. Sex Med Rev. (2021) 9(3):365–80. doi: 10.1016/j.sxmr.2021.01.001
4. Althof SE, Buvat J, Gutkin SW, Belger M, Stothard DR, Fugl-Meyer AR. Sexual satisfaction in men with erectile dysfunction: correlates and potential predictors. J Sex Med. (2010) 7(1 Pt 1):203–15. doi: 10.1111/j.1743-6109.2009.01554.x
5. Carpenter LM, Nathanson CA, Kim YJ. Physical women, emotional men: gender and sexual satisfaction in midlife. Arch Sex Behav. (2009) 38(1):87–107. doi: 10.1007/s10508-007-9215-y
6. Martínez-Borba V, Ripoll-Server P, Yakobov E, Suso-Ribera C. Predicting the physical and mental health status of individuals with chronic musculoskeletal pain from a biopsychosocial perspective: a multivariate approach. Clin J Pain. (2021) 37(3):211–8. doi: 10.1097/AJP.0000000000000913
7. Flegge LG, Barr A, Craner JR. Interdisciplinary pain rehabilitation and sexual functioning: treatment outcomes and patient preferences. Pain Pract. (2023) 23(7):785–92. doi: 10.1111/papr.13257
8. Foley HE, Knight JC, Ploughman M, Asghari S, Audas R. Association of chronic pain with comorbidities and health care utilization: a retrospective cohort study using health administrative data. Pain. (2021) 162(11):2737–49. doi: 10.1097/j.pain.0000000000002264
9. Katz H, Newton-John TRO, Shires A. Sexual difficulties in the population with musculoskeletal chronic pain: a systematic review. Pain Med. (2021) 22(9):1982–92. doi: 10.1093/pm/pnaa451
10. Eluri S, Cross RK, Martin C, Weinfurt KP, Flynn KE, Long MD, et al. Inflammatory bowel diseases can adversely impact domains of sexual function such as satisfaction with sex life. Dig Dis Sci. (2018) 63(6):1572–82. doi: 10.1007/s10620-018-5021-8
11. McCabe MP, Sharlip ID, Lewis R, Atalla E, Balon R, Fisher AD, et al. Risk factors for sexual dysfunction among women and men: a consensus statement from the fourth international consultation on sexual medicine 2015. J Sex Med. (2016) 13(2):153–67. doi: 10.1016/j.jsxm.2015.12.015
12. Zhao S, Tang Z, Xie Q, Wang J, Luo L, Liu Y, et al. Association between epilepsy and risk of sexual dysfunction: a meta-analysis. Seizure. (2019) 65:80–8. doi: 10.1016/j.seizure.2019.01.004
13. Nascimento ER, Maia AC, Pereira V, Soares-Filho G, Nardi AE, Silva AC. Sexual dysfunction and cardiovascular diseases: a systematic review of prevalence. Clinics. (2013) 68(11):1462–8. doi: 10.6061/clinics/2013(11)13
14. Reda M, Ruby D. Female sexual dysfunction among a sample of Egyptian patients with asthma. Open Respir Med J. (2020) 14:38–44. doi: 10.2174/1874306402014010038
15. Hawksworth DJ, Burnett AL. Nonalcoholic fatty liver disease, male sexual dysfunction, and infertility: common links, common problems. Sex Med Rev. (2020) 8(2):274–85. doi: 10.1016/j.sxmr.2019.01.002
16. Tonyali S, Yilmaz M. Sexual dysfunction in interstitial cystitis. Curr Urol. (2017) 11(1):1–3. doi: 10.1159/000447186
17. Abrams P, Kelleher CJ, Kerr LA, Rogers RG. Overactive bladder significantly affects quality of life. Am J Manag Care. (2000) 6(11 Suppl):S580–90.11183901
18. Burri A, Lachance G, Williams FM. Prevalence and risk factors of sexual problems and sexual distress in a sample of women suffering from chronic widespread pain. J Sex Med. (2014) 11(11):2772–84. doi: 10.1111/jsm.12651
