- 1Department of Psychological Science, Loyola Marymount University, Los Angeles, CA, United States
- 2Graduate School of Education and Psychology, Pepperdine University, Malibu, CA, United States
- 3Department of Anesthesiology, Perioperative and Pain Medicine, Stanford University School of Medicine, Palo Alto, CA, United States
Background: Emerging adults, of whom significant numbers report chronic pain, are characterized as having unique needs and challenges. Psychological/behavioral treatments found to be beneficial for reducing pain outcomes in children and adults are understudied in emerging adults. Following a systematic review of the literature, our objective is to report on quantitative studies of psychological/behavioral interventions for chronic pain in emerging adults.
Method: We conducted a search of six databases (Cochrane Central Register of Controlled Trials, Google Scholar, ProQuest, PsycINFO, PubMed, and Web of Science) and reference sections in dissertations and systematic reviews to 4/29/2023. Keywords and phrases were search term combinations of “chronic/persistent pain”, “emerging/young adults,” and “intervention/treatment” using Boolean logic.
Results: Our review resulted in identifying 37 articles, of which 2 duplicates were removed, and 31 were further excluded by a screening process based on various inclusionary and exclusionary criteria. The search yielded four studies on psychological/behavioral interventions (yoga, acceptance and commitment therapy and relaxation), all of which positively affected the pain experience and/or pain-related outcomes. These studies presented issues in design such as not being blinded or randomized, having a small sample size, and potential confounds that were not reported or examined.
Discussion: The low number of studies reveals a large gap in the literature and is a call-to-action to further expand our understanding of effective and safer psychological/behavioral therapies for chronic pain in emerging adults. Successful pain management during this developmental phase may help young adults achieve positive trajectories for personal, occupational, relational, and health aspects of their lives.
1 Introduction
Development from the end of compulsory schooling (e.g., high school) to the onset of adult commitments (e.g., career) is known as emerging adulthood (18–29 years) (1). This stage is characterized by significant life transitions (1–3) in which personal, occupational, relational and health trajectories are determined (4, 5). Chronic pain is persistent pain lasting over 3 months (6). The impact of this type of pain on development and trajectories during emerging adulthood is not well understood. To our knowledge, there are no reviews of quantitative research on psychological/behavioral interventions in emerging adult samples with chronic pain.
Chronic pain affects a significant number of emerging adults, with prevalence rates ranging from 8.5% in the United States (7) to 11.6% worldwide (8), depending on sample and operational definitions of chronic pain (9). Several studies have found that prevalence rates for those attending university are higher compared to the general public. For example, 40% of university samples in Canada (10), 40.9% in Turkey (11), 54% in Norway (12) and 77.9% in Brazil (13) met criteria for chronic pain. In a recent systematic review of prevalence rates in university students, Serbic and colleagues concluded that the typical psychosocial stressors associated with college-life may exacerbate pre-existing chronic pain or even elevate the risk of chronic pain in individuals who were previously healthy (14). Depression and anxiety, higher in emerging adults compared to teens (12, 15), and in those who attend college vs. those who do not, are known associates of chronic pain (14). Stress and distress which are often experienced by typical college students, combined with perceptions of stigma and decreased help-seeking experienced by students with chronic pain may play a role in these enhanced prevalence rates (14).
Many college athletes experience chronic pain as a result of athletic injuries (16) and report higher levels of chronic pain and pain interference in their daily lives after college compared to their non-athlete alumni counterparts (17). Whereas pain perception in athletes is similar to that of non-athletes, in competitive situations, athletes may be less likely to report pain (18). However, outside of competition they are also more likely to seek help for pain than non-athletes (18) and may use different coping strategies compared to non-athletes (19). There is still much to be understood with regard to the elevated chronic pain rates in university students, whether they are athletes or not, and this cohort is in need of interventions for chronic pain.
Consequences of success or failure of pain management during emerging adulthood may be transformative. New freedoms associated with emerging adulthood may reduce positive physical and mental health outcomes in later adulthood (20, 21). Chronic pain can prevent emerging adults from achieving important goals and participating in experiences that might help them to become resilient over their pain, such as exercising and socializing (9, 22, 23). Alcohol, cannabis, and prescription opioid use and abuse escalates during this period (24–27). Mental illness/mood disorders are higher during emerging adulthood compared to adolescence, aged 12–17 years (28, 29), and co-occur more frequently with mental health problems during emerging adulthood than at other stages of development (30). Prescription opioids, self-medication, mental illness/mood disorders and substance abuse problems, relatively common and co-occurring, increase the risk of poor outcomes in adulthood for the emerging adult, whether they have chronic pain or not (29, 30). To better understand the complexity of chronic pain it is important to consider not only the biological factors involved, but psychological and social factors as well, currently integrated within a biopsychosocial model of health (31). Chronic pain affects relationships with peers, family, and medical professionals in ways that may have bidirectional effects on biopsychosocial and lifestyle factors (2, 9). Where persistent pain is linked to substance use/misuse, it can significantly impede psychosocial growth (32, 33).
Effective pain management during emerging adulthood helps to promote resilience and facilitate successfully taking on the roles and responsibilities of adulthood. Inadequate treatment of pain across age groups is a major risk factor for the development of persistent pain (34, 35). However, interventions that require a prescription and access to insurance are a barrier to healthcare in emerging adults, especially in the United States (5). Thus, many emerging adults with chronic pain report using non-pharmacological self-management/pain-coping strategies such as mindfulness meditation (36) and cognitive control (37), pharmacological substances such as cannabis (27, 38, 39), over-the counter (25) and non-prescribed medications (40, 41), as well as alcohol and tobacco (9). Nonmedical use of prescription opioids, reported by a third of a sample of high school seniors in the United States, is associated with worse outcomes in emerging adult years (41).
Pharmacological pain management during emerging adulthood may disrupt life trajectories in important ways that warrant further research. Opioid medications are the primary pharmacological treatment for this group, as they are for many others (25, 26, 42). However, opioid users report greater pain interference (negative effects on quality of life) than those not using opioids (25). Opioids also have serious side effects (43) that include an increase in the risk of hyperalgesia (heightened pain sensitivity) (44), and misuse/abuse disorders (38, 45).