19. Ghajarzadeh M, Jalilian R, Togha M, Azimi A, Hosseini P, Babaei N. Depression, poor sleep, and sexual dysfunction in migraineurs women. Int J Prev Med. (2014) 5(9):1113–8.25317293
20. Yılmaz R, Karpuz S, Akdere E, Yılmaz H. Evaluation of sexual dysfunction in females with neck and upper back myofascial pain syndrome: a cross-sectional study. Rheumatol Int. (2023) 43(9):1723–32. doi: 10.1007/s00296-023-05359-6
21. Fábregas BC, Moura AS, Avila RE, Faria MN, Carmo RA, Teixeira AL. Sexual dysfunction and dissatisfaction in chronic hepatitis C patients. Rev Soc Bras Med Trop. (2014) 47(5):564–72. doi: 10.1590/0037-8682-0147-2014
22. Cano A, Weisberg JN, Gallagher RM. Marital satisfaction and pain severity mediate the association between negative spouse responses to pain and depressive symptoms in a chronic pain patient sample. Pain Med. (2000) 1(1):35–43. doi: 10.1046/j.1526-4637.2000.99100.x
23. Richmond NL, Meyer ML, Hollowell AG, Isenberg EE, Domeier RM, Swor RA, et al. Social support and pain outcomes after trauma exposure among older adults: a multicenter longitudinal study. Clin J Pain. (2018) 34(4):366–74. doi: 10.1097/AJP.0000000000000545
24. Deli G, Bosnyak E, Pusch G, Komoly S, Feher G. Diabetic neuropathies: diagnosis and management. Neuroendocrinology. (2013) 98(4):267–80. doi: 10.1159/000358728
25. Kaufman KR, Struck PJ. Gabapentin-induced sexual dysfunction. Epilepsy Behav. (2011) 21(3):324–6. doi: 10.1016/j.yebeh.2011.04.058
26. Buch-Vicente B, Acosta JM, Martin-Oterino JA, Prieto N, Sanchez-Sanchez ME, Galindo-Villardon P, et al. Frequency of iatrogenic sexual dysfunction associated with antihypertensive compounds. J Clin Med. (2021) 10(22):5214. doi: 10.3390/jcm10225214
27. Deyo RA, Von Korff M, Duhrkoop D. Opioids for low back pain. Br Med J. (2015) 350:g6380. doi: 10.1136/bmj.g6380
28. Tal R, Alphs HH, Krebs P, Nelson CJ, Mulhall JP. Erectile function recovery rate after radical prostatectomy: a meta-analysis. J Sex Med. (2009) 6(9):2538–46. doi: 10.1111/j.1743-6109.2009.01351.x
29. Kwan KS, Roberts LJ, Swalm DM. Sexual dysfunction and chronic pain: the role of psychological variables and impact on quality of life. Eur J Pain. (2005) 9(6):643–52. doi: 10.1016/j.ejpain.2004.12.008
30. McWilliams LA, Higgins KS, Dick BD, Verrier MJ. A longitudinal investigation of pain-related social support preferences in a chronic pain treatment sample. Clin J Pain. (2014) 30(8):672–8. doi: 10.1097/01.ajp.0000435446.89019.f3
31. Cano A. Pain catastrophizing and social support in married individuals with chronic pain: the moderating role of pain duration. Pain. (2004) 110(3):656–64. doi: 10.1016/j.pain.2004.05.004
32. Finn E, Morrison TG, McGuire BE. Correlates of sexual functioning and relationship satisfaction among men and women experiencing chronic pain. Pain Med. (2018) 19(5):942–54. doi: 10.1093/pm/pnx056
33. Davis SN, Bergeron S, Bois K, Sadikaj G, Binik YM, Steben M. A prospective 2-year examination of cognitive and behavioral correlates of provoked vestibulodynia outcomes. Clin J Pain. (2015) 31(4):333–41. doi: 10.1097/AJP.0000000000000128
34. Barr AC, Flegge LG, Craner JR. Predictors of Sexual Dissatisfaction in Patients with Chronic Pain. Minneapolis, MN: American Psychological Association Annual Convention (2022).