While chronic pain poses significant challenges for emerging adults, it also presents unique opportunities for impacting life trajectories in positive ways. One of the characteristics of emerging adulthood is a sense of possibilities and optimism, where many potential futures await them (46). Nurturing habits can be learned during psychological/behavioral pain management, especially in college students, who presumably have easier and greater access to these types of services on campus (5).
There are several advantages of psychological/behavioral therapies relative to pharmacological treatments, including not necessarily requiring access to insurance/healthcare, a known difficulty for emerging adults (5). Although underreported in chronic pain patients, adverse events resulting from psychological/behavioral interventions are less serious than those from prescription medications (47). Interventions such as cognitive behavior therapy (CBT), acceptance and commitment therapy (ACT), mindfulness, and yoga have been shown to be effective for pain or pain-related outcomes in children and adults for some pain conditions (48–54). The most widely studied psychological/behavioral therapy, CBT, has been shown to potentially confer sustainable, healthy coping skills, even in self-administered (50) and single-session interventions (55, 56). Pain-related anxiety significantly and independently predicts opioid abuse problems in emerging adults (38), suggesting that evidence-based interventions targeting psychological factors of chronic pain may be especially effective. Interventions delivered via virtual reality (e.g., mindfulness) also show promise with younger children and older adults and appear to be quite effective for the management of anxiety (50).
2 Method
Because of the unique characteristics and needs of emerging adults, we sought studies that had explicitly examined a sample or performed sub-group analyses where the MAge ± 1 SD was within 18–29 years. Keywords and phrases included in our search of the English language literature used combinations of “chronic/persistent pain”, “emerging/young adults,” and “intervention/treatment” using Boolean logic. Only interventions that were psychological/behavioral are reported here. Electronic searches using Cochrane Central Register of Controlled Trials, Google Scholar, ProQuest, PsycINFO, PubMed, and Web of Science databases were conducted up to 4/29/2023. In addition, reference lists for studies, dissertations, and systematic reviews were examined for relevant references.
Eligible studies had to meet the following criteria: (1) Include young/emerging adults between 18 and 29 years of age with chronic pain as the primary population or a subgroup that was analyzed separately. If emerging adults were only a proportion of the sample for a study, or if the range was not provided, the study was included only if MAge ± 1 SD fell within the target range. The study needed to include participants who had recurrent, frequent episodic, persistent, or chronic pain, meeting International Association for the Study of Pain (IASP) requirements of pain lasting at least 3 months (6, 57). No attempt was made to include/exclude specific types of pain. (2) Clinical study of any design published in an academic journal (qualitative and quantitative studies, clinical trials). (3) Received treatment for chronic pain that included any psychological/behavioral non-pharmacological intervention, but not physical therapy, exercise, or pharmaceuticals (including cannabis/vitamins). (4) Include any pain measurement such as pain frequency, pain intensity, pain duration, pain interference and/or any pain-related outcomes with an empirically-validated relationship to pain such as analgesic use, sleep, pain-related quality of life, pain-condition symptoms and improvement [e.g., rheumatoid arthritis (RA) symptoms and RA symptoms improvement], mood, pain acceptance, fatigue, mindfulness, psychological distress, pain-related anxiety, or pain-related depression and (5) published in English.
Studies were excluded if they (1) described a majority of participants who were younger than 18 years, older than 29 years, or did not conduct separate analyses on emerging adults, (2) did not meet the criteria for chronic pain (≥3 months), (3) described a sample of emerging adults/university students learning about pain but not meeting criteria for chronic pain (e.g., as in a pain neuroscience education class), (4) none of the treatment groups received an intervention that was psychological/behavioral and (5) was primarily a prevalence or descriptive study without a treatment.
Two independent groups of undergraduate reviewers (two in each group) who were trained to 90% reliability (percent of agreement with expert reviewer for each review group) by one of the authors, screened articles at the title and abstract level. Articles where all of the criteria were met and/or those that the reviewers disagreed upon, were then screened by the senior authors (JF and MZ) and the reviewers discussed the full-text reports until consensus was reached.
3 Results
Search results up to 4/29/2023 using the above-mentioned search criteria included 37 articles. Of these, two duplicates and 31 studies not meeting our criteria for inclusion were removed by the two independent groups of reviewers who screened abstracts. Four articles were excluded after review of the full reports because they were outside our target age range, involved a survey but not treatments, and the interventions were not psychological/behavioral.
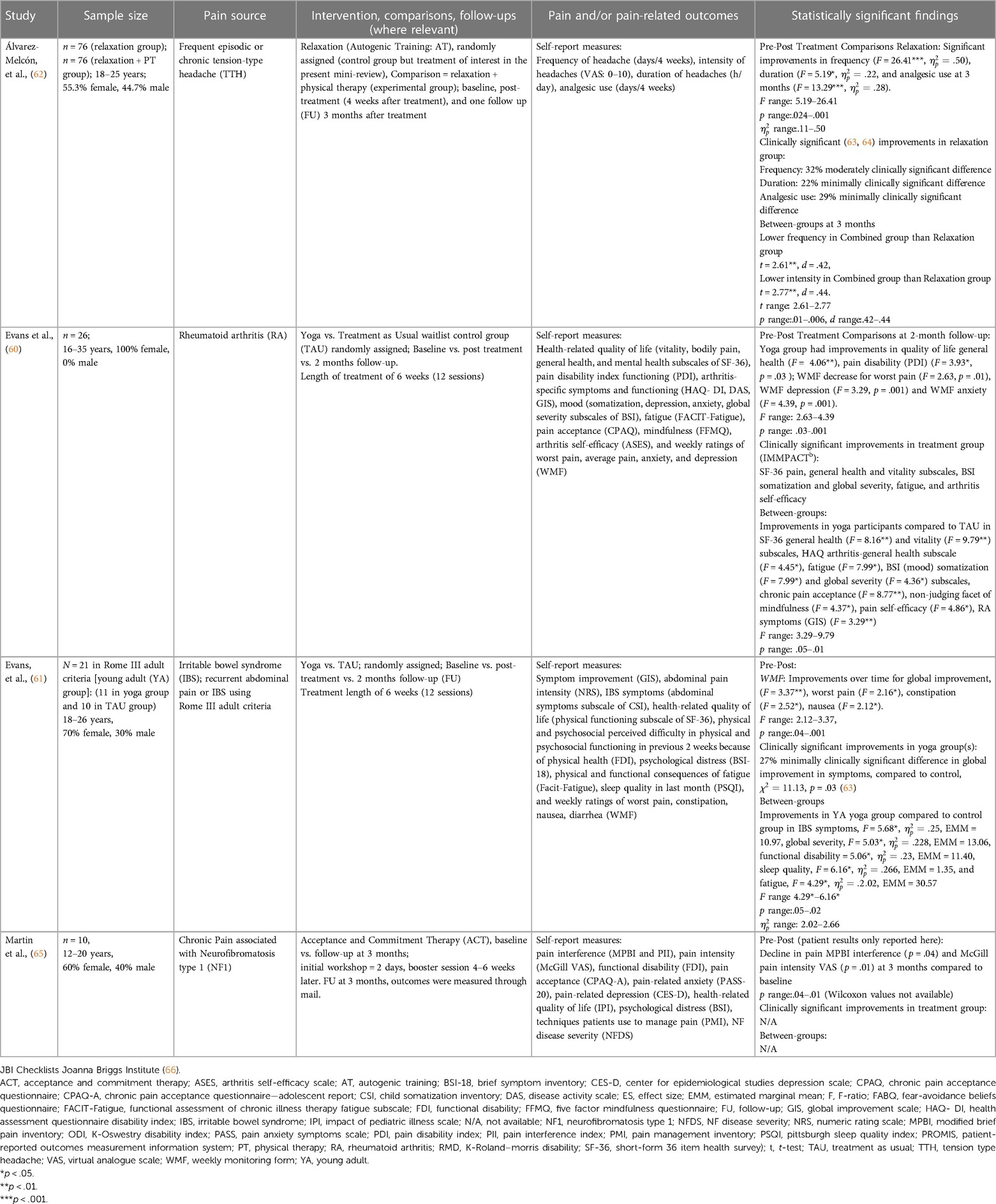
Four quantitative studies on psychological/behavioral treatments for chronic pain in emerging adults (58–61) were identified (see Table 1). Two were on effects of yoga, and another on ACT, both of which demonstrated efficacy in other age-groups (53, 54). Another study (61) was on the effects of autogenic relaxation training (AT), which was used as a comparison condition for physical therapy, an excluded treatment for this review. AT has limited but promising support in other age-groups (65). These studies were published from 2013 onwards, although the literature search was open-ended.
Each of the studies met our inclusion criteria requiring that the MAge ± 1 SD were within 18–29 years, although none of them used the term “emerging adult.” Instead, the term “young adult”, and in the exclusively female study, “young women” was used. Intervention fidelity was monitored to various degrees in all of the studies: weekly monitoring forms (58, 59), weekly follow-up sessions (61), or about 1.5 months before the final assessment at 3 months (60).
All of the studies had small samples focused on one pain type: rheumatoid arthritis (58), irritable bowel syndrome (59), neurofibromatosis type 1 (60), and tension-type headache (61). A variety of chronic pain definitions was used; three of them were clinical definitions for the specific diagnosis (58, 59, 61), while the other study relied on self-report of chronic pain to a nurse practitioner during a physical examination at their most recent visit to the clinic (60).
Random assignment was used in three studies with waitlist treatment-as-usual control groups (58, 59) or an active comparison condition (61). In the ACT study, comparisons were made to the baseline values of the outcome measures. All studies included follow-ups which occurred at two months (58, 59), three months (60), and two assessments at four weeks and three months (61).
At least some concurrent pharmacological treatments were reported in all the studies, but only the relaxation study (54) also reported other nonpharmacological treatments. Two of the studies (58, 59) reported comorbid conditions in their participants.
The studies were conducted in yoga studios (58, 59), in-person clinics (two-day workshop), participants' homes (61), and booster sessions by telephone (60). Interventions were provided by experienced/senior teacher advisors in the yoga studies (58, 59), or specialized therapists (60, 61).
The IASP definition of pain requires that it be assessed in multiple domains, including reports of an individual's experience of pain (62, 67) and include behaviors expressed or not expressed in various clinical and research contexts (67, 68). All the studies assessed more than just reported pain intensity (e.g., visual analogue scale). As shown in Table 1, self-reported pain and pain-related outcomes in these studies included frequency, intensity, and duration of symptoms, as well as ratings of worst pain and average pain, pain functioning, and pain interference. Also included were measures of analgesic use, health-related quality of life, pain acceptance, pain efficacy, mood, anxiety, fatigue, sleep, and mindfulness. Notably, the measures used in the yoga studies (58, 59) assessed the experience of pain (worst pain and average pain in weekly ratings) as well as measures of depression and anxiety, well known to be linked with pain measures (69).
Each of the interventions showed statistically significant effects on pain experiences and several also showed statistically significant results for the secondary measures as shown in Table 1. Pre-post and between-groups findings were reported in the randomized-control trials, which also reported on the clinical significance of findings. The yoga studies (58, 59) used the Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials (IMMPACT: http://www.immpact.org) recommendations (63). One study (61) reported clinical significance of the visual analogue scale (VAS) according to established criteria.
All the studies used designs graded as level II or moderate quality of evidence, a reasonable indication that future studies will replicate this finding (65). Methodologic limitations included internal and external validity issues according to the framework established by the United States Preventive Services Task Force (70), as described in Table 2. Some of these limitations, but not all of them, are typical challenges in psychological/behavioral interventions where participants actively participate in therapy. Internal validity was negatively affected by lack of participant and provider blinding to treatment condition, omission of details on concurrent pharmacological and non-pharmacological pain management, and the potential confounding effects of which were not described and/or analyzed statistically among other flaws. Only two of the studies (59, 61) reported a priori-sample size calculation. Limitations to external validity (Table 2) included small samples. Stringent exclusionary criteria regarding pain type and pain source restricted diversity in the samples. A lack of diversity in providers and settings in which the therapies were conducted also somewhat limit the generalizability of these studies.