35. Craner JR, Lake ES, Bancroft KA, George LL. Treatment outcomes and mechanisms for an act-based 10-week interdisciplinary chronic pain rehabilitation program. Pain Pract. (2020) 20(1):44–54. doi: 10.1111/papr.12824
36. Flegge LG, Barr A, Craner JR. Sexual functioning among adults with chronic pain: prevalence and association with pain-related outcomes. Pain Med. (2023) 24(2):197–206. doi: 10.1093/pm/pnac117
37. Kahl C, Cleland JA. Visual analogue scale, numeric pain rating scale and the McGill pain questionnaire: an overview of psychometric properties. Phys Ther Rev. (2005) 10(2):123–28. doi: 10.1179/108331905X55776
38. Hjermstad MJ, Fayers PM, Haugen DF, Caraceni A, Hanks GW, Loge JH, et al. European palliative care research C. Studies comparing numerical rating scales, verbal rating scales, and visual analogue scales for assessment of pain intensity in adults: a systematic literature review. J Pain Symptom Manage. (2011) 41(6):1073–93. doi: 10.1016/j.jpainsymman.2010.08.016
39. Schalet BD, Pilkonis PA, Yu L, Dodds N, Johnston KL, Yount S, et al. Clinical validity of PROMIS depression, anxiety, and anger across diverse clinical samples. J Clin Epidemiol. (2016) 73:119–27. doi: 10.1016/j.jclinepi.2015.08.036
40. Pilkonis PA, Yu L, Dodds NE, Johnston KL, Maihoefer CC, Lawrence SM. Validation of the depression item bank from the patient-reported outcomes measurement information system (PROMIS) in a three-month observational study. J Psychiatr Res. (2014) 56:112–9. doi: 10.1016/j.jpsychires.2014.05.010
41. Lee AC, Driban JB, Price LL, Harvey WF, Rodday AM, Wang C. Responsiveness and minimally important differences for 4 patient-reported outcomes measurement information system short forms: physical function, pain interference, depression, and anxiety in knee osteoarthritis. J Pain. (2017) 18(9):1096–110. doi: 10.1016/j.jpain.2017.05.001
42. Weinfurt KP, Lin L, Bruner DW, Cyranowski JM, Dombeck CB, Hahn EA, et al. Development and initial validation of the PROMIS sexual function and satisfaction measures version 2.0. J Sex Med. (2015) 12(9):1961–74. doi: 10.1111/jsm.12966
43. Zimet GD, Dahlem NW, Zimet SG, Farley GK. The multidimensional scale of perceived social support. J Pers Assess. (1988) 52(1):30–41. doi: 10.1207/s15327752jpa5201_2
44. Cecil H, Stanley MA, Carrion PG, Swann A. Psychometric properties of the MSPSS and NOS in psychiatric outpatients. J Clin Psychol. (1995) 51(5):593–602. doi: 10.1002/1097-4679(199509)51:5%3C593::AID-JCLP2270510503%3E3.0.CO;2-W
45. Clara IP, Cox BJ, Enns MW, Murray LT, Torgrudc LJ. Confirmatory factor analysis of the multidimensional scale of perceived social support in clinically distressed and student samples. J Pers Assess. (2003) 81(3):265–70. doi: 10.1207/S15327752JPA8103_09
46. Barr AC, Kim S, Atsaphanthong E, Flegge LG, Moore KK, Craner J. Biopsychosocial Risk Factors for Sexual Dissatisfaction among Patients with Chronic Pain. Chicago, IL: Midwest Pain Society (2022).
47. Brody DJ, Gu Q. Antidepressant use among adults: united States, 2015–2018. NCHS Data Brief. (2020) (377):1–8. 33054926.33054926
48. Bachmann GA, Brown CS, Phillips NA, Rawlinson LA, Yu X, Wood R, et al. Effect of gabapentin on sexual function in vulvodynia: a randomized, placebo-controlled trial. Am J Obstet Gynecol. (2019) 220(1):89.e 1–89.8. doi: 10.1016/j.ajog.2018.10.021
49. Aboussouan AB, Mandell D, Johnson J, Thompson N, Huffman KL. An interdisciplinary chronic pain rehabilitation program effectively treats impairment in sexual function, depression, alexithymia, and pain in women with chronic pelvic pain. J Psychosom Obstet Gynaecol. (2021) 42(4):261–71. doi: 10.1080/0167482X.2020.1735341
50. Craner JR, Flegge LG, Lake ES, Perra AEA. Patients with clinically elevated depressive symptoms report improvements in mood, pain, and functioning following participation in interdisciplinary pain rehabilitation. Pain Med. (2022) 23(2):362–74. doi: 10.1093/pm/pnab242
51. Breton A, Miller CM, Fisher K. Enhancing the sexual function of women living with chronic pain: a cognitive-behavioural treatment group. Pain Res Manag. (2008) 13(3):219–24. doi: 10.1155/2008/369382