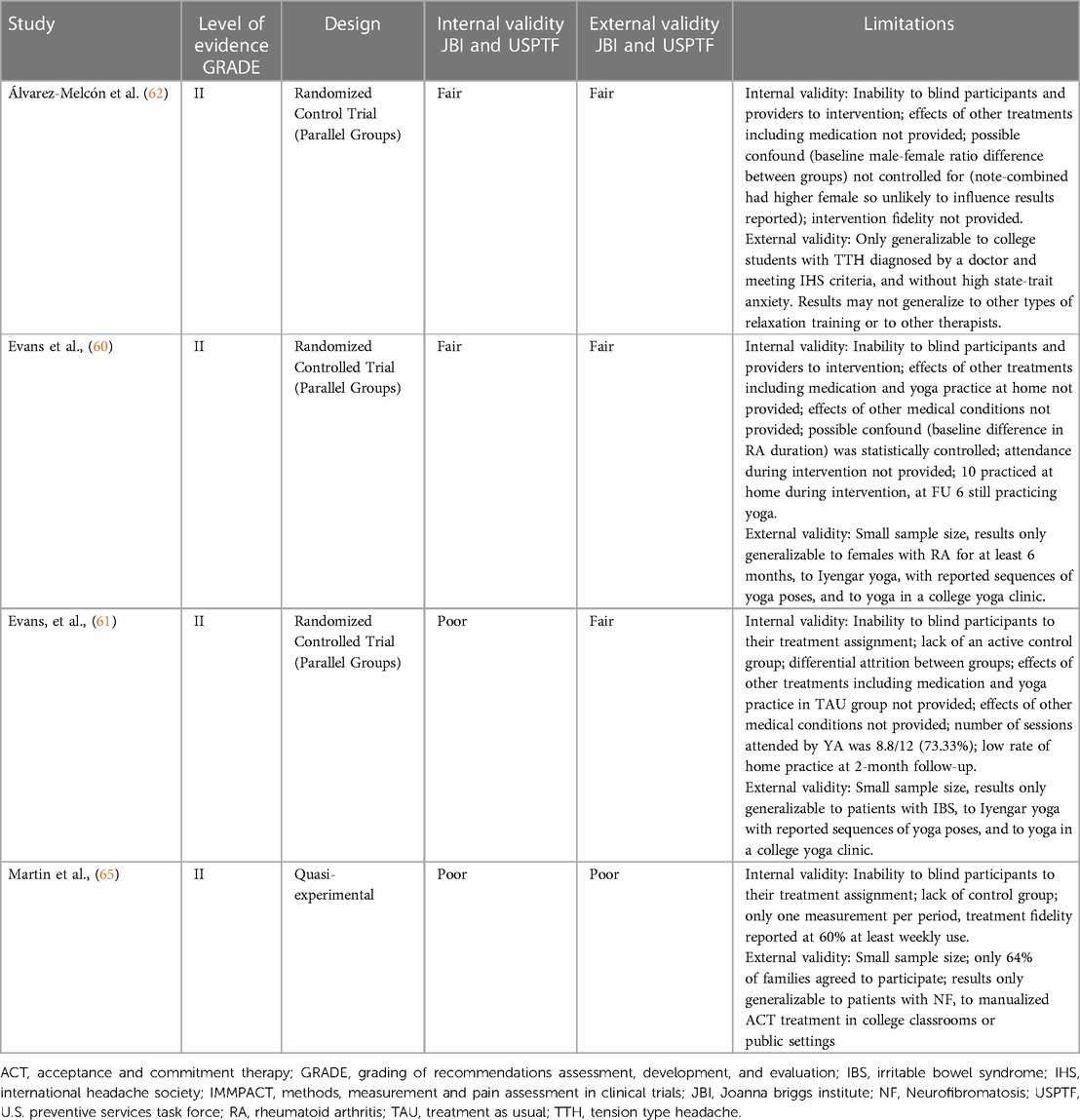
Table 2. Design and methodologic rigor for studies of psychological/behavioral interventions in emerging adults.
4 Discussion
The lack of intervention research in emerging adults with chronic pain is due, in part, to the fact that this population is challenging to recruit and access (5). The reasons for this are complex, and include young adults' reluctance to self-identify as having chronic pain, especially if they are college athletes (18). Additionally, the perception of stigma appears to drive a lack of help-seeking behaviors within this cohort (71). Effective recruitment of large samples of emerging adults, attending as well as not attending institutions of higher education, is needed.
Although all of the studies reported factors related to pain, future studies within this cohort should attempt to utilize a biopsychosocial model of health in their design: for example, biological (e.g., chronic pain in childhood, family history, sex), lifestyle (e.g., sleep, recreational drug use, physical activity), psychological (e.g., anxiety and depression, stress, pain catastrophizing, pain coping), social (e.g., history of abuse, parental mental health and family functioning) factors as well as those related to pain interference (e.g., restriction to daily activities, social, work and college participation (9). Perceptions of social stigma (72, 73), illness invalidation (71), and perceived injustice (74, 75), also related to the pain experience, should be addressed as well. Given that 5% of emerging adults in the United States identify as transgender/nonbinary, and that transgender individuals report higher pain sensitivity to induced mechanical pain stimuli than cisgender individuals (76), we recommend that future studies of pain treatments in emerging adults include information on both sex and gender identification.
The high prevalence rate of chronic pain in college students compared to the general public warrants further research. Understanding risk factors such as participation in college athletics (16, 77) and mental health vulnerabilities like depression and anxiety may help to develop interventions that can help mitigate or prevent persistent pain in emerging adults (14). Psychological interventions with known benefits to mental health in other age groups may help emerging adults with chronic pain whether or not they attend college. Also unknown is the prevalence of foregoing college or professional sports due to chronic pain and the possibility of differential rates of chronic pain in emerging adults who attend compared to those who do not attend college.
In recent years, the introduction of non-traditional mental healthcare services and tools (e.g., mobile apps, peer counselors, online support groups) has increased access to and utilization of behavioral health services (76, 78). For example, tele-health success is linked with the development of self-efficacy (79), a core need of emerging adults (1, 46). Virtual-reality (36, 50, 80), self-administration (50), and single-session practices (55, 56) may also be beneficial to emerging adults with chronic pain, though empirical studies to evaluate these non-traditional services are needed.
Several major limitations of the reviewed studies include small sample size, inability to blind participants, effects of other treatments including medication not identified, possible confounds not statistically controlled, lack of active comparison groups, and limited generalizability to other pain types (Table 2). Future recommendations from this analysis include the assessment of baseline differences between groups in pain studies (81), and the influence of moderating potentially confounding pharmacological substances and psychological/behavioral activities and treatments. An understanding of these critical factors is important to measure and study the effectiveness of different practices in helping control chronic pain in emerging adults.
5 Conclusion
Despite evidence for the effectiveness of psychological/behavioral interventions in other age-groups, especially for CBT (82), we found only four quantitative studies of such treatments for chronic pain targeting emerging adults (58–61), and none for CBT. Whereas these studies showed positive effects of the interventions (yoga, ACT, and relaxation) on pain outcomes, studies are needed that focus on a wider variety of therapies, diverse populations, and pain types. These studies/therapies must address the unique developmental needs (23, 83, 84) and barriers to accessing treatment (5, 9) in emerging adults. Non-traditional delivery models such as virtual-reality (36, 50, 80), self- administration (50), tele-health (79), and single-session modalities (55, 56) may be especially beneficial.
The stakes are high at both individual and societal levels as many important trajectories in life are established during emerging adulthood. Unfortunately, the road to second chances is narrow with respect to earning college degrees and obtaining jobs where individuals can be self-sustaining members of society. The most important influences on mental health in those with chronic pain are the person's ability to work, and psychosocial factors, such as pain catastrophizing, independent of type of pain and pain intensity (85). Psychosocial factors are highly amenable to improvement with psychological/behavioral therapies. A better understanding of resilience trajectories established by emerging adults with chronic pain and moderator influences, such as psychosocial factors on pain outcomes and pain-related experiences can lead to better access to effective therapies, greater utilization of them, and more effective pain management for emerging adults.
Author contributions
JF: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. SK: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Software, Supervision, Writing – original draft, Writing – review & editing. MF: Conceptualization, Resources, Visualization, Writing – review & editing. MZ: Conceptualization, Formal Analysis, Investigation, Methodology, Project administration, Validation, Visualization, Writing – original draft, Writing – review & editing.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Arnett JJ. Emerging adulthood: a theory of development from the late teens through the twenties. Am Psychol. (2000) 55(5):469–80. doi: 10.1037/0003-066X.55.5.469
2. Schwartz SJ, Petrova M. Prevention science in emerging adulthood: a field coming of age. Prev Sci. (2019) 20(3):305–9. doi: 10.1007/s11121-019-0975-0
3. Cleveland MJ, Goldstein AL. Opportunities and challenges for prevention and intervention in emerging adulthood: introduction to the special issue. Prev Sci. (2019) 20(3):301–4. doi: 10.1007/s11121-019-0976-z
4. Stormshak E, Caruthers A, Chronister K, DeGarmo D, Stapleton J, Falkenstein C, et al. Reducing risk behavior with family-centered prevention during the young adult years. Prev Sci. (2019) 20(3):321–30. doi: 10.1007/s11121-018-0917-2
5. Hill LG. Expanding our horizons: risk, protection, and intervention in emerging adulthood. Prev Sci. (2019) 20(3):385–9. doi: 10.1007/s11121-019-00996-5
6. Treede R-D, Rief W, Barke A, Aziz Q, Bennett MI, Benoliel R, et al. A classification of chronic pain for ICD-11. Pain. (2015) 156(6):1003–7. doi: 10.1097/j.pain.0000000000000160
7. Zelaya CE, Dahlhamer JM, Lucas JW, Connor EM. Chronic pain and high-impact chronic pain among US adults, 2019 NCHS data brief. HCHS. Hyattsville, MD: National Center for Health Statistics (2020). p. 1–8.
8. Murray CB, de la Vega R, Murphy LK, Kashikar-Zuck S, Palermo TM. The prevalence of chronic pain in young adults: a systematic review and meta-analysis. Pain. (2022) 163(9):e972–e84. doi: 10.1097/j.pain.0000000000002541
9. Brown D, Schenk S, Genent D, Zernikow B, Wager J. A scoping review of chronic pain in emerging adults. Pain Reports. (2021) 6(1):e920. doi: 10.1097/PR9.0000000000000920
10. Robertson D, Kumbhare D, Nolet P, Srbely J, Newton G. Associations between low back pain and depression and somatization in a Canadian emerging adult population. J Can Chiropr Assoc. (2017) 61(2):96–105. 28928493.28928493
11. Çakmak A, Yücel B, Özyalçn SN, Bayraktar B, Ural HI, Duruöz MT, et al. The frequency and associated factors of low back pain among a younger population in Turkey. Spine. (2004) 29(14):1567–72. doi: 10.1097/01.BRS.0000131432.72531.96
12. Grasdalsmoen M, Engdahl B, Fjeld MK, Steingrímsdóttir ÓA, Nielsen CS, Eriksen HR, et al. Physical exercise and chronic pain in university students. PloS One. (2020) 15(6):e0235419. doi: 10.1371/journal.pone.0235419
13. Falavigna A, Teles AR, Mazzocchin T, de Braga GL, Kleber FD, Barreto F, et al. Increased prevalence of low back pain among physiotherapy students compared to medical students. Eur Spine J. (2011) 20:500–5. doi: 10.1007/s00586-010-1646-9
14. Serbic D, Friedrich C, Murray R. Psychological, social and academic functioning in university students with chronic pain: a systematic review. J Am Coll Health. (2023) 71(9):2894–908. doi: 10.1080/07448481.2021.2006199
15. Kim HJ, Boo S, Meeker TJ. Pain prevalence, management and interference among university students in South Korea: an exploratory cross-sectional study. J Pain Res. (2021) 14:2423–31. doi: 10.2147/JPR.S324758
16. Zale EL, Williams CM, Reynolds LR, Mastroleo NR. Examining sex differences in associations between pain and alcohol use among college student-athletes. Subst Use Misuse. (2022) 57(4):539–47. doi: 10.1080/10826084.2021.2019784
17. Friery K, Bishop P. Long-term impact of athletic participation on physical capabilities. J Exer Physiol Online. (2007) 10(1):34–47.