52. Leonard MT, Issner JH, Cano A, Williams AM. Correlates of spousal empathic accuracy for pain-related thoughts and feelings. Clin J Pain. (2013) 29(4):324–33. doi: 10.1097/AJP.0b013e3182527bfd
53. Laumann EO, Paik A, Rosen RC. Sexual dysfunction in the United States: prevalence and predictors. JAMA. (1999) 281(6):537–44. doi: 10.1001/jama.281.6.537
54. Rogowska AM, Wójcik N, Janik A, Klimala P. Is there a direct link between sexual satisfaction and restrictions during the second wave of the COVID-19 pandemic? Int J Environ Res Public Health. (2022) 19(13):7769. doi: 10.3390/ijerph19137769
55. Qaderi K, Yazdkhasti M, Zangeneh S, Behbahani BM, Kalhor M, Shamsabadi A, et al. Changes in sexual activities, function, and satisfaction during the COVID-19 pandemic era: a systematic review and meta-analysis. Sex Med. (2023) 11(2):qfad005. doi: 10.1093/sexmed/qfad005
56. Hovén E, Flynn KE, Weinfurt KP, Eriksson LE, Wettergren L. Psychometric evaluation of the Swedish version of the PROMIS sexual function and satisfaction measures in clinical and nonclinical young adult populations. Sex Med. (2023) 11(1):qfac006. doi: 10.1093/sexmed/qfac006
57. Velten J, Margraf J. Satisfaction guaranteed? How individual, partner, and relationship factors impact sexual satisfaction within partnerships. PLoS One. (2017) 12(2):e0172855. doi: 10.1371/journal.pone.0172855
58. Samulowitz A, Gremyr I, Eriksson E, Hensing G. “Brave men” and “emotional women”: a theory-guided literature review on gender bias in health care and gendered norms towards patients with chronic pain. Pain Res Manag. (2018) 2018:6358624. doi: 10.1155/2018/6358624
59. Merriwether EN, Wittleder S, Cho G, Bogan E, Thomas R, Bostwick N, et al. Racial and weight discrimination associations with pain intensity and pain interference in an ethnically diverse sample of adults with obesity: a baseline analysis of the clustered randomized-controlled clinical trial the goals for eating and moving (GEM) study. BMC Public Health. (2021) 21(1):2201. doi: 10.1186/s12889-021-12199-1
60. Lindley L, Anzani A, Galupo MP. What constitutes sexual dissatisfaction for trans masculine and nonbinary individuals: a qualitative study. J Sex Marital Ther. (2020) 46(7):612–29. doi: 10.1080/0092623X.2020.1765924
61. Macedo A, Capela E, Peixoto M. Sexual satisfaction among lesbian and heterosexual cisgender women: a systematic review and meta-analysis. Healthcare (Basel). (2023) 11(12):1680. doi: 10.3390/healthcare11121680
62. Zajacova A, Grol-Prokopczyk H, Liu H, Reczek R, Nahin RL. Chronic pain among U.S. sexual minority adults who identify as gay, lesbian, bisexual, or “something else”. Pain. (2023) 164(9):1942–53. doi: 10.1097/j.pain.0000000000002891
63. Anderson KO, Green CR, Payne R. Racial and ethnic disparities in pain: causes and consequences of unequal care. J Pain. (2009) 10(12):1187–204. doi: 10.1016/j.jpain.2009.10.002
64. Choi HY, Graetz I, Shaban-Nejad A, Schwartzberg L, Vidal G, Davis RL, et al. Social disparities of pain and pain intensity among women diagnosed with early stage breast cancer. Front Oncol. (2022) 12:759272. doi: 10.3389/fonc.2022.759272
Keywords: chronic pain, sexual satisfaction, biopsychosocial, antidepressant agents, perceived social support
Citation: Barr A, Moore K, Flegge LG, Atsaphanthong E, Kirby KE and Craner JR (2024) Predictors of sexual satisfaction among patients with chronic pain. Front. Pain Res. 5:1375546. doi: 10.3389/fpain.2024.1375546
Received: 24 January 2024; Accepted: 18 March 2024;
Published: 4 April 2024.
Edited by:
Bernie Carter, Edge Hill University, United KingdomReviewed by:
Hayk Petrosyan, JFK Johnson Rehabilitation Institute, United StatesRamazan Yilmaz, Konya Beyhekim State Hospital, Türkiye
© 2024 Barr, Moore, Flegge, Atsaphanthong, Kirby and Craner. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Aex Barr YWV4LmNhaHVuQGdtYWlsLmNvbQ==
 Aex Barr
Aex Barr Kayla Moore1
Kayla Moore1 Lindsay G. Flegge
Lindsay G. Flegge Emily Atsaphanthong
Emily Atsaphanthong