18. Montgomery TL. No Pain no Gain: Perceived Pain and Injury Reporting in College Athletes and Exercisers [Doctoral Dissertation]. Proquest: Saint Louis University (2017).
19. Zale EL, LaRowe LR, Boissoneault J, Maisto SA, Ditre JW. Gender differences in associations between pain-related anxiety and alcohol use among adults with chronic pain. Am J Drug Alcohol Abuse. (2019) 45(5):479–87. doi: 10.1080/00952990.2019.1578968
20. Schulenberg JE, Sameroff AJ, Cicchetti D. The transition to adulthood as a critical juncture in the course of psychopathology and mental health. Dev Psychopathol. (2004) 16(4):799–806. doi: 10.1017/s0954579404040015
21. Arnett JJ. College students as emerging adults: the developmental implications of the college context. Emerg Adulthood. (2016) 4(3):219–22. doi: 10.1177/2167696815587422
22. Rosenbloom BN, Rabbitts JA, Palermo TM. A developmental perspective on the impact of chronic pain in late adolescence and early adulthood: implications for assessment and intervention. Pain. (2017) 158(9):1629–32. doi: 10.1097/j.pain.0000000000000888
23. Stinson J, White M, Isaac L, Campbell F, Brown S, Ruskin D, et al. Understanding the information and service needs of young adults with chronic pain: perspectives of young adults and their providers. Clin J Pain. (2013) 29(7):600–12. doi: 10.1097/AJP.0b013e31826dce65
24. Key substance use and mental health indicators in the United States. Quality CfBHSa. Rockville, MD: Substance Abuse and Mental Health Services Administration (2021). p. 1–156.
25. Anastas T, Colpitts K, Ziadni M, Darnall BD, Wilson AC. Characterizing chronic pain in late adolescence and early adulthood: prescription opioids, marijuana use, obesity, and predictors for greater pain interference. Pain Rep. (2018) 3(6):e700. doi: 10.1097/PR9.0000000000000700
26. Feldman DE, Nahin RL. National estimates of chronic musculoskeletal pain and its treatment in children, adolescents, and young adults in the United States: data from the 2007–2015 national ambulatory medical care survey. J Pediatr. (2021) 233:212–9e1. doi: 10.1016/j.jpeds.2021.01.055
27. Shorey Fennell B, Magnan RE, Ladd BO, Fales JL. Young adult Cannabis users’ perceptions of Cannabis risks and benefits by chronic pain Status. Subst Use Misuse. (2022) 57(11):1647–52. doi: 10.1080/10826084.2022.2102186
28. Gustavson K, Knudsen AK, Nesvåg R, Knudsen GP, Vollset SE, Reichborn-Kjennerud T. Prevalence and stability of mental disorders among young adults: findings from a longitudinal study. BMC Psychiatry. (2018) 18(1):1–15. doi: 10.1186/s12888-018-1647-5
29. Mental Health by the Numbers. Available online at: https://www.nami.org/mhstats (accessed June 1, 2023).
30. Sheidow AJ, McCart M, Zajac K, Davis M. Prevalence and impact of substance use among emerging adults with serious mental health conditions. Psychiatr Rehabil J. (2012) 35(3):235–43. doi: 10.2975/35.3.2012.235.243
31. Wijma AJ, van Wilgen CP, Meeus M, Nijs J. Clinical biopsychosocial physiotherapy assessment of patients with chronic pain: the first step in pain neuroscience education. Physiother Theory Pract. (2016) 32(5):368–84. doi: 10.1080/09593985.2016.1194651
32. Reif S, Karriker-Jaffe KJ, Valentine A, Patterson D, Mericle AA, Adams RS, et al. Substance use and misuse patterns and disability status in the 2020 U.S. National alcohol survey: a contributing role for chronic pain. Disabil Health J. (2022) 15(2):101290. doi: 10.1016/j.dhjo.2022.101290
33. Sherrell D, Trost Z, Marmorstein N. Examining the longitudinal association between adolescent pain and alcohol use. J Pain. (2018) 19(3):S59. doi: 10.1016/j.jpain.2017.12.151
34. Matamala AM, Hanna M, Perrot S, Varrassi G, Montero A. Avoid postoperative pain to prevent its chronification: a narrative review. Cureus. (2022) 14(2):1–8. doi: 10.7759/cureus.22243
35. Ten Doesschate SF, Kuijper TM, Koopman SS, Mol S, Colen-Kroon L, Brown VV. Pain severity at emergency department discharge as a predictor for chronification of pain. Pain Reports. (2022) 7(6):e1048. doi: 10.1097/PR9.0000000000001048
36. Wren AA, Neiman N, Caruso TJ, Rodriguez S, Taylor K, Madill M, et al. Mindfulness-based virtual reality intervention for children and young adults with inflammatory bowel disease: a pilot feasibility and acceptability study. Children. (2021) 8(5):368. doi: 10.3390/children8050368
37. Firmin MW, Burger AJ, Grigsby ME, Sherman AL, Croft JN. Coping constructs related to college students with chronic pain. J Ethnographic Qual Res. (2011) 6(1):32–44.
38. Rogers AH, Bakhshaie J, Lam H, Langdon KJ, Ditre JW, Zvolensky MJ. Pain-related anxiety and opioid misuse in a racially/ethnically diverse young adult sample with moderate/severe pain. Cogn Behav Ther. (2018) 47(5):372–82. doi: 10.1080/16506073.2018.1436085
39. Fales JL, Ladd BO, Magnan RE. Pain relief as a motivation for cannabis use among young adult users with and without chronic pain. J Pain. (2019) 20(8):908–16. doi: 10.1016/j.jpain.2019.02.001
40. Bennett T, Holloway K. Motives for illicit prescription drug use among university students: a systematic review and meta-analysis. Int J Drug Policy. (2017) 44:12–22. doi: 10.1016/j.drugpo.2017.02.012
41. McCabe SE, Schulenberg JE, O'Malley PM, Patrick ME, Kloska DD. Non-medical use of prescription opioids during the transition to adulthood: a multi-cohort national longitudinal study. Addiction. (2014) 109(1):102–10. doi: 10.1111/add.12347
42. Ellingson R, Wilson R, Bisson EJ, Goldie CL. Investigating specialized chronic pain care among emerging adults. Pain Manag Nurs. (2022) 23(2):188–95. doi: 10.1016/j.pmn.2021.05.013
43. Prescription opioids. Prevention CfDCa. Available online at: https://www.cdc.gov/opioids/basics/prescribed.html
44. Lee M, Silverman SM, Hansen H, Patel VB, Manchikanti L. A comprehensive review of opioid-induced hyperalgesia. Pain Physician. (2011) 14(2):145. doi: 10.36076/ppj.2011/14/145
45. What is the opioid epidemic? Services HaH. (2017). Available online at https://www.cdc.gov/opioids/basics/prescribed.html (accessed June 1, 2023).
46. Arnett JJ, Mitra D. Are the features of emerging adulthood developmentally distinctive? A comparison of ages 18–60 in the United States. Emerg Adulthood. (2018) 8(5):412–9. doi: 10.1177/2167696818810073
47. Sharpe L. “First do no harm”: why don't we measure adverse events routinely in psychological treatment trials for people with chronic pain? Pain. (2020) 161(4):666–7. doi: 10.1097/j.pain.0000000000001771
48. Darnall BD, Mackey SC, Lorig K, Kao MC, Mardian A, Stieg R, et al. Comparative effectiveness of cognitive behavioral therapy for chronic pain and chronic pain self-management within the context of voluntary patient-centered prescription opioid tapering: the EMPOWER study protocol. Pain Med. (2020) 21(8):1523–31. doi: 10.1093/pm/pnz285
49. Seminowicz DA, Shpaner M, Keaser ML, Krauthamer GM, Mantegna J, Dumas JA, et al. Cognitive-behavioral therapy increases prefrontal cortex gray matter in patients with chronic pain. J Pain. (2013) 14(12):1573–84. doi: 10.1016/j.jpain.2013.07.020
50. Garcia L, Birckhead B, Krishnamurthy P, Sackman J, Mackey I, Louis RG, et al. Double-blind, randomized placebo-controlled trial of 8-week self-administered at-home behavioral skills-based virtual reality (VR) for chronic low back pain (during COVID-19). J Med Internet Res. (2021) 23(2):1–35. doi: 10.2196/26292
51. Trindade IA, Guiomar R, Carvalho SA, Duarte J, Lapa T, Menezes P, et al. Efficacy of online-based acceptance and commitment therapy for chronic pain: a systematic review and meta-analysis. J Pain. (2021) 22(11):1328–42. doi: 10.1016/j.jpain.2021.04.003
52. Pardos-Gascón EM, Narambuena L, Leal-Costa C, van-der Hofstadt-Román CJ. Differential efficacy between cognitive-behavioral therapy and mindfulness-based therapies for chronic pain: systematic review. Int J Clin Health Psychol. (2020) 21(1):100197. doi: 10.1016/j.ijchp.2020.08.001
53. Anheyer D, Haller H, Lauche R, Dobos G, Cramer H. Yoga for treating low back pain: a systematic review and meta-analysis. Pain. (2022) 163(4):e504–e17. doi: 10.1097/j.pain.0000000000002416
54. Du S, Dong J, Jin S, Zhang H, Zhang Y. Acceptance and commitment therapy for chronic pain on functioning: a systematic review of randomized controlled trials. Neurosci Biobehav Rev. (2021) 131:59–76. doi: 10.1016/j.neubiorev.2021.09.022
55. Ziadni MS, Gonzalez-Castro L, Anderson S, Krishnamurthy P, Darnall BD. Efficacy of a single-session “empowered relief” zoom-delivered group intervention for chronic pain: randomized controlled trial conducted during the COVID-19 pandemic. J Med Internet Res. (2021) 23(9):e29672. doi: 10.2196/29672
56. Darnall BD, Roy A, Chen AL, Ziadni MS, Keane RT, You DS, et al. Comparison of a single-session pain management skills intervention with a single-session health education intervention and 8 sessions of cognitive behavioral therapy in adults with chronic low back pain: a randomized clinical trial. JAMA Network Open. (2021) 4(8):e2113401. doi: 10.1001/jamanetworkopen.2021.13401
57. Treede R-D, Rief W, Barke A, Aziz Q, Bennett MI, Benoliel R, et al. Chronic pain as a symptom or a disease: the IASP classification of chronic pain for the international classification of diseases (ICD-11). Pain. (2019) 160(1):19–27. doi: 10.1097/j.pain.0000000000001384
58. Evans S, Moieni M, Lung K, Tsao J, Sternlieb B, Taylor M, et al. Impact of iyengar yoga on quality of life in young women with rheumatoid arthritis. Clin J Pain. (2013) 29(11):988–97. doi: 10.1097/AJP.0b013e31827da381
59. Evans S, Lung KC, Seidman LC, Sternlieb B, Zeltzer LK, Tsao JC. Iyengar yoga for adolescents and young adults with irritable bowel syndrome. J Pediatr Gastroenterol Nutr. (2014) 59(2):244–53. doi: 10.1097/MPG.0000000000000366
60. Martin S, Wolters PL, Toledo-Tamula MA, Schmitt SN, Baldwin A, Starosta A, et al. Acceptance and commitment therapy in youth with neurofibromatosis type 1 (NF1) and chronic pain and their parents: a pilot study of feasibility and preliminary efficacy. Am J Med Genet A. (2016) 170(6):1462–70. doi: 10.1002/ajmg.a.37623
61. Álvarez-Melcón A, Valero-Alcaide R, Atín-Arratibel M, Melcón-Álvarez A, Beneit-Montesinos J. Effects of physical therapy and relaxation techniques on the parameters of pain in university students with tension-type headache: a randomised controlled clinical trial. Neurología. (2018) 33(4):233–43. doi: 10.1016/j.nrl.2016.06.008
62. Nicholas M, Vlaeyen JW, Rief W, Barke A, Aziz Q, Benoliel R, et al. The IASP classification of chronic pain for ICD-11: chronic primary pain. Pain. (2019) 160(1):28–37. doi: 10.1097/j.pain.0000000000001390
63. Dworkin RH, Turk DC, Farrar JT, Haythornthwaite JA, Jensen MP, Katz NP, et al. Core outcome measures for chronic pain clinical trials: iMMPACT recommendations. Pain. (2005) 113(1):9–19. doi: 10.1016/j.pain.2004.09.012
64. Kelly AD. The minimally significant differences in visual analogue scale pan score does not differ with severity of pain. Emerg Med J. (2001) 18:205–7. doi: 10.1136/emj.18.3.205
65. Kohlert A, Wick K, Rosendahl J. Autogenic training for reducing chronic pain: a systematic review and meta-analysis of randomized controlled trials. Int J Behav Med. (2022) 29(5):531–42. doi: 10.1007/s12529-10038-6
66. JBI Checklists Joanna Briggs Institute. (2017). Checklist for systematic reviews and research syntheses. Available online at: https://joannabriggs.org/ebp/critical_appraisal_tools (accessed June 1, 2023).
67. Raja SN, Carr DB, Cohen M, Finnerup NB, Flor H, Gibson S, et al. The revised IASP definition of pain: concepts, challenges, and compromises. Pain. (2020) 161(9):1976–82. doi: 10.1097/j.pain.0000000000001939
68. Williams ACC, Craig KD. Updating the definition of pain. Pain. (2016) 157(11):2420–3. doi: 10.1097/j.pain.0000000000000613
69. Mei Q, Li C, Yin Y, Wang Q, Wang Q, Deng G. The relationship between the psychological stress of adolescents in school and the prevalence of chronic low back pain: a cross-sectional study in China. Child Adolesc Psychiatry Ment Health. (2019) 13(1):1–10. doi: 10.1186/s13034-018-0261-0
70. U.S. Preventive services task force procedure manual. Quality AfHRa. Rockville, MD (2021). p. 1–81.
71. Kapoor S. Perceived Stigma, Illness Invalidation, Sleep Difficulties, and Psychological Distress in Emerging Adults in College with Persistent Pain [Doctoral Dissertation]. Tuscaloosa, Alabama: University of Alabama (2015).
72. Davenport JK. Stigma and Disclosure of Chronic Pain in Higher Education: A Qualitative Study [Doctoral Dissertation]. Proquest: University of Arkansas (2020).
73. De Ruddere L, Craig KD. Understanding stigma and chronic pain: a-state-of-the-art review. Pain. (2016) 157(8):1607–10. doi: 10.1097/j.pain.0000000000000512
74. Penn TM, Overstreet DS, Aroke EN, Rumble DD, Sims AM, Kehrer CV, et al. Perceived injustice helps explain the association between chronic pain stigma and movement-evoked pain in adults with nonspecific chronic low back pain. Pain Med. (2020) 21(11):3161–71. doi: 10.1093/pm/pnaa095
75. Ziadni MS, You DS, Sturgeon JA, Mackey SC, Darnall BD. Perceived injustice mediates the relationship between perceived childhood neglect and current function in patients with chronic pain: a preliminary pilot study. J Clin Psychol Med Settings. (2020) 28:349–60. doi: 10.1007/s10880-020-09722-8
76. Strath LJ, Sorge RE, Owens MA, Gonzalez CE, Okunbor JI, White DM, et al. Sex and gender are not the same: why identity is important for people living with HIV and chronic pain. J Pain Res. (2020) 13:829–35. doi: 10.2147/JPR.S248424
77. Friery KB. Long-Term Impact of Athletic Participation on Physical Capabilities. The University of Alabama (2005).
78. Cohen KA, Stiles-Shields C, Winquist N, Lattie EG. Traditional and nontraditional mental healthcare services: usage and preferences among adolescents and younger adults. J Behav Health Serv Res. (2021) 48(4):1–17. doi: 10.1007/s11414-020-09746-w
79. Fernandes LG, Devan H, Fioratti I, Kamper SJ, Williams CM, Saragiotto BT. At my own pace, space, and place: a systematic review of qualitative studies of enablers and barriers to telehealth interventions for people with chronic pain. Pain. (2022) 163(2):e165–e81. doi: 10.1097/j.pain.0000000000002364
80. Hoag JA, Karst J, Bingen K, Palou-Torres A, Yan K. Distracting through procedural pain and distress using virtual reality and guided imagery in pediatric, adolescent, and young adult patients: randomized controlled trial. J Med Internet Res. (2022) 24(4):e30260. doi: 10.2196/30260
81. Tufanaru C, Munn Z, Aromataris E, Campbell J, Hopp L. Systematic Reviews of Effectiveness. Australia: Joanna Briggs Institute reviewer’s manual: The Joanna Briggs Institute Adelaide (2017). p. 3–10.
82. Williams ACC, Fisher E, Hearn L, Eccleston C. Psychological therapies for the management of chronic pain (excluding headache) in adults. Cochrane Database Syst Rev. (2020) 8:CD007407. doi: 10.1002/14651858.CD007407.pub4
83. Schenk S, Genent D, Hartenstein-Pinter A, Zernikow B, Wager J. Specific therapy needs of young adults with chronic pain: results of a qualitative interview study. Der Schmerz. (2022) 37(1):41–51. doi: 10.1007/s00482-021-00617-7
84. Twiddy H, Hanna J, Haynes L. Growing pains: understanding the needs of emerging adults with chronic pain. Br J Pain. (2017) 11(3):108–18. doi: 10.1177/2049463717709641
Keywords: emerging adult, chronic pain, psychological, pain intervention, mini-review
Citation: Foy JG, Kechichian S, Foy MR and Ziadni M (2024) Psychological/behavioral interventions for emerging adults with chronic pain. Front. Pain Res. 5:1253700. doi: 10.3389/fpain.2024.1253700
Received: 6 July 2023; Accepted: 13 February 2024;
Published: 27 February 2024.
Edited by:
Geoffrey Dover, Concordia University, CanadaReviewed by:
Daniel Wolfe, Concordia University, CanadaBrent Rosenstein, Concordia University, Canada
© 2024 Foy, Kechichian, Foy and Ziadni. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Judith G. Foy anVkaXRoLmZveUBsbXUuZWR1
 Judith G. Foy
Judith G. Foy Sandra Kechichian2
Sandra Kechichian2 Maisa Ziadni
Maisa Ziadni